- 1Department of Social Work and Social Administration, Makerere University, Kampala, Uganda
- 2Department of Statistical Methods and Actuarial Sciences, Makerere University, Kampala, Uganda
- 3Department of Population Studies, Makerere University, Kampala, Uganda
- 4Department of Sexual and Reproductive Health and Rights, United Nations Population Fund, Kampala, Uganda
Introduction: Young people living with disability form one of the most vulnerable population groups globally. There is limited information on the use of SRH services among young people living with a disability.
Methods: This analysis is based on household survey data among young people. Drawing on a sample of 861 young people living with a disability (15 -24 years), we investigate the sexual behaviour, and identify the risk factors associated with sexual behavior of young people living with a disability. Multilevel logistic regression was used.
Results: Results indicate that risky sexual behaviour was associated with alcohol consumption (aOR = 1.68; 95%CI: 0.97, 3.01), having limited knowledge of HIV and STI prevention methods (aOR = 6.03; 95%CI: 0.99, 30.00), and low life skills (aOR = 4.23; 95%CI: 1.59, 12.87). The odds of not using a condom at last sex were significantly higher among in-school young people than out of school young people (aOR = 0.34; 95%CI: 0.12, 0.99).
Discussion: Targeted interventions aimed at reaching out to young people living with a disability should consider their sexual and reproductive health needs, barriers, and facilitators. Interventions can also promote self-efficacy and agency of young people living with a disability in making informed sexual and reproductive health choices.
Introduction
The Convention on the Rights of Persons with Disabilities (CRPD) advocates for enjoyment of all human rights and fundamental freedoms among people living with disabilities (1). Disability occurs as a result of an impairment of cognitive, developmental, emotional, physical, mental, sensory or a combination of all that affects one to fully participate in activities (2). Goal Three of the Sustainable Development Goal (SDG) calls for universal access to health including access to sexual and reproductive health (SRH) services and information (3–5).
Young people living with a disability (YPWD) form one of the most vulnerable population groups globally (6). YPWD form a significant proportion of young people in developing countries; with nearly 80 percent of 180–220 million YPWD globally living in developing countries (7, 8). In Uganda, the recent 2016 Uganda Demographic and Health Survey reports that 16% of young people aged (10–19 years) were living with a disability (9). Access to SRH services among YPWD is a public health issue (10). There is limited information on the use of SRH services among this population group (11). While sexual behavior may be regarded as a universal aspect for every human being (12, 13), some literature has pointed to misconceptions surrounding sexual behavior among YPWD (14). For example, there is a view that YPWD do not engage in sexual activity or that they are asexual (15) or that having quality sexual behavior is less important compared to providing medical attention or rehabilitation needed for them (16). These views assume that YPWD do not need information regarding prevention risky sexual behavior or how to maneuver around it.
The quality of life for every individual including YPWD is an important dimension (17), which improves wellbeing (18). Further, YPWD can have unsafe sex (19), or engage in sexual behavior, but may miss the necessary skills, negotiation power and information to engage in safer sexual activity (8, 20). As a result, YPWD are often marginalized, discriminated, and relegated to the background or neglected when it comes to accessing SRH services (21–24). Moreover, health workers often miss some information regarding the sexual behavior of YPWD and are unable to advise them on some prevention strategies against STIs (25). YPWD are unable to receive SRH services or information in the form of contraception to prevent unwanted pregnancies (26), or even prevent STIs because of the misconception that YPWD do not have sex (27). Other challenges associated with limited information or services among YPWD include physical barriers (28), transport challenges (29), long waiting times (30), lack of confidentiality (31), need for an escort (32) and disability-related stigma (33) or negative attitudes (34). While these challenges are common across the board, they tend to be exacerbated among YPWD because they are categorically different, and with different needs. For example, the young people with mental disability would have different requirements from those with physical disability.
In general, given the challenges associated with limited access to SRH services, YPWD tend to engage in risky sexual behavior with far reaching negative consequences (35). For example, YPWD tend to experience child marriage (35), unintended pregnancies (36), induced abortion (21), sexually transmitted infections (STIs) including HIV (37) because of risky sexual behavior. While access to SRHR services is a general problem, YPWD tend to be more vulnerable than their counterparts. YPWD are more likely to engage in risky sexual behavior or abused than young people who are not living with a disability (38).
Most interventions are tailored towards young people without taking into consideration the vulnerable groups such as YPWD (39). This paper therefore seeks to understand the sexual behavior of YPWD, and the determinants associated with sexual behavior of YPWD. The results from such analyses can inform the design of interventions on reproductive health among YPWD. Moreover, the results can contribute to improving the quality of SRH services among YPWD.
Methods
The current analysis is based on household survey data collected for the baseline knowledge, attitudes and practices (KAP) study of the UNFPA's supported program on Advancing Sexual Reproductive Health and Rights (ANSWER) in Northern Uganda. The study population was young people (15–24 years). Data were collected between August and September 2021. The household KAP survey was based on a stratified two-stage cluster design with stratification on districts, cross-stratified on the rural-urban residence. In refugee-hosting districts, cross-stratification was also done on refugee communities and host communities. In the first stage, a probability proportional to the size sample of villages was taken from each stratum. In the second stage, a probability systematic sample of households with young people (15–24 years) was taken.
