- 1Department of Physical Therapy, School of Health Professions, University of Alabama at Birmingham, Birmingham, AL, United States
- 2Department of Nutrition Sciences, School of Health Professions, University of Alabama at Birmingham, Birmingham, AL, United States
- 3Capstone College of Nursing, University of Alabama, Tuscaloosa, AL, United States
- 4Department of Physical Medicine and Rehabilitation, Heersink School of Medicine, University of Alabama at Birmingham, Birmingham, AL, United States
- 5School of Health Professions, University of Alabama at Birmingham, Birmingham, AL, United States
Virtual community-based programming for people with disabilities has become a popular method for advocating for health promotion, specifically exercise, for people with disabilities (PWD). Using theoretical frameworks to better understand the perspective of PWD who participate in virtual exercise programs allows strategies of implementation following completion of virtual exercise programs. The objective of this study was to examine the effect adherence had on perceptions, experiences, and post-program exercise maintenance in participants with disabilities. Eight qualitative interviews were conducted in highly adherent participants using the Social Cognitive Theory (SCT). Interviews were recorded on Zoom, transcribed using Microsoft 365, and analyzed using NVivo software. Data were analyzed by the primary author and an independent coder to increase rigor and reduce bias. Thirty-five unique codes were generated from transcribed interviews. Member-checking was employed to increase internal validity; 100% of participants agreed with the findings. Results demonstrate an overall positive experience in the virtual exercise program, noting specific facilitators (i.e., knowledgeable instructor, program provided equipment, etc.) and barriers (i.e., limited physical space at home to exercise, other participant's attitudes, etc.) of participating. Impressionably, 100% of participants maintained exercise following their time within the virtual exercise program.
Introduction
There are approximately one in eight individuals living with a physical or mobility disability in the United States (U.S.) as reported by the Centers for Disease Control and Prevention (CDC) (1, 2). Of this approximately 12% of the population, data suggest that unhealthy lifestyle concerns, such as obesity (41.6%), smoking (21.9%), heart diseases (9.6%), and diabetes (15.9%) are prominent and likely to occur up to 55% more within the disability demographic (1–3). Within the last decade, a significant shift has been made to prioritize health promotion and maintenance strategies specifically to and for people with disabilities (PWD) (3, 4). However, little to no data exists that illustrates the number of PWD who are recruited or informed about such programs or how many health promotion programs exist for PWD, although such programs are advertised through health agencies such as the CDC (4, 5). Several reports clearly outline health disparities and barriers to health enhancing behaviors encountered by PWD, such as lack of transportation, inaccessible facilities, and negative perceptions of healthcare providers (5–7). According to a recent retrospective surveillance survey that assessed behavioral risk factors among adults with mobility disabilities, approximately 40% of adults with mobility disabilities met one or both weekly physical activity guidelines of aerobic and muscle-strengthening exercises (7). Additionally, according to a recent global perspective analysis, PWD are 16%–62% less likely to meet physical activity guidelines and pose a higher risk of inactivity-related health problems when compared to people without disabilities (3, 8).
Nevertheless, with advocacy at the helm of health equity, diversity, and inclusion for PWD, recent literature has suggested an increase in accessible and inclusive opportunities for PWD (9). For example, community programs are peak areas of interest among participant involvement and research reporting. Community programs such as holistic health and wellness programs, support groups, and sports teams are becoming more popular and have several benefits (10–13). First, community programs offer inclusivity for a myriad of people, health conditions, geographic locations, demographics, and many more variables. Second, as a result of the Covid-19 pandemic, community programs for PWD and older adults are being offered through virtual platforms, such as Zoom (14–16). Finally, virtual participation has been found to alleviate barriers of participation such as travel and time constraints, cost to participate, environmental inaccessibility, and access to knowledgeable personnel (17).
Community programs are, however, benchmarked by success of the program itself, which is why adherence of participants is imperative (15, 16). For community programs delivered virtually to PWD, adherence and retention within the programs lead to successful participation, which leads to lifestyle implementation, leading ultimately to healthy decision-making behaviors (17, 18). One particular area of focus among virtually delivered community programs for PWD is exercise. Exercise is an important activity especially for people living with physical disabilities or mobility impairments, or for people with secondary or chronic health conditions (8, 14, 19–24). The literature consistently reports that exercise can serve as both preventative and restorative including alleviation of symptoms associated with inflammation, fatigue, poor nutrition, loneliness, depression, and sleep disorders (15, 16, 20, 25). Exercise may also produce mental and emotional benefits such as healthy decision-making behaviors that promote a generally healthier lifestyle (20–23). Therefore, virtual exercise programs overcome community barriers to participation and make it easier to participate in these online programs.
Several virtual exercise analyses for PWD confirm the benefits of performing physical activity and exercise within a comfortable setting, such as the participant's home. A recent study analyzed individuals with traumatic brain injury (TBI) in a 3-month tailored exercise program comparing two groups of participants’ adherence and compliance with an asynchronous (without trainer or exercise personnel) prescription program. One group (n = 10) performed aerobic exercises and the other group (n = 10) performed stretching and toning exercises. All participants completed the program, and the group that performed aerobic exercise maintained cardiorespiratory endurance compared to the group that performed stretching exercises (26). Another virtual exercise program evaluated people with Parkinson Disease (PD) who performed virtual physical and cognitive exercises with a trainer on Zoom twice each week for 16 weeks. Participants attended 81% of sessions and expressed their satisfaction and perceived benefits such as the program being useful for their current health management strategy (27). A third study examined the feasibility among individuals with spinal cord injury (SCI) during a home exercise program with a virtual trainer and an upper-body ergometer, where participants performed 30–45 min of exercise, three days/week for eight weeks. There was 100% adherence, increased aerobic capacity, higher volume of physical activity, and improved satisfaction with life. Participants also expressed the at-home intervention as advantageous for overcoming barriers to exercise typically experienced at a fitness facility (28). These studies provide evidence that virtual exercise programs are beneficial for health outcomes in PWD.
To further explore virtual interventions targeting health behavior among PWD, we conducted a qualitative study using Social Cognitive Theory (SCT) as our framework to describe perceptions and experiences of participants who joined a virtual holistic wellness program that included exercise for PWD. To explore relationships between exercise adherence and health behavior, we identified high-adherent participants from the exercise portion of the wellness program to interview regarding their perceptions and experiences of the program. This qualitative study aimed to answer the following question: Does high-adherence within a virtually delivered program impact participants’ desire to implement learned physical activity strategies into their daily lives once the program is over? To address this question, we examined the effect adherence had on perceptions, experiences, and post-program exercise maintenance in participants with disabilities through qualitative evaluation.
