- National Institute for Pharmaceutical Research and Development, Federal Capital Territory, Abuja, Nigeria
Introduction: Lack of access to effective contraception methods can lead to an increased prevalence of unintended pregnancies, as well as possible deleterious health consequences. Community pharmacies represent the most accessible gateway for population medicines' and healthcare needs. Regarding contraceptives, they have also been identified as a platform for the provision of additional services, such as complementary counselling. This study aimed at assessing the knowledge, attitudes, and practices of community pharmacy staff towards contraception.
Methods: A cross-sectional study was undertaken in the Federal Capital Territory, Nigeria. Data were collected from 315 community pharmacy staff using self-administered questionnaires. The participants' knowledge and attitude scores were categorised using Bloom's cut-off point. Analyses were undertaken using Statistical Package for Social Sciences. The data were analysed using frequency distribution, chi-square, and linear regression at a 5% level of significance.
Results: Male participants in the study (165/315, 52.4%) were slightly higher than the female respondents (150/315, 47.6%), and about two-thirds of the study cohort were pharmacists (200/315, 63.5%). The majority of the participants (183/315, 58.1%) had poor knowledge of contraceptive use. A quarter of them (81/315, 25.7%) reported moderate attitudes. Almost all the participants (279/298, 93.6%) indicated recommending contraceptives for married adults, and a significant proportion of them (136/292, 45.5%) were opposed to recommending contraceptives for unmarried adolescents. Study respondents' professional role was also identified as a significant influence on their knowledge of contraceptives and contraception (p < 0.001).
Conclusion: Findings from this study revealed poor knowledge and negative attitudes of community pharmacy staff towards contraception. Government and relevant stakeholders can build on these novel findings to reform pertinent contextual policies and practices. This can significantly improve access to contraceptives amongst the populace, and consequently reduce unintended pregnancies alongside possible health and societal implications.
Introduction
Globally, an estimated 250 million pregnancies occur each year, with up to one-third of these pregnancies being unintended (1, 2). Unintended refers to unwanted or mistimed pregnancies which can occur due to failure to choose an effective contraception method, or incorrect use of contraceptives (3, 4). Such pregnancies can place an economic burden on societies, as well as lead to reproductive health risks for women (5). Close to a quarter of unwanted pregnancies are terminated using unsafe methods, and up to 18% end up in unplanned births (6). Whilst unsafe termination of pregnancies is common in low-income countries, available evidence suggests that the abortion rates in developing and developed countries are of a similar proportion (7). In Nigeria, between 2015 and 2019, 10.5 million pregnancies occur annually, with 2.99 million being unintended, and 1.43 million ending in abortion (7). These high abortion rates alongside associated safety concerns in low-income countries highlight the need for improved access to contraception, especially from frontline healthcare practitioners in community pharmacy practice.
Contraception, also known as birth control, anticonception, and fertility control, refers to various relevant methods used for the prevention of pregnancies. Contraception has been in use for a long time; however, effective and safe methods of birth control only became available in the 20th century (8). Methods such as sterilisation, the use of intrauterine devices, and implantable birth control have been identified as the most effective means of fertility control, and this list is followed by other methods such as oral pills, patches, vaginal rings, and injections (9). Other techniques that are categorised as less effective include barrier methods, such as the use of condoms, diaphragm, and birth control sponges. The least effective birth control methods are the use of spermicides and withdrawal methods. Pregnancies in teenagers are associated with a greater risk of poor outcomes (10). Promoting comprehensive sex education and access to contraceptives for this age group decreases the rate of unwanted pregnancies (11). Birth control can improve women's delivery outcomes and the survival of their children by increasing the length of time between pregnancies (12).
In Nigeria, contraceptive use is shaped by a complex interplay of cultural and systemic factors (13). Deeply rooted religious beliefs and societal stigma often create significant barriers, discouraging open discussions about contraception and complicating access for individuals seeking options (14). These challenges are further exacerbated by gender dynamics, where family planning decisions are frequently dominated by men, limiting women's autonomy in making informed choices (15).
The public can experience barriers in accessing contraceptives, especially when some health providers feel that certain individuals that are unmarried should not receive such services due to their personal belief. These barriers can manifest in various forms, including biased attitudes, lack of comprehensive training on reproductive health, and inadequate communication about contraceptive options (16). Providers may perpetuate stigma by questioning the moral or social appropriateness of contraceptive use among certain populations, leading to discriminatory practices that deny essential services (17). Additionally, the insufficient integration of family planning education into healthcare training programs means that many practitioners lack the knowledge necessary to provide unbiased, evidence-based information about contraceptives (18). As a result, these barriers not only limit access to contraceptives but also undermine broader public health efforts aimed at reducing unintended pregnancies and promoting reproductive rights in Nigeria.
The community pharmacy setting represents an essential point for accessing contraceptives. This setting also serves as a venue for offering counselling services to the public as well as a first point of call for issues relating to birth control pills (19–21). Community pharmacies play a pivotal role in access to contraceptives, and this can be influenced by the knowledge and attitudes of the healthcare personnel practicing in this setting. Appropriate knowledge, positive attitudes, and good practices are critical elements that can enable a community pharmacy staff to provide comprehensive counselling, as well as create necessary awareness regarding contraceptives, thus preventing unintended pregnancies (22, 23). Several studies have been undertaken in relation to knowledge, attitudes, and practices towards contraceptive use in Nigeria (24, 25), there is however paucity of information about the community pharmacy staff in this area. It is against this backdrop that this study aimed at assessing the knowledge, attitudes, and practices of community pharmacy staff towards contraception.
