- Department of Community Health Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Introduction: One of the most important public health concerns is still the Human Immunodeficiency Virus (HIV) and acquired immunodeficiency syndrome (AIDS), particularly in developing countries. Although HIV testing is an important step in both prevention and treatment, its uptake remains low, and no study has looked into the scale of HIV counseling, testing, and test result receipt among East African women all at the same time. Therefore, this study aimed to investigate HIV counseling, testing, and test result receipt, as well as the factors that influence them, among East African women.
Methods: This analysis used Demographic and Health Survey data collected from 10 East African countries between 2011 and 2022. We examined the coverage of HIV counseling, testing, and test result receipt among East African women, as well as other characteristics. To select candidate factors and identify significant explanatory variables related to the outcome variable, binary and multiple logistic regression analyses were conducted, and the results were presented using adjusted odds ratios (AORs) with 95% confidence intervals. In the binary and multiple logistic regression analyses, P values of less than or equal to 0.2 and <0.05 were used to assess significant variables, respectively.
Results: A total of 41,627 weighted women included to this study. HIV counseling, testing, and test result receipt among East African women were found to be 77.86% (95% CI = 77.46, 78.26). Being 25–34 years old (AOR = 1.13, 95% CI, 1.06, 1.21), 35–49 years old (AOR = 1.15, 95% CI, 1.05, 1.26) as compared to 15–24 years old women, primary education (AOR = 1.75, 95% CI, 1.64, 1.86), secondary/higher education level (AOR = 1.96, 95% CI, 1.82, 2.13) as compared to not educated women, poor, (AOR = 1.22, 95% CI, 1.14, 1.29), middle wealth (AOR = 1.12, 95% CI, 1.04, 1.21) as compared to rich wealth index, mass media exposure (AOR = 1.29, 95% CI, 1.22, 1.35), 3–5 parity (AOR = 1.29, 95% CI, 1.21, 1.37), more than 5 parity (AOR = 1.46, 95% CI, 1.33, 1.61) as compared to <3 parity, health institution delivery (AOR = 1.65, 95% CI, 1.53, 1.76), were associated positively with the outcome variable respectively. However, being married (AOR = 0.79, 95% CI, 0.72, 0.87), not using contraceptive (AOR = 0.58, 95% CI, 0.51, 0.61), and traditional contraceptive method user (AOR = 0.47, 95% CI, 0.41, 0.54) as compared to modern users were associated negatively with outcome variable respectively.
Conclusion: This study found that HIV counseling, testing, and test result receipt are still unsatisfactory. Strengthening maternal health services such as institutional delivery, family planning, and women's empowerment, as well as changing mass media and taking advantage of these opportunities, will boost the region's coverage of HIV counseling, testing, and obtaining results.
Introduction
HIV/AIDS is a major global public health concern, with Sub-Saharan Africa having the highest prevalence of infection (1, 2). According to the USAIDS, 2023 estimate, around 39 million individuals were newly infected with HIV in 2022 and lived with the virus (3). Similarly, AIDS-related illnesses claimed the lives of almost 630,000 people this year (3). Of them, two thirds originated in Africa, the continent where most deaths occur (4). However, just 36.9 million persons globally were HIV positive in 2017, with Eastern and Southern Africa making over half of that number (19.6 million) (2, 5). Reports state that while new infections in children decreased by 52% from 310,000 in 2010 to 150,000 in 2019, new infections worldwide decreased by about 40% from 2.9 million in 1997 to 1.7 million in 2019. However, Sub-Saharan Africa (SSA) accounted for over 61% of new infections among children, most likely as a result of mother-to-child HIV transmission (MTCT) (6, 7). The aforementioned various year reports demonstrate that the fight against HIV/AIDS is still ongoing worldwide, particularly in developing nations.
In many countries, it is now national policy for all pregnant women to get provider-initiated testing and counseling during antenatal care (ANC). This is known as “opt-out” HIV testing. In “opt-out” testing, HIV testing, like hemoglobin tests, is included in the standard ANC care package for all pregnant women. All ANC patients are offered the test and counseled on the advantages and disadvantages of knowing their HIV status during pregnancy. However, testing is still voluntary, and women have the option to decline if they so desire. Women are more likely to accept HIV testing if their health care physician counsels and encourages the practice (5, 8). Because of the effects of HIV/AIDS, the United Nations 2020 Global AIDS Update announced significant progress in the fight against the HIV epidemic (6–8). Since the UNAIDS 90-90-90 effort, which aims to provide HIV testing and treatment to the great majority of HIV-infected persons by the end of 2020, more than 80% of people living with HIV were aware of their status, and approximately 67% were receiving antiretroviral therapy (9).
Eastern Africa is the world's second-most HIV/AIDS-affected region, behind Southern Africa. Over the past 20 years, the region's overall frequency has decreased—Kenya saw a reduction in prevalence from 14% to 5% but new worries about infection among the most vulnerable individuals are starting to emerge (10). A number of studies have determined that the following variables are responsible for the higher rate of HIV transmission: types of residencies; exposure to mass media; exposure to HIV/AIDS education; having taken an HIV test; lack of awareness of HIV; poor knowledge; education level; wealth index; inability to access ART prophylaxis; poor adherence to ART; absence of clinic-based HIV education and counseling (11–16).