Methods
MENTOR program
MENTOR (Mindfulness, Exercise, Nutrition to Optimize Resilience) is a virtual community-based program offered to people with a range of disabilities, ages, ethnicities, and geographic locations. The MENTOR program is a free, completely online-delivered program for participants across the United States who have an existing disability or a recent diagnosis. MENTOR does not require a pre-requisite of engaging in mindfulness, exercise, or nutrition, rather the program focuses on teaching participants these strategies using a “from-the-ground-up” approach. To jumpstart engagement, participants receive a wellness box mailed to their physical address with all equipment needed to fully participate (i.e., wrist weights, resistance bands, notebook, yoga mat, etc.) The program is comprised of 3 core wellness domains, mindfulness, exercise, and nutrition, which teach self-care strategies. Each week, participants meet online via Zoom in a group class format to interact with a trained instructor to discuss elements of health and wellness. Class instructors include mindfulness, exercise, and nutrition coaches who have all been trained and certified in disability-specific content and motivational interviewing techniques to foster a inclusive and accessible online environment.
Mindfulness and nutrition have one 60-min class per week each across eight weeks, while exercise has two 60-min classes per week across eight weeks. The primary goal of mindfulness classes are to educate participants on how to focus on living in the present moment while learning coping strategies such as breathwork and learning how to manage stress, anxiety, nerves, etc. among others. Nutrition classes, taught by registered dieticians, focus on educating participants about proper nutrition and creating a healthy foundation for mindful eating. Exercise classes have live-instruction where the instructor exercises alongside participants, adapts movements in real-time, and educates about how movement positively impacts both the body and the mind. Participants create mindfulness, nutrition, and exercise goals and with direct access from their participant portal can set up one-on-one appointments with instructors, re-watch recorded sessions, and document their personal goals, milestones achieved, and experiences about their time within MENTOR.
In this program, participants are tasked with attending as many classes as they are able within their timeframe of participation and engaging with one another and their coaches. By the end of the eight-week program, participants are provided a plethora of information about how to practice better self-care within the areas of mindfulness, exercise, and nutrition. More information about the MENTOR program may be found online (https://www.nchpadconnect.org/mentor/) and elsewhere in literature (29–32).
Sampling procedures and participants
The purpose of this study was to understand the factors that influence adherence to a virtual exercise program, MENTOR, for people with disabilities. Therefore, only the exercise class's adherence was accounted for when sampling for participants. It is important to note that participants who completed exercise could have also completed mindfulness and nutrition classes; however, only their completion and adherence of exercise classes were considered to remain within the scope of the purpose of the study. The primary researcher identified 419 participants who completed the virtual exercise classes between February 2022 through December 2023. Adherence was measured by calculating the number of classes each participant attended and dividing by sixteen, the total number of classes offered each eight-week wave of the program. Non-adherence was defined as attending zero virtual exercise classes, low adherence was defined as attending between 1 and 6 virtual exercise classes, moderate adherence was defined as attending between 7 and 11 virtual exercise classes, and high adherence was defined as attending 12 or more virtual exercise classes. Of 419 participants, 20% were non-adherers, 29% were low adherers, 18% were moderate adherers, and 33% were high adherers.
Purposive sampling was used to recruit high adherers. A complete list of high adherers was organized and randomized for interview selection. Participants were called to be informed about the purpose of the study and to schedule an interview upon interest. Due to the large time frame of program delivery (February 2022 to December 2023), participants were between seven and twenty-two months of having completed MENTOR.
Conceptual framework
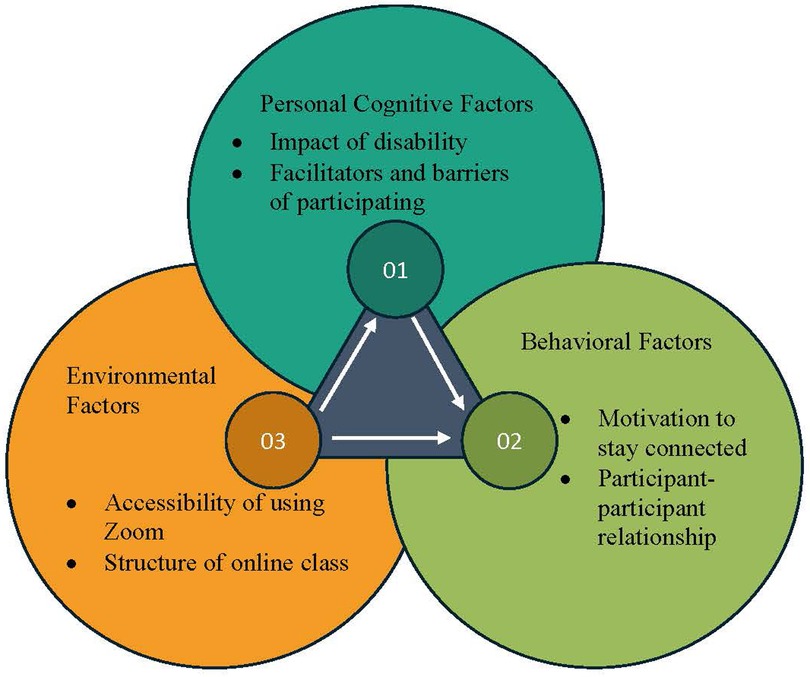
A behavioral explorative strategy which has been widely used in exercise programs targeting individuals with disabilities is the Social Cognitive Theory (SCT) (20–23). SCT is the interplay between behavioral decisions among PWD and strategies for lifestyle implementation. Using SCT allows us to better comprehend participant behaviors, health-related decisions, and programmatic strategies that need improving. SCT uses determinants of personal cognitive factors, socioenvironmental factors, and behavioral factors to determine outcome expectations and behavioral components such as self-efficacy and self-regulatory strategies. Both are major predictors of physical activity and strategies of change, as determined by Dr. Albert Bandura, the creator of SCT (20–23).
