
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Rehabil. Sci., 30 March 2023
Sec. Strengthening Rehabilitation in Health Systems
Volume 4 - 2023 | https://doi.org/10.3389/fresc.2023.1093086
Background: Professional health organizations recommend that outpatient cardiac rehabilitation programs include activities to optimize the physical, mental, and social well-being of patients. The study objectives were to describe among cardiac rehabilitation programs (1) mental health assessments performed; (2) psychosocial services offered; and (3) leadership's perception of barriers to psychosocial services offerings.
Methods: A cross-sectional survey of North Carolina licensed outpatient cardiac rehabilitation programs on their 2018 services was conducted. Descriptive statistics were used to summarize survey responses. Thematic analysis of free text questions related to barriers to programmatic establishment or expansion of psychosocial services was performed by two team members until consensus was reached.
Results: Sixty-eight programs (89%) responded to the survey. Forty-eight programs (70%) indicated offering psychosocial services; however, a majority (73%) of programs reported not directly billing for those services. At program enrollment, mental health was assessed in 94% of programs of which 92% repeated the assessment at discharge. Depression was assessed with the 9-item Patient Health Questionnaire by a majority (75%) of programs. Psychosocial services included individual counseling (59%), counseling referrals (49%), and educational classes (29%). Directors reported lack of internal resources (92%) and patient beliefs (45%) as the top barriers to including or expanding psychosocial services at their facilities.
Conclusions: Cardiac rehabilitation programs routinely assess mental health but lack the resources to establish or expand psychosocial services. Interventions aimed at improving patient education and reducing stigma of mental health are important public health opportunities.
An estimated 805,000 myocardial infarction (MI) events occur in the U.S. each year (1). Most (85%) individuals survive until MI discharge but these patients are at increased risk for future cardiovascular events and death (1). In addition, mental health problems are common in this population. Depression occurs in an estimated 20% of patients surviving an MI (2–4) and is a recognized risk factor for poor cardiovascular outcomes (5). Depressed MI patients were 22% and 13% more likely than non-depressed patients to experience subsequent all-cause mortality or cardiovascular events, respectively (6). Comorbid depression and anxiety are also common among MI survivors (3, 7) and these condition increase their risk of mortality (8).
Comprehensive cardiac rehabilitation (CR) is a class I recommendation from the American Heart Association (AHA) to improve cardiovascular recovery and reduce mortality after MI (9–11). Within AHA's guidance for CR core components is the recommendation to include psychosocial management to reduce the impact of mental health problems on patient health outcomes (12). This recommendation appears alongside patient education for other well-known risk factors of post-MI morbidity and mortality such as uncontrolled hypertension and smoking. Exercise training, a core component of CR, has also been shown to independently improve symptoms of depression and anxiety (13). In addition to exercise, stress management is an evidence-based activity known to improve outcomes in CR participants when compared to programs that do not offer this service (14). Despite the importance of psychosocial services in the prevention of adverse health outcomes following MI, the details of how psychosocial services, including stress management, have been implemented and the barriers affecting implementation in CR are not well described in the literature.
In summarizing current CR practices, Hughes et al. identified the need for descriptive studies of behavioral health as a research priority (15). This current study addresses the need to describe the real-world implementation of psychosocial guidelines in CR programs and elucidates barriers to offering these programs despite AHA recommendation. For this study, we aimed to describe psychosocial and stress management services at outpatient CR facilities in the state of North Carolina (NC) and describe leadership's perspective on barriers to the use of these program offerings. To meet these objectives, we described CR program enrollment assessments, psychosocial and stress management service activities, and service personnel providing psychosocial and stress management services. Additionally, we gather qualitative data on leadership perceptions of barriers to CR psychosocial service and stress management initiation or expansion. Stratified summaries are presented since any potential future interventions might differ by level of current service offered. Comprehensive cardiac rehabilitation (CR) programs have the opportunity to identify patients at risk for mental health problems following an MI and to connect those patients with appropriate services. Our goal in describing assessments and services in NC CR is to call attention to the value of CR programs to provide this function and lay a foundation for future research and quality improvement for CR programs.
