- 1Department of Surgery, College of Medicine and Health Sciences, University of Rwanda, Kigali, Rwanda
- 2Physiotherapy Department, University of the Witwatersrand, Johannesbourg, South Africa
- 3Department of Environmental, College of Medicine and Health Sciences, University of Rwanda, Kigali, Rwanda
- 4Physiotherapy Department, College of Medicine and Health Sciences, University of Rwanda, Kigali, Rwanda
- 5Department of Epidemiology and Biostatistics, Imperial College London, London, United Kingdom
Background: Road traffic injuries (RTIs) leading to long-term disability present a significant public health challenge, causing immense personal and societal consequences. Every year, 50 million people are hurt, 1.2 million die, 30% are permanently disabled, and 14% cannot return to work due to road traffic accidents. However, in many developing countries, information on the social integration of patients post-RTI remains limited. This study aimed to identify factors contributing to social integration following road traffic-related orthopedic injuries (RTOI) in Rwanda.
Methodology: A multicenter, cross-sectional study included 369 adult Road traffic orthopedic injuries (RTOI) victims from five Rwandan referral hospitals. Participants completed the IMPACT-S Questionnaire between 2 June 2022, and 31 August 2022, two years after the injury. It measured social integration in terms of activities and paricipation. We used logistic regression statistical analysis with a significance level of p < 0.05 to estimate odds ratios (OR) and 95% confidence intervals (CI). The Institutional Review Board for Health Sciences and Medicine at the University of Rwanda College of Medicine ethically authorized this study. Participants signed a written consent form before participating in the study. The data was kept private and was used only for this study.
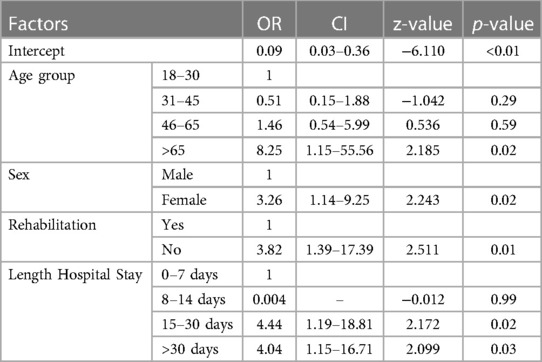
Results: The study's findings indicated that the mean age of RTOI victims was 37.5 ± 11.26 years, with a notable male predominance over females. Of the participants, 5.69% were unable to resume normal life activities. The overall mean score on the IMPACT-S scale was moderate, at 77 ± 17. Specifically, participants achieved an average score of 76 ± 16 for “activities” and a higher average of 84 ± 16 for “participation.” Certain factors were associated with poor social integration compared to others, including belonging to the age group above 65 years (OR = 8.25, p = 0.02), female sex (OR = 3.26, p = 0.02), lack of rehabilitation (OR = 3.82, p = 0.01), and length of hospital stay >15 days (OR = 4.44, p = 0.02).
Conclusion: The majority of RTOI victims in Rwanda achieved successful reintegration into society; nevertheless, their mobility and community engagement were more significantly impacted compared to other aspects assessed by the IMPACT-S scale. The study emphasized the importance of early management, effective rehabilitation, and prompt patient discharge from the hospital in facilitating a successful return to everyday life after road traffic-related orthopedic injuries.
Background
Long-term disability resulting from Road Traffic Injuries (RTIs) is a pressing public health concern with devastating effects on individuals and significant societal and economic impacts worldwide (1, 2). Annually, around 50 million people suffer injuries and 1.2 million lose their lives due to road traffic accidents, leaving 30% of survivors with permanent disabilities and 14% unable to return to work (3–5). This primarily affects the working-age population in low and middle-income countries (LMICs), creating profound consequences for individuals, society, and the economy (6).
Effective management of injured patients aims to restore their normal functioning, and various biopsychosocial factors influence post-RTI functional outcomes (7, 8). Social integration of patients post-RTI is a key outcome of successful management, and early psychological support and educating family members play vital roles in promoting social reintegration (6, 9, 10). The International Classification of Functioning, Disability, and Health (ICF) defines participation in life as a crucial health outcome, encompassing an individual's involvement in society's usual activities (11).
Social integration, as defined by the ICF, necessitates interventions to facilitate interaction with the environment for optimal performance in an individual's life (12–14). Various instruments, such as the IMPACT-S questionnaire, measure participation and activities following the ICF guidelines (15). However, individuals with disabilities may encounter challenges in acceptance by their families, limited job opportunities, and difficulties in reintegrating into society (16–18). Adequate rehabilitative care is essential for positive functional outcomes and social reintegration, particularly in LMICs (19).
More than 38.5% of RTI victims in Sierra Leone, Rwanda, Nepal, and Uganda suffered disability, with head and extremities injuries being most common (20). Disability after RTIs in poor countries is affected by injury severity and economic variables, notably for victims' families (2). Road traffic disability affect 1.2%–14% of victims in many developing nations, mostly from low-income households (21, 22).
Rwanda, with 13 million inhabitants and Kigali as its capital, is in Sub-Saharan Africa. Congenital, Genocide against Tutsi victims, and other RTIs made for 5% of Rwandan disability in 2022 (23). The Rwanda National Police reported 4661 road accident injuries and 700 fatalities in 2019 among them a half had orthopedic injuries and 35.6% had permanent and 36% could not return to work (24). Poor post-injury care impairs victims' functional and social reintegration, especially in LMICs (25). Rwanda has many RTI victims (20), few rehabilitation facilities, and few rehabilitation professionals at health institutions, which impacts victim outcomes (26).
This study employs the IMPACT-S questionnaire to identify factors contributing to social integration after road traffic orthopedic injuries (RTOI) in Rwanda, aiming to shed light on improving outcomes and addressing the challenges faced by RTOI victims in the country.
Methodology
Study design and study settings
A multi-centre cross-sectional study was undertaken to analyze hospital-based data on road traffic-related orthopaedic injuries (RTOI) that occurred in 2019 and were treated at the five Rwandan referral hospitals. These hospitals are referral and teaching hospitals with emergency, orthopaedic, mental health departments, and rehabilitation services. The study took place from the 2 June 2022 to 31 August 2022, two years after the injuries occurred, at Centre Hospitalier Universitaire de Kigali (CHUK), Rwanda Military Hospital (RMH), and King Faisal Hospital (KFH), all located in Kigali City, but which receive patients from across Rwanda. The other two hospitals are Centre Hospitalier Universitaire (CHUB) in the Southern Province and Ruhengeri Hospital (RH) in the Northern Province.