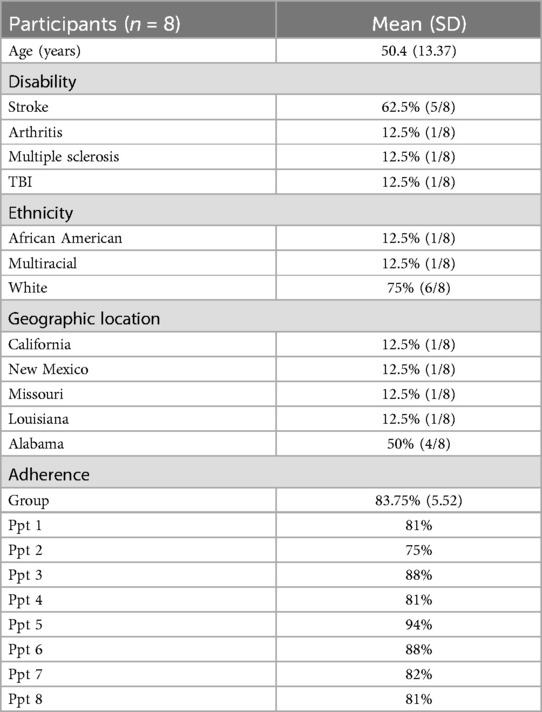
In health promotion programs specifically, SCT analyzes both initiation and maintenance of behavior. It allows participants to regulate their actions by achieving goal-oriented behaviors by learning situational and environmental control, and by reinforcing their learned patterns of control (20–23). Health promotion programs designed using SCT use specific outcome measures to assess readiness for change and implemented change across time. Figure 1 illustrates the determinants of SCT by which participant's behavioral changes are defined and assessed. The MENTOR program uses SCT to encourage positive behavioral change among PWD using a virtual environment by introducing dynamics such as personal attitudes, socioenvironmental influences, and self-efficacy. Figure 2 demonstrates the SCT using constructs specific to the current study.
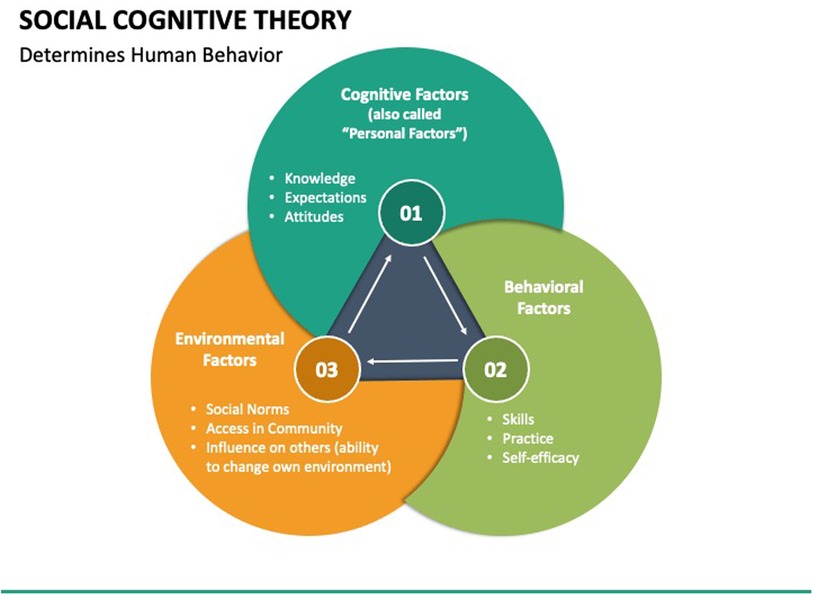
Figure 1. Social cognitive theory framework (33).
The interview guide developed for this study employed Dr. Bandura's concept of reciprocal determinism and SCT's constructs (personal cognitive factors, socioenvironmental factors, and behavioral factors) to develop each question. An independent researcher was part of the survey development iteration process to ensure accuracy and content validity. The survey was formatted to assess participant's perceptions of MENTOR during the program as well as their level of implementation following their completion of the program.
Qualitative approach
A qualitative approach was used in this study to gain a deeper understanding of participants’ retrospective experiences and preferences during and after participating in the MENTOR program. Compared to other methods of data collection, such as surveys, qualitative interviews allow the researcher and participant to have fluid, in-depth conversation to immerse and qualify their perceptions of the exercise portion of the MENTOR program, and how those experiences might have affected their implementation of learned strategies following the program. To best collect this information, our qualitative approach was designed to allow relevant information to be shared between the researcher and participant. Thus, semi-structured, virtual interviews guided by a curated interview guide were employed.
Data collection
Development of interview guide
To increase the rigor and ethics of interviewing individuals with physical disabilities, the primary researcher conducted a focus group panel of expert advisors to review an initial interview guide developed using SCT. Selection criteria for participating in the focus group included: (1) 18 years of age or older; (2) self-identify as having a physical disability/mobility limitation, and/or (3) experience with delivering inclusive/adapted content to people with physical disabilities; (4) able to speak and converse using English language; and (5) willing to provide knowledgeable feedback on readability and inclusive language usage. Five individuals whose expertise included community-based disability programming, disability and physical activity, and disability survey development were identified and invited to attend a focus group session. All five individuals agreed and attended. Following focus group feedback, a final interview guide was developed.
Participant interviews
The interview guide was designed as semi-structured to allow participants to speak about their personal experiences. One-on-one virtual, semi-structured interviews were conducted via Zoom between the primary researcher and participant. Participants were informed their participation was voluntary and that they could discontinue their interview at any time. Participants were also informed that audio and visual data were recorded for data analyzation purposes only and were stored using a HIPAA compliant, duo-authenticated database secured by private networks. To make participants feel comfortable, before interviews began, the researcher asked each participant an ice-breaker question of “Tell me a little bit about yourself,”. Once interviews officially began, the researcher used the interview guide as a checklist of questions to ask, while also asking participants to elaborate more on certain aspects of the conversation that were of interest and not listed in the interview guided questions. For example, if a participant shared an interesting detail about the exercise classes not listed in the interview guide, the researcher might ask the participant to continue sharing. The semi-structured design allowed the researcher insight to participant's complete involvements during the MENTOR exercise classes. Per a priori protocol agreed upon by the research team, interviews would be conducted until qualitative data saturation occurred and was maintained.
