- 1Center for Sleep Medicine, Cliniques Universitaires Saint Luc, Université Catholique de Louvain, Brussels, Belgium
- 2Cliniques Universitaires Saint Luc, Université Catholique de Louvain, Brussels, Belgium
Objective: This retrospective study aimed to address acceptance and long-term adherence to Continuous Positive Airway Pressure (CPAP) treatment among non-responder patients to ImThera THN system who initially declined this therapy.
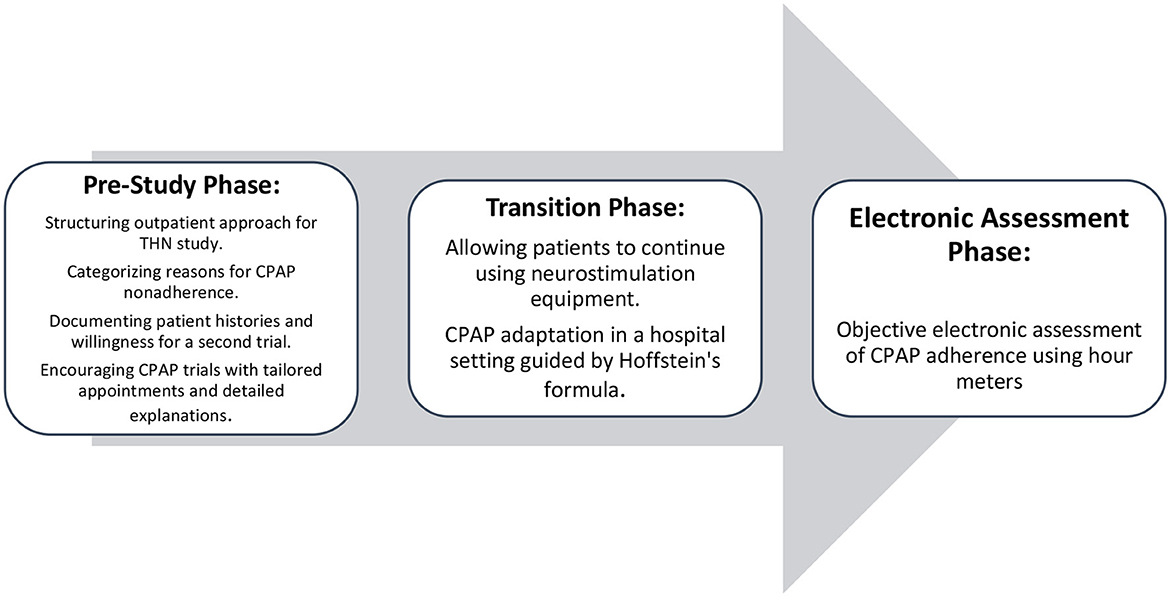
Material and methods: We employed a structured outpatient approach to communicate THN study results, categorize initial CPAP nonadherence reasons, and encourage CPAP trials through tailored appointments. Recorded follow-ups addressed individual concerns, providing medical guidance and acknowledging person-specific challenges. Adherence data were collected using CPAP hour meters at predetermined intervals, following Belgium's social security stipulations.
Results: Between July 2014 and October 2016, eleven participants, including one woman, with prior CPAP experience (average 2 months) were enrolled. Initial non-adherence was linked to ENT or psychological factors. Ten patients agreed to CPAP trials, where interventions included changing CPAP brand, pressure adjustments, mask changes, and additional measures like cognitive-behavioral therapy and nasal spray. After 1 year, mean adherence was 6.3 ± 2 h/day, and average CPAP usage duration was 8.67 ± 2.13 years. As of November 2023, eight out of eleven patients were still actively using CPAP
Conclusion: In this investigation, we challenged the concept of CPAP non-adherence, highlighting evolving adherence and the significance of continuous monitoring and personalized interventions. Our findings underscore ongoing patient education, multidisciplinary support, and dynamic intervention adaptation for enhanced adherence in challenging patient populations. The results provide insights applicable to non-adherent patients with obstructive sleep apnea, emphasizing the importance of individualized care and sustained engagement for improved CPAP acceptance.