We conducted a cross-sectional survey of CR programs for the entire state of NC. Programs were identified from the NC Department of Health and Human Services Division of Health Service Regulation online directory of licensed facilities (accessed online Sep 2018). A unique link to the study questionnaire was sent via email to the program directors of 76 licensed CR facilities in NC to assess program offerings and obstacles to patient participation and program expansion. Directors were asked to provide details based upon what their program offered in calendar year 2018. Interviewees were offered a $25 incentive to complete the survey. We attempted to verify the email address of program directors before survey distribution; however, some messages were not delivered. Follow-up calls were made to CR facilities with rejected email addresses to obtain a valid email address. To promote survey completion, similar calls were made to programs which did not respond within two months of the initial survey distribution. We also encouraged program directors to designate a proxy to complete the survey if they were unavailable. The institutional Office of Human Research Ethics determined that this survey of program directors did not constitute human subjects research therefore did not require IRB approval.
The current study's survey expanded upon questions asked of NC CR programs in 1999 (16, 17) and 2004 (18). The original survey was designed to obtain descriptive information on CR facilities, personnel, services offered, and the patient population that is served by each program. An electronic version of the original paper survey was updated, pilot tested, revised, and distributed via email. New questions were developed to gain further details about psychosocial services currently provided and future intentions. Psychosocial and stress management services were ascertained separately; therefore, leadership could indicate whether they provide both, one, or neither of these services. New open-ended questions were asked to ascertain the types of program activities for psychosocial and stress management services separately (“Please provide a brief description of the program's psychosocial services.” and “Please provide a brief description of the program's stress management services.”). A single open-ended question was used to assess participants' beliefs regarding barriers to establishing or expanding program services (“In your opinion, what are the top 3 barriers to including or expanding psychosocial and/or stress management services within outpatient cardiac rehabilitation programs?”). New health questions assessed what instruments were used to collect health information (“Was the general health status of patients’ assessed with any of the following standardized instruments during 2018?”; “Was the mental health status of patients’ assessed with any of the following standardized instruments during 2018?”; “Was the social support of patients’ assessed with any of the following standardized instruments during 2018?”). Respondents could select multiple instruments if more than one was used during the calendar year. We also asked if instruments were administered at program enrollment, program conclusion and/or at periodic visit during cardiac rehabilitation. The final survey instrument contained sixty questions. Survey responses collected in a web-based survey tool, Qualtrics (Provo, UT), between February and June 2019 were exported and analyzed using SAS software version 9.4 (Cary, NC). The questionnaire was completed in 1 (SD:1.1) hour by 62% of respondents. The remaining respondents started and completed the survey on different days.
Two team members separately reviewed open-ended responses to the question regarding barriers to establishing or expanding program services. Initial code construction was completed using a consensus approach; team members proposed potential codes based on participant response patterns. This resulted in sixteen child codes. Team members then worked simultaneously to apply codes to each response, discussing and rectifying any disagreements. After the initial round of coding was complete, team members repeated this approach with the goal of synthesizing data into categories. This resulted in five themes relevant to program barriers. The approach of developing open-ended codes and further synthesizing codes into coherent categories for the purpose of elucidating themes was derived from Saldana's 2009 manual on qualitative coding (19).
For Tables 1 and 2, descriptive statistics were used to summarize survey responses for programs overall and by if psychosocial services were provided in that program. Standardized differences (20, 21) were computed to detect an imbalance in these non-randomized groups for quantitative survey questions. By convention, a 10% standardized difference between groups was considered meaningful (20). For Table 3, descriptive statistics were used to summarize survey responses by type of service. Psychosocial and stress management services could be provided independent of each other so are summarized separately. Descriptive statistics were used to summarize program barriers in Table 4 overall and by program psychosocial service providers excluding standardized differences since this was a summary of open-ended questions. The lead author had full access to all the data in the study and takes responsibility for its integrity and the data analysis. Anonymized data from this study are available from the corresponding author upon reasonable request.