Data analysis
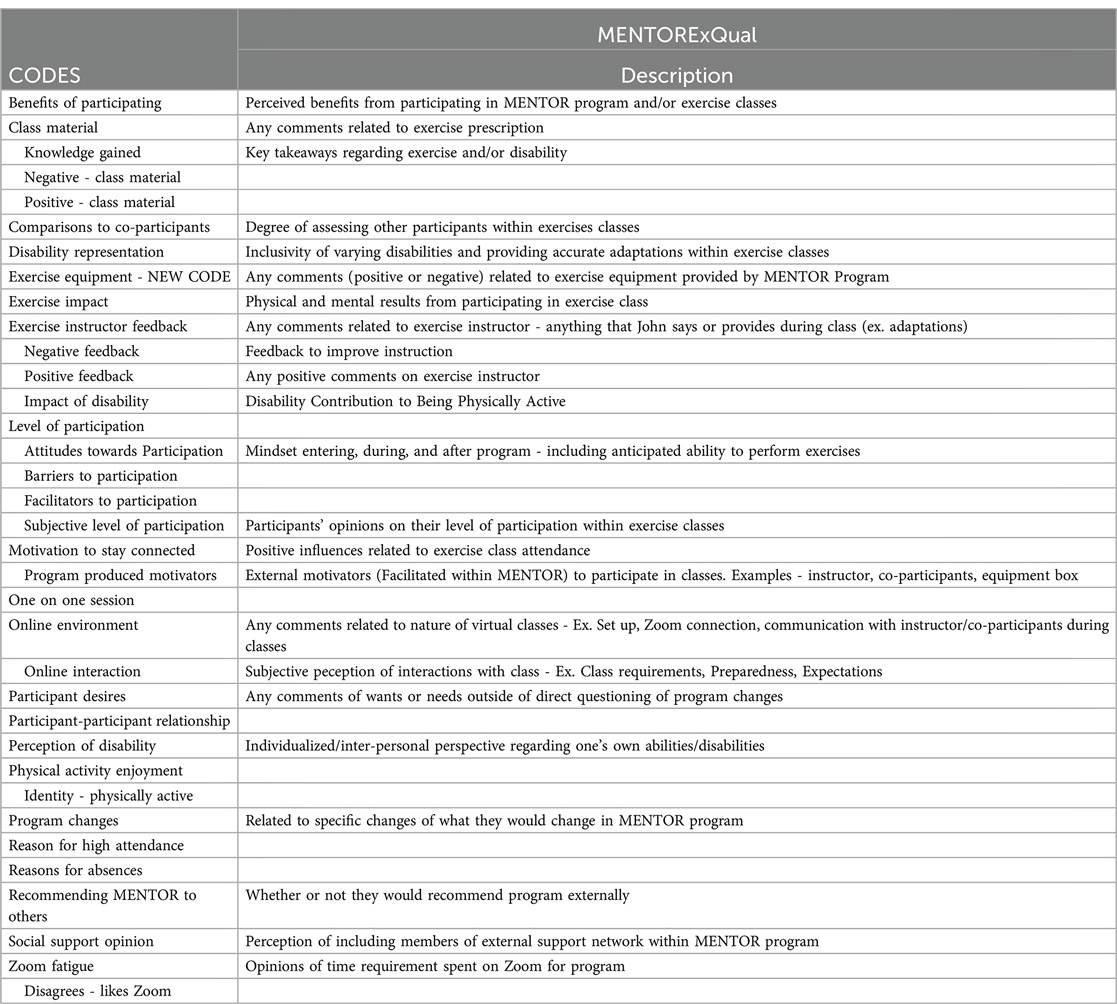
Qualitative data was recorded using Zoom, transcribed using Microsoft 365 Word transcription service, verified by the primary researcher, and analyzed using NVivo Software (version 14). Data was informed by ontological relativism, which means reality is dependent on the person/people interpreting it. To increase the rigor of data analyzation, two coders (M. M. and C. F.) analyzed data independent of one another, then met to agree and merge data. In the event of coding discrepancy, a third coder (L. B.) was contacted. Interview transcripts were analyzed in sequential order of interviews conducted. Codes were created beginning in the first interview and either added-to or deleted depending on the saturation of relevant data as additional interview transcripts were analyzed. M. M. and C. F. created a qualitative codebook with definitions to remain in tandem when interpreting interview transcripts independently. Where new codes were created, M. M. and C. F. met to agree on the new code, defined it, and inserted it into the codebook. This process was repeated until data saturation occurred. See Appendix 1 for codebook.
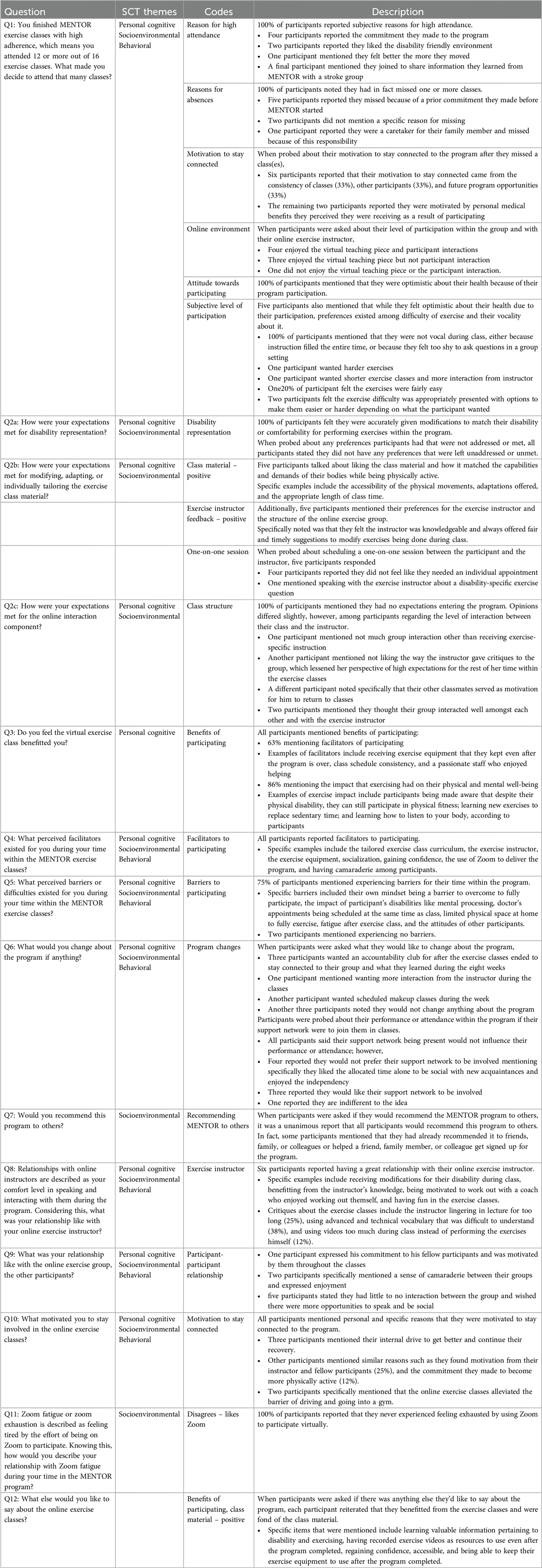
Results of qualitative data were emailed to participants for member checking to increase the internal validity and trustworthiness of the study. Based on a priori significance agreed upon by the research team, qualitative results were considered significant if 5 ore more participants (63%) reported the same code. Table 1 illustrates participant demographics.
