
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Reprod. Health , 19 July 2024
Sec. Access and Barriers to Reproductive Health Services
Volume 6 - 2024 | https://doi.org/10.3389/frph.2024.1353699
 Fassikaw Kebede Bizuneh*
Fassikaw Kebede Bizuneh* Semira Muhidin Mustofa
Semira Muhidin Mustofa
Background: Vaccinating pregnant women with tetanus toxoid (TT) is crucial to prevent neonatal tetanus, reducing related deaths by 94%. In conflict zones with restricted access to deliveries, neonates face a fatality rate of 80%–100%. This study explores the uptake of protective TT vaccine doses and maternal associated factors during pregnancy in an armed conflict zone.
Methods: A hospital-based, descriptive, cross-sectional study was conducted of 357 pregnant women at delivery using simple random sampling. Data were collected through interviews with a structured questionnaire, and entered using Epi-data version 3.1, and exported using SPSS version 22 for further analysis. Binary and multivariable logistic regression analyses were used to identify significant variables for receiving protective TT doses during pregnancy at P < 0.05.
Result: In this study, 355 pregnant women were included, with response rate of 99.4%. The mean age of the participants was 27.65 ± 6.23 years. During the study period, 67.3% of pregnant women received a protective TT vaccine dose while 33.3% were missed due to escalated armed conflict. The dropout rates were significant from TT5 to TT2 (17.6%), TT5 to TT3 (11.9%), and TT5 to TT4 (6.1%). However, maternal associated factors for the uptake of the TT protective vaccine dose were identified, including being aged 36–49 years [adjusted odds ratio (AOR) = 3.7; 95% confidence interval (CI) 1.54–7.8; P = 0.001], completing high school (AOR = 3.05; 95% CI 1.5–8.9; P = 0.02), having an antenatal care follow-up (AOR = 9.4; 95% CI 2.9–24.3; P = 0.001), previous media exposure (AOR = 15.5; 95% CI 7.5–25.3; P = 0.001), and good maternal knowledge (AOR = 2.7; 95% CI 1.8–4.9; P = 0.02).
Conclusion: The uptake of the protective TT vaccine dose among pregnant women in a continued armed conflict area was low compared with previous study findings. Efforts should be made to increase vaccine uptake and reduce dropout rates by addressing both community and individual-level factors.
Tetanus is caused by a neurotoxin produced by the bacterium Clostridium tetani and has a fatality rate of 80%–100% (1, 2). Immunizing pregnant women or women of childbearing age with two doses of the tetanus toxoid (TT) vaccination can potentially reduce neonatal tetanus mortality by 94% (3, 4). To prevent tetanus-related deaths, pregnant women should receive a minimum of three doses of tetanus-specific immunoglobulin (TIG) (5, 6). The World Health Organization (WHO) recommends five TT vaccine doses for individuals with unknown immunization status (7). In the first pregnancy, two doses of the TT vaccine are recommended, with the first dose given during the first antenatal care (ANC) visit and the second dose administered 4 weeks later (8–10). This immunization provides anti-tetanus antibodies for both mother and infant antibodies, transferred across the placenta as IgG, offers protection, and with 0.1–0.15 IU/ml is advised (1, 2, 11).
Globally, tetanus is a significant public health issue, especially in areas with low immunization coverage and limited access to clean deliveries. Each year, an estimated 3.3 million neonatal deaths occur worldwide, with 34,019 deaths attributed to tetanus, as reported by the WHO in 2017 (4, 12). Each year, approximately 303,000 women die from pregnancy-related complications, leading to approximately 830 deaths per day, as per the latest estimates from the WHO (13, 14). The majority (90%) of maternal and neonatal morbidity of tetanus occurred in countries in Southeast Asia and sub-Saharan Africa (15, 16). In India alone, 14,751 cases of tetanus were reported in 2019 (17).
A systematic review and meta-analysis conducted in Ethiopia revealed that only 52.6% of pregnant women received at least two doses of the TT vaccine (6, 13) with significant regional disparities, including 72.5% in SNNPR (18), 39.2% in Oromia (14), 56.2% in Debre Tabor and Amhara regions (19), and 40.2% in Tigray (20). Previously, tetanus infections accounted for 24% of neonatal mortality, a range of 14–31 per 1,000 live births (1, 3, 10). Previous research conducted in Ethiopia (1, 3, 8, 9, 21) has identified factors associated with deterring the protective dose of the TT vaccine, including late initiation of ANC, no ANC visit, poor wealth index, lack of media exposure, maternal unemployment, rural residence, and high community illiteracy (3). A study on reproductive-aged women indicated the dropout rate for TT was reported at 55.6% (TT1 to TT5). The dropout rates were 5.3% for TT1–TT2, 14.7% for TT2–TT3, 20.2% for TT3–TT4, and the highest, 31.1%, for TT4–TT5 (4, 22).
