- 1Research and Community Service Directorate, Hawassa College of Health Sciences, Hawassa, Ethiopia
- 2Hawassa City Health Department, Alamura Health Center, Hawassa, Ethiopia
- 3School of Environmental Health, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
- 4Wonsho Woreda Health Office, Wonsho Woreda, Sidama Regional Health Bureau, Sidama, Ethiopia
- 5Department of Public Health, Hawassa College of Health Sciences, Hawassa, Ethiopia
Background: Despite poor menstrual hygiene practices exposing adolescent females to reproductive health problems, it has not been adequately studied in low-income countries. Due to a lack of proper information, the majority of teenage girls enter puberty without having prepared themselves. The aim of this study was to assess menstrual hygiene practice and associated factors among adolescent female students.
Methods: An institution-based cross-sectional study design was employed from March 10 to April 20, 2022. A random sample of 608 adolescent female students was included in the study. A multistage sampling was applied to employee study participants. Data were collected using a structured questionnaire administered through an interview technique. A logistic regression model was used to analyze the data using version 26 SPSS statistical software. Descriptive statistics were used to summarize the data. An adjusted odds ratio with a 95% confidence interval and a corresponding p-value <0.05 was used to measure the strength of association.
Result: The prevalence of poor menstrual hygiene practices among adolescent girls was 28.4%. Poor knowledge of adolescent girls [AOR = 2.64, 95% CI: 1.74, 4.02], mothers' educational level [AOR = 0.86, 95% CI: 0.79, 0.94], fathers' occupation of private employers and daily laborers [AOR = 3.1, 95% CI: 1.46, 6.69] and [AOR = 1.98, 95% CI: 1.03, 3.8], and having hand washing facilities [AOR = 0.51, 95% CI: 0.34, 0.77] were significantly associated with poor menstrual hygiene management practices among adolescent schoolgirls.
Conclusion: In this study, we determined the level of poor menstrual hygiene practice. We identified factors significantly associated with menstrual hygiene practices. Interventions should focus on creating awareness among adolescent girls, providing menstrual hygiene management facilities, and improving the educational and occupational levels of parents.
Introduction
A female reproductive system undergoes regular cyclic alterations that might be interpreted philosophically as periodic preparation for pregnancy and fertilization (1). The cycle is a menstrual cycle, and its most noticeable feature is the periodic vaginal bleeding that occurs with the shedding of the uterine mucosa. Menstruation begins throughout the adolescent era, which is characterized by significant physiological and emotional changes (1, 2). A significant number of schoolgirls in low-income countries face challenges with menstrual hygiene management practice facilities, which are worsened by ignorance of their menstrual needs by teachers and intimidation by boys and older girls, creating a stressful environment for schoolgirls (3–5). The prevalence of poor management of menstrual hygiene is significantly different among adolescent schoolgirls in different settings (6–9). Accordingly, worldwide, 335 million females attended schools where there was no access to water or soap (10). In the Middle East and Asia, up to 95% of girls claim that their menstruation is the reason they are missing school (11, 12). Around 13% to 75% of girls do not have access to clean sanitary materials and use low-quality products in low- and middle-income countries (6, 13, 14). In Sub-Saharan Africa, findings from a pooled analysis show that the practice of menstrual hygiene management among schoolgirls was 45% (15). Results from a pooled analysis in Ethiopia show that the menstrual hygiene practice was 52.69% (16). Other recent studies show that its practice ranges from 21% to 75% in Ethiopia (7, 8, 10, 17–22).
Prior evidence shows that several factors are influencing the practice of menstrual hygiene management (19, 23–29). These include: family size, cultural beliefs and societal norms, being able to afford menstrual sanitary products, place of residence, prior awareness on sexuality and access to a sanitary napkin, lack of knowledge, socio-economic and environmental constraints, the presence of a private latrine, and living with relatives (9, 15, 30–33). Age of the females, maternal educational level, frequency of discussion with mothers about menstruation, information source about menstruation, having knowledge about menstruation, academic level of the students, wealth indexed of the family, earning permanent pocket money, absence of storage container in the school, occupation of the parents, having infection around their vagina during menarche, place of residence, living with parents, were also identified as risk factors in Ethiopia (7, 10, 18, 19, 21, 34).
Ethiopia is a multicultural country that has more than 80 nations that follow different cultures and religions (35). The levels of menstrual hygiene practice significantly varied from region to region and place to place, as did its associated factors. There was an inconsistence of findings among studies that were previously done in Ethiopia (19, 21). Furthermore, there was a limited study that assessed the level of menstrual hygiene practice in the Sidama region. To our knowledge, there was no study done in Dale woreda. Therefore, the aim of this study was to assess the prevalence of menstrual hygiene practice and its associated factors among adolescents in the Dale Woreda School.
Methods and materials
Study setting
The study was done in Dale woreda, which is one of the administrative woredas of the Sidama national regional states, 311 km from Addis Ababa, the capital of Ethiopia. Dale is bordered from the south by Aleta Wendo and Cucko woreda, from the west by Lokka Abaya woreda, from the north by Shebedino woreda, and from the east by Wonsho woreda. Yirgalem is its capital town, and Woreda has 39 kebele. The estimated population of Woreda in 2014 EFY was 254,658 people, of whom 51% were female. The total estimated number of women belonging to the reproductive age group is 53,478. Dale woreda has 48 schools in total, and the total number of students attending grades 1–8 was 38,228; among them, 18,996 were female students. The total number of adolescent girls who are attending primary school at Dale woreda is 9,873.