Methods
Study design
The study was undertaken between May and August 2022 in Nigeria's Federal Capital Territory using a cross-sectional study design. The data collection tool (Supplementary File) was developed following an extensive literature review (5, 26–29). The items in the instrument were knowledge, attitudes, and practices towards contraceptives, as well as a section on socio-demographic characteristics. The study tool was structured to assess community pharmacy staff in these thematic areas. The items assessing knowledge were answered on a “true/false” basis and an additional “I do not know” option. The questions assessing attitudes were structured as “agree”, “disagree”, and “not sure”, whilst practice questions were answered on a “yes” or “no” basis.
Validation of research instrument
Questionnaire validation was undertaken by an expert panel comprising faculty members engaged in research activities in the field of contraception. These experts were chosen from various institutions, and were made of individuals who are familiar with survey design, validation processes, research methodologies as well as psychometrics and construct validity. Face and content validations were undertaken. The study tool was assessed for appropriateness, complexity, attractiveness, and relevance of the items. Content validity ratio and content validity index tests were undertaken for each item, and only those that passed these tests were included in the questionnaire. Cronbach alpha's test was also conducted to assess the reliability of the questionnaire, and this gave a value of 0.83, indicating internal consistency in the questionnaire items. The questionnaire was pilot-tested by administering it to an initial cohort of 20 participants who were randomly selected. The feedback received did not necessitate any further change, and this led to the final version of the questionnaire.
Sampling
According to a study by Ekpenyong et al. (30), there are 455 registered community pharmacies in the Federal Capital Territory. A minimum sample size of 314 was calculated for an estimated number of 1,700 pharmacists and pharmacy support staff in the Federal Capital Territory. This was computed at 95% confidence level, 5% margin of error, and 50% response distribution using Epi Info software version 7 (31). This is in tandem with Cochran's formula for calculating the sample size of a finite population (32). The sample size was rounded up to 400 to account for non-response. Participants were recruited following a convenience sampling strategy deployed across community pharmacies in the Federal Capital Territory to get enough respondents. Inclusion criteria adopted for the study include pharmacists licensed to practice; trained pharmacy technicians; and support staff involved in roles pertaining to dispensing. Pharmacy staff who did not have any role to play in relation to dispensing medications to patients were excluded from the study. Paper-based questionnaires were administered to the study participants.
Ethics consideration
Prior to the data collection phase, ethical approval was obtained from the Federal Capital Territory Health Research Ethics Committee (Approval number: FHREC/2021/01/97/12-08-21), and participation in the study was voluntary. Written informed consent was obtained from the participants before administering the questionnaires. Confidentiality and anonymity were strictly maintained throughout the data collection process. All information that could link participants to their responses was not included in the data collection tool.
Data analysis
Following the retrieval of questionnaires, data were entered into Statistical Package for Social Sciences version 25. Descriptive statistical analyses were undertaken. For the knowledge section, each correct response was assigned a score of 1, and incorrect responses and unanswered questions were assigned 0. The participants' overall knowledge score was categorised using Bloom's cut-off point as good for 80%–100%, moderate for 60%–79%, and poor for ≤59% (33). Bloom's cut-off point was chosen because it provides a widely accepted framework for interpreting survey scores, ensuring consistency and comparability across studies on knowledge assessment. For the attitude section, questions were assigned 1 point for a positive attitude towards contraception, and 0 was assigned for unanswered or negative feedback. The total attitude score for each participant was categorised by also using Bloom's cut-off as positive for 80%–100%, moderate for 60%–79%, and negative for ≤59%. Findings from the practice section were presented as percentages and frequencies as this approach is more appropriate for capturing behavioral trends.
Student's t-test and analysis of variance (ANOVA) were undertaken to determine relationships between mean knowledge scores and socio-demographic characteristics. post hoc analysis (LSD) was performed in cases of significant ANOVA tests for multiple comparisons. A p-value of 0.05 or less represented the threshold for statistical significance. Linear regression was used with 95% confidence interval to show the strengths of association. Finally, a p-value of less than 0.05 in the multivariate regression analysis was used to identify variables significantly associated with the knowledge of contraception amongst community pharmacy staff.
Results
Demography
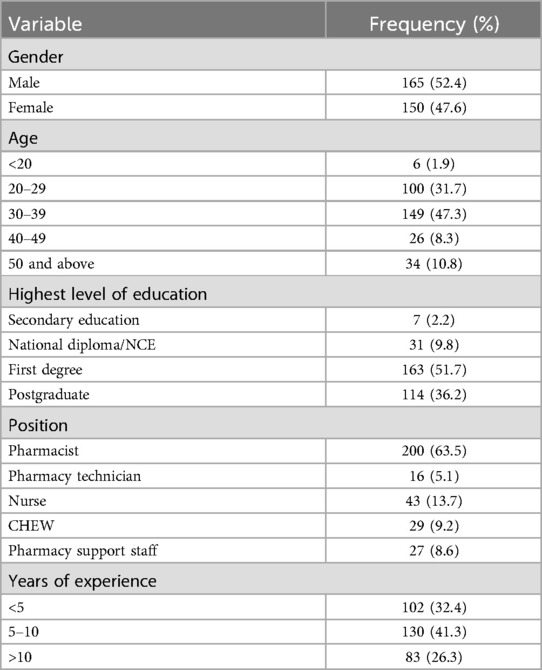
A total of 315 community pharmacy staff comprising (165/315, 52.4%) male participants and (150/315, 47.6%) female respondents participated in the study. Close to half of the sample (149/315, 47.3%) were between the ages of 30–39 years. Slightly above a third of the participants (114/315, 36.2%) were educated up to postgraduate level. Further details on the socio-demographic characteristics of the respondents are provided in Table 1.