1 Introduction
Obstructive Sleep Apnea Syndrome (OSAS) imposes a significant global health burden, characterized by recurrent episodes of upper airway collapse during sleep, leading to intermittent hypoxemia, fragmented sleep, and excessive daytime sleepiness (Peppard et al., 2013). Continuous Positive Airway Pressure (CPAP) therapy is the gold standard treatment for OSAS, effectively mitigating symptoms and improving overall quality of life, but its efficacy heavily relies on patient adherence (Patil et al., 2024). Unfortunately, a substantial proportion of individuals struggle with long-term adherence (Barbé et al., 2001). Side effects and discomfort associated with the mask and air pressure lead many patients to discontinue CPAP (Rotty et al., 2021). Additionally, continuous education and support are crucial, as personalized approaches such as selecting appropriate masks and managing leaks can significantly improve adherence (Leemans et al., 2018). Socioeconomic barriers, physical discomfort, and patient mistrust also contribute to low adherence rates, highlighting the need for personalized medicine and patient-centered approaches (Leemans et al., 2018; Gentina et al., 2023). Multidisciplinary clinics that offer personalized treatment solutions have been shown to significantly decrease non-adherence rates (Masoud et al., 2020; Taweesedt et al., 2022). Leveraging technology, such as wearable devices and interactive education, can enhance patient adherence and outcomes in sleep medicine (Falcone et al., 2014). Moreover, close patient interactions and engagement, including regular face-to-face meetings and thorough monitoring, are critical for improving adherence and achieving long-term success in OSA treatment (Bouloukaki et al., 2014).
In clinical practice and research literature, there is often a notable emphasis on reporting positive treatment outcomes, which can obscure our understanding of the true clinical landscape and hinder efforts to develop tailored management strategies for patients who do not respond favorably to therapy (Ioannidis, 2005). While primary treatment modalities such as CPAP are extensively studied, comparatively little attention is devoted to alternative interventions and their outcomes in non-responsive patients. Among these alternative interventions, targeted hypoglossal nerve stimulation (THN) has emerged as a promising therapeutic option for individuals intolerant of or non-compliant with CPAP therapy (Mwenge et al., 2013). THN operates by delivering electrical stimulation to the hypoglossal nerve, promoting tongue protrusion, and upper airway patency during sleep. Initial studies have shown promising results in reducing the apnea-hypopnea index (AHI) and improving sleep parameters, yet the efficacy of THN remains variable across patient populations, with certain individuals failing to achieve clinically significant improvement (Schwartz et al., 2023).
It is crucial to understand why CPAP, a proven effective treatment, did not work in patients who did not respond to hypoglossal nerve stimulation (THN), in order to address clinical challenges. Although advances in CPAP technology are numerous, they have not demonstrated an overall improvement in adherence (Kim et al., 2009; Hwang et al., 2018; Benjafield et al., 2019). This retrospective study explores the dynamics of acceptance and adherence in OSA treatment, focusing on patients initially resistant to CPAP therapy who later participated in THN studies. We hypothesize that if these technological advancements are applied in a personalized manner, they could enhance adherence to CPAP therapy among initially non-compliant patients. By retrospectively examining these factors, we aim to provide valuable insights into improving treatment adherence and outcomes for patients with OSAS, ultimately contributing to enhanced clinical practices and patient care.
2 Material and methods
2.1 Study design
This retrospective observational study assessed patients with an ImThera THN system who failed to achieve a significant reduction in the Apnea-Hypopnea Index (AHI) below 30 after 12 months. The timeline of the study is illustrated in Figure 1.
2.2 Patient selection
At Cliniques Universitaires Saint Luc, we conducted two studies on Targeted Hypoglossal Nerve Stimulation (THN) using the aura6000™ system, which stimulates nerve segments to activate dilator muscles. Inclusion criteria were a baseline Apnea-Hypopnea Index (AHI) of ≥20 events·h−1, refusal of CPAP therapy, BMI between 25 and 40 kg·m−2, age between 25 and 70 years, a modified Mallampati score of I to III, and palatine tonsils graded as 0, 1, or 2. Selection was independent of apnea or hypopnea indices.