Additionally, gender raises the risk of HIV infection. In 2015, 25% of new HIV infections among adults were among young women, but in SSA, 56% of new infections were among women (17). The WHO and the United Nations Program on HIV/AIDS released guidelines for provider-initiated HIV testing and counseling in 2007 in response to the low testing rates (18). In order to facilitate enhanced availability of HIV prevention, treatment, and care, the World Health Organization (WHO) recommended in 2015 that quick diagnostic HIV testing be carried out by trained lay practitioners (19). The risk variables associated with HIV testing have not been thoroughly studied, and there exist regional and gender-specific variations.
Although community-owned interventions are critical for increasing HIV testing and counseling for women, the country's little research in this area focuses solely on individual drivers, leaving the combination effect of counseling, testing, and receiving the results. Previous research focused on either on counseling, testing, or just getting the results. Therefore, utilizing recent demographic and health surveys conducted in East Africa, the goal of this study was to assess the prevalence, and factors related to HIV counseling, testing, and obtaining the results among women in reproductive age in that region.
Methods
Study setting, and period
The data used in this study comes from the most recent standard Demographic and Health Survey (DHS) dataset for East African states. The dataset covers 10 years from 2012 to 2022 and includes data from ten East African countries: Burundi, Ethiopia, Kenya, Comoros, Madagascar, Malawi, Mozambique, Rwanda, Tanzania, Uganda, Zambia, and Zimbabwe. The study utilized a standard dataset to acquire a substantial sample size that is representative of the population source and all circumstances (20). On a global basis, DHS collects analogous statistics. The surveys feature large sample sizes, are population-based, and are nationwide in scope (20). Eastern Africa comprises 14 countries across the Horn of Africa, the Indian Ocean islands, and the Great Lakes region. These countries share similar economic, social, and environmental challenges. Furthermore, they are worried about their ability to achieve the targets set by the Millennium Development Goals (21). East Africa is the region of the African continent located in the horn and east of the Sahara Desert. They are home to 486,766,759 people and cover an area of 6,667,493 Km2 (2,574,332 square miles), accounting for 6.03% of the global population.
Data source and study population
We utilized DHS data from 2012 to 2022, specifically from individual record (IR) files. Out of the 14 eastern countries where DHS surveys were conducted during this period, only approximately 10 were included in our study due to the absence of information concerning the outcome variable in the remaining surveys. After incorporating the data from each country, we had a total weighted sample of 41,627 pregnant women and an unweighted sample of 41,881 reproductive-age pregnant women who had undergone HIV counseling and testing and received their results. These samples were used for the final analysis (Table 1).
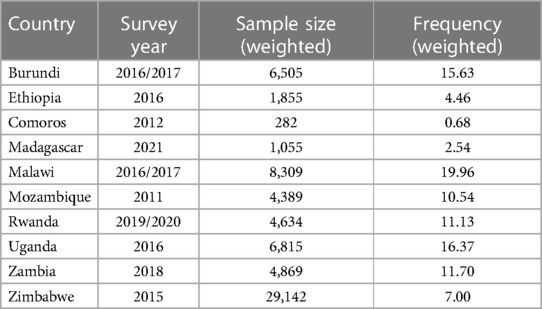
Table 1. Countries, sample size, and survey year of demographic and health surveys included in the analysis for 10 East African countries.
Sample size determination and sampling method
Recent Demographic and Health Survey (DHS) reports were available for approximately 12 out of the 13 nations in East Africa. Each of the surveys conducted in the listed nations used the most up-to-date conventional census framework. In the DHS samples, the areas are usually divided into urban and rural regions within each administrative geographic area. During the first round of sampling, enumeration areas (EAs) were selected based on their size within each stratum using a probability-proportional approach. In the second step of sampling, a systematic sampling method was used to select a specific number of homes in the designated EAs. After the household listing, systematic sampling with equal probability was employed to choose a certain number of households from within the defined cluster (20).
Data management and statistical analysis
We used STATA version 17 to extract, clean, and recode the variables in our study. To account for the differential probability of selection in the DHS data sampling procedure, we weighted the data using sample weights during any statistical analysis. This ensured that the survey results were representative. For the bivariable analysis, we considered variables with a p-value of 0.2 for the multivariable analysis. In the multivariable logistic model, we provided the Adjusted Odds Ratio (AOR) with a 95% confidence interval to determine the associated factors of HIV counseling, testing, and obtaining findings. For categorical data, descriptive studies such as frequency count and proportion were utilized to summarize the descriptive data. Bivariable logistic regression was used to determine candidate variables for multiple logistic regression. A logistic model was fitted using the variance inflation factor to investigate multicollinearity among the independent variables. To assess the overall fitness of the final regression model, the Hosmer and Lemeshow tests were used. The statistical significance of the final model was set at p 0.05. We tested it for the assumption of multilevel model analysis using the intra-class correlation (ICC) coefficient because the data could be hierarchical, but it was 3%, which did not meet the minimal threshold to perform it. As a result, it was determined that traditional logistic regression was preferred.
Variables of the study
The outcome variable
The outcome variable of this study was the number of pregnant women who received counseling on HIV, tested for an HIV test during antenatal care, and received the results of the test. The outcome variable was then recategorized as Yes = “1” if the women were counseled on HIV, tested for HIV, and received the test results accordingly, and No = “0” if the women did not receive either of them. This classification and analysis were made according to the guide in the DHS statistics book (20).
