- 1Division of Health Sciences, Warwick Medical School, University of Warwick, Coventry, United Kingdom
- 2Department of Psychology, University of Warwick, Coventry, United Kingdom
- 3Turner Institute for Brain and Mental Health, School of Psychological Sciences, Monash University, Melbourne, VIC, Australia
Introduction: Shift work can lead to sleep disturbances and insomnia during the sleeping period, as well as excessive sleepiness and fatigue during the waking period. While Cognitive Behavioral Therapy (CBT-i) is recommended as the first line of treatment for insomnia, key elements of CBT-i, such as maintaining a consistent sleep schedule, can be challenging for shift workers, highlighting the need for tailored sleep interventions. This mini review provides a narrative synthesis of non-pharmacological sleep interventions for shift workers and informs the development of a preventative, multicomponent sleep management programme.
Method: An informal review was conducted in line with Phase 1 of the Framework for the Development and Evaluation of Complex Interventions.
Results: A variety of strategies have been employed to help manage the impacts of shift work on sleep, including: CBT-i, adjusting shift schedules, controlled light exposure, sleep hygiene education, planned napping, caffeine consumption, and mind-body interventions (e.g., yogic relaxation).
Discussion: Recommendations, limitations, and directions for future research are discussed; notably, the role of the family, the commute to and from the workplace, and the eating behaviors of employees appear to have been overlooked in current intervention efforts. Digital CBT-i platforms could help to provide an effective, scalable, and low-cost method of reducing insomnia in shift workers.
1 Introduction
Many organizations rely upon shift workers to maintain round-the-clock services and operations, with shift workers estimated to comprise 20% of the global workforce (Torquati et al., 2019; Booker et al., 2022). While shift schedules may vary greatly, individuals engaged in shift work are often required to work irregular hours and nights, resulting in a changeable sleep-wake pattern at odds with their body-clocks (circadian rhythms) and the world around them (Rajaratnam et al., 2013; Walker et al., 2020). The resulting “circadian misalignment” can lead to excessive sleepiness and fatigue during the waking period, as well as sleep disturbances and insomnia during the sleeping period (Chatterjee and Ambekar, 2017; James et al., 2017; Walker et al., 2020). When accompanied by significant distress and impairment, and not attributable to other underlying causes, these symptoms may be indicative of Shift Work Disorder (SWD), which is estimated to impact 26.5% of shift workers (Pallesen et al., 2021).
In addition to having a negative impact on sleep, circadian misalignment can also have detrimental consequences for physical health and psychological functioning, and has been associated with increased risk of cancer, cardiovascular diseases, and mood disorders (James et al., 2017; Torquati et al., 2019; Sletten et al., 2020; Walker et al., 2020). The effects of circadian misalignment can also be problematic for the workplace, leading to reduced levels of alertness and productivity, higher rates of sickness absence and staff turnover, and increased risk of accident and injury (Wong et al., 2011; Hui and Grandner, 2015; Ryu et al., 2017). Thus, as well as having a significant impact on the individual, the health and safety consequences associated with shift work also present a substantial socioeconomic burden (Culpepper, 2010).
When it comes to tackling insomnia in the general population, Cognitive Behavioral Therapy (CBT-i) is recommended as the first line of treatment (Edinger et al., 2021); however, elements of CBT-i – such as maintaining a consistent sleep schedule and sleep restriction – may not be possible for shift workers who work irregular hours and already experience sleep loss (Reynolds et al., 2022). Night workers who need to sleep during the day may also have difficulty accessing in-person therapies delivered during standard clinical hours. As a result, alternative strategies, such as adjusting shift schedules, controlled light exposure, and sleep hygiene education have been employed to help manage sleep problems in this population (Bragge et al., 2023).
Here, it should be noted that attempts to modify CBT-i for shift workers have been made more recently (Järnefelt et al., 2020), with digital platforms also providing 24/7 access options (Wickwire, 2019). Nevertheless, interventions that consider both the individual and the workplace may be more appropriate for this population, given that cognitive-behavioral factors and the organizational environment are likely to contribute to sleep problems in tandem (Papantoniou et al., 2017; Wong et al., 2019). Indeed, as well as focusing on individual-level factors, CBT-i targets those who are already engaged in shift work and/or already suffer from sleep problems as a result, highlighting the need to provide employees with the skills and knowledge to manage sleep from the outset of employment as part of a preventative approach (Wong et al., 2019).
Despite the existence of multiple strategies, however, efforts to combine and administer them as part of a preventative, multicomponent programme remain scarce, and research evidence for the effectiveness of organizational-level interventions is lacking (Redeker et al., 2019; Bragge et al., 2023). Given the widespread impacts of shift work and the associated costs to the individual, the workplace, and society, a preventative, multicomponent approach may therefore hold promise for improving the health and wellbeing of this population (Papantoniou et al., 2017; Wong et al., 2019).