Study design and the source population
A school-based cross-sectional study was conducted in Dale district from March 20 to April 20, 2022. Adolescent girls attending the primary schools in the regular program and age group 10–17 were included in the study. Those girls whose menarche has not started, who have severe mental problems, refuse to participate, refuse to participate, and who were absent during data collection period were excluded from the study.
Sample size determination and sampling procedure
A single population proportion formula was used to calculate sample size with the following assumptions: at 95% CI = 1.96, P = 60.3% proportion of poor menstrual hygiene practice in southern Ethiopia (36), d = margin of error taken as 5%. The sample size was calculated using the formula: n = (Z α/2)2 p (1-p)/d2, n = (1.96)2*(0.603) (1–0.603) (0.05)2, n = 368. By adding 10% of the non-response rate, the sample size becomes 405. Considering the design effect of 1.5 (to improve the efficiency or precision of an estimator), the final sample size was 608. A multi-stage sampling technique was applied to recruit the participants. First, Dale woreda was selected purposefully. From all schools found in Dale Woreda 10 schools were selected randomly. Each selected school received a proportional allocation of the total sample size. Then, adolescent girls from selected schools who fulfilled the inclusion criteria were enrolled in the study using a simple random sampling technique. To apply simple random sampling, a sampling frame was created by taking a list of adolescent girl students from each school.
Main study outcome variable
Menstrual hygiene practice was the outcome variable in this study, which was assessed using a ten-item “yes” or “no” question. Each item's response was scored as “1” for correct answers and “0” for incorrect answers. The tool's total sum score ranges from 0 to 10. Girls with a total sum score less than the mean score are considered to have poor menstrual hygiene practices, while those who scored more than the mean score were considered to be good.
Data collection tools and procedures
An interviewer-administered structured questionnaire was developed that addresses the objectives of the study after thorough reviewing relevant literature. A questionnaire was developed in English and translated to the local language (Sidaamu Afoo) by a language expert, then back to English to check its consistency. A five percent of the total sample size was pretested at another school to evaluate the validity of the instruments. The data were collected on socio-demographic, gynecologic, and knowledge-related characteristics. One-day training was given for both the data collectors and supervisor to explain the aim and content of the instrument. Data was collected by five female nurse professionals under supervision of one MSc. midwife professional. The data were checked for completeness and consistency on the spot during the data collection period.
Data analysis
The completeness of the data swas checked, coded, and entered into Epi Data version 3.1. Then the data were exported and analyzed using Statistical Package for Social Sciences (SPSS) version 26. The data were summarized using the descriptive statistics. The binary logistic regression model was conducted to identify candidate variables for the final model, with a p-value of ≤0.25. The model's fitness was evaluated using the Hosmer-Lemeshow fitness of good test, which yielded a non-significant value, indicating the data fit reasonably well. An adjusted odds ratio (AOR) with a 95% confidence interval was employed to identify factors significantly associated with menstrual hygiene practices.
Results
Socio-demographic features of the participants
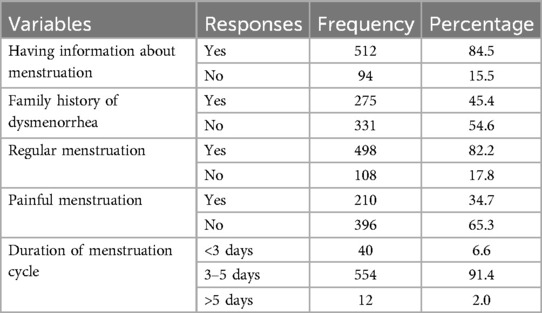
In our study, a total of 606 study subjects participated, with a response rate of 99.8%. Majority of the subjects (87.7%) were rural residents, with an average age of 14.9 years (SD ± 1.25 years). The majority of participants (94.4%) live with their parents. More than three-fourths of participants (79.9%) were protestant religion followers. Almost all (99.3%) subjects were from the Sidama ethnic group. More than two-thirds (68%) of participants attended grades 7 and above. More than four-fifths (87%) of participants mothers were housewives, and nearly three-fourths (71.1%) of participants fathers were farmers. Approximately three-fourths (74.5%) of participants receive money from their parents to buy sanitary pads. More than two third (71.0%) of participants had private latrine to change menstrual pads and nearly three fourth (72.3%) had got hand washing facility during changing pads (Table 1).
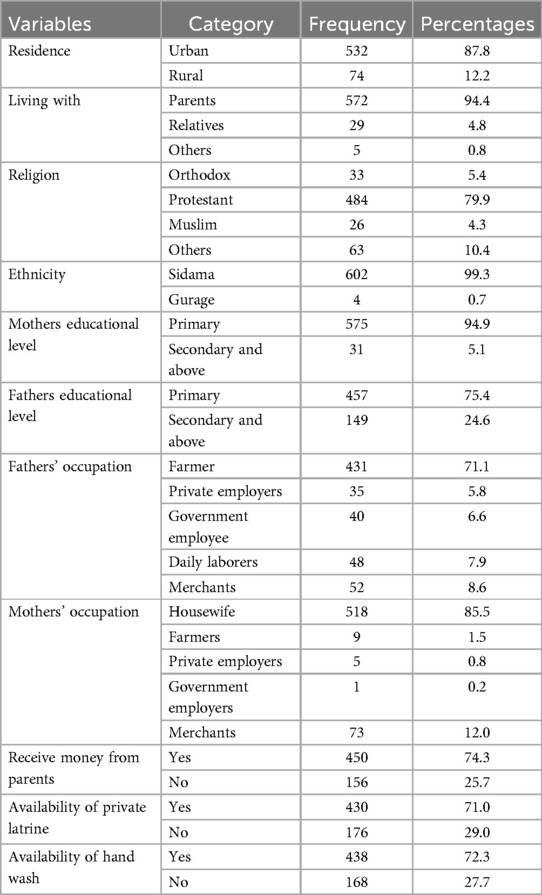
Table 1. Socio-demographic characteristic of adolescent female students in Dale Woreda, 2022; (n = 606).