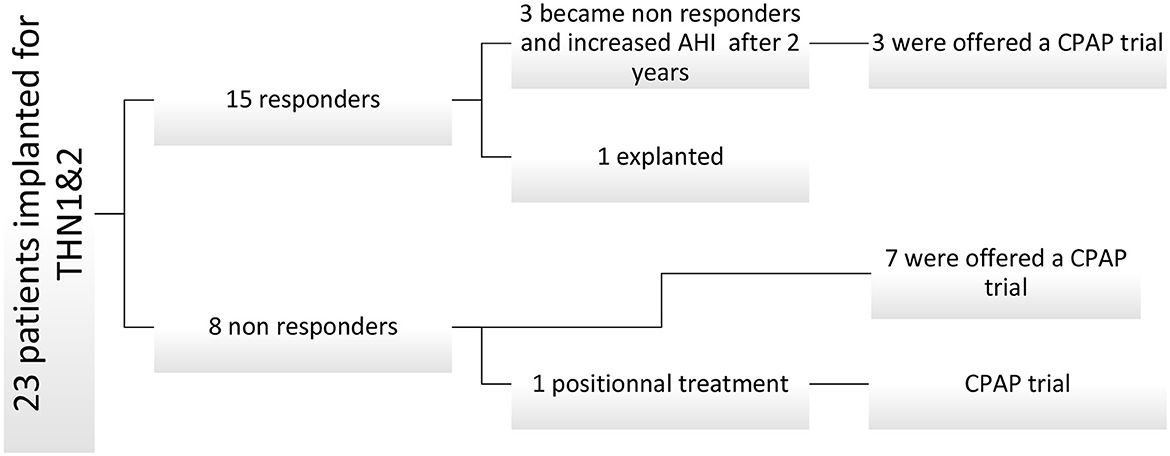
In our center, 23 patients received THN implants. Fifteen met responder criteria, achieving an AHI below thirty events per hour. Post-THN studies revealed subjective symptoms in three patients, resulting in unsuccessful AHI reduction attempts. In three patients, stimulation ceased after 3 years due to a fibrinoleukocyte membrane hindering electrode-nerve contact. Subsequently, eleven patients explored CPAP as an alternative (see Figure 2).
2.3 Data collection
Data were collected from medical records, focusing on reasons for initial CPAP non-adherence and demographic characteristics. Key variables included polysomnography parameters and types of interventions for modifying CPAP and adherence.
2.4 Patient monitoring
During each visit and in the absence of alternatives, patients were encouraged to continue CPAP therapy. The number of outpatient visits post-study before accepting CPAP was closely monitored.
2.5 CPAP adaptation
Patients were hospitalized for 3 days for adaptation. They were supervised and could report any tolerance difficulties if present. Mask selection was tailored, and the effective pressure was determined by Hoffstein's formula (Lacedonia et al., 2012), starting 4 cm of water lower, with a ramp of at least 15 min. Expiratory pressure relief (EPR) was applied if necessary, either during the ramp or throughout the night. Polysomnography was utilized to assess treatment effectiveness.
2.6 Follow-up
Device usage data were collected at each follow-up appointment and reported after 1 year. This includes the device reading date, total usage hours, and patient compliance, calculated as total CPAP usage hours divided by days since treatment began. We also recorded the number of patients continuing treatment in December 2023 and the average compliance over 365 days.
2.7 Statistical analysis
The data were analyzed using descriptive statistics, including mean and median ± SD presentation. Paired t-tests were employed to assess baseline and follow-up differences, while Chi-squared tests were utilized for discontinuous variables. Statistical analysis was conducted using SPSS Statistics 23.