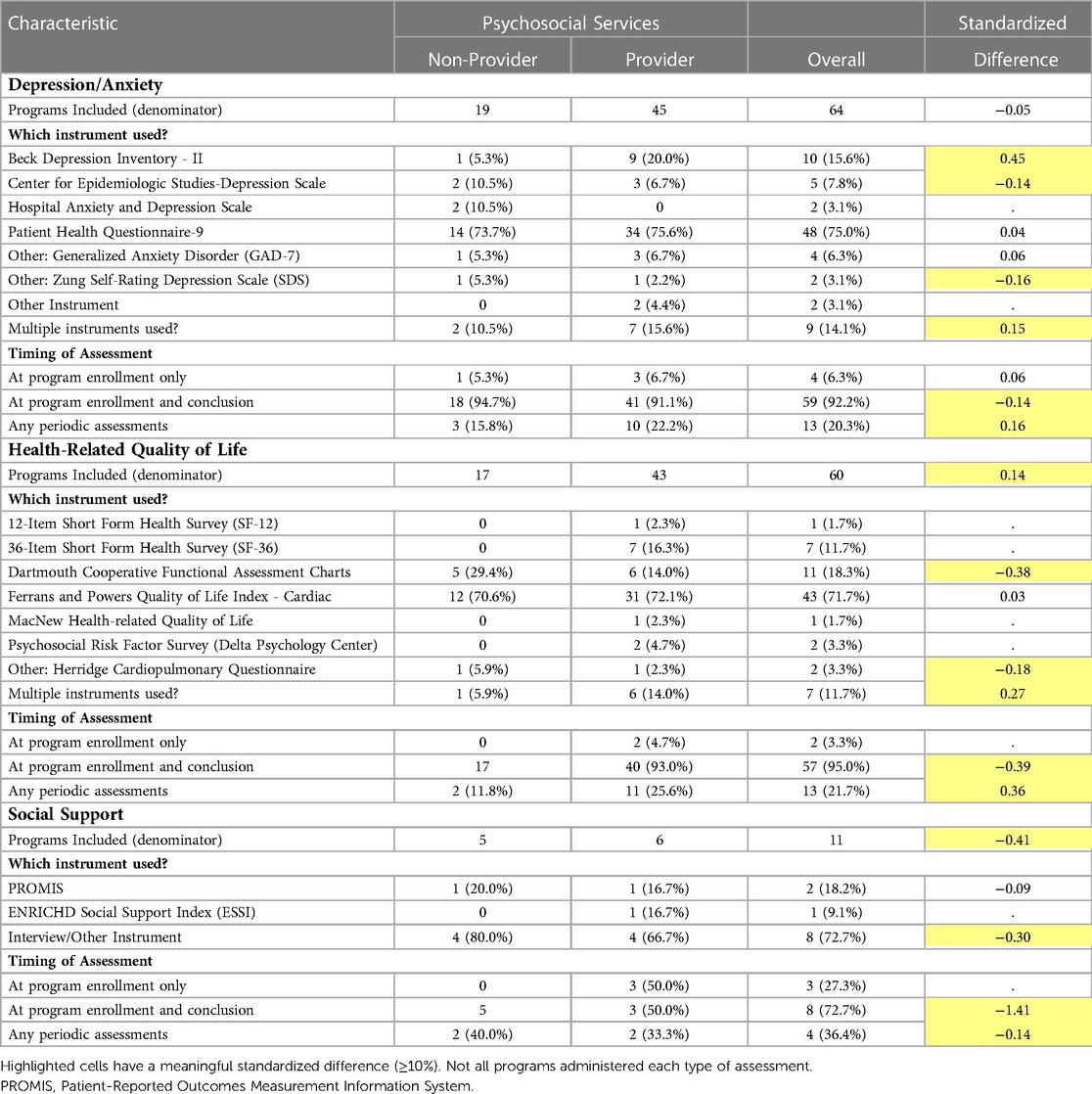
Table 2. Summary of psychosocial assessments performed at outpatient cardiac rehabilitation programs .