In Ethiopia during the civil war of North East Ethiopia (between July 2021 and 28 November 2023), the Amhara region was heavily impacted, with 50% of healthcare facilities damaged, resulting in interrupted maternal health services for 70,000 pregnant women (11, 22) and including 1.4 million displacements and 600,000 reported death (1, 22). The civil war impacted delivery of the TT vaccination service in areas of conflict due to security issues and the destruction of healthcare facilities (7, 10). Therefore, the aim of this hospital-based, cross-sectional study was to assess the level of uptake of the protective TT vaccine dose and maternal factors during pregnancy in an armed conflict zone of Saint Lalibela.
A facility-based, cross-sectional study was conducted at St. Lalibela General Hospital between 16 February and 7 March 2023. Situated in Lalibela town, the hospital serves the capital of the Lasta Lalibela district in the North Wollo Zone of northern Ethiopia. It is located 622.5 km away from Addis Ababa and 310 km from Bahir Dare. The hospital provides healthcare services to a population of approximately 600,000 people annually. The study area was selected due to the long-lasting armed conflicts during the civil war, which resulted in numerous disruptions, including over 1,000 recorded civilian deaths and injuries in the region.
A hospital-based, cross-sectional study was employed among 357 pregnant women in St. Lalibela General Hospital.
All pregnant women receiving delivery services at St. Lalibela General Hospital during the study period were included in the interviews. However, mothers who were not pregnant and seeking maternal and child health services, including family planning or care for illnesses, at the hospital were excluded from the study.
Uptake of the protective TT vaccine dose refers to the protection provided to pregnant women who have received at least two doses of TT (2, 23); or tetanus toxoid protective dose immunization (TTPDI) is defined as the proportion of mothers who have received any of the following documented TT doses: (1) two TT injections during the pregnancy; (2) two or more injections, with the last one administered within 3 years of the birth; (3) three or more injections, with the last one administered within 5 years of the birth; (4) four or more injections, with the last one administered within 10 years of the birth; or (5) five or more injections at any time before the birth (2).
Neonatal tetanus typically occurs within 3–21 days of birth and is caused by the introduction of tetanus spores through the umbilical cord during delivery, often as a result of using unclean materials to cut the cord (24).
Reproductive-aged women were asked about their exposure to TT vaccine messages through television, radio, newspaper, and mobile messages. To simplify the analysis, a variable called “exposure to mass media messages” was created, coded as “yes” if respondents had previous exposure to these messages (25).
The dependent variable in this study is TT vaccine uptake (Yes/No).
The independent variables included sociodemographic factors (age, marital status, level of education, occupation, residence, and income), obstetric and related factors (nulliparity, planned pregnancy, pregnancy-related complications), health and health-related factors (distance from the health facility, ANC follow-up), and media exposure.
The sample size of this study was estimated using a single population proportion formula: n = (z2 × p × (1 − p))/d2. Based on a prevalence of 69.8% reported from Gondar University Hospital in 2019 (10), with a 95% confidence interval (CI; z = 1.96) and a margin of error of 5% (d = 0.05), the formula yielded a sample size of approximately 324. Finally, after considering a non-response rate of 10%, the final sample size was 357.
Pregnant mothers who received immediate postnatal care were interviewed, excluding severely deaf and mentally ill individuals. The questionnaire was prepared in English and translated into Amharic. Face-to-face interviews were conducted using the Kobo Toolbox, involving data collectors, supervisors, and investigators. The interview questions covered sociodemographic data, conflict-related factors, health facility-related information, and TT vaccination. A pre-test was conducted at Woldia Health Centre with 18 mothers (5% of the sample size) to ensure questionnaire consistency. The questionnaire was translated back to English from Amharic to ensure understandability and consistency. Data collection was carried out by a public health supervisor and two trained nurses. The interview questions focused on sociodemographic data, such as age, marital status, educational status, occupation, economic status, residence, number of children, and ANC follow-up, vaccination information, distance from the health facility, media exposure related to vaccination, and history of previous ANC follow-up and immunization.
Data were checked for completeness and consistency before analysis. The Kobo toolbox was used for data collection, and the collected data were exported to SPSS version 25 for further analysis. The descriptive analysis determined means, frequency, and percentage distributions. Bivariate and multivariable logistic regressions were conducted. Independent variables with a p-value < 0.25 in bivariate logistic regression were included in the multivariable logistic regression, considering collinearity and data normality using a stepwise backward elimination procedure. The model's fitness was assessed using the Hosmer–Lemeshow goodness-of-fit test. Categorical variables with adjusted odds ratios (AOR) and 95% CIs were selected as determinants of TT vaccine coverage at p < 0.05. Knowledge about the TT vaccination was assessed using nine structured questions, and a mean score was calculated. Scores below the mean were considered poor knowledge, while scores above the mean were considered good knowledge. The Cronbach alpha test was conducted, and the overall knowledge-related assessment questions yielded a p-value of 0.76 (12, 26, 27).