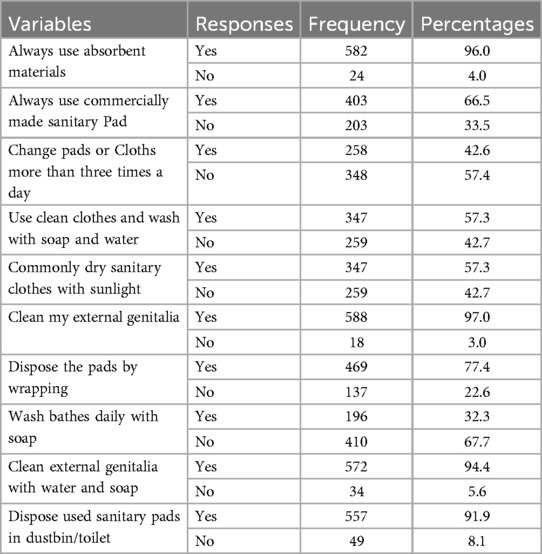
Gynecologic characteristics of respondents
The mean age at menarche for participants was 12.85 (SD ± 1.05). More than four-fifths (84.5%) of participants got information about menstruation before the onset of menarche, of which nearly two-thirds (62.9%) got information regarding menstruation from their school teachers (Figure 1).
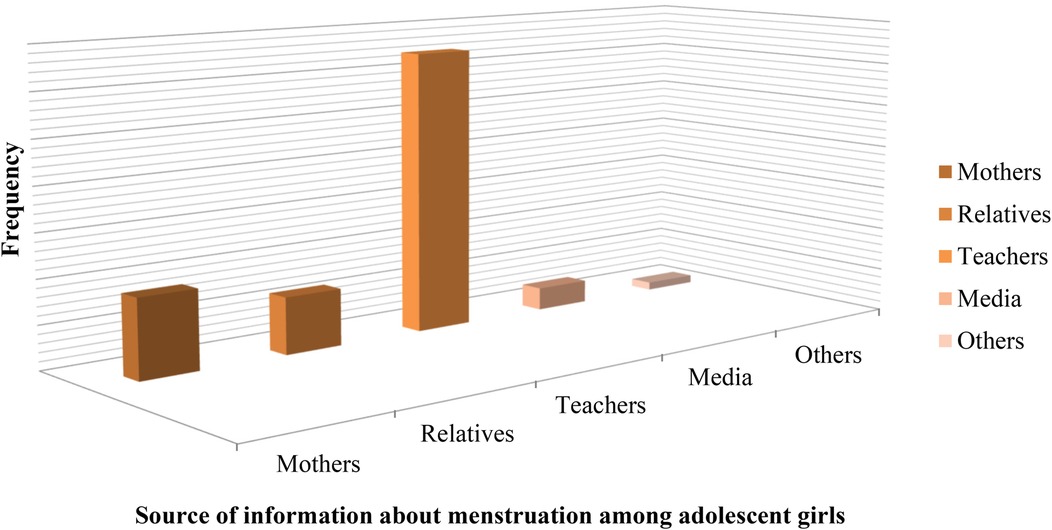
Figure 1. Source of information about menstruation for adolescent female students in Dale Woreda, 2022; (n = 606).
Majority (82.2%) of the respondents had regular menstruation and nearly half (45.4%) of them had a family history of dysmenorrhea. Majority (91.4%) of participants had a menstrual cycle which stays for 3–5 days duration (Table 2).
Knowledge of participants toward menstruation
The majority (83.8%) of the participants knows that menstruation is a physiological process and three-fourths (75.1%) of participants believe that the cause of menstruation is hormonal. More than two-thirds (67.8%) of respondents know that the source of bleeding is the uterus. The majority (91.6%) of participants know about menstrual hygiene, and nearly all (95.4%) of the participants believe that menstruation has a foul smell. The majority (91.7%) of the participants knew that menstrual blood was not hygienic (Table 3).
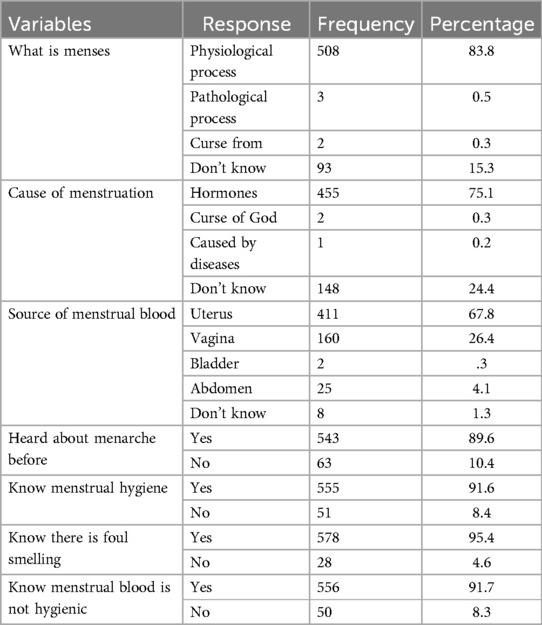
Table 3. Knowledge of adolescent female students toward menstruation in Dale Woreda, 2022; (n = 606).