3 Results
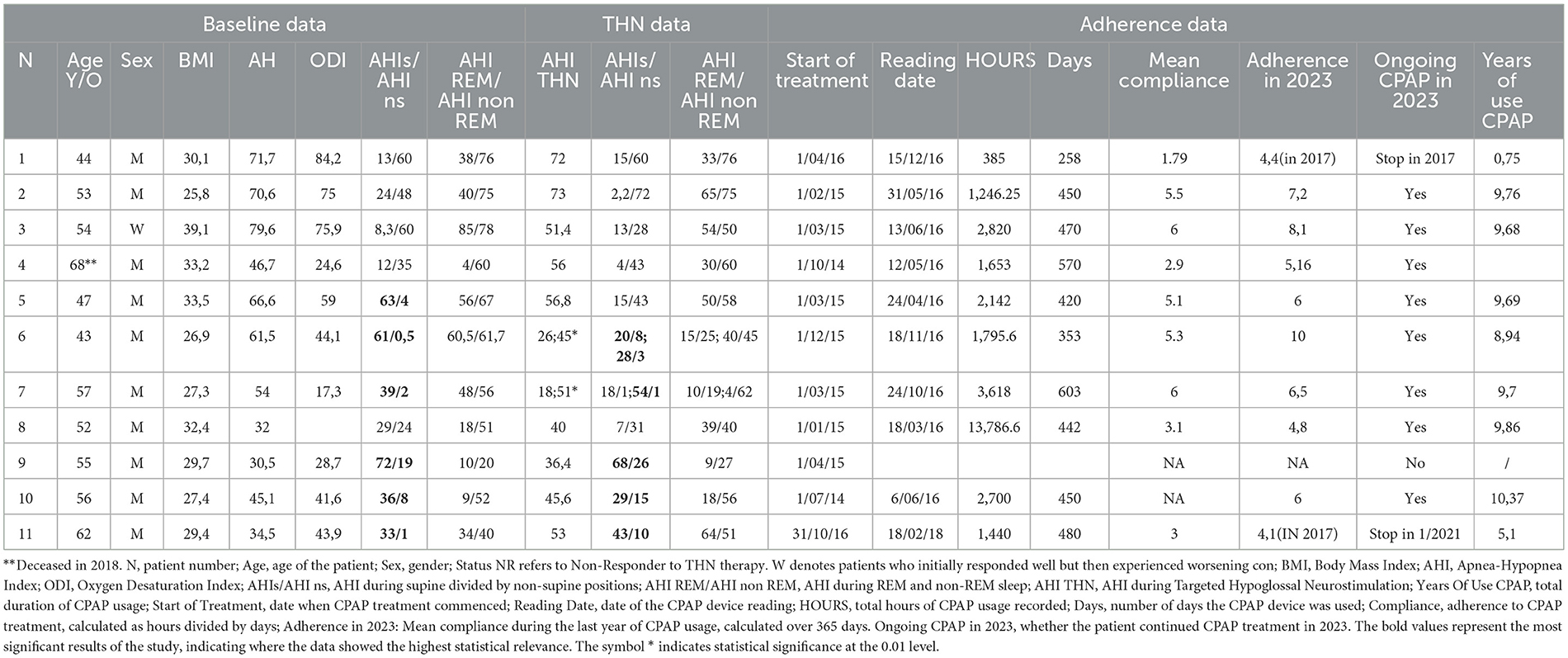
Table 1 describes the characteristics of patients, baseline polysomnography data, and adherence data.
In this study, eleven patients (one woman) were monitored. The baseline mean AHI was 54.9 ± 14. Six patients had positional sleep apnea, which persisted after neurostimulation. No patients had predominance associated with REM sleep events. The mean THN AHI was 47 ± 12.
All patients had ENT evaluations, including endoscopy and rhinomanometry, before the study. After detailed explanations, 10 out of 11 patients agreed to CPAP trials between July 2014 and October 2016, with a mean of 2.3 outpatient visits before acceptance. After 1 year, 8 out of 10 patients used CPAP for over 4 h. One patient stopped after 9 months, and another after 5 years, with average usage close to 4 h. As of November 2023, 8 patients continued CPAP with a mean usage of 8.67 ± 2.13 years and a mean adherence of 6.9 ± 1.4 h per day.
