- 1Department of Health Sciences, University of Missouri, Columbia, MO, United States
- 2Department of Epidemiology and Biostatistics, Saint Louis University, St. Louis, MO, United States
- 3College for Health, Community and Policy, University of Texas at San Antonio, San Antonio, TX, United States
- 4Office of the Vice President for Research and Scholarly Activity, University of Health Sciences and Pharmacy, St. Louis, MO, United States
Background: Life course perspectives suggest that optimizing men's health before conception is requisite to equitably improve population health, an area of increasing public health focus. Although scholarship on the social determinants of health (SDOH) suggests that men's health and health behaviors do not occur in a vacuum, preconception health studies have not explicitly examined how these factors influence men's preconception health.
Objective: To identify latent classes of men's preconception health and the role of the SDOHs in predicting class membership.
Methods: Pooled data from the 2011–2019 male file of the National Survey of Family Growth were analyzed (n = 10,223). Latent class analysis (LCA) was used to identify distinct classes of men's preconception health. Eight manifest variables were used to fit latent class models. A classify-analyze approach was subsequently used to create a preconception health phenotype (PhP) outcome variable. SDOHs (exposure variable) were assessed in four domains (rural/urban residence, health access, socioeconomic status, and minority/immigrant status) to predict class membership. Survey-weighted multinomial regression models were fitted to examine the association between the exposure and the outcome.
Results: Three unique PhPs were identified (lowest risk (69%), substance users (22.9%), and sexual risk-takers (8.1%) from the LCA model. Health access, socioeconomic status, and minority/immigrant status were significant predictors of class membership but not rural/urban residence. Sexual risk takers were more likely to be uninsured (aOR: 1.25, 95% CI 1.02, 1.52), college-educated (aOR: 1.94 95% CI: 1.34, 2.79), and non-Hispanic Black (aOR: 1.99 95% CI: 1.55, 2.54) while substance users were more likely to have unstable employment (aOR: 1.23 95% CI:1.04, 1.45) and have a high school degree or higher (aOR 1.48 95% CI: 1.15, 1.90) than men in the lowest risk category.
Conclusion: Social determinants may impact men's preconception health in ways that are not conventionally understood. These findings raise important questions about how preconception health interventions should be created, tailored, and/or retooled. Specifically, studies that examine the sociocultural and political contexts underpinning the relationship between social class, masculinity, and men's preconception health are needed to provide nuanced insights on factors that shape these outcomes.
Background
Preconception health, defined as the health of women and men from pubarche to when they can have a child (1), is critical to improving population health across the life course. Most preconception health research disproportionately focuses on women with the greatest progress toward understanding the salience of men's preconception health made only in the past 10 years. These studies, which often focus on men's biological contributions to pregnancy, suggest that men's poor preconception health can impair fertility, and reduce semen quality and quantity (2–7). Less is known about the social factors that contribute to men's preconception health or how these factors impact the aggregation of preconception health indicators at the population level. In 2006, the Centers for Disease Control and Prevention (CDC) recommended ten surveillance indicators that could optimize the health of men preconceptionally. These indicators include: making a reproductive plan, preventing sexually transmitted diseases, quitting substance use, avoiding exposure to toxic substances, preventing infertility, maintaining a healthy weight, knowing family history, seeking help for violence, staying mentally healthy, and supporting partners (8).
Despite the awareness of these factors, optimizing preconception health is constrained by a host of factors including a) an inconsistent definition of the preconception period b) difficulties with making and sustaining behavior change without a clear understanding of the effects of contextual factors c) the persistently high prevalence of unintended pregnancies and d) persistent disparities in access to and utilization of health care resources (9–11). In addition to these factors, men face other unique challenges to optimizing their health preconceptionally. For instance, compared to women, men are more likely to engage in risky behaviors and less likely to modify these behaviors over time, less aware of the health behavior changes they need to make or how these behaviors can impact their offspring and are less inclined to seek health care (12–15).
Men's health conditions and health behaviors do not occur in a vacuum. Research has increasingly acknowledged the role of the social determinants of health - i.e., where people are born, live, play, learn, work, pray, and age - in creating and shaping health trajectories across the life course (16). Approximately 9% of men between the ages of 18 to 64 lived in poverty, 10.6% had less than a high school education, and 3.4% of men 20 years and over were unemployed in 2018 (17–19). Of these, racial and ethnic minorities accounted for the greater proportion of those at lower socioeconomic status [poverty rate: non-Hispanic Black (20.8%), Hispanics (17.6%), and foreign-born populations (13.8%)]. Among non-Hispanic Black and Hispanic males, those with less than a high school degree accounted for 11.7 and 29.3% respectively (17, 18). These minority populations often reported poorer health than their non-Hispanic White counterparts. Social factors intertwine with biological factors across the life course to shape health outcomes, which can adversely impact men's preconception health (20, 21). Given the stark social disparities that underlie men's health, studies examining how men's social environment influences their preconception health status with attention to rural/urban residence, health access, socioeconomic and minority/immigrant status are needed.
The objective of this study, therefore, was to utilize data from the National Survey of Family Growth (NSFG) to a) characterize latent clustering of men's preconception health at the population level and b) examine the relationship between the social determinants of health – rural/urban residence health access, socioeconomic status, and minority/immigrant status on these preconception health clusterings. Preconception risk factors such as risky sexual behaviors and substance use or chronic disease and poor nutrition often co-occur and are intertwined with social factors like socioeconomic status and racial/ethnic background (22, 23). Therefore, this study hypothesized that a) latent classes of men's preconception health will be observed and b) that men's preconception latent class membership will be predicted by the social determinants of health.
Materials and methods
Study participants and data source
Pooled data from the National Survey for Family Growth (NSFG) from 2011 to 2019 was used. The NSFG is a multi-stage, stratified, probability sample of the non-institutionalized U.S. population with in-person interviews conducted continuously at 2-year intervals. Details on data collection methods are reported elsewhere (24). Data were collected from both males and females ages 15–44 years (extended to 49 years in the 2015–2019 cycles) with data collection among men only beginning in 2002. Men included in this study were sexually experienced with a female, fecund, and had at least one fecund partner (25, 26). Those who also reported a current pregnant partner were excluded. These criteria were selected to identify those who at the time of data collection, were at risk of experiencing a pregnancy with their partner. Data were weighted to account for the complex survey design and provide estimates that are generalizable to the U.S male population.
Measures of men's preconception health indicators
Preconception health indicators are used in this study to capture men's health behaviors (e.g., substance use, condom use, and the number of sexual partners) and health status (e.g., body mass index), and these factors constitute a common definition of men's preconceptual health (8, 25, 26). These variables were measured with eight lifestyle variables – the number of sexual partners, sexual risk-taking behavior, condom use consistency, general health status, alcohol, and drug use, exposure to sexually transmitted infections (STI), and body mass index. These variables were further categorized into 5 domains - sexual behavior and awareness, general health status, substance use history, infectious disease status, and healthy weight. Only these five domains were assessed because of the availability of these variables in the NSFG data. These manifest variables were dichotomized following sensitivity analysis which showed no significant differences between the categories by sociodemographic characteristics. A detailed description of these variables is provided elsewhere (Authors (under review)– BLINDED FOR REVIEW).
