- 1Division of Maternal and Child Health, Japan Association of Obstetricians and Gynecologists, Tokyo, Japan
- 2Japanese Foundation for Sexual Health Medicine, Tokyo, Japan
Background: This study aimed to analyze the recent prevalence of neonatal herpes simplex virus infection, maternal symptoms in the presence of neonate who has herpes simplex virus infection, and mode of delivery in Japan.
Methods: We requested 2.078 obstetrical facilities that are members of the Japan Association of Obstetricians and Gynecologists (JAOG) to provide information on neonatal herpes simplex virus infection involving deliveries at or after 22 weeks of gestation between 2020 and 2022. Of these, 1.371 (66.0%) facilities responded with information that could undergo statistical analysis.
Results: There were 10 cases of neonatal herpes simplex virus infection, and the incidence of neonatal herpes simplex virus infection in Japan was about 1 in 1.4 × 105 live births. There were no characteristic maternal findings common to cases of neonatal herpes simplex virus infection.
Conclusion: The incidence of neonatal herpes simplex virus infection in Japan was low. We could not identify any characteristic maternal findings common to cases of neonatal herpes simplex virus infection.
1 Introduction
Common sexually transmitted infections, such as genital herpes simplex virus (HSV) infection, are spread by close personal contact (1–4). For example, HSV-1 can be transmitted to another person through kissing or oral sex, while HSV-2 can be acquired via vaginal, anal, or oral contact with an infected individual (1–4). When a woman of reproductive age contracts an infection, HSV infection may be vertically transmitted to neonates.
Neonatal HSV infection may be uncommon; however, the morbidity and mortality associated with infection are high (1–4). The global estimate of the incidence of neonatal HSV has been reported to be 10 cases/100,000 live births; however; however, the incidence and mortality rates have been believed to be underestimated (5–7). It develops after an incubation period of 2 to 10 days, and it is characterized by unclear initial symptoms (3). The first symptoms of neonatal HSV infection can vary from fever, small blisters, lethargy, dyspnea, large abdomen due to ascites or large liver, or no symptoms. HSV encephalitis or infections of other organs such as the liver, lungs, and kidneys can result from HSV infection with or without skin symptoms. Neonatal HSV infection typically causes viral pneumonia and intravascular coagulopathy. Neonates who survive severe infection typically can have lifelong neurological conditions. Although most neonatal HSV infections are acquired perinatally through the birth canal, many newborns with HSV infection have been reported to be born to mothers with no prior history of HSV infection or symptoms (1, 3, 8).
Therefore, to prevent trans-vaginal infections if genital lesions are present at delivery, cesarean section has been recommended for pregnant women with HSV infection (1, 2, 8, 9). For example, in the guidelines for obstetrical practice in Japan 2020 (= Japanese guidelines) (9) elective cesarean delivery has been recommended before labor or premature rupture of the membranes under the following conditions: (a) genital lesions of HSV infection recognized or strongly suspected at admission for delivery, (b) delivery within a month after primary HSV infection, and (c) delivery within a week after recurrent or non-primary HSV infection.
In our earlier survey in Japan in 2017, the proportion of women with symptoms of genital HSV infection during pregnancy was 1 in 536, and cesarean delivery indicated for genital HSV infection was performed in 15% (about 280) of the women (10). However, approximately 30% of mothers with neonatal HSV infections have been reported to show symptoms of the disease (1, 3). In addition, in our earlier observation in Japan, none of 6 cases with cerebral palsy due to neonatal HSV infection showed any findings suggestive of HSV infection in mothers (11). Furthermore, it has been suggested to be uncommon for HSV to be transmitted vertically during the preclinical phase of the disease (12, 13). Therefore, it may be important to investigate mothers whose neonates develop neonatal HSV infection.
To evaluate the effectiveness of cesarean section as recommended by the guidelines (9) and re-examine strategies to prevent the development of neonatal HSV infection in the future, this study aimed to analyze the recent status of neonatal HSV infection, maternal symptoms in the presence of a neonate who has HSV infection, and mode of delivery in Japan.