Accordingly, this mini review aims to provide a concise overview of non-pharmacological interventions for shift workers to inform the development of a preventative, multicomponent sleep management programme in line with Phase 1 of the Framework for the Development and Evaluation of Complex Interventions (Skivington et al., 2021). To direct the review phase, co-authors with expertise in the areas of shift work and sleep pooled insights and relevant articles. Systematic reviews of the literature were explored to identify interventions; discussion papers, narrative reviews, and guidelines were consulted to determine current practice recommendations; and original intervention studies were examined for methodological details.
2 Narrative synthesis
Systematic reviews have explored interventions for shift workers (e.g., Neil-Sztramko et al., 2014; Richter et al., 2016; Robbins et al., 2021; Bragge et al., 2023). The most-to-least frequently implemented strategies include: (1) Adjusting shift schedules; (2) Controlled light exposure; (3) Sleep hygiene education; (4) Planned napping; (5) Caffeine consumption;1 (6) CBT-i; and (7) Mind-body interventions (see Figure 1). A summary of the literature is provided in Supplementary Table 1.
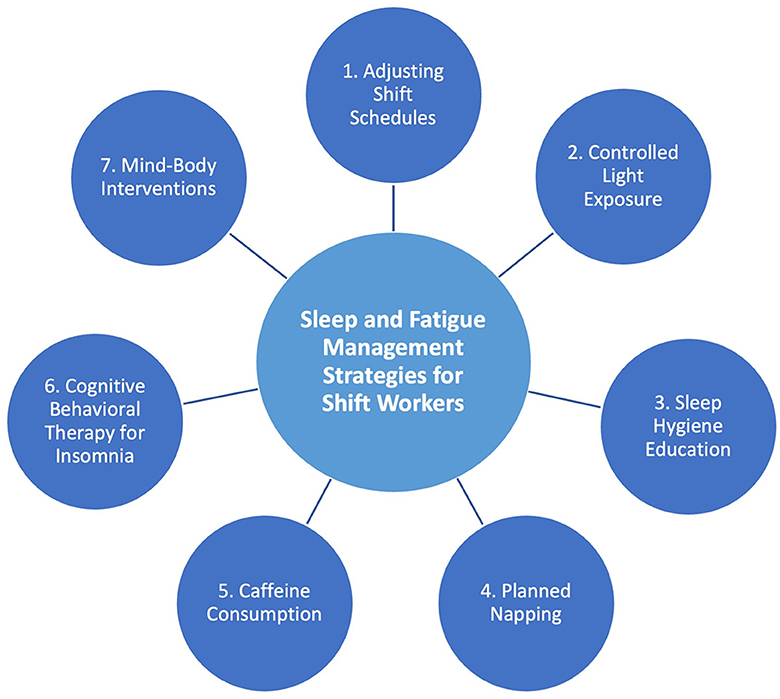
Figure 1. Current non-pharmacological sleep interventions for shift workers, most (1) to least (7) frequently implemented.
2.1 Adjusting shift schedules
Adjusting shift schedules is one of the most frequently employed forms of intervention for shift workers. Here, it should be noted that interventions often modify multiple aspects of the shift in tandem (i.e., direction and speed of rotation, duration), making it difficult to determine the impact of specific adjustments.
2.1.1 Rotation direction
Compared to backwards rotation (Night Shift → Evening Shift → Morning Shift), forwards rotation (Morning Shift → Evening Shift → Night Shift) has been shown to benefit sleep and alertness (Knauth and Hornberger, 2003; Bambra et al., 2008; Sallinen and Kecklund, 2010; Neil-Sztramko et al., 2014; Arlinghaus et al., 2019; Robbins et al., 2021; Bragge et al., 2023). Forward rotation accommodates the delay in timing of the circadian pacemaker and allows longer intervals between shifts, providing more time for recovery sleep and social activity (Garde et al., 2020).
2.1.2 Rotation speed
Compared to slow rotation (7 Morning Shifts → 2 Days Off → 7 Evening Shifts → 2 Days Off → 7 Night Shifts → 2 Days Off), fast rotation (2 Morning Shifts → 2 Evening Shifts → 2 Night Shifts → 2 Days Off) has been shown to improve employee sleep (Knauth and Hornberger, 2003; Bambra et al., 2008; Sallinen and Kecklund, 2010). Fast rotation requires limited adjustment of circadian timing and enables swifter resynchronization to regular biological and social rhythms, while slow rotation makes an individual unavailable for social activity over a greater number of days (i.e., when working 7 consecutive nights; Arlinghaus et al., 2019).
2.1.3 Self-rostering
Giving employees control over their work pattern can help to facilitate positive individual, social, and workplace outcomes by increasing autonomy and reducing stress (Knauth and Hornberger, 2003; Bambra et al., 2008; Garde et al., 2012, 2020; Arlinghaus et al., 2019). Indeed, intervention studies have shown that employees who specify their preferred shift start time, duration, and/or duties, exhibit improved mood, sleep, and recovery compared to those who do not, without compromising the total number of hours worked (Garde et al., 2020).