Results
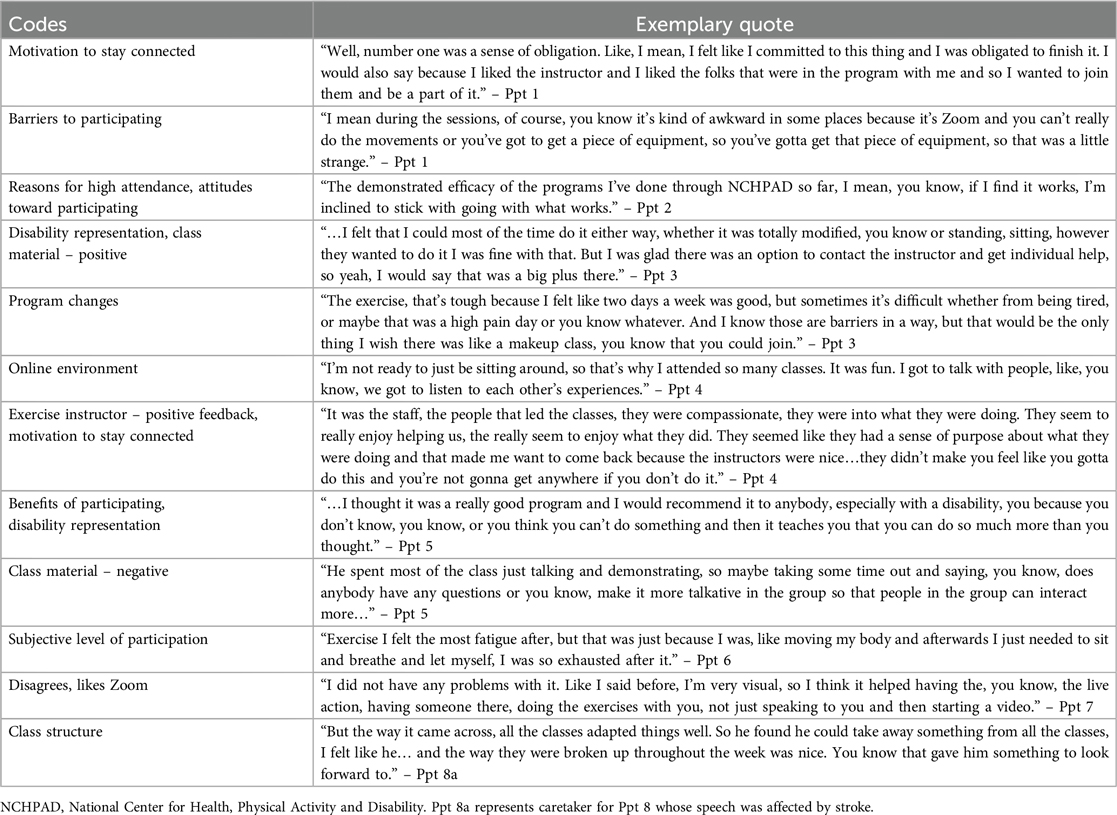
A total of eight high-adherers (n = 8) to the MENTOR virtual exercise classes were invited to complete interviews, and 100% of participants consented and completed their interviews. Data saturation occurred at the sixth interview and was maintained through the eighth interview, at which point no more interviews were conducted from the remaining pool of high adherers. Average interview length was 47 min with a range from 34 to 69 min. Thirty-five participant-generated codes were identified. These participant-generated codes were categorized using SCT constructs, personal cognitive factors, socioenvironmental factors, and behavioral factors. These existing constructs were pre-determined as themes to shape the interpretation of participant-generated codes found from interviews. Table 2 reflects interview guide questions and results of coding analysis. Only significant results are presented here, which we defined at an a priori value of 63% or more of participant report per code. To increase internal validity and trustworthiness of the results, member checking was employed. All participants were emailed a copy of their transcript as well as comprehensive findings, to which 100% of participants responded in agreement to the data.
Table 2 provides participant responses to each of 12 interview questions. Overall, participants described the exercise classes as motivating, disability friendly, easily adaptable when questioned about their involvement during classes. Outside of the confines of the interview questions, 100% of participants mentioned still being physically-active today using MENTOR exercise-specific content including recorded videos, exercise equipment, and communication with fellow participants they keep in contact with since their time in the program ended. When asked about their perception of the virtual exercise program structure, participants reported benefits of participating, more facilitators than barriers, a positive relationship with their virtual exercise instructor, and willingness to recommend the program with others. Additionally, 100% of participants informed us they never experienced Zoom fatigue or exhaustion of participating in weekly classes online.
Table 3 highlights the overarching quotes that participants made about the exercise classes. Overall, participants expressed great satisfaction and gratitude for this type of program existing for PWD, reasons they found motivation to continue with high attendance, and the impact MENTOR had on them personally.
Discussion
This study was a qualitative evaluation of highly adherent participants who participated in an eight-week virtual wellness program that included two days a week of exercise classes. The purpose of evaluating this sample of PWD was to analyze how their adherence affected their participation in and perception of the program. Results suggest that the eight-week online exercise classes were effectively received for those participants who maintained high adherence. The thematic coding of the participant interviews produced positive findings about the virtual exercise classes, signifying that participants had an overall positive experience with minor critiques regarding their perception of program delivery. Moreover, participants expressed comfort with the online atmosphere and interactions among their instructor and co-participants. These follow-up interviews ranging from seven months to twenty-two months post-program completion found that 100% of participants were still maintaining their exercise regimens, using the program-provided exercise equipment, and utilizing the recorded exercise videos as a resource to continue physical activity.