Study population and sample size
The study population comprised 2019 road traffic injury (RTI) survivors aged 18 and above admitted to the above five hospitals for both upper and lower limbs injuries. According to the records of the above five mentioned hospitals, around 4,600 cases post-RTIs with 1986 orthopaedic injuries were admitted during the selected study period. We used Krejcie and Morgan's formula (27) for sample calculation and random sampling for sample size. The sample size representative of these RTOI victims was 369.
We consulted the hospital records from the emergency departments, outpatients and admission for patients' demographics and contacts, details of the injury pattern, and the length of stay in the hospital. We excluded participants who were not oriented to time and space and could not respond to the questionnaire and patients with injuries other than orthopaedic. Those fulfilling the inclusion criteria of being above 18 years and having an orthopaedic road injury in 2019 were contacted via telephone for their demographic details and requested to come to the hospital for further evaluation.
Psychometric properties of the instruments
Participation and activities (Social integration) were evaluated using IMPACT-S (ICF Measure of Participation and ACTivities), an ICF-based participation tool called Patient Reported Outcome Measures (PROMS). The measure is designed to describe functioning and disability independent of health conditions and guide the participation level of patients with disabilities. This tool consists of 32 items grouped into nine domains (learning and applying knowledge, general tasks and demands, communication, mobility, self-care, domestic life, interpersonal interactions and relationships, major life areas, community, social and civic life). The IMPACT-S also has two sub-total scores for Activities and Participation and one IMPACT-S total score. All summary scores were averaged item scores, converted into 0–100 scales. Higher IMPACT-S scores reflect better functioning (or less disability), meaning nearly entirely socially reintegrated in life after a road traffic injury.
This tool was validated by Marcel Post et al. 2008, in 197 road traffic survivors (28) with good psychometric properties according to the ICF framework. The IMPACT-S tool has been validated in conditions like carpal tunnel syndrome (29) and many languages, including Turkish (30). Amir Javanmard et al. 2020 compared six instruments used in the participation and activities evaluation for patients with spinal cord injuries and found that the IMPACT-Shas had higher psychometric measures than other instruments (31). The questionnaire was translated from English to Kinyarwanda by two language experts and back to English by two other language experts to address the cultural and linguistic equivalence, and the responses were the same. Also, we sent the questionnaire to experts in orthopaedic and rehabilitation for their opinion on the quality of translation, clarity and suitability for the Rwandan participants.
Procedure
Of the 1986 patients with orthopaedic injuries, we contacted 1,721 on the phone; some had died, or their phones malfunctioned. The severity of the injury was evaluated using the Kampala Trauma Score (KTS), which is classified as mild, moderate and severe. After sampling, participants were invited to the hospital to assess their current status after almost two years post-RTIs. Using the IMPACT-S questionnaire, we measured the patient's overall level of social integration (participation and activities) after road traffic orthopaedic injuries in Rwanda. Participants filled out the questionnaire by considering how much their impairments interfered with their lives in the last 30 days before the interview. They answered on a 4-point response scale from 0 to 3 (Extreme, considerable, some and no limitations), and the research assistants helped the participants to complete the questionnaire if they could not write.
We calculated each IMPACT-S domain's mean and standard deviation (learning and applying knowledge, general tasks and demands, communication, mobility, self-care, domestic life, interpersonal interactions and relationships, major life areas, community, social and civic life). The participant's socioeconomic status (Ubudehe) was collected according to the Rwanda government classification, where category I include impoverished and vulnerable citizens. Category II includes citizens who can afford some form of rented or owned accommodation but are not gainfully employed and can only afford to eat once or twice a day. Category III includes citizens who were gainfully employed or employers of labour. Category IV are citizens who are chief executive officers of big businesses, full-time employees with organisations, industries or companies, government employees, owners of shops or markets and owners of commercial transport vehicles or trucks (32).
The study's primary outcome is social integration (activities and participation). The risk factors include demographic data, the Kampala Trauma Scale, length of hospital stay, and rehabilitation.
Data management and statistical analysis
Data were collected using the questionnaires, entered into a computer by a Google form data entry mode, and analysed using the R Software. We performed a descriptive analysis of the patient-reported outcome measure scale (IMPACT-S). Categorical variables were summarised using frequencies and percentages, continuous variables with means and standard deviations (SD). We used a student's t-test to compare continuous variables and the Chi-Square test for nominal (categorical) variables. We utilised multivariate logistic regression to assess associations between risk factors and IMPACT-S score categories. We considered the p-value <0.05 to be statistically significant.
Ethical consideration
We obtained ethical approval to conduct the study from the University of Rwanda, College of Medicine and Health Sciences Institutional Review Board (18/CMHS IRB/2022). The Rwanda National Research Committee operating in the Ministry of Health approved this study (NHRC/2022/PROT/014), and we collaborated with the Rwanda Biomedical Center (5535/RBC/2022) injury department. We obtained local ethical approvals from the five hospitals' ethics committees; CHUK(EC/CHUK/051/2022), CHUB (REC/UTHB/089/2022), RH(313/RRH/DG/2022), KFH(EC/KFH/015/2022), RMH(RMH IRB/027/2022). We obtained written consent from all participants before enrollment into the study, after explaining the purpose of the study, and all data were kept confidential and only used for the purpose of this study.