Sexual risk behavior and awareness
Men's sexual risk behavior was measured using three variables that assessed the number of sexual partners, condom use, and STI/HIV risk-taking behavior. The first variable assessed the number of female partners a man had with the question “number of female partners in the last 12 months” and was recoded as 1= none or one female partner, and 2=more than one female partner (26). The question, “in the last 12 months, how often did you use a condom with your partner or partners” was used to measure condom use with response options 1=every time, 2=most, 3=about half, 4=some of the time, and 5=none of the time. These responses were recoded to measure condom use consistency where those who used condoms every time were coded as “1= used consistently” and those in categories 2 to 5 where coded as “2= inconsistent use to no use” (25). Sexually transmitted infection and HIV risk-taking behaviors were measured using five questions that asked whether a man (a) had sex with a female intravenous drug user, (b) gave money or drugs to a female for sex, (c) took money or drugs from a female for sex, (d) had sex with an HIV-positive female, and e) had any other sexual experience with another man with a binary (yes/no) response option. The first four questions inquired about past 12 months exposure whereas the fifth question inquired about lifetime exposure. These variables were used to create a single STI/HIV risk dummy variable. An experience with any of these STI/HIV risk-taking behaviors was coded as “yes” and no experience with any of these risk behaviors was coded as “no” (26).
General health status
Men's general health status was measured using the question “In general, how is your health?” with responses on a five-point scale ranging from excellent to poor. For analysis, this variable was recoded to a dummy variable 1= excellent to good and 2= fair to poor. Since only the 2015–2019 NSFG files measured high blood pressure and medication use among males, these variables were not used for this analysis. The general health status measure is the most commonly available measure of perceived overall health in national surveys and previously showed fair to good test-retest reliability in a population study (27).
Substance use history
Alcohol use was measured using three questions that assessed the frequency and quantity of alcohol use. These variables were recoded as “no drinking” if no alcohol use was reported in the past 12 months and 30 days, “low risk” if alcohol use was reported in the past 30 days but not at binge levels, “medium risk” if they binge drank <5 times in the past 30 days and “high risk” if they binge drank 5 or more times in the past 30 days (28). For analytical purposes, these risk categories were further recategorized into two risk groups: 1 = no to low-risk drinking and 2 = medium to high-risk drinking. Six questions on drug use inquired about marijuana, cocaine, crack, methamphetamine, and injection drug use in the past 12 months. These variables were recoded into a single “any drug use” category with a binary (yes/no) response. Since only the 2015–2019 NSFG questionnaire collected responses on smoking status, substance use history was measured using the respondent's alcohol and drug use history only.
Infectious disease status
Five questions were used to measure the presence or absence of sexually transmitted infections. These questions asked whether the respondent was told that they had gonorrhea, chlamydia, herpes, genital warts, and/or syphilis in the last 12 months. Responses to these questions were used to create a single STI status dummy variable with a binary (yes/no) response.
Body mass index
Body mass index is the most commonly used marker to ascertain healthy weight status (29). Body mass index was collected as a continuous variable and was categorized into 4 distinct groups – underweight (<18.0), normal weight (19 to <25), overweight (26 to <29), and obese (30 or higher)(30). These groups were recategorized further into a dichotomous variable “under to normal weight” and “overweight to obese.”
Social determinants of men's preconception health (predictor variables)
Rural/urban residence was measured using participants' place of residence with a 3-item response scale that was determined by the Metropolitan Statistical Area (1=Principal city of MSA, 2 = Other MSA, and 3 = not MSA) that we renamed as urban, suburban, and rural residence, respectively.
Health access was measured with the question “In the last 12 months was there any time that you did not have any health insurance or coverage?” with a binary (yes/no) response. Health care utilization was measured with two questions that assessed the type of doctor's visit (1 = routine physical exam, 2 = a physical exam for sports or work, 3 = a doctor visit when you were sick or hurt, 4 = did not have any visits to a doctor) and whether the doctor's visit was for reproductive health care. These variables were recoded as “reproductive wellness visit” if the participants went to the doctor and received reproductive health information, screening, exam, or treatment; “no reproductive wellness visit” if they went to the doctor for reasons other than for reproductive health and “no visit” if they did not have any doctor's visit in the past 12 months.
Socioeconomic factors were measured in three domains - employment consistency, poverty level, and educational attainment. Employment consistency was examined for the past 12-months and was categorized as “unemployed” if the respondent was not employed in the last 12 months, “unstable employment” if the respondent was employed for <12 months, and “stable employment” if the respondent was employed for 12 months. The federal poverty-to-income ratio (PIR) grouped into two subcategories - at or below 100% of family poverty level vs. above 100% of the family poverty level – was used to determine poverty level (31). Educational attainment was measured on a four-point scale - less than high school, high school, some college, and college degree or more.
Racial/ethnic belonging and immigration status were used as a proxy measure for social and cultural contexts. Race/ethnicity and immigration status can influence an individual's perceptions and/or experiences of the roles, resources, and relationships that society offers them through public and social institutions (32). These variables were used to denote the underlying cultural and normative beliefs and practices around preconception health. Immigration status was a dichotomized variable (i.e., immigrant vs. non-immigrant) utilized in this study to measure. Race/ethnicity was a four-level categorical variable - non-Hispanic White, non-Hispanic Black, Hispanic and Other.
Covariates
Covariates were sociodemographic characteristics that were independently associated with the exposure, outcome, or both variables and relevant to the literature. These included union type (married, separated/widowed/divorced, and never married), age (20 to 29 or 30 to 44years), number of children they ever fathered (none vs. one or more), and age of sexual debut (<15 or 15 and older). Survey year was also included as a covariate in the analysis to adjust for temporal changes.
Statistical analysis
Descriptive statistics including frequencies and bivariate analysis were used to describe the preconception health indicators and sociodemographic factors. A latent class analytical approach was used to characterize men's preconception health.
Latent class analysis
Logistic regression models with binary outcomes and multiple predictors are pervasive in the epidemiologic literature. These methods usually estimate the effect of one variable on an outcome after accounting for the effects of other variables in the model. This approach, often referred to as a variable-centered approach, precludes the opportunity to observe an underlying phenomenon that can provide a more nuanced understanding of precursors to health outcomes (33). As public health researchers increasingly focus on the interrelated factors that contribute to health outcomes over the life course, there is a need to employ statistical methods that utilize person-centered approaches to understand the complex relationships between these factors (5).
Latent variable models provide unique tools to analyze multivariate data (33). Latent variable models are methods applied to measure multidimensional constructs that are not easily measured by a single variable. Its principle lies in measuring unobserved phenomena that influence patterns of behavior or responses. It utilizes and captures the concordance and discordance in health behaviors within a person (34, 35). By using several observed variables to assess the underlying latent variable, we can reduce measurement errors (36).
Latent class analysis (LCA) is a latent variable framework that utilizes observed categorical data (such as alcohol use and drug use) to examine unobserved phenomena and identify subgroups of individuals in a set of two or more mutually exclusive and exhaustive latent classes based on multiple observed variables (36). This method was used because of the heterogeneity in preconception health behaviors and health conditions, interrelatedness between these risk factors, and the utility of this method to identify unique dimensions of preconception health from these variables. This method utilized indicators of preconception health (i.e., sexual risk behavior, general health status, substance use history, infectious disease status, and healthy weight status) as manifest variables to identify two or more dimensions of men's preconception health. The data were analyzed to determine the number of classes that best describe the patterns of response, the size of each class, and the probability of men responding in a certain way within those classes. An iterative maximum likelihood method specified two parameters: (1) the prevalence of latent classes (Gamma parameters) and (2) the item response probability representing the probability of endorsing a particular item within each class.
