- 1Department of Obstetrics and Gynecology, University of Michigan, Ann Arbor, MI, United States
- 2Program on Women’s Healthcare Effectiveness Research, University of Michigan, Ann Arbor, MI, United States
- 3Department of Obstetrics and Gynecology, Corewell Health William Beaumont University Hospital, Royal Oak, MI, United States
- 4Department of Psychiatry, University of Michigan, Ann Arbor, MI, United States
- 5Department of Health Management and Policy, University of Michigan School of Public Health, Ann Arbor, MI, United States
- 6Center for Clinical Management Research (CCMR), VA Ann Arbor Healthcare System, Ann Arbor, MI, United States
- 7Institute for Healthcare Policy and Innovation, University of Michigan, Ann Arbor, MI, United States
- 8College of Human Medicine, Michigan State University, East Lansing, MI, United States
- 9Department of Biology, Spelman College, Atlanta, GA, United States
- 10Department of Systems, Populations and Leadership, University of Michigan School of Nursing, Ann Arbor, MI, United States
- 11Population Studies Center, Institute for Social Research, University of Michigan, Ann Arbor, MI, United States
- 12Institute for Firearm Injury Prevention, University of Michigan, Ann Arbor, MI, United States
Objectives: Intimate partner violence (IPV) and non-intimate domestic violence (DV) during pregnancy may result in poor maternal and infant health outcomes. Whether state-level abortion restrictions, enacted by many states even prior to the 2022 Dobbs v. Jackson Women's Health Organization decision, are associated with IPV/DV remains unknown. This study aimed to investigate the relationship between IPV/DV during pregnancy and abortion restrictions among Black and White birthing people.
Study design: We analyzed 2020 data from 36 states participating in the CDC Pregnancy Risk Assessment Monitoring System representing 1,931,458 deliveries of which 1,368,237 deliveries (70.84%) are from Black and White birthing individuals. We divided states into restrictive (N = 17) and less restrictive (N = 19) based on a modified Guttmacher Abortion Policy Hostility Index. We used weighted logistic regression to assess the relationship between state abortion restrictiveness and self-reported IPV/DV.
Results: Overall, birthing individuals in restrictive states had higher odds of reporting IPV/DV during pregnancy than those in less restrictive states (aOR: 1.36, 95% CI: 1.15–1.60). Within racial groups, we found that Black birthing individuals in restrictive states had higher odds of reporting IPV/DV than Black birthing individuals in less restrictive states (aOR:1.75, 95% CI: 1.24–2.47). We saw a similar relationship for White birthing individuals (aOR:1.50, 95% CI: 1.17–1.94).
Discussion: Even when access to abortion was federally protected, individuals in restrictive states had higher odds of experiencing IPV/DV than those in less restrictive states, particularly among Black individuals. These findings suggest possible detrimental impacts of abortion restrictions and their potential to worsen existing health inequities.
1 Introduction
Nearly 10% of pregnant people report experiencing either physical or sexual violence during their pregnancy, and Black individuals experience intimate partner violence (IPV) rates (1) at least twice as high as White individuals (2). IPV and non-intimate domestic violence (DV) during pregnancy have serious maternal and infant health consequences, including pregnancy loss, premature birth, low birthweight, and infant mortality (3, 4)—outcomes that disproportionately impact Black birthing people and infants (5). Pregnancy is also a period of heightened risk. Pregnant or recently pregnant individuals are more likely to die by homicide than of the three most common obstetric causes of death (hypertensive disorders, hemorrhage, sepsis) (6), and rates are increasing (7). Female victims of homicide are disproportionately more likely to be Black, especially in pregnancy-associated homicides; between 2008 and 2019, nearly 50% of pregnancy-associated homicide victims were Black (8). IPV also precipitates half of pregnancy-associated suicides (2, 6, 9).
Prior research has described the complicated relationships among pregnancy intention, abortion access, and IPV. Compared to individuals with intended pregnancies, people with unwanted or unplanned pregnancies are four times more likely to experience IPV (10) and individuals victimized by IPV are three times more likely to have an abortion during their lifetime (11, 12). Partner conflict or IPV is often a factor in the decision to have an abortion, and those who obtain abortions end their abusive relationships faster and experience less partner violence than those who give birth (13). The reported relationships among pregnancy intention, abortion, and IPV underlie concerns that restricting access to abortion could increase IPV prevalence around the time of pregnancy, especially among Black pregnant people (14).
Clarifying the relationships between abortion access, IPV or non-intimate DV (IPV/DV), and racial disparities in birth outcomes reached new urgency following the June 2022 U.S. Supreme Court's Dobbs v. Jackson Women's Health Organization decision. As of November 2023, 18 states enacted complete bans, or gestational age cutoffs at 12 weeks or less—severely restricting abortion access for nearly half of the United States. Although years may pass before the health consequences of complete bans become clear, even before the Dobbs decision, many states enacted policies that created barriers to abortion services, such as physician and hospital requirements, gestational limits, funding restrictions, and waiting periods (15). Even these less severe restrictions have been associated with decreases in abortion rates (16) and increases in suicide rates (17), but their relationship to IPV and DV is unknown. Moreover, although often asserted, it is unknown whether states with and without highly restrictive abortion policies exhibit differential racial disparities in IPV. This study aimed to characterize rates of IPV/DV around the time of pregnancy among Black and White individuals living in states with highly restrictive abortion policies compared to their counterparts living in less restrictive states.