The independent variables
Independent variables: Various maternal-related factors were included. These included maternal age, educational status, types of places of residence, marital status, household wealth index, current employment status, mass media exposure, place of delivery, number of health visits, total children born, under-five children, contraceptive utilization, distance to the health facility, knowledge of HIV/AIDS, sex of the household head, and breastfeeding status.
Results
Sociodemographic characteristics of the study participant
In this study, a total of 41,627 pregnant women of reproductive age were included in East African countries. About 18,761 (45.07%) of the study women were between 25 and 34 years of reproductive age. Regarding marital status, more than half of the women (27,177, or 65.29%) were married. Concerning place of residence types, 32,156 (77.25%) had rural areas as their place of residence, educational status 22,140 (53.18%) had primary education, wealth index 8,752 (21.03%) belonged to the poorest households, and breastfeeding status, 28,374 (68.17%) of mothers were currently breastfeeding. Furthermore, about 36,958 (88.78%), 22,200 (53.33%), and 26,343 (63.28%) women who have given birth at health institutions did not have mass media exposure (either listening to the radio, watching television, or reading magazines or newspapers) and are currently employed, respectively. However, slightly more than half of the 21,694 (52.12%) and the majority of the 24,994 (60.05%) mothers did not utilize any method of contraception, and they reported that the distance to the health facility is a major problem in accessing it. About 16,185 (38.88%) of women have given birth to approximately 3–5 children; of these, 35,065 (84.23%) of mothers have under-five children. However, 39,511 (94.92%) of mothers did not have comprehensive knowledge of HIV/AIDS, and almost 32,345 (77.70%) of mothers visited health facilities once a year. Similarly, about 16,629 (39.95%) of females have reported that the distance from the health facility was a major problem in accessing services (Table 2).
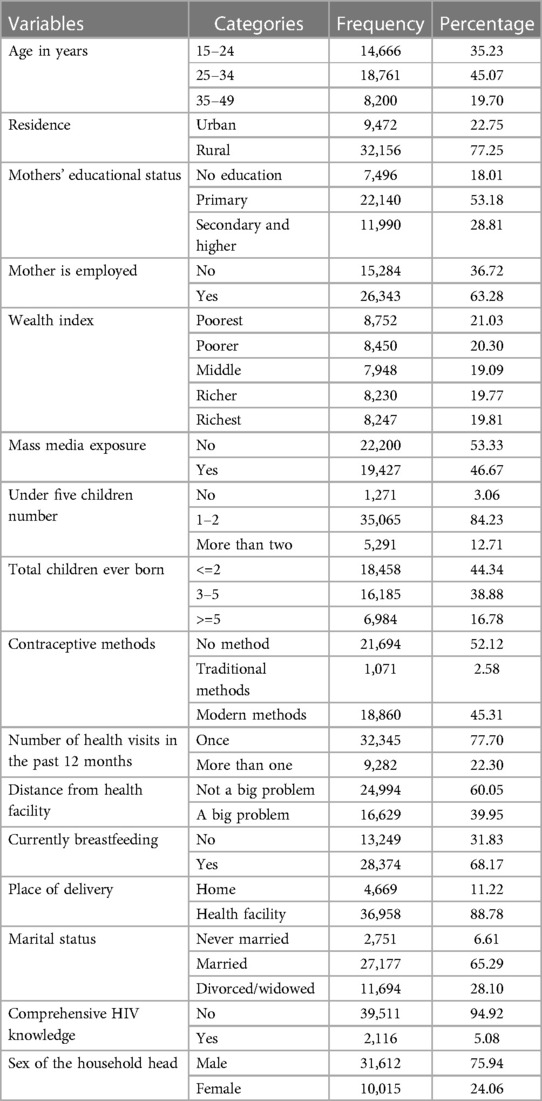
Table 2. Socio-demographic and maternal related characteristics of respondent's HIV counselling testing and received results among reproductive age women in east African countries (weighted n = 41,627): based on east African the recent DHS data.
Factors associated with HIV counseling, testing and receiving the results among reproductive age women in East Africa
The odds of HIV counseling, testing, and receiving the results increased by 13% (AOR = 1.13, 95% CI: 1.06–1.21) and 15% (AOR = 1.15, 95% CI: 1.05–1.26), respectively, among women aged 25–34 years and 35–49 years, compared to women aged 15–24 years. Additionally, compared to uneducated women, those who had completed primary and secondary/higher education showed (AOR = 1.75; 95% CI: 1.64–1.86) and (AOR = 1.96; 95% CI: 1.82–2.13) higher chances of receiving HIV counseling, testing, and results. Similarly, about the household wealth index, mothers from poor and middle households had a higher likelihood of receiving counseling, testing, and results compared to women from wealthy households, with odds of (AOR = 1.22, 95% CI, 1.14–1.29) and (AOR = 1.12, 95% CI, 1.04–1.21) respectively. 29% of mothers with mass media exposure received proper HIV counseling, testing, and results, with odds of (AOR = 1.29, 95% CI = 1.22, 1.35), compared to their counterparts. Mothers with 3–5 children and more than five children had a higher likelihood of receiving counseling, testing, and results, with odds of (AOR = 1.29, 95% CI: 1.21–1.37) and (AOR = 1.46, 95% CI: 1.33–1.61) respectively, compared to mothers with fewer than three children. Married mothers had a 21% lower likelihood of not receiving HIV counseling, testing, and results (AOR = 0.79, 95% CI: 0.72–0.87) compared to never-married women. On the other hand, mothers who gave birth at health institutions had a higher likelihood of receiving HIV counseling, testing, and results compared to those who gave birth at home. Compared to users of modern contraceptive methods, those who used no method and traditional contraceptive methods had a lower tendency to receive HIV counseling, testing, and results, with odds of (AOR = 0.58, 95% CI, 0.51–0.61) and (AOR = 0.47, 95% CI, 0.41–0.54) respectively (Table 3).