2.1.4 Shift duration and timing
Research evidence for the optimal shift duration remains inconclusive; however, reducing shifts from ≥12 h to ≤ 10 h (or ≤ 9 h in the case of night shifts) has generally been shown to benefit sleep and reflects research-backed recommendations (Knauth and Hornberger, 2003; Sallinen and Kecklund, 2010; Arlinghaus et al., 2019; Wong et al., 2019; Garde et al., 2020; Bragge et al., 2023). Notably, reducing shift length has received a mixed reception in the healthcare sector, with fewer hours perceived as compressing workload and compromising education (Bragge et al., 2023). Nevertheless, 12 h shifts have not been shown to benefit staffing costs, productivity, performance, sickness absence, sleepiness, or wellbeing in this population (Dall'Ora et al., 2022).
To minimize circadian disruption, morning shifts should start as late as possible (i.e., 7 am vs. 6 am), while evening shifts should finish as early as possible (i.e., 10 pm vs. 11 pm; Knauth and Hornberger, 2003).
2.1.5 Consecutive shifts and rest days
To improve employee outcomes and reduce the risk of fatigue-related accidents, consensus reviews recommend that individuals work a maximum of 5–7 consecutive shifts, and no more than 3 consecutive night shifts (Knauth and Hornberger, 2003; Garde et al., 2020). In instances where night work could pose greater risk (i.e., during pregnancy), 1 night shift per week is advised (Garde et al., 2020).
When it comes to rest periods between shifts, a minimum of 11hrs is recommended by the Working Time Society (Wong et al., 2019). To allow adequate time for recovery, days off should be scheduled to occur after night shifts, and single days off in-between workdays should be avoided; giving employees a 2-day off weekend equivalent per rotation can also protect work-life balance (Knauth and Hornberger, 2003; Wong et al., 2019).
2.1.6 Chronotype
Individuals with morning chronotypes experience greater circadian misalignment on night shifts and may require additional on-shift interventions as a result, while individuals with later circadian phases exhibit better resilience and recovery (Sallinen and Kecklund, 2010; Juda et al., 2013). Accordingly, chronotype may be an important factor to consider when recruiting employees and allocating shifts; however, further research is needed to understand its effects on shift work tolerance and associations with age and sex (Ritonja et al., 2019).
2.2 Controlled light exposure
Light is essential to the regulation of the circadian system and has positive, non-visual effects on alertness, productivity, and sleep (Burgess et al., 2002). Accordingly, researchers have experimented with the timing, intensity, and color temperature of workplace lighting to help facilitate adaptation to night work or improve alertness and productivity (Robbins et al., 2021; Bragge et al., 2023). Indeed, the American Academy of Sleep Medicine recommended timed light exposure in the treatment of SWD (Morgenthaler et al., 2007).
Compared to standard lighting, blue-enriched light has been shown to improve sleep quality, alertness, concentration, and performance (Mills et al., 2007; Viola et al., 2008; Motamedzadeh et al., 2017; Sletten et al., 2021). Exposure to high intensity, blue-enriched light – particularly at the point of peak circadian sleepiness – can delay rhythms and facilitate adaptation to permanent or slow-rotating night shifts (Eastman and Martin, 1999; Horowitz et al., 2001; Burgess et al., 2002; Crowley et al., 2003). To prepare the body for the return to a “normal” sleep-wake pattern (i.e., on days off), the presentation of light can be timed to occur later each consecutive night shift (Eastman and Martin, 1999; Burgess et al., 2002). Here, it is important to note that employees on rapidly rotating shifts will not benefit from this gradual “circadian entrainment,” given the comparably slower nature of biological rhythms (Eastman and Martin, 1999).
To prevent morning light from advancing circadian rhythms and promoting wakefulness upon leaving the workplace, dark sunglasses can be worn on the commute home (Crowley et al., 2003); however, this may not be practical for those driving themselves, especially on dark mornings when the suppression of light could compromise safety. Once home, going straight to bed in a dark environment can improve sleep (Burgess et al., 2002). Avoiding light the morning before a night shift, where feasible, is also recommended (Morgenthaler et al., 2007).
2.3 Sleep hygiene education
SHE can cultivate awareness of healthy sleep practices; however, as is the case outside of the shift work population, evidence for its effectiveness as a standalone treatment for sleep problems in shift workers remains mixed (Robbins et al., 2021; Bragge et al., 2023), with many intervention studies reporting little to no effect on sleep and alertness (Arora et al., 2007; James et al., 2018; Pylkkönen et al., 2018; Booker et al., 2022).
SHE also tends to contradict accepted fatigue management strategies for shift workers (i.e., napping during the day and consuming caffeine on night shifts), while advice to maintain a consistent sleep-wake schedule fails to accommodate irregular working hours (Shriane et al., 2023). Accordingly, Shriane et al. (2023) recently utilized the Delphi method to develop a series of 18 “healthy sleep practices” for shift workers, wherein the unique challenges faced by this population were addressed; for instance, using napping as a tool to achieve 7 h−9 h of sleep per 24 h period. Determining the acceptability and effectiveness of these guidelines and/or incorporating them into multicomponent programmes present an opportunity for future research.