2 Materials and methods
We analyzed data from 36 states participating in the Centers for Disease Control and Prevention (CDC) Pregnancy Risk Assessment Monitoring System (PRAMS) in 2020. PRAMS is a state-based surveillance system of maternal behaviors, attitudes, and experiences around the time of pregnancy conducted by the CDC in collaboration with state health departments (18). The Institutional Review Board at the University of Michigan approved this study (HUM00204182).
Our cohort represents 1,931,458 deliveries of which 1,368,237 deliveries (70.84%) are from non-Hispanic Black and White birthing individuals. We used two PRAMS core questions to identify individuals experiencing IPV/DV: “In the 12 months before you got pregnant with your new baby, did any of the following people push, hit, slap, kick, choke, or physically hurt you in any other way?” and “During your most recent pregnancy, did any of the following people push, hit, slap, kick, choke, or physically hurt you in any other way?” Participants who (1) selected “yes” to either core question and (2) identified husband or partner, ex-husband or ex-partner, or another family member were classified as experiencing IPV/DV.
We defined pregnancy intention by categorizing participants into two groups based on their responses to the PRAMS core question: “Thinking back to just before you got pregnant with your new baby, how did you feel about becoming pregnant? Check ONE answer.” If the participants selected “I wanted to be pregnant later,” “I didn't want to be pregnant then or at any time in the future,” or “I wasn't sure what I wanted,” we categorized them as not intended pregnancy. If the participants selected “I wanted to be pregnant then” or “I wanted to be pregnant sooner,” we categorized them as intended pregnancy.
Archived annual state-level policy data on abortion restrictions were obtained from the Guttmacher Institute. We divided states into highly restrictive (N = 17) and less restrictive (N = 19) categories using a modified version of the Guttmacher Abortion Policy Hostility Index from 2019 to 2020 (Figure 1). The modified index assigned each state an annual score ranging from 0 to 10 based on the presence of restrictive policies, including gestational limits, inaccurate or misleading counseling requirements, mandatory in-person counseling followed by a waiting period, ultrasound mandates, insurance coverage restrictions, medication abortion restrictions such as telemedicine bans, parental involvement laws, and Targeted Regulation of Abortion Providers (TRAP) laws. A score greater than or equal to 6 indicates that the state is extremely hostile to abortion rights (19).
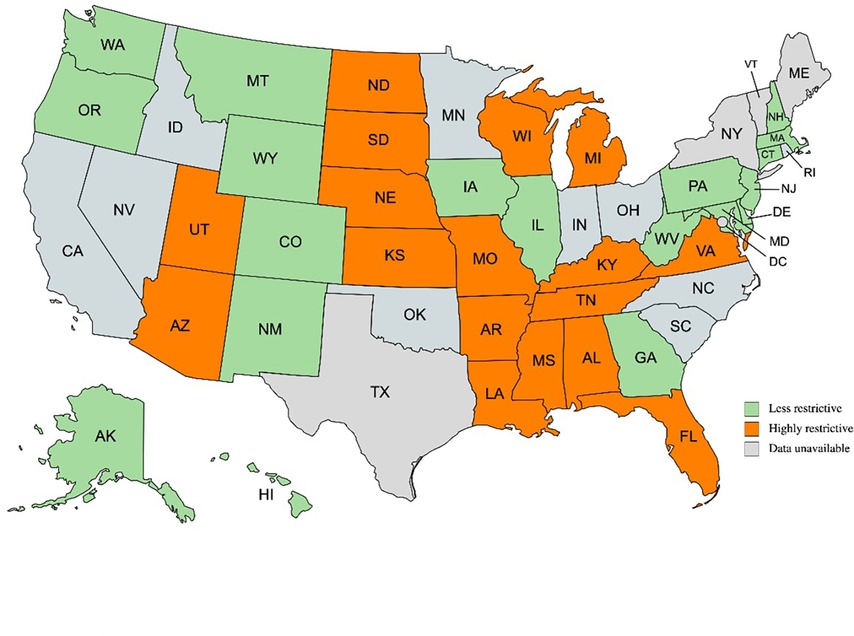
Figure 1. Map of states with PRAMS data available in 2020 categorized into highly restrictive and less restrictive to abortion (19). PRAMS, pregnancy risk assessment monitoring system. Created with mapchart.net.
Initially, we summarized weighted demographic characteristics by state restrictiveness, IPV/DV status, and Black or White race. Next, we used weighted logistic regression to assess the relationship between state abortion restrictiveness and self-reported physical IPV/DV overall and stratified by race. In the overall model, we adjusted for race, marital status, age, education, and insurance coverage. Since income has high rates of missingness in our sample, we used insurance coverage as a proxy for income. We also tested for a statistical interaction between state restrictiveness and race and did not find a significant interaction (p > 0.10). To further examine the relationships between state restrictiveness, race, and IPV/DV around the time of a pregnancy, we conducted stratified models by race, adjusting for age, education, insurance coverage, and marital status. To explore the influence of pregnancy intention on the relationship between state restrictiveness and IPV/DV, we ran each model again adjusting for pregnancy intention. We performed all data management using SAS, version 9.4 (SAS Institute) and Stata/SE, version 15.1 (StataCorp) and all statistical analyses in SAS, version 9.4.