The outcome variables in this study included: involvement in risky sexual behavior (RSB) in the past 12 months, that is multiple sexual partnerships, transactional sex and non-use of condoms at last sex with a non-marital partner. The explanatory variables included age, education, marital status, nationality, alcohol consumption, household wealth, religion, exposure to media, attitudes towards teenage pregnancy and condom use, knowledge of sexually transmitted infections, HIV and their prevention methods, life skills, self-efficacy, gender norms, type of disability. The assessment of attitudes toward teenage pregnancy was based on a proxy indicator, where respondents were asked to justify having a child whilst still a teenager. These included: (a) having a baby to love, (b) moving out of parent's house, (c) getting married early, (d) proving one's fertility, (e) enjoying the child/children growing up, (f) having a partner to love, and (g) proving you are a man/woman. However, we note that we are likely to miss out on the bad/negative attitudes especially from teenagers who have ever been pregnant since the response options available are only about the positive/good things.
Household asset index as a proxy measure for the economic wellbeing of a household was constructed through Principal Component Analysis model of household owned domestic items (radio, television set, sofa sets, mattress, solar/electricity for lighting, access to running in the house or yard), transport assets (bicycle, motorcycle, car), and productive assets (computer, mobile phones) and has an income generating activity. Generally, based on the pca scores, households were classified as having high household assets index if they had at least 6 of these 12 items assessed.
Knowledge of preventing HIV/AIDS and STIs, and their treatment was obtained from alpha factoring of six items. Respondents were asked to affirm the following: (a) having and being faithful to only one sexual partner is an effective way of preventing HIV, (b) a person can reduce their chances/risk of getting HIV by not having sex, (c) a person can reduce their chances/risk of getting HIV by using condoms when having sex, (d) the HIV/AIDS virus can be transmitted by mosquito bites, (e) the HIV/AIDS virus can be transmitted by supernatural means, (f) a person can become infected by sharing food with a person who has the AIDS virus, (g) a girl or boy cannot get HIV the first time she/he has sexual intercourse, and in addition to knowledge at least two other STIs in addition to HIV/AIDS, and source of their treatment.
The score for gender and social norms was computed from the responses to the following questions, with Likert scale options: (a) boys and girls have equal abilities, (b) Giving a bath and feeding kids are the mother's responsibility, (c) Woman's role is taking care of her home and family, (d) a man should have the final word about decisions in the home, (d) preventing pregnancy is a woman's responsibility, (a) Young people like you/me should not be allowed to use contraceptive services; (b) It is wrong for young girls who are sexually active to use contraceptives, (c) Women who use contraception may become promiscuous.
Life skills score for self-efficacy to avoid risky sex, including using a condom was measured by asking the respondents to affirm to the following statements: (a) I am confident I can get the person with whom I have sex to use a condom, even if he/she doesn't want me to use a condom, (b) I am confident If my partner and I do not have a condom, I can say no to sex, (e) I make smart decisions to avoid unsafe sex. Self-efficacy was measured by asking the respondents to affirm to the following statements: (a) I am confident if I did not want to have sex, I would be able to refuse sex with a person who has power over me, like a teacher, employer, relative, etc., (b) I am confident I can get the person with whom I have sex to use a condom, even if he/she doesn't want me to use a condom, and (c) I am confident If my partner and I do not have a condom, I can say no to sex.
Positive attitude condom use was measured by asking respondents to respond to the following statements: (a) condoms reduce sexual pleasure, (b) condoms can slip off a man's penis and enter a woman's body, (c) it is too embarrassing for someone like you to buy or obtain condoms, and (d) if a girls suggested to her partner to use a condom it would mean that she does not trust him.
An additional module based on the Short Set of questions developed by the Washington Group on Disability Statistics to estimate the prevalence of disabilities was also included in the Household Questionnaire. The Short Set questions address six core functional domains—seeing, hearing, communication, cognition, walking, and self-care.
The analysis is based on 861 young people living with disability, from among the 6,056 young people aged 15–24 years. These were mainly individuals with some difficulties with their sight (42%), hearing (25%), and memory (17%), and 27% had physical disabilities. We note that this sample size, based on sample size formula by Cochran (1963), is adequate for estimating of a proportion of YPWDs involved in risky sexual behaviour within the two standard errors with 95% certainty. This holds for population level proportions of at least 10% of YPWDs engaging in risky sexual behaviour.
At the bivariate analysis level, F-test was used to test for associations. Variables with p < 0.10 at the bivariate level and those contextually important (sex, age, schooling status and marital status) were included in multilevel logistic regression model for each of the three outcome variables. In addition, inverse probabilities of selection were included in the models as weights to further account for the complex sample survey design features. Analyses were executed in Stata V15. In multivariable regression models, adjusted model coefficients and their 95% confidence intervals (95% CI) were computed using the stepwise approach. Hosmer-Lemeshow test statistics were conducted to check model goodness of fitness. This study was approved by Uganda National Counsil for Science and Technology (UNCST) (HS1079ES).
