- 1School of Physical and Occupational Therapy, Faculty of Medicine and Health Sciences, McGill University, Montreal, QC, Canada
- 2Faculty of Medicine and Health Sciences, McGill University, Montreal, QC, Canada
- 3The Research Center of the Jewish Rehabilitation Hospital, Centre Intégré de Santé et de Services Sociaux de Laval, Laval, QC, Canada
- 4Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal, Montreal, QC, Canada
Background: Children with neurodevelopmental disabilities (NDDs, e.g., cerebral palsy) and their caregivers face lifelong and impactful challenges, particularly during life-transition periods such as adolescence. One's resilience emerges as an essential ability to navigate this vulnerable phase. Resilience is a complex concept that embeds multiple factors on various levels. Little is known about what resilience factors are pivotal in youth with NDDs and their families as they transition into adolescence and how these are addressed as part of existing targeted interventions.
Objectives: This review explored the concept of resilience in youth with NDDs and their families. Specific aims included describing salient resilience factors in adolescents with NDDs and their families and to describe how resilience is addressed as part of targeted interventions.
Methods: Using the Arskey and O'Malley framework, six steps were undertaken, including a comprehensive literature search (n = 5 databases), transparent study selection, detailed data extraction with a coding scheme (n = 46 factors), results' collating with numerical and inductive content analysis, and consultation with three key stakeholders.
Results: The study screened 1,191 publications, selecting fifty-eight (n = 58; n = 52 observational and n = 6 intervention) studies. Findings revealed that resilience in this context is closely linked to more than forty factors across four levels (individual; family; school/peers; and community). Pivotal factors include social and emotional competence, optimism, and family/peer relationships. While existing interventions targeting resilience show promising results, few programs are available and generalizable to different NDDs. Stakeholders highlighted the importance of addressing resilience factors that are not targeted in existing interventions: caregivers' self-efficacy and self-esteem, as well as youth's and caregiver's confidence. Preferences for and advantages of online delivery for support programs and individual/group features also emerged.
Conclusion: The review emphasizes the need for a holistic approach to support youth with NDDs and their families during adolescence transition. To enhance their resilience, recognizing caregivers' roles, customizing interventions, and exploring new implementation formats are avenues that align with the current evidence and opportunities for practical development in this field.
Introduction
Neurodevelopmental disabilities (NDDs) are highly prevalent and found to affect about 1 in 6 children (1), with an estimated total of 240 million children worldwide (2). NDDs, such as cerebral palsy or autism spectrum disorder (ASD) are chronic health conditions that may present life-long challenges. Children with NDDs can experience barriers in their physical, behavioral, verbal, cognitive, and social developmental trajectories, which can severely impact their participation in functional activities, leisure, and productivity (3, 4). In addition to these limitations, it is well established that children with NDDs are at a higher risk of experiencing mental health challenges than their typically developing peers (5–8), where a higher incidence (30%–50% vs. 8%–18%) of mental health disorders is reported (9). Mental health and well-being concerns are increasingly significant during life-transition periods, such as the shift from childhood to adolescence (10, 11) where many mental health disorders are being detected for the first time (12) and are known to persist into adulthood resulting in chronic and significant effects on health and social factors (13). Adolescence is a pivotal phase in life given the multitude of changes that are taking place simultaneously (e.g., physical/hormonal developments, social relationships, and new environments) (14, 15). Moreover, this transition period can be equally stressful for caregivers, who may also struggle with their mental health, yet are under pressure to rapidly adjust to support their child through their hardships (16).
In the context of adolescent transition, over the past decade, there has been a notable surge in anxiety and depression rates among the general youth population (17). This trend has been attributed, in part, to a decrease in independent engagement opportunities among youngsters (17), which are known to promote self-regulation (18). The importance of self-regulation cannot be overstated, as it contributes to the acquisition of skills crucial for coping with stressors and navigating vulnerable periods in life (19–23). In addition, emerging research highlighted the role of technology and social media, accessed by a staggering 97% of teenagers (24), in exacerbating mental health concerns such as anxiety, depression, and low self-esteem. The detrimental effects of excessive social media use extend further, with adolescents reporting increased incidents of cyberbullying and technology addiction (25). Notably, there exists a direct correlation between adolescents' social media usage levels and subsequent risks of self-harm (26). A survey conducted by the Youth Risk Behavior Surveillance System underscores the gravity of the situation, revealing that nearly 20% of high school students in the United States have seriously contemplated suicide, shedding light on the pressing adolescent mental health crisis (27). Considering the pervasive mental health struggles experienced by neurotypical children and adolescents, it is unsurprising that those with NDDs find themselves increasingly vulnerable to these challenges.
Resilience, defined as the ability to overcome life challenges and encompassing protective and vulnerability factors, becomes a crucial aspect during this transitional phase (28). Individuals use internal and external resources (protective factors) to surmount vulnerability factors. Protective factors refer to skills, strengths or physical resources that support individuals' ability to manage health conditions and strengthen their ability to overcome adversity. For instance, problem-solving abilities, emotional health, and community support may greatly impact overall levels of resilience. Conversely, vulnerability factors are elements that contribute to the worsening of health conditions. For instance, vulnerability factors may include bullying, lack of familial support, social isolation, and communication impairments (14). When vulnerability factors outweigh protective factors, overall well-being is likely to decline, and there is an increased risk of developing health conditions that could negatively impact critical life transitions.
Resilience during the shift from childhood to adolescence appears to be a particularly powerful tool for adolescents with NDDs and their caregivers when navigating this distinct time (29). The adolescent phase is known to be marked by an increased inclination towards risky behaviors, jeopardizing their health and well-being. This vulnerability extends to mental health challenges, encompassing depression, suicidal behaviors, eating disorders, and substance abuse. The positive or negative progression of adolescents' development hinges on the risks and protective factors they encounter. The dynamic interaction between these factors plays a crucial role in shaping resilience mechanisms (30). Consequently, it was suggested that research emphasis should be placed on identifying factors contributing to adolescent resilience (29, 31). While a recent systematic review provided a comprehensive overview of resilience in the general adolescent population and those with adverse experiences (31) there remains a notable gap in understanding the specific resilience factors at play for youth with NDDs as they transition into adolescence. Conducting a knowledge synthesis exercise in this area would offer valuable insights into the unique challenges and factors that contribute to resilience in adolescents with NDDs during this crucial developmental period. This would not only enhance our understanding of the nuanced interplay between resilience, NDDs, and the challenges of adolescence but also provide a foundation for developing targeted interventions and support strategies tailored to the specific needs of this vulnerable population, along with potential policy changes.
The purpose of this scoping review was to explore the concept of adolescent resilience in youth with NDDs and their families. Specific objectives included to (1) Describe impactful resilience factors in adolescents with NDDs and their families, (2) Describe how resilience is addressed as part of targeted interventions, and (3) Identify existing gaps in this field's research and clinical practice.
Methods
Study design
The Arksey and O'Malley framework (32), later expanded on by Levac et al. (33) was used to guide the methodology of this review in six stages.
Step 1—Identify the research question
The research question of this scoping review is:
What resilience factors are impactful in adolescents with NDDs and their families, and how is resilience addressed as part of targeted interventions for this population?
Step 2—Identify relevant studies
We conducted a comprehensive literature search in the following databases (n = 5): Ovid MEDLINE(R) and In-Process, In-Data-Review and Other Non-Indexed Citations 1996 to February 27, 2023, Social Work Abstracts 1968 to December 2022, Embase 1996 to 2023 Week 08, PsycINFO 2002 to February Week 3 2023, PubMed NCBI National Library of Medicine. The search was performed on February 28th, 2023, and embedded three main themes, including resilience, adolescence, and neurodevelopmental disabilities (Supplementary Material S1). All study designs were considered (e.g., randomized clinical trial, observational design) if they focused on the concept of resilience (or its individual/family/peers-school/community related factors) in adolescents with NDDs (mean age between 10 and 18 years old) and their families (e.g., caregivers and/or siblings). No date limit was applied. No language limits were applied. Unpublished or grey literature was excluded because we aimed to examine existing evidence-supported approaches. When information about important resilience factors or resilience interventions could not have been extracted from the publication (e.g., the design of a measure, a short conference abstract), the citation was excluded.