2 Methods
2.1 Study population
The protocol for this study was approved by the Ethics Committee of the Japan Association of Obstetricians and Gynecologists (JAOG). In March 2023, we requested 2.078 obstetrical facilities that are members of JAOG to provide information on neonatal HSV infection in deliveries at or after 22 weeks of gestation between January 2020 and December 2022. In Japan, all infants are required to undergo a physical examination at the delivery institutes one month after birth, and so obstetricians at the institutes can always be aware of cases with onset of neonatal HSV infection within 10 days after birth. Furthermore, institutes affiliated with JAOG report the number of deliveries each year in detail to the JAOG office, so the incidence of neonatal HSV infection can be calculated based on those figures.
Of the 2.078 facilities, 1.371 (66.0%) facilities responded with information that could undergo statistical analysis. At the 1.371 facilities, 1.433.001 neonates were born during the study period, which corresponded to about 59.2% of the total number of births in Japan (average number of births during the year: about 810.000).
2.2 Clinical assessment
The information requested was as follows: maternal age, past history of HSV infection, gestational age at delivery, premature rupture of the membranes, maternal symptoms indicating viral infection around the time of delivery, delivery mode, timing of the onset of neonatal HSV infection, disease type and HSV type of neonatal HSV infection.
3 Results
3.1 Incidence of neonatal HSV infection in Japan
During the study period, there were 10 cases of neonatal HSV infection. Therefore, the incidence of neonatal HSV infection in Japan was about 1 in 1.4 × 105 live births.
3.2 Characteristics of neonates in 10 cases of HSV infection
Table 1 shows the maternal and neonatal characteristics of the 10 cases of neonatal HSV infection. The average maternal age was 27.6 ± 6 years, and 2 mothers were in their teens. One case delivered at 29 weeks because of premature rupture of the membranes, while the other 9 cases delivered at term.
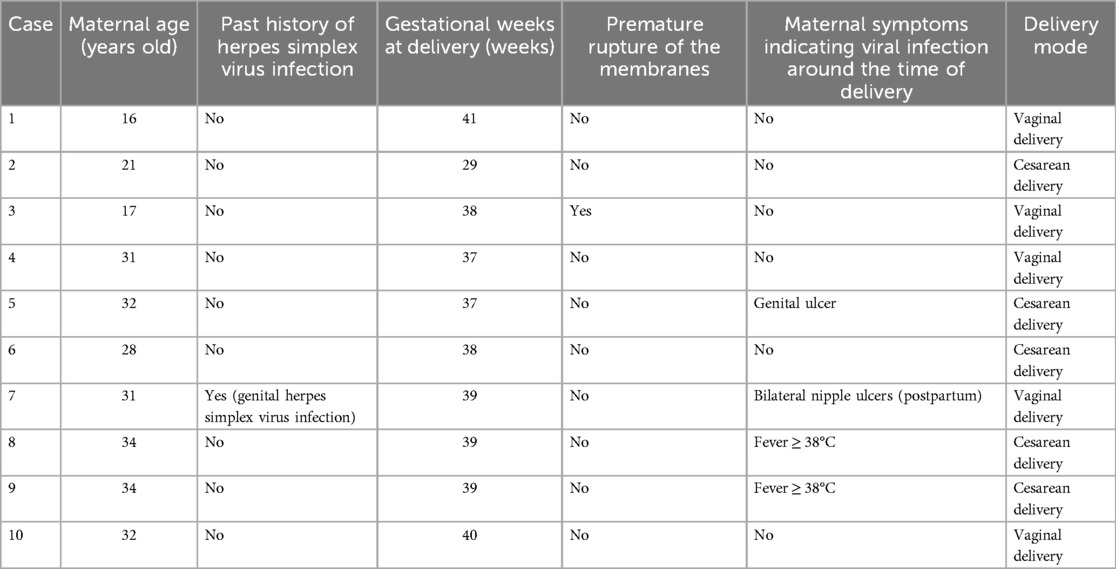
Table 1. Clinical characteristics of mothers in 10 cases of neonatal herpes simplex virus infection in Japan.
