- 1Department of Burn and Plastic Surgery, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 2Department of Stomatology, the 960th Hospital of People’s Liberation Army of China (PLA), Jinan, China
Background: Burns are a global health issue causing significant mortality and high medical costs. Non-pharmacological interventions such as music therapy and virtual reality (VR) therapy have shown potential in alleviating pain and anxiety in burn patients. This study systematically evaluates the impact of these interventions using a network meta-analysis.
Methods: A systematic review and network meta-analysis were conducted according to PRISMA 2020 guidelines and registered in PROSPERO (CRD42024566536). Searches in PubMed, Cochrane Library, Web of Science, and Embase up to November 22, 2023, identified randomized controlled trials (RCTs) involving music therapy or VR therapy in burn patients. The Cochrane Risk of Bias Tool (2.0) assessed study quality. Data were analyzed using StataMP-64 software.
Results: Seventeen RCTs with 1,119 burn patients were included. Both music therapy and VR therapy significantly reduced pain and anxiety compared to control groups. Music therapy was more effective for pain reduction (SUCRA: 85.4%), while VR therapy was superior for anxiety relief (SUCRA: 79.5%).
Conclusion: Music therapy and VR therapy effectively reduce pain and anxiety in burn patients. Integrating these interventions into burn care can enhance patient outcomes. Further research is needed to confirm these findings and optimize individualized treatment plans.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, PROSPERO (CRD42024566536).
1 Introduction
Burns are injuries to body tissue caused by exposure to various sources of heat, electricity, chemicals or radiation. These sources include hot liquids such as water, oils and soups, as well as steam, hot gases, flames, molten metals such as iron, aluminium and copper, and their liquid slags (1). Burns are a global public health problem, accounting for approximately 180,000 deaths each year (2, 3). Direct medical costs of burns can vary widely, but are typically high. In addition, indirect costs such as lost wages, long-term care for disability and psychological trauma, and invested family resources can further exacerbate the social and economic impact of burn injuries (2). Technological advances in burn injury treatment have led to declining mortality rates and extended life expectancy. However, previous studies have shown that burns can result in sequelae that reduce life satisfaction for the affected individual (4–7).
Burn patients frequently experience intense pain during treatments such as debridement and dressing changes, as well as during rehabilitation exercises (8). Patients often face emotional challenges, including anxiety and fear. Hence, it's essential that we bolster nursing interventions to alleviate patients’ suffering and anxiety, thereby enhancing therapeutic outcomes. These interventions are therefore very important in burn care and have been associated with improved survival rates in burn patients, a testament to advances in burn surgery (9, 10). Clinically, we usually divide interventions into drug interventions and non-drug interventions, and two common methods of the latter are music therapy and virtual reality (VR).While physicians are primarily responsible for administering pharmacological interventions, some non-pharmacological interventions can only be performed by nursing staff (11). Non-pharmacological interventions are important to the nursing process. A burn care guideline mentions non-pharmacological treatments, such as distraction, multimodal distraction (MMD), computer-based distraction, music-based distraction, virtual reality, hypnosis, and others (12).
The advantages of music therapy in the rehabilitation process of burn patients are mainly reflected in emotional support and psychological relaxation (13). It helps patients relieve anxiety and depression by providing positive emotional experiences and guided relaxation, while distracting attention from pain and reducing pain (14). Music therapy is personalized, that is, it can be customized according to the patient's preferences, is low-cost and easy to operate (15, 16).
Virtual reality (VR) therapy uses immersive technology and multi-sensory stimulation to provide a novel rehabilitation aid for burn patients (17). It distracts patients from pain and enhances a sense of control by creating an attractive virtual environment, and may be used to simulate real-life scenarios to help patients gradually adapt and overcome fear (18). VR therapy can also provide situational education and training, while allowing the medical team to evaluate the treatment effect through system-recorded data, bringing innovative treatment options to the field of burn rehabilitation (19). The advantages of virtual reality therapy in the rehabilitation process of burn patients are personalized customization, immersive experience, safe control and pleasure, which help improve patients’ rehabilitation effects and quality of life (20, 21).
Specifically, VR can cause interference not only visually but also auditorily, while music therapy mainly causes interference in the auditory sense (22). In addition to the different ways of inducing interference during the intervention process, there are also some differences in the implementation of music therapy and VR. On the one hand, music therapy is relatively cheaper and more practical, while VR requires expensive equipment and additional operating expenses (23). This makes music therapy more popular in many cases, especially for institutions and individuals who want to intervene on a limited budget (20). However, virtual reality technology can also provide burn patients with a pleasant and interesting rehabilitation experience, increase the fun and motivation of the rehabilitation process, and thus promote the patient's rehabilitation progress (24).
As two non-drug treatment methods, music therapy and virtual reality (VR) therapy provide different sensory stimulation and psychological intervention in the rehabilitation process of burn patients (13). Music therapy affects emotions and psychological states through auditory pathways, focusing on emotional expression and emotion regulation, and has the characteristics of low cost and easy popularization (25). It combines humanistic care and art therapy to provide emotional comfort and psychological relaxation for patients. VR therapy uses multiple pathways to work, including vision, hearing, etc. Through intuitive perception, control and exploration of the virtual environment, patients can participate more actively, improve their initiative, and help strengthen doctor-patient cooperation (24). Incorporating cutting-edge technology into healthcare, virtual reality (VR) treatment methods exemplify the advancement in scientific and technological fields. Moreover, by integrating with medical practices, VR therapy enhances patient outcomes and delivers additional advantages. Although the cost is relatively high, it shows great potential in personalized treatment (22).
These two methods were selected for comparison because they each represent different treatment concepts and technical applications, and can provide a comprehensive evaluation of treatment effects (26). The popularity and acceptability of music therapy combined with the innovation and personalization of VR therapy can provide a more comprehensive understanding of their mechanisms of action, advantages and limitations in burn rehabilitation (21, 27, 28). Through comparison, medical professionals can provide patients with more personalized and effective treatment plans, while exploring the possible complementarity and synergy of the two treatment methods to improve rehabilitation effects (25).