Knowledge
The total mean knowledge score for the participants was 11.55 ± 3.33 (range; 1–21). The majority of the participants (183/315, 58.1%) had poor knowledge regarding contraception, a third of the participants (110/315, 34.9%) reported moderate knowledge, whilst only a few of the respondents (22/315, 7.0%) had good knowledge.
In terms of medical eligibility criteria for contraceptive use, a strong majority of the participants (273/315, 86.7%) indicated correctly that the eligibility criteria provide guidance regarding which clients can use contraception methods safely. About three-quarters (231/315, 73.3%) of the participants knew that cigarette smoking could increase the risk of serious cardiovascular problems from combined oral contraceptive use. Only a third of the participants were fully knowledgeable about hormonal contraceptives' lack of association (108/315, 34.3%) with permanent infertility. Further details on knowledge of contraceptives are provided in Table 2.
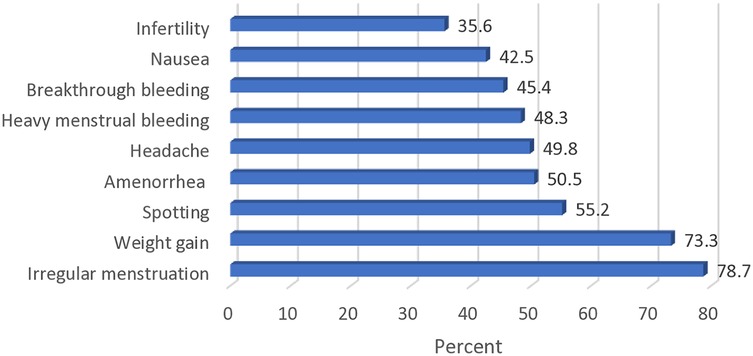
As presented in Figure 1, the most frequently indicated side effect of contraceptives reported by the study participants was irregular menstruation (248/315, 78.7%), and this was closely followed by weight gain (231/315, 73.3%).
Also, from Figure 1, it can be seen that infertility was the least reported side effect (112/315, 35.6%) of hormonal contraceptives as indicated by the respondents, whilst half of the study participants (159/315, 50.5%) knew that the use of contraceptives could cause amenorrhea.
Attitudes
The total mean score for the attitudes of the participants towards contraceptive use was 7.36 ± 2.40 (range; 1–10). Half of the participants (171/315, 56.6%) had a negative attitude towards contraception, a quarter of them (81/315, 25.7%) reported moderate attitudes, whilst only (63/315, 20.0%) of the respondents had positive attitudes in this regard.
More than half of the participants (169/297, 56.9%) were of the opinion that parental consent was not required by adolescents for contraceptive use, whilst a similar proportion (157/287, 54.7%) opined that providing contraceptives for this age group could promote promiscuity. The influence of religious and cultural beliefs is notable, as 56.7% cited religious opposition, and 39.6% align with cultural norms discouraging adolescent contraceptive use. Other relevant details are provided in Table 3.
Practice
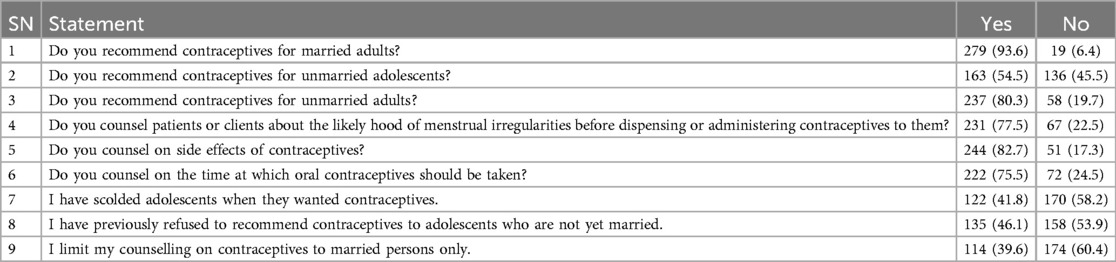
Almost all the participants (279/298, 93.6%) indicated recommending contraceptives to married adults, whilst only half of them (163/299, 54.5%) supported contraceptives' use for adolescents. A significant proportion of the participants (136/292, 46.1%) reported to have scolded adolescents who requested contraceptives. Further details on practice are provided in Table 4.