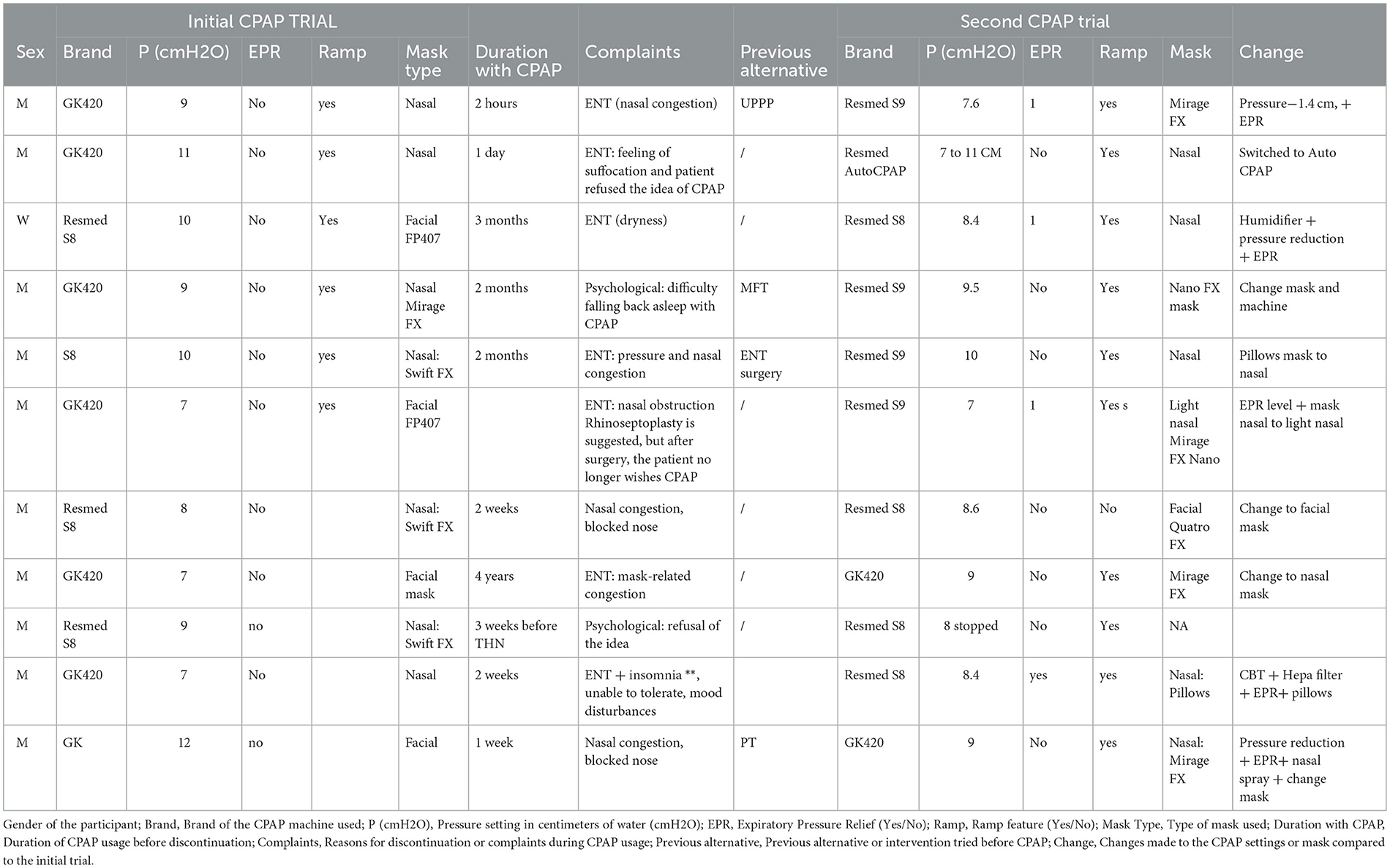
Table 2 patient experience and interventions in CPAP therapy: initial and second trials.
Participants had prior CPAP experience averaging 2 months (range: 2 h to 4 years). They faced side effects such as nasal congestion, suffocation feelings, dryness, difficulty sleeping, pressure, and nasal obstruction. Common complaints included pressure and nasal congestion, sometimes leading to rhinoseptoplasty, and persistent nasal obstruction despite CPAP use. Psychological factors like CPAP refusal, mood disturbances, and insomnia were also observed.
During the second CPAP trial, interventions included changing CPAP brand, pressure adjustments, mask changes, cognitive-behavioral therapy, and nasal spray use. There were seven mask changes, pressure adjustments for four patients, and Expiratory Pressure Relief added for four. Most patients changed machines, with one retaining a humidifier and another switching to Autocpap.
Despite no ENT surgery, side effects either dissipated or were accepted after 2 months. Nasal masks were predominantly used, with nasal pillow masks for two patients.