Step 3—Select studies
Citations found using the search strategy were exported and de-duplicated using reference software (EndNoteTM 21). Following scoping review guidelines, authors TO and NZ individually and independently proceeded to the selection by title and abstracts. All the identified citations by abstract and title were then assessed for full-text eligibility by NZ following training from the senior author (TO). Uncertainties were resolved through discussion between NZ and TO. Once the studies were selected, the reference lists were searched manually to see if any additional records met the inclusion criteria.
Step 4—Chart the data
Two extraction forms (one for observational and one for intervention studies) were developed a priori by senior author (TO) and revised by co-authors for completeness and relevance. Extraction forms included the citation details [author(s), year, country], study design and objective, definition of resilience, theories/models used, sample size and description of sample, outcomes/measurement, and study findings. For intervention studies, we extracted information on the intervention content, duration, frequency, participants, and delivery methods. For both types of studies, the resilience factors that were addressed were clearly identified. Following the development of the extraction form, two eligible articles were included in a pilot extraction phase by the senior author (TO). Another author (NZ) was trained in data extraction using the forms by the senior author and completed the extractions on all remaining citations. The senior author (TO) verified 100% of all extracted data and resolved any remaining inconsistencies or uncertainties.
Step 5—Collate, summarize, and report the results
A coding scheme (Supplementary Material S2) was developed by the senior author (TO) based on recent and comprehensive knowledge synthesis and consensus projects related to child and adolescent mental health and resilience-focused interventions (28, 34–36). The coding scheme includes four main resilience levels. These are individual (internal protective factors) as well as family, school/peers, and community levels (external protective factors). When extracting data from the selected publications, the coding scheme was applied to each citation to describe which factors were addressed in the intervention and the corresponding assessment and descriptive studies.
When possible, a numerical summary analysis was used to describe the study characteristics, methodology, and outcomes. An inductive content analysis was used to summarize additional information that could not be quantified (37). Once this was complete, all authors reviewed the results to ensure consistency and validity.
Step 6—Consultation exercise involving key stakeholders
Engaging stakeholders in the discussion on scoping review findings can validate findings, promote understanding of results, and identify important gaps (19). We recruited a key stakeholder advisory committee composed of two caregivers (n = 1 mother, Mrs. L., of a 10-year-old boy with CP [i.e., approaching adolescence]; n = 1 mother, Mrs. N., of two young 15 and 22 years old boys with ASD [i.e., passed adolescence transition]) and one young adult, Mr. M., a 28 years old man with CP [i.e., passed adolescence transition].
Individual, one-time, semi-structured online consultation meetings (45–60 min in duration) were conducted with the stakeholders to support the interpretation of study results and discuss their perspectives. To begin, the results of the scoping review were presented to participants in the form of a short PowerPoint presentation. This included an outline of the most salient resilience factors that were identified, as well as a description of available intervention programs. The discussion included the following questions, prompting participants to reflect on these factors and on their own experience (the varied questions reflect the diverse life experiences/different life stages of the participating stakeholders):
(1) For Mr. M. and Mrs. N.: Think about your/your child's teenage years, what was most difficult to overcome and why? What was helpful and how? What would you have liked to get as support back in those days?
(2) For Mrs. L.: What are your biggest concerns with regards to your child approaching the teenage years? What do you think would be helpful to be included in a coaching intervention for caregivers and children to facilitate this transition?
(3) For all: What do you think about the delivery methods (e.g., group vs. individual, online vs. in-person) of a resilience-coaching intervention?
Results
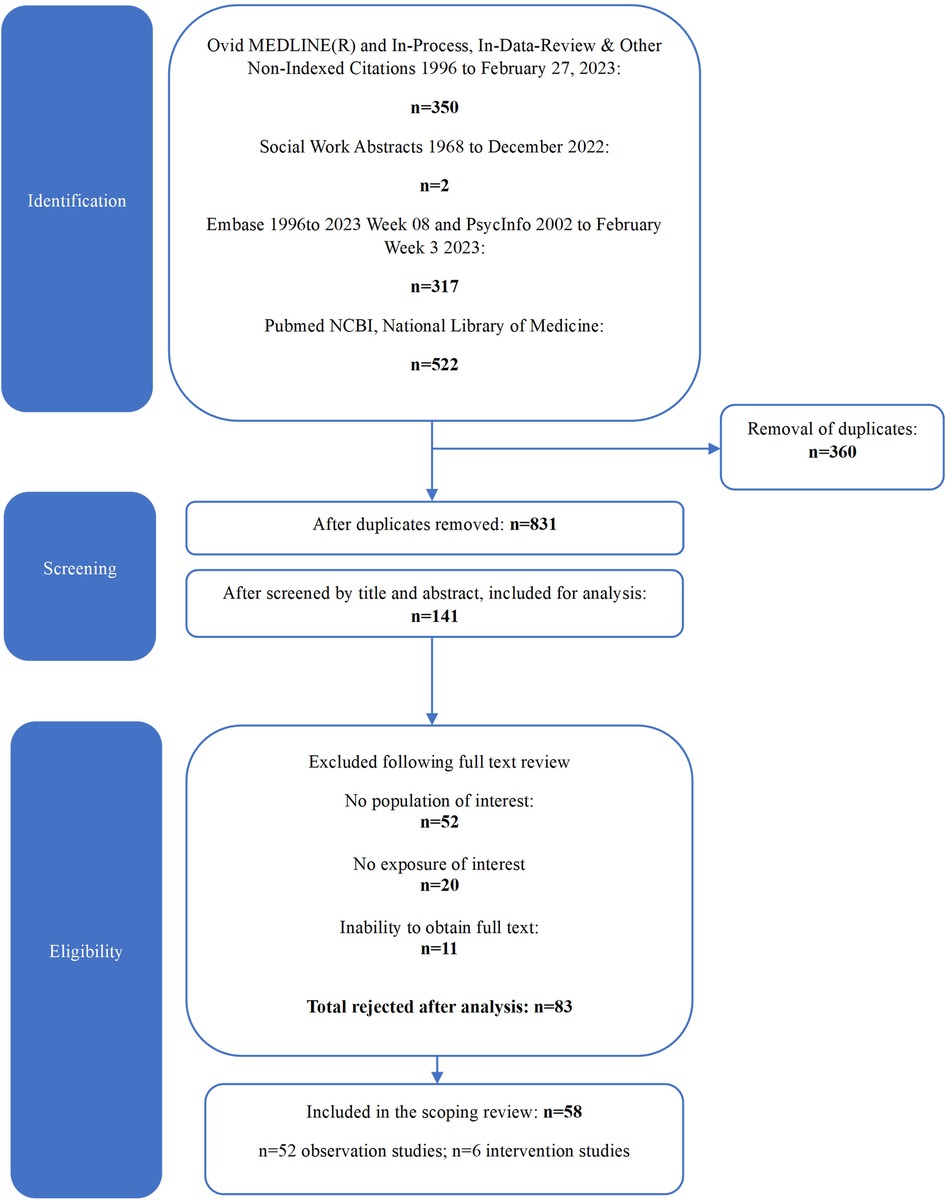
The study selection process is outlined in Figure 1. Our search revealed a total of 1,191 citations. Following duplicates removal, screening by title and abstract and full text, a total of 58 publications met our inclusion criteria and were included for analysis. Of these, 89.6% (n = 52 studies) were observational studies and 10.3% (n = 6) were intervention studies. The main reasons for excluding citations during the full text review were related to the population (e.g., mean age outside of 10–18 years old range and/or no presence of NDDs, n = 52, 62.6% of excluded citations) and exposure (i.e., work unrelated to the concept of resilience or measurement tool development, n = 20, 24.1%). A full list of excluded citations with reasons is available in Supplementary Material S3.