Although selected controlled clinical trials have shown that these two interventions provide some benefit, the results are not uniformly clear. Therefore, further demonstration is required to establish the role and value of these two interventions in the burn care process. The purpose of this paper is to use the method of reticulated Meta-analysis to collect relevant studies involving music therapy and VR interventions in the process of burn care. The aim is to systematically evaluate the impact of the two interventions on relieving pain, anxiety and other factors arising during the treatment process of burn patients. This will provide valuable decision-making basis for providing patients with comfortable treatment and improving their prognosis.
2 Methods
The study design was a systematic review that included a meta-analysis and was developed on the basis of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines (29). The study protocol was registered in the PROSPERO database (Registration number: CRD42024566536).
2.1 Search strategy
The search strategy was designed by two independent researchers, with a third researcher making decisions in cases of disagreement. Relevant articles were searched for supplements using computer searches of PubMed, Cochrane Library, Web of Science, and Embase databases from the date of construction to 22 November 2023, as appropriate. The search strategy was based on the following medical subject headings: “Burns”, “Music therapy”, and “Virtual Reality”. (Supplementary Table S1)
2.2 PICOS and inclusion/exclusion criteria for the study
Patients (P): Burn patients, regardless of burn area, age, race, gender, underlying disease, etc., regardless of treatment stage.
Intervention (I): “Music therapy” or “VR treatment”.
Comparison (C): Standard care without intervention.
Outcomes (O): Our primary outcomes of interest are changes in pain levels and symptoms of psychological conditions such as anxiety and relaxation. The secondary outcome is basic vital signs (including heart rate, respiratory rate and blood pressure).
Study Design (S): Only randomized controlled trials (RCTs) were included in this review.
Inclusion Criteria:(1) randomized controlled trial (RCT); (2) patients of any age, gender or ethnicity who had suffered burns, regardless of their severity, were included in the review;(3) with applied “Music therapy” or “VR treatment”; (4) with measured pain or anxiety outcomes.
Exclusion Criteria:(1) study types other than RCTs (quasi-randomized trials, non-randomized trials, observational studies, case reports, abstracts, or letters from the review.); (2) burn patients with hearing impairment, cognition impairment or communication disorder.
2.3 Outcomes
2.3.1 Primary outcomes
• Pain, which was measured with visual analogue scales, numerical rating scales or other validated instruments.
• Symptoms of psychological, including anxiety and relaxation.
2.3.2 Secondary outcome
• Basic vital signs (including heart rate, respiratory rate and blood pressure).
2.4 Literature screening and data extraction
Two researchers conducted an independent literature screening. They imported all retrieved literature into EndNote X9 software deleted duplicates, and initially screened literature by reading titles and abstracts. Finally, they screened literature that met the criteria by reading the full text based on the inclusion and exclusion criteria that had been previously developed. Relevant data such as author, publication year, participant characteristics, type of intervention, sample size, detailed information about intervention (like procedure, duration, frequency), type of scale were loaded onto a data extraction form. Decisions were made through discussion or with the involvement of a third researcher in cases of disagreement during the screening and data counting process.
2.5 Risk of bias assessment
The Cochrane Risk of Bias Tool (2.0) for RCTs was used to assess the quality of the included studies. The tool is based on five domains: bias in the randomization process, bias away from the intended intervention, bias in missing outcome data, bias in outcome measurement, and bias in selective reporting of results (30). The studies were categorised as “low-risk”, “high-risk” and “some concern”. Decisions were made through discussion or with the involvement of a third researcher in cases of disagreement during the literature quality assessment process.
2.6 Data synthesis and statistical analysis
We used StataMP-64 software to perform the Network Meta-Analysis. The data collected were summarised on the basis of continuous and dichotomous variables, and effect sizes were calculated using the mean difference (MD) for continuous variables and the odds ratio (OR) for dichotomous variables, both with 95% confidence intervals. The network evidence plot was created using the “Network map” command, which visualises the network relationships between different interventions. In addition, the area under the cumulative ranking curve (SUCRA) was used to rank and predict the strengths and weaknesses of each intervention, with the intervention with the greater area under the curve considered superior. Finally, to assess the presence of small sample effects and publication bias, we drew a funnel plot using the “netfunnel” command.
2.7 Ethical approval
As our research aggregates data from already published studies, we did not need to seek ethical approval for this meta-analysis. Each of the underlying studies adhered to the appropriate ethical standards and had received the required clearances from the responsible parties.
3 Results
3.1 Study and identification and selection
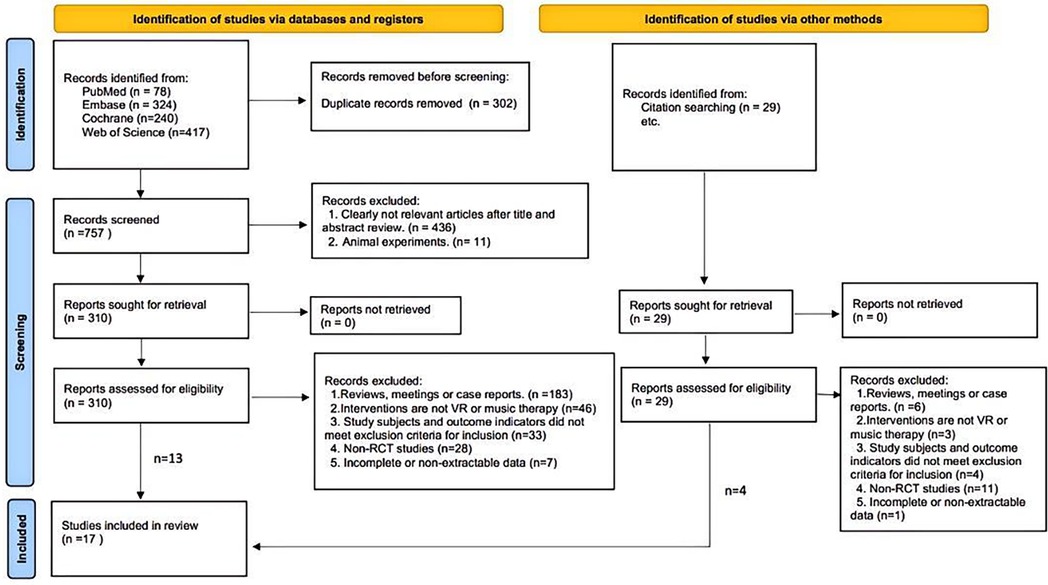
A total of 1059 documents were retrieved from the electronic database, and an additional 29 documents were manually searched. After eliminating duplicates, the remaining 786 documents were screened for titles and abstracts, and 447 documents were again excluded. The remaining 339 documents were read in full and 322 documents were again excluded (for reasons including non-randomized trials, meetings, case reports, incomplete data, and failure to meet the interventions or outcomes included in this review), leaving a final remaining 17 documents to be included in this study (Figure 1).