Results
Sample characteristics of respondents
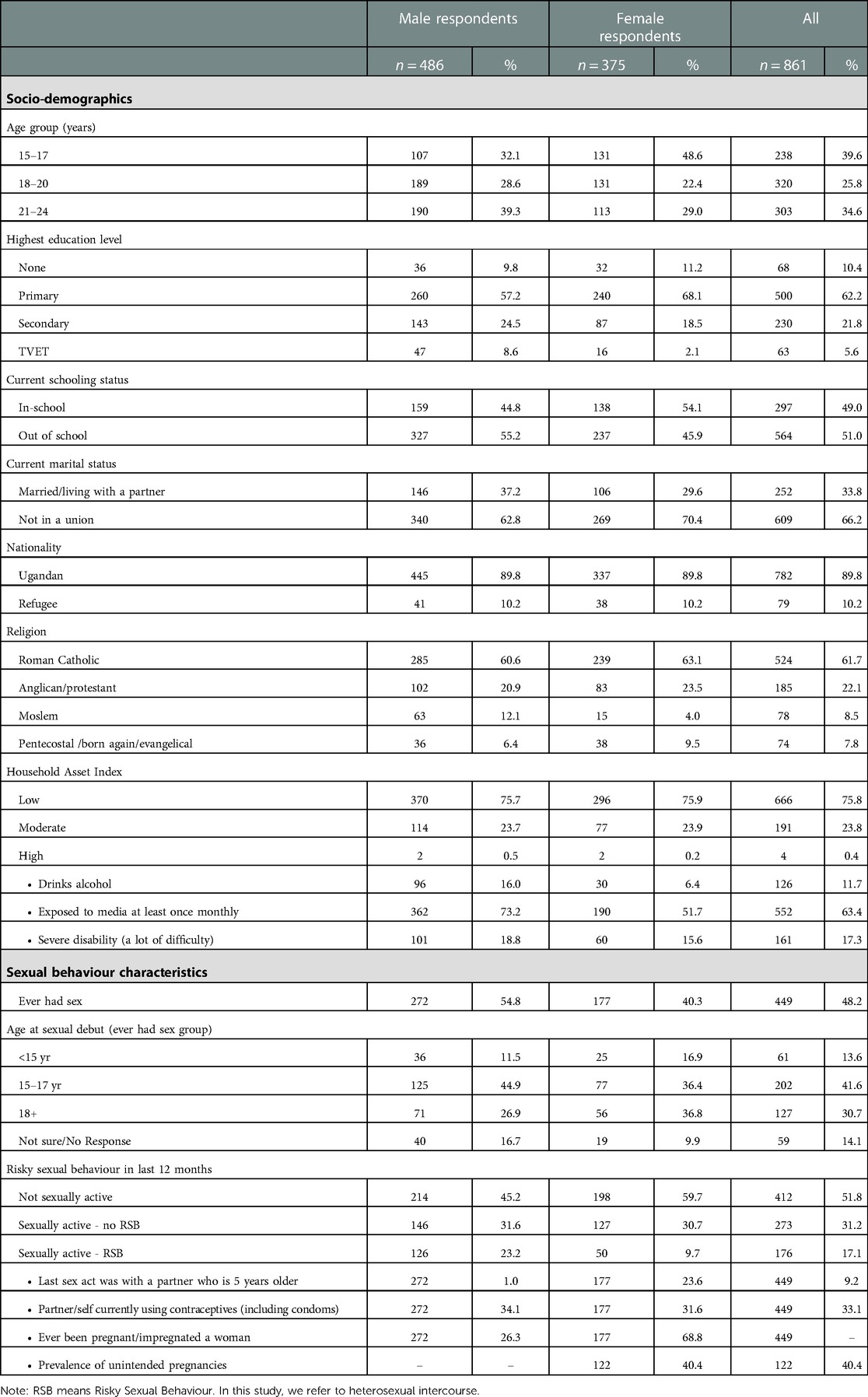
Of the 861 respondents, 45.4% were female, 44.4% were aged 20-24 years, and 50.9% were out of school (Table 1). Further, 10.2% were refugees (10.2% males vs. 10.2% females), 61.7% were Roman Catholics (60.6% males vs. 63.1% females), and 33.8% were living in a marital relationship (37.2% males vs. 29.6% females), and only 21.8% had a secondary school education (24.5% males vs. 18.5% females). Sixty-three percent reported exposure to media at least once a month, notably radios, newspapers, tabloids, television, and social media. Most of the respondents (75.8%) were from households with less than four of the 12 household assets assessed, and less than 1% were from households that had at least 10 assets. About 12% reported alcohol consumption within the last week. The distribution of age groups was similar between male and female respondents but there were slightly more females married than males (33.8% vs. 29.6%), and more males consume alcohol than females (16.0% vs. 6.4%).
Sexual behaviour of respondents
Of the 861 individuals, 48.2% (40.3% of females and 54.8% of males) reported having ever had sex, and 17.1% (9.7% of females and 23.2% of males) reported having been involved in risky sexual behavior (RSB) in the past 12 months preceding the survey, i.e., multiple sexual partnerships, transactional sex and no use of condom use in the last sex act with a non-marital partner. Fourteen percent (16.9% of the females and 11.5% of the males) had sex before turning 15 years of age, and 53.3% of females and 56.4% of males had sex before the age of 18 years. Equivalently, among all the YPWD, 6.6% (6.3% of the male and 6.8% of the female) and 26.6% (32.2% of the male and 22.0% of the female) had sex before the ages of 15 years and 18 years, respectively. Nearly, one in four young women and girls reported their last sexual partner in the past 12 months to have been at least five years older than them.
The current use of modern contraceptives (including consistent use of male condoms) was reported by 33.1% of the young people while 40.4% of the girls and young women reported their last pregnancy as unintended.