The LCA model was fitted starting with the 2-class model with a one-unit increment in the number of classes (3-, 4-, and 5-class models). The model of best fit was determined based on the Bayesian Information Criterion (BIC), entropy, mean posterior probabilities and class size (36), the interpretability of the solution, parsimony of the model, and relevance to the literature. The smaller BIC value indicates a better model fit. Entropy denotes how accurately a model defines a class with values closer to 1 considered ideal (35). Mean posterior probabilities are presented in a matrix with probabilities of membership in each class on the diagonal. Diagonals close to 1 (0.8 and above) and off-diagonals close to zero are considered more reliable models. Analyses were completed using the PROC LCA procedure in SAS 9.4 (37). The combined 8-year weight for the 2011–2019 period was applied to all analyses.
Using the posterior probabilities derived from the latent class models, a preconception health phenotype (PhP) variable was created, by applying a classify-analyze approach (35) and was subsequently used to fit multinomial logistic regression models to determine the relationship between PhP and the social determinants of health. Although “phenotype” is a biological term that refers to the physical expression of genes, it was used in this study to denote the set of observable characteristics that distinguished members within a specific latent class from those in other latent classes. Regression models estimated odds ratios with corresponding 95% CI. Independent crude and adjusted regression models were fitted for each social determinant and controlled for the covariates - union type, age, number of children ever fathered, age of sexual debut, and survey year. Statistical significance was placed at a p-value < 0.05 and 95% CIs not overlapping 1.0.
Results
Descriptive statistics
A total of 10,223 men were included in the final sample and the 53% majority were between 30 and 44 years. Most men were non-Hispanic White (57.4%), never married (55.4%), had some college education (32.0%) with stable employment (72.4%). The majority also had health insurance (71.1%) and reported good to excellent health (93.9%). In line with the objectives of this study, the pooled eight-year sample was used to identify the weighted frequencies of positive endorsement of the preconception risk manifest variables. Overall, more than 80% of men reported inconsistent to no condom use, 61.9% reported being overweight or obese and 18.6% reported having two or more sexual partners. About a third (32.2%) used drugs and 41.8% used alcohol at medium to high-risk levels (Table 1).
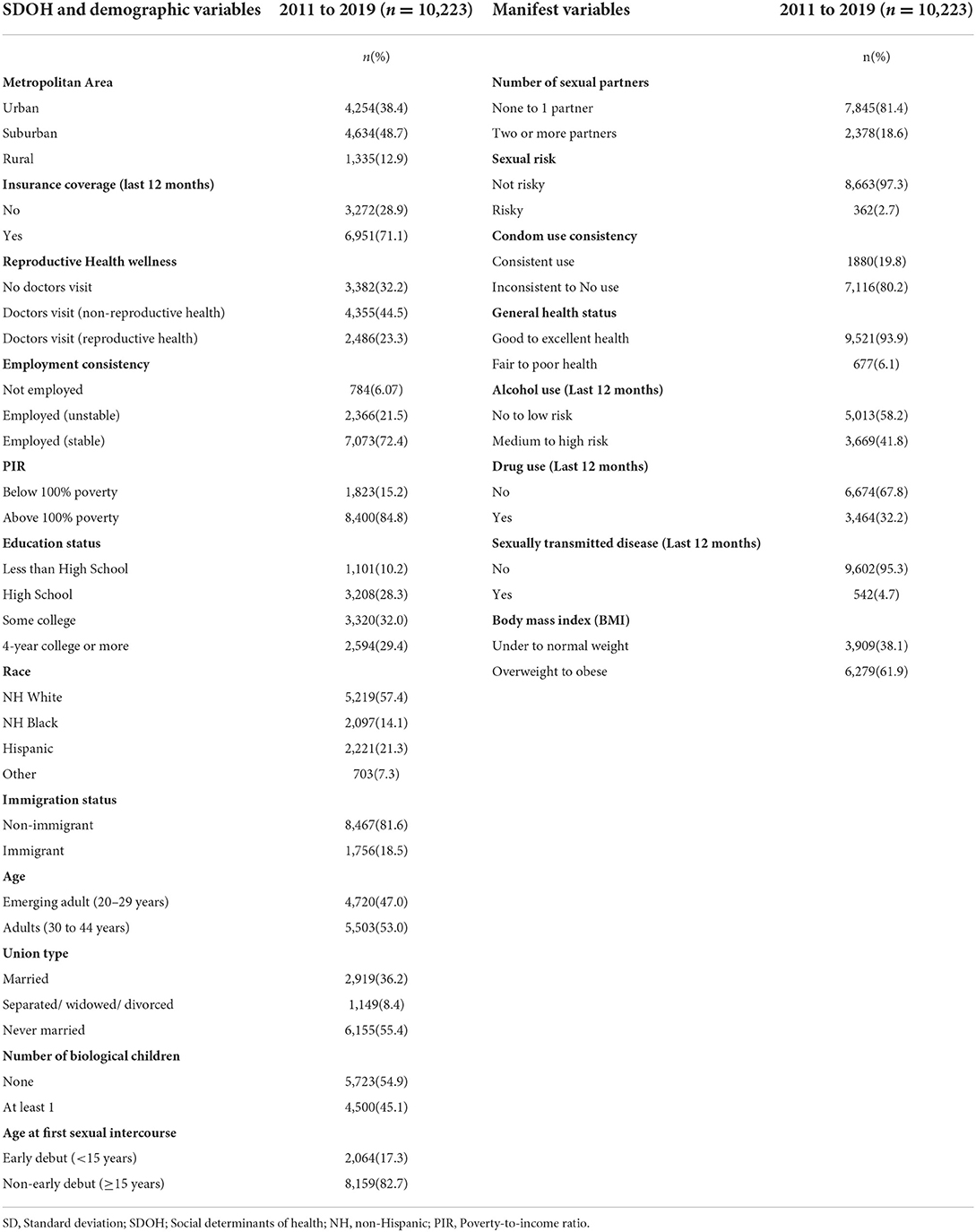
Table 1. Weighted descriptive statistics of National Survey of Family Growth male sample (2011–2019).
Latent classes of men's preconception health
The 3-class model provided the best fit across the eight preconception health manifest variables given 50 random start values, highest entropy values, and separation into distinct classes based on posterior probabilities of class membership (probability ranging from 0.84 to 0.97 within the class). Since a classify-analyze technique was applied to create a preconception health variable, the mean posterior probabilities for class membership needed to be high to reduce the effect of random error (Supplementary Tables S1A, B).