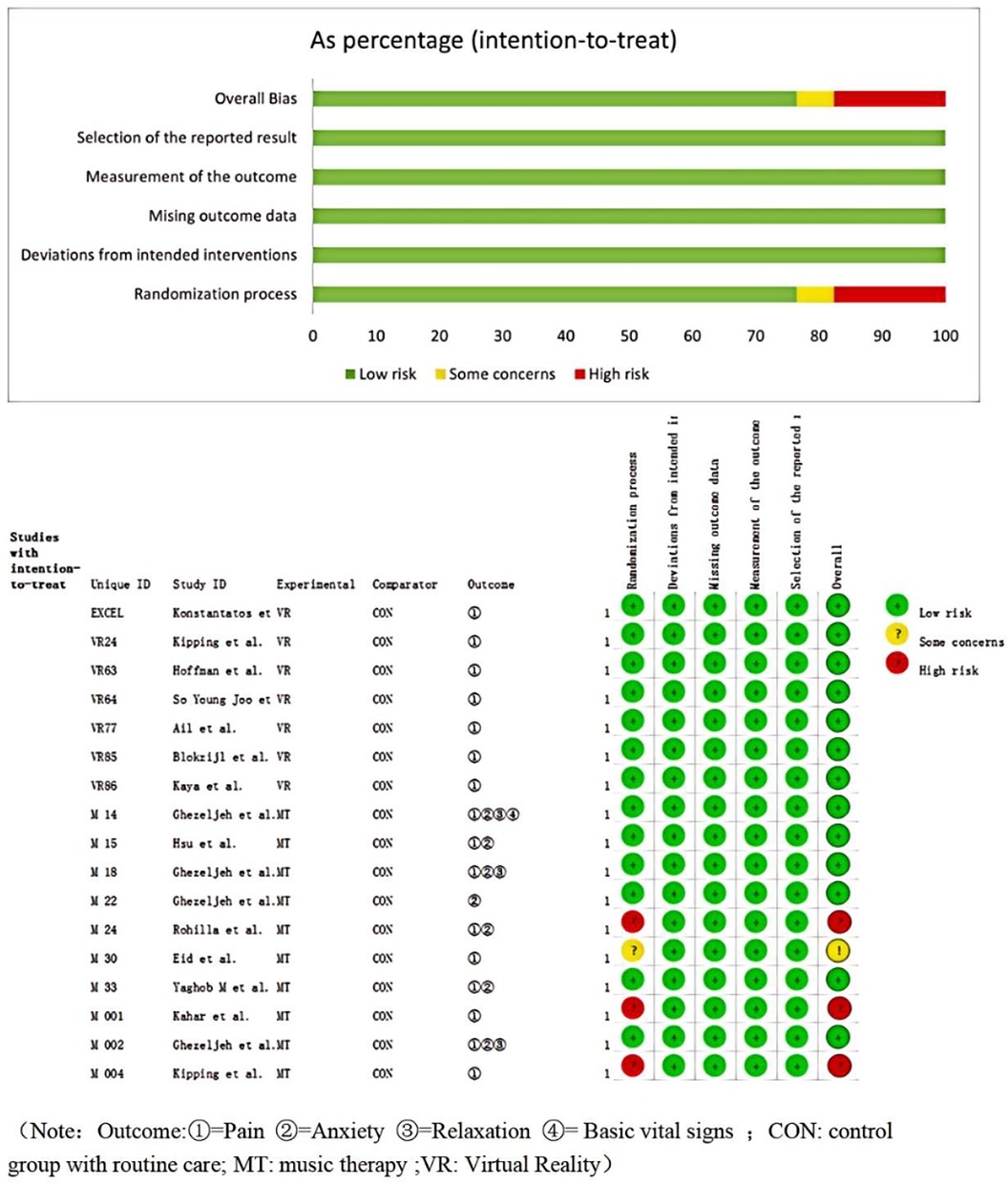
3.2 Quality assessment of the included studies
The assessment of the quality of the literature indicates a low risk of bias for both individual papers and the literature as a whole. The 17 relevant papers included in the study were of good quality and were considered acceptable for inclusion (Figure 2).