Factors associated with risky sexual behavior
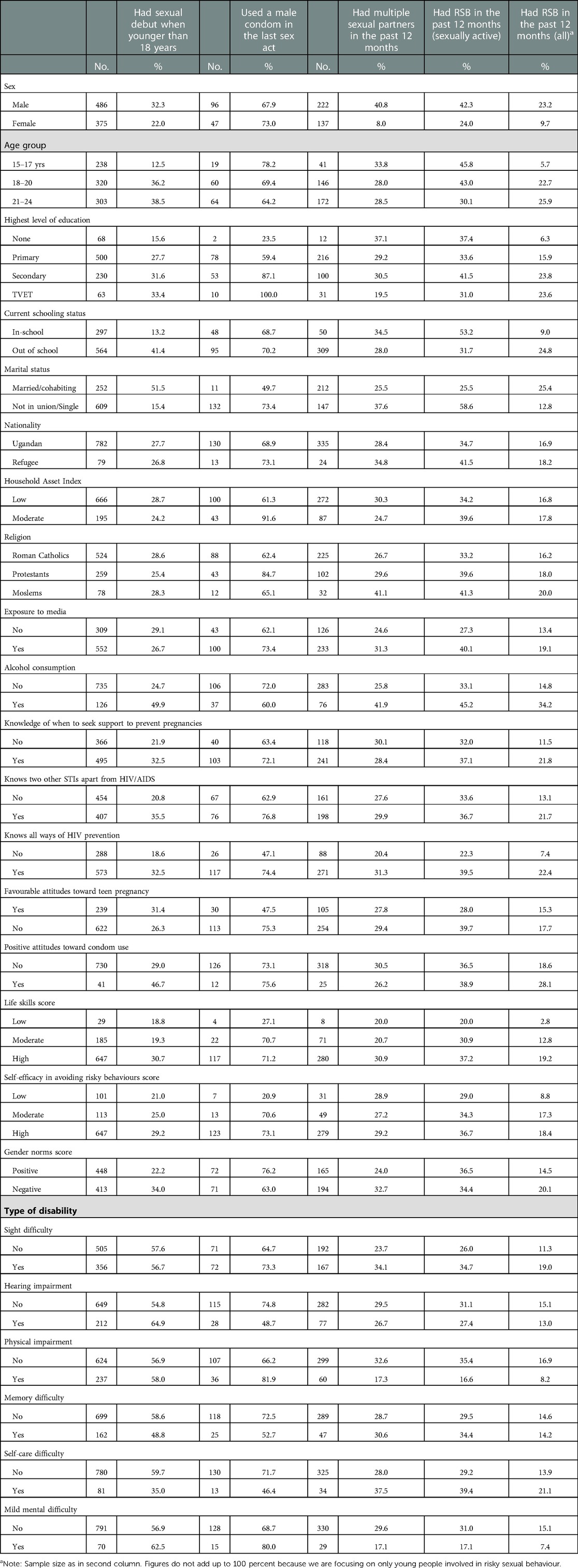
Engagement in multiple sexual partnerships in the past 12 months: The involvement in multiple sexual partnerships within the past 12 months was mostly reported by men and boys, the YPWD who consume alcohol, and those negative gender norms. A higher proportion of individuals who consume alcohol reported multiple sexual partners than the proportion of individuals who do not consume alcohol (41.9% vs. 25.8%, F = 4.99; pval = 0.027). Moreover, a significantly higher proportion of individuals with negative gender norms than that of individuals with equitable gender norms reported multiple sexual partnerships (32.7% vs. 24.0%, F = 2.89, pval = 0.049).
Condom use in the last risky sex act in the past 12 months: Results in Table 2 show that up to 32% of male respondents and 27% of female respondents did not use a condom in their most recent risky sex act. At bivariate analysis, secondary education level, knowledge of HIV prevention methods, knowledge of other STIs (in addition to HIV/AIDS), knowledge of where to obtain contraceptives (including condoms), positive gender norms, high score of life skills and self-efficacy, and unfavorable attitudes toward teen pregnancy were associated high percentages using a condom. Eighty-seven percent of respondents with secondary school education as compared to only 23.5% of those without formal education reported condom use in the last risky sex act (F = 7.10; pval = 0.049). Similarly, a higher percentage of individuals with good knowledge of HIV prevention methods (74.4%) used a condom as compared to 47.1% of those with limited knowledge (F = 3.951; pval = 0.036). More individuals (76.2%) with positive gender norms as compared to 63.0% of those with negative gender norms used a condom (F = 2.93, pval = 0.049), and 73.1% of individuals with high self-efficacy to avoid risky behavior as compared to 20.9% of individuals with low self-efficacy used the condom (F = 5.945; pval = 0.001). However, positive, or negative attitudes toward condom use did not matter.
Involvement in risky sexual behavior (composite score) among sexually active young people in the last 12 months: Bivariate analysis results in Table 2 show that a lower proportion of female YPWD (24.0%) engaged in RSB than the male YPWD (42.3%) (F = 11.06; pval = 0.001); and lower proportion of out of school YPWD (31.7%) than the proportion of in-school YPWDs (53.2%) reported RSB in the past 12 months preceding the survey (F = 5.55, pval = 0.019). The results also show that a higher percentage of individuals with good knowledge of HIV prevention methods engaged in risky sexual behavior as compared to those with limited knowledge (39.5% vs. 22.3%; F = 6.96; pval = 0.009).
