- 1Department of Health Behavior, University of North Carolina, Gillings School of Global Public Health, Chapel Hill, NC, United States
- 2Department of Maternal and Child Health, University of North Carolina, Gillings School of Global Public Health, Chapel Hill, NC, United States
Background: In vitro fertilization (IVF) is an increasingly common method of assisted reproduction given the high rates of infertility in the United States (U.S.). However, despite growing utilization of IVF technologies, there is little known about the experiences of those accessing or undergoing IVF, particularly among adults in the U.S. The aims of this review are to (1) explore how economic, emotional and physical health, and interpersonal relationships impact and are impacted by accessing or undergoing IVF, and (2) understand the role of healthcare providers and the healthcare system.
Methods: A narrative review was conducted to summarize the current literature and provide insight into potential channels for care improvement. Eligible studies were published in English from 2013 to 2024 which qualitatively evaluated experiences of individuals and couples accessing or undergoing IVF. Peer-reviewed publications were identified from three electronic bibliographic databases. Methodologic rigor was assessed by two reviewers who also abstracted data on the study's characteristics as they pertained to four domains: health systems, economic, interpersonal, and physical and emotional health. Among the 32 papers retrieved for review, 22 met inclusion criteria and were retained for analysis.
Results: The available literature suggests accessing and undergoing IVF can be positively and negatively influenced by health systems, economic, interpersonal, and physical and emotional health factors. Often an individual or couple experiences multiple factors that compound to create a complex situation. Health systems-related factors included physician interaction and challenges with information volume and processing. Economic challenges primarily pertained to financing IVF and navigating insurance coverage. Interpersonal factors related to changes in relationships with partners, family members, and friends due to IVF. Physical health concerns (e.g., pain) and emotional health concerns (e.g., sadness, stress) were also noted by all included papers.
Conclusions: Efforts to improve care experiences of adults accessing or undergoing IVF are urgently needed. The evidence base points to a need for provider sensitivity trainings, clinic-based intervention, and community education in both physical and virtual spaces.
Introduction
Over the past decades, in vitro fertilization (IVF) has become an established and effective medical treatment for various forms of infertility (1)—in partial response to the demographic trend of delayed parenting in the United States (U.S) (2). Infertility is defined as an inability to attain a successful pregnancy after timed unprotected intercourse or therapeutic donor insemination for 12 or more months (3, 4). Approximately 19% of married women aged 15–49 years in the U.S. experience infertility (5), resulting in roughly 7 million U.S. couples seeking care for infertility each year (6). The number of pregnancies that are conceived via IVF in the U.S. increases annually, representing 79,942 live births stemming from IVF in 2020 or 2.2% of all births in the U.S (7, 8). An IVF treatment cycle commonly includes ovarian stimulation, the retrieval of oocytes, and fertilization of collected oocytes and embryo culture, followed by the resultant embryos being transferred to the patient's uterus for immediate conception and/or being transferred to cryostorage for later use, and progesterone supplementation (1, 3, 4, 9). IVF patients and their partners undergo these medical treatments and required monitoring at varying pace through the health care system (10). An IVF cycle is complete once all frozen and/or fresh embryos have been transferred (3, 4, 9).
Qualitative research elicits beliefs and opinions about people's lived experiences using their own words and can provide rich contextual insight to inform clinical practice (11). Yet, despite increasing utilization of IVF in the U.S. and a growing recognition by the assisted reproduction community to understand IVF care practices, there is limited qualitative evidence regarding U.S. patients’ IVF care experiences. Most U.S.-based studies of IVF-treated patients have centered on quantitative clinical outcomes relating to pregnancy and childbirth (12–15). On the other hand, most qualitative studies with patients and providers at fertility clinics have been conducted outside of the U.S., predominately in in Europe (10, 16–22), Asia (23–27), Australia (28, 29), and some regions of Africa (30).
Qualitative research outside of the U.S. has shown that IVF patients and their partners face a number of challenges. Undergoing IVF treatment can involve pain from the hormonal injections and emotional distress, such as anxiety, sadness, or depression, in anticipation of or after a cycle fails (16, 22, 25, 28, 30, 31). Patients must also manage disruptions to their daily lives from treatment appointments and cope with the financial stress of affording the resources they need for treatment (16, 17, 25). IVF couples undergo an average of 2.7 cycles, spending $61,377 USD out-of-pocket, to achieve a live birth (32, 33). In addition, despite technological advances, success rates of IVF are moderate. Although a total of 326,471 IVF cycles were carried out in the U.S. in 2020 (7, 34), only 23% resulted in a live birth (7). Thus, the majority of IVF patients must consider other pathways to parenthood, such as foregoing their desires for parenthood or adoption. At increasing costs, patients may repeat IVF treatments for months or years prior to pregnancy or prior to discontinuing attempts of biological parenthood. This has resulted in some patients voicing frustration about fertility clinics providing overly positive false hopes regarding their chances of success (18, 28, 35).
Despite the abundance of qualitative research in other countries, little is known about U.S. women's IVF care experiences in their own words. Questions remain about qualitative themes relating to health systems experiences, such as how patients select fertility clinics, their perceptions of how providers present IVF information and subsequently discuss procedures and chances, their views on how clinics support them through treatment challenges, or quality and continuity of care (16–18). Questions also remain about themes relating to economic experiences, such as how patients determine expected IVF care costs and the perceived impact of IVF expenses on households (10, 36). Only 15 out of 50 states (∼30%) mandate private insurance coverage for some infertility treatments and only four states (e.g., IL, MA, NJ, RI) offer comprehensive mandated health insurance for IVF (up to 4 IVF cycles) (13, 14). Further, only one state (e.g., NY) mandates Medicaid coverage for fertility services, specifically fertility testing and fertility medications, while no state Medicaid program provides coverage for intra-uterine insemination (IUI) or IVF (14, 37). Information is also lacking on the physical and emotional experiences of IVF patients, such as coping with time requirements, pain, or anxiety, or interpersonal experiences, such as how patients decide to continue or end treatment, how they discuss IVF with others, or how they adjust to parenting or non-parenting outcomes (38). A deeper analysis of existing qualitative IVF studies in the U.S. could help to develop appropriate interventions and policies to improve patients’ experiences during assisted reproduction. Ultimately, reducing infertility-related stressors could improve maternal and child health outcomes of biological and adopted children (22, 39–41).