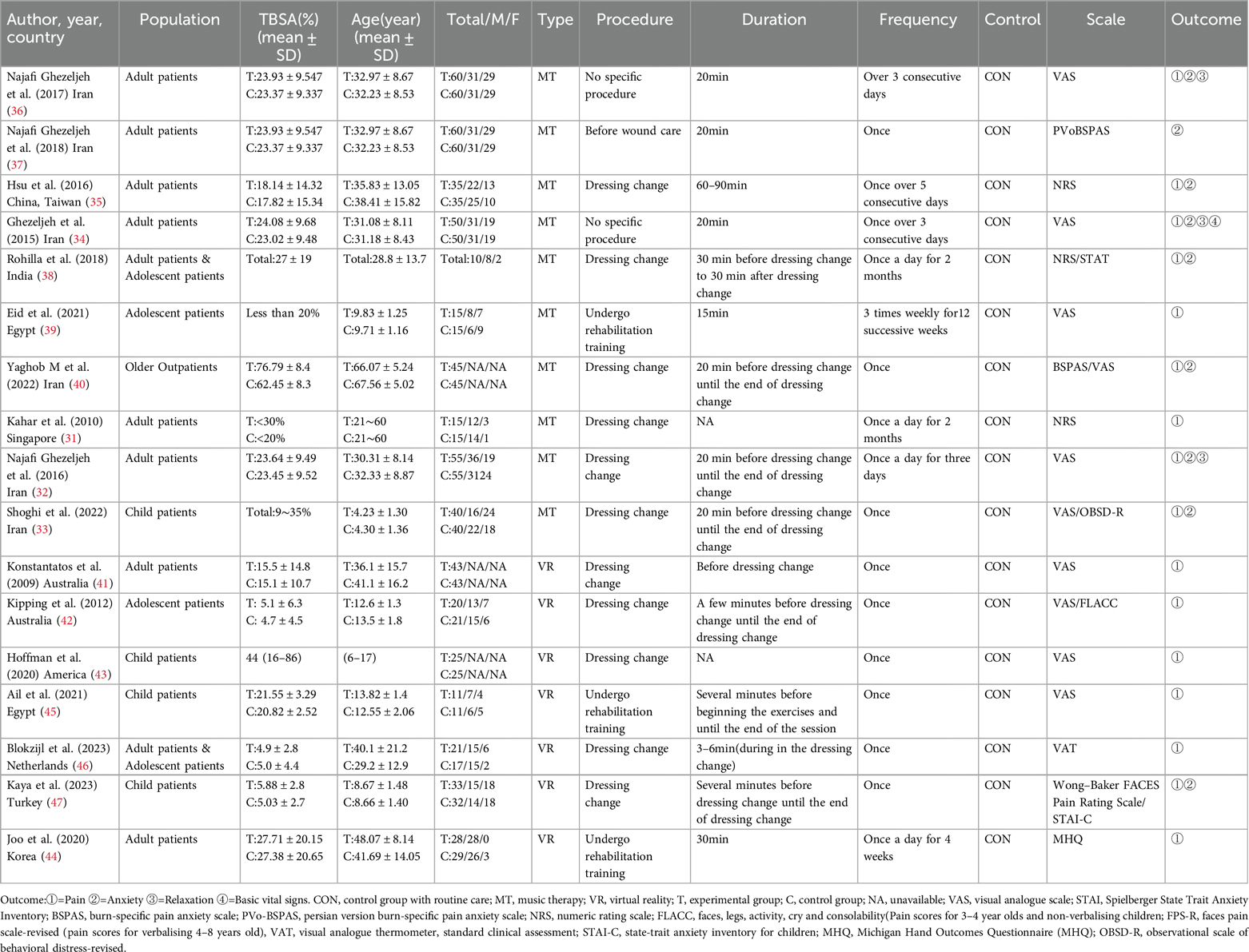
3.3 Characteristics of the included studies
In total, we included studies from 17 randomised controlled trials, which included 1119 burn patients (including inpatients and outpatients). Interventions in the control group included music therapy (ten studies) (31–40), and virtual reality therapy (seven studies) (41–47). Sixteen studies reported “pain” as an outcome indicator and nine studies reported “anxiety” as an outcome indicator. The characteristics of the included studies are shown in Table 1.
3.4 Network meta-analysis
3.4.1 Pain
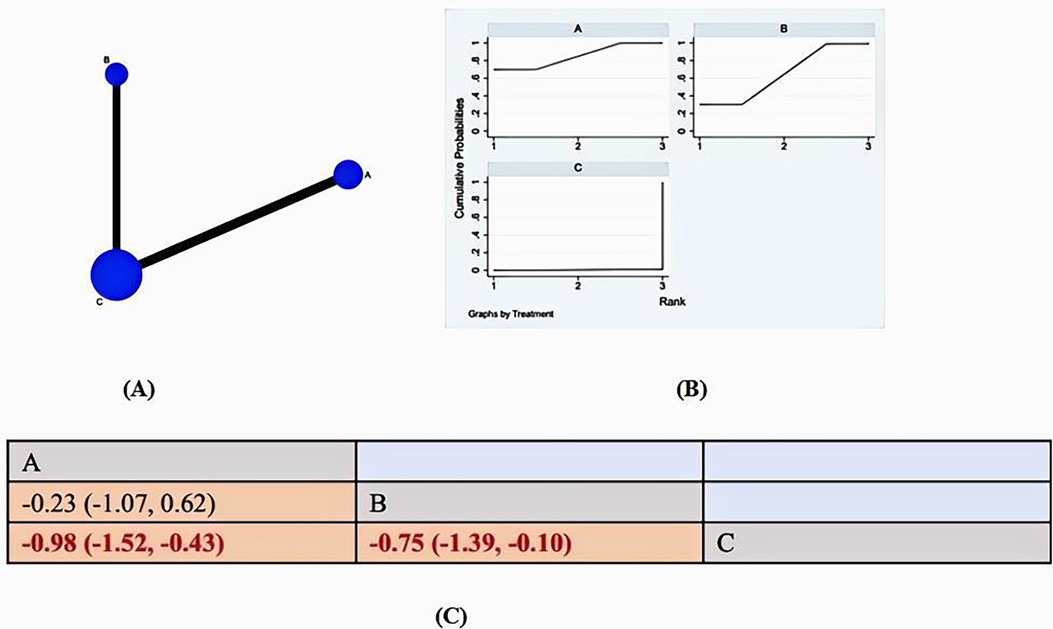
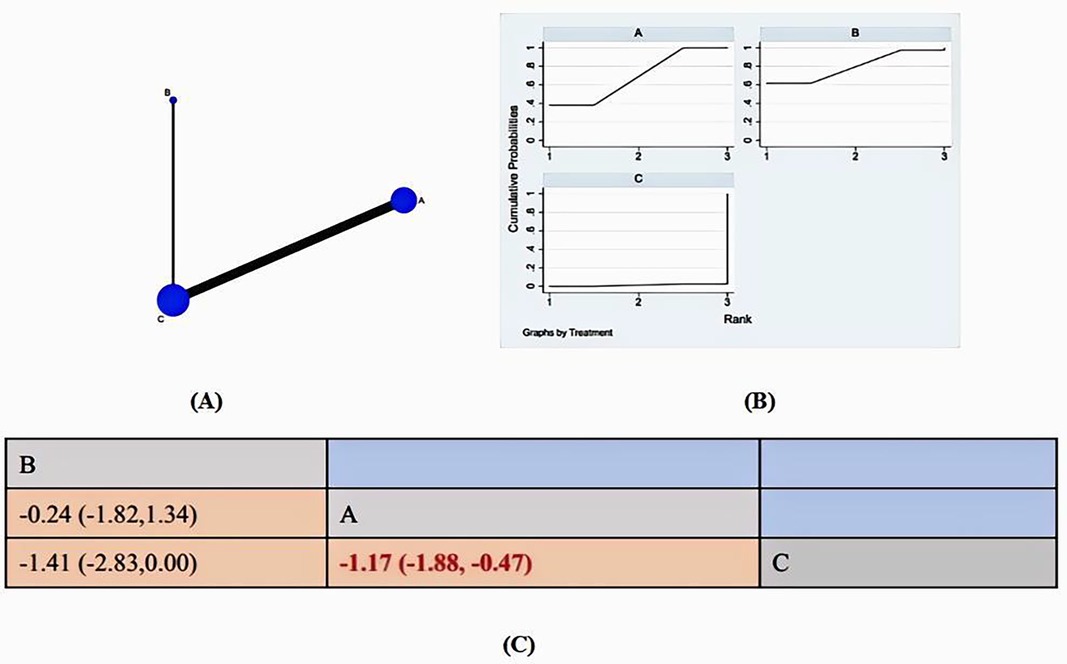
The literature review included 16 studies that reported on pain. Of these, 9 studies (31–36, 38–40) used music therapy as the intervention, while 7 studies (41–47) used virtual reality. All 16 reports provided data that was suitable for statistical analysis. Therefore, 16 studies with 1009 patients and 3 pharmacological treatments are reported. Figure 3A reports the network plot for the 2 treatment classes analyzed. The main results are reported in Figure 3B and Figure 3C: SUCRA and Pain League chart.