3 Results
Among the 1,368,237 Black and White birthing individuals in our sample, 50,418 (3.8%) reported experiencing IPV/DV in the period beginning 12 months prior to their most recent delivery through the postpartum period. A higher percentage of both Black and White individuals living in highly restrictive states reported experiencing IPV/DV compared to their counterparts in less restrictive states. Within both highly restrictive and less restrictive states, a higher percentage of Black individuals reported experiencing IPV/DV compared to White individuals (6.6% vs. 4.0%, respectively in highly restrictive states; 3.6% vs. 2.4%, respectively in less restrictive states). The weighted demographic characteristics of our study sample appear in Table 1.
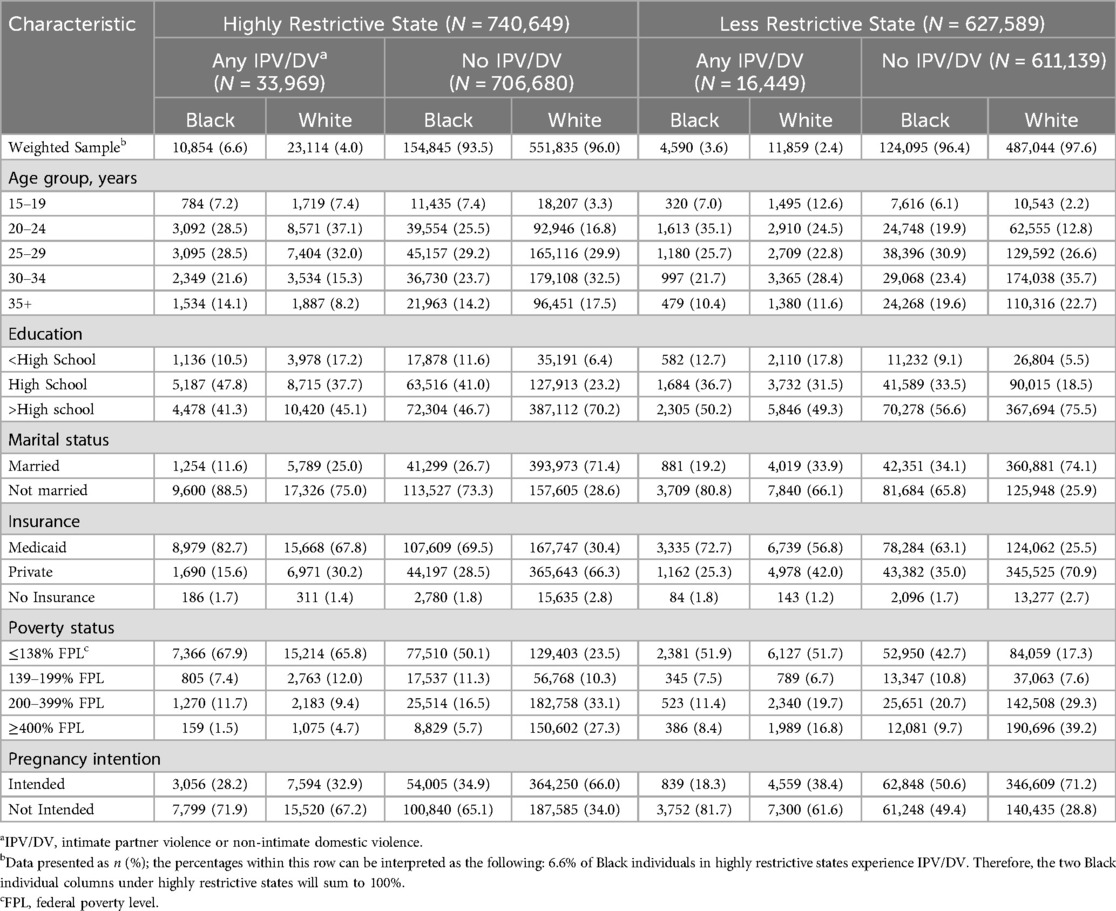
Table 1. Weighted demographic frequencies by state restrictiveness, IPV/DV, and race, black and white birthing individuals, United States, 2020.
Overall, we found that birthing individuals are more likely to experience IPV/DV when living in highly restrictive states compared to less restrictive states (aOR: 1.36, 95% CI: 1.15–1.60) (Table 2). For context, this corresponds to a predicted probability for IPV/DV of 3.27% in less restrictive states and 4.93% in highly restrictive states.