This study aimed to explore the following research questions: (1) How does IVF impact the financial, emotional, and physical wellbeing of women who access or undergo IVF treatment or consultation? (2) What is the role of the healthcare system, including fertility clinics and providers, in the overall experience of accessing or undergoing IVF treatment or consultation? (3) How does accessing or undergoing IVF impact interpersonal relationships? This study reviews what is known about IVF care experiences in the U.S. among studies using qualitative data generated from women undergoing, planning to undergo, or having undergone IVF. To our knowledge, this study is one of the first narrative reviews of qualitative studies examining IVF care experiences in the United States. Findings are intended to summarize the state of the qualitative evidence and to provide insight on potential ways to improve clinical and community-based IVF practices.
Methods
Search strategy
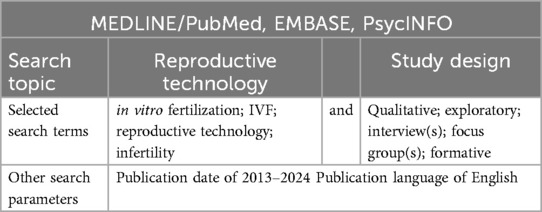
Table 1 lists the search topics, terms, and parameters used in the narrative review. We aimed to identify in vitro fertilization studies that involved qualitative research methods. Three electronic bibliographic databases were used. These were: MEDLINE/PubMed, PsycINFO, and Excerpta Medica Database (EMBASE). These databases were selected to cover a broad range of disciplines, including medical, public health, psychological, and social science research. The search terms included words related to the review's topic (e.g., IVF) and study design (e.g., qualitative) and included synonyms and spelling variations, where applicable (Table 1).
Inclusion criteria
Studies that met the following criteria were included: (i) research on women who had experience with IVF consultation or treatment; (ii) research that reported qualitative findings of IVF experiences; (iii) research that was performed in the United States (U.S.); and (iv) research that was published in English over the last decade, between 2013 and 2024, up to the time of publication of this review. Exclusion criteria included non-research publications (e.g., chapters, commentaries, protocols, editorials, conference abstracts), studies published in languages other than English, studies conducted with populations outside of the U.S., and studies that lacked qualitative findings relating to IVF.
Title, abstract, and article screening
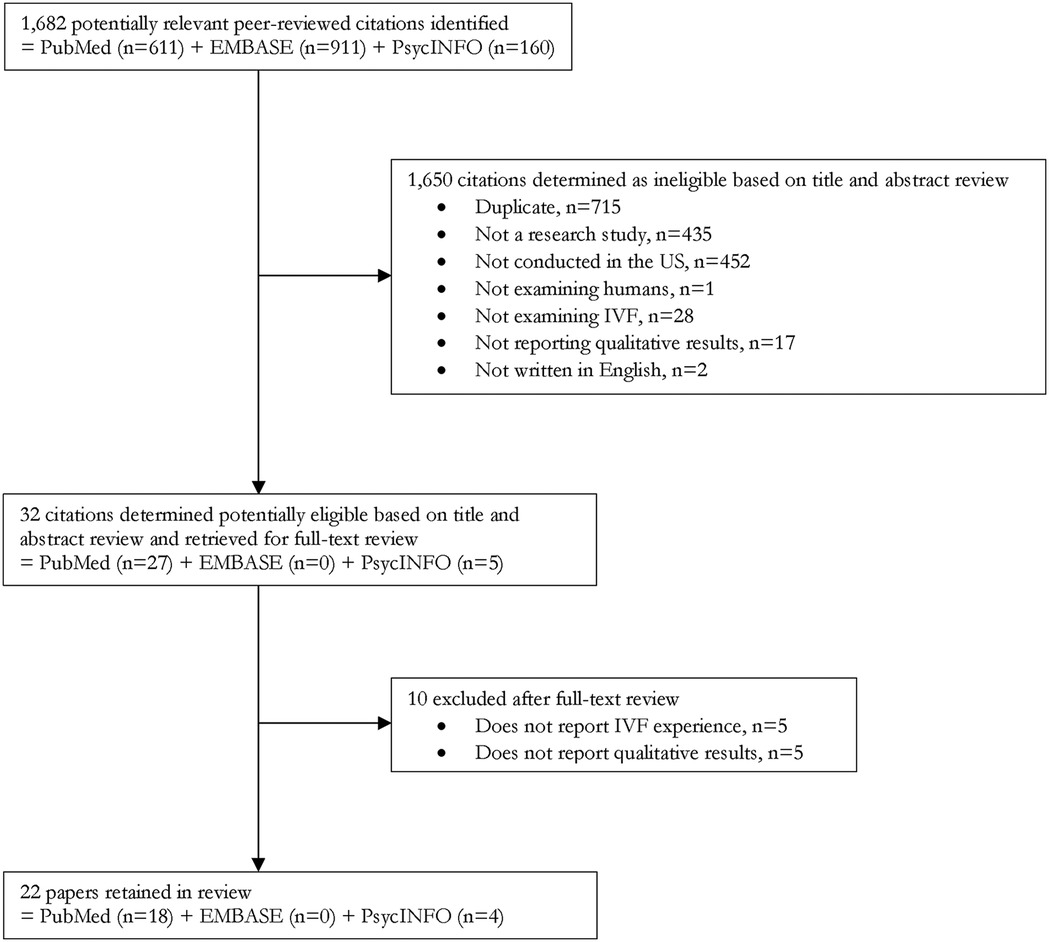
Figure 1 illustrates the search and screening process. Once the search terms were applied to the electronic databases, potentially relevant citations were selected based on the screening of the title and abstract by the primary reviewer (e.g., the first author), who then downloaded the full-text publication. All full-text publications were then reviewed by two reviewers (e.g., the first and second or third authors) to further assess eligibility. Each reviewer independently excluded publications not meeting the inclusion criteria. Discrepancies in study eligibility were discussed and corrected based on consensus. Once this process was completed with MEDLINE/PubMed, the reviewers began the process again with PsycINFO and EMBASE databases and extracted and reviewed potentially relevant citations that were not duplicates. All citations were entered into an Excel database to track the retrieval process and document reasons for inclusion or exclusion.