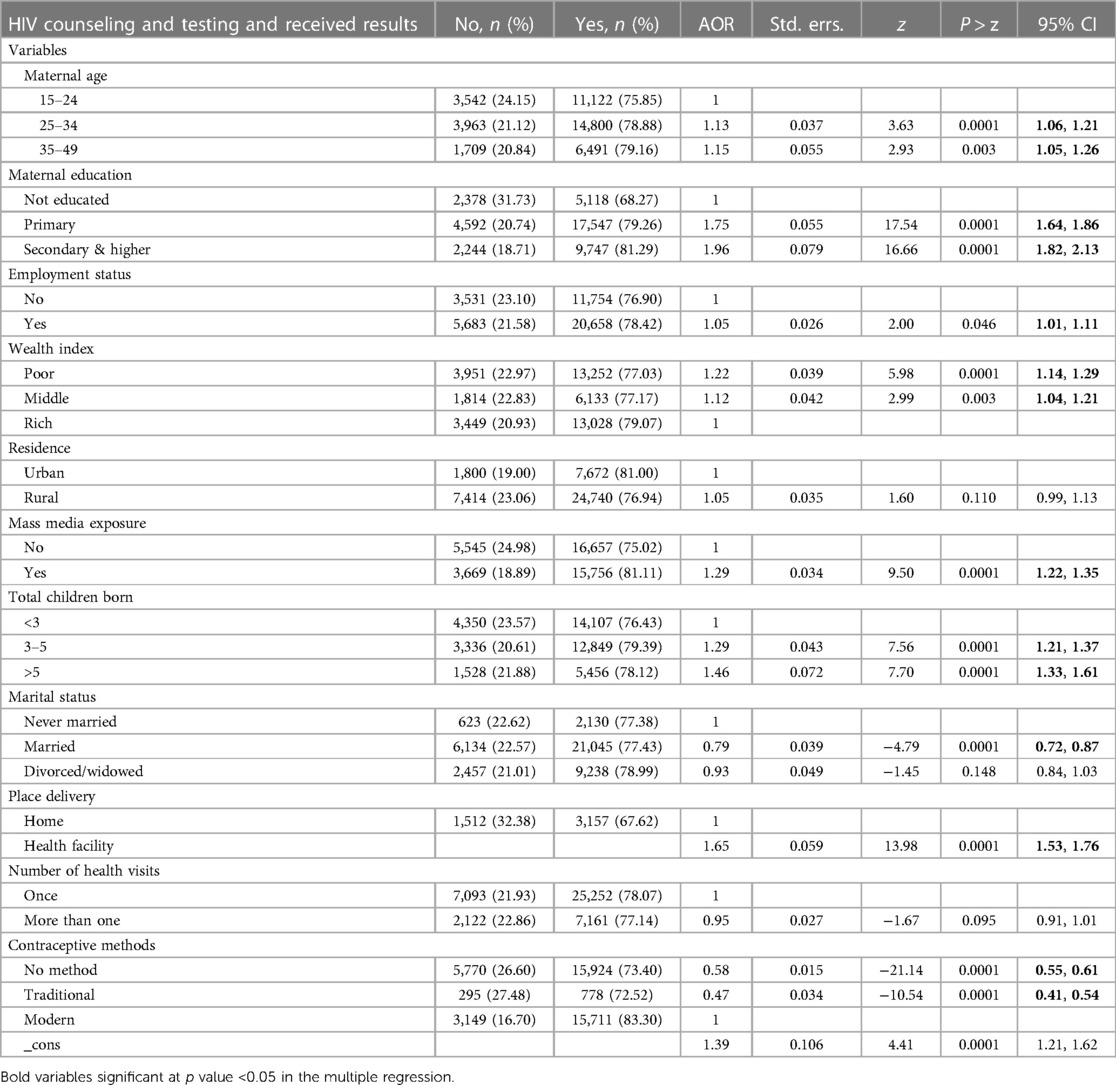
Table 3. Multiple logistic regression analysis results on determinants of HIV counselling testing and received results among reproductive age women in east Africa, based on the recent DHS data (weighted n = 41,627).
Discussion
This study aimed to determine the prevalence and associated factors of HIV counseling, testing, and test result receipt among East African women of reproductive age. The final model included age, educational level, wealth index, media exposure, use of contraception, access to healthcare facilities, marital status, parity, and work status as factors connected to HIV counseling, testing, and receipt results in East Africa. HIV counseling and testing are widely recognized as essential components of all HIV preventive strategies. Testing can identify individuals who are HIV positive and in need of treatment and care, as well as those who are HIV negative and should be referred for HIV prevention and care. Regular HIV testing will be crucial for pre-exposure prophylaxis-based preventive strategies. HIV counseling and testing not only help women, couples, and families learn their HIV status and receive personalized risk reduction counseling and further care based on their status, but they can also help communities overcome the stigma and discrimination associated with HIV/AIDS (22, 23). This study employs a nationally representative cross-sectional sample of women to evaluate the factors that influence HIV counseling, testing, and receiving results among East African women of reproductive age. As a result, the findings of this study suggest that various variables are associated with women of reproductive age.