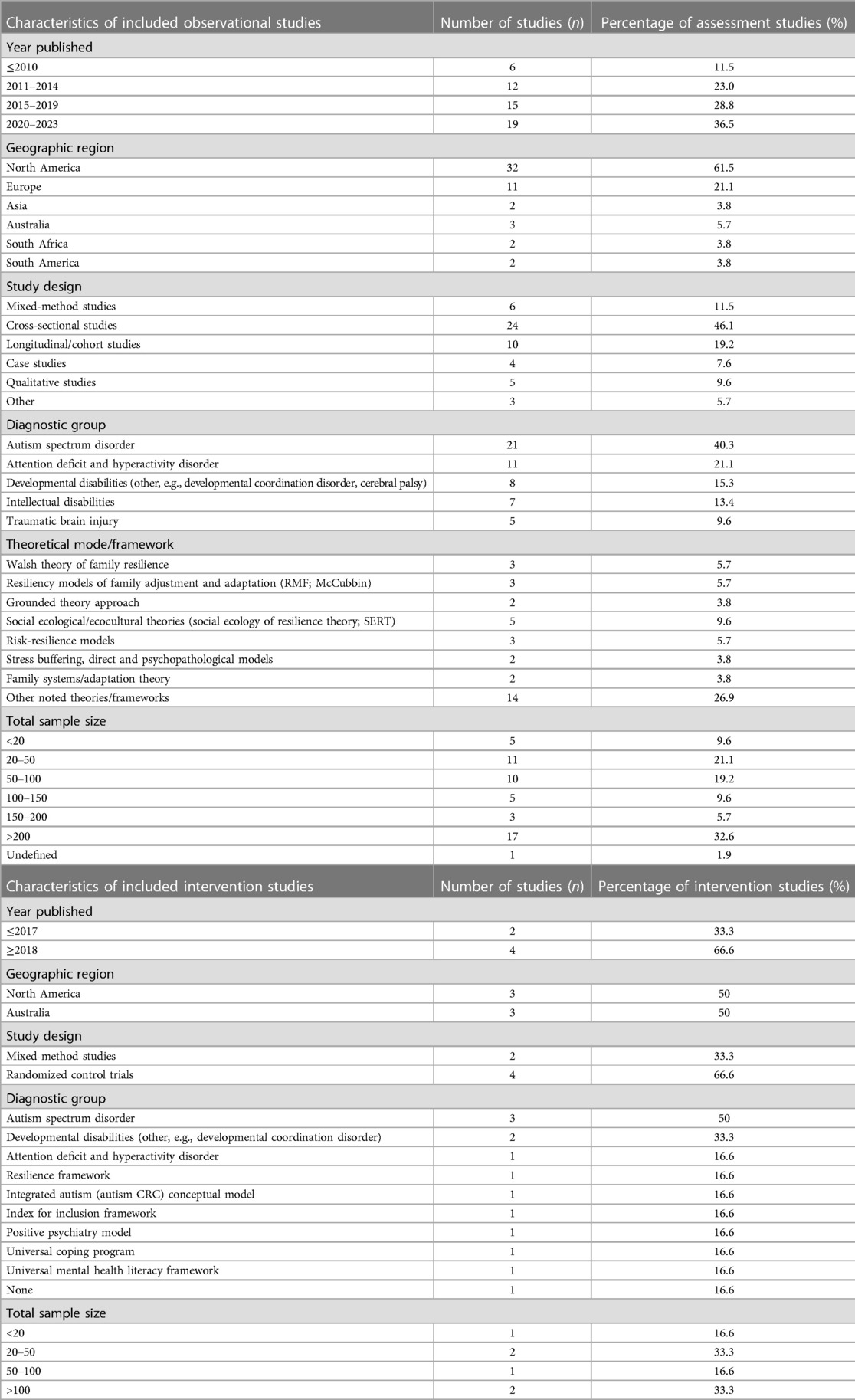
Tables 1, 2 provide an overview of all included studies. Over 60% of the observational studies were published after 2015 and in North America. These were mainly mixed-method, cross-sectional, and longitudinal study designs. In more than 30% of these studies, the sample size was greater than 200 individuals. The main population groups that were addressed were adolescents (and/or their caregivers and siblings) with ASD (n = 21, 40.4% of observational studies) and those with attention deficit and hyperactivity disorder (ADHD, n = 11, 21.1%). Resilience was defined in most assessment studies (n = 32, 61.54%) as a dynamic coping adaptation in the context of adversity and despite challenging circumstances, and many projects were anchored in a resilience-related framework or model (n = 34, 65.3%) (e.g., Social Ecology of Resilience Theory, Resiliency Models of Family Adjustment and Adaptation) (Supplementary Material S4A).
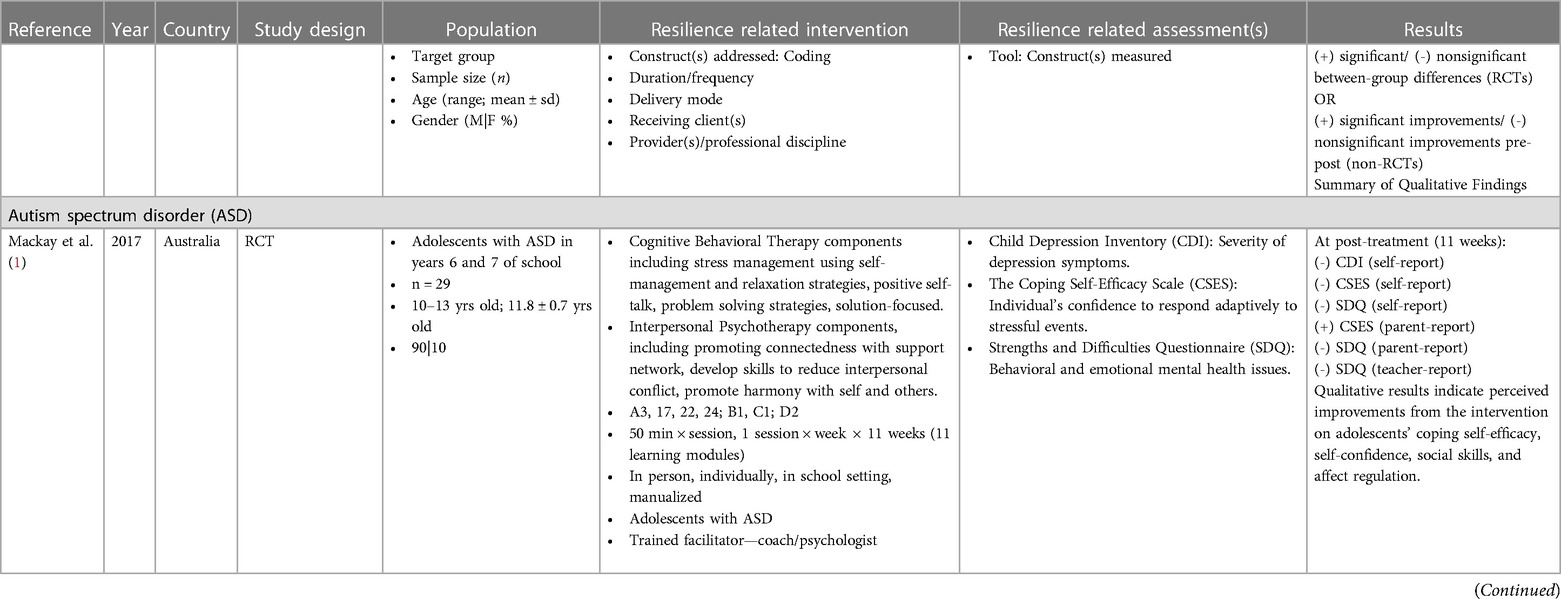
The coded resilience factors that were addressed as part of these studies at large and emerged as significant are displayed in Supplementary Material S5. Figure 2 outlines the main resilience factors that emerged from observational studies. It includes factors that were found to be significantly associated with the individuals' resilience levels and/or as having a mediating effect in regression models defining resilience. For an adolescent with a disability, the most salient individual-based resilience factors were social and emotional competence (40.4% of studies), optimism and positive attitude (30.8%), social and emotional skills (28.8%), cognitive competence (26.9%), and emotional regulation (23.1%). For caregivers and/or siblings, impactful individual-based resilience factors were coping (57.7%), communicational and cooperation (26.9%), and empowerment (17.3%). For both groups, in terms of family, school/peers, and community-based resilience factors, home relationships (21.2% of studies—adolescents; 40.7%—family), peer relationships and connections (26.9%; 17.3%), as well as community relationships (15.4%; 23.1%) were respectively identified as critical.