Involvement in risky sexual behavior (composite score) among all young people in the last 12 months: Among all YPWD (sexually active and non-sexually active), only 17.2% (23.2% of male and 9.7% of female) of young people were involved in risky sexual behaviour (RSB) within the last 12 months (Table 2). Bivariate analysis presented in Table 2 show that having secondary school education, being out of school, consuming alcohol, and holding inequitable gender norms were associated with RSB within the past 12 months. Twenty percent of individuals with inequitable gender norms as compared to 14.5% of individuals with equitable gender norms were engaged in RSB (F = 3.19; pval = 0.045); and 34.2% of individuals who drink alcohol as compared to only 14.8% of those who do not reported RSB. Overall, being in school was protective of engagement in RSB as only 9.0% of the in-school YPWD engaged in RSB as compared to 24.8% of the out of school young people (F = 17.00; pval < 0.001). Taken together with results in the previous section, this implies that schooling is a protective factor to RSB but the few in-school young people who become sexually active face higher risks of pregnancy, and STIs than the out of school young people.
Sexual debut before 18 years of age: The results are presented in Table 2. At bivariate analysis, factors associated with early initiation of sexual debut were being male (32.2% vs. 22.0% of females; F = 11.25, pval = 0.004); being out of school (41.4% vs. 13.2% of in-school; F = 45.29; pval < 0.001); alcohol consumption (49.9% vs. 24.7% of non-alcohol consumers; F = 24.46; pval < 0.001); and holding negative gender norms (34.0% vs. 22.2% of individuals with positive gender norms; F = 9.06, pval = 0.003).
Multivariable analysis of factors associated with risky sexual behavior
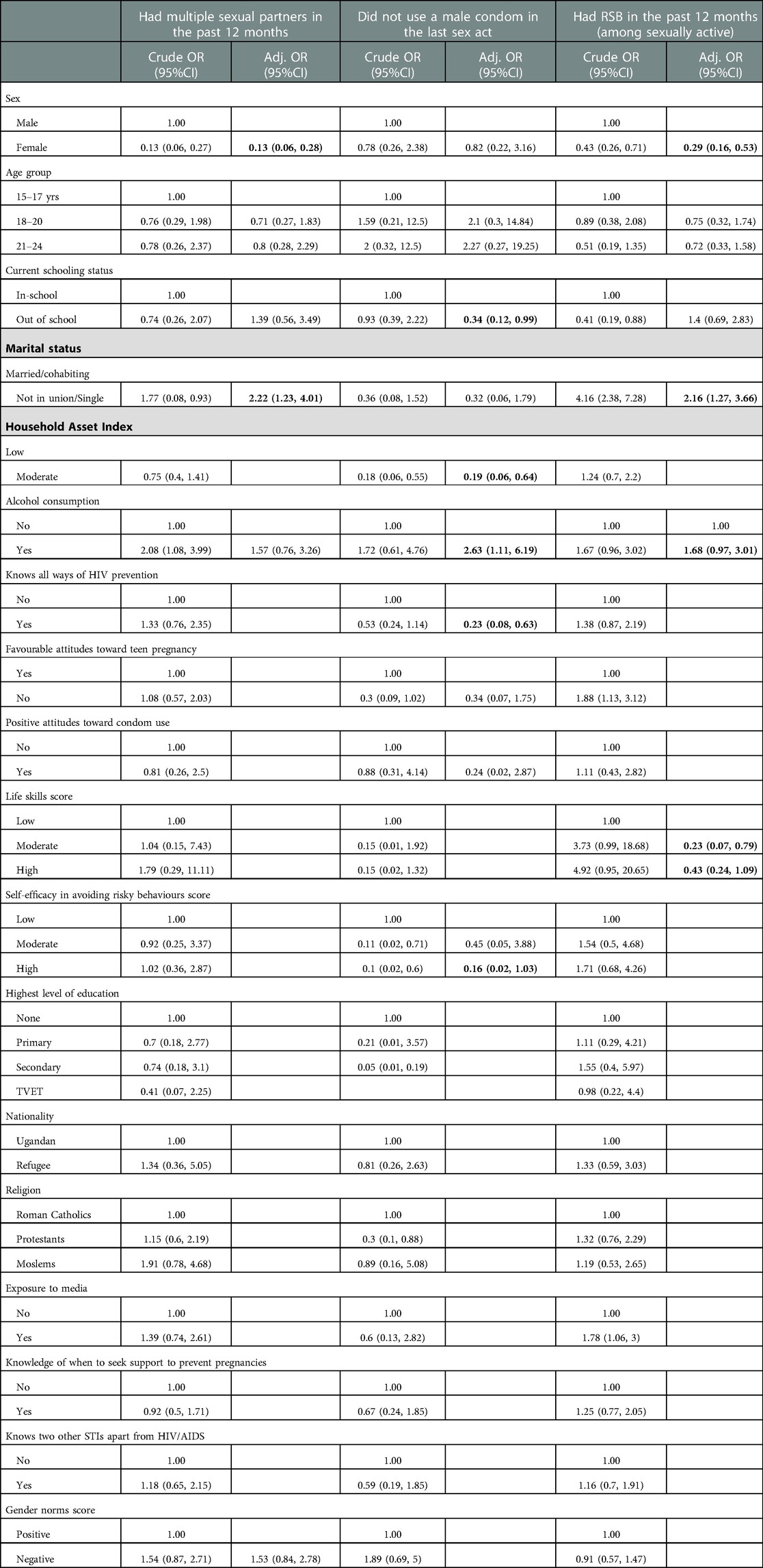
The odds of involvement in RSB relative to other sexually active young people were independently increased by alcohol consumption (aOR = 1.68; 95%CI: 0.97, 3.01) and higher among boys and men than girls and women (see Table 3). The odds of engaging in RSB was low among young people with life skills; young people who reported below average scores of life skills had more than four times the odds of engaging in RSB than those with above average scores – above vs. below average had (aOR = 0.23; 95%CI: 0.07, 0.79). Similarly, the involvement in RSB with respect to the whole population of YPWD was also driven by these same factors, in addition to age group.