Out of 357 postnatal women, 355 were interviewed, resulting in a response rate of 99.5%. The participants had a mean age of 27.65 ± 6.23 years, with the majority (72.4%) in the age range of 26–34. Of the participants, 91 (37.3%) had completed primary education or higher. Over half of the participants (91.5%) were married, with 220 (62.2%) being housewives. The majority of respondents (89.1%) identified as Orthodox religious followers, while 110 (30.9%) had to travel over 10 km to reach a health institution for ANC care (Table 1).
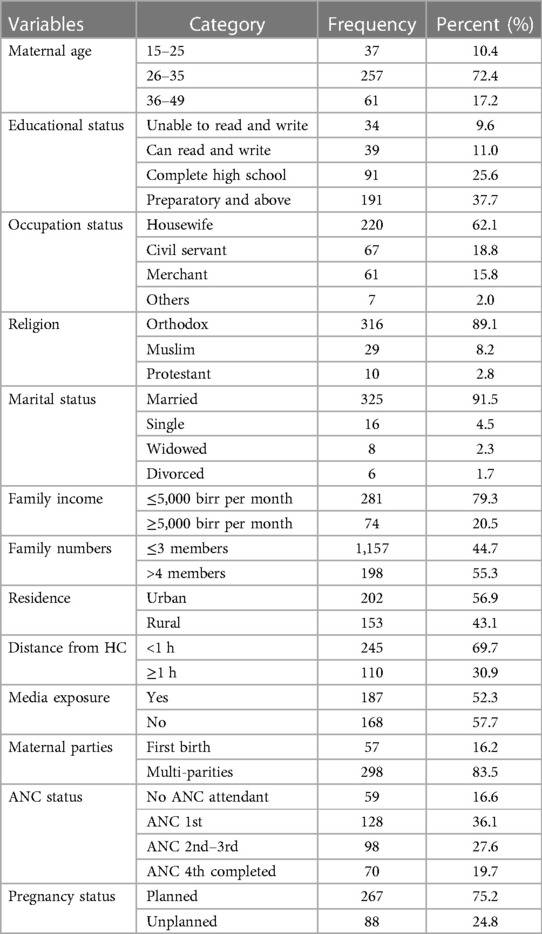
Table 1 Socio-demographic characteristics of study participants in St. Lalibela General Hospital for protective doses of TT vaccine.
Of the total participants, majorities 267 (71.6%) of women had response for planned pregnancies and received support from their families. Moreover, 298 (83.5%) postnatal women were multiparous women, 70 (33.8%) completed fourth ANC visit, but 59 (16.6%) did not have any ANC follow-up.
The majority of participants (84.5%) were aware of the benefits of the TT vaccine, with 80.6% knowing that it is free of cost. In addition, 52.3% of participants had previous exposure to media messages about the importance of TT vaccine uptake. More than half (64.5%) believed that the TT vaccine had dual benefits for infants. Furthermore, 81.7% were aware that tetanus can be caused by unsafe delivery and injuries. Lastly, 73.5% of participants had good knowledge about the recommended TT vaccination dose for the protection of neonates and mothers (Table 2).
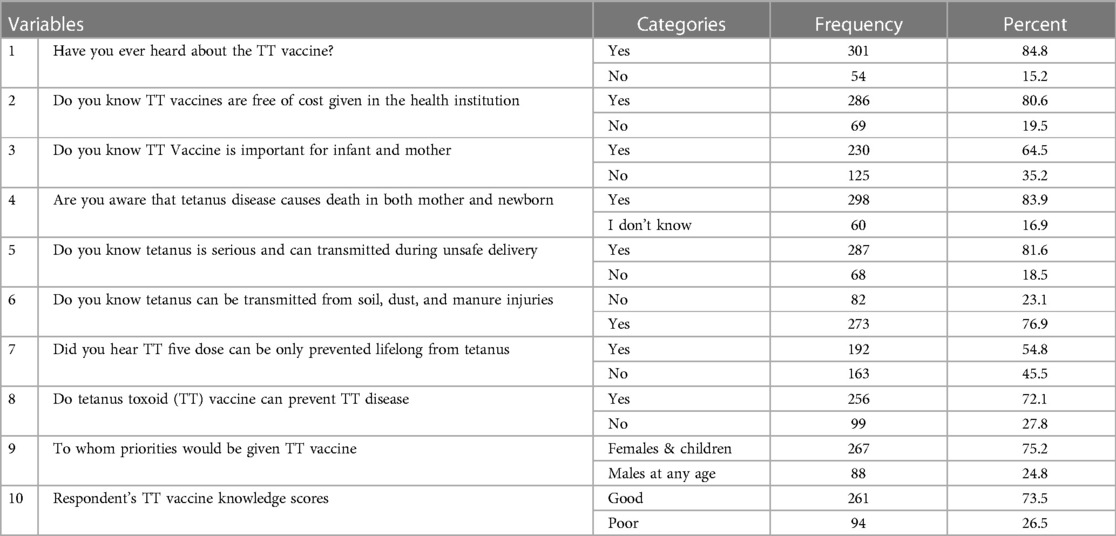
Table 2 Level of maternal knowledge about TT vaccine protective doses for participant s women in St. Lalibela General Hospital for.