Results
Demographic characteristics of the participants
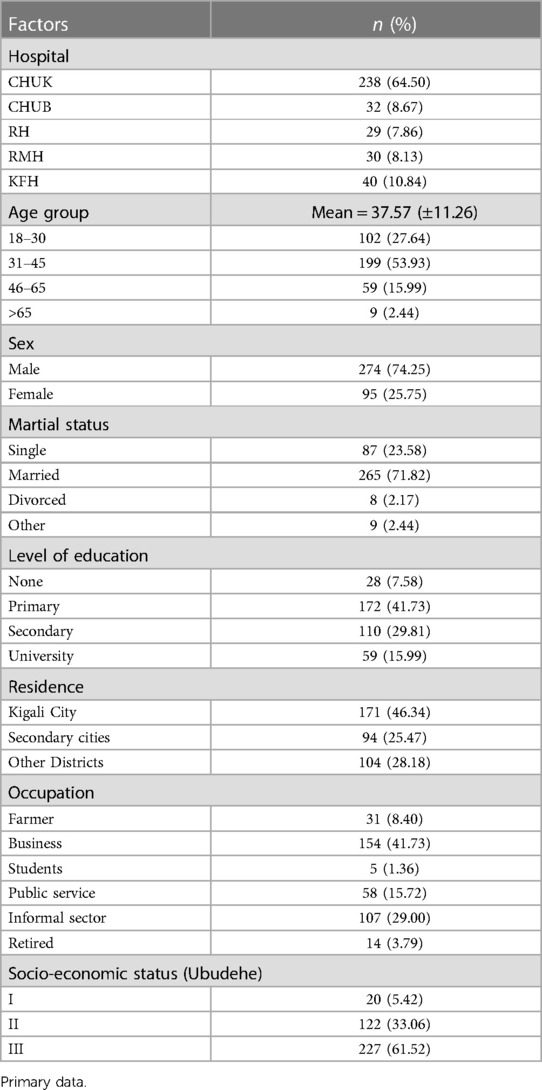
Based on the data provided in Table 1, a total of 369 individuals responded to the survey. Among these, 64.5% (238 participants) were recruited from CHUK. The average age of all participants was 37.5 ± 11.26 years, with the majority falling within the age range of 31–50 years. Males constituted the majority at 74.25%. Approximately 41.73% (172) of all participants attended primary school, and 46.34% (171) resided in Kigali city. A significant portion, 41.73% (154), were engaged in business, while 29% (107) were part of the informal sector without fixed employment. The majority of our participants belonged to category III of the socioeconomic class (Ubudehe), comprising 61.52% (227) of individuals. This was followed by category II, which represented 33.06% of the participants. Additionally, 61.52% of the reported injuries were associated with motorcycle-related accidents.
Clinical factors
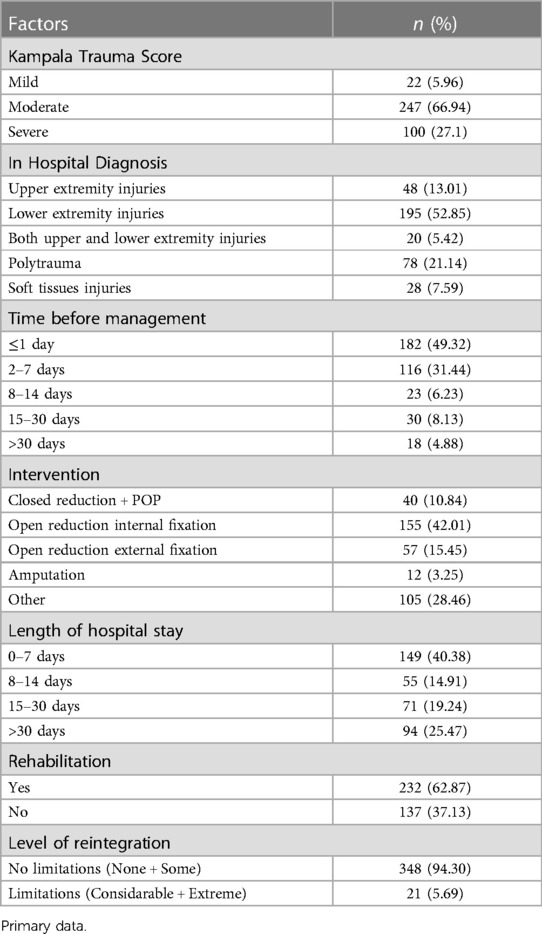
Table 2 shows that 52.85% (195) of all participants had isolated lower limb injuries, while polytrauma represented 21.14% (78) of cases. Half of our participants were managed within one day (49.32%), with a mean treatment duration of 30 days, and 42.01% (155) were treated with Open Reduction and Internal Fixation (ORIF). Regarding hospital stay, about 55.29% (204) were discharged within 14 days, and the mean hospital stay was 30 days. Our findings indicate that 66.84% (246) had a moderate Kampala Trauma Score (KTS). After completing their injury treatment, 37.13% of the participants were unable to undergo rehabilitation, and 5.69% experienced limitations in integrating into Rwandan society.
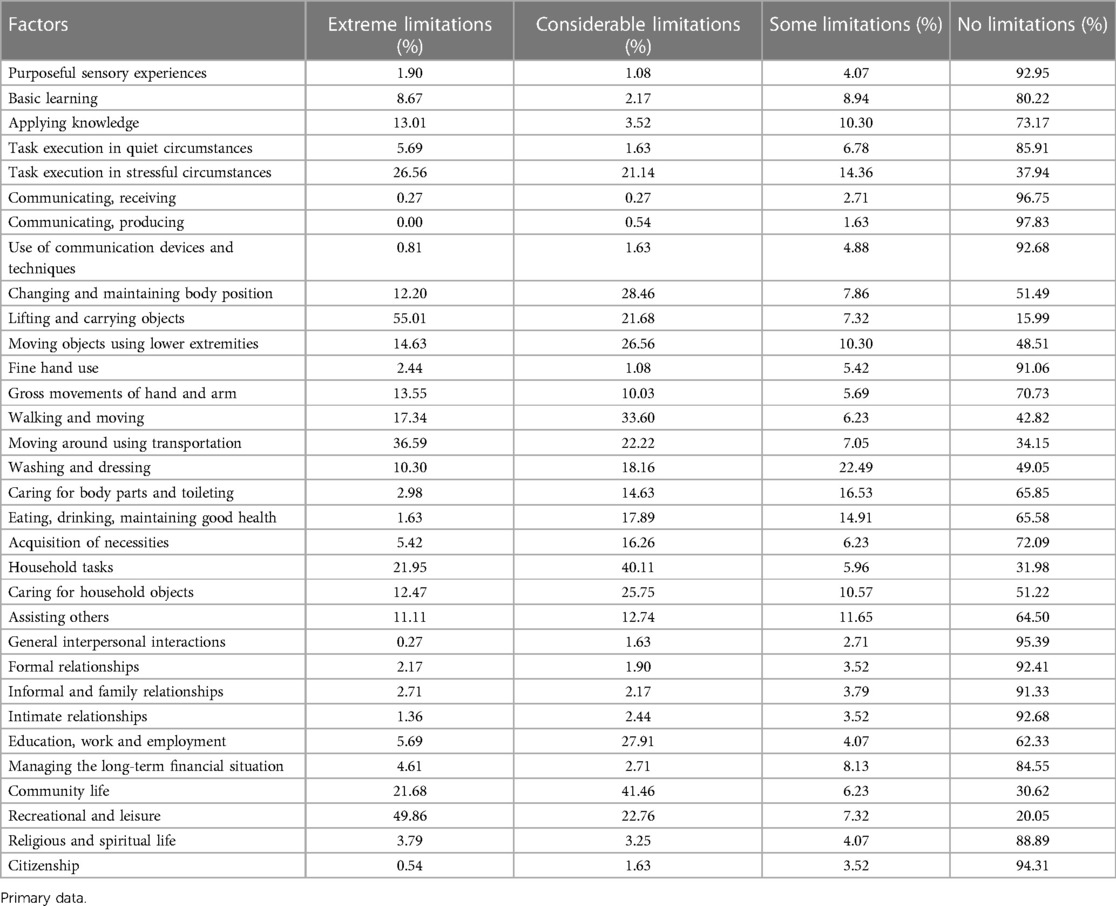
The IMPACT-S Table 3 provides a complete overview of many situations and the accompanying levels of limitation experienced by people. As an example, a substantial majority of persons have no limitations in the areas of “Purposeful sensory experiences” (92.95%) and “Communicating, receiving” (96.75%). On the other hand, it is important to acknowledge that there are more significant limitations seen in tasks such as “Lifting and carrying objects” (55.01%) and “Recreational and leisure” (49.86%). Multiple categories, such as “Household tasks” and “Community life,” suggest that a considerable fraction of adults have notable limitations, with corresponding percentages of 40.11% and 41.46%. The data shown in the table indicates that although a significant number of individuals do not have limitations in different activities, a substantial fraction of the population encounters significant challenges in certain important tasks and relationships.
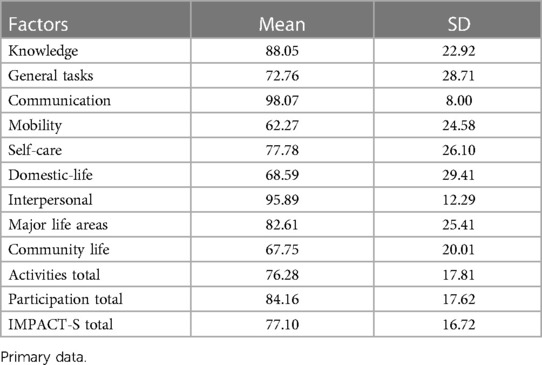