Regarding the overall knowledge level of the participant, nearly three fourth (72.3%) of respondents had a good knowledge about menstruation (Figure 2).
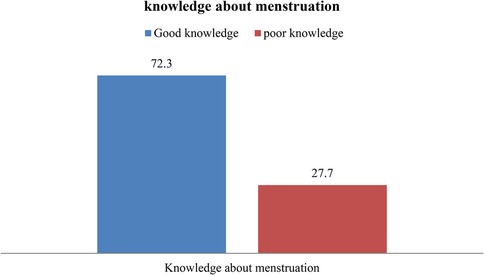
Figure 2. Knowledge of adolescent female students toward menstruation in Dale Woreda, 2022; (n = 606).
Menstrual hygiene practice
Vast majority of the participants (96.0%) use absorbent pads during each menstruation cycle. Two-thirds of them (66.5%) use commercially available sanitary pads, and more than one-third (42.6%) change their pads three times per day. More than half (57.3%) of participants used clean cloth by washing with soap and water. Almost all (97.0%) of the respondents cleaned their external genitalia during menstruation, and most (94.4%) of them used soap and water. More than three-fourths (77.4%) of the participants discarded used pads by wrapping them, and most (91.9%) of them discarded used pads in dustbins. Nearly one third (32.3%) of the respondents took a bath daily during menstrual cycles (Table 4).
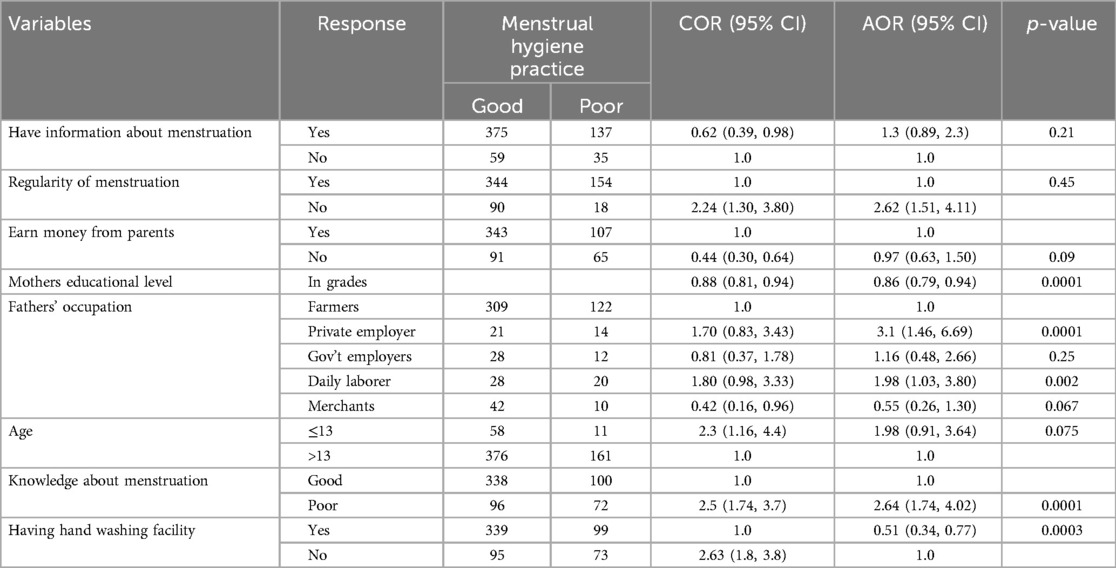
Table 5. Factor associated with poor menstrual hygiene practice among adolescent female students in Dale Woreda; multivariable analysis (n = 606).
The prevalence of poor menstrual hygiene practice was 28.4% (95% CI 25%–32%) which is more than one fourth (Figure 3).
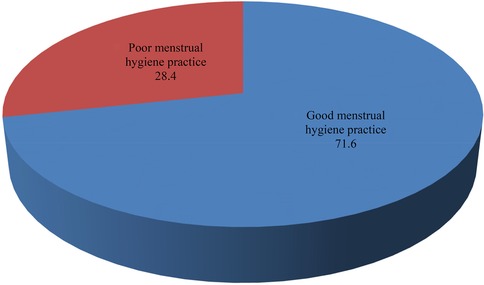
Figure 3. Menstrual hygiene management practices of adolescent female students in Dale Woreda, 2022; (n = 606).
Factors associated with poor menstrual hygiene practice
Knowledge of adolescent girls toward menstruation, fathers' occupation, information about menstruation, regularity of menstruation cycle, earning money from parents, availability of hand washing facilities at the time of changing the menstrual pad, age of the female student, and mother's educational levels had p-values less than 0.25 with poor menstrual hygiene practice, in bivariate logistic regression.
After adjusting for potential confounders, knowledge of adolescent girls toward menstruation, fathers' occupation, availability of hand washing facilities at the time of changing menstrual pads, and mothers' educational level were associated significantly with poor menstrual hygiene practice among adolescent female students in dale woreda.