Study appraisal
A final set of selected articles underwent a systematic appraisal by two appraisers (e.g., the first and second or third authors) in addition to a rapid review by an ad hoc reviewer (e.g., the second author) (Table 2). Data were extracted and documented in a study appraisal form for the following items: article identification number, author, year of publication, title, search strategy source, publication journal, study design, study objective, sample/participants, and key findings across four assessment domains: (i) health systems findings, (ii) economic findings, (iii) interpersonal/social findings, and (iv) physical and emotional findings. Data were also extracted on suggestions made by the publications’ authors relating to strategies to improve IVF care. Each publication's two appraisal forms were compared and used to synthesize and write the review's results.

Table 2. Summary of publication characteristics and research findings by domain for selected studies (N = 22).
Quality assessment
As part of the study appraisal, the methodological rigor of each article's qualitative methods was also assessed Table 3). We adapted Jennings & Gagliardi's 10-item quality assessment checklist for use in the current review (64). The checklist item “Report of intervention implementation detail to facilitate replication” was removed as it is not relevant for the current review's inclusion criteria. The checklist evaluated whether the study included: prolonged engagement in a study setting, justification for design and methods selected, justification of the sampling strategy, description of analytical methods, use of verification methods to demonstrate credibility, provision of a reflexivity account, detailed report of findings, balanced representation of viewpoints, or presentation of conclusions supported by the data. Each quality item was scored on a binary scale, with 0 indicating the absence of the quality item and 1 indicating the presence of the quality item. Studies that received ≤4 points were categorized as having weak quality compared to moderate quality (5–6 points) or high quality (7–9 points).
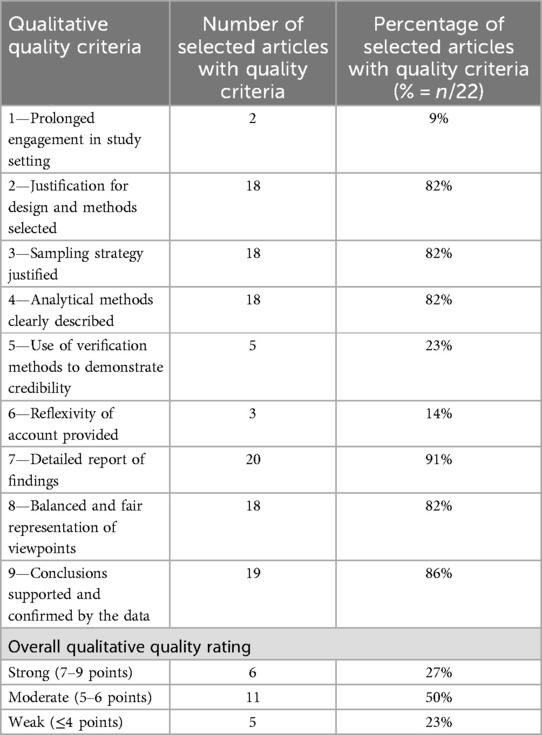
Table 3. Distribution of qualitative quality criteria and overall rating for selected articles (N = 22).
Synthesis process
A content analysis approach was used to synthesize findings. First, we extracted and summarized findings by assessment domain for each article using the study appraisal form. Assessment domains were chosen to capture the scope of the literature based on an exploratory review and selected to inform future improvements in quality of care at the community and clinical levels (65, 66). To do so, all three reviewers (e.g., the first, second, and third authors) read each publication and its appraisal forms several times to interpret the summation of findings. These findings are reported by article row in Table 2. Next, we synthesized findings across applicable studies within each assessment domain by discussing connections between the article findings and each assessment domain. This synthesis of the findings for the total sample of articles by assessment domain is reported in the review's results section. A final step included summarizing implications for improving IVF care for adults in clinical or community settings in the U.S.
Results
Search and review process
Thirty-two (n = 32) full-text articles were retrieved for review from 1,682 potentially relevant citations based on the publication's title and abstract (Figure 1). The retrieved full-text articles were reviewed for eligibility, and ten (n = 10) were excluded. The most common reasons for exclusion were lack of assessment of experiences relating to IVF and lack of qualitative findings. We also excluded duplicates and publications that were not research articles, such as commentaries, protocols, editorials, or conference abstracts. An account of the number of exclusions is shown in Figure 1.
Characteristics of selected studies
Twenty-two (n = 22) studies were retained in the final group of articles (42, 63). All the selected studies were pulled from an electronic database. The characteristics of the final set of studies are presented in Table 2. Although the search spanned over the past decade, most studies (n = 15; 68%) (42–44, 46, 47, 52, 53, 55–57, 59–63) were recently published within the last four and a half years (2020–2024). The majority of studies (n = 15; 68%) (44–46, 48–55, 57, 58, 62, 63) involved cross-sectional individual interviews with the exception of three studies (14%) that extracted qualitative online posts from social media (56, 59, 60), one study (5%) that involved repeated individual interviews (42), and three studies (14%) that used an open-text qualitative question that was added to a quantitative survey (43, 47, 61) (Table 2). Other qualitative methods such as focus group discussions or direct observations were not used. The qualitative sample sizes included small to large samples of 3–202 study participants in addition to 97–452 online qualitative posts (Table 2). All studies reported qualitative findings pertaining to at least one of the review's four assessment domains.