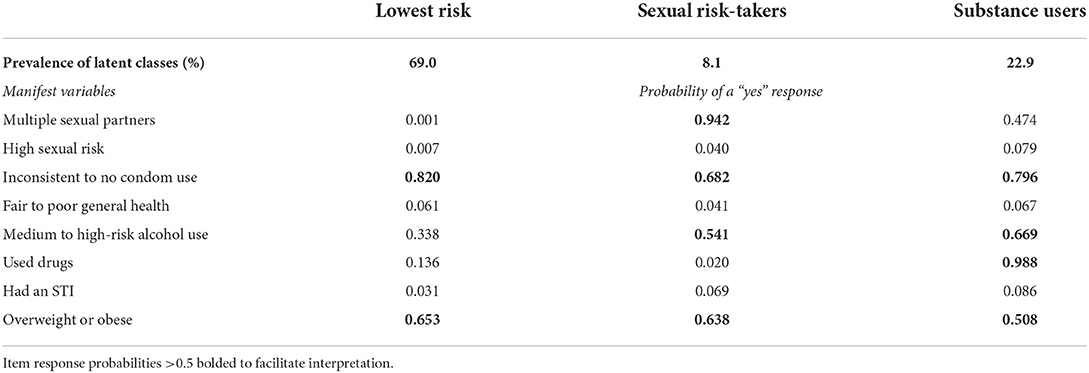
Table 2 represents the latent class probabilities (gamma estimates) i.e., the proportion of men expected to belong in each latent class, and the item response probabilities i.e., the proportion of men who positively endorsed these preconception health indicators within each class. Most men (69%) belonged to Class 1 “lowest risk group.” This class was characterized by a high endorsement probability of inconsistent /no condom use (82%) and overweight/obese (65.3%); all other prevalence estimates for each manifest variable were low. Class 2 “sexual risk-takers” had the lowest prevalence of latent classes (8.1%) and was characterized by high endorsement probability for multiple sexual partners (94.2%), inconsistent/no condom use (68.2%), medium/ high alcohol use (54.1%) and overweight/obese (63.8%). Approximately 23% of men belonged to Class 3 “substance users” and were characterized by high endorsement probability for inconsistent/no condom use (79.6%), medium/high-risk alcohol use (66.9%), drug use (98.8%), and overweight/obese (50.8%). Item response probabilities >0.50 were selected to characterize and facilitate interpretation of class membership. Because men across all three classes had a high probability of endorsing inconsistent condom use and overweight/obese, each additional class was subsequently labeled based on an additional preconception risk factor that characterized class membership.
Latent class structure and the social determinants of health
A description of the study sample, as they differed by the social determinants of health within their distinct preconception health groups, is provided in Table 3. More men in the “lowest risk” category lived in suburban areas (51%), whereas more men in the “sexual risk-takers” group lived in urban centers (44.3%). More men in the “substance users” category lived in suburban areas (47.3%). Across the PhP categories, most men were insured and had non-reproductive health visits to the doctor. Most men had stable employment, however, 30.7% of men in the “substance users” category had unstable employment, and 22.2% of “sexual risk-takers” also had unstable employment. Most men in the “lowest risk” category had a college degree or more (32.2%), whereas most substance users (36%) and sexual risk-takers (36%) had finished some college. Across all PhPs, most non-Hispanic White men belonged to the “substance users” category while the majority of non-Hispanic Black men belonged to the “sexual risk-takers” category. There was an even distribution of Hispanic men in the “lowest risk” and “sexual risk-takers” categories. Immigrants were more frequently in the “lowest risk” group compared to non-immigrants.
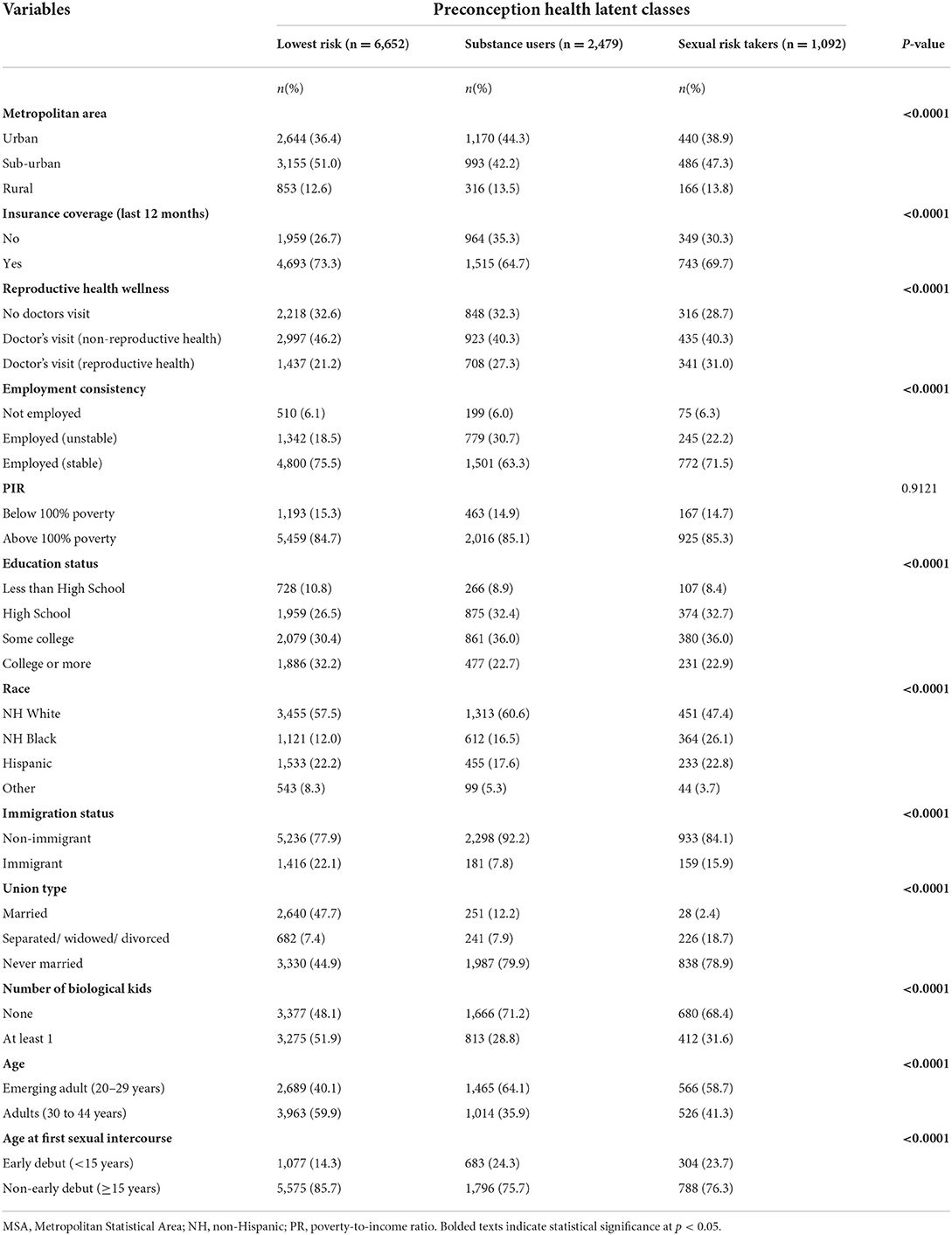
Table 3. Weighted distributions of social determinants of health by men's preconception health phenotypes.
Crude and adjusted multinomial regression models
Table 4 presents the result from the multinomial regression models fitted using the “lowest risk” level of the PhP variable as the outcome reference category to estimate the effects of the independent variables on the “sexual risk takers” and “substance user's” categories. All models were adjusted for the covariates: union type, number of biological children, participant age, and age of sexual debut. The survey year was further included in the models to account for any temporal variations in the exposures and outcome over time. For the current analysis, the regression models fitted did not control for all SDOHs in a single model, because it aimed to provide an initial examination of the relationship between each SDOH and men's preconception health. The limitations to this approach are noted in the discussion section.