In our study, poor menstrual hygiene was significantly associated with the knowledge of adolescent girls. The odds of poor menstrual hygiene were three times [AOR = 2.64; 95% CI: 1.74, 4.02] higher among those who had poor knowledge regarding menstruation as compared to those who had good knowledge. The study found that menstrual hygiene was significantly associated with mothers' educational level. The odds of poor menstrual hygiene decreased by 14% [AOR = 0.86, 95% CI: 0.79, 0.94] as mothers' educational level increased by 1 grade compared to lower grades. In this study, fathers' occupations were significantly associated with poor menstrual hygiene practices. The odds of poor menstrual hygiene practice were three [AOR = 3.1; 95% CI: 1.46, 6.69] and two [AOR = 1.98; 95% CI: 1.03, 3.8] times higher among those whose parents work as private employers and daily laborers, respectively, as compared to farmers. The availability of hand washing facilities at the time of changing menstrual pads was related to a lower incidence of poor menstrual hygiene practices. The odds of poor menstrual hygiene practice were 49% [AOR = 0.51, 95% CI: 0.34, 0.77] less among those who had hand washing facilities at the time of changing menstrual pads as compared to their counterparts (Table 5).
Discussion
The aim of this study was to assess menstrual hygiene practices and associated factors among adolescent female students in the Dale woreda. Accordingly, the prevalence of poor menstrual hygiene practice was 28.4% (95% CI: 25%–32%). Poor knowledge of adolescent girls concerning menstrual hygiene, mothers' educational level, fathers' occupation of private employers and daily laborers, and having hand-washing facilities were factors influencing menstrual hygiene practice among school girls. Its prevalence is still considerably high among schoolgirls due to the aforementioned and other contextual factors. To improve menstrual hygiene practice and keep dignity, gender-specific WASH facilities together with awareness creation activities should be implemented in the schools. In addition, schoolgirls require effective, safe, and free/affordable menstrual hygiene products to improve menstrual hygiene practice and academic performance or productivity.
This finding (28.4%) was consistent with a study conducted in Kenya, which reported that 28.8% of adolescent girls had poor menstrual hygiene practices (4). However, this finding was lower when compared with finding from studies conducted in, Dilla, Ethiopia, which showed poor menstrual hygiene management practices of 68.3% (36). Similarly, studies done in India and Ethiopia show a higher prevalence of poor menstrual hygiene management practices (46.4%) and 48.98%, respectively (37, 38). But the finding was higher than the finding from a study conducted in the Amhara region of Mehalmeda, Ethiopia, which showed poor menstrual hygiene management practices of 9.1% (39). The possible explanation for this discrepancy might be socio-demographic and cultural difference among participants. Additionally, poor menstrual hygiene practices, often a result of inadequate access to clean products, toilets, or hygiene education, can have significant health and social consequences (40–42). Good menstrual hygiene management involves safe product use, regular changing, proper disposal, and personal hygiene, all supported by education and resources (40, 43, 44). Studies consistently emphasize the importance of both individual behavior and systemic support in promoting menstrual health (45, 46). Good menstrual hygiene practices can prevent infections, discomfort, and other health complications, while poor menstrual hygiene practices can lead to various physical, emotional, and social challenges (47, 48).
This study found that poor menstrual hygiene was significantly associated with the knowledge level of adolescent girls. The odds of poor menstrual hygiene practice were 2.64 times higher among those who had poor knowledge regarding menstruation as compared to their counterparts. This finding was consistent with studies conducted in Ethiopia and Indonesia (8, 38, 39, 49), which shows, poor knowledge of girls was significantly associated with poor menstrual hygiene practice. A possible explanation for this might be that those adolescent female students who had good knowledge maintained their personal hygiene. Poor knowledge of menstrual hygiene among adolescent female students might make them prone to poor menstrual hygiene practices because they might have no idea what to do during and after menstruation.
Our study showed that having hand washing facilities at the time of changing the menstrual pad was significantly associated with poor menstrual hygiene practices. The odds of poor menstrual hygiene practices were 49% lower among those who had access to hand washing facilities as compared to those who had no access to hand washing facilities. This finding was in line with studies conducted in Kenya and the Amhara region, which showed access to hand washing facilities was associated with increased odds of good menstrual hygiene practices (4, 39). Water with hand washing facilities is an essential component of life to maintain hygiene and other day-to-day activities. Access to water and hand-washing facilities might help the adolescent female students maintain their menstrual hygiene and personal hygiene as well.
In this study, the occupation of a father was significantly associated with the menstrual hygiene practices of adolescent female students. The odds of poor menstrual hygiene practice were three and two times higher among adolescent female students whose parents' occupations were private employers and daily laborers, respectively, as compared to adolescent female students whose parent occupations were farmers. This finding was comparable to a study done in Ghana, which showed decreased odds of poor menstrual hygiene practices and being the daughter of a farmer as compared to other occupations (50). This might be due to the fact the fact that family socio-economic status influences girls' choice of menstrual care products and this may further explain the association between fathers’ occupation and the menstrual hygiene practices of the female students.
The current study found that mothers' educational level and menstrual hygiene practice were significantly associated. The odds of poor menstrual hygiene decreased by 14% when mothers educational level increased by 1 grade. This finding was consistent with different studies conducted in Ethiopia, Indonesia, and Nepal, which revealed that higher mother`s educational level was associated with decreased odds of poor menstrual hygiene practice (8, 49, 51, 52). A possible explanation for this could be that educated mothers might have a better awareness of menstrual hygiene practices, and thus, they could have an open discussion with their daughters about menstruation and/or more likely provide appropriate sanitary materials for them to maintain their menstrual hygiene.
Limitation
The study was conducted on sensitive topic which might make it prone for social desirability bias. Furthermore, participants were adolescent female students aged from 10 to 17 years, they might forget thing easily, so this might cause information bias.