In this study, more than half of the participants 258 (57.5%) experienced food insecurity, and 16.3% (59) lost at least one family member during the escalated war of Tigray people liberation front (TPLF) with Northern parts of Amhara region (Table 3).
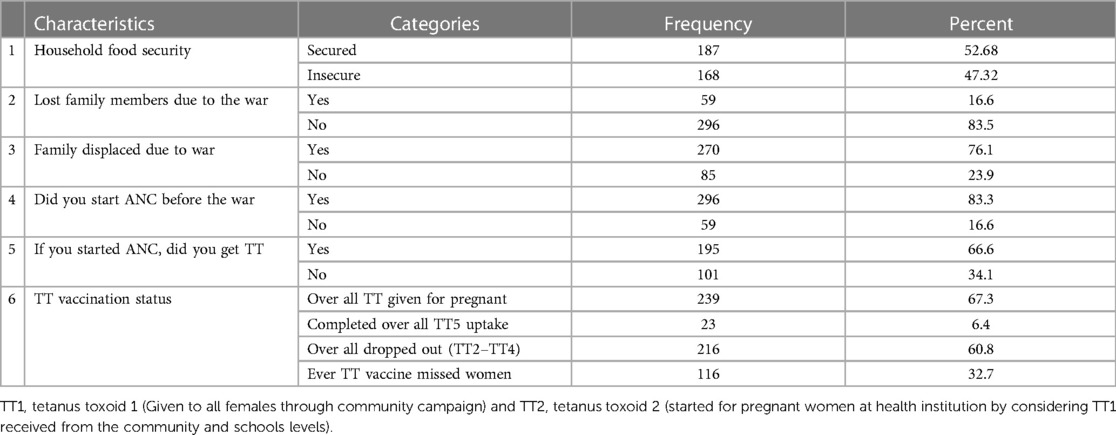
Table 3 Burden of maternal individual characteristics factors during escalated war among participant women in St. Lalibela General Hospital, 2023.
The overall TT vaccine protective dose uptake was found 67.3% received the protective doses (TT2), nonetheless only 6.4% participant's women completed TT5 dose (Figure 1).
During the interview, significant dropout rates were observed across different TT uptake intervals, with 17.6% from TT5 to TT2, 11.9% from TT5 to TT3, and 6.1% from TT5 to TT4, attributed to reasons such as war outbreaks (41.6%), forgetting their schedule (31.4%), and fear of side effects (28.2%), indicating notable variation in TT vaccine uptake interval (Figure 2).
In the regression analysis, variables associated with the coverage of a protective dose of TT vaccine were identified using a significance threshold of p < 0.25. Eight variables, including age, residence, pregnancy status, level of education, occupation, number of ANC visits, and marital status, were included in the final multivariable logistic regression model. The results showed that age, knowledge of the TT vaccine, previous mass media exposure, level of education, and fourth ANC follow-up status were significantly associated with achieving protective TT doses within a 95% CI. Specifically, mothers aged 15–25 years were 3.7 times more likely to receive the protective dose compared to those aged 36–49 years (AOR = 3.7; 95% CI 1.54–7.8; p = 0.001). Completing high school or above (AOR = 3.05; 95% CI 1.5–8.9; p = 0.02), having the fourth ANC follow-up (AOR = 9.4; 95% CI 2.9–24.3; p = 0.001), exposure to media for TT (AOR = 15.5; 95% CI 7.5–25.3; p = 0.001), and having good knowledge (AOR = 2.7; 95% CI 1.8–4.9; p = 0.02) were also significantly associated with achieving the protective dose of TT2 during pregnancy (Table 4).