Table 4 shows that the results obtained from the IMPACT-S summary scores reveal that people have shown diverse experiences throughout several domains of their life. The mean scores obtained for Knowledge (M = 88.05, SD = 22.92), Communication (M = 98.07, SD = 8.00), and Interpersonal relationships (M = 95.89, SD = 12.29) demonstrate strong findings within these particular areas. However, it is important to note that there are significant challenges reported in the areas of Mobility (62.27 ± 24.58), Domestic-life (68.59 ± 29.41), and Community life (67.75 ± 20.01). The research participants exhibited a reasonable level of management across all areas, as shown by the mean IMPACT-S score of 77.10 ± 16.72. This highlights the importance of ongoing rehabilitation and support for the victims.
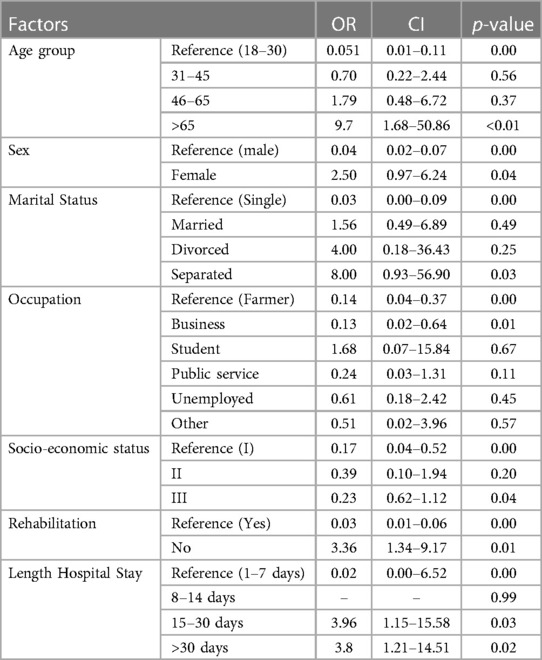
IMPACT-S scored 0 for extreme limitations, 1 for considerable limitations, 2 for some limitations, and 3 for no limitations. The binary score combined extreme and considerable limitations into one category labelled as a limitation (score 1), while the remaining categories were combined and labelled as no limitation (score 0). Poor social integration was associated with the age group >65 years (p-value <0.01) and female sex (p-value = 0.04). Marital status for separated couples (p-value = 0.03), people in the business category (p-value = 0.01), socioeconomic status category III (p-value = 0.04), lack of rehabilitation management (p-value = 0.01), and length of hospital stay (p-value = 0.02) were also identified as factors negatively affecting social integration (Table 5).
Table 6 is about the The multivariate logistic regression study of IMPACT-S and related covariates yields numerous noteworthy conclusions. The model's intercept has an OR of 0.09, which is substantially different from zero with a p-value of less than 0.01. This shows that the social integration restriction probabilities are 0.09 times the reference group odds when all predictors are at their reference levels. Individuals over 65 had a considerably greater chances (OR = 8.25, p = 0.02) of social integration restriction than the reference group (18–30 years old). Women are 3.26 times more likely than men (p = 0.02) to have social integration issues.
Rehabilitation status is important because people who did not undertake rehabilitation are 3.82 times more likely to have social integration (p = 0.01). Another indicator is hospital stay length. Patients with a hospital stay of 15–30 days and those with a stay longer than 30 days are more likely to have social integration problems, with ORs of 4.44 (p = 0.02) and 4.04 (p = 0.03), respectively, compared to those with a stay of 0–7 days. Notably, the 8–14 day hospital stay group had similar chances to the reference group (p = 0.99). In conclusion, our model shows that older age (>65), female gender, not receiving rehabilitation, and longer hospital stays (15–30 days or >30 days) are substantially linked with social integration problems.