All of the p-values for the indirect and direct comparisons between all of the studies were tested for consistency and inconsistency, and all of the p-values were greater than 0.05, indicating that the effect of consistency between the studies was acceptable. (Supplementary Table S2)
The results of the network meta-analysis showed that relative to the control groups’ routine measures, music therapy [MD = 0.98, 95% CI = (1.52, 0.43)], VR [MD = 0.75, 95% CI = (−1.39, 0.10)] were superior to the control group in reducing burn patients’ pain, the details of which are shown in Figure 3C. Compared to the control group, both music therapy and VR were found to significantly reduce pain in burn patients. The SUCA results show the following probability-based ranking for the efficacy of the two interventions in reducing burn patients’ pain: MT(85.4%)>VR(64%)>CON (0.6%). Music therapy is considered the most effective method for reducing pain in burn victims.
3.4.2 Anxiety
The literature review included 9 studies that reported on pain. Of these, 8 studies (32–38, 40) used music therapy as the intervention, while 1studies (47) used virtual reality. All 9 reports provided data that was suitable for statistical analysis. Therefore, 9 studies with 865 patients and 2 treatments are reported. Figure 4A reports the network map for the 2 treatment classes analyzed. The main results are reported in Figures 4B,C: SUCRA and Anxiety League chart.
All of the p-values for the indirect and direct comparisons between all of the studies were tested for consistency and inconsistency, and all of the p-values were greater than 0.05, indicating that the effect of consistency between the studies was acceptable (Supplementary Table S2).
The network meta-analysis results indicate that music therapy [MD = −1.17, 95% CI = (−1.18, −0.47)] was more effective in reducing pain in burn patients than conventional measures in the control group. Although VR [MD = −1.41, 95% CI = (−2.83,0.00)] was included, the confidence interval was at the zero boundary, suggesting that it may be related to the inclusion of less relevant literature, the details of which are shown in Figure 4C. Compared to the control group, both music therapy and VR were found to significantly reduce anxiety in burn patients. The SUCA results show the following probability-based ranking for the efficacy of the two interventions in reducing burn patients’ anxiety: VR(79.5%)>MT(69.2%)>CON (1.3%). VR therapy is considered the most effective method for alleviating anxiety in burn victims.
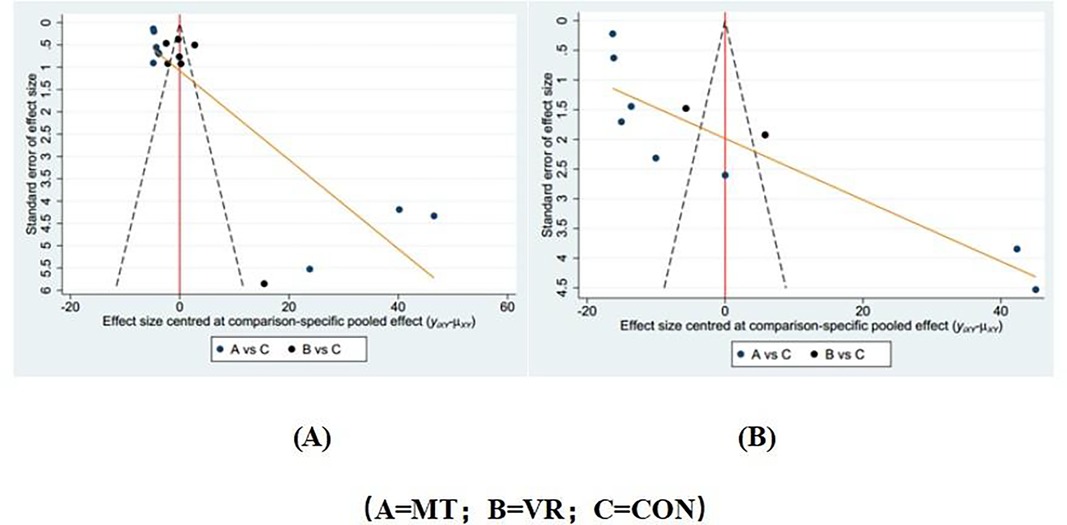
3.5 Publication bias test
Separate funnel plots were constructed for all outcome indicators to test for possible publication bias. Visual inspection of the funnel plots did not reveal any significant publication bias (48). Details as shown in Figure 5.
3.6 Other results
Analysis of other expected outcomes, such as relaxation and basic vital signs (including heart rate, respiratory rate and blood pressure) was unsuccessful due to lack of measurement or insufficient data in the manuscripts.