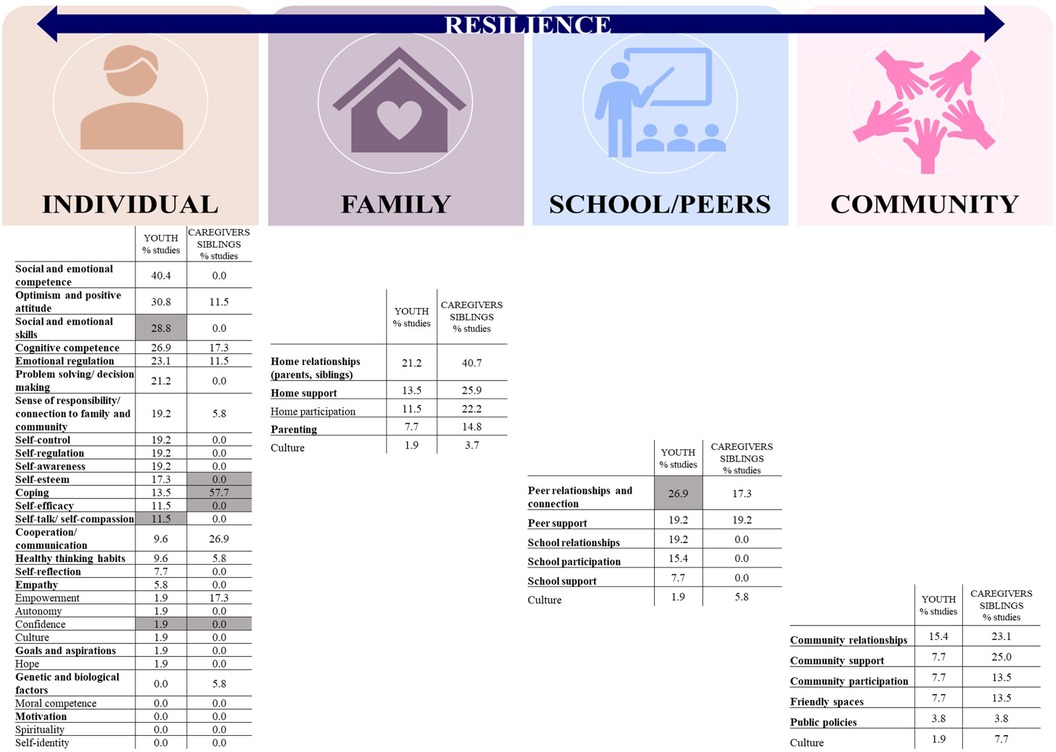
Figure 2. Listed factors with percentages refer to significant resilience factors in assessment studies (% of studies reporting these factors). Bolded factors refer to resilience factors that were addressed as part of interventions in intervention studies highlighted factors (in gray) refer to resilience factors identified as important through discussion with key stakeholders.
All intervention studies (n = 6/6, 100%) were published after 2017, where 50% were completed in North America and 50% in Australia. Most (n = 5/6, 83.3%) were randomized clinical trials. In intervention studies, the concept of resilience was defined in four studies and five studies mentioned the use of a resilience-related framework or model (e.g., Integrated Autism Conceptual Model, Index for Inclusion Framework) (Supplementary Material S4B). Over 50% of intervention studies had a sample size of more than 50 participants. The main population groups that were addressed in these interventions were adolescents (and/or their caregivers and siblings) with ASD (n = 3 studies, 50% of intervention studies), learning disability and a mixed of developmental disabilities (n = 2, 33.3%), as well as ADHD (n = 1, 16.6%), with mean age of 12.1 ± 1.5 years old (Table 1). On average, 10.8 ± 1.5 intervention sessions were offered, and most were in-person (n = 5/6, 83.3% of studies). All studies provided individual interventions, while some (n = 3/6, 50%) offered a group component. Interventions were mostly delivered by trained specialists/coaches, psychologists, or teachers. Overall, the existing interventions were found to be effective in improving resilience in general, including resilience-related components such as coping mechanisms, self-efficacy, positive emotions, behavioral and emotional functioning, and sense of connectedness or belonging (Table 2). Figure 2 further depicts the resilience factors addressed as part of these interventions (bolded). We found that multiple individual-based factors of resilience (e.g., self-regulation and communication) were addressed in most projects targeting youth. However, caregivers' individual-based factors of resilience (problem solving, decision making, self-efficacy, self-reflection, and sense of responsibility) were addressed in only one study. For siblings, individual factors such as coping and positive thinking were targeted in one intervention. In school/peers and community-based factors, peer relationship and connectedness were commonly addressed (66.7% of studies), along with community relationships and support and friendly spaces (50% of studies). It is important to note that several individual-based resilience factors (e.g., confidence and autonomy) were not addressed as part of interventions yet they have emerged as important in mediating one's resilience.
Semi-structured interviews with key stakeholders revealed the importance of additional factors. Mrs. L. reported that her main concern regarding her son revolves around his transition to high school and his ability to build and sustain peer relationships. She refers to an individual-based factor of self-advocacy, a skill that she wishes to instill in her son.
Mrs. N. reports that the caregiver's internal assets, such as coping, confidence, and self-esteem, are essential:
“Resilience is a skill that is built over time and through experience. So, coping and having good and healthy coping mechanisms is critically important, no question.”
“Having a neurodiverse child impact directly our level of confidence, our level of competence, our level of self-esteem in terms of that role of now being a parent of a child with special needs.”
For Mr. M., the individual factors of negative thoughts and self-talk were impactful when going through adolescent transition:
“I would have negative thoughts that would creep up where it’s a little bit frustrating when I can’t perform as well as I would like to”.
In addition, he reports that one's confidence could be affected and in turn negatively impact resilience:
“Confidence is something that I am always trying to improve. It was never really that high because I was always comparing myself to others”.
This discussion also revealed that future resilience interventions to support adolescents could be delivered in an online format to enhance accessibility and feasibility. Stakeholders also reported that group sessions (in addition to individual sessions) might be beneficial:
Mrs. L.: “Nobody understands you quite like somebody else going through it”.
Mr. M.: “I think there is a lot of benefit in seeing other youth who are in similar situations. The shared experience allows you to learn some techniques that they are using and vice-versa”.
Figure 2 further highlights resilience factors that were reported to be important by key stakeholders (in grey). For the individual-based resilience factor (confidence) we note that although it was identified as critical in the literature (for youth, in 1.9% of studies) and by key stakeholders (for both youth and caregivers), it is not addressed as part of existing interventions.
Other important gaps were identified. Namely, the individual-based resilience factors related to self-identify, spirituality, and moral competence were not examined in any of the observational studies, nor addressed as part of the existing intervention programs.
Discussion
This review sought to synthesize evidence from a wide range of sources to describe influential resilience factors in youth with NDDs and their families as they navigate the transition to adolescence. The review also explored how resilience is addressed as part of targeted interventions and highlighted existing gaps in research and clinical practice. Our findings demonstrated that over the past decade, the concept of resilience among youth with NDDs and their families as they transition into adolescence has been identified as an important topic to understand and develop. A growing body of evidence illustrates that fostering resilience in youth with NDDs and their families is a multifaceted process, with nearly forty emerging essential factors.
Adolescent perspectives
Our findings pinpointed several individual-based protective factors in youth with NDDs that arose from more than 20% of selected observational studies. These include emotional and social competence, positive attitude, emotional regulation, as well as problem-solving and decision-making.