In this study, 3 mothers had cesarean section because of the symptoms of viral infection such as genital ulcers or fever (≥ 38℃), while 2 had cesarean sections for other obstetric indications unrelated to the infection. One mother had ulcers on both nipples after vaginal delivery. She was the only one with a history of genital HSV infection.
In this study, the average timing of the onset of neonatal HSV infection was 4.1 ± 3 days after delivery. Four neonates had disseminated infections, 2 had central nervous system (CNS) infections, and 4 had skin/eye/mouth disease of HSV infection as shown in Table 2.
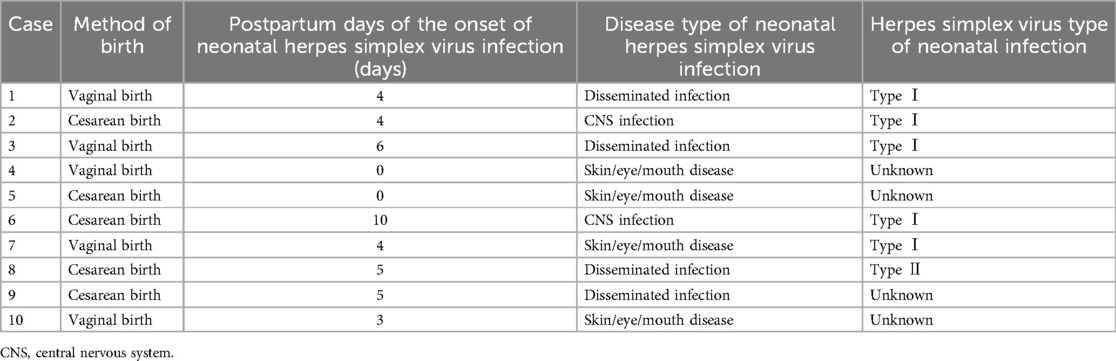
Table 2. Clinical characteristics of neonates in 10 cases of neonatal herpes simplex virus infection in Japan.
4 Discussion
In this study, the incidence of neonatal HSV infection in Japan was about 1 in 1.4 × 105 live births. In addition, we analyzed the characteristics of the mothers whose neonates had HSV infection to examine the risk of developing neonatal HSV infection. However, we could not find any other characteristic maternal findings common to cases of neonatal HSV infection except that the average age of mothers was slightly lower than that of Japanese average (27.6 vs. 30.7 years) (14).
Recently, neonatal HSV infection was reported to be identified at an incidence of 1 in 9 × 105 live births in Denmark (15) and 1 in 0.4 × 105 live births in Germany (16). There were no significant differences in neonatal HSV prevention measures, such as the use of prophylactic antiviral medications and prophylactic cesarean delivery in these countries (9, 15, 16). However, there may be room for improvement in strategies for the prevention of neonatal HSV infection in Japan.
To date, risk factors for neonatal HSV infection included vaginal delivery, first HSV infection, and prolonged premature rupture of the membranes (9, 17). One previous large-scale study in 2009 reported that HSV was isolated from the genital tract of the mother during delivery and that primary infection of HSV was a risk factor for neonatal HSV infection (18). In this study, it is considered that all cases would have been managed according to the Japanese guidelines (9), and since no case-control study was conducted, it is not possible to assess whether management according to the Japanese guidelines, including prophylactic cesarean section, is effective for preventing neonatal HSV infection. However, the current results, as well as those of other reports (1–4), reconfirmed that many mothers of neonates with HSV infection had no symptoms of the infection.
In this study, only 3 of the 10 mothers had symptoms of HSV at delivery, including one mother with a genital ulcer. Despite the fact that prophylactic cesarean delivery was performed for the 3 women as indicated by the guidelines (9), it did not prevent the development of neonatal HSV infection. Therefore, additional factors to prevent neonatal HSV infection in Japan should be examined in further studies.