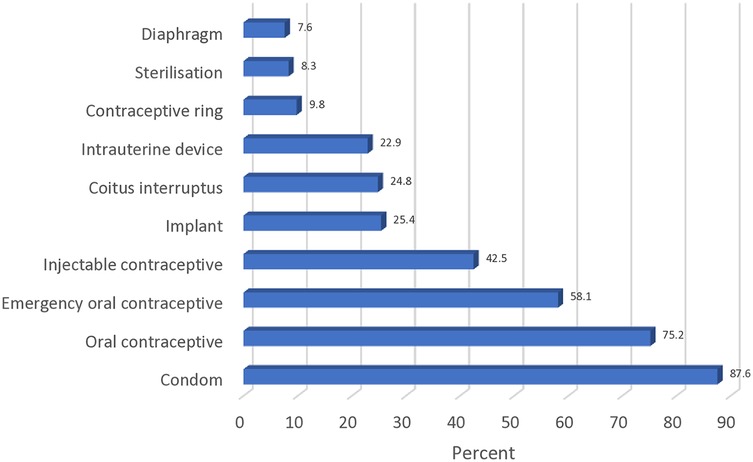
In terms of contraception methods promoted by the participants, condoms (276/315, 87.6%) emerged as the most commonly presented. This was closely followed by oral contraceptives (237/315, 75.2%). Further relevant details are provided in Figure 2.
Figure 2 shows the most common method of contraception promoted by the sampled community pharmacy staff. The least common methods of contraception were the diaphragm (24/315, 7.6%), sterilisation (26/315, 8.3%), and contraceptive ring (31/315, 9.8%). A quarter of the participants (78/315, 24.8%) indicated promoting coitus interruptus.
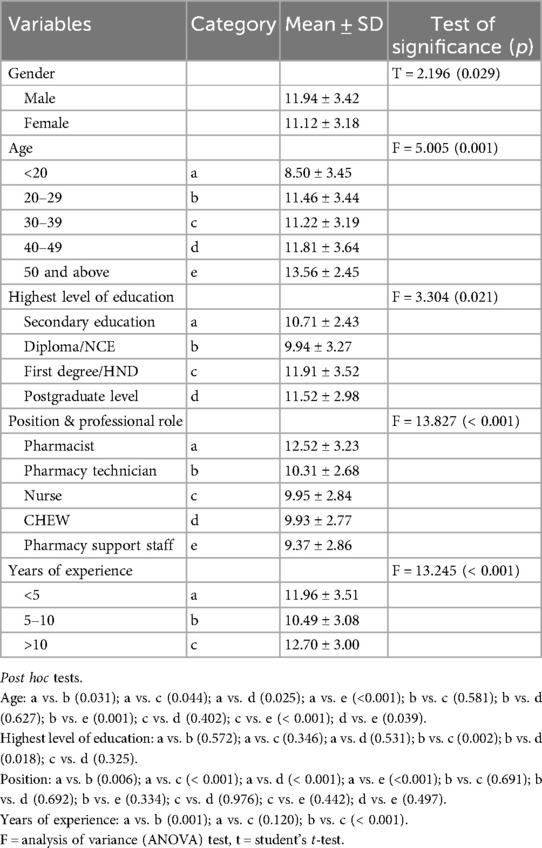
Inferential statistical analysis of demography and knowledge
From the inferential statistical analysis undertaken, it was observed that the knowledge of the participants on contraceptive use was influenced by their socio-demographic characteristics. Male participants were more knowledgeable than the female respondents (p = 0.029), older participants had better knowledge (p = 0.001), and pharmacists reported a higher mean score compared to other groups of pharmacy staff (p < 0.001). Further details are provided in Table 5.
Additionally, multivariate linear regression was undertaken to determine multiple association. The R2 value was 0.21, indicating that 21% of the variance in the knowledge score was predicted by socio-demographic characteristics. The regression equation was significant (F = 12.11, p < 0.001) indicating that at least one of the six independent variables could significantly affect participants' knowledge. Participants' knowledge was influenced by age. Compared to those who were less than 20 years, respondents who were 20–29 years (β = 2.62; 95% CI = 0.07–5.17; p = 0.044), 30–39 (β = 2.85; 95% CI = 0.31–5.38; p = 0.028) as well as 50 and above (β = 3.18; 95% CI = 0.33–6.03; p = 0.029), were more knowledgeable and this was significant. Similarly, the position and professional role of the community pharmacy staff was another factor that affected knowledge. Pharmacists were significantly more knowledgeable (β = 2.85; 95% CI = 1.48–4.22; p = <0.001) than pharmacy support staff. Also, whilst pharmacy technicians, nurses and CHEW had more knowledge than the pharmacy support staff, this was not significant. Further details are presented in Table 6.
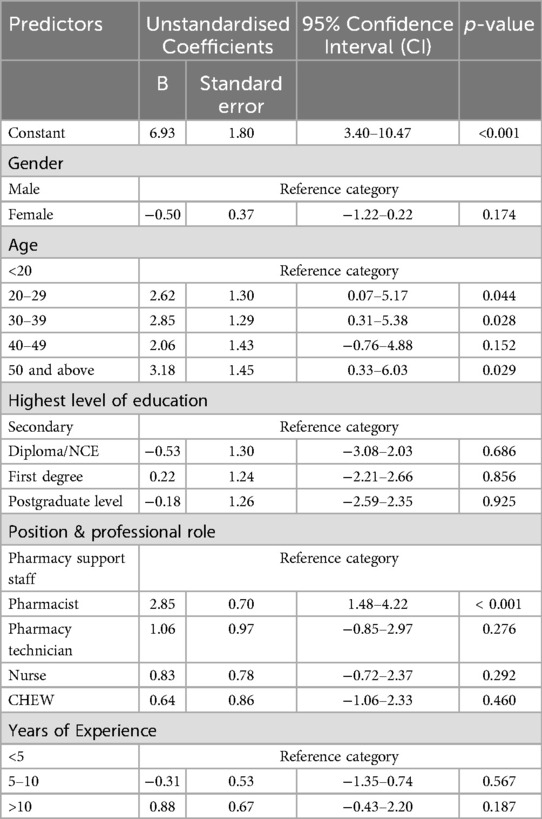
Table 6. Multivariable linear regression to determine the socio-demographic variables influencing knowledge.