Emotional and social competencies refer to the adolescents' ability to successfully manage their emotional arousal and positively engage in social settings (38). Adolescence is a period of significant growth in which social and emotional development shapes youth's trajectory (39, 40). Fostering one's emotional awareness is foundational to this process; it includes recognizing and labeling feelings, understanding the sources of emotions, and being in touch with one's strengths and weaknesses (41). A recent study examined the associations between emotional competence and prosocial behaviors with peers among children with ASD. Authors found that those with ASD showed significantly lower rates of emotion regulation and use of discrete coping strategies during peer interactions in comparison to their neurotypical peers (42). Another study conducted with neurotypical adolescents evidenced that social competence was associated with emotional intelligence and social anxiety (43). More specifically, youth who had higher emotional intelligence and lower social anxiety demonstrated overall stronger social skills. In addition, it is suggested that these skills are important for adolescents' general engagement in social activities (43). This evidence suggests that social and emotional competencies are integral to positive social relationships. Thus, we propose that skill development in this area should be considered as an integral aspect of future resilience interventions for youth with NDDs and their families.
Our scoping review also determined that emotional regulation was a key resilience factor in adolescents with NDDs, especially given that young people experience a wide range of distinct turbulent emotions (44). Emotional regulation refers to one's ability to not only understand their emotions but also to have control over which emotions are experienced, as well as when and how they are experienced and expressed. In 1994, Thompson explained that “emotion regulation consists of the extrinsic and intrinsic processes responsible for monitoring, evaluating, and modifying emotional reactions, especially their intensive and temporal features, to accomplish one's goals” p. 28–29 (41). It includes recognizing and labelling one's feelings, understanding the triggers for said emotions, and distinguishing between different emotional states (45). In fact, emotional regulation is found to be affected in children (46, 47) and adolescents (48, 49) with NDDs. Nonetheless, emotional regulation, as a resilience factor, was found to be addressed in only 50% of the selected intervention studies, and primarily in adolescents with ASD and ADHD. In relation to that, we identified an important gap in targeted resilience interventions for youth with CP. Indeed, emotional regulation is a major challenge in children with CP that commonly translates and intensifies in adolescence and significantly affects multiple life areas such as peer interactions, relationships and overall mental health (49–52). Consequently, we advocate for future developments in resilience coaching programs for children with physical developmental disabilities, such as CP.
Furthermore, youth's optimism and positive attitudes were found to play a significant role affecting their resilience and well-being. In accordance to our finding, a recent systematic review of 31 studies and a cohort of 46,262 adolescents aged between 13 and 17 years old showed that optimism contributes significantly to their overall mental health (53). The review concluded that optimism and positive attitude act as “buffers against the impact of stress, […] pathological symptoms and risky behaviors” (53). Overall, positive thinking can help adolescents better manage stress and cope with the challenges of this transitional period (54). Similarly to emotional regulation the factor of optimism and positive attitude was addressed in 50% of the intervention studies, and this primarily among youth with ASD, ADHD, and language disorders. Provided that over 30% observational studies have determined this factor to be influential (i.e., second on the list of most common significant factors) and the importance of optimism to overall youth's well-being, we suggest that future coaching interventions supporting resilience ensure its inclusion.
In addition, our review pinpointed that problem-solving and decision-making are equally important factors that contribute to resilience. In fact, youth with NDDs are particularly likely to face challenges in these areas (55, 56). Studies evaluating existing interventions have shown that improving the problem-solving and decision-making skills of teenagers with NDDs can result in improved independence, day-to-day functioning, and general health (57–60). Therefore, optimizing these capabilities has immense potential.
Our review also explored family and peer relationships as key protective home-based and school-based factors. The well-being and resilience of adolescents with developmental impairments is supported by a loving and caring family environment that offers emotional support, open communication, and a consistent schedule (61). Equally important are the experiences and connections adolescents have with peers in the school environment, as positive peer relationships may improve emotional well-being, school achievements (62, 63), psychological adjustment (64, 65), and self-esteem (66, 67). The research suggests that adolescents with NDDs benefit significantly from inclusive educational approaches because they create opportunities for social involvement and acceptance (40).
Finally, it is noteworthy that adolescents with NDDs are known to undergo a heterogeneous and complex process to develop their disability identity (68). Despite the evident importance of this factor as protective (69), our scoping review found that the concept of self-identity was not addressed as part of observational and intervention studies. Adolescents' understanding of their unique circumstances and subsequent implications is just one element that influences their path to positive self-identification, as adolescents' self-esteem may be affected (70, 71). In relation to that, our key stakeholder interviews added a qualitative dimension to this evidence, highlighting the importance of factors like self-advocacy, confidence, and self-esteem in building resilience (individually and relationally) among adolescents with NDDs. Indeed, by fostering self-advocacy through cultivating self-determination, adolescents can be empowered to actively participate in their own treatment and decision-making (72).
Moreover, the discussion with key stakeholders also revealed the potential benefits of remote interventions and group sessions for supporting adolescent transitions, as these formats can enhance accessibility and the shared experience of learning from peers. These results are aligned with previous evidence in the field of pediatric telehealth, which has been shown to be an effective alternative to traditional face-to-face methods and well accepted by caregivers and teens (73). Specifically, to address the mental health of children and youth with NDDs, a call to implement and benefit from online programs has been put forward (74).
Caregiver perspectives
The scoping review also provided valuable insights into the experiences of caregivers who support adolescents with NDDs, highlighting the challenges and opportunities within this context. Notably, some caregivers' perspectives were intertwined with those of adolescents, as they often play a significant role in the lives of their children (61, 75). For instance, many of the included observational studies examined the various situations common during adolescence that may present issues, such as helping their children transition into high school and build and sustain peer relationships. Further, caregiver concerns are often related to the development of individual-based factors in their children, such as self-advocacy, health coping mechanisms and confidence. Interviews with caregivers revealed that their internal assets are essential in supporting their children's internal assets. These findings highlight the significance of caregivers' own well-being and mental health in promoting positive trajectories for their adolescents with developmental disabilities. The stakeholder discussion revealed that having a neurodiverse child can impact caregivers' perceived competence. Thus, more research to support caregivers in developing a positive self-concept is important as only a small number of studies addressed individual-based resilience factors in caregivers themselves. Despite this, there is great potential for positive and inclusive interventions (such as group sessions). These provide an opportunity to share experiences and connect with other caregivers ultimately to better support those with NDDs. It is indisputable that caregivers play a critical role in fostering resilience among adolescents with developmental disabilities, and the multifaceted nature of caregiving for this population cannot be overlooked.
Common perspectives
Developing positive coping strategies emerged as a key theme for both adolescents and caregivers. This demonstrates the importance of developing adaptive mechanisms to navigate the unique challenges associated with NDDs. Self-regulation, both for individuals with NDDs and their caregivers, was similarly identified as important for encouraging healthy emotional regulation and promoting resilience. Previous research suggests that coping strategies are affected in youth with NDDs, where they often “ignore” the issues (60). In caregivers of children and youth with chronic illness, coping strategies were found to correlate with quality of life (76). Beyond employing coping strategies, young individuals with diverse NDDs have conveyed that their sense of well-being hinges on engagement and participation, interpersonal connections, family dynamics, and personal growth (77). Their perception of well-being was found to revolve around feeling supported, included, and respected, while also sensing value and capability (77). In relation to that, our review emphasized the significance of social support, clarifying the need for situation-specific resources and encouraging family environments. Nonetheless, in many studies, cultural considerations were underscored for both adolescents and caregivers. Moving forward, interventions should not only focus on coping strategies but also embrace a holistic approach that acknowledges and integrates diverse cultural backgrounds. This comprehensive approach is crucial for fostering a supportive environment that addresses the multifaceted needs of both individuals with NDDs and their caregivers.
Finally, the evidence reiterated the importance of public policies relating to adolescents with NDDs and their families. For instance, previous work in the field of leisure for children with disabilities highlighted that few policies have specific mechanisms and action plans in place (78). It emerges that there is a need for policy initiatives that not only recognize the diverse challenges faced by adolescents with NDDs and their families but also outline targeted strategies and concrete action plans. These policies should be designed to promote inclusivity, accessibility, and support across various domains, including education and health. By addressing these aspects, policymakers can contribute significantly to fostering an environment that empowers adolescents with NDDs and their families, ensuring their equitable participation and well-being in society.