Conclusion
This study was conducted to assess the menstrual hygiene management practices and associated factors of adolescent girls attending primary school in Dale woreda. The study found that poor menstrual hygiene management practice was significantly high. Poor knowledge of adolescent girls toward menstrual hygiene, lack of hand washing facilities at the time of changing menstrual pads, fathers' occupation being private employers and daily laborers, and mothers' educational level were factors significantly associated with poor menstrual hygiene practice in the study area among adolescent female students.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Hawassa University College of Medicine and Health Sciences Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
AA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MG/M: Data curation, Methodology, Conceptualization, Investigation, Validation, Writing – review & editing, Formal Analysis, Supervision, Writing – original draft. HB: Formal Analysis, Writing – original draft, Project administration, Conceptualization, Supervision, Data curation, Methodology, Validation, Investigation, Writing – review & editing. AT: Conceptualization, Writing – original draft, Project administration, Validation, Formal Analysis, Writing – review & editing, Supervision, Investigation, Methodology, Software, Data curation. DT: Supervision, Writing – review & editing, Writing – original draft, Validation, Project administration, Methodology, Data curation. TS: Investigation, Writing – review & editing, Conceptualization, Methodology, Formal Analysis, Writing – original draft, Data curation. TB: Data curation, Project administration, Validation, Resources, Conceptualization, Formal Analysis, Supervision, Writing – original draft, Software, Writing – review & editing, Visualization, Methodology, Investigation.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to acknowledge Hawassa University and the Dale woreda education Office for providing support to conduct this study. We would also like to express our deepest appreciation and gratitude to data collectors, supervisors, and study participants for providing relevant data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Thiyagarajan DK, Basit H, Jeanmonod R. Physiology, Menstrual Cycle. Florida, United States: StatPearls (2020).
2. Dasgupta A, Sarkar M. Menstrual hygiene: how hygienic is the adolescent girl? Indian J Community Med. (2008) 33(2):77. doi: 10.4103/0970-0218.40872
3. Shah V, Nabwera HM, Sosseh F, Jallow Y, Comma E, Keita O, et al. A rite of passage: a mixed methodology study about knowledge, perceptions and practices of menstrual hygiene management in rural Gambia. BMC Public Health. (2019) 19:1–15. doi: 10.1186/s12889-018-6343-3
4. Korir E, Okwara FN, Okumbe G. Menstrual hygiene management practices among primary school girls from a pastoralist community in Kenya: a cross sectional survey. Pan Afr Med J. (2018) 31(1):1–11. doi: 10.11604/pamj.2018.31.222.13521
5. Girod C, Ellis A, Andes KL, Freeman MC, Caruso BA. Physical, social, and political inequities constraining girls’ menstrual management at schools in informal settlements of Nairobi, Kenya. J Urban Health. (2017) 94:835–46. doi: 10.1007/s11524-017-0189-3
6. Kuhlmann AS, Henry K, Wall LL. Menstrual hygiene management in resource-poor countries. Obstet Gynecol Surv. (2017) 72(6):356–76. doi: 10.1097/OGX.0000000000000443
7. Shumie ZS, Mengie ZA. Menstrual hygiene management knowledge, practice and associated factors among school girls, northeast Ethiopia. PLoS One. (2022) 17(7):e0271275. doi: 10.1371/journal.pone.0271275
8. Mohammed Gena H. Menstrual hygiene management practices and associated factors among secondary school girls in east Hararghe zone, eastern Ethiopia. Adv Public Health. (2020) 20:1–7. doi: 10.1155/2020/8938615
9. Manyara MB, Okube OT. Challenges associated with menstrual hygiene among adolescent girls attending bocharia primary school in Nyamira county, Kenya. Open J Obstet Gynecol. (2023) 13(9):1610–24. doi: 10.4236/ojog.2023.139135
10. Hussein J, Gobena T, Gashaw T. The practice of menstrual hygiene management and associated factors among secondary school girls in eastern Ethiopia: the need for water, sanitation, and hygiene support. Women’s Health. (2022) 18:1–12. doi: 10.1177/17455057221087871
11. Vashisht A, Pathak R, Agarwalla R, Patavegar BN, Panda M. School absenteeism during menstruation amongst adolescent girls in Delhi, India. J Family Community Med. (2018) 25(3):163–8. doi: 10.4103/jfcm.JFCM_161_17
12. Yücel G, Kendirci M, Gül Ü. Menstrual characteristics and related problems in 9-to 18-year-old Turkish school girls. J Pediatr Adolesc Gynecol. (2018) 31(4):350–5. doi: 10.1016/j.jpag.2018.03.002
13. Enzler DM, Gass T. Knowledge, attitudes and practices concerning menstrual hygiene management (MHM) of adolescents in rural primary schools in Malawi. Barcelona Inst Glob Heal. (2018) 1947:4–10.