Discussion
This study provides novel insights regarding the knowledge, attitudes, and practices of community pharmacy staff towards contraception. Findings that emerged from this study suggest that the overall knowledge of the participants was suboptimal. However, the participants demonstrated adequate knowledge in certain aspects. For instance, a strong majority of the study cohort answered correctly that medical eligibility criteria for contraception provide guidance for practitioners regarding persons who should be considered fit to use contraceptive methods safely. The overall mean score for knowledge was just a little above average, suggesting a lack of comprehensive knowledge towards contraception. These findings are similar to other studies where an unsatisfactory level of knowledge was reported amongst pharmacists (5, 34).
Whilst findings from this study are consistent with international reports on the gaps in knowledge of contraceptives among pharmacy staff, the specific barriers identified in this study require context-specific solutions. Compared to studies in high-income countries, the respondents of this study exhibited concerns about providing contraception to unmarried adolescents, which may have been influenced by moral and cultural considerations (35–38). This underscores the need for targeted training and education to bridge these gaps. In contrast, studies from countries with more comprehensive adolescent contraceptives' policies, are associated with robust integration of such services within their primary healthcare system (39).
In this study, participants included various categories of staff working in the community pharmacy setting, such as pharmacists and technicians. Findings from this study indicate a critical need for regular training and capacity building of community pharmacy staff to ensure that they are adequately informed as regards contraception and various relevant areas related to sexual health. This novel finding is particularly important, considering that community pharmacies are usually the first port of call for minor ailments and healthcare services (40, 41). Values clarification and further training on adolescent sexual and reproductive health, ethical considerations in healthcare, and non-judgmental counselling are essential components to be incorporated in the training curriculum of healthcare practitioners. These recommendations are in line with the goals of Nigeria's National Family Planning Blueprint (2020–2024), which emphasises the importance of training healthcare providers to improve contraceptive knowledge and accessibility (42).
Participants in this study were familiar with the common side effects associated with the use of contraceptives, as more than three-quarters of them indicated irregular menstruation as one of these effects. Respondents' age and years of practice significantly influenced the level of knowledge exhibited by the participants, as older professionals and those with longer years of practice reported higher knowledge scores. This implies that relevant knowledge acquired increased, based on the duration of practice. Pharmacists also reported a higher knowledge score compared to other categories of community pharmacy staff, and this was expected considering their more robust training as regards provision of healthcare services (35).
Insights from this study reveal that community pharmacy staff play a significant role in either facilitating or obstructing adolescents' access to necessary healthcare, particularly in the area of contraception. Collectively, close to half of the participants reported moderate and positive attitudes towards contraceptive use, whilst the remaining half of the study cohort had negative attitudes. The participants were against providing contraceptives to unmarried adolescents as the majority of them felt this could promote sexual promiscuity. These findings are similar to those of studies amongst other categories of healthcare professionals in Nigeria, and those undertaken in other settings (36–38, 43). Available evidence suggests that adolescents avoid accessing public health facilities due to these negative attitudes, alongside their fear of stigmatisation (44, 45). Young individuals seeking to prevent unwanted pregnancies often face criticism from pharmacy staff when they are merely trying to access essential healthcare services. A considerable proportion of the participants felt that parental consent should be sought before providing contraceptives to people of young age whilst, in essence, there is no provision for this in Nigerian legislation. Currently, Nigeria's reproductive health policies are ambiguous regarding access to contraceptive by adolescents, particularly in community pharmacies, consequently creating a gap that needs be addressed through contextual reforms. For government and policymakers, this provides an opportunity to articulate a robust and comprehensive framework to guide healthcare workers in the discharge of their responsibilities as it relates to population access to contraceptives. Establishing such frameworks, can enable government address the confusion around adolescent contraceptives' access and ensure that healthcare providers, particularly in community pharmacies, have the necessary guidelines to serve young populations responsibly.
A strong majority of the participants demonstrated good practice in their outlook for the recommendation of contraceptives to both married and unmarried adults. However, a little less than half of the participants opposed providing adolescents with contraceptives. Whilst this may be attributable to issues relating to morality, the phenomenon is worthy of further study. Abstinence from sex represents the best strategy to prevent unwanted pregnancies amongst young people, however, professionals need to be better trained as regards contraceptive access for populations unable to abstain. This is important especially as policy guidelines regarding the provision of contraceptives to unmarried adolescents seem to remain unclear amongst healthcare professionals (36). This gap in policy guidance necessitates immediate attention from Nigerian authorities to clarify the role of healthcare providers in providing contraception to adolescents, ensuring that all healthcare workers are aligned with national goals.
The commonly recommended contraceptive method indicated by the study participants was the use of condoms, closely followed by the use of oral contraceptive pills. The least recommended were diaphragms, contraceptive rings, and sterilisation. The recommendation pattern may be attributable to the community pharmacy study setting which inadvertently influenced the choice of contraceptive methods easily dispensed within their premises. Further studies that build on these emergent findings also need to be undertaken in other settings, as well as amongst other healthcare professional groups.