Future opportunities and limitations
The findings presented above described the state of research and interventions focusing on young people with NDDs and their families, particularly in the context of adolescent resilience. While the existing literature and interventions have made significant contributions, there remain several gaps and areas for improvement. Existing interventions often only speak to the adolescent experience, with limited attention paid to the well-being and resilience of their caregivers. Caregivers play a pivotal role in the lives of these youth and require dedicated support to effectively fulfill their caregiving responsibilities (79, 80). Future work must focus on individual-based factors specific to caregivers, such as self-esteem, self-efficacy, and coping, as they are closely linked to caregivers' ability to provide effective support (and, in turn, influence the resilience of their children).
Adolescent-focused interventions could further prioritize the interconnected nature of family, school, peer, and community-based factors in developing resiliency. A more comprehensive approach would address the broader context to provide a more holistic support system for youth and their families. One way to do so would be to customize interventions to cater to context-specific needs and strengths, rather than falling back on adopting a one-size-fits-all approach to health and well-being. On a similar thread, there is room for increased integration of firsthand perspectives in intervention development. Engaging caregivers and adolescents themselves in the design and evaluation of interventions will lead to more relevant, effective and sustainable solutions (81–83). Moreover, future interventions should be family-centered and address the unique challenges and strengths of both the teen and the caregiver. They should be inclusive and include the necessary tools and resources for both parties. Additionally, as suggested by stakeholders, exploring novel intervention formats (such as an online setting or a group environment) may also make support more accessible and feasible.
Our scoping review has limitations. Despite efforts to be comprehensive, it is possible that some relevant papers were overlooked, as search algorithms may not capture all potential terms used to describe resilience in this population. While a total of five databases were included, there might be a bias towards health-related literature, potentially neglecting to consider relevant studies in other domains. In addition, we conducted individual semi-structured interviews with our stakeholders. A common discussion might have resulted in additional arising themes and ideas. Moreover, we did not include experts in the field in the key stakeholder consultation exercise. Nevertheless, our team is presently launching a nation-wide survey and follow-up semi-structured interviews, exploring topics of interest for a resilience coaching program, from the perspectives of caregivers, young adults with NDDs, and experts in the field.
Conclusion
This scoping review provided a comprehensive overview of the factors influencing resilience in youth with NDDs and their families, offering valuable insights for future research, clinical practice, and policy development in this area. These findings underscore the importance of a holistic and inclusive approach to support young people and their families throughout the complexities involved with the transition to adolescence. This type of review contributes to the ongoing dialogue surrounding adolescent resilience and offers valuable insights for stakeholders seeking to better support this vulnerable population.
The path forward in developing more comprehensive approaches and interventions to research and practice involves recognizing the indispensable role of caregivers, tailoring interventions to specific contexts, and exploring emerging implementation formats. By bridging these gaps and pursuing sustainable change, we can foster greater resilience among adolescents with developmental disabilities and create a more inclusive and supportive environment for their families. This opportunity not only aligns with the findings of the scoping review and current research landscape but also contributes to the ongoing advancement of practical development in this field.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed todGF0aWFuYS5vZ291cnRzb3ZhQG1jZ2lsbC5jYQ==.
Author contributions
NZ: Data curation, Formal Analysis, Investigation, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. EB: Investigation, Validation, Writing – original draft, Writing – review & editing. ML: Writing – original draft, Writing – review & editing. TO: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
TO is supported by the Kids Brain Health Network, the Foundation of the Jewish Rehabilitation Hospital, and the Fonds de Recherche du Québec Santé.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2024.1341740/full#supplementary-material
References
1. Zablotsky B, Black LI, Maenner MJ, Schieve LA, Danielson ML, Bitsko RH, et al. Prevalence and trends of developmental disabilities among children in the United States: 2009–2017. Pediatrics. (2019) 144(4):1–11. doi: 10.1542/peds.2019-0811
2. Olusanya BO, Kancherla V, Shaheen A, Ogbo FA, Davis AC. Global and regional prevalence of disabilities among children and adolescents: analysis of findings from global health databases. Front Public Health. (2022) 10:977453. doi: 10.3389/fpubh.2022.977453
3. Perrin JM, Bloom SR, Gortmaker SL. The increase of childhood chronic conditions in the United States. JAMA. (2007) 297(24):2755–9. doi: 10.1001/jama.297.24.2755
4. Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, et al. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics. (2011) 127(6):1034–42. doi: 10.1542/peds.2010-2989
5. Slomski A. Chronic mental health issues in children now loom larger than physical problems. JAMA. (2012) 308(3):223–5. doi: 10.1001/jama.2012.6951
6. Emerson E, Einfeld S. Emotional and behavioural difficulties in young children with and without developmental delay: a bi-national perspective. J Child Psychol Psychiatry. (2010) 51(5):583–93. doi: 10.1111/j.1469-7610.2009.02179.x
7. Baker BL, Neece CL, Fenning RM, Crnic KA, Blacher J. Mental disorders in five-year-old children with or without developmental delay: focus on ADHD. J Clin Child Adolesc Psychol. (2010) 39(4):492–505. doi: 10.1080/15374416.2010.486321
8. Volkmar FR, Tsatsanis K. Psychosis and psychotic conditions in childhood and adolescence. In: Marsh DT, Fristad MA, editors. Handbook of Serious Emotional Disturbance in Children and Adolescents. Hoboken, NJ, US: John Wiley & Sons, Inc. (2002). p. 266–83.
9. Einfeld SL, Ellis LA, Emerson E. Comorbidity of intellectual disability and mental disorder in children and adolescents: a systematic review. J Intellect Dev Disabil. (2011) 36(2):137–43. doi: 10.1080/13668250.2011.572548
11. Burns JM, Durkin LA, Nicholas J. Mental health of young people in the United States: what role can the internet play in reducing stigma and promoting help seeking? J Adolesc Health. (2009) 45(1):95–7. doi: 10.1016/j.jadohealth.2008.12.006
12. Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. (2007) 369(9569):1302–13. doi: 10.1016/S0140-6736(07)60368-7
13. Smetanin P, Briante C, Khan M, Stiff D, Ahmad S. The life and economic impact of major mental illnesses in Canada: Economic impact of major mental illnesses in Canada. Ottawa, Ontario, Canada (2015). Available online at: https://policycommons.net/artifacts/1218759/the-life-and-economic-impact-of-major-mental-illnesses-in-canada/1771835/ (accessed February 9, 2024).