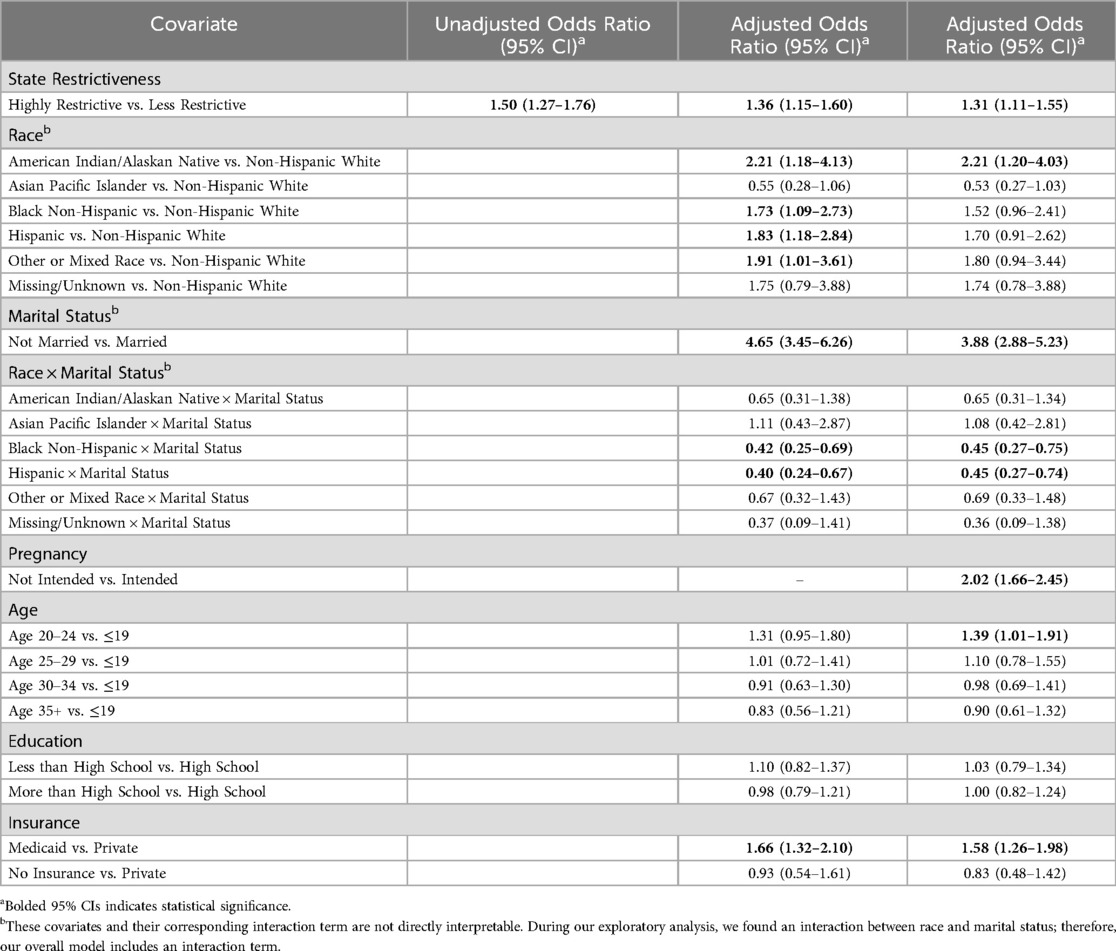
Table 2. Weighted IPV/DV logistic regression models among all races, with and without pregnancy intention, United States, 2020.
In our stratified analyses by race, Black individuals living in highly restrictive states had higher odds of experiencing IPV/DV compared to those living in less restrictive states (aOR: 1.75, 95% CI: 1.24–2.47) after controlling for marital status, age, education, and insurance coverage (Table 3). Similarly, White individuals living in highly restrictive states also had elevated odds of experiencing IPV/DV compared to their counterparts living in less restrictive states (aOR: 1.50, 95% CI: 1.17–1.94) (Table 3).
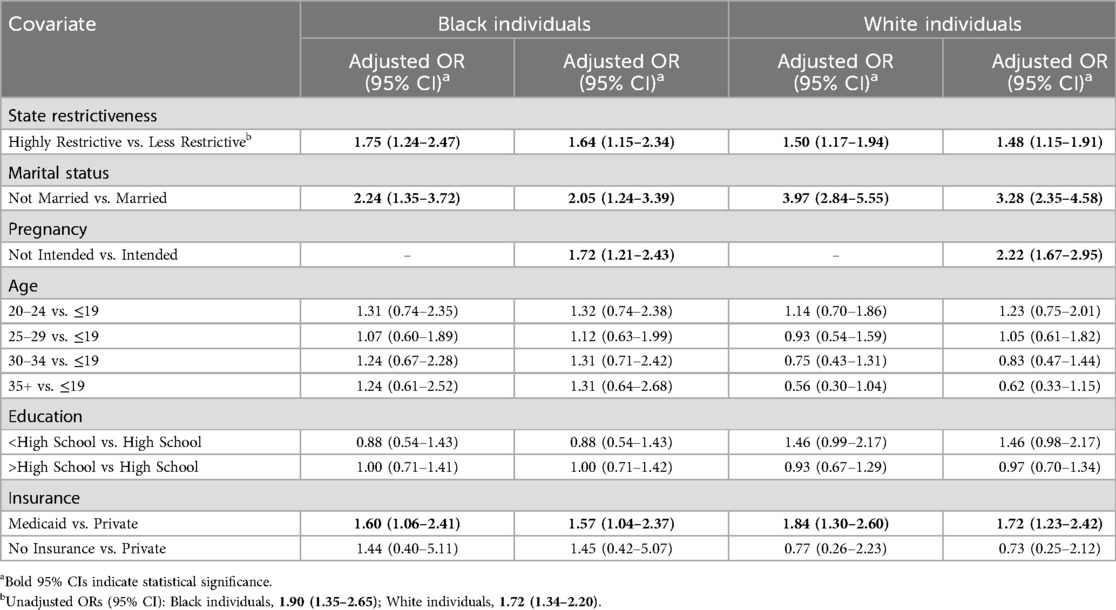
Table 3. Weighted IPV/DV logistic regression models stratified by race among black and white birthing individuals, with and without pregnancy, United States, 2020.