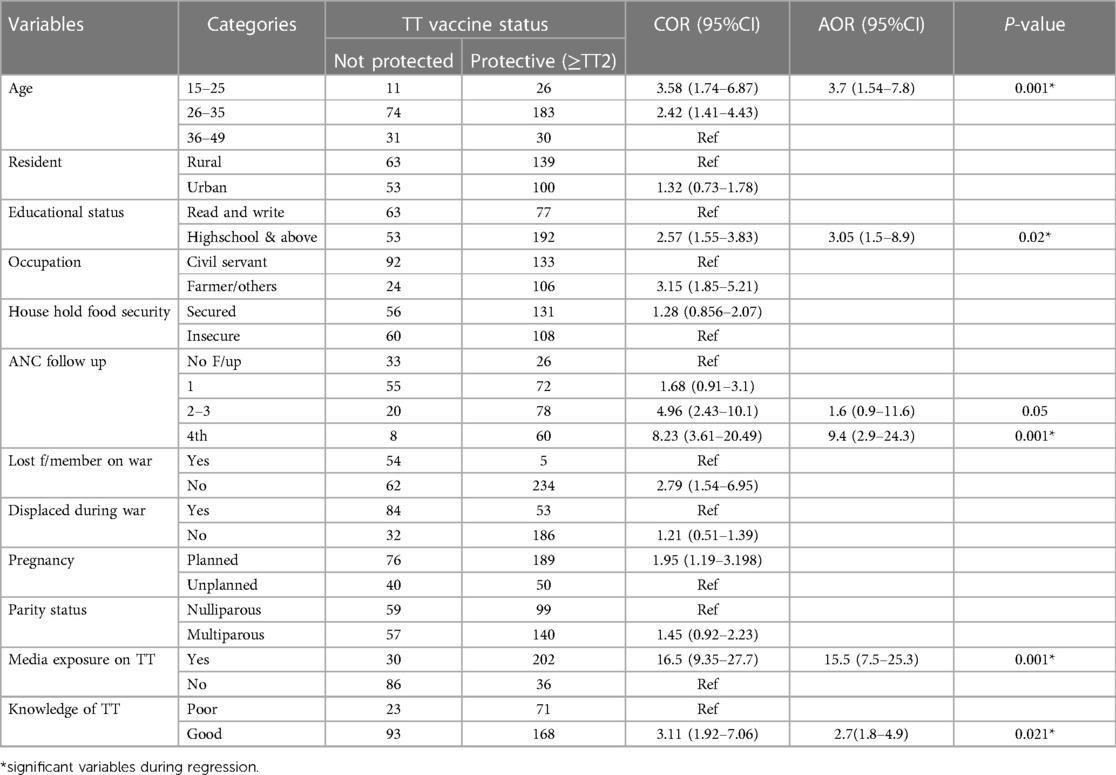
Table 4 Factors associated with uptake of protective tetanus toxoid vaccine doses among mothers during pregnancy in St. Lalibela Hospital, North Wollo Zone, Northeast Ethiopia.
Tetanus is a vaccine-preventable disease that can occur in all populations, with neonates and pregnant women at highest risk. Ethiopia has the highest maternal and neonatal tetanus morbidity and mortality rates and only 49% of mothers get vaccinated with adequate tetanus toxoid in Ethiopia (3). Despite growing recognition of the detrimental effects of conflict on maternal and child healthcare, the literature is bereft of studies robustly quantifying the association between conflict and TT protective dose uptake of pregnant women during ANC service in Ethiopia, particularly in the Amhara region (8, 9). The continued civil war in Ethiopia, specifically in the Amhara region, has led to extensive damage to healthcare facilities, disrupting maternal health services for more than 70,000 pregnant women, causing 1.4 million displacements and 600,000 reported deaths (11, 22).
The conflict affected the delivery service of TT vaccination services due to security concerns, disrupting resource allocations, and facility destruction. This study estimated the level of TT vaccine uptake and maternal associated factors during the escalated war in St. Lalibela Hospital.
At the end of the study period, 67.3% (95% CI 62.3–72.0) of pregnant women received a protective dose of the TT vaccine. This report is in line with the previous study findings in Gondar Hospital (69.8%) (10), Debre Birhan Town (72.3%) (28), Damboya, SNNR (72.5%) (18), in Sudan (73.7%) (1), and North India (68%) (29). However, this finding is higher than previously reported in Debre Tabor (56.2%) (30), Tigray (40.2%) (20), Oromia (39.2%) (14) and Somali (51.8%) (6), and EDHS (42.4%) (9). The observed discrepancy in TT vaccine coverage rates between this study may be attributed to time variations and differences in maternal knowledge.
On the other hand, the final report of this study is lower than previously reported in the Lao People's Democratic Republic (79.7%) (31) and in Nigeria (81.1%) (32). The variation in TT vaccine coverage rates could be attributed to cultural differences, health-seeking behavior, healthcare coverage, economic and infrastructural access, and the impact of war. In our study, out of 296 pregnant women who initiated ANC before the war outbreak, 239 (67.1%) received a protective dose of the TT vaccine, while only 23 (6.4%) completed the full TT vaccination. In addition, 270 (76.3%) pregnant women were temporarily displaced from their residences during the war (16).
On the other hand, there was a significant TT dropout recorded at each TT uptake interval; this revealed the overall dropout rates from TT5 to TT2 (TT5–TT2), from TT5 to TT3 (TT5–TT3), and from TT5 to TT4 (TT5–TT4) were 17.6%, 11.9%, and 6.1%, respectively, with significant variation among each consecutive interval of TT vaccine uptake for pregnant women. This is consistent with the findings in previous studies conducted among pregnant women with TT vaccine uptake in Sudan (21) and Sierra Leone (33). The possible elucidation for this significant difference between each consecutive interval of TT vaccine uptake was related to the continued armed conflict in both Ethiopia and Sudan, which led to larger coverage of TT for pregnant women.
Maternal factors associated with achieving a protective dose of the TT vaccine during pregnancy were identified; accordingly, pregnant women aged 15–25 years had a three times higher likelihood of receiving the protective dose compared to those aged 36–49 years. This is consistent with previous findings in the southern region (SNNR) (8) and in Sudan (1). The possible reasons for the increased likelihood of younger pregnant women, particularly those aged 15–25 years, to be more likely to receive the TT vaccine during ANC is due to their curiosity, attentiveness, and proactive approach toward their pregnancy and them actively seeking out the vaccine as they believe it offers crucial protection during pregnancy.