The odds of HIV counseling, testing, and receiving the results were increased by 13% more among women whose ages are 25–34 years old and 35–49 years old, respectively, as compared to women whose ages are younger. This survey's findings are comparable with those of other research, demonstrating that HIV counseling, testing, and receiving outcomes improve with age (24–27). Previous research on HIV/AIDS awareness and knowledge among women of reproductive age has discovered that as women get older, their chances of being aware of and knowledgeable about HIV/AIDS also increase. This, in turn, may result in a higher likelihood of them seeking HIV counseling and testing and receiving their test results as outlined in the protocol (28). This is most likely due to the older age group's lower fear of stigma and prejudice from society about HIV counseling and testing uptake compared to the younger age group (29).
Furthermore, when comparing educated women to those without formal education, it was determined that those who had completed primary and secondary/higher education had a 1.75% and 1.96% higher likelihood of receiving HIV counseling, testing, and obtaining the results. This discovery supports previous research that suggests women with higher levels of education are more likely to achieve positive outcomes (1, 25, 26, 30, 31). This result highlights the importance of education and higher wealth in promoting HIV testing and counseling. This may be because educated women and women from wealthier households tend to have greater HIV awareness and knowledge (28). Formal education also encourages healthcare-seeking behavior, which can contribute to a higher quality of life (32, 33).
Similarly, regarding household wealth index, mothers who came from poor and middle households have shown a higher likelihood of being counseled and tested and receiving the results as compared to women who came from rich households. This finding agrees with several studies done elsewhere (24–26, 34). Due to significant distances from health facilities and challenging transportation networks in Africa, impoverished households' mothers may find it more difficult to get HIV counseling, testing, and receiving findings than wealthier and more educated women (35). Also, women with greater incomes and educational levels are more likely to seek maternal health care services, have women's autonomy, and are closer to information (36, 37).
Mothers who have been exposed to mass media have a higher rate of properly receiving HIV counseling and testing results (29%) compared to those who have not been exposed. Mass media is an effective and affordable tool for disseminating health information and promoting health activities to a wide audience (38). Previous research has demonstrated that the media can positively influence HIV testing rates (39–41), as well as other critical public health issues (42). Turk and colleagues' 2017 impact data analysis found that the media can positively influence HIV test rates as well as unhelpful/stigmatizing attitudes and behaviors (38).
Mothers who have given from 3 to 5 and more than five children have revealed a higher likelihood of being counseled, tested, and receiving the result accordingly as compared to mothers who have less than three children, respectively. Consistent with earlier studies in SS (43). The number of children a woman had was shown to be related to HIV testing, with women who had more children having a higher likelihood of testing for HIV than those who did not have children. This finding can be linked to women's access to healthcare during pregnancy, delivery, and postpartum (43–45).
Married mothers have shown a 21% lower likelihood of not having HIV counseling, testing, or receiving the results when compared to never-married women. Previous research found that divorced and separated people were more likely to be tested for HIV than married people (45–47). Divorced and separated people were more than four times more likely than married people to die from HIV/AIDS. Single or never-married people were 13 times more likely than married people to die from HIV/AIDS (48, 49). Because of their larger sexual network, single/never married and divorced/separated people are at a higher risk of contracting HIV/AIDS and dying from with (50). Marriage appears to impose a sort of social control (49, 51), which helps to limit a spouse's number of sexual partners. Individuals at high risk (single and divorced) should be targeted with behavior change communications to encourage them to seek HIV testing, which is the cornerstone of HIV prevention (52).
On the other hand, when it comes to the place of delivery, mothers who have given birth at healthcare institutions have shown a higher likelihood of receiving HIV counseling, being tested, and obtaining results compared to mothers who gave birth at home. In comparison to users of modern contraceptive methods, those who do not use any method or opt for traditional contraceptive methods have shown a lower inclination towards HIV counseling, testing, and receiving the results accordingly. This is because mothers who have utilized maternal reproductive health services such as delivering at a healthcare facility and using modern contraception are more likely to receive information from healthcare professionals about HIV/AIDS, STIs, and available health treatments. As a result of these and other factors, they may enhance their health-seeking behavior, attitudes, and prevention methods (43, 53, 54).
Strength and limitation of the study
The utilization of nationally representative surveys from different East African nations to evaluate HIV counseling, testing, and getting results coverage and its related factors is a fundamental strength of this study. As a result, we believe our findings are applicable to other SSA nations. Another significant strength of this study is the integration of all three (HIV counseling, testing, and obtaining results). The study data was gathered using conventional and verified data gathering procedures and could be affected by the number of countries. Nonetheless, the following limitations apply to the study. So, first of all, a cause-and-effect relationship cannot be proved due to the cross-sectional nature of the study. Second, the DHS may be biased by memory because it depends on self-reported statistics. Issues including accessibility to treatment, factors pertaining to health professionals, other cultural, biological or clinical related variables, and support programs were not included in the analysis. Finally, we had to rely on surveys conducted at different locations within the chosen countries due to data constraints and availability.