Pregnancy intention status was significantly associated with experiencing IPV/DV in the overall and stratified models (Tables 2, 3). The inclusion of pregnancy intention status in our models resulted in a small decrease in the overall odds ratio characterizing the relationship between state restrictiveness and IPV/DV (aOR: 1.36; 95% CI: 1.15–1.60] vs. aOR: 1.31; 95% CI: 1.11–1.55) (Table 2). In our stratified models, the inclusion of pregnancy intention status resulted in a larger magnitude of change among Black delivering individuals, where the adjusted odds ratio of experiencing IPV/DV decreased from 1.75 (95% CI: 1.24–2.47) to 1.64 (95% CI: 1.15–2.34) (Table 3). The adjusted odds ratio among White individuals also decreased, to a smaller degree, from 1.50 (95% CI: 1.17–1.94) to 1.48 (95% CI: 1.15–1.91) (Table 3).
4 Discussion
Even prior to the enactment of total or near total abortion bans, individuals living in states with higher levels of abortion restrictions had 50%–75% higher odds of experiencing IPV/DV around their most recent birth. Further, the magnitude of this relationship was greater for Black individuals than White individuals (aORs = 1.75 and 1.50, respectively). These findings provide further evidence for concerns that abortion bans are associated with greater health disparities and higher rates of IPV for Black individuals.
Although we cannot determine whether the observed association is causal in nature, we hypothesize multiple potential pathways could potentially explain the amplified chance of experiencing IPV during pregnancy and living in a restrictive state. First, individuals who would like to obtain an abortion because they are in a violent relationship may not be able to access one because of restrictions. Even prior to the Dobbs decision, restrictive abortion policies were associated with decreased rates of abortion and a higher likelihood of pregnancy continuation (16, 20). Prior studies consistently demonstrate that people undergoing abortion report higher rates of IPV (11, 12, 21), and that partner conflict is often a factor in the decision to seek an abortion (13). The Turnaway Study, a landmark study of the consequences of denied abortion, found that individuals unable to obtain a wanted abortion were slower to end a violent relationship and more likely to continue to experience violence compared to those who obtained an abortion (22). Consistent with previous work, we found evidence that pregnancy intention underlies some of the relationship between state abortion policy and IPV, especially among Black delivering individuals.
Second, the observed association between abortion restrictiveness and IPV/DV may also be due to fewer policies or programs aimed at supporting the health and well-being of pregnant people and their families in states that restrict abortions. For instance, restrictive states tend not to have expanded Medicaid, which may result in decreased access to prenatal care and family planning services (23). As noted in an amicus brief filed by hundreds of public health organizations for Jackson Women's Health Organization, the 14 states with the most severely restrictive abortion policies also have the worst health outcomes for birthing people and infants (24).
Third, states that restrict abortion may have fewer policies or state laws that protect people experiencing IPV. For example, although most U.S. states have enacted some form of firearm restriction laws for IPV perpetrators, over half of the states that banned abortion have no domestic violence-related gun regulations. Nonfatal gun use in IPV is common (25) and is used to facilitate coercive control (26), including as a means to ensure the relationship continues.
We focused on disparities in IPV/DV between Black and White individuals in this study. Black individuals are more likely than White individuals to experience reproductive coercion, IPV, and unintended pregnancy (27, 28). Socioeconomic factors such as poverty also disproportionately impact Black individuals, increasing their vulnerability to violent relationships (29). Among Black individuals, IPV is associated with negative physical health outcomes, mental health conditions, and sexual and reproductive health outcomes (30). However, we recognize that other groups experience high rates of IPV and its consequences as well, especially teens, Native American/Alaskan, non-binary, and LGBTQ + individuals (1). These populations are more likely to experience IPV/DV and may experience additional structural and cultural barriers to both health care and legal support. Future studies that are sufficiently powered to examine the relationship between abortion restrictions and IPV among other groups of at-risk people are urgently needed.
This study contributes to a growing body of literature that asserts access to abortion may represent an important structural determinant of health, particularly given the known potential negative health consequences of exposure to IPV/DV during pregnancy (23). It highlights that restrictive abortion policies and higher rates of IPV are clustered in the same states, as well as that the magnitude of the relationship between state restrictiveness and IPV/DV was larger for Black individuals than for White individuals. This is consistent with related literature that identifies racism as a fundamental cause of adverse health outcomes, which acts through multiple, overlapping pathways including structural barriers, cultural racism, and discrimination (31). Within the context of this analysis, racism reduces access to health care including reproductive health services, legal protections that may support individuals experiences IPV/DV, and resources which may help obtain both reproductive health services and protection against IPV/DV. As racial disparities in maternal mortality worsen in the United States, further understanding of these complex dynamics is essential for advancing health equity.
Restrictive abortion policies, IPV/DV, and structural racism directly impact patient care and outcomes. Therefore, health care providers and health care systems must actively recognize and navigate these barriers to improve health outcomes. For instance, in 2012, ACOG recommended routine IPV/DV screening for all perinatal patients (33). Additionally, the Alliance for Innovation on Maternal Health Community Care Initiative (AIM CCI) offers an IPV/DV safety bundle which includes recommendations for culturally appropriate screening and intervention to assuage racial disparities in IPV/DV (34). Provider awareness that individuals experiencing restricted abortion access, as well as structural racism, could be at increased risk of experiencing IPV/DV and its consequences is crucial to protect the health of women.