The use of SCT deepened our understanding of how participants perceived integrating a virtual exercise program into their life. Personal cognitive factors that applied to our sample included outcome expectations, knowledge, and behavioral capability. Participants stated in several instances they used MENTOR for their own medical benefit. This signified their readiness for engaging in self-managed personal health. Socioenvironmental factors that affected participant's perceptions and behaviors during and after MENTOR exercise included the mandatory use of Zoom to interact and participate. While participants were unbothered by the time they spent on Zoom, regarding class structure, participants expressed preferences such as more opportunities to socialize outside of instruction time (n = 7) and more group-facilitated interactions compared to instructor-led lecture (n = 6). Additionally, they noted certain facilitators and barriers of virtual participation. Facilitators included the tailored exercise class curriculum, the exercise instructor, the exercise equipment, gaining confidence, the use of Zoom to deliver the program, and having camaraderie among participants. Barriers included mindsets to overcome to fully participate, the impact of participant's disabilities (i.e., mental processing), doctor's appointments being scheduled at the same time as class, limited physical space at home to fully exercise, fatigue after exercising, and the attitudes of other participants.
Finally, behavioral factors that were noted by the participants were self-regulatory practices such as skill, intensity, and self-monitoring which includes goal setting, planning, and awareness of one's health. All participants consistently mentioned the effect exercise had on their health while they were in classes. They also learned how to adapt and modify exercises to fit their personal needs related to their function and disability. All participants noted the impact that learning through a disability-friendly environment had on motivating them to maintain and implement what they learned from the MENTOR exercise classes into their daily lives.
To our knowledge, there are currently no other accessible, virtual holistic-based health and wellness programs offered specifically for PWD that target comprehensive areas of health such as mindfulness, exercise, and nutrition (3, 25, 34). As mentioned by participants, this program alleviated barriers to participation and included facilitators that allowed them to successfully participate and implement what they learned into their lifestyles after they completed the program.
A few post-evaluation recommendations were noted by participants. First, future iterations of MENTOR should incorporate participant feedback to the exercise instructor while the program is ongoing so that barriers can be removed as soon as they are identified. Second, seven out of eight participants (88%) desired more interaction between their group and their instructor, less intimidating vocabulary, and less lecture format with a limited number of pre-recorded videos played during class time. Third, participants noted that a specific barrier was not having their room and equipment ready before the start of class. They recommended that the instructor should let them know in advance which exercises were going to be performed before class so that the participant could have an appropriate amount of space and the correct equipment prior to the start of class.
A 2011 study that surveyed PWD identified important factors to make them want to participate in physical activity, including accessible exercise facilities, instructors knowledgeable about adapted exercise, a sense of belonging, support from friends and family, and disability awareness (35). MENTOR circumvents and accommodates these variables by offering a free, completely tailored online program for different types of disabilities, age groups, races, and geographic locations. The most reported reasons PWD have given when asked why they discontinue exercise are inaccessibility, fear, and the fatigue that follows physical exertion (36–39). These barriers can be overcome with personnel trained in disability fitness, inclusivity, and accessibility (38). Currently, blueprints for improving exercise adherence now exist so that future studies can shift from reporting facilitators and barriers to developing strategies and interventions that address reported barriers and use key facilitators to promote adherence (40–42). Furthermore, more interventions specific to PWD are incorporating theories and frameworks, which allows data to be empirical and clinically translatable (35, 36, 43). The aforementioned strategies allude to the continued need of health promotion to, for, and among PWD, especially targeting holistic wellness.
This study had limitations. First, we intentionally developed an interview guide specifically for the high adherent completers of MENTOR exercise classes. A more complete profile of adherence may have been obtained if interviews were conducted with non-, low-, and moderate-adherers. Second, the majority of participants were stroke survivors over the age of fifty and could have perceived exercise differently than other participants. Third, data analyzation included the primary researcher and a secondary independent researcher, which may have introduced bias, whereas a coder not affiliated with the interviews might have different impressions of the data. Finally, only exercise classes were used for interview purposes considering the scope of our aim. To fully understand the comprehensibility of the full program, interviews should be conducted among all core program classes to incorporate mindfulness and nutrition. Future delivery of MENTOR should incorporate feedback from participants who completed the program with high adherence, and more independent interviews should be completed within all areas including mindfulness and nutrition. Nonetheless, the data illustrate the theoretical factors associated with a successful online exercise program in a small group PWD with a variety of races, ages, and geographic locations.
Conclusions
This qualitative study guided by the SCT framework provided an insightful examination regarding high adherent participants within the MENTOR exercise classes and their perception of the program delivery. MENTOR exercise classes produced efficient and effective results for participants who were high adherers to the program. We found participants (1) were motivated to stay connected, (2) self-reported benefits of participating in the program, (3) felt represented regarding their disabilities, (4) would recommend the program to others, and (5) enjoyed their instructor, the class material, their fellow participants, and the virtual delivery. These results also included suggestions, feedback, and recommendations including (1) more instructor interaction during class, (2) less lecture time and format from instructor, 3) prior knowledge about what exercises participants would be performing and with what equipment, and 4) scheduled make-up classes for missed classes due to prior commitments. These results provide MENTOR personnel with guidelines to support future iterations of the program from a successful participant's perspective, as well as a beneficial framework for other exercise-promoting programs.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by University of Alabama at Birmingham Office of Institutional Review Board for Human Use. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this study did not conduct physical testing. Participants were sent an IRB approved information sheet prior to scheduling an interview. Participants were notified they could discontinue interview at any time with no penalty. Participants verbally consented before the start of each interview.
Author contributions
MM: Conceptualization, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. CF: Resources, Supervision, Validation, Writing – review & editing. LD: Conceptualization, Resources, Supervision, Writing – review & editing. JW: Resources, Supervision, Writing – review & editing. JR: Funding acquisition, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Funding for this [project] was provided by the National Center on Health, Physical Activity and Disability (NCHPAD). NCHPAD is a public health practice center providing inclusive health promotion programs and resources for people with disabilities. NCHPAD is funded by the Centers for Disease Control and Prevention (CDC), National Center on Birth Defects and Developmental Disabilities (NCBDDD), Division of Human Development and Disability, Disability and Health Promotion Branch, Grant #NU27DD000022.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Prevention CfDCa. Disability Impacts ALL of US. Center for Disease Control and Prevention. Available online at: https://www.cdc.gov/ncbddd/disabilityandhealth/infographic-disability-impacts-all.html (accessed June 10, 2024).