Methodological quality
Table 3 summarizes the quality assessment of the selected articles. Six studies (27%) were rated as having strong qualitative methodological rigor (7–9 points). Eleven studies (50%) were rated as moderate (5–6 points), and five studies (23%) were rated as weak (≤4 points). We did not exclude studies with weak ratings given the limited number of relevant publications and the need to summarize findings. This is recommended for low-rated studies with no critical deficiencies (64). The most common methodological strengths were detailed report of findings with confirming quotations and conclusions supported and confirmed by the data (Table 3). The most common methodological weaknesses were absence of verification methods (e.g., member checking, triangulation, divergent case finding), omitted reflexivity, and lack of prolonged engagement, such as use of repeated or longitudinal inquiries.
Health systems findings
Health systems findings, both positive and negative, were reported in the full set of included qualitative studies (N = 22), although most findings highlighted challenges in navigating IVF clinical systems (Table 2). Positive health systems findings were that patients found clinicians helpful in providing information and literature to understand the IVF process. They also valued living in communities with accredited fertility clinics given the challenge of transferring records and embryos. In some cases, patients also described appreciating mental health counseling referrals that were integrated into their IVF protocol. Despite these positive findings, the literature described numerous challenges in quality and continuity of care for individuals seeking or undergoing IVF. These challenges included feeling overwhelmed by the amount and type of clinical information, difficulty understanding information provided, feeling excluded in or misled by care decisions, disliking insensitive language used by clinicians, having difficulty managing multiple and uncoordinated providers and specialists, feeling that fertility concerns were invalidated by clinicians, and having difficulty obtaining timely diagnoses and care. Women were reported to be the most common initial contact to the health system for IVF usually with their primary care physician or OB/GYN who then referred them to a reproductive endocrinologist. They also relied on online patient data and reviews to select a fertility clinic or online forums to assist in interpreting IVF lab results. A few studies examined differences in health systems experiences for IVF patients due to COVID protocols, gender, age, or provider characteristics, although this was a less common approach.
Economic findings
Economic experiences relating to IVF were assessed by about half of the included studies (N = 13), all describing the cost of IVF as a negative experience and primary barrier to utilization (Table 2). IVF patients reported using their credit cards and savings, taking out loans, or selling their belongings to cover care costs, which varied by state or metropolitan area. Some individuals regretted their lack of financial preparation for IVF or regretted not spending money earlier in life on fertility preservation (e.g., cryopreservation or egg freezing). Others reported difficulty understanding the potential costs and worry about whether insurance would cover any of the cost of treatment. In contrast, the literature also showed that some IVF patients struggled to rationalize whether the payments they made were worth it, including attributing decisions to discontinue IVF to high costs. Still others’ limited knowledge of their financial options (e.g., insurance, co-pays, loans) were described as a barrier to seeking care. The current literature also showed that individuals experienced additional financial strain when paying for complementary medical procedures (e.g., supplements, acupuncture, counseling) to cope with and supplement IVF. A few studies reported differences in economic experiences of IVF patients, noting that individuals from higher-income households could initiate IVF treatment more quickly or that clinicians sometimes made assumptions about one's ability to pay based on race or socio-economic status. A final economic finding was that IVF patients were concerned about the profit interests of clinics who encouraged paying patients to continue treatment even if their chance of success was low.
Interpersonal and social findings
Interpersonal IVF experiences were almost always assessed in the qualitative literature (N = 20) and included concurrently affirming and non-affirming encounters (Table 2). For example, friends and families were characterized as important sources of social support, but were also reported as sources of stress from negative feedback, unwanted advice, and limited knowledge on how to help. Individuals also found it burdensome to have to educate their friends and family about IVF. A complaint was also how little infertility was discussed in participants’ current or former social circles. For this reason, the literature often noted that individuals undergoing IVF received the most support from people who had prior IVF experiences, especially women. Counseling and support groups were also described as positive opportunities to learn more about IVF and to connect with others with similar experiences. Yet, for some individuals, the literature also reported reluctance to discuss IVF with others to maintain privacy. Complex experiences were most commonly described with sexual partners, where the ups and downs of IVF were experienced jointly—as a couple. Yet, sometimes, individuals were uncertain how to alleviate their partner's stress or found it difficult to express their feelings with their partner.
Physical and emotional findings
Nearly all articles (N = 21) reported on physical and emotional effects of IVF (Table 2). The most common finding was that individuals undergoing IVF experience frustration, anger, fear, and sadness from their IVF experiences. Findings also suggested that emotional effects varied by gender. One study found that men felt emasculated by infertility diagnoses, while women felt alarmed and surprised given the dominant narrative on pregnancy prevention. Another study found that the partner of the woman undergoing IVF felt worried for her future physical health given the impact the treatment would have on his partner's body. While most articles described negative emotions, two studies discussed feelings of happiness, excitement, and gratefulness for the benefits provided by IVF. However, a lack of knowledge around mental health resource options was expressed as a contributing factor to the overall emotional experience. Physical findings centered on the difficulty managing pain, fatigue, or related IVF side effects.
Authors’ suggestions to improve IVF care
Numerous suggestions were provided by authors to improve IVF care (Table 2). At the clinic level, suggested interventions included increased training of health care providers, provision of more information on IVF options and costs, changes in policies requiring infertility diagnosis or assignment, standardized referrals for mental health services, and encouragement of clinic attendance with partners, as applicable. At the community level, suggested interventions included sharing more stories of IVF experiences across various racial and socio-economic groups (to minimize stereotypes), educating friends and families about how to help IVF peers, and expanding sexual health education to include use of assisted reproductive technologies (ART). Many of these suggestions were also mentioned by study participants.