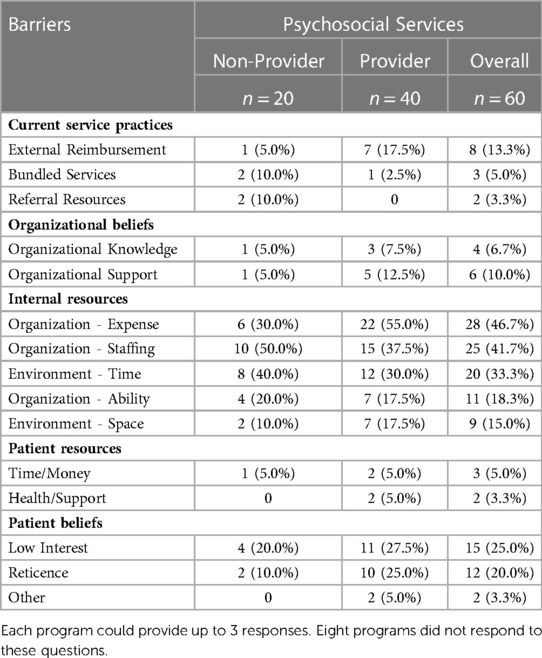
Table 4. Perceived barriers to including or expanding psychosocial or stress management services in outpatient cardiac rehabilitation program.
Sixty-eight programs (89%) across North Carolina participated in this cross-sectional survey. A majority of programs (69%) offered maintenance (i.e., phase III) CR but very few offered an intensive CR program (3%) or a home-based CR program (1%) (Table 1). Most programs (70%) reported offering psychosocial services and almost all (94%) programs reported offering stress management services (Table 1). Programs which offered psychosocial services had on average slightly higher patient populations during the year 2018 (Mean: 270, SD: 201) than programs not offering these services (Mean: 231, SD: 180). The qualifying event for 75% of patients attending CR sessions at responding programs was either MI, coronary artery bypass grafting, angioplasty/stent placement. There were only minor differences in demographic characteristics and qualifying events between programs that did and did not offer psychosocial services. Overall, the typical (median proportion ≥60%) characteristics of program participants included White race, male sex, at least 65 years old, English speaking, and Medicare insured.
In line with AHA and American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) (12) guidelines, psychosocial assessments were completed at CR program enrollment and at additional times depending upon the type of assessment. Depression/anxiety specific instruments were used in 64 (94%) programs and health-related quality of life (QoL) instruments were used in 60 (88%) programs (Table 2). QoL instruments assessed psychological symptoms as well as other factors related to quality of life such as physical functioning. Eighty-two percent of CR programs used both depression/anxiety and QoL instruments in 2018. Social support was infrequently (16%) assessed independently of QoL. There was no consensus method of assessing social support from study participants.
The nine-item Patient Health Questionnaire (PHQ-9) (22), the most common depression assessment instrument, was used by 75% of programs (Table 2). The Beck Depression Inventory (23) was also used by 20% of programs providing psychosocial services. Approximately 13% of programs reported using more than one depression/anxiety assessment instrument during the study period. The seven-item Generalized Anxiety Disorder (24) assessment and PHQ-9 were administered by 4 programs. Other programs administered the PHQ-9 and either the Center for Epidemiologic Studies-Depression Scale (25) (n = 2) or Beck Depression Inventory (n = 2). All programs that performed a depression/anxiety assessment did so at program enrollment. Over 90% of these programs also assessed depression/anxiety at program conclusion. Between enrollment and program conclusion, 20% of programs periodically reassessed depression/anxiety.