14. Pandey S, Agarwal S, Scholar R, Professor A. Transition to adulthood for youth with disability: issues for the disabled child and family. J Human Soc Sci. (2013) 17:41–5. doi: 10.9790/0837-1734145
15. Christie D, Viner R. Adolescent development. Br Med J. (2005) 330(7486):301–4. doi: 10.1136/bmj.330.7486.301
16. Marquis SM, McGrail K, Hayes MV. Mental health outcomes among parents of a child who has a developmental disability: comparing different types of developmental disability. Disabil Health J. (2020) 13(2):100874. doi: 10.1016/j.dhjo.2019.100874
17. Gray P, Lancy DF, Bjorklund DF. Decline in independent activity as a cause of decline in children’s mental well-being: summary of the evidence. J Pediatr. (2023) 260:113352. doi: 10.1016/j.jpeds.2023.02.004
18. Howard SJ, Williams KE. Early self-regulation, early self-regulatory change, and their longitudinal relations to adolescents’ academic, health, and mental well-being outcomes. J Dev Behav Pediatr. (2018) 39(6):489–96. doi: 10.1097/DBP.0000000000000578
19. Galla BM, Duckworth AL. More than resisting temptation: beneficial habits mediate the relationship between self-control and positive life outcomes. J Pers Soc Psychol. (2015) 109(3):508. doi: 10.1037/pspp0000026
20. Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proc Natl Acad Sci U S A. (2011) 108(7):2693–8. doi: 10.1073/pnas.1010076108
21. Bierman KL, Nix RL, Greenberg MT, Blair C, Domitrovich CE. Executive functions and school readiness intervention: impact, moderation, and mediation in the head start REDI program. Dev Psychopathol. (2008) 20(3):821–43. doi: 10.1017/S0954579408000394
22. Bogg T, Roberts BW. Conscientiousness and health-related behaviors: a meta-analysis of the leading behavioral contributors to mortality. Psychol Bull. (2004) 130(6):887. doi: 10.1037/0033-2909.130.6.887
23. Duckworth AL, Tsukayama E, May H. Establishing causality using longitudinal hierarchical linear modeling: an illustration predicting achievement from self-control. Soc Psychol Personal Sci. (2010) 1(4):311–7. doi: 10.1177/1948550609359707
24. Woods HC, Scott H. #Sleepyteens: social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. J Adolesc. (2016) 51:41–9. doi: 10.1016/j.adolescence.2016.05.008
25. O'Reilly M, Dogra N, Whiteman N, Hughes J, Eruyar S, Reilly P. Is social media bad for mental health and wellbeing? Exploring the perspectives of adolescents. Clin Child Psychol Psychiatry. (2018) 23(4):601–13. doi: 10.1177/1359104518775154
26. George M. The importance of social media content for teens’ risks for self-harm. J Adolesc Health. (2019) 65(1):9–10. doi: 10.1016/j.jadohealth.2019.04.022
27. Bitsko RH, Claussen AH, Lichstein J, Black LI, Jones SE, Danielson ML, et al. Mental health surveillance among children—United States, 2013–2019. MMWR Suppl. (2022) 71(2):1–42. doi: 10.15585/mmwr.su7102a1
28. Dray J, Bowman J, Campbell E, Freund M, Wolfenden L, Hodder RK, et al. Systematic review of universal resilience-focused interventions targeting child and adolescent mental health in the school setting. J Am Acad Child Adolesc Psychiatry. (2017) 56(10):813–24. doi: 10.1016/j.jaac.2017.07.780
29. Ostaszewski K. The importance of resilience in adolescent mental health promotion and risk behaviour prevention. Int J Public Health. (2020) 65:1221–2. doi: 10.1007/s00038-020-01508-x
30. Fergus S, Zimmerman MA. Adolescent resilience: a framework for understanding healthy development in the face of risk. Annu Rev Public Health. (2005) 26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357
31. Mesman E, Vreeker A, Hillegers M. Resilience and mental health in children and adolescents: an update of the recent literature and future directions. Curr Opin Psychiatry. (2021) 34(6):586. doi: 10.1097/YCO.0000000000000741
32. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8(1):19–32. doi: 10.1080/1364557032000119616
33. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. (2010) 5(1):69. doi: 10.1186/1748-5908-5-69
34. Dray J. Child and adolescent mental health and resilience-focussed interventions: a conceptual analysis to inform future research. Int J Environ Res Public Health. (2021) 18(14):7315. doi: 10.3390/ijerph18147315
35. Masten AS, Lucke CM, Nelson KM, Stallworthy IC. Resilience in development and psychopathology: multisystem perspectives. Annu Rev Clin Psychol. (2021) 17:521–49. doi: 10.1146/annurev-clinpsy-081219-120307
36. Beyond B. Building Resilience in Children Aged 0–12—A Practice Guide. Australia: Beyondblue (2018). 2018-01-23.
37. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. (2008) 62(1):107–15. doi: 10.1111/j.1365-2648.2007.04569.x
38. Ladd GW, Profilet SM. The child behavior scale: a teacher-report measure of young children’s aggressive, withdrawn, and prosocial behaviors. Dev Psychol. (1996) 32(6):1008. doi: 10.1037/0012-1649.32.6.1008
39. Ford ME. Social cognition and social competence in adolescence. Dev Psychol. (1982) 18(3):323. doi: 10.1037/0012-1649.18.3.323
40. Woodgate RL, Gonzalez M, Demczuk L, Snow WM, Barriage S, Kirk S. How do peers promote social inclusion of children with disabilities? A mixed-methods systematic review. Disabil Rehabil. (2020) 42(18):2553–79. doi: 10.1080/09638288.2018.1561955
41. Thompson RA. Emotion regulation: a theme in search of definition. Monogr Soc Res Child Dev. (1994) 59(2–3):25–52. doi: 10.1111/j.1540-5834.1994.tb01276.x
42. Jahromi LB, Kirkman KS, Friedman MA, Nunnally AD. Associations between emotional competence and prosocial behaviors with peers among children with autism spectrum disorder. Am J Intellect Dev Disabil. (2021) 126(2):79–96. doi: 10.1352/1944-7558-126.2.79
43. Inam A, Khalil H, Tahir WB, Abiodullah M. Relationship of emotional intelligence with social anxiety and social competence of adolescents. Nurture. (2014) 8(1):20–9. doi: 10.55951/nurture.v8i1.70
44. Silvers JA. Adolescence as a pivotal period for emotion regulation development. Curr Opin Psychol. (2022) 44:258–63. doi: 10.1016/j.copsyc.2021.09.023
45. Lane RD, Smith R. Levels of emotional awareness: theory and measurement of a socio-emotional skill. J Intell. (2021) 9(3):42. doi: 10.3390/jintelligence9030042
46. Gottman JM, Guralnick MJ, Wilson B, Swanson CC, Murray JD. What should be the focus of emotion regulation in children? A nonlinear dynamic mathematical model of children’s peer interaction in groups. Dev Psychopathol. (1997) 9(2):421–52. doi: 10.1017/S0954579497002113
47. Wilson BJ. Entry behavior and emotion regulation abilities of developmentally delayed boys. Dev Psychol. (1999) 35(1):214. doi: 10.1037/0012-1649.35.1.214
48. Brinke LW T, Schuiringa HD, Matthys W. Emotion regulation and angry mood among adolescents with externalizing problems and intellectual disabilities. Res Dev Disabil. (2021) 109:103833. doi: 10.1016/j.ridd.2020.103833
49. Brossard-Racine M, Waknin J, Shikako-Thomas K, Shevell M, Poulin C, Lach L, et al. Behavioral difficulties in adolescents with cerebral palsy. J Child Neurol. (2013) 28(1):27–33. doi: 10.1177/0883073812461942
50. Weber P, Bolli P, Heimgartner N, Merlo P, Zehnder T, Kätterer C. Behavioral and emotional problems in children and adults with cerebral palsy. Eur J Paediatr Neurol. (2016) 20(2):270–4. doi: 10.1016/j.ejpn.2015.12.003
51. Sigurdardottir S, Indredavik MS, Eiriksdottir A, Einarsdottir K, Gudmundsson HS, Vik T. Behavioural and emotional symptoms of preschool children with cerebral palsy: a population-based study. Dev Med Child Neurol. (2010) 52(11):1056–61. doi: 10.1111/j.1469-8749.2010.03698.x
52. Whittingham K, Bodimeade HL, Lloyd O, Boyd RN. Everyday psychological functioning in children with unilateral cerebral palsy: does executive functioning play a role? Dev Med Child Neurol. (2014) 56(6):572–9. doi: 10.1111/dmcn.12374
53. Rincon Uribe FA, Neira Espejo CA, Pedroso J. The role of optimism in adolescent mental health: a systematic review. J Happiness Stud. (2022) 23(2):815–45. doi: 10.1007/s10902-021-00425-x
54. Gloria CT, Steinhardt MA. Relationships among positive emotions, coping, resilience and mental health. Stress Health. (2016) 32(2):145–56. doi: 10.1002/smi.2589
55. Wehmeyer ML, Kelchner K. Interpersonal cognitive problem-solving skills of individuals with mental retardation. Educ Train Mental Retardat Dev Disabil. (1994) 29(4):265–78.