4 Discussion
4.1 Pain
Regarding pain reduction, our study (as shown in the SUCRA results) showed that both music therapy and VR were effective in relieving pain in burn patients, but music therapy had the advantage in significantly relieving pain, a result consistent with previous studies (34–36, 38–43, 45–47), These studies found that patients who received the intervention had significantly lower pain scores than those who did not receive such intervention. Although Konstantatos et al. 41 found that virtual therapy was an effective means of relieving patients’ pain, through our multifaceted comparison, we found that music therapy may be a more effective tool relative to virtual reality. Our study provides an evidence base for the effectiveness of non-pharmacological interventions such as VR and music therapy in managing pain.
Acute pain is a frequent challenge in healthcare, especially for burn patients, who endure significant pain with significant physical and psychological consequences. Currently, the main clinical strategy for treating this type of pain is pharmacologic analgesia (8). However, it is worth noting that long-term use of analgesics has certain side effects, and continued use will reduce the patient's tolerance to such drugs, thus reducing their efficacy. Considering the special characteristics of burn patients (who may frequently change dressings or undergo debridement surgery) (49), some methods with relatively minor side effects should be explored and found. Interventions such as music therapy and virtual reality also offer proven methods for relieving acute pain. Our study highlights the potential of these methods to provide effective analgesia while reducing the side effects and risks of medical treatments, providing patients with more treatment options and advocating for improved burn patient care. Towards more comprehensive, patient-centered pain management strategies.
4.2 Anxiety
According to SUCRA results, virtual reality technology is the most effective intervention for improving anxiety in burn patients. However, it is worth noting that the 95% confidence interval (CI) of the research results we obtained includes 0. The possible reason is that the sample size is small, so more subsequent RCTs are needed to strengthen the conclusions we obtained.
Our research aligns with earlier findings that show music can help patients feel less anxious and more relaxed (34–36, 38–40). While music has been looked at a lot, not many studies have explored how virtual reality can help burn patients deal with anxiety (41–43, 45–47). However, a handful of studies—including one with kids who have burn injuries—point to virtual reality being a good way to cut down on anxiety in pediatric patients (47). This backs up what we found in our research, showing that virtual reality could be a way to help ease anxiety for patients during their burn treatment.
Anxiety is often linked to the pain experienced during wound healing and after burns. Pain can also cause stress and anxiety, which in turn can worsen the pain (50). Our study contributes to the understanding of this complex relationship by showing that both music and virtual reality technology can serve as effective distractive interventions during dressing changes and treatment, thereby reducing pain and inducing relaxation (51).
4.3 Basic vital signs
Owing to the constraints posed by our modest sample size, we made the decision not to delve into an analysis of vital signs. Nonetheless, aligning with Najafi et al.'s research, it appears that music intervention could be more attuned to influencing respiratory rate specifically, rather than casting a wide net across all vital signs—including pulse rate, blood pressure (both systolic and diastolic), and a spectrum of other physiological metrics—reference 34. Hopefully, more data will be available in the future to support this conclusion, and perhaps these findings can serve as a basis for future discussions and research to explore the subtle effects of music on the physiological responses of burn patients.
5 Strengths and limitations
Our study conducted an extensive literature search and included as many relevant and eligible literature as possible. A total of 17 studies involving 1,119 patients were included, providing a relatively large sample size to reduce publication bias. The Cochrane Library Handbook was strictly followed to minimize relevant bias. In this study, we compared two common clinical non-drug treatments, music therapy and VR, to provide updated and comprehensive evidence-based recommendations.
However, based on basic research, our study has some limitations. This study only analyzed some outcome indicators, such as the length and frequency of intervention and the stage of intervention, and factors such as the patient's age, gender, and burn area were not included in the analysis. In addition, regarding the observation indicator of “anxiety”, there are relatively few literatures on virtual reality, and more RCTs are needed to support our conclusions.
Finally, readers should be cautious when interpreting our results. There are still few clinical studies that meet the inclusion and exclusion criteria, the sample size is insufficient, and the possibility of false positive rate is high. In addition, there is limited evidence for direct comparison of certain interventions. It is hoped that relevant clinical research will be expanded to improve the accuracy of the results.
6 Conclusions
In our study of the treatment process for burn patients, we recommend music therapy for the relief of pain and VR therapy for the relief of anxiety.
In the treatment of burn patients, it is important to consider not only the ranking results but also the absolute risk differences between interventions. Therefore, a comprehensive assessment should be conducted, taking into account the relevant conditions of the patients, in order to develop individualized treatment plans.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