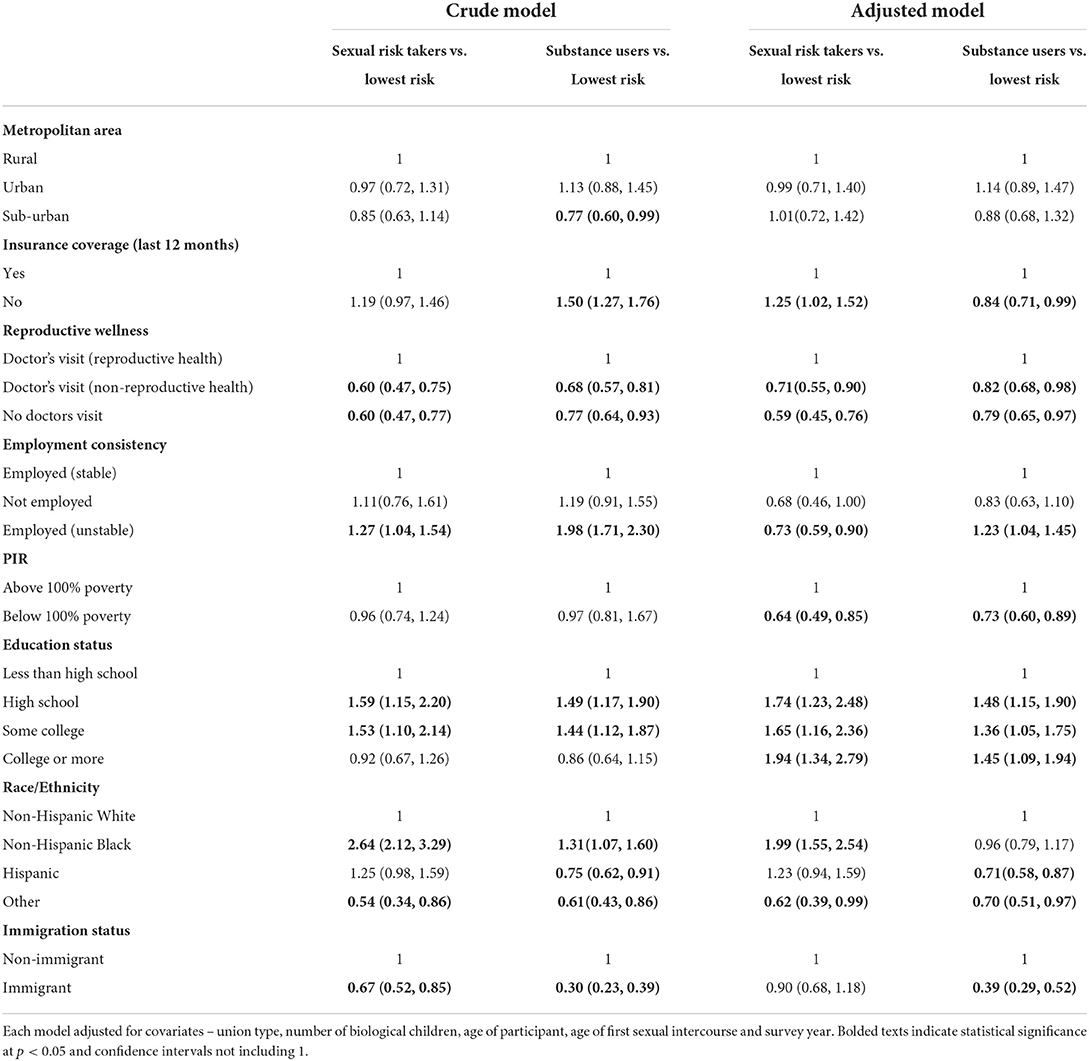
Table 4. Social determinants of health and correlates of men's preconception health latent class membership (N = 10,223).
Health access, socioeconomic status, and minority/immigrant status but not rural/urban residence were significant predictors of class membership. Men's access to health insurance coverage and type of health care service received were significant predictors of men's preconception health status. A lack of health insurance coverage was associated with 16% reduced odds for belonging to the “substance users” (aOR:0.84, 95%CI:0.71, 0.99) and 25% increased odds for belonging in the “sexual risk takers” category than in the “lowest risk” category compared to those who had insurance coverage (aOR: 1.25, 95%CI: 1.02, 1.52). Whereas, not having a doctor's visit or having a non-reproductive health visit were associated with reduced odds of belonging either to the sexual risk takers or substance users' categories than the lowest risk class.
Employment consistency, poverty level and educational status were associated with men's preconception health status. Compared to men with stable employment, employment instability was associated with reduced odds of belonging in the “sexual risk takers” category (aOR: 0.73, 95% CI: 0.59, 0.90) than the “lowest risk” category but increased odds for belonging in the “substance users” category (aOR: 1.23: 95% CI: 1.04, 1.45) than in the “lowest risk” category. Unemployed status did not have a statistically significant effect on preconception health class membership. Living below 100% of poverty level reduced the odds of belonging to the “sexual risk takers” and “substance users” categories by 36 and 27%, respectively (aOR: 0.64, 95%CI 0.49, 0.85; aOR: 0.73, 95% CI: 0.60, 0.89, respectively).
Education status was significantly associated with men's preconception health status. Compared to those with less than high school education, having a high school degree, some college or a college degree or more was associated with increased odds of belonging in the “sexual risk takers” category (aOR: 1.74, 95% CI: 1.23, 2.48; aOR: 1.65, 95% CI:1.16, 2.36; aOR: 1.94, 95% CI:1.34, 2.79, respectively) and the “substance users” category (aOR:1.48, 95% CI: 1.15, 1.90; aOR:1.36, 95% CI:1.05, 1.75 and aOR:1.45, 95% CI:1.09, 1.94, respectively).
Racial and ethnic background was also a significant predictor of preconception health status latent class belonging. Compared to their non-Hispanic White counterparts, being non-Hispanic Black was associated with 99% increased odds of belonging in the “sexual risk takers” category (aOR:1.99, 95% CI: 1.55, 2.54) than to the “lowest risk” category. Whereas, identifying as Hispanic was associated with 29% reduced odds of belonging in the “substance users” category (aOR:0.71; 95%CI: 0.58, 0.87) than in the “lowest risk” category. Immigration status was also a significant determinant of men's preconception health status. Compared to non-immigrants, immigrant status was associated with reduced odds of belonging in the “substance users” category (aOR = 0.39; 95% CI: 0.29, 0.52) than in the “lowest risk” category.
Given the changed direction in the odds ratios for the relationship between men's preconception health and insurance status, employment consistency, education status and race/ethnicity, a further assessment of confounders was conducted. Confounding effects were assessed using 10% change in the crude model compared to the adjusted model. This assessment showed all the covariates to be significant confounders except for the effect of age on the relationship between PhP and race/ethnicity (Supplementary Tables S2A, D). These confounding effects of the covariates observed in this study (i.e., age, age at sexual debut, union status etc.) suggest that future studies should also seek to examine the moderating effects of these factors by applying an intersectionality lens to better understand the pathways and mechanisms by which men's sociodemographic factors and SDOH's differentially impact preconception health.
Discussion
This population-level study utilized pooled cross-sectional data from the 2011–2019 NSFG dataset to identify latent classes of men's preconception health and examine associations between these latent classes and the social determinants of health – health access, socioeconomic status, and minority/immigrant status. Per the hypothesis of this study, three latent classes of men's preconception health were identified – lowest risk, substance users, and sexual risk-taker categories. These classes were predicted by all the social determinants of health domains except for men's rural/urban residence. The salience of these findings is discussed in the following paragraphs.