2. Prevention CfDCa. Physical Activity for People with Disability. Center for Disease Control and Prevention. Available online at: https://www.cdc.gov/ncbddd/disabilityandhealth/features/physical-activity-for-all.html (accessed June 4, 2024).
3. Carroll DD, Courtney-Long EA, Stevens AC, Soan ML, Lullo C, Visser SN, et al. Vital Signs: Disability and Physical Activity - United States, 2009–2012. Center for Disease Control and Prevention (CDC). Available online at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6318a5.htm (accessed June 4, 2024).
4. Jones M, Morris J, Deruyter F. Mobile healthcare and people with disabilities: current state and future needs. Int J Environ Res Public Health. (2018) 15(3):515. doi: 10.3390/ijerph15030515
5. National Center on Birth Defects and Developmental Disabilities CfDCaP. Including People with Disabilities in Public Health Programs and Activities. Available online at: https://www.cdc.gov/ncbddd/disabilityandhealth/disability-public-health.html (accessed June 4, 2024).
6. Marrocco A, Krouse HJ. Obstacles to preventive care for individuals with disability: implications for nurse practitioners. J Am Acad Nurse Pract. (2017) 29(5):282–93. doi: 10.1002/2327-6924.12449
7. Hollis ND, Zhang QC, Cyrus AC, Courtney-Long E, Watson K, Carroll DD. Physical activity types among US adults with mobility disability, behavioral risk factor surveillance system, 2017. Disabil Health J. (2020) 13(3):100888. doi: 10.1016/j.dhjo.2020.100888
8. Ginis KAM, van der Ploeg HP, Foster C, Lai B, McBride CB, Ng K, et al. Participation of people living with disabilities in physical activity: a global perspective. Lancet. (2021) 398:433–55. doi: 10.1016/S0140-6736(21)01164-8
9. Okoro CA HN, Cyrus AC, Griffin-Blake S. Prevalence of Disabilities and Health Care Access by Disability Status and Type Among Adults — United States, 2016. (2016). Available online at: https://www.cdc.gov/mmwr/volumes/67/wr/mm6732a3.htm?s_cid=mm6732a3_w (accessed June 4, 2024).
10. Staff MC. Support groups: Make connections, get help. Available online at: https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/support-groups/art-20044655 (accessed June 10, 2024).
11. Society NMS. Find Support Groups and Programs. National Multiple Sclerosis Society. (2024). Available online at: https://www.nationalmssociety.org/resources/get-support/find-support-groups-and-programs (accessed June 7, 2024).
12. McLoughlin G, Weisman Fecske C, Castaneda Y, Gwin C, Graber K. Sport participation for elite athletes with physical disabilities: motivations, barriers, and facilitators. Adapt Phys Activ Q. (2017) 34(4):421–41. doi: 10.1123/apaq.2016-0127
13. Sahlin KB, Lexell J. Impact of organized sports on activity, participation, and quality of life in people with neurologic disabilities. PM&R. (2015) 7(10):1081–8. doi: 10.1016/j.pmrj.2015.03.019
14. Vincenzo JL, Hergott C, Schrodt L, Rohrer B, Brach J, Tripken J, et al. Capitalizing on virtual delivery of community programs to support health and well-being of older adults. Phys Ther. (2021) 101(4):1–4. doi: 10.1093/ptj/pzab001
15. Evaluation ASfPa. Virtual Human Service Delivery: Scan of Implementation and Lessons Learned. Available online at: https://aspe.hhs.gov/virtual-human-service-delivery-scan-implementation-lessons-learned (accessed June 7, 2024).
16. Labrie D, Lapierre N, Mortenson WB, Allaire A-S, Schmouth M-È, Routhier F. Exploratory study on the adaptation of online services offered to people with disabilities, in the context of the COVID-19 pandemic. Disability and Rehabilitation: Assistive Technology. (2024) 1–11. https://www.tandfonline.com/doi/full/10.1080/17483107.2024.2326593#infos-holder38462813
17. Ware ME, deMarrais KB, McCully KK. Adherence and continued participation in a wellness class for individuals with disabilities. Rehabil Process Outcome. (2019) 8:1179572719843257. doi: 10.1177/1179572719843257
18. Newitt R, Barnett F, Crowe M. Understanding factors that influence participation in physical activity among people with a neuromusculoskeletal condition: a review of qualitative studies. Disabil Rehabil. (2016) 38(1):1–10. doi: 10.3109/09638288.2014.996676
19. Labbé D, Desai N, Herman C, Elder C. “I never really thought that a virtual ride would be that good!”: experiences of participants with disabilities in online leisure-time physical activity during COVID-19. Disabil Health J. (2023) 16(1):101395. doi: 10.1016/j.dhjo.2022.101395
20. Silveira SL, Richardson EV, Motl RW. Social cognitive theory as a guide for exercise engagement in persons with multiple sclerosis who use wheelchairs for mobility. Health Educ Res. (2020) 35(4):270–82. doi: 10.1093/her/cyaa013
21. Ginis KAM, Latimer AE, Arbour-Nicitopoulos KP, Bassett RL, Wolfe DL, Hanna SE. Determinants of physical activity among people with spinal cord injury: a test of social cognitive theory. Ann Behav Med. (2011) 42(1):127–33. doi: 10.1007/s12160-011-9278-9
22. Fifolt M, Richardson EV, Barstow E, Motl RW. Exercise behaviors of persons with multiple sclerosis through the stepwise implementation lens of social cognitive theory. Disabil Rehabil. (2020) 42(7):948–56. doi: 10.1080/09638288.2018.1514077
23. Ma JK, Martin Ginis KA. A meta-analysis of physical activity interventions in people with physical disabilities: content, characteristics, and effects on behaviour. Psychol Sport Exerc. (2018) 37:262–73. doi: 10.1016/j.psychsport.2018.01.006
24. Fiuza-Luces C, Santos-Lozano A, Joyner M, Carrera-Bastos P, Picazo O, Zugaza JL, et al. Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat Rev Cardiol. (2018) 15(12):731–43. doi: 10.1038/s41569-018-0065-1