Results from the multivariable linear regression analysis suggest that both age and professional role of the study participants significantly influenced their knowledge of contraception. This finding aligns with several studies (46–48), which also highlight age as a key factor influencing contraceptive knowledge. Additionally, the bivariate linear regression analysis indicates that as knowledge about contraception increases, attitudes toward contraception become more positive. This finding is consistent with a study by Dehlendorf and colleagues (49) which also emphasized the positive relationship between knowledge and attitudes towards contraception
A convenience sampling strategy was adopted to recruit participants, meaning that the sample may not have been representative of the population of community pharmacy staff in the Federal Capital Territory. However, this limitation was mitigated by various strengths of the study, which include validation and a robust pre-testing of the research instrument. Another limitation of this study is the potential for self-reporting bias, where participants may provide socially desirable answers or intentionally misrepresent their views to create a favourable impression. This weakness was minimized by employing the use of a validated questionnaire.
Conclusion
This study reported poor knowledge and negativity in attitudes towards contraception. Although the overall knowledge of the participants was suboptimal, the participants demonstrated adequate knowledge in certain aspects, such as medical eligibility criteria for contraceptive use as well as the effect of cigarette smoking on some methods of contraception. Negative attitudes amongst healthcare providers can prevent people from accessing relevant services in the area of reproductive health. The participants appear to be familiar with the common side effects of contraceptives. Age and years of practice significantly influenced the level of knowledge exhibited by participants. Also, pharmacists reported a higher knowledge score compared to other categories of community pharmacy staff. Furthermore, the majority of the participants demonstrated good practice in their outlook for the recommendation of contraceptives to both married and unmarried adults. This study revealed that a little less than half of the participants opposed providing adolescents with contraceptives. The novel findings that emerged from this study can guide government and policymakers in developing relevant strategies that prevent unintended pregnancies amongst the populace.
Clear contextual policy guidelines can enable access to contraceptives for members of the public and prevent discriminative practice among healthcare professionals. Also, this is critically important to provide training for, and build the capacity of healthcare workers as regards service provision for the public in this area. As well as reducing unintended pregnancies, this intervention will also mitigate consequent health complications and associated socio-economic burden.
As this is the first study amongst community pharmacy staff in this setting, the novel findings that emerged provide an empirical basis for contextual policy and practice reforms which can be led by government and other relevant stakeholders. The development of relevant reproductive health guidelines that are fit for purpose in this context can enable improved access to contraceptives in community pharmacies and similar healthcare settings. Further studies can be undertaken to deepen the emergent findings from this study.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
This study was approved by the National Institute for Pharmaceutical Research and Development Health Research Ethics Committee. The research was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
OA: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Resources, Validation, Writing – review & editing. GO: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Validation, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frph.2025.1488707/full#supplementary-material
References
1. Goyal M, Zhao H, Mollen C. Exploring emergency contraception knowledge, prescription practices, and barriers to prescription for adolescents in the emergency department. Pediatrics. (2009) 123(3):765–70. doi: 10.1542/peds.2008-0193
2. Alam K, Snover A, Sultana N, Munir TA, Shah SS. Emergency contraception: knowledge, attitude and practices among doctors of a tertiary care hospital. J Ayub Med Coll Abbottabad. (2013) 25(1-2):141–4.25098079
3. Santelli J, Rochat R, Hatfield-Timajchy K, Gilbert BC, Curtis K, Cabral R, et al. The measurement and meaning of unintended pregnancy. Perspect Sex Reprod Health. (2003) 35(2):94–101. doi: 10.1363/3509403
4. Centers for Disease Control. Unintended Pregnancy. (2021). Available online at: https://www.cdc.gov/reproductivehealth/contraception/unintendedpregnancy/index.htm (accessed July 15, 2022).
5. Shakya S, Shrestha S, Shrestha RK, Giri U, Shrestha S. Knowledge, attitude and practice of emergency contraceptive pills among community pharmacy practitioners working in Kathmandu valley: a cross-sectional study. BMC Health Serv Res. (2020) 20:699. doi: 10.1186/s12913-020-05543-5
6. Singh S, Sedgh G, Hussain R. Unintended pregnancy: worldwide levels, trends, and outcomes. Stud Fam Plann. (2010) 41(4):241–50. doi: 10.1111/j.1728-4465.2010.00250.x
7. Bearak JM, Popinchalk A, Beavin C, Ganatra B, Moller A-B, Tunçalp Ö, et al. Country-specific estimates of unintended pregnancy and abortion incidence: a global comparative analysis of levels in 2015–2019. BMJ Glob Health. (2022) 7:e007151. doi: 10.1136/bmjgh-2021-007151
8. Hanson SJ, Burke AE. Fertility control: contraception, sterilization, and abortion. In: Hurt KJ, Guile MW, Bienstock JL, Fox HE, Wallach EE, editors. The Johns Hopkins Manual of Gynecology and Obstetrics. 4th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins (2010). p. 382–95.
9. World Health Organisation. Family Planning: A Global Handbook for Providers: Evidence-based guidance Developed Through Worldwide Collaboration. Geneva: Centre for Communication Programs and World Health Organization (2011). Available online at: https://fphandbook.org/sites/default/files/hb_english_2012.pdf (accessed July 15, 2022).