The Ferrans and Powers Quality of Life Index—Cardiac questionnaire (26) was the most frequently administered (72%) health-related QoL assessment (Table 2). The Dartmouth Cooperative Function Assessment (27, 28), the second most popular of these types of assessments, was administered by a greater proportion of programs not providing psychosocial services than programs providing these services. Short Form Health Surveys (29, 30) (both 36- and 12-item) were used by psychosocial service providing programs but not by non-providing programs. Health-related QoL was assessed at program enrollment and conclusion by 95% of programs that completed this type of assessment. A larger proportion of psychosocial service providing programs than non-providing programs completed additional periodic QoL assessments between enrollment and program conclusion.
Programs that indicated providing psychosocial services and stress management services were also asked to provide details of activities associated with these services (Table 3). A majority (64%) indicated providing educational stress management classes. Several programs also provided individual counseling (22%) and/or skills/technique practice (19%) as stress management activities. A smaller proportion (14%) provided a referral for other stress management services. On average, program leadership reported that 65% of CR participants attended at least one stress management session when offered. Nurses were the most common healthcare provider utilized to deliver stress management services, 44% of programs. Stress management services were also provided by either an exercise physiologist, psychiatrist, and/or psychologist in 19% of programs. Almost half (48%) of programs provided stress management 1 day a week and few (12%) offered these services 4–5 days a week. While these services were typically provided before 5pm, two programs provided these services after 5 pm.
Individual counseling (59%) and referral to counseling (49%) were the top psychosocial services provided by responding programs. Psychosocial educational classes were also provided by 29% of programs. On average, psychosocial services were utilized by 52% of CR participants. The top 3 professions providing psychosocial services were physiologists/psychiatrists (35%), nurses (31%), and social workers (23%). Similar to stress management services, psychosocial services were offered once a week by 50% of programs; however, more programs (18%) offered psychosocial services 4–5 days a week. Only 1 program reported providing psychosocial services after 5 pm.
Sixty programs (88%) responded with their top three barriers to expansion of psychosocial or stress management services provided in outpatient CR programs (Table 4). Free-text responses were grouped into 5 main categories (Current service practices, Organizational beliefs, Internal resources, Patient resources, and Patient beliefs) with multiple subcategories. The top 3 barriers identified by program directors were lack of internal resources related to organizational expense (47%), organizational staffing (42%), and environmental time (33%). These categories were derived from survey responses like “budget constraints/costs”, “staffing resources/availability of resources” and “time constraints/schedule” respectively. Patient beliefs were identified by 45% of programs as a barrier. Specifically, both low patient interest and patient reticence were reported by at least 20% of respondents. Survey responses used to derive these categories included “patient interest/patient participation” and “patient unwilling/fear.”
Since mental health assessment is one of the recommended core components of CR, CR programs provide an opportunity to identify participants with psychosocial risk factors for poor cardiovascular outcomes. CR programs not only have the capacity to identify participants who are at high risk of psychological distress at clinical diagnosis thresholds but also those patients with no/low psychological symptom burden initially who may progress to clinical diagnoses. Since psychological symptom burden changes over time, CR programs afford the exceptional opportunity to monitor symptom persistence within the early recovery period after an acute event.
All programs in this study assessed for psychological symptom burden at program enrollment using depression screening instruments or as a component of a health-related quality of life assessment. NC CR programs also have excellent surveillance of changes in patients' symptom burden with approximately 95% of programs administering these assessments more than once. The high assessment rate at program entry and exit is consistent with what has been reported in other high-income countries (31, 32) and represents a marked increase in assessment rates of 29% to 68% observed across the globe between 1995 and 2010 (33, 34). Similar to Australian practice (32), validated instruments were used to assess depression and/or anxiety in NC CR programs but it was unlikely that validated instruments were used to assess social support. Social support was also less likely to be assessed in NC CR programs than Australian CR programs (16% vs. 80%) (32).