This study found that 22% of all men belonged to the “substance users” class and almost 10% belonged to the “sexual risk-takers.” While Class 1 “lowest risk” may not be “low risk” or “no risk,” compared to the other classes they bear the lowest risk given the constellation of preconception risk endorsement probabilities in the other latent classes. The latent classes observed in this study, specifically on substance use and risky sexual behaviors, may not be a function of “free choice.” These classes may signify a constellation of the individual, structural, contextual, and social factors, including hegemonic practices, that have intertwined over the life course to define masculinity and masculine behaviors. There is a gendered narrative to risk-taking and risk behaviors with men more likely to engage in risky sexual behaviors or substance use than women (38). Our study supports this narrative to the extent that distinct categories of men within both risk categories were explicitly identified. This finding, however, continues to raise questions about the structures that have created and continue to perpetuate masculinity as inherently risky. Given the risks for adverse health outcomes for men, the potential influence on their partners' health and well-being, and the well-documented negative outcomes for pregnancies and families (5, 15, 39), concerted efforts are needed to better engage men in pre-conceptional health care.
Rural/urban residence was not associated with men's preconception health status. This finding was contrary to a seminal study that used the NSFG data and found men's preconception health status to differ by rural/urban residence (26). This difference may be explained by Choiriyyah and colleagues' focus on men who needed preconception care (i.e., men intending a pregnancy). The current study provides additional insight by examining all fecund men between 20 to 44 years, independent of their fertility intentions. Because about 40% of men reported unintended pregnancies (40), this approach allowed the examination of risk exposure and background differences independent of pregnancy intentions. Rural/urban residence alone has well-acknowledged limitations in examining the nuances of residential context and its contributions to poorer health. Among men specifically, Thorpe et al. (41) argued for a place-based approach that examines the social environment in which men live to create a better understanding of the effect of place on men's health in general and on their preconception health specifically. More studies are needed that examine the social contexts, particularly neighborhood factors – such as social cohesion and racial composition - in which men live and plan to establish families.
Although most men in this study had health insurance, the majority, across all latent classes did not have a reproductive health visit. This finding is consistent with previous studies in which men were found to have increased access to health care through insurance coverage, yet did not necessarily translate into increased access to reproductive health services (12). Men may be uncomfortable discussing their reproductive health or see it as an inherently female domain, hence they are less likely to utilize these services (42). Health care providers may be implicitly biased toward providing reproductive health services for females rather than for males (43, 44). Providers' bias toward men's reproductive health screening may make them less inclined to inquire about men's reproductive health if their patients did not exhibit or report sexual risk-taking explicitly.
Men in high-risk preconception health categories may be more inclined to seek reproductive care compared to other men in lower risk categories which may explain the reduced odds of non-reproductive health utilization. Given the preconception health phenotypes of men in this study, identifying the barriers men face when seeking care, beyond access to health insurance, and finding ways to surmount these barriers should remain a public health priority. Several studies and reports have emphasized the value of effectively incorporating reproductive health screening into men's routine health care visits (12, 45, 46). By making intentional changes toward ensuring that each health care encounter, specifically with men between ages 20 to 44 years, provides an opportunity for reproductive wellness, practitioners can begin to improve men's health status pre-conceptionally.
This study found that men living below the poverty line were less likely to belong to the “sexual risk takers” or “substance users” categories which contradicts previous findings. Previous studies showed that men who have a higher education status were more likely to make health behavior changes preconceptionally (47). Specifically, Marcell et al. (14) did not find any association between poverty status and men's need for family planning. Increased socioeconomic status can reduce stress for men and be motivational toward starting a family (5). In some contexts, however, financial independence increases the chance for risky behaviors due to perceptions of what masculine behaviors should look like for those in higher income brackets (48). Substance use and sexual risk-taking may be more difficult to afford at the lower ends of socioeconomic status. Conversely, men with a high school degree and higher were more likely to belong to higher-risk latent classes.
Previous studies examining men's preconception health suggest that men with higher education status are more likely to make health behavior changes pre-conceptionally (47). Stressors related to achievement and career advancement may lead men to engage in more risky behaviors as a coping strategy (48). An alternative explanation could be the accumulation of wealth and negative masculine perceptions which may influence men to engage in risky behaviors as a sign of manhood or masculinity (38). More studies are needed to examine the contexts of men's masculinities and their influence on men's health behaviors. Similar findings were identified with employment status which suggests that changes in employment can influence the social class and masculinities pathway. Men often perceive themselves or have traditionally been socially constructed as “breadwinners” (49). Unstable employment can impact men's perceptions of themselves as providers, consequently increasing the likelihood of engaging in risky behaviors, including substance use (48).
Men's immigration status was associated with decreased odds of belonging to any of the high-risk preconception health phenotypes. This finding was expected given that many other studies that explored immigration status on health often indicate the “healthy immigrant” paradox, in which immigrants to the US are healthier overall than the general US population (50). An unexpected finding, however, was the increased odds for belonging to the sexual risk takers category than the substance user's category among immigrants. Since this study examined all immigrants, our understanding of immigrants' preconception health statuses at the intersection of race/ethnic belonging is limited. Further, given the context of acculturation, through which immigrants are thought to lose their health advantage over time, more studies are needed to explore – alongside racial/ethnic backgrounds – how acculturation in male populations impacts preconception health. Future studies will benefit from approaches that examine how long immigrants have lived in the US and variations in preconception health outcomes by racial/ethnic belonging.
Limitations and implications for future research
This study was limited by several factors. First, cross-sectional data were used, which limits any causal associations between the exposure and outcome. Second, only a few preconception risk factors were examined. For instance, measures on smoking, high blood pressure, and other preconception health indicators were not utilized because they were either not measured in the dataset or were inconsistently measured across the survey years utilized in this study. LCA is also sensitive to the variables included in the model (34). In other words, the preconception health phenotypes observed are subject to the manifest variables included in the analysis. While the NSFG data were well-suited to answer the questions posed by this study, preconception indicators could be grossly understated. Future studies will benefit from utilizing a broader range of preconception health indicators. Further, all variables utilized in this study were self-reported, which can introduce social desirability, reporting, and recall biases.
There were also limitations in terms of the social determinants of health measures that were utilized. For instance, immigration status was measured as a binary variable (i.e., whether a man was an immigrant or not) which is less informative than the length of time an immigrant had spent in the U.S. The length of time an immigrant spends in a host country has been associated with acculturation and stresses which can, in turn, impact preconception health. Future studies should consider using earlier years of NSFG data to explore these phenomena. Future studies should also pay attention to the upper stream (e.g., wealth and material resources) and downstream (e.g., social networks and intimate relationships) determinants as well as potential pathways in shaping men's preconception health. This study provides valuable insight into men's preconception health. The data source, however, does not capture measures of masculinity which limits our understanding of why we observed these results. Future studies will benefit from qualitatively examining these phenomena among men, specifically exploring the factors that contribute to reduced contraceptive use, perceptions of health, and the influence on fatherhood.
The regression models fitted in this study did not control for all SDOHs in a single model. For instance, race/ethnicity and immigration status which may affect the relationship between education and preconception health, was unobserved. Hence the association between SDOHs and men's preconception health may be limited by the variables included in each model. Emerging evidence from men's health studies however suggest that controlling for these effects such as age, education and race/ethnicity may prevent research from identifying the significant effects of these variables on health outcomes (51–53). The paucity of research on men's preconception health, and the effect of social conditions on these health states necessitated an initial examination on how SDOHs may impact men's preconception health.