Discussion
Our study aimed to determine the level of social integration (activities and participation) following road traffic orthopaedic injuries (RTOI) in Rwanda. The findings of our study revealed several significant factors contributing to limitations in social integration after RTIs in Rwanda, including the age group above 65, female sex, lack of rehabilitation, and a hospital stay of more than two weeks.
In 2019, half of the road traffic injuries in Rwanda were limb trauma, consistent with findings from other studies conducted in LMICs (33, 34). Males were more predominant than females, which can be explained by the higher mobility of men and their greater involvement in general activities in Rwanda, a pattern observed in other Sub-Saharan African countries as well (35–37). Globally, road traffic injury victims are typically in the working age group (38–40) with fewer unemployed (41–43) and our study confirmed this finding. The mean age of our participants was 37.5 years, with a predominant representation in the age group of 31–50 years. The results of our study indicate that the majority of the RTI victims were able to integrate back into their daily activities after the accident.
More than half of the participants in our study belonged to socioeconomic class category III, which included individuals who were gainfully employed or even employers themselves. This finding highlights the association between accidents and a high rate of movement among the victims. Motorcycles were identified as the leading cause of accidents, followed by motor vehicles. As of 2021, there were over 100,000 motorcycles in Rwanda, with half of them operating as moto-taxis (44). It is noteworthy that more than half of the victims in our study had lower limb injuries, and a quarter of them experienced polytrauma at the time of injury. This trend aligns with findings from studies conducted in LMICs, where lower limb injuries are commonly observed in road traffic injuries (45, 46). Among the orthopaedic injuries, more than half of the cases required surgical intervention, either through open reduction and internal fixation or external fixation. The average hospital stay for the participants was 30 days. It is important to note that polytrauma patients who required multiple interventions tended to have extended hospital stays.
Our findings showed that half of our participants were managed within one day (49.32%), with a mean of 30 days and 42.01% were treated by Open Reduction and Internal Fixation (ORIF). The majority were discharged within 14 days (40.38%), mean hospital stay was 30 days 246/368 (66.84%) had moderate Kampala Trauma Score (KTS). After injury treatment, 37.13% of the victims could not undergo any rehabilitation management. For our study, 37% of the prescribed rehabilitation was not done after injury management, primarily due to financial issues and the long distance between their homes and the district hospitals. The same findings were observed in other studies from LMICs where access to rehabilitation ranges from 5%–59%, and in many countries, rehabilitation centres are lacking (47–49). Lack of rehabilitation in post-RTOI has been associated with a low rate of return to work through a significant impact on the activities and participation of the victims, which is the case in our findings. Many researchers have suggested community-based rehabilitation in post-RTI for complete social integration (50–52).
The primary outcome of this study was the evaluation of social integration using the Measure of Participation and Activities Screener (IMPACT-S). The results indicated that participants had higher scores in the category of no limitations for activities such as communication and production, while the lowest scores were observed in the category of lifting and carrying objects, suggesting that participants were more comfortable with communication tasks compared to tasks that required physical strength. Participants who had some limitations in activities and participation performed relatively well in communication and production but faced difficulties with tasks related to washing and dressing. The category of considerable limitations included participants who encountered significant challenges in executing community life activities, struggling with various daily tasks. More than half of the participants experienced extreme limitations when it came to lifting and carrying objects. These findings underscore the impact of road traffic orthopaedic injuries on important aspects of daily life.
The study findings revealed that while participants scored high in terms of social participation, they faced difficulties in performing activities. This can be attributed to the focus of our research on orthopaedic injuries, which predominantly affect the limbs compared to other body systems. These findings align with similar studies conducted in different countries, such as the study by M. Post et al. in 2008, which validated the IMPACT-S tool. Ahmed Nour et al. (2023) conducted a study in Cameroon and found that more than 39% of patients with limb injuries experienced difficulties with activities of daily living (28, 53).These findings emphasize the need to improve rehabilitation services from the early stages of post-road traffic injuries to address the limitations in activities and promote better social integration.
Studies have consistently shown that the IMPACT-S tool is the most effective tool for summarizing all chapters of the International Classification of Functioning, Disability and Health (ICF) when compared to other tools (15, 31). The IMPACT-S tool consists of nine domains and two subtotals.In this study, the overall IMPACT-S mean score was found to be good for the participants, which is consistent with findings reported by other authors who have also used this tool. These authors have explained that the level of activities and participation becomes acceptable after accidents (29, 30).
Among the domains of the IMPACT-S tool, communication had a higher mean score compared to mobility, which had a lower mean across all domains. This can be explained by the high number of lower limb injuries observed in this study, which is consistent with findings from other studies (28, 30). Furthermore, the activity domain had a lower mean for the IMPACT-S subtotal compared to the participation domain. These findings can be attributed to the specific injuries sustained by these patients at the time of the accident.
After calculating the IMPACT-S scores, we analyzed the factors associated with activities and participation using a binary score. In this scoring system, scores 0 and 1 were combined to represent limitations, while scores 2 and 3 were grouped into 1 to indicate no limitations. Several factors were found to be associated with limitations in social integration. These included being above 65 years of age, female sex, being in a separated marital status, belonging to the business category for occupation, and falling into socioeconomic status category III. These findings provide insights into the univariate factors that can help explain the long-term outcomes of victims of road traffic orthopaedic injuries (RTOI) and their ability to return to everyday life.
Among the clinical factors, the lack of rehabilitation management was also found to contribute to limitations in social integration and longer hospital stays. These factors align with findings from other studies that have identified them as predictors of poor participation and activities in post-RTI scenarios in low- and middle-income countries (LMICs) (48, 54).
Social integration following road traffic injuries (RTIs) is a critical health outcome influenced by various factors. Through multiple logistic regression analysis, we have identified the factors that contribute to limitations in social integration among individuals post-accident. Among these factors, the age group above 65 years was found to contribute eight times more to social integration limitations compared to other age groups. Additionally, females were found to contribute three times more to these limitations compared to males. Lack of rehabilitation had a significant impact, contributing nearly four times more to limitations in social integration compared to attending rehabilitation sessions.