For some of the individual components of RSB such as the odds of not using a condom in a high-risk sexual act were driven by alcohol consumption (aOR = 2.63; 95%CI: 1.11, 6.19), limited knowledge of HIV and STI prevention methods (aOR = 6.03; 95%CI: 0.99, 30.00), and low life skills score (or low self-efficacy) (aOR = 4.23; 95%CI: 1.59, 12.87). The odds of not using a condom was significantly higher among in-school young people than out of school young people (aOR = 0.34; 95%CI: 0.12, 0.99).
Discussion
Our findings demonstrate that on average about two in ten YPWD engage in high risky sexual behavior such as multiple sexual partnerships, transactional sex and non-use of condom in the last sex act with a non-marital partner. Studies conducted in other low- and middle-income countries have found similar results that point to risky sexual behaviour among YPWD (20, 39–42). For example, Oladunni (2012) found that about a third of adolescents with a disability in Nigeria had multiple sexual partners at a time and engage in multiple sexual relationships and about 12 percent do not take any action to prevent pregnancy.
Results show early initiation of sex before 15 years (sexual debut) and by the age of 18 years more than a quarter of YPWD have had sex, and cross-generational sex was high among female YPWD. These results are in conformity with those from other studies in Africa and from other low-income countries (21, 41). For example, Oladunni (2012) found that more than half of adolescents with a disability had sex by the age of 15 years. Similarly, a study conducted in Ghana established that young people with hearing and vision loss had a higher likelihood of engaging in casual sex (42). This further reemphasizes the need to prioritise and integrate disability in programming for SRHR (43).
Consistent use of male condoms was low among YPWD, and this may explain the very high rate of unintended pregnancies that affects four in five girls and young women. Results confirm those of other studies conducted in relatively similar contexts in Africa and low-income countries (36). For example, in a study carried out in Ethiopia among YPWD, Kassa and colleagues (2014) found that only a third of them used contraceptives (21).
Individuals who consume alcohol had almost twice the odds of engaging in RSB than those who do not. These results are similar to a number of studies that underscore alcohol consumption as a risk factor for engagement in risky sexual behaviour for YPWD (44–46). For example, Marshal (2014) found that alcohol use and other risk-taking behaviours and risky sexual behaviour emerge in adolescence and tend to cluster together.
Conclusion
This study has demonstrated that YPWD are sexually active and engage in sex as early as 15 years. The YPWD are at risk of unintended pregnancies and acquiring of sexually transmitted infections, and associated consequences. The risks are heightened by low life skills, limited agency, and alcohol consumption. The study underscores the importance of schooling and access to sexuality education. This means policies and programmes for government and non-government entities should be intentional in promoting access and completion of schooling for YPWD. This further emphasizes the need to address barriers of access to education for YPWD including social and gender norms that create stigma and downplay education for them and the other structural barriers related to infrastructure, skilled human resources especially teachers and other service providers as well as the required equipment. Interventions designed to promote safe sexual practices and negative SRH outcomes should integrate addressing alcohol as a risk factor. The results also highlight the need for interventions targeting YPWD starting early in their adolescence to ensure they have the appropriate sexuality education, life skills and agency to make informed choices related to engaging in safe sex to prevent undesirable reproductive health outcomes. The YPWD should also be engaged in co-design of interventions and services designed to meet their SRH needs and to promote safe sexual practices.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Makerere University School of Public Health Research and Ethics Committee. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
Conceptualization: PB, SPW, PK, VK, CK. Data curation: SPW, PK. Formal analysis: SPW. Investigation: PB, SPW, PK, VK, CK, WM, SN, CA. Methodology: SPW. Resources: VK, CK, WM, SN, CA. Writing – original draft: PK, SPW, PB. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/articles/10.3389/frph.2023.1065437/full#supplementary-material.
References
1. United Nations Division for Social Policy and Development Disability. Convention on the Rights of Persons with Disabilities (CRPD). 2018.
2. Ganle JK, Baatiema L, Quansah R, Danso-Appiah A. Barriers facing persons with disability in accessing sexual and reproductive health services in sub-Saharan Africa: a systematic review. Plos One. (2020) 15(10):e0238585. doi: 10.1371/journal.pone.0238585
3. Mac-Seing M, Zarowsky C, Yuan M, Zinszer K. Disability and sexual and reproductive health service utilisation in Uganda: an intersectional analysis of demographic and health surveys between 2006 and 2016. BMC Public Health. (2022) 22(1):438. doi: 10.1186/s12889-022-12708-w
4. Djilas S, Trumpfheller L, Bayingana M-E, Latif A-MA. The intersection of disability and youth sexual and reproductive health programming in francophone West Africa. 2020.
5. United Nations Statistical Commission. Report of the Inter-Agency and Expert Group on Sustainable Development Goal Indicators. 2016.
6. Pearce E. ‘Ask Us What We Need’: Operationalizing Guidance on Disability Inclusion in Refugee and Displaced Persons Programs. 2017.