4 Discussion
Our study aimed to explore the dynamics of acceptance and adherence in the treatment of obstructive sleep apnea (OSA), particularly focusing on patients who initially resisted CPAP therapy and subsequently participated in studies on Hypoglossal Nerve Stimulation. The hypothesis stated in the introduction was that patient-centric approaches and technological advancements could improve adherence to CPAP therapy among initially non-compliant patients.
The results demonstrated that intensive, personalized interventions could significantly enhance adherence to CPAP therapy. At the beginning of the study, the mean Apnea-Hypopnea Index (AHI) was 54.9 ± 14 among the participants, with a mean (THN) AHI of 47 ± 12 after neurostimulation, indicating a high baseline severity of OSA. Notably, six patients presented with positional sleep apnea syndrome, but positional predominance persisted post-neurostimulation. The findings that 10 out of 11 patients agreed to CPAP trials following detailed explanations highlight the importance of patient education and engagement in improving treatment acceptance.
Out of these 10 patients, 8 exhibited compliance exceeding 4 h per night after 1 year of CPAP use, showcasing a marked improvement in adherence compared to their initial resistance. This outcome suggests that non-surgical interventions, coupled with personalized support, can effectively address initial barriers to CPAP adherence in most OSA. In November 2023, eight patients continued with CPAP therapy, with a mean adherence of 6.9 ± 1.4 h per day over 8.67 ± 2.13 years, indicating sustained long-term compliance.
These findings are reinforced by the study conducted by Pépin et al. (2023), which found that 26% of individuals who initially terminated CPAP therapy resumed it within 12 months, with 65% continuing use for at least 1 year. This study also showed a significant reduction in all-cause mortality among patients who resumed CPAP therapy, underscoring the critical importance of offering a second trial of CPAP to ensure effective therapy is not withheld from those who might benefit.
However, our study observed higher adherence rates, partly due to the failure of THN treatment. The lack of success with neurostimulation likely motivated patients to reconsider and commit more seriously to CPAP therapy, resulting in improved adherence rates. This suggests that experiencing failure with an alternative treatment can drive patients to engage more diligently with CPAP therapy, as evidenced by the improved adherence in our study. Most of these patients had already tried other alternatives without success, and the severity of their sleep apnea syndrome offered no other viable options. Their commitment to neurostimulation devices, despite the challenges, underscored the complexity of their conditions and the critical need for effective solutions to their sleep apnea struggles. This may also explain the consistent daily use once the treatment was accepted (El Dib et al., 2015).
The detailed exploration of reasons for initial CPAP discontinuation, such as side effects and discomfort, is consistent with previous findings in the literature (Rotty et al., 2021). Our interventions, which included changing CPAP brands, adjusting pressures, switching masks, and implementing additional measures like cognitive-behavioral therapy and nasal sprays, were effective in mitigating these issues (Ryan et al., 2009; Genta et al., 2020). This aligns with the broader literature emphasizing the importance of personalized approaches and continuous patient support to improve CPAP adherence (Taweesedt et al., 2022).
Unexpectedly, despite no ENT surgery being performed, side effects dissipated or were accepted after 2 months of CPAP use during the second trial. This outcome suggests that non-surgical interventions, coupled with personalized support, can effectively address initial barriers to CPAP adherence. Additionally, the persistence of side effects like nasal congestion and psychological difficulties underscores the need for comprehensive, multidisciplinary approaches to manage OSA treatment effectively (Ryan et al., 2009).
Our findings have several implications for research and clinical practice. The demonstrated effectiveness of patient-centric and technologically advanced approaches in improving CPAP adherence among initially resistant patients provides a valuable framework for developing tailored interventions. This study contributes to the ongoing discourse on optimal therapeutic strategies for OSA, emphasizing the importance of personalized medicine and continuous patient engagement.
However, our study has limitations, including the small sample size and the lack of marital status data (Goosmann et al., 2022), which could influence adherence. The short duration of the initial CPAP experience among participants also limits the generalizability of our findings. Future research should aim to include larger, more diverse populations and explore the long-term impacts of various patient-centric interventions on CPAP adherence.