WZ: Writing – original draft, Writing – review & editing, Conceptualization, Funding acquisition, Investigation, Resources, Software, Validation. XS: Writing – review & editing, Data curation, Formal Analysis, Project administration. LinZ: Writing – original draft, Conceptualization, Data curation, Software, Validation. LipZ: Writing – review & editing, Investigation, Methodology, Resources. HY: Writing – review & editing, Investigation, Methodology, Resources. SS: Writing – original draft, Writing – review & editing, Data curation, Methodology, Project administration, Supervision.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This article is supported by Shandong Provincial Natural Science Foundation, China (No. ZR2023MH061).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2024.1479833/full#supplementary-material
References
1. Gianotti L, Alexander JW, Nelson JL, Fukushima R, Pyles T, Chalk CL. Role of early enteral feeding and acute starvation on postburn bacterial translocation and host defense: prospective, randomized trials. Crit Care Med. (1994) 22(2):265–72. doi: 10.1097/00003246-199402000-00018
2. Smolle C, Cambiaso-Daniel J, Forbes AA, Wurzer P, Hundeshagen G, Branski LK, et al. Recent trends in burn epidemiology worldwide: a systematic review. Burns. (2017) 43(2):249–57. doi: 10.1016/j.burns.2016.08.013
3. Bateman RM, Sharpe MD, Jagger JE, Ellis CG, Solé-Violán J, López-Rodríguez M, et al. 36th International symposium on intensive care and emergency medicine: brussels, Belgium. 15–18 March 2016. Crit Ccare. (2016) 20(Suppl 2):94. doi: 10.1186/s13054-016-1208-6
4. Amtmann D, Bocell FD, McMullen K, Bamer AM, Johnson KL, Wiechman SA, et al. Satisfaction with life over time in people with burn injury: a national institute on disability, independent living, and rehabilitation research burn model system study. Arch Phys Med Rehabil. (2020) 101(1):S63–s70. doi: 10.1016/j.apmr.2017.09.119
5. Royse D, Badger K. Near-death experiences, posttraumatic growth, and life satisfaction among burn survivors. Soc Work Health Care. (2017) 56(3):155–68. doi: 10.1080/00981389.2016.1265627
6. Goverman J, Mathews K, Nadler D, Henderson E, McMullen K, Herndon D, et al. Satisfaction with life after burn: a burn model system national database study. Burns. (2016) 42(5):1067–73. doi: 10.1016/j.burns.2016.01.018
7. Takasi P, Falakdami A, Ghorbani Vajargah P, Mollaei A, Mehrabi H, Ghazanfari MJ, et al. Dissatisfaction or slight satisfaction with life in burn patients: a rising cause for concern of the world’s burn community. Burns. (2022) 48(8):2000–2. doi: 10.1016/j.burns.2022.09.007
8. Summer GJ, Puntillo KA, Miaskowski C, Green PG, Levine JD. Burn injury pain: the continuing challenge. J Pain. (2007) 8(7):533–48. doi: 10.1016/j.jpain.2007.02.426
9. Church D, Elsayed S, Reid O, Winston B, Lindsay R. Burn wound infections. Clin Microbiol Rev. (2006) 19(2):403–34. doi: 10.1128/CMR.19.2.403-434.2006
10. Sheridan RL, Tompkins RG. What’s new in burns and metabolism. J Am Coll Surg. (2004) 198(2):243–63. doi: 10.1016/j.jamcollsurg.2003.11.007
11. de Jong AE, Middelkoop E, Faber AW, Van Loey NE. Non-pharmacological nursing interventions for procedural pain relief in adults with burns: a systematic literature review. Burns. (2007) 33(7):811–27. doi: 10.1016/j.burns.2007.01.005
12. Shiferaw A, Mola S, Gashaw A, Sintayehu A. Evidence-based practical guideline for procedural pain management and sedation for burn pediatrics patients undergoing wound care procedures. Ann Med Surg. (2022) 83:104756. doi: 10.1016/j.amsu.2022.104756
13. Bradt J, Dileo C. Music interventions for mechanically ventilated patients. The Cochrane Database of Syst Rev. (2014) 12:Cd006902. doi: 10.1002/14651858.CD006902.pub3
14. Abdul Hamid MR, Mansor MB, Zainal Abidin MF. Music therapy for reducing anxiety in patients undergoing total knee replacement surgery under subarachnoid anesthesia. J Orthop Surg (Hong Kong). (2022) 30(2):10225536221122347. doi: 10.1177/10225536221122347
15. Mu PF, Chen YC, Cheng SC. The effectiveness of non-pharmacological pain management in relieving chronic pain for children and adolescents. JBI Libr Syst Rev. (2009) 7(34):1489–543. doi: 10.11124/01938924-200907340-00001
16. Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database Syst Rev. (2006) 2:Cd004843. doi: 10.1002/14651858.CD004843.pub2
17. Hoffman HG, Patterson DR, Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study. Clin J Pain. (2000) 16(3):244–50. doi: 10.1097/00002508-200009000-00010
18. Das DA, Grimmer KA, Sparnon AL, McRae SE, Thomas BH. The efficacy of playing a virtual reality game in modulating pain for children with acute burn injuries: a randomized controlled trial [ISRCTN87413556]. BMC Pediatr. (2005) 5(1):1. doi: 10.1186/1471-2431-5-1
19. Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev. (2010) 30(8):1011–8. doi: 10.1016/j.cpr.2010.07.001
20. Triberti S, Repetto C, Riva G.: psychological factors influencing the effectiveness of virtual reality-based analgesia: a systematic review. Cyberpsychol Behav Soc Netw. (2014) 17(6):335–45. doi: 10.1089/cyber.2014.0054
21. Li A, Montaño Z, Chen VJ, Gold JI.: virtual reality and pain management: current trends and future directions. Pain Manag. (2011) 1(2):147–57. doi: 10.2217/pmt.10.15
22. Garrett B, Taverner T, Gromala D, Tao G, Cordingley E, Sun C. Virtual reality clinical research: promises and challenges. JMIR Serious Games. (2018) 6(4):e10839. doi: 10.2196/10839
23. Guétin S, Soua B, Voiriot G, Picot MC, Hérisson C. The effect of music therapy on mood and anxiety-depression: an observational study in institutionalised patients with traumatic brain injury. Ann Phys Rehabil Med. (2009) 52(1):30–40. doi: 10.1016/j.annrmp.2008.08.009
24. Maples-Keller JL, Bunnell BE, Kim SJ, Rothbaum BO. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv Rev Psychiatry. (2017) 25(3):103–13. doi: 10.1097/HRP.0000000000000138
25. Chan MF, Wong ZY, Onishi H, Thayala NV. Effects of music on depression in older people: a randomised controlled trial. J Clin Nurs. (2012) 21(5-6):776–83. doi: 10.1111/j.1365-2702.2011.03954.x
26. Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect Psychol Sci. (2011) 6(1):21–37. doi: 10.1177/1745691610393527