Although the utilization of LCA was a novel approach to characterizing men's preconception health, it has limitations. LCA assigns class membership based on conditional probabilities, therefore a “true” class assignment is not guaranteed. In addition, a classify-analyze approach was used to create a PhP variable that hard-assigned men to each latent class. This approach is limited because it assumes a “true” latent class belonging (i.e., it ignores that latent class membership is a probability function). However, the 3-class model was selected as the LCA solution of choice after fitting the model using multiple starting values to achieve a global maximum likelihood and examining posterior probabilities. The BIC, entropy, parsimony of the model, and relevance to the literature were important considerations in selecting the final model. This model selection approaches minimized the risk of a poorly specified model given the >80% probability that men would belong in the classes identified in this study. This study showed strong homogeneity and high separation into latent classes.
Conclusion
Taken together, men's health access, socioeconomic status, and minority/immigrant status can collectively have meaningful impacts on preconception health, even though it may be through different pathways. In some contexts, manliness is expressed through men's ability to engage in risky behaviors, including substance use and sexual promiscuity, while also remaining financially successful as demonstrated by achievement in educational advancement and social mobility. This study underscores the need to explore more in-depth the relationship between social class, masculinity, and men's preconception health. This study suggests that other underlying factors nested in men's experiences of their social contexts influence men's preconception health, however, nationally representative datasets are not designed to measure these unique experiences. Studies that examine how men, on the cusp of fatherhood, view themselves, their roles as fathers, and their health status at this intersection can improve our knowledge of the socio-cultural processes that intertwine to shape men's preconception health.
Data availability statement
Publicly available datasets were analyzed in this study. The datasets generated and analyzed during the current study are available in the Harvard Dataverse repository doi: 10.7910/DVN/4X4IEG.
Ethics statement
This study was based on a publicly available anonymized database, and was exempt from ethical compliance.
Author contributions
AA: conceptualized and designed the study, analyzed data, and drafted the initial manuscript. RB: contributed to study conceptualization and design, analysis, and critically manuscript revisions. HX: contributed to data analysis and interpretation. PX: contributed to study design and critically revised the manuscript for intellectual content. All authors contributed to the article and approved the submitted version.
Funding
The open access publication cost was covered by the Society for Family Planning Research Fund (Grant Number: SFPRF14-ES2).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frph.2022.955018/full#supplementary-material
References
1. Centers for Disease Control and Prevention. Before pregnancy: Preconception health. 2020; Available online at: https://www.cdc.gov/preconception/overview.html (accessed May 22, 2022).
2. Almeling, Waggoner MR. More and less than equal: how men factor in the reproductive equation. Gend Soc. (2013) 27:4510. doi: 10.1177/0891243213484510
3. Frey KA, Navarro SM, Kotelchuck M, Lu MC. The clinical content of preconception care: preconception care for men. Am J Obstet Gynecol. (2008) 199(6 Suppl 2):S389-95. doi: 10.1016/j.ajog.2008.10.024
4. Han JY, Nava-Ocampo AA, Koren G. Unintended pregnancies and exposure to potential human teratogens. Birth Defects Res A Clin Mol Teratol. (2005) 73:245–8. doi: 10.1002/bdra.20132
5. Kotelchuck M, Lu M. Father's role in preconception health. Mat Child Health J. (2017) 21:2025–39. doi: 10.1007/s10995-017-2370-4
6. McPherson NO, Fullston T, Aitken RJ, Lane M. Paternal obesity, interventions, and mechanistic pathways to impaired health in offspring. Ann Nutr Metab. (2014) 64:231–8. doi: 10.1159/000365026
7. Montagnoli C, Ruggeri S, Cinelli G, Tozzi AE, Bovo C, Bortolus R, et al. Anything new about paternal contribution to reproductive outcomes? A review of the evidence. World J Men's Health. (2021) 39:626–44. doi: 10.5534/wjmh.200147
8. Centers for Disease Control and Prevention. Before Pregnancy. (2020) Available online at: https://www.cdc.gov/preconception/men.html
9. Finer LB, Zolna MR. Declines in Unintended Pregnancy in the United States, 2008–2011. N Engl J Med. (2016) 374:843–52. doi: 10.1056/NEJMsa1506575
10. Johnson K, Posner SF, Biermann J, Cordero JF, Atrash HK, Parker CS, et al. Recommendations to improve preconception health and health care–United States. A report of the CDC/ATSDR preconception care work group and the select panel on preconception care. MMWR Recomm Rep. (2006) 55:1–23. doi: 10.1037/e506902006-001
11. McQueen DV. Three challenges for the social determinants of health pursuit. Int J Public Health. (2009) 54:1. doi: 10.1007/s00038-008-8167-x
12. Besera G, Moskosky S, Pazol K, Fowler C, Warner L, Johnson DM, et al. Male attendance at title X family planning clinics - United States, 2003–2014. MMWR Morb Mortal Wkly Rep. (2016) 65:602–5. doi: 10.15585/mmwr.mm6523a3
13. Goossens J, Van Hecke A, Beeckman D, Verhaeghe S. The intention to make preconception lifestyle changes in men: associated socio-demographic and psychosocial factors. Midwifery. (2019) 73:8–16. doi: 10.1016/j.midw.2018.12.006
14. Marcell AV, Gibbs SE, Choiriyyah I, Sonenstein FL, Astone NM, Pleck JH, et al. National needs of family planning among US men aged 15 to 44 years. Am J Public Health. (2016) 106:733–9. doi: 10.2105/AJPH.2015.303037
15. O'Brien AP, Hurley J, Linsley P, McNeil KA, Fletcher R, Aitken JR. Men's preconception health: a primary health-care viewpoint. Am J Mens Health. (2018) 12:1575–81. doi: 10.1177/1557988318776513
16. HealthyPeople 2020. Social Determinants of Health. (2014) Available online at: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health.
17. National Center of Education Statistics, Educational Attainment. (2019). Available online at https://nces.ed.gov/programs/digest/d18/tables/dt18_104.10.asp
18. Semega J, Kollar M, Creamer J, Mohanty A. U.S. Census Bureau, Current Population Reports, P60-266(RV), Income and Poverty in the United States: 2018. Washington, DC: U.S. Government Printing Office (2020).
19. U.S. Bureau Labor Statistics. Unemployment Rate Unchanged at 3.6 percent in May 2019. 2019; Available online at: https://www.bls.gov/opub/ted/2019/unemployment-rate-unchanged-at-3-point-6-percent-in-may-2019.htm
20. Guzzo KB, Hayford SR. Pathways to parenthood in social and family contexts: decade in review, 2020. J Marr Fam. (2020) 82:117–44. doi: 10.1111/jomf.12618
21. Lu MC, Jones L, Bond MJ, Wright K, Pumpuang M, Maidenberg M, et al. Where is the Fin MCH? Father involvement in African American families. Ethnicity Dis. (2010) 20:49–61.