The key strengths of this study include that PRAMS allows for birthing population estimates at the state level due to its sampling design, inclusion of three-quarters of states, and inclusion of core questions that address IPV/DV victimization. There are, however, several limitations. First, we cannot establish causal relationships between state abortion restrictiveness and IPV/DV using a cross-sectional design. It is likely that there are unaccounted for state-level factors that confound the relationship between abortion restrictiveness and IPV/DV. Specifically, state-level policies regarding mandatory reporting, no-fault divorce, and protective orders may further influence these factors. It is also likely that our study generated conservative estimates of IPV/DV because PRAMS utilizes self-reporting, which may result in underreporting. IPV/DV represents a highly sensitive topic, and respondents may not fully report IPV/DV experiences due to stigma or fear, in addition to common survey limitations such as recall bias. Furthermore, PRAMS does not collect information on psychological violence. Our analysis explores racial trends among Black and White individuals, however we were unable to account for additional or intersecting identities such as gender identity, sexual orientation, and immigration status, which may further impact both risk of IPV/DV and impact of abortion restrictions. Similarly, there is likely within-group heterogeneity among the racial categories used in this analysis, particularly regarding Black subgroups such as African Americans, African immigrants, and Caribbean immigrants. While our data do not support these subgroup analyses, future research should further explore how IPV/DV and abortion restrictions differentially impact other marginalized communities.
Our study included data collected prior to the most extreme category of abortion restrictions— bans or near bans, which may have stronger associations with IPV/DV during pregnancy. Future studies should explore the impact of bans or near bans on the prevalence of IPV/DV and its consequences, including maternal morbidity and mortality. Further, studies should specifically monitor the impact among groups who experience IPV/DV and its health consequences at already high rates, including Black individuals.
5 Conclusion
Our finding that even prior to the enactment of abortion bans, individuals in states with more restricted access to abortion were more likely to report IPV/DV alerts us to another possible detrimental impact of abortion restrictions on health. Furthermore, the observation that the magnitude of this relationship was greater among Black individuals than White individuals raises concern that abortion restrictions have the potential to worsen existing health inequities. To translate these findings into action, policymakers should support efforts to address IPV, including wide-ranging approaches such as improving access to education, reducing poverty, implementing and enforcing restraining orders, and offering no-fault divorce (32) — particularly in highly restrictive states. Since Black individuals face greater risk, policies should also comprehensively address the specific needs of this population, including addressing structural barriers to seeking care such as historical racism, perceived discrimination, and medical distrust (30). Health care providers play a critical role in identifying and intervening on IPV/DV, while health care systems may help reduce structural barriers to care and advocate for appropriate health care policy. Finally, future research is needed to determine if abortion restrictions disproportionately impact IPV/DV rates among other vulnerable subpopulations. The relationship between abortion restrictions, IPV/DV, and race remains complex and demonstrates the importance of ensuring access to reproductive health care in all populations.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The datasets analyzed for this study are available to researchers via request to the Center for Disease Control and Prevention's (CDC's) Pregnancy Risk Assessment Monitoring System (PRAMS). Requests to access these datasets should be directed to https://www.cdc.gov/prams/php/data-research/index.html.
Ethics statement
The studies involving humans were approved by HUM00204182; University of Michigan. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
KN: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. SH: Writing – original draft, Writing – review & editing. RO: Conceptualization, Methodology, Writing – review & editing. AP: Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing. KZ: Conceptualization, Funding acquisition, Writing – review & editing. AM-E: Investigation, Methodology, Writing – review & editing. LM: Investigation, Writing – review & editing. YK: Writing – review & editing. AZ: Methodology, Validation, Writing – review & editing. KD-W: Project administration, Supervision, Writing – review & editing. AC: Writing – review & editing. VD: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Institute on Minority Health and Health Disparities (grant number R01 MD014958), which played no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Acknowledgments
We thank the PRAMS Working Group, which includes the PRAMS Team, Division of Reproductive Health, CDC and the following PRAMS sites for their role in conducting PRAMS surveillance and allowing the use of their data: PRAMS Alabama, PRAMS Alaska, PRAMS Arizona, PRAMS Arkansas, PRAMS Colorado, PRAMS Connecticut, PRAMS Delaware, PRAMS Florida, PRAMS Georgia, PRAMS Hawaii, PRAMS Illinois, PRAMS Iowa, PRAMS, Kansas, PRAMS Kentucky, PRAMS Louisiana, PRAMS Maryland, PRAMS Massachusetts, PRAMS Michigan, PRAMS Mississippi, PRAMS Missouri, PRAMS Montana, PRAMS, Nebraska, PRAMS New Hampshire, PRAMS New Jersey, PRAMS New Mexico, PRAMS North Dakota, PRAMS Oregon, PRAMS Pennsylvania, PRAMS South Dakota, PRAMS Tennessee, PRAMS Utah, PRAMS Virginia, PRAMS Washington, PRAMS West Virginia, PRAMS Wisconsin, PRAMS Wyoming.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Leemis RW, Friar N, Khatiwada S, Chen MS, Kresnow M-j, Smith SG, et al. The National Intimate Partner and Sexual Violence Survey: 2016/2017 Report on Intimate Partner Violence (2022). Available online at: https://www.cdc.gov/violenceprevention/pdf/nisvs/nisvsreportonipv_2022.pdf (Accessed February 22, 2024).