8. Obasi M, Manortey S, Kyei KA, Addo MK, Talboys S, Gay L, et al. Sexual and reproductive health of adolescents in schools for people with disabilities. Pan Afr Med J. (2019) 33:1–11. doi: 10.11604/pamj.2019.33.299.18546
9. Uganda Bureau of Statistics (UBOS) and ICF. Uganda Demographic and health survey 2016. Kampala, Uganda and Rockville, Maryland, USA: UBOS and ICF (2018).
10. Kumi-Kyereme A. Sexual and reproductive health services utilisation amongst in-school young people with disabilities in Ghana. Afr J Disabil. (2021) 10:1–9. doi: 10.4102/ajod.v10i0.671
11. Burke E, Kébé F, Flink I, van Reeuwijk M, le May A. A qualitative study to explore the barriers and enablers for young people with disabilities to access sexual and reproductive health services in Senegal. Reprod Health Matters. (2017) 25(50):43–54. doi: 10.1080/09688080.2017.1329607
12. World Health Organization. Promoting sexual and reproductive health for persons with disabilities. 2009.
13. Mesiäislehto V, Katsui H, Sambaiga R. Disparities in accessing sexual and reproductive health services at the intersection of disability and female adolescence in Tanzania. Int J Environ Res Public Health. (2021) 18(4):1–14. doi: 10.3390/ijerph18041657
14. Olaleye AO, Anoemuah OA, Ladipo OA, Delano GE, Idowu GF. Sexual behaviours and reproductive health knowledge among in-school young people with disabilities in Ibadan, Nigeria. Health Educ. (2007) 107:208–18. doi: 10.1108/09654280710731566
15. Stein S, Dillenburger K. Ethics in sexual behavior assessment and support for people with intellectual disability. Int J Disabil Human Dev. (2017) 16(1):11–7. doi: 10.1515/ijdhd-2016-0023
16. Holdsworth E, Trifonova V, Tanton C, Kuper H, Datta J, Macdowall W, et al. Sexual behaviours and sexual health outcomes among young adults with limiting disabilities: findings from third British national survey of sexual attitudes and lifestyles (natsal-3). BMJ Open. (2018) 8(7):e019219. doi: 10.1136/bmjopen-2017-019219
17. Smith AE, Molton IR, McMullen K, Jensen MP. Brief report: sexual function, satisfaction, and use of aids for sexual activity in middle-aged adults with long-term physical disability. Top Spinal Cord Inj Rehabil. (2015) 21(3):227–32. doi: 10.1310/sci2103-227
18. Taleporos G, McCabe MP. Relationships, sexuality and adjustment among people with physical disability. Sex Relation Ther. (2003) 18(1):25–43. doi: 10.1080/1468199031000061245
19. Baines S, Emerson E, Robertson J, Hatton C. Sexual activity and sexual health among young adults with and without mild/moderate intellectual disability. BMC Public Health. (2018) 18(1):1–12. doi: 10.1186/s12889-018-5572-9
20. Oladunni TM. Sexual behavior and practices among adolescents with disabilities in southwest Nigeria. Sex Disabil. (2012) 30(3):289–99. doi: 10.1007/s11195-012-9270-8
21. Kassa TA, Luck T, Birru SK, Riedel-Heller SG. Sexuality and sexual reproductive health of disabled young people in Ethiopia. Sex Transm Dis. (2014) 41(10):583–8. doi: 10.1097/OLQ.0000000000000182
22. Taiwo MO. Access to sexuality information among adolescents with disability. IFE PsychologIA. (2012) 20(2):142–9. doi: 10.10520/EJC124270
23. Rohwerder B, Wong S, Pokharel S, Khadka D, Poudyal N, Prasai S, et al. Describing adolescents with disabilities’ experiences of COVID-19 and other humanitarian emergencies in low- and middle-income countries: a scoping review. Glob Health Action. (2022) 15(1):2107350. doi: 10.1080/16549716.2022.2107350
24. Tanabe M, Nagujjah Y, Rimal N, Bukania F, Krause S. Intersecting sexual and reproductive health and disability in humanitarian settings: risks, needs, and capacities of refugees with disabilities in Kenya, Nepal, and Uganda. Sex Disabil. (2015) 33(4):411–27. doi: 10.1007/s11195-015-9419-3
25. Kassa TA, Luck T, Bekele A, Riedel-Heller SG. Sexual and reproductive health of young people with disability in Ethiopia: a study on knowledge, attitude and practice: a cross-sectional study. Global Health. (2016) 12(1):5. doi: 10.1186/s12992-016-0142-3
26. Mekonnen AG, Bayleyegn AD, Aynalem YA, Adane TD, Muluneh MA, Asefa M. Level of knowledge, attitude, and practice of family planning and associated factors among disabled persons, north-shewa zone, amhara regional state, Ethiopia. Contracept Reprod Med. (2020) 5(1):8. doi: 10.1186/s40834-020-00111-y
27. Isler A, Tas F, Beytut D, Conk Z. Sexuality in adolescents with intellectual disabilities. Sex Disabil. (2009) 27(1):27–34. doi: 10.1007/s11195-009-9107-2
28. Shields N, Synnot AJ, Barr M. Perceived barriers and facilitators to physical activity for children with disability: a systematic review. Br J Sports Med. (2012) 46(14):989. doi: 10.1136/bjsports-2011-090236