2.4 Planned napping
Napping before and/or during a night shift – particularly at the point of peak circadian sleepiness – can help to manage alertness and improve performance (Morgenthaler et al., 2007; Rajaratnam et al., 2013; Ruggiero and Redeker, 2014; Martin-Gill et al., 2018). Research suggests that a 20 min−30 min nap provides employees with the benefits of rest, whilst reducing the likelihood of entering deep sleep, which can lead to inertia upon awakening and compromise the subsequent sleep period (Ruggiero and Redeker, 2014; Martin-Gill et al., 2018). Nevertheless, employees may still need 15 min post-nap to regain cognitive faculties before resuming work (Ruggiero and Redeker, 2014; Martin-Gill et al., 2018).
2.5 Caffeine consumption
Like napping, the stimulating effects of caffeine have been shown to decrease sleepiness, reduce the risk of errors, and facilitate cognitive performance in the workplace (Ker et al., 1996; Temple et al., 2018). Regular, low dose caffeine consumption throughout the night shift counteracts performance deficits associated with extended wakefulness; however, consumption too near to the planned sleep period (i.e., < 6 h before) may disrupt sleep quality and duration (Wyatt et al., 2004; McHill et al., 2014).
2.6 Cognitive behavioral therapy for insomnia
Recommended as the first line of treatment for chronic insomnia in the general population, CBT-i has also been used to treat insomnia in shift workers. Findings from a recent meta-analysis revealed that CBT-i significantly reduced insomnia severity and improved sleep quality; however, values did not reach the threshold for clinical significance, and heterogeneity in intervention design, methodology, and delivery limited conclusions (Reynolds et al., 2022). High levels of attrition also suggest that current efforts may not sufficiently address the needs of this population (Reynolds et al., 2022).
Indeed, elements of CBT-i are challenging for shift workers, who may be unable to maintain consistent sleep schedules, rely upon naps to manage fatigue, and have restricted sleep durations (Järnefelt et al., 2012, 2020; Reynolds et al., 2022). Accordingly, researchers have attempted to modify CBT-i for this population by implementing a 4 h “anchor sleep” period instead of a consistent sleep schedule and allowing shift workers to have an extra hour in bed if their sleep duration is already restricted by work (Järnefelt et al., 2012, 2020). Other modifications involve adapting SHE to include advice on napping and light exposure, and emphasizing the use of relaxation techniques to reduce post-shift arousal (Järnefelt et al., 2012, 2020; Booker et al., 2022).
When it comes to accessing CBT-i, digital platforms could offer a relatively inexpensive and scalable option for employees and employers (Robbins et al., 2021). Encouragingly, 4–6 weeks of self-guided online CBT-i has been shown to improve insomnia symptoms in shift workers (Peter et al., 2019; Omeogu et al., 2020), although further research is needed to draw conclusions (Reynolds et al., 2022).
2.7 Mind-body interventions
Evidence for the effectiveness of mind-body interventions (e.g., mindfulness-based stress reduction, yogic relaxation, physical activity etc.,) remains limited within the shift work population (Robbins et al., 2021); however, a handful of studies have demonstrated that yogic relaxation and exercise can reduce stress and increase sleep quantity (Fang and Li, 2015; Raghul et al., 2018).
Given their effectiveness in other workplace settings (Pérez-Fuentes et al., 2020), mind-body interventions may be an additional element to consider incorporating into future multicomponent programmes (Robbins et al., 2021). Indeed, SHE and CBT-i encourage relaxation for reducing pre-sleep arousal, while mindfulness-based therapies for insomnia have proven to be effective in other working populations (Ong and Moore, 2020).
3 Discussion
This mini review highlights various strategies that have been employed to help manage the impacts of shift work on sleep; however, research evidence for the effectiveness of preventative, multicomponent programmes is currently lacking (Redeker et al., 2019; Bragge et al., 2023). A summary of the evidence pertaining to each intervention category is presented below; future directions and limitations are also considered.
Adjustments to shift schedules and changes to workplace lighting have been shown to mitigate the effects of shift work-related circadian misalignment; however, balancing the needs of employees against what is feasible for the organization may be complex (Wong et al., 2019). For instance, while reducing shift duration and enhancing workplace lighting might benefit employees, such organizational-level changes have substantial costs for employers (e.g., recruiting additional staff to make-up for lost hours). Thus, as well as emphasizing organizational benefits, government regulation of research-backed recommendations may be required to encourage implementation.
Given the health and safety consequences of shift work-related circadian misalignment, intervention programmes should aim to educate employers and equip employees with the skills needed to manage sleep from the outset of employment. Collective ownership of employee sleep could be achieved by delivering tailored forms of SHE as part of staff inductions and training. As employers are legally required to protect staff from health and safety risks, night workers could also be provided with personal protective equipment to facilitate daytime sleeping (e.g., eye-masks and earplugs).