2. Roman-Galvez RM, Martin-Pelaez S, Fernandez-Felix BM, Zamora J, Khan KS, BuenoCavanillas A. Worldwide prevalence of intimate partner violence in pregnancy. A systematic review and meta-analysis. Front Public Health. (2021) 9:738459. doi: 10.3389/fpubh.2021.738459
3. Pastor-Moreno G, Ruiz-Pérez I, Henares-Montiel J, Escribà-Agüir V, Higueras-Callejón C, Ricci-Cabello I. Intimate partner violence and perinatal health: a systematic review. BJOG. (2020) 127(5):537–47. doi: 10.1111/1471-0528.16084
4. Shah PS, Shah J. Knowledge synthesis group on determinants of preterm LBWB. Maternal exposure to domestic violence and pregnancy and birth outcomes: a systematic review and meta-analyses. J Womens Health. (2010) 19(11):2017–31. doi: 10.1089/jwh.2010.2051
5. Sheikh J, Allotey J, Kew T, Fernández-Félix BM, Zamora J, Khalil A, et al. Effects of race and ethnicity on perinatal outcomes in high-income and upper-middle-income countries: an individual participant data meta-analysis of 2,198,655 pregnancies. Lancet. (2022) 400(10368):2049–62. doi: 10.1016/S0140-6736(22)01191-6
6. Lawn RB, Koenen KC. Homicide is a leading cause of death for pregnant women in US. Br Med J. (2022) 379:o2499. doi: 10.1136/bmj.o2499
7. Margerison CE, Roberts MH, Gemmill A, Goldman-Mellor S. Pregnancy-associated deaths due to drugs, suicide, and homicide in the United States, 2010–2019. Obstet Gynecol. (2022) 139(2):172–80. doi: 10.1097/AOG.0000000000004649
8. Modest AM, Prater LC, Joseph NT. Pregnancy-associated homicide and suicide: an analysis of the national violent death reporting system, 2008–2019. Obstet Gynecol. (2022) 140(4):565–73. doi: 10.1097/AOG.0000000000004932
9. Campbell J, Matoff-Stepp S, Velez ML, Cox HH, Laughon K. Pregnancy-associated deaths from homicide, suicide, and drug overdose: review of research and the intersection with intimate partner violence. J Womens Health. (2021) 30(2):236–44. doi: 10.1089/jwh.2020.8875
10. D'Angelo DV, Bombard JM, Lee RD, Kortsmit K, Kapaya M, Fasula A. Prevalence of experiencing physical, emotional, and sexual violence by a current intimate partner during pregnancy: population-based estimates from the pregnancy risk assessment monitoring system. J Fam Violence. (2022) 38(1):117–26. doi: 10.1007/s10896-022-00356-y
11. Woo J, Fine P, Goetzl L. Abortion disclosure and the association with domestic violence. Obstet Gynecol. (2005) 105(6):1329–34. doi: 10.1097/01.AOG.0000159576.88624.d2
12. Coyle CT, Shuping MW, Speckhard A, Brightup JE. The relationship of abortion and violence against women: violence prevention strategies and research needs. Issues Law Med. (2015) 30(2):111–27.26710370
13. Roberts SC, Biggs MA, Chibber KS, Gould H, Rocca CH, Foster DG. Risk of violence from the man involved in the pregnancy after receiving or being denied an abortion. BMC Med. (2014) 12:144. doi: 10.1186/s12916-014-0144-z
14. Tobin-Tyler E. A grim new reality—ntimate-partner violence after dobbs and bruen. N Engl J Med. (2022) 387(14):1247–9. doi: 10.1056/NEJMp2209696
15. Guttmacher Institute. Interactive Map: US Abortion Policies and Access After Roe (2024). Available online at: https://states.guttmacher.org/policies/ (Accessed February 22, 2024).
16. Brown BP, Hebert LE, Gilliam M, Kaestner R. Association of highly restrictive state abortion policies with abortion rates, 2000–2014. JAMA Netw Open. (2020) 3(11):e2024610. doi: 10.1001/jamanetworkopen.2020.24610
17. Zandberg J, Waller R, Visoki E, Barzilay R. Association between state-level access to reproductive care and suicide rates among women of reproductive age in the United States. JAMA Psychiatry. (2023) 80(2):127–34. doi: 10.1001/jamapsychiatry.2022.4394
18. Shulman HB, D'Angelo DV, Harrison L, Smith RA, Warner L. The pregnancy risk assessment monitoring system (PRAMS): overview of design and methodology. Am J Public Health. (2018) 108(10):1305–13. doi: 10.2105/AJPH.2018.304563
19. Nash E, Guttmacher Institute. State Abortion Policy Landscape: From Hostile to Supportive (2019). Available online at: https://www.guttmacher.org/article/2019/08/state-abortionpolicy-landscape-hostile-supportive (Accessed February 22, 2024).