In conclusion, our study supports the hypothesis that personalized approaches, continuous support, and technological advancements can significantly enhance CPAP adherence among patients initially resistant to therapy. These findings underscore the complexity of managing OSA and advocate for a nuanced, patient-centered approach to treatment, contributing to improved clinical outcomes and patient quality of life.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Université Catholique de Louvain Number 2016/24NOV/503. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
GM: Writing – review & editing, Writing – original draft, Supervision, Software, Methodology, Investigation, Data curation, Conceptualization. JB: Investigation, Conceptualization, Writing – original draft, Writing – review & editing. DR: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frsle.2024.1380373/full#supplementary-material
Abbreviations
CPAP, Continuous Positive Airway Pressure; AHI, Apnea-Hypopnea Index; THN, Targeted Hypoglossal Nerve Stimulation; ENT, Ear, Nose, and Throat; BMI, Body Mass Index; ODI, Oxygen Desaturation Index; ESS, Epworth Sleepiness Scale; SD, Standard Deviation; PSG, Polysomnography.
References
Barbé, F., Mayoralas, L. R., Duran, J., Masa, J. F., Maimó, A., Montserrat, J. M., et al. (2001). Treatment with continuous positive airway pressure is not effective in patients with sleep apnea but no daytime sleepiness: a randomized, controlled trial. Ann. Intern. Med. 134:1015. doi: 10.7326/0003-4819-134-11-200106050-00007
Benjafield, A. V., Pépin, J. L., Valentine, K., Cistulli, P. A., Woehrle, H., Nunez, C. M., et al. (2019). Compliance after switching from CPAP to bilevel for patients with non-compliant OSA: big data analysis. BMJ Open Respir. Res. 6:e000380. doi: 10.1136/bmjresp-2018-000380
Bouloukaki, I., Giannadaki, K., Mermigkis, C., Tzanakis, N., Mauroudi, E., Moniaki, V., et al. (2014). Intensive versus standard follow-up to improve continuous positive airway pressure compliance. Eur. Respir. J. 44, 1262–1274. doi: 10.1183/09031936.00021314
El Dib, R., Jorge, E. C., Kamegasawa, A., Daher, S. R., Spagnuolo, R. S., Silva, M. P. D., et al. (2015). Differences between the real and the desired worlds in the results of clinical trials. Clinics 70, 618–622. doi: 10.6061/clinics/2015(09)04
Falcone, V. A., Damiani, M. F., Quaranta, V. N., Capozzolo, A., and Resta, O. (2014). Polysomnograph chart view by patients: a new educational strategy to improve CPAP adherence in sleep apnea therapy. Respir. Care 59, 193–198. doi: 10.4187/respcare.02491
Genta, P. R., Kaminska, M., Edwards, B. A., Ebben, M. R., Krieger, A. C., Tamisier, R., et al. (2020). The importance of mask selection on continuous positive airway pressure outcomes for obstructive sleep apnea. An official American Thoracic Society workshop report. Ann. Am. Thorac. Soc. 17, 1177–1185. doi: 10.1513/AnnalsATS.202007-864ST
Gentina, T., Gentina, E., Douay, B., Micoulaud-Franchi, J. A., Pépin, J. L., Bailly, S., et al. (2023). Investigating associations between social determinants, self-efficacy measurement of sleep apnea and CPAP adherence: the SEMSA study. Front. Neurol. 14:1148700. doi: 10.3389/fneur.2023.1148700
Goosmann, M., Williams, A. M., Springer, K., and Yaremchuk, K. L. (2022). The impact of marital status and race in obstructive sleep apnea. Ear. Nose Throat J. 2022, 014556132211200. doi: 10.1177/01455613221120068
Hwang, D., Chang, J. W., Benjafield, A. V., Crocker, M. E., Kelly, C., Becker, K. A., et al. (2018). Effect of telemedicine education and telemonitoring on continuous positive airway pressure adherence. the Tele-OSA randomized trial. Am. J Respir. Crit. Care Med. 197, 117–126. doi: 10.1164/rccm.201703-0582OC