In this study, pregnant women who completed high school have a 3.05 times higher likelihood of receiving the protective dose compared to illiterate pregnant women. This report is consistent with previous findings in Ethiopia (13), Tigray, Ethiopia (20), Debre Tabor town (30), and a Somali region (6). When increased level of education the more likely hood of aware women about to importantly of TT vaccine protective doses for infant and increased the likelihood of intention to took it during pregnancy.
The findings of the study revealed that mothers who attended their fourth ANC visits were 9.4 times more likely to receive two doses of TT injection than mothers who attended fewer than two ANC visits. This is consistent with the findings of previous studies in southern Ethiopia (8), Amhara region, and Tigray region (14, 20). This might be due to the pregnant mothers having regular ANC visits, the likelihood of receiving comprehensive healthcare services and completing the recommended TT vaccine doses, and increased contact time with healthcare professionals who provide mothers with valuable health information, which can positively influence their healthcare-seeking behavior.
There was a significant association between pregnant women and previous media exposure. This study found that mothers who were exposed to media about the importance of the TT vaccine were more likely to receive the protective dose (AOR = 15.5; 95% CI 7.5–25.3; p = 0.001). This is consistent with a systematic review conducted in Ethiopia (13) and in previous national-level studies (3, 9). This might be because media exposure increases awareness, knowledge, and accurate information about the benefits of TT vaccination during pregnancy. It helps address misconceptions and cultural beliefs, improves access to healthcare services, and builds trust between healthcare providers and pregnant women.
Consistent with previous findings in Egypt (34), Gondar (2), a Somali region (35), and Sierra Leone (33), pregnant women with a good knowledge of protective TT vaccination doses have a 2.7 times higher likelihood of increased uptake of protective doses compared with the pregnant group of pregnant women (AOR = 2.7; 95% CI 1.8–4.9; p = 0.02). This might be the pregnant mothers had regular ANC visits, the probability of getting comprehensive and completed the recommended healthcare service including, the probability of getting full TT vaccine protective doses had increased. Healthcare providers, public health campaigns, and educational initiatives play a crucial role in disseminating accurate information about the vaccine's benefits and safety.
Unlike the findings in previous studies (1, 8, 9, 21), in this study, family income, displacement during war, and the number of families did not significantly affect the uptake of protective TT vaccine doses for pregnant women. However, the pregnant women's knowledge of the tetanus vaccine and their level of education significantly impacted the uptake of the vaccine, highlighting the importance of addressing these factors to improve immunization rates, reduce hesitancy, and promote a culture that values vaccination.
The present study has some limitations. The cross-sectional survey design makes it difficult to establish clear causal relationships between the factors described and uptake of the TT vaccine. Recall bias may have influenced the study's results, as participants did not present their vaccination cards during data collection. Nevertheless, the study offers valuable insights to inform the development of health education interventions targeting increased uptake of the TT vaccine among pregnant women in Ethiopia.
The utilization of the protective TT vaccine dose among mothers in the study area was low. Factors that enhanced the protective TT dose included level of education, ANC visits, age of respondent, fourth ANC follow-up, media exposure, and good knowledge about TT. Low utilization of the protective TT vaccine dose among pregnant in the study area can be addressed by focusing on raising awareness about regular ANC visits, establishing mobile clinics or outreach programs for healthcare access, enhancing security through collaboration, conducting community-based education campaigns involving community and religious leaders, providing training on safe vaccine administration, fostering coordination among healthcare providers and organizations, supporting healthcare facilities, and recognizing the psychological impact of conflict and offering mental health support services.
The original contributions presented in the study will be made available upon reasonable request. Further inquiries can be directed to the corresponding author.
The study adhered to the Declaration of Helsinki and relevant guidelines. Ethical approval was obtained from the institutional review board of Woldia University (Approval Ref. No. 757/2022) on February 25, 2022. The studies followed local legislation and institutional requirements, with written informed consent obtained from participants' guardians/next of kin.