In addition to the above, employers could consider facilitating nap opportunities and providing access to caffeine on nights shifts to help manage alertness. Advice on timing and dosage could also be incorporated into SHE, although negative attitudes toward “sleeping on the job” may present a barrier to the implementation of napping. While educating employers and being selective with terminology – i.e., “controlled rest” vs. “naps” – could help to overcome such challenges, providing suitable rest conditions may still pose difficulties for sectors with noisy and/or outdoor working environments. Indeed, it should be noted that the implementation of any intervention component must be tailored to job role, setting and circumstances.
As shift work increases the risk of clinical sleep problems, organizations should be prepared to support employees with the relevant resources. Digital CBT-i platforms could offer an inexpensive and scalable option for employers, while providing an external access option for employees who may have anxieties about revealing sleep problems in the workplace. Despite this, further research is needed to identify modifications that could improve the acceptability and effectiveness of digital CBT-i for shift workers (Reynolds et al., 2022). Similarly, the effectiveness of mind-body interventions remains unclear, despite benefits being found in other working populations (Pérez-Fuentes et al., 2020). While these approaches may help to address sleep problems associated with shift work-related circadian misalignment, it is also important to acknowledge their limited application to sleep disorders with other causal underpinnings (i.e., obstructive sleep apnea), which should be addressed via additional and/or alternative treatments (i.e., continuous positive airway pressure).
Lastly, it should be noted that personal demands also constrain sleep time and increase sleepiness (Knauth and Hornberger, 2003; Gurubhagavatula et al., 2021). Despite this, factors such as family life, the commute, and eating behaviors appear to have been overlooked in current intervention efforts. In light of this, working with shift workers and employers to co-develop preventative, multicomponent approaches represents an essential step for future research, and may help to identify further intervention opportunities (Wong et al., 2019; Reynolds et al., 2022).
Author contributions
AT: Conceptualization, Investigation, Project administration, Visualization, Writing—original draft, Writing—review & editing. NT: Conceptualization, Funding acquisition, Writing—review & editing. TS: Conceptualization, Funding acquisition, Writing—review & editing. CT: Conceptualization, Funding acquisition, Writing—review & editing. CK: Conceptualization, Funding acquisition, Writing—review & editing. CM: Conceptualization, Funding acquisition, Writing—review & editing. SR: Conceptualization, Funding acquisition, Writing—review & editing. TM: Conceptualization, Funding acquisition, Supervision, Writing—original draft, Writing—review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This publication was supported by the UK Medical Research Council's Public Health Intervention Development grant (MR/Y503241/1).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frsle.2024.1343393/full#supplementary-material
Footnotes
1. ^As a widely available, prescription-free stimulant, caffeine is considered as a non-pharmacological intervention in this mini review.
References
Arlinghaus, A., Bohle, P., Iskra-Golec, I., Jansen, N., Jay, S., Rotenberg, L., et al. (2019). Working time society consensus statements: evidence-based effects of shift work and non-standard working hours on workers, family and community. Indust. Health 57, 184–200. doi: 10.2486/indhealth.SW-4
Arora, V. M., Georgitis, E., Woodruff, J. N., Humphrey, H. J., and Meltzer, D. (2007). Improving sleep hygiene of medical interns: can the sleep, alertness, and fatigue education in residency program help? Arch. Int. Med. 167, 1738–1744. doi: 10.1001/archinte.167.16.1738
Bambra, C. L., Whitehead, M. M., Sowden, A. J., Akers, J., and Petticrew, M. P. (2008). Shifting schedules: the health effects of reorganizing shift work. Am. J. Prev. Med. 34, 427–434. doi: 10.1016/j.amepre.2007.12.023
Booker, L. A., Sletten, T. L., Barnes, M., Alvaro, P., Collins, A., Chai-Coetzer, C. L., et al. (2022). The effectiveness of an individualized sleep and shift work education and coaching program to manage shift work disorder in nurses: a randomized controlled trial. J. Clin. Sleep Med. 18, 1035–1045. doi: 10.5664/jcsm.9782
Bragge, P., Burns, J., Kellner, P., Allan, M., Fitzgerald, D., Grundy, E., et al. (2023). Sleep Health Interventions for Managing Mental Health in Shift Workers: A Systematic Review. Monash Sustainable Development Institute Evidence Review Service. Melbourne, ACT: Monash University.