Conclusion
This study found that HIV counseling, testing, and test result receipt among East African women was low. The study also indicated that the status of HIV counseling, testing, and test result receipt was determined by several factors. Generally, more than three-fourths of women of reproductive age had been counseled, tested, and had their HIV examination. After controlling for confounders, determinants such as age, educational attainment, wealth index, mass media exposure, contraceptive utilization, health facility delivery, marital status, parity, and employment status were associated with HIV counseling, testing, and receiving results in East Africa. As a result, in order to reduce the spread of HIV/AIDS, efforts must be made to address the obstacles that impede HIV counseling, testing, and obtaining results among women. Any stakeholder involved in HIV/AIDS prevention and control in any country should take into account factors such as educational levels and wealth status. These factors significantly influence the uptake of HIV counseling, testing, and obtaining results in East Africa. To improve the utilization of maternal health services, it is crucial to support economically marginalized women and enhance HIV/AIDS education in working and educational environments. Additionally, strengthening maternal health services, including institutional delivery, family planning, and women's empowerment, will be beneficial. This can be achieved by changing mass media and making use of the opportunities available to increase the coverage of HIV counseling, testing, and obtaining results in the region. Ultimately, these efforts will help improve women's health and reduce the incidence of HIV/AIDS in East Africa.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was conducted after obtaining a permission letter from www.dhsprogram.com, on an online request to access east African DHS data after reviewing the submitted brief descriptions of the survey to the DHS program. The datasets were treated with the utmost confidence. This study was done based on secondary data from east Africa DHS. Issues related to informed consent, confidentiality, anonymity, and privacy of the study participants are already done ethically by the DHS office.
Author contributions
BT: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author declares that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
I would like to acknowledge the DHS program for providing permission for this study following research ethics.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Qiao S, Zhang Y, Li X, Menon JA. Facilitators and barriers for HIV-testing in Zambia: a systematic review of multi-level factors. PLoS One. (2018) 13(2):e0192327. doi: 10.1371/journal.pone.0192327
2. Gelaw YA, Magalhães RJS, Assefa Y, Williams G. Spatial clustering and socio-demographic determinants of HIV infection in Ethiopia, 2015–2017. Int J Infect Dis. (2019) 82:33–9. doi: 10.1016/j.ijid.2019.02.046
3. USAIDS. The path that ends AIDS 2023 USAIDS global AIDS update. (2023). Available online at: https://www.unaids.org/en (accessed February 01, 2024).
4. World Health Organization. Key facts on HIV and AIDS. (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/hiv-aids (accessed February 01, 2024).
5. World Health Organization. Counselling for Maternal and Newborn Health Care: a Handbook for Building Skills. Geneva: World Health Organization (2010).
6. Ending AIDS. Progress Towards the 90-90-90 targets–global AIDS update. Geneva: Joint United Nations Programme on HIV/AIDS (2017).
7. Alfvén T, Erkkola T, Ghys P, Padayachy J, Warner-Smith M, Rugg D, et al. Global AIDS reporting-2001 to 2015: lessons for monitoring the sustainable development goals. AIDS Behav. (2017) 21:5–14. doi: 10.1007/s10461-016-1662-9
8. World Health Organization. Consolidated Guidelines on HIV Prevention, Testing, Treatment, Service Delivery and Monitoring: Recommendations for a Public Health Approach. Geneva: World Health Organization (2021).
9. Abuogi LL, Humphrey JM, Mpody C, Yotebieng M, Murnane PM, Clouse K, et al. Achieving UNAIDS 90-90-90 targets for pregnant and postpartum women in Sub-Saharan Africa: progress, gaps and research needs. J Virus Erad. (2018) 4:33–9. doi: 10.1016/S2055-6640(20)30343-5
10. USAIDS: Global Report. Eastern and southern Africa: Regional fact sheet. (2023). Available online at: https://thepath.unaids.org/wp-content/themes/unaids2023/assets/files/regional_fs_eastern_southern_africa.pdf (accessed February 01, 2024).
11. Mude W, Oguoma VM, Gesesew HA, Ameyaw EK, Njue C, Nyanhanda T, et al. HIV/AIDS knowledge and attitudes assessment among women of child-bearing age in South Sudan: findings from a household survey. PLoS One. (2020) 15(12):e0243969. doi: 10.1371/journal.pone.0243969
12. Teshale AB, Tessema ZT, Alem AZ, Yeshaw Y, Liyew AM, Alamneh TS, et al. Knowledge about mother to child transmission of HIV/AIDS, its prevention and associated factors among reproductive-age women in Sub-Saharan Africa: evidence from 33 countries recent demographic and health surveys. PLoS One. (2021) 16(6):e0253164. doi: 10.1371/journal.pone.0253164
13. Darteh EKM, Abraham SA, Seidu A-A, Chattu VK, Yaya S. Knowledge and determinants of women’s knowledge on vertical transmission of HIV and AIDS in South Africa. AIDS Res Ther. (2021) 18(1):1–9. doi: 10.1186/s12981-020-00324-w
14. Haile ZT, Teweldeberhan AK, Chertok IR. Correlates of women’s knowledge of mother-to-child transmission of HIV and its prevention in Tanzania: a population-based study. AIDS Care. (2016) 28(1):70–8. doi: 10.1080/09540121.2015.1062465
15. Luba TR, Feng Z, Gebremedhin SA, Erena AN, Nasser AM, Bishwajit G, et al. Knowledge about mother–to–child transmission of HIV, its prevention and associated factors among Ethiopian women. J Glob Health. (2017) 7(2):1–6. doi: 10.7189/jogh.07.020414
16. Okoko NA, Owuor KO, Kulzer JL, Owino GO, Ogolla IA, Wandera RW, et al. Factors associated with mother to child transmission of HIV despite overall low transmission rates in HIV-exposed infants in rural Kenya. Int J STD AIDS. (2017) 28(12):1215–23. doi: 10.1177/0956462417693735