FKB: Resources, Software, Visualization, Writing – original draft. SMM: Resources, Software, Supervision, Validation, Visualization, Writing – review & editing.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors would like to thank St. Lalibela General Hospital data collectors and staff.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Mohamed SOO, Ahmed EM. Prevalence and determinants of antenatal tetanus vaccination in Sudan: a cross-sectional analysis of the multiple indicator cluster survey. Trop Med Health. (2022) 50(1):7. doi: 10.1186/s41182-022-00398-4
2. Mihret MS, Limenih MA, Gudayu TW. The role of timely initiation of antenatal care on protective dose tetanus toxoid immunization: the case of northern Ethiopia postnatal mother. BMC Pregnancy Childbirth. (2018) 18:235. doi: 10.1186/s12884-018-1878-y
3. Liyew AM, Ayalew HG. Individual and community-level determinants of poor tetanus toxoid immunization among pregnant women in Ethiopia using data from 2016 Ethiopian demographic and health survey; multilevel analysis. Arch Public Health. (2021) 79(1):1–10. doi: 10.1186/s13690-021-00622-3
4. Mugagga N, Bagaya BS, Nantongo M, Muwanda F, Mukunya D, Musaba MW, et al. Antitetanus toxoid antibodies in mothers and neonates: a single-center study from Uganda. BMJ Paediatrics Open. (2023) 7:e001334. doi: 10.1136/bmjpo-2021-001334
5. Messeret ES, Masresha B, Yakubu A, Daniel F, Mihigo R, Nshimirimana D, et al. Maternal and neonatal tetanus elimination (MNTE) in the WHO African region. J Immunol Sci. (2018) 15:103. doi: 10.29245/2578-3009/2018/si.1115
6. Gebremedhin TS, Welay FT, Mengesha MB, Assefa NE, Werid WM. Tetanus toxoid vaccination uptake and associated factors among mothers who gave birth in the last 12 months in Errer district, Somali regional state, eastern Ethiopia. BioMed Res Int. (2020) 2020:4023031. doi: 10.1155/2020/4023031
7. Abu-Raya B, Maertens K, Edwards KM, Omer SB, Englund JA, Flanagan KL, et al. Global perspectives on immunization during pregnancy and priorities for future research and development: an international consensus statement. Front Immunol. (2020) 11:1282. doi: 10.3389/fimmu.2020.01282
8. Dubale Mamoro M, Kelbiso Hanfore L. Tetanus toxoid immunization status and associated factors among mothers in Damboya woreda, Kembata Tembaro zone, SNNP, Ethiopia. J Nutr Metab. (2018) 2018:2839579. doi: 10.1155/2018/2839579
9. Fentie B, Alemu TG, Techane MA, Wubneh CA, Assimamaw NT, Belay GM, et al. Spatial distribution and determinants of tetanus toxoid immunization among pregnant women in Ethiopia using data from Ethiopian demographic and health survey 2016. BMC Pregnancy Childb. (2023) 23(1):745. doi: 10.1186/s12884-023-05911-z
10. Gessesse DN, Yismaw AE, Yismaw YE, Workneh TW. Coverage and determinants of protective dose tetanus toxoid vaccine among postnatal women delivered at university of Gondar Comprehensive Specialized Hospital, northwest Ethiopia, 2019. Clin Epidemiol Glob Health. (2021) 12:100814. doi: 10.1016/j.cegh.2021.100814
11. Mezen MK, Lemlem GA, Biru YB, Yimer AM. Association of war with vaccination dropout among children younger than 2 years in the North Wollo Zone, Ethiopia. JAMA Network Open. (2023) 6(2):e2255098. doi: 10.1001/jamanetworkopen.2022.55098
12. Mirzazada S, Padhani ZA, Jabeen S, Fatima M, Rizvi A, Ansari U, et al. Impact of conflict on maternal and child health service delivery: a country case study of Afghanistan. Confl Health. (2020) 14:38. doi: 10.1186/s13031-020-00285-x
13. Nigussie J, Girma B, Molla A, Mareg M. Tetanus toxoid vaccination coverage and associated factors among childbearing women in Ethiopia: a systematic review and meta-analysis. BioMed Res Int. (2021) 2021:5529315. doi: 10.1155/2021/5529315
14. Anatea MD, Mekonnen TH, Dachew BA. Determinants and perceptions of the utilization of tetanus toxoid immunization among reproductive-age women in Dukem Town, Eastern Ethiopia: a community-based cross-sectional study. BMC Int Health Hum Rights. (2018) 18(1):1–10. doi: 10.1186/s12914-018-0168-0
15. Brook I. Current concepts in the management of Clostridium tetani infection. Expert Rev Anti Infect Ther. (2008) 6(3):327–36. doi: 10.1586/14787210.6.3.327
16. Gashaw A, Hunie M, Amare E, Zewdie A, Abebe M, Demeke M, et al. Proportion of births protected against neonatal tetanus and its associated factors among mothers who gave birth within the past 6 months in Gozamn district, Northwest Ethiopia, 2022. Hum Vaccin Immunother. (2023) 19(2):2223066. doi: 10.1080/21645515.2023.2223066
17. Karnad DR, Gupta V. Intensive care management of severe tetanus. Indian J Crit Care Med. (2021) 25(Suppl 2):S155–60. doi: 10.5005/jp-journals-10071-23829
18. Dubale Mamoro M, Kelbiso Hanfore L. Tetanus toxoid immunization status and associated factors among mothers in Damboya woreda, Kembata Tembaro zone, SNNP, Ethiopia. J Nutr Metab. (2018) 2018:2839579. doi: 10.1155/2018/2839579
19. Kidane T. Factors influencing TT immunization coverage and protection at birth coverage in Tselemti district, Ethiopia. Ethiop J Health Dev. (2004) 18(3):153–8. Available online at: https://www.ejhd.org/index.php/ejhd/article/view/742/559
20. Mengesha MB, Weldegeorges DA, Assefa NE, Gebremeskel SG, Hidru HD, Teame H, et al. Tetanus toxoid immunization status and associated factors among mothers in Hawzen, eastern zone of Tigray, Ethiopia, 2019. Open Public Health J. (2020) 13(1):281–8. doi: 10.2174/1874944502013010281
21. Ibrahim ZA, Sabahelzain MM, Elhadi YAM, Malande OO, Babiker S. Predictors of tetanus vaccine uptake among pregnant women in Khartoum state, Sudan: a hospital-based cross-sectional study. Vaccines (Basel). (2023) 11(7):1268. doi: 10.3390/vaccines11071268
22. Jamal M, Kebede F. Exploring multi-level risk factors and post-war burdens of trachomatous trichiasis among displaced population in Raya Kobo districts, implication for urgent action. Int J Ophthalmol. (2023) 16(8):1299–308. doi: 10.18240/ijo.2023.08.17
23. Njuguna HN, Yusuf N, Raza AA, Ahmed B, Tohme RA. Progress toward maternal and neonatal tetanus elimination—worldwide, 2000–2018. Morb Mortal Wkly Rep. (2020) 69(17):515. doi: 10.15585/mmwr.mm6917a2
24. Martins MJ. Sacroiliac dysfunction-diagnosis and treatment approaches: a clinical study. Universidade de Évora (2022).