Burgess, H. J., Sharkey, K. M., and Eastman, C. I. (2002). Bright light, dark and melatonin can promote circadian adaptation in night shift workers. Sleep Med. Rev. 6:40. doi: 10.1053/smrv.2001.0215
Chatterjee, K., and Ambekar, P. (2017). Study of insomnia in rotating shift-workers. Ind. Psychiatr. J. 26:82. doi: 10.4103/ipj.ipj_59_17
Crowley, S. J., Lee, C., Tseng, C. Y., Fogg, L. F., and Eastman, C. I. (2003). Combinations of bright light, scheduled dark, sunglasses, and melatonin to facilitate circadian entrainment to night shift work. J. Biol. Rhythms 18, 513–523. doi: 10.1177/0748730403258422
Dall'Ora, C., Ejebu, O. Z., and Griffiths, P. (2022). Because they're worth it? A discussion paper on the value of 12-h shifts for hospital nursing. Hum. Resour. Health 20, 1–7. doi: 10.1186/s12960-022-00731-2
Eastman, C. I., and Martin, S. K. (1999). How to use light and dark to produce circadian adaptation to night shift work. Annal. Med. 31, 87–98. doi: 10.3109/07853899908998783
Edinger, J. D., Arnedt, J. T., Bertisch, S. M., Carney, C. E., Harrington, J. J., Lichstein, K. L., et al. (2021). Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline. J. Clin. Sleep Med. 17, 255–262. doi: 10.5664/jcsm.8986
Fang, R., and Li, X. (2015). A regular yoga intervention for staff nurse sleep quality and work stress: a randomised controlled trial. J. Clin. Nurs. 24, 3374–3379. doi: 10.1111/jocn.12983
Garde, A. H., Albertsen, K., Nabe-Nielsen, K., Carneiro, I. G., Skotte, J., Hansen, S. M., et al. (2012). Implementation of self-rostering (the PRIO project): effects on working hours, recovery, and health. Scand. J. Work Environ. Health 12, 314–326. doi: 10.5271/sjweh.3306
Garde, A. H., Begtrup, L., Bjorvatn, B., Bonde, J. P., Hansen, J., Hansen, Å. M., et al. (2020). How to schedule night shift work in order to reduce health and safety risks. Scand. J. Work Environ. Health 46:557. doi: 10.5271/sjweh.3920
Gurubhagavatula, I., Barger, L. K., Barnes, C. M., Basner, M., Boivin, D. B., Dawson, D., et al. (2021). Guiding principles for determining work shift duration and addressing the effects of work shift duration on performance, safety, and health: guidance from the American academy of sleep medicine and the sleep research society. Sleep 44:zsab161. doi: 10.1093/sleep/zsab161
Horowitz, T. S., Cade, B. E., Wolfe, J. M., and Czeisler, C. A. (2001). Efficacy of bright light and sleep/darkness scheduling in alleviating circadian maladaptation to night work. American J. Physiol. Endocrinol. Metab. 281, E384–E391. doi: 10.1152/ajpendo.2001.281.2.E384
Hui, S. K. A., and Grandner, M. A. (2015). Trouble sleeping associated with lower work performance and greater healthcare costs: longitudinal data from Kansas state employee wellness program. J. Occup. Environ. Med. 57:1031. doi: 10.1097/JOM.0000000000000534
James, L., Samuels, C. H., and Vincent, F. (2018). Evaluating the effectiveness of fatigue management training to improve police sleep health and wellness. J. Occup. Environ. Med. 60, 77–82. doi: 10.1097/JOM.0000000000001174
James, S. M., Honn, K. A., Gaddameedhi, S., and Van Dongen, H. P. (2017). Shift work: disrupted circadian rhythms and sleep—implications for health and well-being. Curr. Sleep Med. Rep. 3, 104–112. doi: 10.1007/s40675-017-0071-6
Järnefelt, H., Härm,ä, M., Sallinen, M., Virkkala, J., Paajanen, T., Martimo, K. P., et al. (2020). Cognitive behavioural therapy interventions for insomnia among shift workers: RCT in an occupational health setting. Int. Arch. Occupat. Environ. Health 93, 535–550. doi: 10.1007/s00420-019-01504-6
Järnefelt, H., Lagerstedt, R., Kajaste, S., Sallinen, M., Savolainen, A., Hublin, C., et al. (2012). Cognitive behavioral therapy for shift workers with chronic insomnia. Sleep Med. 13, 1238–1246. doi: 10.1016/j.sleep.2012.10.003
Juda, M., Vetter, C., and Roenneberg, T. (2013). Chronotype modulates sleep duration, sleep quality, and social jet lag in shift-workers. J. Biol. Rhythms 28, 141–151. doi: 10.1177/0748730412475042
Ker, K., Edwards, P. J., Felix, L. M., Blackhall, K., and Roberts, I. (1996). Caffeine for the prevention of injuries and errors in shift workers. Cochrane Datab. Syst. Rev. 2010:508. doi: 10.1002/14651858.CD008508
Knauth and Hornberger, S. (2003). Preventive and compensatory measures for shift workers. Occup. Med. 53, 109–116. doi: 10.1093/occmed/kqg049