25. Gondim OS, de Camargo VTN, Gutierrez FA, de Martins PFO, Passos MEP, Momesso CM, et al. Benefits of regular exercise on inflammatory and cardiovascular risk markers in normal weight, overweight and obese adults. PLoS One. (2015) 10(10):e0140596. doi: 10.1371/journal.pone.0140596
26. Ding K, Juengst SB, Neaves S, Turki A, Wang C, Huang M, et al. Usability of a two-way personalized mobile trainer system in a community-based exercise program for adults with chronic traumatic brain injury. Brain Inj. (2022) 36(3):359–67. doi: 10.1080/02699052.2022.2059817
27. Domingos J, Dean J, Fernandes JB, Godinho C. An online dual-task cognitive and motor exercise program for individuals with Parkinson disease (PD3 move program): acceptability study. JMIR Aging. (2022) 5(4):e40325. doi: 10.2196/40325
28. Lai B, Rimmer J, Barstow B, Jovanov E, Bickel CS. Teleexercise for persons with spinal cord injury: a mixed-methods feasibility case series. JMIR Rehabil Assist Technol. (2016) 3(2):e8. doi: 10.2196/rehab.5524
29. Rimmer JH, Young HJ, Bachiashvili V, Baidwan NK, Mehta T. Enhancements to a telewellness program for people with physical disabilities: mindfulness, exercise, and nutrition to optimize resilience (MENTOR 2.0). Prev Chronic Dis. (2024) 21:E02. doi: 10.5888/pcd21.230181
30. Rimmer JH, Wilroy J, Galea P, Jeter A, Lai BW. Retrospective evaluation of a pilot eHealth/mHealth telewellness program for people with disabilities: Mindfulness, Exercise, and Nutrition to Optimize Resilience (MENTOR). Mhealth. (2022) 8:15. doi: 10.21037/mhealth-21-34
31. Ferguson CC, Clina JG, Young HJ, Gammon L, Jeter A, Abadie A, et al. Improvements in nutrition knowledge among adults with physical disabilities: a program evaluation of the Mindfulness, Exercise, and Nutrition to Optimize Resilience (MENTOR) program 2020–2021. Disabil Health J. (2024) 17(2):101577. doi: 10.1016/j.dhjo.2023.101577
32. Rimmer JH, Wilroy J, Young HJ, Young R, Sinha T, Currie M, et al. Qualitative evaluation of a comprehensive online wellness program (MENTOR) among people with spinal cord injury. Front Rehabil Sci. (2022) 3:917898. doi: 10.3389/fresc.2022.917898
33. Main P. Social Cognitive Theories. Available online at: https://www.structural-learning.com/post/social-cognitive-theories (accessed June 7, 2024).
34. Halabchi F, Alizadeh Z, Sahraian MA, Abolhasani M. Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC Neurol. (2017) 17(1):185. doi: 10.1186/s12883-017-0960-9
35. Junker L, Carlberg EB. Factors that affect exercise participation among people with physical disabilities. Adv Physiother. (2011) 13(1):18–25. doi: 10.3109/14038196.2011.556752
36. Rimmer JH, Riley B, Wang E, Rauworth A, Jurkowski J. Physical activity participation among persons with disabilities: barriers and facilitators. Am J Prev Med. (2004) 26(5):419–25. doi: 10.1016/j.amepre.2004.02.002
37. Buffart LM, Westendorp T, van den Berg-Emons RJ, Stam HJ, Roebroeck ME. Perceived barriers to and facilitators of physical activity in young adults with childhood-onset physical disabilities. J Rehabil Med. (2009) 41:881–5. doi: 10.2340/16501977-0420
38. Malone LA, Barfield JP, Brasher JD. Perceived benefits and barriers to exercise among persons with physical disabilities or chronic health conditions within action or maintenance stages of exercise. Disabil Health J. (2012) 5(4):254–60. doi: 10.1016/j.dhjo.2012.05.004
39. Stroud N, Minahan C, Sabapathy S. The perceived benefits and barriers to exercise participation in persons with multiple sclerosis. Disabil Rehabil. (2009) 31(26):2216–22. doi: 10.3109/09638280902980928
40. Ginis KAM, Ma JK, Latimer-Cheung AE, Rimmer J. A systematic review of review articles addressing factors related to physical activity participation among children and adults with physical disabilities. Health Psychol Rev. (2016) 4:478–94. doi: 10.1080/17437199.2016.1198240
41. Williams T, Ma J, Ginis K. Participant experiences and perceptions of physical activity-enhancing interventions for people with physical impairments and mobility limitations: a meta-synthesis of qualitative research evidence. Health Psychol Rev. (2017) 11:1–37. doi: 10.1080/17437199.2017.1299027
42. Lai B, Yong H-J, Bickel S, Motl R, Rimmer JH. Current trends in exercise intervention research, technology, and behavioral change strategies for people with disabilities a scoping review. Phys Med Rehabil. (2017) 96(10):748–61. doi: 10.1097/PHM.0000000000000743
43. Wilroy J, Herbey I, Ivankova N, Rimmer J. 24402 Grounded theory model for adherence to home exercise among people with a mobility disability. J Clin Transl Sci. (2021) 5:1–2. doi: 10.1017/cts.2021.573
Appendix 1
Keywords: qualitative evaluation, people with physical disabilities, community programs, virtual exercise, program adherence, social cognitive theory (SCT)
Citation: Mintz M, Ferguson C, Dayton LAB, Wilroy J and Rimmer JH (2024) Qualitative evaluation of factors influencing adherence to virtual exercise programs for people with physical disabilities. Front. Rehabil. Sci. 5:1470630. doi: 10.3389/fresc.2024.1470630
Received: 25 July 2024; Accepted: 20 September 2024;
Published: 11 October 2024.
Edited by:
Brendan McCormack, The University of Sydney, AustraliaReviewed by:
Zhuoying Qiu, University of Health and Rehabilitation Sciences, ChinaKerri Morgan, Washington University in St. Louis, United States
Copyright: © 2024 Mintz, Ferguson, Dayton, Wilroy and Rimmer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Madison Mintz, bXJjdXJyaWVAdWFiLmVkdQ==
 Madison Mintz
Madison Mintz Christine Ferguson1,2
Christine Ferguson1,2 Leigh Anne Bray Dayton
Leigh Anne Bray Dayton Jereme Wilroy
Jereme Wilroy James H. Rimmer
James H. Rimmer