10. Black AY, Fleming NA, Rome ES. Pregnancy in adolescents. Adolescent Medicine: State of the art Reviews. (2012) 23(1):123–38.22764559
11. Rowan SP, Someshwar J, Murray P. Contraception for primary care providers. Adolesc Med State Art Rev. (2012) 23(1):95–110.22764557
12. Cleland J, Conde-Agudelo A, Peterson H, Ross J, Tsui A. Contraception and health. Lancet. (2012) 380(9837):149–56. doi: 10.1016/S0140-6736(12)60609-6
13. Akinyemi OO, Harris B, Kawonga M. ‘Our culture prohibits some things’: qualitative inquiry into sociocultural challenges to scale-up of community-based injectable contraceptives in Nigeria. BMJ Open. (2020) 10(7):e035311. doi: 10.1136/bmjopen-2019-035311
14. Sinai I, Nyenwa T, Oguntunde O. Unmet need for family planning and barriers to contraceptive use in northern Nigeria. J Fam Plann Reprod Health Care. (2019) 45(3):167–74. doi: 10.1080/13691058.2019.1672894
15. Udechukwu F, Ezumah N, Ngwu A, Amujiri O, Okafor O. Family planning policy and gender in Nigeria: a thematic analysis of the literature. Ikenga Int J Inst Afr Stud. (2022) 23(2):1–12. doi: 10.53836/ijia/2022/23/2/010
16. Fapohunda BM, Orobaton N. Barriers to contraceptive use in Nigeria: a qualitative study. Afr J Reprod Health. (2013) 17(1):58–66.24069752
17. Schwandt HM, Speizer IS, Corroon M. Contraceptive service provider imposed restrictions to contraceptive access in urban Nigeria. BMC Health Serv Res. (2017) 17:268. doi: 10.1186/s12913-017-2233-0
18. Ogunbajo A, Oduola A. Barriers to contraceptive use among women in Nigeria: a systematic review. J Public Health Africa. (2020) 11(2):123–30.
19. Corroon M, Kebede E, Spektor G, Speizer I. Key role of drug shops and pharmacies for family planning in Urban Nigeria and Kenya. Glob Health Sci Pract. (2016) 4(4):594–609. doi: 10.9745/GHSP-D-16-00197
20. Hobbs MK, Taft AJ, Amir LH, Stewart K, Shelley JM, Smith AM, et al. Pharmacy access to the emergency contraceptive pill: a national survey of a random sample of Australian women. Contraception. (2011) 83(2):151–8. doi: 10.1016/j.contraception.2010.06.003
21. Rafie S, Stone RH, Wilkinson TA, Borgelt LM, El-Ibiary SY, Ragland D. Role of the community pharmacist in emergency contraception counseling and delivery in the United States: current trends and future prospects. Integr Pharm Res Pract. (2017) 6:99–108. doi: 10.2147/IPRP.S99541
22. Latthe M, Latthe P, Charlton R. Quality of information on emergency contraception on the internet. Br J Fam Plann. (2000) 26(1):39–43.10781966
23. Omotoso O, Ajuwon AJ. Emergency contraceptive pill knowledge, attitudes and dispensing practices of pharmacists in Ibadan and Lagos metropolis, Nigeria. Sierra Leone J Biomed Res. (2010) 2(2):135–41. doi: 10.4314/sljbr.v2i2.64017
24. Kasso T, Alegbeleye JO. Knowledge, attitude and practice of contraceptive use among women of reproductive age in Port Harcourt, Nigeria. Advances in Reproductive Sciences. (2023) 11(4):93–105. doi: 10.4236/arsci.2023.114009
25. Utoo BT, Mutihir TJ, Utoo PM. Knowledge, attitude and practice of family planning methods among women attending antenatal clinic in Jos, North-central Nigeria. Niger J Med. (2010) 19(2):214–8. https://doi: doi: 10.4314/njm.v19i2.56524
26. Idowu A, Fehintola FO, Popoola FG. Knowledge, attitude and practice of contraception by female junior secondary school students in an urban community of oyo-state, south west, Nigeria. Int J Reprod Contracept Obstet Gynecol. (2017) 6(11):4759–65. doi: 10.18203/2320-1770.ijrcog20174983
27. Anderson C, Blenkinsopp A. Community pharmacy supply of emergency hormonal contraception: a structured literature review of international evidence. Hum Reprod. (2006) 21(1):272–84. doi: 10.1093/humrep/dei287
28. Hussainy SY, Stewart K, Chapman CB, Taft AJ, Amir LH, Hobbs MK, et al. Provision of the emergency contraceptive pill without prescription: attitudes and practices of pharmacists in Australia. Contraception. (2011) 83(2):159–66. doi: 10.1016/j.contraception.2010.07.001
29. Thaci J, Foster AM. Emergency contraception in Albania: a multimethods qualitative study of awareness, knowledge, attitudes and practices. Contraception. (2018) 98(2):110–4. doi: 10.1016/j.contraception.2018.03.033
30. Barakat M, Al-Qudah RA, Akour A, Al-Qudah N, Dallal Bashi YH. Unforeseen uses of oral contraceptive pills: exploratory study in Jordanian community pharmacies. PLoS One. (2020) 15(12):e0244373. doi: 10.1371/journal.pone.0244373
31. Ekpenyong A, Udoh A, Kpokiri E, Bates I. An analysis of pharmacy workforce capacity in Nigeria. J Pharm Policy Pract. (2018) 11(1):1–9. doi: 10.1186/s40545-018-0147-9
32. Centers for Disease Control. EPI Info: Stat Calc. (2022). Available online at: https://www.cdc.gov/epiinfo/user-guide/statcalc/statcalcintro.html (accessed February 13, 2024).