Discussion
To our knowledge, this narrative review is the first to-date to examine the current qualitative evidence of IVF experiences among U.S. adults. Findings showed that individuals accessing and undergoing IVF encounter complex and intersecting positive and negative experiences when navigating the health system, interpersonal relationships, and economic, emotional, and physical treatment requirements. We found that, while the current qualitative literature has variable methodological quality, it has grown in recent years and provides several recommendations for potentially improving IVF care experiences in community and clinical settings.
Findings showed that interactions with the healthcare system, via clinics and practitioners, yielded mixed feelings about standard of care procedures and treatment. The cost-prohibitive nature of IVF and navigating variable insurance coverage were both sources of stress and barriers to treatment utilization. The review also found that accessing or undergoing IVF impacted friendships, families, and partner relationships the most. In few cases relationships were strengthened, but in most others unsolicited advice, insensitive language, and lack of understanding caused strain. Many of the included studies also reported on the physical (e.g., pain, medication side effects) and emotional (e.g., stress, negative affect) toll of IVF. The literature points to a need for improved IVF care experience in clinical settings, and increased support in both the clinical and community spheres. The authors of the included studies also provided potential solutions, including health care provider trainings (e.g., trauma-informed care, provider sensitivity trainings), increased information dissemination, and experience sharing in clinics and the community.
While much of the literature centers around heterosexual women, particularly White women, and their experiences with IVF, one encouraging finding was the query of men and people of color on their experiences with IVF in the analyzed sample. However, we didn't find any literature centered around non-binary individuals, same-sex couples, or single (i.e., unpartnered) individuals, which is an area for future research. Understanding how ethical issues concerning malpractice and negligence in the IVF setting [e.g., failure to fully genetically test donor sperm (67), switching patient embryos (68)] impact patient-provider relationships, patient trust in the healthcare system, and fertility outcomes is an important area for further exploration. Future studies should also further examine the impact of location of intervention delivery, with the increasing reliance on digital spaces (i.e., social media) for information acquisition in addition to clinics and doctors’ offices. Finally, given the overturning of Roe v. Wade and its implications for reproductive and fertility care in the US, future research should explore the impact of healthcare access policy on IVF care experiences.
Limitations
The limitations of this study should be considered. The search process was limited to studies that were published in English and that were available in peer-reviewed databases. As a result, findings may not be transferrable to non-English-speaking communities or representative of studies published in the gray literature. Additionally, the search was limited to studies that contained search strategy terminology in the title or abstract, leaving potentially relevant literature unidentified. However, strengths of this review include use of a systematic approach to identify, appraise, and synthesize findings of studies, review by multiple members of the study team, assessment of multiple topical domains, review of methodological rigor, and inclusion of the last 10 years of literature on IVF experiences.
Conclusion
The qualitative literature of IVF experience necessitates more research specifically aimed at improving access, care experience, and social support in the health system and economic realms, and at the community level through interpersonal relationships. Currently, findings suggest that the experience of those accessing or undergoing IVF is fraught with stressors, from cost of treatment and complementary therapies to interactions with health care providers, friends, and family. In tandem with more research, increased education is urgently needed to begin de-stigmatizing the use ARTs and promoting, rather than hindering, positive social support and interactions.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the submitted systematic review focuses on qualitative studies and all data analyzed have been previously published in other peer-reviewed journals. Additionally, no primary data are being made available with this manuscript. Requests to access these datasets should be directed to corresponding authors of included manuscripts. All manuscripts included in the review are cited in-text and in the references.
Author contributions
SP: Writing – original draft, Writing – review & editing. LJ: Writing – original draft, Writing – review & editing. LS: Writing – original draft, Writing – review & editing. IM: Writing – original draft, Writing – review & editing. AP: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded through faculty discretionary resources provided by the University of North Carolina. The content is solely the responsibility of the authors and does not necessarily represent the official views of UNC.
Acknowledgments
The authors wish to thank the qualitative researchers, fertility clinics, and study participants who contributed to the articles included in this narrative review, without whom this analysis would not have been possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ART, assisted reproductive technology; CA, California; DC, Washington D.C.; GYN, gynecologist; IVF, in vitro fertilization; IL, Illinois; IUI, intra-uterine insemination; MA, Massachusetts; MO, Missouri; ND, not discussed; NJ, New Jersey; OB, obstetrician; PCP, primary care physician; RI, Rhode Island; US, United States; USD, United States dollar.
References
1. Niederberger C, Pellicer A, Cohen J, Gardner DK, Palermo GD, O'Neill CL, et al. Forty years of IVF. Fertil Steril. (2018) 110(2):185–324.e5. doi: 10.1016/j.fertnstert.2018.06.005
2. Matthews TJ, Hamilton BE. Delayed childbearing: more women are having their first child later in life. NCHS Data Brief. (2009) 21:1–8. https://www.cdc.gov/nchs/data/databriefs/db21.pdf
3. American Society of Reproductive Medicine (ASRM) Practice Committee. Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril. (2013) 99(1):63. doi: 10.1016/j.fertnstert.2012.09.023
4. Beckmann C. Infertility Obstetrics and Gynecology. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins (2014). p. 371–80.
5. Centers for Disease Control and Prevention (CDC). Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion. Infertility FAQs. Atlanta, GA: Centers for Disease Control and Prevention (2023). Available online at: https://www.cdc.gov/reproductive-health/infertility-faq/ (Accessed May 04, 2023).