Furthermore, the length of hospital stay has been shown in other studies to be a determinant of social integration following RTOI (17, 45). In our study, a hospital stay of more than two weeks contributed four times more to social integration limitations compared to individuals who spent less than two weeks in the hospital. These findings highlight the importance of considering these factors in understanding and addressing limitations in social integration among individuals recovering from RTOI.
This study will serve as a foundation for future research aimed at assessing the quality of life of individuals with long-term disabilities resulting from orthopedic injuries sustained in road traffic accidents. The findings from this study will provide valuable insights for stakeholders in developing policies and interventions to enhance activities and participation after road traffic injuries (RTIs). Social reintegration following Rwandan road traffic accident-related orthopedic injuries requires a comprehensive approach. After RTIs, efficient treatment should prioritize early hospital discharge and a personalized rehabilitation plan. Victims of Road RTOI breaches need financial aid to overcome their problems and get necessary medical care and support. Additionally, reducing road traffic injury disability rates must be prioritized. Rehabilitative programs and community support networks may help resume everyday activities quickly. Comprehensively evaluating these factors may promote social reintegration and quality of life for Rwandans with orthopaedic injuries from road accident occurrences.
Our study has identified several limitations that should be acknowledged. Firstly, there was a two-year gap between the time of injury and the assessment of patient outcomes. This time lapse may have introduced variability and could affect the generalizability of our findings. Secondly, we relied on secondary data for both the baseline and follow-up measurements, which presented certain challenges. The use of existing data may have led to missing information and limited our ability to obtain a comprehensive understanding of the patients' conditions. Furthermore, the presence of missing information in the recorded data was another limitation that impacted the generalizability of our findings. The incomplete data may have introduced biases and affected the accuracy of our analysis. Additionally, we acknowledge the lack of qualitative data even as we recognize the potential depth that this kind of data may bring in understanding the variables driving social reintegration in our research.
Conclusion
Our study findings indicate that the majority of road traffic orthopedic injury victims in Rwanda are able to reintegrate into society following the accident. However, certain domains such as mobility and community life are more adversely affected than others. We identified several factors that have a negative impact on social integration after road traffic injuries in Rwanda. These factors include older age, being female, lack of rehabilitation, and longer hospital stays. The study highlights the significance of early management, rehabilitation, and timely discharge from the hospital in facilitating the return to everyday life after the accident. These factors play a crucial role in improving social integration outcomes for individuals affected by road traffic orthopedic injuries.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
We obtained ethical approval to conduct the study from the University of Rwanda, College of Medicine and Health Sciences Institutional Review Board (18/CMHS IRB/2022). The Rwanda National Research Committee operating in the Ministry of Health approved this study (NHRC/2022/PROT/014), and we collaborated with the Rwanda Biomedical Center (5535/RBC/2022) injury department. We obtained local ethical approvals from the five hospitals' ethics committees; CHUK(EC/CHUK/051/2022), CHUB (REC/UTHB/089/2022), RH(313/RRH/DG/2022), KFH(EC/KFH/015/2022), RMH(RMH IRB/027/2022). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JAI: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing; AS: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing; CU: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing; DM: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing; JS: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing; GU: Conceptualization, Data curation, Formal Analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing; DT: Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Conceptualization, Data curation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
JAI was supported by the Consortium for Advanced Research Training in Africa (CARTA). CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Carnegie Corporation of New York (Grant No. G-19-57145), Sida (Grant No: 54100113), Uppsala Monitoring Center, Norwegian Agency for Development Cooperation (Norad), and by the Wellcome Trust (reference no. 107768/Z/15/Z) and the UK Foreign, Commonwealth & Development Office, supported by the Developing Excellence in Leadership, Training, and Science in Africa (DELTAS Africa) program. The statements made, and views expressed are solely the responsibility of the Fellow. JAI also was funded by the University of Rwanda through the SIDA open grant 2021–2023.
Acknowledgments
The authors acknowledge everyone who supported and contributed to this study, including the participants and research assistants from the five referral hospitals, especially Joel Nshumuyiki, the chief research assistant. Special thanks go to my Supervisors for the PhD project entitled” Health Outcomes of long term disabilities following Road Traffic Injuries in Rwanda”.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views and opinions expressed in the submitted article are the author's own and not the official position of the affiliated institutions.
References
1. Organização Mundial da Saúde. Global Status report on road. Geneva: World Health Organization (2018). p. 20.
2. Gathecha GK, Ngaruiya C, Mwai W, Kendagor A, Owondo S, Nyanjau L, et al. Prevalence and predictors of injuries in Kenya: findings from the national STEPs survey. BMC Public Health. (2018) 18(S3):1–9. doi: 10.1186/s12889-018-6061-x
3. Alemany R, Ayuso M, Guillén M. Impact of road traffic injuries on disability rates and long-term care costs in Spain. Accid Anal Prev. (2013) 60:95–102. doi: 10.1016/j.aap.2013.08.016
4. Afolabi OJ, Gbadamosi Kolawole T. Road traffic crashes in Nigeria: causes and consequences. Int J Shipp Transp Logist. (2017) 17(42):40–9.
5. Hyder A, Puvanachandra P, Allen K. Road Traffic Injury and Trauma Care: Innovations for Policy (Road Trip). WISH Road Traffic Injury Report. (2013).
6. Üzümcüoǧlu Y, Özkan T, Lajunen T, Morandi A, Orsi C, Papadakaki M, et al. Life quality and rehabilitation after a road traffic crash: a literature review. Transp Res Part F Traffic Psychol Behav. (2016) 40:1–13. doi: 10.1016/j.trf.2016.02.002
7. Gopinath B, Jagnoor J, Elbers N, Cameron ID. Overview of findings from a 2 - year study of claimants who had sustained a mild or moderate injury in a road traffic crash: prospective study. BMC Res Notes. (2017) 10:1–7. doi: 10.1186/s13104-017-2401-7
8. Alharbi R, Mosley I, Miller C, Hillel S, Lewis V. Transportation research interdisciplinary perspectives factors associated with physical, psychological and functional outcomes in adult trauma patients following Road Traffic Crash: a scoping literature review. Transp Res Interdiscip Perspect. (2019) 3:100061. doi: 10.1016/j.trip.2019.100061
9. Brakenridge CL, Gane EM, Smits EJ, Andrews NE, Johnston V. Impact of interventions on work-related outcomes for individuals with musculoskeletal injuries after road traffic crash: a systematic review protocol. Syst Rev. (2019) 8(1):1–7. doi: 10.1186/s13643-019-1178-2
10. Sabet FP, Tabrizi KN, Khankeh HR, Saadat S, Abedi HA, Bastami A. Road traffic accident victims’ experiences of return to normal life: a qualitative study. Iran Red Crescent Med J. (2016) 18(4):1–6. doi: 10.5812/ircmj.29548
11. Post MWM, De Witte LP, Reichrath E, Manon M, Wijlhuizen GJ, Perenboom RJM. Original report development and validation of impact-s, an ICF-based questionnaire to measure activities and participation. J Rehabil Med. (2008) 40:620–7. doi: 10.2340/16501977-0223
12. Perenboom ROMJM, Chorus AMJ. Measuring Participation According to the International Classification of Functioning, Disability and Health (ICF). (2003).