14. Fisseha MA, Kebede Y, Yeshita HY. Menstrual hygiene practice and associated factors among secondary school girls in wegera district, northwest Ethiopia; a cross-sectional study. Comput Biol Bioinform. (2017) 5(1):6–11. doi: 10.11648/j.cbb.20170501.12
15. Anbesu EW, Asgedom DK. Menstrual hygiene practice and associated factors among adolescent girls in Sub-Saharan Africa: a systematic review and meta-analysis. BMC Public Health. (2023) 23(1):33. doi: 10.1186/s12889-022-14942-8
16. Sahiledengle B, Teferu Z, Tekalegn Y, Zenbaba D, Seyoum K, Atlaw D, et al. A multilevel analysis of factors associated with childhood diarrhea in Ethiopia. Environ Health Insights. (2021) 15:11786302211009894. doi: 10.1177/11786302211009894
17. Melaku A, Addis T, Mengistie B, Kanno GG, Adane M, Kelly-Quinn M, et al. Menstrual hygiene management practices and determinants among schoolgirls in Addis Ababa, Ethiopia: the urgency of tackling bottlenecks-water and sanitation services. Heliyon. (2023) 9(5):1–9. doi: 10.1016/j.heliyon.2023.e15893
18. Mulugeta Demmu Y, Shifera GM, Ayana GM, Adare D, Yazew B, Damtew YT, et al. Menstrual hygiene management and associated factors among adolescent school girls in Gursum district, eastern Ethiopia: institution-based a cross-sectional study. BMC Women’s Health. (2023) 23(1):328. doi: 10.1186/s12905-023-02461-6
19. Daniel N, Kejela G, Fantahun F, Desalegn M, Guteta F. Menstrual hygiene management practice and its associated factors among in-school adolescent girls in western Ethiopia. Contracept Reprod Med. (2023) 8(1):1. doi: 10.1186/s40834-022-00196-7
20. Degefu Birhane A, Kaba Serbessa M, Tilahun Degfie T. Menstrual hygiene management: a study of adolescent schoolgirls in Sebeta town, Oromia region, Ethiopia. Glob Drugs Ther. (2019) 4:1–8. doi: 10.15761/gdt.1000175
21. Deriba BS, Garedew G, Gemeda D, Geleta TA, Jemal K, Bala ET, et al. Safe menstrual hygiene management practice and associated factors among female adolescent students at high schools in central Ethiopia: a mixed-method study. Front Public Health. (2022) 10:913262. doi: 10.3389/fpubh.2022.913262
22. Bikis Y. Menstrual hygiene management practice and its associated factors among schoolgirls in north Wollo zone, northeast Ethiopia, 2020: a comparative cross-sectional study. PLoS One (2020):16(1118):e0257853–11. doi: 10.1371/journal.pone.0257853
23. Worku Y, Kassa GM, Mekonen B, Desta M, Bishaw KA, Gedfaw M, et al. Menstrual hygiene management practice and associated factors among high school and preparatory school adolescent students in Debre Markos town, northwest, Ethiopia: a mixed-method study. BMC Women’s Health. (2024) 24(1):420. doi: 10.1186/s12905-024-03265-y
24. Roy D, Kasemi N, Halder M, Majumder M. Factors associated with exclusive use of hygienic methods during menstruation among adolescent girls (15-19 years) in urban India: evidence from NFHS-5. Heliyon. (2024) 10(8):e29731–8. doi: 10.1016/j.heliyon.2024.e29731
25. Girma R, Cheru A, Adare Mengistu D, Bayu K, Dirirsa G, Temesgen S, et al. Menstrual hygiene management practice and associated factors among secondary school girls in eastern Ethiopia: the influence of water, sanitation and hygiene facilities. Women’s Health. (2024) 20:17455057241275606. doi: 10.1177/17455057241275606
26. Htun NN, Laosee O, Rattanapan C. Factors that influence menstrual hygiene management in adolescent girls in Mudon township, Mon state, Myanmar. J Health Sci Med Res. (2020) 39(3):207–17. doi: 10.31584/jhsmr.2021778
27. Akoth C, Wambiya EO, Kibe PM, Mbuthia GW, Ng’ang’a L, Otieno P, et al. Prevalence and factors associated with unmet need for menstrual hygiene management in six countries in Sub-Saharan Africa: a multilevel analysis. BMC Women’s Health. (2024) 24(1):473. doi: 10.1186/s12905-024-03211-y
28. Tesfay E, Redae GH, Goitom G, Asgedom AA. WASH Services and menstrual hygiene management among reproductive age females in the IDPs camps of Shire town in Tigray region of Ethiopia: a cross-sectional study. Sci Rep. (2024) 14(1):22730. doi: 10.1038/s41598-024-73896-6
29. Saini B, Khapre M, Kumar P, Bharadwaj R, Gupta A, Kumar S. Prevalence and barriers of menstrual hygiene practices among women of reproductive age group in rural field practice areas of a tertiary care center in Rishikesh. Indian J Community Med. (2024) 49(1):82–90. doi: 10.4103/ijcm.ijcm_871_22
30. Bhusal CK. Practice of menstrual hygiene and associated factors among adolescent school girls in Dang district, Nepal. Adv Prev Med. (2020) 1:1–7. doi: 10.1155/2020/1292070
31. Ssewanyana D, Bitanihirwe BKY. Menstrual hygiene management among adolescent girls in sub-saharan Africa. Glob Health Promot. (2019) 26(1):105–8. doi: 10.1177/1757975917694597
32. Etoh ECI, Ekanem US, Umoiyoho AJ. Attainment of menstrual hygiene by girls in boarding secondary schools in a state in Sub-Saharan Africa. Int J Reprod Contracept Obstet Gynecol. (2020) 9(3):984. doi: 10.18203/2320-1770.ijrcog20200861
33. Lahme AM, Stern R, Cooper D. Factors impacting on menstrual hygiene and their implications for health promotion. Glob Health Promot. (2018) 25(1):54–62. doi: 10.1177/1757975916648301