6. Eisenberg ML, Lathi RB, Baker VL, Westphal LM, Milki AA, Nangia AK. Frequency of the male infertility evaluation: data from the national survey of family growth. J Urol. (2013) 189(3):1030–4. doi: 10.1016/j.juro.2012.08.239
7. Centers for Disease Control and Prevention (CDC). ART National Data: Clinic Services and Profile. 2020 National Summary. Atlanta, GA: Centers for Disease Control and Prevention (2020). Available online at: https://nccd.cdc.gov/drh_art/rdPage.aspx?rdReport=DRH_ART.ClinicInfo&rdRequestForward=True&ClinicId=9999&ShowNational=1 (Accessed May 04, 2023).
8. Hamilton BE, Martin JA, Osterman MJK, National Vital Statistics System (NVSS). “NVSS Vital Statistics Rapid Release, Births: Provisional Data for 2020”. U.S. Department of Health and Human Services. Centers for Disease Control and Prevention (CDC). Hyattsville, MD: National Center for Health Statistics (2021). Available online at: https://www.cdc.gov/nchs/data/vsrr/vsrr012-508.pdf (Accessed May 04, 2023).
9. Fitzgerald O, Paul RC, Harris K, Chambers GM. Assisted Reproductive Technology in Australia and New Zealand 2016. Sydney: National Perinatal Epidemiology and Statistics Unit, the University of New South Wales (2018).
10. Redshaw M, Hockley C, Davidson LL. A qualitative study of the experience of treatment for infertility among women who successfully became pregnant. Hum Reprod. (2007) 22(1):295–304. doi: 10.1093/humrep/del344
11. Cristancho SM, Goldszmidt M, Lingard L, Watling C. Qualitative research essentials for medical education. Singapore Med J. (2018 Dec) 59(12):622–7. doi: 10.11622/smedj.2018093
12. Gunderson S, Jungheim ES, Kallen CB, Omurtag K. Public reporting of IVF outcomes influences medical decision-making and physician training. Fertil Res Pract. (2020) 6:1. doi: 10.1186/s40738-020-00070-7
13. Sunderam S, Kissin DM, Crawford SB, Folger SG, Boulet SL, Warner L, et al. Assisted reproductive technology surveillance—united States, 2014. MMWR Surveill Summ. (2018) 67(SS-3):1–28. doi: 10.15585/mmwr.ss6703a1
14. Weigel G, Ranji U, Long M, Salganicoff A. Coverage and use of Fertility Services in the U.S. Women's Health Policy. KFF. (2020). Available online at: https://www.kff.org/womens-health-policy/issue-brief/coverage-and-use-of-fertility-services-in-the-u-s/ (Accessed September 15, 2022).
15. Ribas-Maynou J, Yeste M, Becerra-Tomás N, Aston KI, James ER, Salas-Huetos A. Clinical implications of sperm DNA damage in IVF and ICSI: updated systematic review and meta-analysis. Biol Rev Camb Philos Soc. (2021) 96(4):1284–300. doi: 10.1111/brv.12700
16. Harrison C, Boivin J, Gameiro S. Talking about possible IVF/ICSI failure and need for multiple cycles in treatment planning: qualitative investigation of multi-cycle planning and its acceptability to patients and staff. Hum Reprod. (2022) 37(3):488–98. doi: 10.1093/humrep/deab278
17. Harrison C, Gameiro S, Boivin J. Patient willingness, preferences and decision-making about planning for three complete cycles of IVF/ICSI treatment. Hum Reprod. (2021) 36(5):1339–52. doi: 10.1093/humrep/deab040
18. Peddie VL, van Teijlingen E, Bhattacharya S. A qualitative study of women's decision-making at the end of IVF treatment. Hum Reprod. (2005) 20(7):1944–51. doi: 10.1093/humrep/deh857
19. van Peperstraten AM, Nelen WL, Hermens RP, Jansen L, Scheenjes E, Braat DD, et al. Why don’t we perform elective single embryo transfer? A qualitative study among IVF patients and professionals. Hum Reprod. (2008) 23(9):2036–42. doi: 10.1093/humrep/den156
20. Garel M, Blondel B, Karpel L, Blanchet V, Breart G, Frydman R, et al. Women’s views on friendly IVF: a qualitative preliminary study. J Psychosom Obstet Gynaecol. (2009) 30(2):101–4. doi: 10.1080/01674820802604896
21. Silva S, Barros H. Perspectives on access to in vitro fertilization in Portugal. Rev Saude Publica. (2012) 46(2):344–50. doi: 10.1590/S0034-89102012000200017
22. Hjelmstedt A, Widström AM, Wramsby H, Collins A. Emotional adaptation following successful in vitro fertilization. Fertil Steril. (2004) 81(5):1254–64. doi: 10.1016/j.fertnstert.2003.09.061
23. Yao H, Chan CHY, Hou Y, Chan CLW. Ambivalence experienced by infertile couples undergoing IVF: a qualitative study. Hum Fertil (Camb). (2022) 26:1–13. doi: 10.1080/14647273.2022.2099314
24. Lee GL, Hui Choi WH, Chan CH, Chan CL, Ng EH. Life after unsuccessful IVF treatment in an assisted reproduction unit: a qualitative analysis of gains through loss among Chinese persons in Hong Kong. Hum Reprod. (2009) 24(8):1920–9. doi: 10.1093/humrep/dep091
25. Ying LY, Wu LH, Loke AY. The experience of Chinese couples undergoing in vitro fertilization treatment: perception of the treatment process and partner support. PLoS One. (2015) 10(10):e0139691. doi: 10.1371/journal.pone.0139691
26. Boz İ, Teskereci G, Akgün M. The experience of becoming a mother following successful in vitro fertilization: a grounded theory. J Adv Nurs. (2021) 77(10):4170–83. doi: 10.1111/jan.14958
27. Su TJ, Chen YC. Transforming hope: the lived experience of infertile women who terminated treatment after in vitro fertilization failure. J Nurs Res. (2006) 14(1):46–54. doi: 10.1097/01.JNR.0000387561.03823.8e