In cases of neonatal HSV infection, the initiation of long-term antiviral suppressive therapy at an early stage of the disease has been reported to facilitate significant improvement in morbidity (3); however, the initial action might be delayed in cases without findings of HSV infection in the mother. Mothers of infants who acquire neonatal HSV infection sometimes lack histories of clinically evident genital HSV infection; therefore, clinicians should also recognize asymptomatic primary genital HSV infections (19). Based on the current results, the incidence of neonatal HSV infection might be low in Japan; however, we always have to keep in mind that neonatal HSV infection may develop under any circumstances. Therefore, at this point in time, it is important when mothers feel somewhat strange regarding their neonates and infants, and they should always communicate such feelings to medical professionals (13). In addition, medical professionals must always listen to the mother's complaints.
We understand the serious limitation of the short study period: the prevalence of HSV is low, and the 2-year study period may not have been sufficient to reflect the characteristics of neonatal HSV infection in Japan. Also, because reporting cases of HSV infections has not been mandatory in Japan, it may be challenging to increase awareness of the reporting of HSV infection. In addition, it was not possible to account for confounders concerning individual factors associated with neonatal HSV infection. There is also a possibility of response bias because the questionnaire was aimed at obstetric institutes. Although it may be important to identify the route of neonatal HSV infection, we could not identify trends in the risk of developing neonatal HSV infection in mothers.
A further study with the accumulation of many more cases of neonatal HSV infection may promote prevention in the future; however, in this study, only the need for awareness of the indeterminate complaints of neonates was recognized.
5 Conclusions
The incidence of neonatal HSV infection in Japan was about 1 in 1.4 × 105 live births. The current study could not address the merits of the Japanese guidelines on prophylactic cesarean section. In addition, we could not identify any characteristic findings common to cases of neonatal HSV infection in most mothers.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the ethics committee of Japan Association of Obstetricians and Gynecologists. No personal information (pregnant women or children) was collected in the institutional survey. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
JK: Data curation, Formal Analysis, Methodology, Project administration, Writing – original draft. SS: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. S-IH: Investigation, Methodology, Writing – review & editing. AS: Investigation, Methodology, Writing – review & editing. YS: Investigation, Methodology, Writing – review & editing. HM: Investigation, Methodology, Writing – review & editing. II: Investigation, Methodology, Writing – review & editing. TK: Investigation, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We thank JAOG members for their cooperation with the questionnaire.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pinninti SG, Kimberlin DW. Preventing herpes simplex virus in the newborn. Clin Perinatol. (2014) 41(41):945–55. doi: 10.1016/j.clp.2014.08.012
2. Pinninti SG, Kimberlin DW. Neonatal herpes simplex virus infections. Semin Perinatol. (2018) 42(3):168–75. doi: 10.1053/j.semperi.2018.02.004
3. Kimberlin DW, Lin CY, Jacobs RF, Powell DA, Frenkel LM, Gruber WC, et al. National institute of allergy and infectious diseases collaborative antiviral study group. Natural history of neonatal herpes simplex virus infections in the Acyclovir era. Pediatrics. (2001) 108(2):223–9. doi: 10.1542/peds.108.2.223
4. Harris JB, Holmes AP. Neonatal herpes simplex viral infections and Acyclovir: an update. J Pediatr Pharmacol Ther. (2017) 22(2):88–93. doi: 10.5863/1551-6776-22.2.88
5. Looker KJ, Magaret AS, May MT, Turner KME, Vickerman P, Newman LM, et al. First estimates of the global and regional incidence of neonatal herpes infection. Lancet Glob Health. (2017) 5(3):e300–e9. doi: 10.1016/S2214-109X(16)30362-X
6. Matthias J, du Bernard S, Schillinger JA, Hong J, Pearson V, Peterman TA. Estimating neonatal herpes simplex virus incidence and mortality using capture-recapture, Florida. Clin Infect Dis. (2021) 73(3):506–12. doi: 10.1093/cid/ciaa727
7. Melvin AJ, Mohan KM, Vora SB, Selke S, Sullivan E, Wald A. Neonatal herpes simplex virus infection: epidemiology and uutcomes in the modern era. J Pediatric Infect Dis Soc. (2022) 11(3):94–101. doi: 10.1093/jpids/piab105
8. Anzivino E, Fioriti D, Mischitelli M, Bellizzi A, Barucca V, Chiarini F, et al. Herpes simplex virus infection in pregnancy and in neonate: status of art of epidemiology, diagnosis, therapy and prevention. Virol J. (2009) 6:40. doi: 10.1186/1743-422X-6-40
9. Itakura A, Shoji S, Shigeru A, Kotaro F, Junichi H, Hironobu H, et al. Guidelines for obstetrical practice in Japan: japan society of obstetrics and gynecology and Japan association of obstetricians and gynecologists 2020 edition. J Gynecol Oncol. (2023) 34(1):e10. doi: 10.1111/jog.15438
10. Japan Association of Obstetricians and Gynecologists. Report on the results of a survey on genital herpes infection during pregnancy (in Japanese) (2018). Available online at: https://www.jaog.or.jp/wp/wp-content/uploads/2018/01/20180126.pdf (accessed February 2024).