The type of healthcare system will influence the type of subsequent psychosocial health services. Results from this study and Canada indicate that 50%-60% of programs offer psychological counseling (31) while psychosocial follow-up across a survey of European countries was over 60% (34). However, not all respondents to our survey indicated offering psychosocial services and those that did also indicated referral to another entity for counseling. Cahill et al. summarized the effects of depression screening on depression outcomes (33), however, outcomes were not the focus of this research project since we did not assess patients directly. Future research could investigate the influence of models of mental health service on physical and mental health outcomes including adherence to CR participation and of other lifestyle changes.
Psychosocial services are an essential component of CR programs; however, this study identified barriers to implementing these services in practice. Insurance coverage constraints fuel financial barriers to psychosocial services within CR programs. For example, Medicare coverage focuses on medically supervised exercise training with ECG monitoring, as necessary, for 2 to 3 sessions per week up to 12 to 18 weeks without the need for special permission (35). Medicare policy updates have required the inclusion of education and counseling without increasing the number of covered sessions resulting in the majority of NC CR programs providing such services without insurance reimbursement (Table 3). Financial barriers to CR implementation were not just a problem in this study population but were prevalent in other countries (32, 36, 37).
Outside of changes to the payment structure for CR programs, additional effort is necessary to remove the perceived stigma of addressing mental health among patients. To reap the benefit of psychosocial services, patients need a greater awareness of the connection between mental and physical health and of the benefits of addressing both aspects of their health following a cardiac event. Patients do not feel that they need CR in general or psychosocial services in particular (38, 39). Given the low numbers of eligible patients attending CR, overall patient participation in CR programs needs to be increased to maximize benefits of psychosocial services in cardiovascular disease patients (40–42).
Comprehensive cardiac rehabilitation recommendations (12) address multiple evidence-based risk factors for poor health outcomes after an acute coronary event. Although mental health status is an established risk factor for poor physical health outcomes in heart disease patients, there is still controversy on if mental health assessments should occur in these patients (43, 44). Resistance to implementing psychological screening in outpatient practice exists despite recommendation for outpatient depression screening for the general public and patients with cardiovascular disease specifically (45). Treatment initiation requires evaluation. CR programs are one avenue where evaluation can routinely occur.
This study described the psychosocial aspects from a broader survey designed to summarize services offered by CR programs in North Carolina (46). The strength of this study is that it is one of the first statewide descriptions of CR program services and referral processes (33). Considering the limited research in this area, this study provides a guide for other states to identify state and local level practices for advancement and quality improvement of CR programs as well as resource needs to improve mental and physical collaborative care for patients after a cardiac event. The potential for information bias is a limitation of this study. However, programs that participate in the AACVPR registry, other quality improvement programs, or have organizational requirements for data such as those collected in this study will have access to more accurate information than programs that do not participate in those activities. In addition, most questions were straightforward and familiar to those respondents who participated in the two previous surveys of NC CR programs.
Despite its limitations, this statewide study is important because by highlighting that the mental health of CR patients will be routinely assessed it illustrates how CR can play a role in optimal health care of patients. Statewide, CR programs were compliant with psychosocial assessment and regardless of restricted funding, a majority of CR programs provide at least basic psychosocial services. Psychosocial services and education are a critical component of post-acute care that needs additional support for improvement in the comprehensive care of patients recovering from cardiac events. Future research could include investigate implementation of different payment models to overcome financial barriers to program enhancement. Literature suggests there are numerous barriers to integrating psychosocial services into primary care type settings (47, 48); therefore, implementation research into facilitators for psychosocial follow-up among the sizeable number of programs not currently providing psychosocial services is also needed. In addition, more research is needed on the assessment and mental health status of CR eligible patients that do not attend at least one CR session since only 30% to 50% of eligible patients attend at least one session of CR (40, 42).
Data generated for this study are available upon reasonable request to the corresponding author in a de-identified format after the requestor completes our data use agreement.