17. UNAIDS GA. Global AIDS update 2016. Geneva, Switzerland: World Health Organization Library (2016).
18. World Health Organization. Guidance on provider-initiated HIV testing and counselling in health facilities. (2007).
19. World Health Organization. Consolidated guidelines on HIV testing services: 5Cs: consent, confidentiality, counselling, correct results and connection 2015. (2015).
20. Croft TN, Marshall AM, Allen CK, Arnold F, Assaf S, Balian S. Guide to DHS statistics. Rockville: ICF (2018). p. 645.
21. United Nations, African Union Commission, and African Development Bank. Report on sustainable development goals for the Eastern Africa subregion. Addis Ababa: UN Economic Commission for Africa (2015).
22. Grabbe KL, Menzies N, Taegtmeyer M, Emukule G, Angala P, Mwega I, et al. Increasing access to HIV counseling and testing through mobile services in Kenya: strategies, utilization and cost-effectiveness. J Acquir Immune Defic Syndr. (2010) 54(3):317. doi: 10.1097/QAI.0b013e3181ced126
23. Padian NS, McCoy SI, Karim SSA, Hasen N, Kim J, Bartos M, et al. HIV Prevention transformed: the new prevention research agenda. Lancet. (2011) 378(9787):269–78. doi: 10.1016/S0140-6736(11)60877-5
24. Leta TH, Sandøy IF, Fylkesnes K. Factors affecting voluntary HIV counselling and testing among men in Ethiopia: a cross-sectional survey. BMC Public Health. (2012) 12:1–12. doi: 10.1186/1471-2458-12-1
25. Lépine A, Terris-Prestholt F, Vickerman P. Determinants of HIV testing among Nigerian couples: a multilevel modelling approach. Health Policy Plan. (2015) 30(5):579–92. doi: 10.1093/heapol/czu036
26. Teklehaimanot HD, Teklehaimanot A, Yohannes M, Biratu D. Factors influencing the uptake of voluntary HIV counseling and testing in rural Ethiopia: a cross sectional study. BMC Public Health. (2016) 16:1–13. doi: 10.1186/s12889-016-2918-z
27. Alem AZ, Teshale AB, Liyew AM, Tesema GA, Tesema AK, Yeshaw Y. Determinants of HIV voluntary counseling and testing: a multilevel modelling of the Ethiopian demographic and health survey. BMC Women’s Health. (2022) 22(1):1–10. doi: 10.1186/s12905-021-01559-z
28. Kasymova S. Awareness and knowledge about HIV/AIDS among women of reproductive age in Tajikistan. AIDS Care. (2020) 32(4):518–21. doi: 10.1080/09540121.2019.1695736
29. Gebremedhin KB, Tian B, Tang C, Zhang X, Yisma E, Wang H. Factors associated with acceptance of provider-initiated HIV testing and counseling among pregnant women in Ethiopia. Patient Prefer Adher. (2018) 4:183–91. doi: 10.2147/PPA.S148687
30. Bibiana N, Emmanuel P, Amos D, Ramsey Y, Idris A. Knowledge, attitude and factors affecting voluntary HIV counseling and testing services among women of reproductive age group in an Abuja suburb community, Nigeria. Med J Zambia. (2018) 45(1):13–22. doi: 10.55320/mjz.45.1.155
31. Berendes S, Rimal RN. Addressing the slow uptake of HIV testing in Malawi: the role of stigma, self-efficacy, and knowledge in the Malawi BRIDGE project. J Assoc Nurses AIDS Care. (2011) 22(3):215–28. doi: 10.1016/j.jana.2010.08.005
32. Jamison EA, Jamison DT, Hanushek EA. The effects of education quality on income growth and mortality decline. Econ Educ Rev. (2007) 26(6):771–88. doi: 10.1016/j.econedurev.2007.07.001
33. Zegeye B, Adjei NK, Ahinkorah BO, Ameyaw EK, Budu E, Seidu A-A, et al. Barriers and facilitators to accessing health care services among married women in Ethiopia: a multi-level analysis of the Ethiopia demographic and health survey. Int J Transl Med Res Public Health. (2021) 5:1–9. doi: 10.21106/ijtmrph.380
34. Erena AN, Shen G, Lei P. Factors affecting HIV counselling and testing among Ethiopian women aged 15–49. BMC Infect Dis. (2019) 19(1):1–12. doi: 10.1186/s12879-019-4701-0
36. Latunji O, Akinyemi O. Factors influencing health-seeking behaviour among civil servants in Ibadan, Nigeria. Ann Ib Postgrad Med. (2018) 16(1):52–60. PMID: 30254559
37. Kifle D, Azale T, Gelaw YA, Melsew YA. Maternal health care service seeking behaviors and associated factors among women in rural Haramaya district, eastern Ethiopia: a triangulated community-based cross-sectional study. Reprod Health. (2017) 14(1):1–11. doi: 10.1186/s12978-016-0270-5