29. Cochran AL. Understanding the role of transportation-related social interaction in travel behavior and health: a qualitative study of adults with disabilities. J Transp Health. (2020) 19:100948. doi: 10.1016/j.jth.2020.100948
30. Redmond B, Richardson V. Just getting on with it: exploring the service needs of mothers who care for young children with severe/profound and life-threatening intellectual disability. J Appl Res Intellect Disabil. (2003) 16(3):205–18. doi: 10.1046/j.1468-3148.2003.00165.x
31. Adugna MB, Nabbouh F, Shehata S, Ghahari S. Barriers and facilitators to healthcare access for children with disabilities in low and middle income sub-saharan African countries: a scoping review. BMC Health Serv Res. (2020) 20(1):15. doi: 10.1186/s12913-019-4822-6
32. Leal Rocha L, Vieira de Lima Saintrain M, Vieira-Meyer APGF. Access to dental public services by disabled persons. BMC Oral Health. (2015) 15(1):35. doi: 10.1186/s12903-015-0022-x
33. Green SE. “What do you mean ‘what's wrong with her?’”: stigma and the lives of families of children with disabilities. Soc Sci Med. (2003) 57(8):1361–74. doi: 10.1016/S0277-9536(02)00511-7
34. Carew MT, Braathen SH, Swartz L, Hunt X, Rohleder P. The sexual lives of people with disabilities within low- and middle-income countries: a scoping study of studies published in English. Glob Health Action. (2017) 10(1):1337342. doi: 10.1080/16549716.2017.1337342
35. Addlakha R. How young people with disabilities conceptualize the body, sex and marriage in urban India: four case studies. Sex Disabil. (2007) 25(3):111–23. doi: 10.1007/s11195-007-9045-9
36. Alhusen JL, Bloom T, Laughon K, Behan L, Hughes RB. Perceptions of barriers to effective family planning services among women with disabilities. Disabil Health J. (2021) 14(3):101055. doi: 10.1016/j.dhjo.2020.101055
37. McCabe MP, Taleporos G. Sexual esteem, sexual satisfaction, and sexual behavior among people with physical disability. Arch Sex Behav. (2003) 32(4):359–69. doi: 10.1023/A:1024047100251
38. Löfgren-Mårtenson L, Sorbring E, Molin M. “T@ngled up in blue”: views of parents and professionals on internet use for sexual purposes among young people with intellectual disabilities. Sex Disabil. (2015) 33(4):533–44. doi: 10.1007/s11195-015-9415-7
39. Wazakili M, Mpofu R, Devlieger P. Experiences and perceptions of sexuality and HIV/AIDS among young people with physical disabilities in a South African township: a case study. Sex Disabil. (2006) 24(2):77–88. doi: 10.1007/s11195-006-9006-8
40. Maart S, Jelsma J. The sexual behaviour of physically disabled adolescents. Disabil Rehabil. (2010) 32(6):438–43. doi: 10.3109/09638280902846368
41. Cissé K, Ouedraogo HG, Lougué S, Zoungrana C, Clement B, Kouanda S. Predicting factors of sexual behaviours at risk of HIV infection among people living with disabilities: a generalized structural equation model. AIDS Care. (2022) 34(sup1):35–45. doi: 10.1080/09540121.2022.2051422
42. Kumi-Kyereme A, Adam I, Adongo CA, Oduro GY, Darteh EKM, Adjakloe YA. Influence of leisure on sexual behaviour of young people with hearing and vision loss in Ghana. Ann Leisure Res. (2022):1–21. doi: 10.1080/11745398.2022.2089180
43. Wiggins J, Hepburn S, Rossiter R. Reducing harmful sexual behaviour in adolescents. Learn Disabil Pract. (2013) 16(8):16–23. doi: 10.7748/ldp2013.10.16.8.16.e1447
44. Rohleder P, Eide AH, Swartz L, Ranchod C, Schneider M, Schür C. Gender differences in HIV knowledge and unsafe sexual behaviours among disabled people in South Africa. Disabil Rehabil. (2012) 34(7):605–10. doi: 10.3109/09638288.2011.599915
Keywords: sexual behaviour, young people, disability, Uganda, northern Uganda
Citation: Bukuluki P, Wandiembe SP, Kisaakye P, Kiwujja V, Kajungu C, Mugwanya W, Nabakooza S and Anyii C (2023) The sexual behavior of young people living with a disability: Findings from the KAP study in Northern Uganda. Front. Reprod. Health 5:1065437. doi: 10.3389/frph.2023.1065437
Received: 9 October 2022; Accepted: 30 January 2023;
Published: 15 March 2023.
Edited by:
Janet Seeley, University of London, United KingdomReviewed by:
Emmanuel Ochola, St. Mary's Hospital Lacor, UgandaLangelihle Mlotshwa, University of the Witwatersrand, South Africa
© 2023 Bukuluki, Wandiembe, Kisaakye, Kiwujja, Kajungu, Mugwanya, Nabakooza and Anyii. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peter Kisaakye cGtpc2Fha3llQGdtYWlsLmNvbQ==
†ORCID Peter Kisaakye orcid.org/0000-0003-1859-2078
Specialty Section: This article was submitted to Adolescent Reproductive Health and Well-being, a section of the journal Frontiers in Reproductive Health
 Paul Bukuluki
Paul Bukuluki Symon Peter Wandiembe2
Symon Peter Wandiembe2 Peter Kisaakye
Peter Kisaakye