MB contributed to the study design and the acquisition, analysis, and interpretation of study data. MB drafted and gave final approval of the manuscript. KE, AKN contributed to the study design and the acquisition and interpretation of study data. KE, AKN critically revised the manuscript and gave final approval of the manuscript. AA contributed to the acquisition and interpretation of study data. AA critically revised the manuscript and gave final approval of the manuscript. JC contributed to the analysis and interpretation of study data. JC critically revised the manuscript and gave final approval of the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the University of North Carolina at Chapel Hill School of Medicine.
We thank the North Carolina Cardiac Rehabilitation Program Directors for their participation in the survey.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics-2021 update: a report from the American heart association. Circulation. (2021) 143(8):e254–743. doi: 10.1161/CIR.0000000000000950
2. Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, et al. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. (2006) 21(1):30–8. doi: 10.1111/j.1525-1497.2005.00269.x
3. Pogosova N, Kotseva K, De Bacquer D, von Kanel R, De Smedt D, Bruthans J, et al. Psychosocial risk factors in relation to other cardiovascular risk factors in coronary heart disease: results from the EUROASPIRE IV survey. A registry from the European society of cardiology. Eur J Prev Cardiol. (2017) 24(13):1371–80. doi: 10.1177/2047487317711334
4. Smolderen KG, Buchanan DM, Gosch K, Whooley M, Chan PS, Vaccarino V, et al. Depression treatment and 1-year mortality after acute myocardial infarction: insights from the TRIUMPH registry (translational research investigating underlying disparities in acute myocardial infarction patients’ health status). Circulation. (2017) 135(18):1681–9. doi: 10.1161/CIRCULATIONAHA.116.025140
5. Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American heart association. Circulation. (2014) 129(12):1350–69. doi: 10.1161/CIR.0000000000000019
6. Meijer A, Conradi HJ, Bos EH, Anselmino M, Carney RM, Denollet J, et al. Adjusted prognostic association of depression following myocardial infarction with mortality and cardiovascular events: individual patient data meta-analysis. Br J Psychiatry. (2013) 203(2):90–102. doi: 10.1192/bjp.bp.112.111195
7. Tully PJ, Cosh SM, Baumeister H. The anxious heart in whose mind? A systematic review and meta-regression of factors associated with anxiety disorder diagnosis, treatment and morbidity risk in coronary heart disease. J Psychosom Res. (2014) 77(6):439–48. doi: 10.1016/j.jpsychores.2014.10.001
8. Doering LV, Moser DK, Riegel B, McKinley S, Davidson P, Baker H, et al. Persistent comorbid symptoms of depression and anxiety predict mortality in heart disease. Int J Cardiol. (2010) 145(2):188–92. doi: 10.1016/j.ijcard.2009.05.025
9. Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American heart association and American college of cardiology foundation. Circulation. (2011) 124(22):2458–73. doi: 10.1161/CIR.0b013e318235eb4d
10. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr., Ganiats TG, Holmes DR Jr., et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. (2014) 130(25):2354–94. doi: 10.1161/CIR.0000000000000133
11. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr., Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation. (2013) 127(4):e362–425. doi: 10.1161/CIR.0b013e3182742cf6
12. Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update A scientific statement from the American heart association exercise, cardiac rehabilitation, and prevention committee, the council on clinical cardiology; the councils on cardiovascular nursing, epidemiology and prevention, and nutrition, physical activity, and metabolism; and the American association of cardiovascular and pulmonary rehabilitation. Circulation. (2007) 115:2675–82. doi: 10.1161/CIRCULATIONAHA.106.180945