Martin-Gill, C., Barger, L. K., Moore, C. G., Higgins, J. S., Teasley, E. M., Weiss, P. M., et al. (2018). Effects of napping during shift work on sleepiness and performance in emergency medical services personnel and similar shift workers: a systematic review and meta-analysis. Prehospital Emerg. Care 22, 47–57. doi: 10.1080/10903127.2017.1376136
McHill, A. W., Smith, B. J., and Wright, K. P. (2014). Effects of caffeine on skin and core temperatures, alertness, and recovery sleep during circadian misalignment. J. Biol. Rhythms 29, 131–143. doi: 10.1177/0748730414523078
Mills, P. R., Tomkins, S. C., and Schlangen, L. J. (2007). The effect of high correlated colour temperature office lighting on employee wellbeing and work performance. J. Circadian Rhythms 5, 1–9. doi: 10.1186/1740-3391-5-2
Morgenthaler, T. I., Lee-Chiong, T., Alessi, C., Friedman, L., Aurora, R. N., Boehlecke, B., et al. (2007). Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. Sleep 30, 1445–1459. doi: 10.1093/sleep/30.11.1445
Motamedzadeh, M., Golmohammadi, R., Kazemi, R., and Heidarimoghadam, R. (2017). The effect of blue-enriched white light on cognitive performances and sleepiness of night-shift workers: a field study. Physiol. Behav. 177, 208–214. doi: 10.1016/j.physbeh.2017.05.008
Neil-Sztramko, S. E., Pahwa, M., Demers, P. A., and Gotay, C. C. (2014). Health-related interventions among night shift workers: a critical review of the literature. Scand. J. Work Environ. Health 21, 543–556. doi: 10.5271/sjweh.3445
Omeogu, C., Shofer, F., and Gehrman Green-McKenzie, J. (2020). Efficacy of a mobile behavioral intervention for workers with insomnia. J. Occup. Environ. Med. 62, 246–250. doi: 10.1097/JOM.0000000000001819
Ong, J. C., and Moore, C. (2020). What do we really know about mindfulness and sleep health? Curr. Opin. Psychol. 34, 18–22. doi: 10.1016/j.copsyc.2019.08.020
Pallesen, S., Bjorvatn, B., Waage, S., Harris, A., and Sagoe, D. (2021). Prevalence of shift work disorder: a systematic review and meta-analysis. Front. Psychol. 12:638252. doi: 10.3389/fpsyg.2021.638252
Papantoniou, K., Vetter, C., and Schernhammer, E. S. (2017). Shift work practices and opportunities for intervention. Occup. Environ. Med. 74, 2–3. doi: 10.1136/oemed-2016-103904
Pérez-Fuentes, M. D. C., Molero Jurado, M. D. M., Mercader Rubio, I., Soriano Sanchez, J. G., and Gazquez Linares, J. J. (2020). Mindfulness for preventing psychosocial risks in the workplace: a systematic review and meta-analysis. Appl. Sci. 10:1851. doi: 10.3390/app10051851
Peter, L., Reindl, R., Zauter, S., Hillemacher, T., and Richter, K. (2019). Effectiveness of an online CBT-I intervention and a face-to-face treatment for shift work sleep disorder: a comparison of sleep diary data. Int. J. Environ. Res. Pub. Health 16:3081. doi: 10.3390/ijerph16173081
Pylkkönen, M., Tolvanen, A., Hublin, C., Kaartinen, J., Karhula, K., Puttonen, S., et al. (2018). Effects of alertness management training on sleepiness among long-haul truck drivers: a randomized controlled trial. Accident Anal. Prev. 121, 301–313. doi: 10.1016/j.aap.2018.05.008
Raghul, S., Vasanthan, S., Bhavanani, A. B., Jaiganesh, K., and Madanmohan, T. (2018). Effects of overnight sleep deprivation on autonomic function and perceived stress in young health professionals and their reversal through yogic relaxation (Shavasana). Nat. J. Physiol. Pharm. Pharmacol. 8, 1256–1256. doi: 10.5455/njppp.2018.8.0415003052018
Rajaratnam, S. M., Howard, M. E., and Grunstein, R. R. (2013). Sleep loss and circadian disruption in shift work: health burden and management. Med. J. Australia 199, S11–S15. doi: 10.5694/mja13.10561
Redeker, N. S., Caruso, C. C., Hashmi, S. D., Mullington, J. M., Grandner, M., Morgenthaler, T. I., et al. (2019). Workplace interventions to promote sleep health and an alert, healthy workforce. J. Clin. Sleep Med. 15, 649–657. doi: 10.5664/jcsm.7734
Reynolds, A. C., Sweetman, A., Crowther, M. E., Paterson, J. L., Scott, H., Lechat, B., et al. (2022). Is cognitive behavioral therapy for insomnia (CBTi) efficacious for treating insomnia symptoms in shift workers? A systematic review and meta-analysis. Sleep Med. Rev. 12:101716. doi: 10.1016/j.smrv.2022.101716
Richter, K., Acker, J., Adam, S., and Niklewski, G. (2016). Prevention of fatigue and insomnia in shift workers—a review of non-pharmacological measures. EPMA J. 7, 1–11. doi: 10.1186/s13167-016-0064-4
Ritonja, J., Aronson, K. J., Matthews, R. W., Boivin, D. B., and Kantermann, T. (2019). Working time society consensus statements: individual differences in shift work tolerance and recommendations for research and practice. Industr. Health 57, 201–212. doi: 10.2486/indhealth.SW-5