13. Ifver RRJ, Berg MHHY. Quality of life following road traffic injury: the impact of age and gender. Qual Life Res. (2020) 29:0123456789. doi: 10.1007/s11136-020-02427-3
14. Pélissier C, Fort E, Fontana L, Charbotel B, Hours M. Factors associated with non-return to work in the severely injured victims 3 years after a road accident: a prospective study. Accid Anal Prev. (2017) 106:411–9. doi: 10.1016/j.aap.2017.06.020
16. Kohler RE, Tomlinson J, Chilunjika TE, Young S, Hosseinipour M, Lee CN. “Life is at a standstill” quality of life after lower extremity trauma in Malawi. Qual Life Res. (2017) 26(4):1027–35. doi: 10.1007/s11136-016-1431-2
17. Resnik L, Borgia M, Silver B. Measuring community integration in persons with limb trauma and amputation: a systematic review. Arch Phys Med Rehabil. (2016) 98:1863–92.e14 (1-29). doi: 10.1016/j.apmr.2016.08.463
18. Grimm MM, Treibich CC. Socio-economic determinants of road traffic accident fatalities in low and middle income countries. ISS Work Pap Ser Gen Ser. (2010) 504(504):1–44.
19. Neagu M, Alexa O. Insights on the estimate of costs in road traffic accidents. Rev Med Chir Soc Med Nat. (2020) 121(3):624–30.
20. Nabeel S, Canner JK, Nagarajan N, Kushner AL. Road tra ffi c injuries: cross-sectional cluster randomized countrywide population data from 4 low-income countries. Int J Surg. (2018) 52:237–42. doi: 10.1016/j.ijsu.2018.02.034
21. Lin T, Li N, Du W, Song X, Zheng X. Road traffic disability in China: prevalence and socio-demographic disparities. J Public Health (Bangkok). (2013) 35(4):541–7. doi: 10.1093/pubmed/fdt003
22. Hoang CL, Vu HM, Pham HQ, Nguyen HLT, Vu LG, Tran BX, et al. Psychological distress of patients experiencing different types of road traffic injuries in Vietnam. Int J Environ Res Public Health. (2020) 17(10):1–9. doi: 10.3390/ijerph17103429
24. Allen Ingabire JC, Stewart A, Sagahutu JB, Urimubenshi G, Tumusiime DK, Georges B. Prevalence and levels of disability post road traffic orthopaedic injuries in Rwanda. Afr J Disabil. (2023) 12:a1251.
25. Wu J, Faux SG, Estell J, Wilson S, Harris I, Poulos CJ, et al. Early rehabilitation after hospital admission for road trauma using an in-reach multidisciplinary team: a randomised controlled trial. Clin Rehabil. (2017) 31(9):1189–200. doi: 10.1177/0269215517694462
26. Locke HN, Randriamarotsiresy V, Chamberlain MA, O’Connor RJ. Delays to accessing healthcare and rehabilitation following trauma in Madagascar–a qualitative study. Disabil Rehabil. (2020) 43:1–8. doi: 10.1080/09638288.2020.1741696
27. Fincham JE, Draugalis JR. The importance of survey research standards. Am J Pharm Educ. (2013) 77(1):7–10. doi: 10.5688/ajpe7714
28. Post MWM, de Witte LP, Reichrath E, Verdonschot MM, Wijlhuizen GJ, Perenboom RJM. Development and validation of impact-s, an ICF-based questionnaire to measure activities and participation. J Rehabil Med. (2008) 40(8):620–7. doi: 10.2340/16501977-0223
29. Sharma MP, Choudhary V. Validity of IMPACT-S for assessing activities and participation in patients with carpal tunnel syndrome. Int Multispeciality J Health (IMJH). (2022) 3:1–9. doi: 10.5281/zenodo.6397647
30. Aşkın A, Atar E, Tosun A, Demirdal Ü, Koca Ö. Activities and participation after stroke: validity and reliability of the Turkish version of IMPACT-S questionnaire. Disabil Rehabil. (2020) 42(13):1912–7. doi: 10.1080/09638288.2018.1542038
31. Javanmard A, Abdi K, Ebadi A, Hosseinzadeh S. Participation instruments in persons with spinal cord injury: a narrative review. Med J Islam Repub Iran. (2020) 34(1):1–9. doi: 10.34171/mjiri.34.66
32. Sabates-Wheeler R, Yates S, Wylde E, Gatsinzi J. Challenges of measuring graduation in Rwanda. IDS Bull. (2015) 46(2):103–14. doi: 10.1111/1759-5436.12133
33. Mousazadeh Y, Sadeghi-Bazargani H, Janati A, Poustchi H, Zakeri R, Shafiee-Kandjani A, et al. Functional consequences of road traffic injuries: preliminary results from PERSIAN traffic cohort (PTC). Trauma Mon. (2021) 26(6):294–304. doi: 10.30491/TM.2021.289262.1314
34. Access O. Pattern of road traffic injuries in Yemen: a hospital-based study. Pan Afr Med J. (2018) 8688:1–9.
35. Ingabire A, Petroze RT, Calland F, Okiria JC, Byiringiro JC. Profile and economic impact of motorcycle injuries treated at a university referral hospital in Kigali, Rwanda. Rwanda Med J. (2015) 72(4):5–11.