22. Parkes A, Waltenberger M, Mercer C, Johnson A, Wellings K, Mitchell K. Latent class analysis of sexual health markers among men and women participating in a British probability sample survey. BMC Public Health. (2020) 20:14. doi: 10.1186/s12889-019-7959-7
23. Toivonen KI, Oinonen KA, Duchene KM. Preconception health behaviours: a scoping review. Prev Med. (2017) 96:1–15. doi: 10.1016/j.ypmed.2016.11.022
24. National Survey of Family Growth. Public-use data file and documentation, 2015–2017 [internet]. 2018; Available online at: https://www.cdc.gov/nchs/nsfg/nsfg_2015_2017_puf.htm
25. Casey FE, Sonenstein FL, Astone NM, Pleck JH, Dariotis JK, Marcell AV. Family planning and preconception health among men in their mid-30s: developing indicators and describing need. Am J Mens Health. (2016) 10:59–67. doi: 10.1177/1557988314556670
26. Choiriyyah I, Sonenstein FL, Astone NM, Pleck JH, Dariotis JK, Marcell AV. Men aged 15–44 in need of pre-conception care. Matern Child Health J. (2015) 19:2358–65. doi: 10.1007/s10995-015-1753-7
27. Martikainen P, Aromaa A, Heliövaara M, Klaukka T, Knekt P, Maatela J, et al. Reliability of perceived health by sex and age. Soc Sci Med. (1999) 48:1117–22. doi: 10.1016/S0277-9536(98)00416-X
28. National Institute on Alcohol Abuse and Alcoholism. Drinking Levels Defined. (n.d.). Available online at: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking
29. Stephenson J, Heslehurst N, Hall J, Schoenaker DAJM, Hutchinson J, Cade JE, et al. Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. Lancet. (2018) 391:1830–41. doi: 10.1016/S0140-6736(18)30311-8
30. Centers for Disease Control and Prevention. Defining Adult Overweight and Obesity. (2020). Available online at: https://www.cdc.gov/obesity/adult/defining.html (accessed May 10, 2021).
31. US Census Bureau. How the Census Bureau Measures Poverty. (2019) Available online at: https://www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html
32. Eiroa-Orosa FJ. The sociocultural context of psychosocial interventions. Front Media SA. (2018) 3:1795. doi: 10.3389/978-2-88945-648-2
33. Bartholomew DJ, Knott M, Moustaki I. Latent Variable Models and Factor Analysis: A Unified Approach: Vol. 904. West Sussex: John Wiley & Sons. (2011). doi: 10.1002/9781119970583
34. Mollborn S, Lawrence EM, Saint Onge JM. Contributions and challenges in health lifestyles research. J Health Soc Behav. (2021) 62:388–403. doi: 10.1177/0022146521997813
35. Collins LM, Lanza ST. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences, Vol. 718. Hoboken, NJ: John Wiley & Sons (2009). Vol. 718. doi: 10.1002/9780470567333
36. Lanza S.T., Bray B.C., Collins L.M. An introduction to latent class and latent transition analysis. In: Schinka JA, Velicer WF, Weiner IB, editors. Handbook of Psychology: Research Methods in Psychology. Hoboken, NJ: John Wiley & Sons, Inc (2013). p. 691–716.
37. SAS Institute. Base SAS 9.4 Procedures Guide: Statistical Procedures. Cary, NC: SAS Institute Inc, (2013).
38. Griffith DM, Thorpe Jr RJ. Men's physical health and health behaviors. in APA Handbook of Men and Masculinities. Washington, DC: American Psychological Association. (2016). p. 709-722. doi: 10.1037/14594-032
39. Harlow A, Wesselink AK, Rothman KJ, Hatch EE, Wise LA. Male marijuana use and spontaneous abortion. Fertil Steril. (2019) 112:e3. doi: 10.1016/j.fertnstert.2019.07.1333
40. Lindberg LD, Kost K, Maddow-Zimet I. The role of men's childbearing intentions in father involvement. J Marr Fam. (2017) 79:44-59. doi: 10.1111/jomf.12377
41. Thorpe Jr RJ, Kennedy-Hendricks A, Griffith DM, Bruce MA, Coa K, Bell CN, et al. Race, social and environmental conditions, and health behaviors in men. Fam Commun Health. (2015) 38:297. doi: 10.1097/FCH.0000000000000078
42. Marcell AV, Morgan AR, Sanders R, Lunardi N, Pilgrim NA, Jennings JM, et al. The socioecology of sexual and reproductive health care use among young urban minority males. J Adolesc Health. (2017) 60:402–10. doi: 10.1016/j.jadohealth.2016.11.014
43. Robbins CL, Gavin L, Zapata LB, Carter MW, Lachance C, Mautone-Smith N, et al. Preconception care in publicly funded US clinics that provide family planning services. Am J Prev Med. (2016) 51:336–43. doi: 10.1016/j.amepre.2016.02.013
44. Short WR, Simone JM, Chakraborty R, Finocchario-Kessler S, and HIV Preconception Care Study Team. Addressing fertility desires and preconception care needs of men living with HIV: perspectives from HIV providers about addressing the reproductive needs of male patients. AIDS care. (2021) 33:80–5. doi: 10.1080/09540121.2020.1719965
45. Men's Health Caucus of the American Public Health Association. APHA Men's Health Caucus National Policy Agenda. Washington, D.C: Men's Health Caucus (MHC) (2011). p. 1-16.
46. Warner JN, Frey KA. The well-man visit: addressing a man's health to optimize pregnancy outcomes. J Am Board Family Med. (2013) 26:196–202. doi: 10.3122/jabfm.2013.02.120143
47. Shawe J, Patel D, Joy M, Howden B, Barrett G, Stephenson J. Preparation for fatherhood: a survey of men's preconception health knowledge and behaviour in England. PLoS ONE. (2019) 14:3897. doi: 10.1371/journal.pone.0213897
48. Liu WM, Colbow AJ, Rice AJ. Social class and masculinity. In: APA Handbook of Men and Masculinities. Washington, DC: American Psychological Association. (2016): p. 413-432. doi: 10.1037/14594-019
49. Robertson S, Kilvington-Dowd L. Masculinity and Men's Health Disparities. In: Men's Health Equity: A Handbook. Griffith DM, M.A. Bruce, R.J. Thorpe Jr (Editors). New York: Routledge. (2019). p. 10-26. doi: 10.4324/9781315167428-2
50. Daniel-Ulloa J, Ornelas IJ, Alejandra E. Cultural, Social, and Historical Factors Influencing Latino Men's Health. In: Men's Health Equity, Griffith DM, Bruce MA, Thorpe Jr RJ, (Editors): New York: Taylor & Francis (2019). p. 458. doi: 10.4324/9781315167428-28
51. Williams DR. The health of men: structured inequalities and opportunities. Am J Public Health. (2008) 98(9 Suppl):S150–7. doi: 10.2105/AJPH.98.Supplement_1.S150
52. Assari S. Combined racial and gender differences in the long-term predictive role of education on depressive symptoms and chronic medical conditions. J Racial Ethn Health Disparities. (2017) 4:385–96. doi: 10.1007/s40615-016-0239-7
53. Anderson V. Racism Derails Black Men's Health, Even as Education Levels Rise. in Kaiser Health News. KHN (2021). Available online at: https://khn.org/news/article/racism-derails-black-mens-health-even-as-education-levels-rise/
Keywords: preconception health, latent class analysis, social determinants, quantitative, men
Citation: Anakwe A, Xian H, BeLue R and Xaverius P (2022) Men's preconception health and the social determinants of health: What are we missing? Front. Reprod. Health 4:955018. doi: 10.3389/frph.2022.955018
Received: 27 May 2022; Accepted: 01 August 2022;
Published: 13 September 2022.
Edited by:
Michael J. Rovito, University of Central Florida, United StatesReviewed by:
Patrick Gordon, Leeds Teaching Hospitals NHS Trust, United KingdomXiao Yu, Michigan State University, United States
Copyright © 2022 Anakwe, Xian, BeLue and Xaverius. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adaobi Anakwe, YWdhdjIyQGhlYWx0aC5taXNzb3VyaS5lZHU=
 Adaobi Anakwe
Adaobi Anakwe Hong Xian2
Hong Xian2