27. Bradt J, Dileo C, Grocke D, Magill L. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev. (2011) 8:Cd006911. doi: 10.1002/14651858.CD006911.pub2
28. Maani CV, Hoffman HG, Fowler M, Maiers AJ, Gaylord KM, Desocio PA. Combining ketamine and virtual reality pain control during severe burn wound care: one military and one civilian patient. Pain Med. (2011) 12(4):673–8. doi: 10.1111/j.1526-4637.2011.01091.x
29. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
30. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
31. Noor Ahsikin BAK, Kanageswari S, Tay YB, Koh KX. A pilot study of the effects of music listening for pain relief among burns patients. Proc Singap Healthc. (2011) 20(3):162–73. doi: 10.1177/201010581102000305
32. Najafi Ghezeljeh T, Mohades Ardebili F, Rafii F, Haghani H. The effects of patient-preferred music on anticipatory anxiety, post-procedural burn pain and relaxation level. Eur J Integr Med. (2017) 9:141–7. doi: 10.1016/j.eujim.2016.12.004
33. Shoghi M, Aghtaii MZ, Kheradmand M. The effect of the active and passive distraction techniques on the burn children’s pain intensity and anxiety during dressing changes. J Nurs Midwifery Sci. (2022) 9(3):167–72. doi: 10.4103/jnms.jnms_139_21
34. Najafi Ghezeljeh T, Mohades Ardebili F, Rafii F, Haghani H. The effects of music intervention on background pain and anxiety in burn patients: randomized controlled clinical trial. J Burn Care Res. (2016) 37(4):226–34. doi: 10.1097/BCR.0000000000000266
35. Hsu KC, Chen LF, Hsiep PH. Effect of music intervention on burn patients’ pain and anxiety during dressing changes. Burns. (2016) 42(8):1789–96. doi: 10.1016/j.burns.2016.05.006
36. Najafi Ghezeljeh T, Mohades Ardebili F, Rafii F. The effects of massage and music on pain, anxiety and relaxation in burn patients: randomized controlled clinical trial. Burns. (2017) 43(5):1034–43. doi: 10.1016/j.burns.2017.01.011
37. Najafi Ghezeljeh T, Mohaddes Ardebili F. Comparing the effect of patients preferred music and Swedish massage on anticipatory anxiety in patients with burn injury: randomized controlled clinical trial. Complement Ther Clin Pract. (2018) 32:55–60. doi: 10.1016/j.ctcp.2018.05.002
38. Rohilla L, Agnihotri M, Trehan SK, Sharma RK, Ghai S. Effect of music therapy on pain perception, anxiety, and opioid use during dressing change among patients with burns in India: a quasi-experimental, cross-over pilot study. Ostomy Wound Manage. (2018) 64(10):40–6. doi: 10.25270/owm.2018.10.4046
39. Eid MM, Abdelbasset WK, Abdelaty FM, Ali ZA. Effect of physical therapy rehabilitation program combined with music on children with lower limb burns: a twelve-week randomized controlled study. Burns. (2021) 47(5):1146–52. doi: 10.1016/j.burns.2020.11.006
40. Moradipoor Y, Rejeh N, Heravi Karimooi M, Tadrisi SD, Dahmardehei M, Bahrami T, et al. Comparing auditory and visual distractions for reducing pain severity and pain anxiety in older outpatients with burn: a randomized controlled trial. Geriatrics (Basel). (2022) 7(3):54. doi: 10.3390/geriatrics7030054
41. Konstantatos AH, Angliss M, Costello V, Cleland H, Stafrace S. Predicting the effectiveness of virtual reality relaxation on pain and anxiety when added to PCA morphine in patients having burns dressings changes. Burns. (2009) 35(4):491–9. doi: 10.1016/j.burns.2008.08.017
42. Kipping B, Rodger S, Miller K, Kimble RM. Virtual reality for acute pain reduction in adolescents undergoing burn wound care: a prospective randomized controlled trial. Burns. (2012) 38(5):650–7. doi: 10.1016/j.burns.2011.11.010
43. Hoffman HG, Patterson DR, Rodriguez RA, Pena R, Beck W, Meyer WJ. Virtual reality analgesia for children with large severe burn wounds during burn wound debridement. Front Virtual Real. (2020) 1:602299. doi: 10.3389/frvir.2020.602299
44. Joo SY, Cho YS, Lee SY, Seok H, Seo CH. Effects of virtual reality-based rehabilitation on burned hands: a prospective, randomized, single-blind study. J Clin Med. (2020) 9(3):731. doi: 10.3390/jcm9030731
45. Ali RR, Selim AO, Abdel Ghafar MA, Abdelraouf OR, Ali OI. Virtual reality as a pain distractor during physical rehabilitation in pediatric burns. Burns. (2022) 48(2):303–8. doi: 10.1016/j.burns.2021.04.031
46. Blokzijl SJ, Lamberts KF, Nieuwenhuis MK, Beerthuizen G, Spikman JM. Virtual reality as pain relief in burn care: a pilot randomized controlled trial on the effectiveness on pain during multiple dressing changes. J Burn Care Res. (2023) 44(5):1125–33. doi: 10.1093/jbcr/irad039
47. Kaya M, Karaman Özlü Z. The effect of virtual reality on pain, anxiety, and fear during burn dressing in children: a randomized controlled study. Burns. (2023) 49(4):788–96. doi: 10.1016/j.burns.2022.06.001
48. Wallace BC, Schmid CH, Lau J, Trikalinos TA. Meta-Analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol. (2009) 9:80. doi: 10.1186/1471-2288-9-80
49. Bradt J, Dileo C, Potvin N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database Syst Rev. (2013) 2013(12):Cd006577. doi: 10.1002/14651858.CD006577.pub3
50. Tan X, Yowler CJ, Super DM, Fratianne RB. The efficacy of music therapy protocols for decreasing pain, anxiety, and muscle tension levels during burn dressing changes: a prospective randomized crossover trial. J Burn Care Res. (2010) 31(4):590–7. doi: 10.1097/BCR.0b013e3181e4d71b
Keywords: burn, VR, music therapy, pain, anxiety
Citation: Zhang W, Sui X, Zhang L, Zhang L, Yan H and Song S (2024) Effects of two non-drug interventions on pain and anxiety in the nursing process of burn patients: a literature review with meta-analysis. Front. Rehabil. Sci. 5:1479833. doi: 10.3389/fresc.2024.1479833
Received: 15 August 2024; Accepted: 14 October 2024;
Published: 29 October 2024.
Edited by:
Badii Amamou, University of Monastir, TunisiaReviewed by:
Amjed Ben Haouala, Hospital Fatuma Bourguiba Monastir, TunisiaDaniele Vieira Dantas, Federal University of Rio Grande do Norte, Brazil
Copyright: © 2024 Zhang, Sui, Zhang, Zhang, Yan and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuangshuang Song, c29uZ3NodWFuZzIwMjRAMTI2LmNvbQ==
 Wei Zhang
Wei Zhang Xiaona Sui2
Xiaona Sui2 Liping Zhang
Liping Zhang Shuangshuang Song
Shuangshuang Song