28. Copp T, Kvesic D, Lieberman D, Bateson D, McCaffery KJ. ‘Your hopes can run away with your realistic expectations’: a qualitative study of women and men’s decision-making when undergoing multiple cycles of IVF. Hum Reprod Open. (2020) 2020(4):hoaa059. doi: 10.1093/hropen/hoaa059
29. Payne D, Goedeke S, Balfour S, Gudex G. Perspectives of mild cycle IVF: a qualitative study. Hum Reprod. (2012) 27(1):167–72. doi: 10.1093/humrep/der361
30. Zaake D, Kayiira A, Namagembe I. Perceptions, expectations and challenges among men during in vitro fertilization treatment in a low resource setting: a qualitative study. Fertil Res Pract. (2019) 5:6. doi: 10.1186/s40738-019-0058-8
31. Eugster A, Vingerhoets AJ. Psychological aspects of in vitro fertilization: a review. Soc Sci Med. (1999) 48(5):575–89. doi: 10.1016/S0277-9536(98)00386-4
32. Katz P, Showstack J, Smith JF, Nachtigall RD, Millstein SG, Wing H, et al. Costs of infertility treatment: results from an 18-month prospective cohort study. Fertil Steril. (2011) 95(3):915–21. doi: 10.1016/j.fertnstert.2010.11.026
33. Stewart LM, D'Arcy JH, Roger H, Finn J, Mai Q, Preen D. How effective is in vitro fertilization, and how can it be improved? Fertil Steril. (2011) 95(5):1677–83. doi: 10.1016/j.fertnstert.2011.01.130
34. Society for Assisted Reproductive Technology (SART). National Summary Report. Society for Assisted Reproductive Technology. (2020). Available online at: https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx (Accessed May 01, 2023).
35. Blakely B, Williams J, Mayes C, Kerridge I, Lipworth W. Conflicts of interest in Australia’s IVF industry: an empirical analysis and call for action. Hum Fertil. (2019) 22:230–7. doi: 10.1080/14647273.2017.1390266
36. Nachtigall RD, MacDougall K, Davis AC, Beyene Y. Expensive but worth it: older parents’ attitudes and opinions about the costs and insurance coverage for in vitro fertilization. Fertil Steril. (2012) 97(1):82–7. doi: 10.1016/j.fertnstert.2011.10.019
37. Vu M, Stuehling D, Li D, Alur-Gupta S. Fertility care for all: impact of New York State’s medicaid expansion on infertility care. J Assist Reprod Genet. (2024) 41(2):423–8. doi: 10.1007/s10815-023-02979-6
38. Vassard D, Lund R, Pinborg A, Boivin J, Schmidt L. The impact of social relations among men and women in fertility treatment on the decision to terminate treatment. Hum Reprod. (2012) 27(12):3502–12. doi: 10.1093/humrep/des353
39. Huffhines L, Coe JL, Busuito A, Seifer R, Parade SH. Understanding links between maternal perinatal posttraumatic stress symptoms and infant socioemotional and physical health. Infant Ment Health J. (2022) 43(3):474–92. doi: 10.1002/imhj.21985
40. Martins MV, Peterson BD, Almeida VM, Costa ME. Direct and indirect effects of perceived social support on women's infertility-related stress. Hum Reprod. (2011) 26(8):2113–21. doi: 10.1093/humrep/der157
41. Bush NR, Savitz J, Coccia M, Jones-Mason K, Adler N, Boyce WT, et al. Maternal stress during pregnancy predicts infant infectious and noninfectious illness. J Pediatr. (2021) 228:117–125.e2. doi: 10.1016/j.jpeds.2020.08.041
42. Anguzu R, Cusatis R, Fergestrom N, Cooper A, Schoyer KD, Davis JB, et al. Decisional conflict among couples seeking specialty treatment for infertility in the USA: a longitudinal exploratory study. Hum Reprod. (2020) 35(3):573–82. doi: 10.1093/humrep/dez292
43. Borowczak M, Rotoli S. A qualitative exploration of social support in males and females experiencing issues with infertility. Cureus. (2022) 14(9):e29763. doi: 10.7759/cureus.29763
44. Buechel J, Spalding CN, Brock WW, Dye JL, Todd N, Wilson C, et al. A grounded theory approach to navigating infertility care during U.S. military service. Mil Med. (2022) 189:usac174. doi: 10.1093/milmed/usac174
45. Ceballo R, Graham ET, Hart J. Silent and infertile: an intersectional analysis of the experiences of socioeconomically diverse African American women with infertility. Psychol Women Q. (2015) 39(4):497–511. doi: 10.1177/0361684315581169
46. Cebert-Gaitors M, Shannon-Baker PA, Silva SG, Hart RE, Jahandideh S, Gonzalez-Guarda R, et al. Psychobiological, clinical, and sociocultural factors that influence black women seeking treatment for infertility: a mixed-methods study. F S Rep. (2022) 3(2 Suppl):29–39. doi: 10.1016/j.xfre.2022.02.004
47. Cusatis R, Johnson C, Schoyer KD, Tsaih SW, Balza J, Sandlow J, et al. Decision regret among couples experiencing infertility: a mixed methods longitudinal cohort study. Reprod Health. (2023) 20(1):165. doi: 10.1186/s12978-023-01699-5
48. Ferland P, Caron SL. Exploring the long-term impact of female infertility: a qualitative analysis of interviews with postmenopausal women who remained childless. Fam J. (2013) 21(2):180–8. doi: 10.1177/1066480712466813
49. Gentile K. The business of being made: exploring the production of temporalities in assisted reproductive technologies. Stud Gend Sex. (2013) 14(4):255–76. doi: 10.1080/15240657.2013.848318