25. USAID. Guide to DHS Statistics DHS-7 (version 2), the Demographic and Health Surveys Program (2020). Available online at: https://www.dhsprogram.com/pubs/pdf/DHSG1/Guide_to_DHS_Statistics_DHS-7_v2.pdf (Accessed May 7, 2020).
26. Chi PC, Bulage P, Urdal H, Sundby J. Perceptions of the effects of armed conflict on maternal and reproductive health services and outcomes in Burundi and Northern Uganda: a qualitative study. BMC Int Health Hum Rights. (2015) 15:7. doi: 10.1186/s12914-015-0045-z
27. Fenta SM, Fenta HM. Magnitude of tetanus toxoid immunization and associated factors among pregnant women in Ethiopia. Open Public Health J. (2023) 16(1):e187494452301091. doi: 10.2174/18749445-v16-e230111-2022-161
28. Belihu KD, Tesso FY, Woldetsadik TD. Dropout rate of tetanus toxoid immunization and associated factors among reproductive age group of women in Debrebirhan town, Amhara region, Northern Ethiopia. J Women's Health Care. (2017) 6(4):4–11. doi: 10.4172/2167-0420.1000390
29. Lodha N. Utilisation of antenatal care services and its determinants among pregnant women attending tertiary care hospital in Western India: a cross-sectional study. J Clin Diagn Res. (2022) 16(8):LC22–6. doi: 10.7860/JCDR/2022/58290.16755
30. Mihret MS, Limenih MA, Gudayu TW. The role of timely initiation of antenatal care on protective dose tetanus toxoid immunization: the case of northern Ethiopia post natal mothers. BMC Pregnancy Childbirth. (2018) 18(1):1–10. doi: 10.1186/s12884-018-1878-y
31. Fuchs FE, Pauly M, Black AP, Hübschen JM. Seroprevalence of ToRCH pathogens in Southeast Asia. Microorganisms. (2021) 9(3):574. doi: 10.3390/microorganisms9030574
32. Orimadegun AE, Orimadegun BE, Bamgboye EA. Non-protective immunity against tetanus in primiparous women and newborns at birth in rural and urban settings in Ibadan, Nigeria. Pan Afr Med J. (2017) 27(Suppl 3):26. doi: 10.11604/pamj.supp.2017.27.3.11869
33. Yaya S, Kota K, Buh A, Bishwajit G. Prevalence and predictors of taking tetanus toxoid vaccine in pregnancy: a cross-sectional study of 8,722 women in Sierra Leone. BMC Public Health. (2020) 20(1):855. doi: 10.1186/s12889-020-08985-y
34. Mehanna A, Ali MH, Kharboush I. Knowledge and health beliefs of reproductive-age women in Alexandria about tetanus toxoid immunization. J Egypt Public Health Assoc. (2020) 95(1):22. doi: 10.1186/s42506-020-00049-8
Keywords: armed conflict, Ethiopia, protective dose, pregnancy, tetanus toxoid vaccine
Citation: Kebede Bizuneh F and Muhidin Mustofa S (2024) Uptake of protective tetanus toxoid vaccine doses and maternal associated factors during pregnancy in armed conflict zone, hospital-based cross-sectional study. Front. Reprod. Health 6: 1353699. doi: 10.3389/frph.2024.1353699
Received: 11 December 2023; Accepted: 5 April 2024;
Published: 19 July 2024.
Edited by:
Emmanuel Senanu Morhe, University of Health and Allied Sciences, GhanaReviewed by:
Emmanuel Ekanem, University of Calabar, Nigeria© 2024 Kebede Bizuneh and Muhidin Mustofa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fassikaw Kebede Bizuneh, ZmFzc2lrYXcxMjNAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.