38. Turk T, Malau C, Andrew R. An integrated approach to strategic communication an condom social marketing to address the HIV/AIDS epidemic in Papua New Guinea. SciFed J AIDS HIV Res. (2017) 1(1):1–9. doi: 10.23959/sfahrj-1000002
39. Kirakoya-Samadoulougou F, Jean K, Maheu-Giroux M. Uptake of HIV testing in Burkina Faso: an assessment of individual and community-level determinants. BMC Public Health. (2017) 17(1):1–11. doi: 10.1186/s12889-017-4417-2
40. Walker GR. “Out there it’s YOLO”: youth perspectives on a mass media HIV-and gender-based violence campaign in South Africa. Afr J AIDS Res. (2021) 20(1):79–87. doi: 10.2989/16085906.2021.1872666
41. Somefun OD, Wandera SO, Odimegwu C. Media exposure and HIV testing among youth in Sub-Saharan Africa: evidence from demographic and health surveys (DHS). Sage Open. (2019) 9(2):2158244019851551. doi: 10.1177/2158244019851551
42. Jackson CA, Henderson M, Frank JW, Haw SJ. An overview of prevention of multiple risk behaviour in adolescence and young adulthood. J Public Health (Bangkok). (2012) 34(suppl_1):i31–40. doi: 10.1093/pubmed/fdr113
43. Seidu A-A, Oduro JK, Ahinkorah BO, Budu E, Appiah F, Baatiema L, et al. Women’s healthcare decision-making capacity and HIV testing in Sub-Saharan Africa: a multi-country analysis of demographic and health surveys. BMC Public Health. (2020) 20(1):1–11. doi: 10.1186/s12889-019-7969-5
44. Ndao-Brumblay SK, Mbaruku G, Kruk ME. Parity and institutional delivery in rural Tanzania: a multilevel analysis and policy implications. Health Policy Plan. (2013) 28(6):647–57. doi: 10.1093/heapol/czs104
45. Zegeye B, Adjei NK, Ahinkorah BO, Tesema GA, Ameyaw EK, Budu E, et al. HIV testing among women of reproductive age in 28 Sub-Saharan African countries: a multilevel modelling. Int Health. (2023) 5:ihad031. doi: 10.1093/inthealth/ihad031
46. Benavides-Torres RA, Wall KM, Rocha GMN, Rodríguez DJO, Hopson L. Factors associated with lifetime HIV testing in Texas by race/ethnicity. Open AIDS J. (2012) 6:232. doi: 10.2174/1874613601206010232
47. Inungu J, Lewis A, Younis MZ, Wood J, O’Brien S, Verdun D. HIV testing among adolescents and youth in the United States: update from the 2009 behavioral risk factor surveillance system. Open AIDS J. (2011) 5:80. doi: 10.2174/1874613601105010080
48. Kposowa AJ. Marital status and HIV/AIDS mortality: evidence from the US national longitudinal mortality study. Int J Infect Dis. (2013) 17(10):e868–74. doi: 10.1016/j.ijid.2013.02.018
49. Kposowa AJ. Marital status and suicide in the national longitudinal mortality study. J Epidemiol Community Health. (2000) 54(4):254–61. doi: 10.1136/jech.54.4.254
50. Klovdahl AS, Potterat JJ, Woodhouse DE, Muth JB, Muth SQ, Darrow WW. Social networks and infectious disease: the Colorado springs study. Soc Sci Med. (1994) 38(1):79–88. doi: 10.1016/0277-9536(94)90302-6
51. Harawa NT, Greenland S, Cochran SD, Cunningham WE, Visscher B. Do differences in relationship and partner attributes explain disparities in sexually transmitted disease among young white and black women? J Adolesc Health. (2003) 32(3):187–91. doi: 10.1016/S1054-139X(02)00458-5
52. Maulsby CH, Ratnayake A, Hesson D, Mugavero MJ, Latkin CA. A scoping review of employment and HIV. AIDS Behav. (2020) 24:2942–55. doi: 10.1007/s10461-020-02845-x
53. Bashemera DR, Nhembo MJ, Benedict G. The role of women’s empowerment in influencing HIV testing. Rockville, Maryland: ICF (2013).
Keywords: counseling, East Africa, HIV testing, receipt result, women
Citation: Terefe B (2024) HIV counseling, testing, and test result receipt among East African women of reproductive age using recent national health surveys. Front. Reprod. Health 6:1305671. doi: 10.3389/frph.2024.1305671
Received: 2 October 2023; Accepted: 26 January 2024;
Published: 7 February 2024.
Edited by:
Dorina Onoya, Health Economics and Epidemiology Research Office (HE2RO), South AfricaReviewed by:
Arshad Altaf, WHO Regional Office for the Eastern Mediterranean, EgyptHussaini Zandam, Brandeis University, United States
© 2024 Terefe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bewuketu Terefe d29sZGVhYndvbWFyaWFtQGdtYWlsLmNvbQ==
 Bewuketu Terefe
Bewuketu Terefe