50. Lee M. I wish I had known sooner: stratified reproduction as a consequence of disparities in infertility awareness, diagnosis, and management. Women Health. (2019) 59(10):1185–98. doi: 10.1080/03630242.2019.1593283
51. Leyser-Whalen O, Greil AL, McQuillan J, Johnson KM, Shrefffler KM. ‘Just because a doctor says something, doesn't Mean that [it] will happen’: self-perception as having a fertility problem among infertility patients. Sociol Health Illn. (2018) 40(3):445–62. doi: 10.1111/1467-9566.12657
52. Leyser-Whalen O, Bombach B, Mahmoud S, Greil AL. From generalist to specialist: a qualitative study of the perceptions of infertility patients. Reprod Biomed Soc Online. (2021) 14:204–15. doi: 10.1016/j.rbms.2021.10.003
53. LoGiudice JA. A narrative analysis of the in vitro fertilization experiences of survivors of sexual abuse. Nurs Womens Health. (2022) 26(2):107–15. doi: 10.1016/j.nwh.2022.01.007
54. Mac Dougall K, Beyene Y, Nachtigall RD. Age shock: misperceptions of the impact of age on fertility before and after IVF in women who conceived after age 40. Hum Reprod. (2013) 28(2):350–6. doi: 10.1093/humrep/des409
55. Mayette E, Scalise A, Li A, McGeorge N, James K, Mahalingaiah S. Assisted reproductive technology (ART) patient information-seeking behavior: a qualitative study. BMC Womens Health. (2024) 24(1):346. doi: 10.1186/s12905-024-03183-z
56. Osadchiy V, Mills JN, Eleswarapu SV. Understanding patient anxieties in the social media era: qualitative analysis and natural language processing of an online male infertility community. J Med Internet Res. (2020) 22(3):e16728. doi: 10.2196/16728
57. Öztürk R, Herbell K, Morton J, Bloom T. The worst time of my life": treatment-related stress and unmet needs of women living with infertility. J Community Psychol. (2021) 49(5):1121–33. doi: 10.1002/jcop.22527
58. Palmer-Wackerly AL, Voorhees HL, D'Souza S, Weeks E. Infertility patient-provider communication and (dis)continuity of care: an exploration of illness identity transitions. Patient Educ Couns. (2019) 102(4):804–9. doi: 10.1016/j.pec.2018.12.003
59. Perone HR, Stump H, Herweck A, Levine H, Wong AJ, Carugno J. Trends in social media topics during COVID-19 among women undergoing assisted reproductive technology treatments. Cureus. (2020) 12(10):e11049. doi: 10.7759/cureus.11049
60. Perone HR, Herweck AM, Stump HM, Levine HM, Wong AJ, Carugno J. The virtual infertility community: a qualitative analysis of patient experiences shared on Instagram. J Assist Reprod Genet. (2021) 38(3):613–20. doi: 10.1007/s10815-020-02028-6
61. Peterson ZD, Buday SK. Sexual coercion in couples with infertility: prevalence, gender differences, and associations with psychological outcomes. Sex Relation Ther. (2020) 35(1):30–45. doi: 10.1080/14681994.2018.1435863
62. Sira N, McNeil S, Hegde A, Geistman K, Schwartz A. Infertility and identity: a closer look into experiences of emerging young adult childhood cancer survivors. J Pediatr Hematol Oncol Nurs. (2024) 41(1):32–43. doi: 10.1177/27527530231190386
63. Wagi CR, Ali NA, Santiago-Datil WL, Rickloff MA, Corvin JA. Suffering in silence: graduate student infertility. J Am Coll Health. (2022) 70(8):2295–302. doi: 10.1080/07448481.2020.1851233
64. Jennings L, Gagliardi L. Influence of mhealth interventions on gender relations in developing countries: a systematic literature review. Int J Equity Health. (2013) 12(1):85. doi: 10.1186/1475-9276-12-85
65. Bedrick BS, Anderson K, Broughton DE, Hamilton B, Jungheim ES. Factors associated with early in vitro fertilization treatment discontinuation. Fertil Steril. (2019) 112(1):105–11. doi: 10.1016/j.fertnstert.2019.03.007
66. Read SC, Carrier ME, Boucher ME, Whitley R, Bond S, Zelkowitz P. Psychosocial services for couples in infertility treatment: what do couples really want? Patient Educ Couns. (2014) 94(3):390–5. doi: 10.1016/j.pec.2013.10.025
68. Nguyen A. Glendale Couple Sues Fertility Clinic After Woman Gives Birth to Their son in Embryo Snafu. Los Angeles, CA: Glendale News Press (2019). Available online at: https://www.latimes.com/socal/glendale-news-press/news/tn-gnp-me-fertility-clinic-lawsuit-implantation-20190711-story.html
Keywords: in vitro fertilization, IVF, qualitative, narrative review, United States, health care
Citation: Peterson SK, Jennings Mayo-Wilson L, Spigel L, Morgan I and Parker A (2025) Health care experiences of individuals accessing or undergoing in vitro fertilization (IVF) in the U.S.: a narrative review of qualitative studies. Front. Reprod. Health 7:1490917. doi: 10.3389/frph.2025.1490917
Received: 23 September 2024; Accepted: 15 January 2025;
Published: 13 February 2025.
Edited by:
Vijay Sirohi, University of Florida, United StatesReviewed by:
David Yiu Leung Chan, The Chinese University of Hong Kong, ChinaArun Verma, Saint Louis University, United States
Copyright: © 2025 Peterson, Jennings Mayo-Wilson, Spigel, Morgan and Parker. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Summer K. Peterson, c3VtbWVyLnBldGVyc29uQHVuYy5lZHU=
 Summer K. Peterson
Summer K. Peterson Larissa Jennings Mayo-Wilson1,2
Larissa Jennings Mayo-Wilson1,2