Ioannidis, J. P. A. (2005). Why most published research findings are false. PLoS Med. 2:e124. doi: 10.1371/journal.pmed.0020124
Kim, J. H., Kwon, M. S., Song, H. M., Lee, B. J., Jang, Y. J., Chung, Y. S., et al. (2009). Compliance with positive airway pressure treatment for obstructive sleep apnea. Clin. Exp. Otorhinolaryngol. 2, 90–96. doi: 10.3342/ceo.2009.2.2.90
Lacedonia, D., Sabato, R., Carpagnano, G. E., Carrat,ù, P., Falcone, A., Gadaleta, F., et al. (2012). Predictive equations for CPAP titration in OSAS patients. Sleep Breath. 16, 95–100. doi: 10.1007/s11325-010-0461-1
Leemans, J., Rodenstein, D., Bousata, J., and Mwenge, G. B. (2018). Impact of purchasing the CPAP device on acceptance and long-term adherence: a Belgian model. Acta Clin. Belg. 73, 34–39. doi: 10.1080/17843286.2017.1336294
Masoud, O., Ramsay, M., Suh, E.S, Kaltsakas, G., Srivastava, S, Pattani, H., et al. (2020). Long-term adherence to home mechanical ventilation: a 10-year retrospective, single-centre cohort study. J. Thorac. Dis. 12, S120–S128. doi: 10.21037/jtd-cus-2020-003
Mwenge, G. B., Rombaux, P., Dury, M., Lengelé, B., and Rodenstein, D. (2013). Targeted hypoglossal neurostimulation for obstructive sleep apnoea: a 1-year pilot study. Eur. Respir. J. 41, 360–367. doi: 10.1183/09031936.00042412
Patil, S. P., Billings, M. E., Bourjeily, G., Collop, N. A., Gottlieb, D. J., Johnson, K. G., et al. (2024). Long-term health outcomes for patients with obstructive sleep apnea: placing the Agency for Healthcare Research and Quality report in context—a multisociety commentary. J. Clin. Sleep Med. 20, 135–149. doi: 10.5664/jcsm.10832
Pépin, J. L., Tamisier, R., Benjafield, A. V., Rinder, P., Lavergne, F., Josseran, A., et al. (2023). CPAP resumption after a first termination and impact on all-cause mortality in France. Eur. Respir. J. 63:2301171. doi: 10.1183/13993003.01171-2023
Peppard, P. E., Young, T., Barnet, J. H., Palta, M., Hagen, E. W., Hla, K. M., et al. (2013). Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol. 177, 1006–1014. doi: 10.1093/aje/kws342
Rotty, M. C, Suehs, C. M., Mallet, J. P., Martinez, C., Borel, J. C., Rabec, C., et al. (2021). Mask side-effects in long-term CPAP-patients impact adherence and sleepiness: the InterfaceVent real-life study. Respir. Res. 22:17. doi: 10.1186/s12931-021-01618-x
Ryan, S., Doherty, L. S., Nolan, G. M., and McNicholas, W. T. (2009). Effects of heated humidification and topical steroids on compliance, nasal symptoms, and quality of life in patients with obstructive sleep apnea syndrome using nasal continuous positive airway pressure. J. Clin. Sleep Med. 5, 422–427. doi: 10.5664/jcsm.27596
Schwartz, A. R., Jacobowitz, O., Eisele, D. W., Mickelson, S. A., Miller, M. B., Oliven, A., et al. (2023). (2023). Targeted hypoglossal nerve stimulation for patients with obstructive sleep apnea: a randomized clinical trial. JAMA Otolaryngol. Neck Surg. 149:512. doi: 10.1001/jamaoto.2023.0161
Keywords: CPAP, sleep apnea, adherence, target hypoglossal neurostimulation, patient-centered approach
Citation: Mwenge GB, Bousata J and Rodenstein D (2024) Revitalizing CPAP adherence: lessons from THN study in patients with hypoglossal nerve stimulators. Front. Sleep 3:1380373. doi: 10.3389/frsle.2024.1380373
Received: 01 February 2024; Accepted: 05 June 2024;
Published: 05 July 2024.
Edited by:
Prachi Singh, Pennington Biomedical Research Institute, United StatesReviewed by:
Edward C. Mader, Louisiana State University, United StatesDing Zou, University of Gothenburg, Sweden
Copyright © 2024 Mwenge, Bousata and Rodenstein. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gimbada Benny Mwenge, Ym5td2VuZ2VAZ21haWwuY29t
†ORCID: Gimbada Benny Mwenge orcid.org/0000-0001-7392-8078
 Gimbada Benny Mwenge
Gimbada Benny Mwenge Jamila Bousata
Jamila Bousata Daniel Rodenstein
Daniel Rodenstein