33. Ahmad H, Halim H. Determining sample size for research activities. Selangor Business Review. (2017) 2(1):20–34.
34. Seid MA, Hussen MS. Knowledge and attitude towards antimicrobial resistance among final year undergraduate paramedical students at university of gondar, Ethiopia. BMC Infect Dis. (2018) 18(1):312. doi: 10.1186/s12879-018-3199-1
35. Azmi NL, Azman NF, Romainor NN, Abdul MH, Rahman MS. Knowledge, awareness and perception about contraception among pharmacy staffs: a single centre experience. Pharm Res Rep. (2020) 3(1):10–7.
36. Adigwe OP, Mohammed EN, Onavbavba G. International training of pharmacists and fitness to practice in Nigeria: emergent issues and novel insights. Curr Pharm Teach Learn. (2022) 14(5):618–25. doi: 10.1016/j.cptl.2022.04.006
37. Ahanonu EL. Attitudes of healthcare providers towards providing contraceptives for unmarried adolescents in Ibadan, Nigeria. J Family Reprod Health. (2014) 8(1):33–40.24971131
38. Warenius LU, Faxelid EA, Chishimba PN, Musandu JO, Ong’any AA, Nissen EB-M. Nurse-midwives’ attitudes towards adolescent sexual and reproductive health needs in Kenya and Zambia. Reprod Health Matters. (2006) 14:119–28. doi: 10.1016/S0968-8080(06)27242-2
39. Wood K, Jewkes R. Blood blockages and scolding nurses: barriers to adolescent contraceptive use in South Africa. Reprod Health Matters. (2006) 14:109–18. doi: 10.1016/S0968-8080(06)27231-8
40. Ketting E, Esin A. Integrating sexual and reproductive health in primary health care in Europe: position paper of the European forum for primary care. International Exchange. (2010) 18(4):269–82.
41. Hassell K, Rogers A, Noyce P. Community pharmacy as a primary health and self-care resource: a framework for understanding pharmacy utilization. Health Soc Care Community. (2008) 8(1):40–9. doi: 10.1046/j.1365-2524.2000.00222.x
42. Tonna AP, Weidmann AE, Sneddon J, Stewart D. Views and experiences of community pharmacy team members on antimicrobial stewardship activities in Scotland: a qualitative study. Int J Clin Pharm. (2020) 42:1261–9. doi: 10.1007/s11096-020-01042-z
43. Federal Ministry of Health. Nigeria’s National Family Planning Blueprint (2020–2024). Abuja: Federal Ministry of Health (2020). Available online at: https://policyvault.africa/policy/nigeria-family-planning-blueprint-2020-2024/ (Accessed: 22 December, 2024).
44. Mngadi PT, Faxelid E, Zwane IT, Höjer B, RansjoArvidson AB. Health providers’ perceptions of adolescent sexual and reproductive health care in Swaziland. Int Nurs Rev. (2008) 55:148–55. doi: 10.1111/j.1466-7657.2007.00625.x
45. Mmari KN, Magnani RJ. Does making clinic-based reproductive health services more youth-friendly increase service use by adolescents? Evidence from Lusaka, Zambia. J Adolesc Health. (2003) 33:259–70. doi: 10.1016/S1054-139X(03)00062-4
46. Lindberg C, Lewis-Spruill C, Crownover R. Barriers to sexual and reproductive health care: urban male adolescents speak out. Issues Compr Pediatr Nurs. (2006) 29:73–88. doi: 10.1080/01460860600677577
47. Abubakar IB, Abubakar HB. Nigerian Women’s modern contraceptive use: evidence from NDHS 2018. Reprod Fertil. (2024) 5(2):e230063. doi: 10.1530/RAF-23-0063%3E
48. Fadeyibi O, Alade M, Adebayo S, Erinfolami T, Mustapha F, Yaradua S. Household structure and contraceptive use in Nigeria. Front Glob Women’s Health. (2022) 3:821178. doi: 10.3389/fgwh.2022.821178
Keywords: pregnancy, abortion, contraceptives, birth control, family planning
Citation: Adigwe OP and Onavbavba G (2025) Knowledge, attitudes, and practices regarding contraception amongst community pharmacy staff: a cross-sectional study in Nigeria. Front. Reprod. Health 7:1488707. doi: 10.3389/frph.2025.1488707
Received: 30 August 2024; Accepted: 21 January 2025;
Published: 24 March 2025.
Edited by:
Dabney Evans, Emory University, United StatesReviewed by:
Collins Ouma, Maseno University, KenyaSarah Danielson Compton, University of Michigan, United States
Copyright: © 2025 Adigwe and Onavbavba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Obi Peter Adigwe, by5wLmFkaWd3ZUBuaXByZC5nb3Yubmc=; Godspower Onavbavba, b25hdmJhdmJhZ29kc3Bvd2VyQGdtYWlsLmNvbQ==
†ORCID:
Obi Peter Adigwe
orcid.org/0000-0001-8832-6459
Godspower Onavbavba
orcid.org/0000-0002-4803-8804
 Obi Peter Adigwe
Obi Peter Adigwe Godspower Onavbavba
Godspower Onavbavba