56. Agran M, Blanchard C, Wehmeyer M, Hughes C. Increasing the problem-solving skills of students with developmental disabilities participating in general education. Remedial Spec Educ. (2002) 23(5):279–88. doi: 10.1177/07419325020230050301
57. Mackay BA, Shochet IM, Orr JA. A pilot randomised controlled trial of a school-based resilience intervention to prevent depressive symptoms for young adolescents with autism Spectrum disorder: a mixed methods analysis. J Autism Dev Disord. (2017) 47(11):3458–78. doi: 10.1007/s10803-017-3263-5
58. Shochet IM, Saggers BR, Carrington SB, Orr JA, Wurfl AM, Kelly RL, et al. A school-based approach to building resilience and mental health among adolescents on the autism spectrum: a longitudinal mixed methods study. Sch Mental Health Multidiscipl Res Pract J. (2022) 3:753–75. doi: 10.1007/s12310-022-09501-w
59. Ahmadi N, Chaudhry S, Salam T, Rodriguez J, Kase M, Olango G, et al. A randomized controlled feasibility trial of reminder-focused positive psychiatry in adolescents with comorbid attention-deficit/hyperactivity disorder and posttraumatic stress disorder. Prim Care Companion CNS Disord. (2020) 22(5):23035. doi: 10.4088/PCC.19m02579
60. Firth N, Frydenberg E, Steeg C, Bond L. Coping successfully with dyslexia: an initial study of an inclusive school-based resilience programme. Dyslexia. (2013) 19(2):113–30. doi: 10.1002/dys.1453
61. Hadiloo N. Enhancing psychological development in children with disabilities: the power of environment and family. Eur J Med Health Sci. (2023) 5(5):108–17. doi: 10.34104/ejmhs.023.01080117
62. Buhs ES, Ladd GW. Peer rejection as antecedent of young children’s school adjustment: an examination of mediating processes. Dev Psychol. (2001) 37(4):550. doi: 10.1037/0012-1649.37.4.550
63. Wentzel KR. Sociometric status and adjustment in middle school: a longitudinal study. J Early Adolesc. (2003) 23(1):5–28. doi: 10.1177/0272431602239128
64. Hymel S, Rubin KH, Rowden L, LeMare L. Children’s peer relationships: longitudinal prediction of internalizing and externaliziing problems from middle to late childhood. Child Dev. (1990) 61(6):2004–21. doi: 10.1111/j.1467-8624.1990.tb03582.x
65. Ladd GW, Troop-Gordon W. The role of chronic peer difficulties in the development of children’s psychological adjustment problems. Child Dev. (2003) 74(5):1344–67. doi: 10.1111/1467-8624.00611
66. Aftab MJ, Iqbal MN, Rehman NU, Sani R. Impact of peer relationship on the self-concept of children with multiple disabilities in Pakistan. J Educ Sci. (2021) 8(1):218–32.
67. McCarroll EM, Lindsey EW, MacKinnon-Lewis C, Chambers JC, Frabutt JM. Health status and peer relationships in early adolescence: the role of peer contact, self-esteem, and social anxiety. J Child Fam Stud. (2009) 18:473–85. doi: 10.1007/s10826-008-9251-9
68. Forber-Pratt AJ, Minotti BJ, Burdick CE, Kate Brown M, Hanebutt RA. Exploring disability identity with adolescents. Rehabil Psychol. (2021) 66(4):550. doi: 10.1037/rep0000411
69. Bogart KR. Disability identity predicts lower anxiety and depression in multiple sclerosis. Rehabil Psychol. (2015) 60(1):105. doi: 10.1037/rep0000029
70. Miyahara M, Piek J. Self-esteem of children and adolescents with physical disabilities: quantitative evidence from meta-analysis. J Dev Phys Disabil. (2006) 18:219–34. doi: 10.1007/s10882-006-9014-8
71. Williamson S, Craig J, Slinger R. Exploring the relationship between measures of self-esteem and psychological adjustment among adolescents with Asperger syndrome. Autism. (2008) 12(4):391–402. doi: 10.1177/1362361308091652
72. Berglund Melendez A, Malmsten M, Einberg EL, Clausson EK, Garmy P. Supporting students with neurodevelopment disorders in school health care-school nurses’ experiences. Int J Environ Res Public Health. (2020) 17(16):5752. doi: 10.3390/ijerph17165752
73. Ogourtsova T, Boychuck Z, O'Donnell M, Ahmed S, Osman G, Majnemer A. Telerehabilitation for children and youth with developmental disabilities and their families: a systematic review. Phys Occup Ther Pediatr. (2023) 43(2):129–75. doi: 10.1080/01942638.2022.2106468
74. Ogourtsova T. Telerehabilitation for the mental health of children with physical disabilities and their families: let’s Look out the window of opportunity! Phys Occup Ther Pediatr. (2023) 43(2):176–81. doi: 10.1080/01942638.2022.2130023
75. Iacob CI, Avram E, Cojocaru D, Podina IR. Resilience in familial caregivers of children with developmental disabilities: a meta-analysis. J Autism Dev Disord. (2020) 50(11):4053–68. doi: 10.1007/s10803-020-04473-9
76. Fairfax A, Brehaut J, Colman I, Sikora L, Kazakova A, Chakraborty P, et al. A systematic review of the association between coping strategies and quality of life among caregivers of children with chronic illness and/or disability. BMC Pediatr. (2019) 19:1–16. doi: 10.1186/s12887-019-1587-3
77. Foley K-R, Blackmore A, Girdler S, O’Donnell M, Glauert R, Llewellyn G, et al. To feel belonged: the voices of children and youth with disabilities on the meaning of wellbeing. Child Indic Res. (2012) 5:375–91. doi: 10.1007/s12187-011-9134-2
78. Shikako-Thomas K, Law M. Policies supporting participation in leisure activities for children and youth with disabilities in Canada: from policy to play. Disabil Soc. (2015) 30(3):381–400. doi: 10.1080/09687599.2015.1009001
79. Isa SNI, Ishak I, Ab Rahman A, Saat NZM, Din NC, Lubis SH, et al. Health and quality of life among the caregivers of children with disabilities: a review of literature. Asian J Psychiatr. (2016) 23:71–7. doi: 10.1016/j.ajp.2016.07.007
80. Murphy NA, Christian B, Caplin DA, Young PC. The health of caregivers for children with disabilities: caregiver perspectives. Child Care Health Dev. (2007) 33(2):180–7. doi: 10.1111/j.1365-2214.2006.00644.x
81. Ogourtsova T, Gonzalez M, Zerbo A, Gavin F, Shikako K, Weiss J, et al. Lessons learned in measuring patient engagement in a Canada-wide childhood disability network. Res Involv Engagem. (2024) 10(18):1–26. doi: 10.1186/s40900-024-00551-9
82. Ogourtsova T, O’Donnell ME, Filliter JH, Wittmeier K, Group BC, Majnemer A, et al. Patient engagement in an online coaching intervention for parents of children with suspected developmental delays. Dev Med Child Neurol. (2021) 63(6):668–74. doi: 10.1111/dmcn.14810
Keywords: resilience, adolescents with developmental disabilities, caregivers, wellbeing, scoping review, youth mental health
Citation: Zukerman N, Bottone E, Low M and Ogourtsova T (2024) Resilience and adolescence-transition in youth with developmental disabilities and their families: a scoping review. Front. Rehabil. Sci. 5:1341740. doi: 10.3389/fresc.2024.1341740
Received: 20 November 2023; Accepted: 15 February 2024;
Published: 27 February 2024.
Edited by:
Paula Silva de Carvalho Chagas, Universidade Federal de Juiz de Fora, BrazilReviewed by:
Lu Lu, National Taiwan University Hospital, TaiwanCamila Santana, Federal University of São Carlos, Brazil
© 2024 Zukerman, Bottone, Low and Ogourtsova. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tatiana Ogourtsova dGF0aWFuYS5vZ291cnRzb3ZhQG1jZ2lsbC5jYQ==
 Naomi Zukerman
Naomi Zukerman Emily Bottone
Emily Bottone Maya Low
Maya Low Tatiana Ogourtsova
Tatiana Ogourtsova