20. Upadhyay UD, McCook AA, Bennett AH, Cartwright AF, Roberts SCM. State abortion policies and medicaid coverage of abortion are associated with pregnancy outcomes among individuals seeking abortion recruited using Google Ads: a national cohort study. Soc Sci Med. (2021) 274:113747. doi: 10.1016/j.socscimed.2021.113747
21. Saftlas AF, Wallis AB, Shochet T, Harland KK, Dickey P, Peek-Asa C. Prevalence of intimate partner violence among an abortion clinic population. Am J Public Health. (2010) 100(8):1412–5. doi: 10.2105/AJPH.2009.178947
22. Mauldon J, Foster DG, Roberts SC. Effect of abortion vs. Carrying to term on a woman’s relationship with the man involved in the pregnancy. Perspect Sex Reprod Health. (2015) 47(1):11–8. doi: 10.1363/47e2315
23. Redd SK, Hall KS, Aswani MS, Sen B, Wingate M, Rice WS. Variation in restrictive abortion policies and adverse birth outcomes in the United States from 2005 to 2015. Womens Health Issues. (2022) 32(2):103–13. doi: 10.1016/j.whi.2021.10.006
24. Waters ET, Escoriaza PA, Griffin RG, Leifer FT. Amici Curiae Brief of 547 Deans, Chairs, Scholars and Public Health Professionals, the American Public Health Association, the Guttmacher Institute, and the Center for U.S. Policy, in Support of Respondents. Available online at: https://www.supremecourt.gov/DocketPDF/19/191392/193302/20210921172339465_19-1392%20Brief.pdf (Accessed February 22, 2024).
25. Truman JL, Morgan RE, Bureau of Justice Statistics. Nonfatal Domestic Violence, 2003–2012 (2014). Available online at: https://bjs.ojp.gov/library/publications/nonfatal-domestic-violence2003-2012 (Accessed February 22, 2024).
26. Sorenson SB, Schut RA. Nonfatal gun use in intimate partner violence: a systematic review of the literature. Trauma Violence Abuse. (2018) 19(4):431–42. doi: 10.1177/1524838016668589
27. Holliday CN, McCauley HL, Silverman JG, Ricci E, Decker MR, Tancredi DJ, et al. Racial/ethnic differences in women’s experiences of reproductive coercion, intimate partner violence, and unintended pregnancy. J Womens Health. (2017) 26(8):828–35. doi: 10.1089/jwh.2016.5996
28. Basile KC, Smith SG, Liu Y, Miller E, Kresnow MJ. Prevalence of intimate partner reproductive coercion in the United States: racial and ethnic differences. J Interpers Violence. (2021) 36(21–22):NP12324-NP41. doi: 10.1177/0886260519888205
29. Gillum TL. The intersection of intimate partner violence and poverty in black communities. Aggress Violent Behav. (2019) 46:37–44. doi: 10.1016/j.avb.2019.01.008
30. Stockman JK, Hayashi H, Campbell JC. Intimate partner violence and its health impact on ethnic minority women [corrected]. J Womens Health. (2015) 24(1):62–79. doi: 10.1089/jwh.2014.4879
31. Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. (2019) 40:105–25. doi: 10.1146/annurev-publhealth-040218-043750
32. Oram S, Fisher HL, Minnis H, Seedat S, Walby S, Hegarty K, et al. The lancet psychiatry commission on intimate partner violence and mental health: advancing mental health services, research, and policy. Lancet Psychiat. (2022) 9(6):487–524. doi: 10.1016/S2215-0366(22)00008-6
33. ACOG committee opinion No. 518: intimate partner violence. Obstet Gynecol. (2012) 119(2 Pt 1):412–7. doi: 10.1097/AOG.0b013e318249ff74
34. Alliance for Innovation on Maternal Health. Community Care to Address Intimate Partner Violence During and After Pregnancy. Available online at: https://www.aimcci.org/community-care-to-address-intimate-partner-violence-during-and-after-pregnancy/ (accessed March 14, 2025).
Keywords: intimate partner violence, domestic violence, abortion, policy, health disparities
Citation: Neff K, Hall SV, Owda R, Pangori A, Zivin K, Montoya A, McDonnaugh-Eaddy L, Kusunoki Y, Zeoli AM, Davis-Wilson K, Courant A and Dalton VK (2025) State abortion restrictiveness and prevalence of intimate partner violence and domestic violence among recently birthing black and white individuals. Front. Reprod. Health 7:1535865. doi: 10.3389/frph.2025.1535865
Received: 28 November 2024; Accepted: 26 March 2025;
Published: 14 April 2025.
Edited by:
Courtenay Sprague, University of Massachusetts Boston, United StatesReviewed by:
Muswamba Mwamba, Stephen F. Austin State University, United StatesShelley Brown, Boston University, United States
Copyright: © 2025 Neff, Hall, Owda, Pangori, Zivin, Montoya, McDonnaugh-Eaddy, Kusunoki, Zeoli, Davis-Wilson, Courant and Dalton. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Katherine Neff, bmVmZmtAdW1pY2guZWR1
 Katherine Neff
Katherine Neff Stephanie V. Hall
Stephanie V. Hall Rieham Owda1,2
Rieham Owda1,2 Andrea Pangori
Andrea Pangori April M. Zeoli
April M. Zeoli Vanessa K. Dalton
Vanessa K. Dalton