Robbins, R., Underwood, P., Jackson, C. L., Jean-Louis, G., Madhavaram, S., Kuriakose, S., et al. (2021). A systematic review of workplace-based employee health interventions and their impact on sleep duration among shift workers. Workplace Health Safety 69, 525–539. doi: 10.1177/21650799211020961
Ruggiero, J. S., and Redeker, N. S. (2014). Effects of napping on sleepiness and sleep-related performance deficits in night-shift workers: a systematic review. Biol. Res. Nurs. 16, 134–142. doi: 10.1177/1099800413476571
Ryu, J., Jung-Choi, K., Choi, K. H., Kwon, H. J., Kang, C., Kim, H., et al. (2017). Associations of shift work and its duration with work-related injury among electronics factory workers in South Korea. Int. J. Environ. Res. Pub. Health 14:1429. doi: 10.3390/ijerph14111429
Sallinen, M., and Kecklund, G. (2010). Shift work, sleep, and sleepiness—differences between shift schedules and systems. Scand. J. Work Environ. Health 21, 121–133. doi: 10.5271/sjweh.2900
Shriane, A. E., Rigney, G., Ferguson, S. A., Bin, Y. S., and Vincent, G. E. (2023). Healthy sleep practices for shift workers: consensus sleep hygiene guidelines using a Delphi methodology. Sleep 5:zsad182. doi: 10.1093/sleep/zsad182
Skivington, K., Matthews, L., Simpson, S. A., Craig, P., Baird, J., Blazeby, J. M., et al. (2021). A new framework for developing and evaluating complex interventions: update of medical research council guidance. BMJ 374:n2061. doi: 10.1136/bmj.n2061
Sletten, T. L., Cappuccio, F. P., Davidson, A. J., Van Cauter, E., Rajaratnam, S. M., Scheer, F. A., et al. (2020). Health consequences of circadian disruption. Sleep 43:zsz194. doi: 10.1093/sleep/zsz194
Sletten, T. L., Raman, B., Magee, M., Ferguson, S. A., Kennaway, D. J., Grunstein, R. R., et al. (2021). A blue-enriched, increased intensity light intervention to improve alertness and performance in rotating night shift workers in an operational setting. Nat. Sci. Sleep 25:647–657. doi: 10.2147/NSS.S287097
Temple, J. L., Hostler, D., Martin-Gill, C., Moore, C. G., Weiss, P. M., Sequeira, D. J., et al. (2018). Systematic review and meta-analysis of the effects of caffeine in fatigued shift workers: implications for emergency medical services personnel. Prehosp. Emerg. Care 22, 37–46. doi: 10.1080/10903127.2017.1382624
Torquati, L., Mielke, G. I., Brown, W. J., Burton, N. W., and Kolbe-Alexander, T. L. (2019). Shift work and poor mental health: a meta-analysis of longitudinal studies. Am. J. Public health 109, e13–e20. doi: 10.2105/AJPH.2019.305278
Viola, A. U., James, L. M., Schlangen, L. J., and Dijk, D. J. (2008). Blue-enriched white light in the workplace improves self-reported alertness, performance and sleep quality. Scand. J. Work Environ. Health 17, 297–306. doi: 10.5271/sjweh.1268
Walker, W. H., Walton, J. C., DeVries, A. C., and Nelson, R. J. (2020). Circadian rhythm disruption and mental health. Transl. Psychiatr. 10:28. doi: 10.1038/s41398-020-0694-0
Wickwire, E. M. (2019). The value of digital insomnia therapeutics: what we know and what we need to know. J. Clin. Sleep Med. 15, 11–13. doi: 10.5664/jcsm.7558
Wong, I. S., McLeod, C. B., and Demers, P. A. (2011). Shift work trends and risk of work injury among Canadian workers. Scand. J. Work Environ. Health 14, 54–61. doi: 10.5271/sjweh.3124
Wong, I. S., Popkin, S., and Folkard, S. (2019). Working Time Society consensus statements: a multi-level approach to managing occupational sleep-related fatigue. Ind. Health 57, 228–244. doi: 10.2486/indhealth.SW-6
Keywords: sleep, intervention, shift work, mini review, prevention
Citation: Tout AF, Tang NKY, Sletten TL, Toro CT, Kershaw C, Meyer C, Rajaratnam SMW and Moukhtarian TR (2024) Current sleep interventions for shift workers: a mini review to shape a new preventative, multicomponent sleep management programme. Front. Sleep 3:1343393. doi: 10.3389/frsle.2024.1343393
Received: 23 November 2023; Accepted: 11 January 2024;
Published: 08 February 2024.
Edited by:
Stuart F. Quan, Harvard Medical School, United StatesReviewed by:
Montserrat Diaz-Abad, University of Maryland, United StatesCopyright © 2024 Tout, Tang, Sletten, Toro, Kershaw, Meyer, Rajaratnam and Moukhtarian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amber F. Tout, YW1iZXIudG91dEB3YXJ3aWNrLmFjLnVr
 Amber F. Tout
Amber F. Tout Nicole K. Y. Tang2
Nicole K. Y. Tang2 Tracey L. Sletten
Tracey L. Sletten Carla T. Toro
Carla T. Toro Shantha M. W. Rajaratnam
Shantha M. W. Rajaratnam Talar R. Moukhtarian
Talar R. Moukhtarian