34. Shallo SA, Willi W, Abubekar A. Menstrual hygiene management practice and factors affecting it among high school females in Ambo city, Oromia state, Ethiopia, 2018: a cross-sectional mixed method. bioRxiv(2019): 1 806422. doi: 10.1101/806422
35. Adamu AY. Diversity in Ethiopia: a historical overview of political challenges. Int J Community Divers. (2013) 12(3):17. doi: 10.18848/2327-0004/CGP/v12i03/39924
36. Belayneh Z, Mekuriaw B. Knowledge and menstrual hygiene practice among adolescent school girls in southern Ethiopia: a cross-sectional study. BMC Public Health. (2019) 19(1):1–8. doi: 10.1186/s12889-018-6343-3
37. Patil VV, Udgiri R. Menstrual hygienic practices among adolescent girls of rural north Karnataka region, India. Int J Community Med Public Health. (2016) 3(7):1872–6. doi: 10.18203/2394-6040.ijcmph20162058
38. Yalew M, Adane B, Arefaynie M, Kefale B, Damtie Y, Mitiku K, et al. Menstrual hygiene practice among female adolescents and its association with knowledge in Ethiopia: a systematic review and meta-analysis. PLoS One. (2021) 16(8):e0254092. doi: 10.1371/journal.pone.0254092
39. Gultie TK. Practice of menstrual hygiene and associated factors among female Mehalmeda high school students in Amhara regional state, Ethiopia. Sci J Public Health. (2014) 2(3):189–95. doi: 10.11648/j.sjph.20140203.18
40. Sommer M, Figueroa C, Kwauk C, Jones M, Fyles N. Attention to menstrual hygiene management in schools: an analysis of education policy documents in low-and middle-income countries. Int J Educ Dev. (2017) 57:73–82. doi: 10.1016/j.ijedudev.2017.09.008
41. Pednekar S, Some S, Rivankar K, Thakore R. Enabling factors for sustainable menstrual hygiene management practices: a rapid review. Discov Sustain. (2022) 3(1):28. doi: 10.1007/s43621-022-00097-4
42. Chandra-Mouli V, Patel SV. Mapping the Knowledge and Understanding of Menarche, Menstrual Hygiene and Menstrual Health among Adolescent Girls in Low-And Middle-Income Countries. In: The Palgrave Handbook of Critical Menstruation Studies. London: Biomed Central ltd. (2020):609–36.
43. Goddard S, Marni S. Menstrual health and hygiene management and water, sanitation and hygiene (WASH) in urban slums: gaps in the evidence and recommendations. J Gend Water. (2020) 7:4–7.
44. Soto Mendez E. The Case of Menstrual Hygiene Management (MHM) for Improving Girls’ Educational Outcomes in India. Available at SSRN 3825951.
45. Sommer M, Hirsch JS, Nathanson C, Parker RG. Comfortably, safely, and without shame: defining menstrual hygiene management as a public health issue. Am J Public Health. (2015) 105(7):1302–11. doi: 10.2105/AJPH.2014.302525
46. Loughnan L, Mahon T, Goddard S, Bain R, Sommer M. Monitoring Menstrual Health in the Sustainable Development Goals. In: The Palgrave handbook of critical menstruation studies. Springer nature, Singapore (2020). p. 577–92.
47. Zulaika G, Otieno FO, Mason L, van Eijk AM, Bhaumik R, Green SJ, et al. Menstrual cups to reduce bacterial vaginosis and STIs through reduced harmful sexual and menstrual practices among economically vulnerable women: protocol of a single arm trial in western Kenya. BMC Public Health. (2024) 24(1):3089. doi: 10.1186/s12889-024-20491-z
48. Sommer M, Kjellén M, Pensulo C. Girls’ and women’s unmet needs for menstrual hygiene management (MHM): the interactions between MHM and sanitation systems in low-income countries. J Water Sanit Hyg Dev. (2013) 3(3):283–97. doi: 10.2166/washdev.2013.101
49. Hadi EN, Atiqa UD. Menstrual hygiene management of junior high school students in rural areas of Indonesia (study in Tinambung sub-district, Poliweli Mandar, west Sulawesi). J Int Dent Med Res. (2021) 14(3):1230–5.
50. Mohammed S, Larsen-Reindorf RE, Awal I. Menstrual hygiene management and school absenteeism among adolescents in Ghana: results from a school-based cross-sectional study in a rural community. Int J Reprod Med. (2020) 2020:6872491. doi: 10.1155/2020/6872491
51. Upashe SP, Tekelab T, Mekonnen J. Assessment of knowledge and practice of menstrual hygiene among high school girls in western Ethiopia. BMC women’s Health. (2015) 15(1):1–8. doi: 10.1186/s12905-015-0245-7
Keywords: menstrual hygiene, practice, adolescents, associated factors, Sidama, Ethiopia
Citation: Ayele A, G/Mariam M, Beyene H, Tolcha A, Tediso D, Shalamo T and Belayneh T (2025) Menstrual hygiene practice and associated factors among adolescent primary school females in Dale Woreda, Sidama, Ethiopia: a cross sectional study. Front. Reprod. Health 7:1458132. doi: 10.3389/frph.2025.1458132
Received: 1 July 2024; Accepted: 29 January 2025;
Published: 20 February 2025.
Edited by:
Emmanuel Senanu Komla Morhe, University of Health and Allied Sciences, GhanaReviewed by:
Abu Bakkar Siddique, Jahangirnagar University, BangladeshShobha Shah, SEWA Rural, India
Kshitij Karki, G.T.A. Foundation, Nepal
Charles M. Senaya, Kwame Nkrumah University of Science and Technology, Ghana
Copyright: © 2025 Ayele, G/Mariam, Beyene, Tolcha, Tediso, Shalamo and Belayneh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amanuel Ayele, YW1hbnVlbGF5ZWxlNTMzNUBnbWFpbC5jb20=
 Amanuel Ayele
Amanuel Ayele Meskerem G/Mariam2
Meskerem G/Mariam2 Hunachew Beyene
Hunachew Beyene Dansamo Tediso
Dansamo Tediso Teshale Shalamo
Teshale Shalamo Teshale Belayneh
Teshale Belayneh