36. Lugo LH, García HI, Cano BC, Arango-Lasprilla JC, Alcaraz OL. Multicentric study of epidemiological and clinical characteristics of persons injured in motor vehicle accidents in Medellín, Colombia, 2009–2010. Colomb Med. (2013) 44(2):100–7. doi: 10.25100/cm.v44i2.1106
37. O’Hara NN, Mugarura R, Potter J, Stephens T, Rehavi MM, Francois P, et al. The socioeconomic implications of isolated tibial and femoral fractures from road traffic injuries in Uganda. J Bone Joint Surg Am. (2018) 100(7):e43. doi: 10.2106/JBJS.17.00439
38. Gopinath B, Jagnoor J, Harris IA, Nicholas M, Casey P, Blyth F, et al. Prognostic indicators of social outcomes in persons who sustained an injury in a road traffic crash. Injury. (2015) 46(5):909–17. doi: 10.1016/j.injury.2015.01.002
39. Marquez P. The challenge of non-communicable diseases and Road Traffic Injuries. World Bank Rep. (2013):1–108.
40. Gheshlaghi LA, Shari H. Quality of life after motorcycle traffic injuries: a cohort study in Northwest of Iran. Bull Emerg Trauma. (2020) 9:1–14. doi: 10.30476/BEAT.2021.87236.1182
41. Gane EM, Smits EJ, Brakenridge CL, Gangathimmaiah V, Jagnoor J, Cameron ID, et al. Functional and employment outcomes following road traffic crashes in Queensland, Australia: protocol for a prospective cohort study. J Transp Health. (2019) 15:100678. doi: 10.1016/j.jth.2019.100678
42. Herrera-escobar JP, Apoj M, Weed C, Harlow AF, Sanam S, Rafai A, et al. Association of pain after trauma with long-term functional and mental health outcomes. J Trauma Acute Care Surg. (2018) 85(4):773–9. doi: 10.1097/TA.0000000000002017
43. Davey S, Bulat E, Massawe H, Pallangyo A, Premkumar A, Sheth N. The economic burden of non-fatal musculoskeletal injuries in Northeastern Tanzania. Ann Glob Health. (2019) 85(1):1–9. doi: 10.5334/aogh.2411
45. Chauhan A, Ahmed N, Singh JV, Singh VK, Singh A, Kumar S. Disability and mortality following road traffic injury: a follow-up study from a tertiary care centre of India. Int J Community Med Public Health. (2017) 4(12):4712. doi: 10.18203/2394-6040.ijcmph20175356
46. Mahdian M, Fazel MR, Sehat M, Khosravi G, Mohammadzadeh M. Epidemiological profile of extremity fractures and dislocations in road traffic accidents in Kashan, Iran: a glance at the related disabilities. Arch Bone Jt Surg. (2017) 5(3):186–92.28656167
47. Odland ML, Abdul-Latif AM, Ignatowicz A, Alayande B, Appia Ofori B, Balanikas E, et al. Equitable access to quality trauma systems in low-income and middle-income countries: assessing gaps and developing priorities in Ghana, Rwanda and South Africa. BMJ Glob Health. (2022) 7(4):1–8. doi: 10.1136/bmjgh-2021-008256
48. Patel A, Id J, Id AT, Antipas T, Id P, Id JR, et al. PLOS GLOBAL PUBLIC HEALTH barriers to accessing follow up care in post- hospitalized trauma patients in Moshi, Tanzania: a mixed methods study. PLOS Glob Public Health. (2022) 2:1–18. doi: 10.1371/journal.pgph.0000277
49. Chatukuta M, Groce N, Mindell JS, Kett M. Access to rehabilitation services for road traffic injury patients in Namibia.pdf. Disabil Rehabil. (2022) 44(25):7985–92. doi: 10.1080/09638288.2021.2008521
50. Samuel JU. Utilization of community based rehabilitation for persons’ with disabilities (PWD) in Nigeria: the way forward. Eur Sci J. (2015) 11(25):1857–7881.
51. Godlwana L, Stewart A, Musenge E. The effect of a home exercise intervention on persons with lower limb amputations: a randomized controlled trial. Clin Rehabil. (2020) 34(1):99–110. doi: 10.1177/0269215519880295
52. Madsen LS, Handberg C, Jensen CM, Nielsen CV. Community-based rehabilitation approaches in outdoor settings: a systematic review of people with disabilities’ and professionals’ experiences and perceptions. Disabil Soc. (2021) 36(7):1073–98. doi: 10.1080/09687599.2020.1783206
53. Ahmed Nour FM, Tiee MS, Oke RA, Motwani GN, Azemafac KE, Mbeboh SN, et al. Limb injuries and disability in the Southwest Region of Cameroon. J Am Acad Orthop Surg Glob Res Rev. (2023) 7(2):1–10. doi: 10.5435/JAAOSGlobal-D-22-00148
54. Chi WC, Chang KH, Escorpizo R, Yen CF, Liao HF, Chang FH, et al. Measuring disability and its predicting factors in a large database in Taiwan using the world health organization disability assessment schedule 2.0. Int J Environ Res Public Health. (2014) 11(12):12148–61. doi: 10.3390/ijerph111212148
Keywords: social integration, road traffic orthopaedic injuries, activities and participation, IMPACT-S, rehabilitation
Citation: Allen Ingabire J, Stewart A, Uwakunda C, Mugisha D, Sagahutu JB, Urimubenshi G, Tumusiime DK and Bucyibaruta G (2024) Factors affecting social integration after road traffic orthopaedic injuries in Rwanda. Front. Rehabil. Sci. 4:1287980. doi: 10.3389/fresc.2023.1287980
Received: 3 September 2023; Accepted: 27 December 2023;
Published: 16 January 2024.
Edited by:
Hassan Izzeddin Sarsak, Batterjee Medical College, Saudi ArabiaReviewed by:
Masauso Chirwa, University of Zambia, ZambiaKhaled Al Hindi, Batterjee Medical College, Saudi Arabia
© 2024 Allen Ingabire, Stewart, Uwakunda, Mugisha, Sagahutu, Urimubenshi, Tumusiime and Bucyibaruta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: JC Allen Ingabire aWplYTIwMDBAZ21haWwuY29t
 JC Allen Ingabire
JC Allen Ingabire Aimee Stewart
Aimee Stewart Carine Uwakunda1
Carine Uwakunda1 Jean Baptiste Sagahutu
Jean Baptiste Sagahutu Gerard Urimubenshi
Gerard Urimubenshi David K. Tumusiime
David K. Tumusiime