11. Suzuki S. Emergent serious condition of the neonates associated with cerebral palsy in Japan. Placenta Reprod Med. (2022) 1(1):5. doi: 10.54844/prm.2022.0084
12. Caviness AC, Demmler GJ, Selwyn BJ. Clinical and laboratory features of neonatal herpes simplex virus infection: a case-control study. Pediatr Infect Dis J. (2008) 27:425–30. doi: 10.1097/INF.0b013e3181646d95
13. Suzuki S. Transmission of the herpes simplex virus in the preclinical phase of disease progression during childbirth. JMA J. (2023) 6(2):223–5. doi: 10.31662/jmaj.2022-0200
14. Ministry of Health, Labour and Welfare. Summary of birth statistics (in Japanese) (2021). Available online at: https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/tokusyu/syussyo07/index.html (accessed June 2024).
15. Dungu KHS, Lund S, Malchau Carlsen EL, Hartling UB, Matthesen AT, Franck KT, et al. Herpes simplex virus infection among neonates suspected of invasive bacterial infection: a population-based cohort study. Arch Dis Child Fetal Neonatal Ed. (2023) 108(6):655–60. doi: 10.1136/archdischild-2023-325583
16. Kidszun A, Bruns A, Schreiner D, Tippmann S, Winter J, Pokora RM, et al. Characteristics of neonatal herpes simplex virus infections in Germany: results of a 2-year prospective nationwide surveillance study. Arch Dis Child Fetal Neonatal Ed. (2022) 107(2):188–92. doi: 10.1136/archdischild-2021-321940
17. James SH, Kimberlin DW. Neonatal herpes simplex virus infection. Infect Dis Clin North Am. (2015) 29(3):391–400. doi: 10.1016/j.idc.2015.05.001
18. Corey L, Wald A. Maternal and neonatal herpes simplex virus infections. N Engl J Med. (2009) 361(14):1376–85. doi: 10.1056/NEJMra0807633
Keywords: herpes simplex virus infection, neonate: risk factor, Japan, maternal symptom, incidence
Citation: Kojima J, Suzuki S, Hoshi S-I, Sekizawa A, Sagara Y, Matsuda H, Ishiwata I and Kitamura T (2024) Challenges for early diagnosis of neonatal herpes infection in Japan. Front. Reprod. Health 6:1393509. doi: 10.3389/frph.2024.1393509
Received: 29 February 2024; Accepted: 30 July 2024;
Published: 8 August 2024.
Edited by:
Elizabeth Bukusi, Kenya Medical Research Institute (KEMRI), KenyaReviewed by:
Eleftheria Hatzidaki, University of Crete, GreeceDasja Pajkrt, Academic Medical Center, Netherlands
© 2024 Kojima, Suzuki, Hoshi, Sekizawa, Sagara, Matsuda, Ishiwata and Kitamura. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shunji Suzuki, c2h1bkBubXMuYWMuanA=
 Junya Kojima1
Junya Kojima1 Shunji Suzuki
Shunji Suzuki