13. Zheng X, Zheng Y, Ma J, Zhang M, Zhang Y, Liu X, et al. Effect of exercise-based cardiac rehabilitation on anxiety and depression in patients with myocardial infarction: a systematic review and meta-analysis. Heart Lung. (2019) 48(1):1–7. doi: 10.1016/j.hrtlng.2018.09.011
14. Blumenthal JA, Sherwood A, Smith PJ, Watkins L, Mabe S, Kraus WE, et al. Enhancing cardiac rehabilitation with stress management training: a randomized, clinical efficacy trial. Circulation. (2016) 133(14):1341–50. doi: 10.1161/CIRCULATIONAHA.115.018926
15. Hughes JW, Serber ER, Kuhn T. Psychosocial management in cardiac rehabilitation: current practices, recommendations, and opportunities. Prog Cardiovasc Dis. (2022) 73:76–83. doi: 10.1016/j.pcad.2021.12.006
16. Evenson KR, Fleury J. Barriers to outpatient cardiac rehabilitation participation and adherence. J Cardiopulm Rehabil. (2000) 20(4):241–6. doi: 10.1097/00008483-200007000-00005
17. Evenson KR, Rosamond WD. Outpatient cardiac rehabilitation in North Carolina. N C Med J. (2000) 61(2):75–9. PMID: 10737027
18. Evenson KR, Johnson A, Aytur SA. Five-year changes in North Carolina outpatient cardiac rehabilitation. J Cardiopulm Rehabil. (2006) 26(6):366–76. doi: 10.1097/00008483-200611000-00006
19. Saldaña J. The coding manual for qualitative researchers. Thousand Oaks, CA: Sage Publications Ltd (2009). xi, 223-xi.
20. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. (2009) 28(25):3083–107. doi: 10.1002/sim.3697
21. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, N.J: L. Erlbaum Associates (1988). xxi, 567.
22. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. (1999) 282(18):1737–44. doi: 10.1001/jama.282.18.1737
23. Beck AT, Steer RA, Brown GK. Manual for the beck depression inventory - II. San antonio, TX: Psychological Corporation (1996).
24. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166(10):1092–7. doi: 10.1001/archinte.166.10.1092
25. Radloff LS. The CES-D scale:a self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1(3):385–401. doi: 10.1177/014662167700100306
26. Ferrans CE, Powers MJ. Quality of life index: development and psychometric properties. ANS Adv Nurs Sci. (1985) 8(1):15–24. doi: 10.1097/00012272-198510000-00005
27. Nelson E, Wasson J, Kirk J, Keller A, Clark D, Dietrich A, et al. Assessment of function in routine clinical practice: description of the COOP chart method and preliminary findings. J Chronic Dis. (1987) 40(Suppl 1):55S–69S. doi: 10.1016/S0021-9681(87)80033-4
28. Nelson EC, Landgraf JM, Hays RD, Wasson JH, Kirk JW. The functional status of patients. How can it be measured in physicians’ offices? Med Care. (1990) 28(12):1111–26. doi: 10.1097/00005650-199012000-00001
29. McHorney CA, Ware JE Jr., Raczek AE. The MOS 36-item short-form health survey (SF-36): iI. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. (1993) 31(3):247–63. doi: 10.1097/00005650-199303000-00006
30. Ware J J, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. (1996) 34(3):220–33. doi: 10.1097/00005650-199603000-00003
31. Turk-Adawi KI, Terzic C, Bjarnason-Wehrens B, Grace SL. Cardiac rehabilitation in Canada and arab countries: comparing availability and program characteristics. BMC Health Serv Res. (2015) 15:521. doi: 10.1186/s12913-015-1183-7
32. Jackson AC, Le Grande MR, Higgins RO, Rogerson M, Murphy BM. Psychosocial screening and assessment practice within cardiac rehabilitation: a survey of cardiac rehabilitation coordinators in Australia. Heart Lung Circ. (2017) 26(1):64–72. doi: 10.1016/j.hlc.2016.04.018
33. Cahill MC, Bilanovic A, Kelly S, Bacon S, Grace SL. Screening for depression in cardiac rehabilitation: a REVIEW. J Cardiopulm Rehabil Prev. (2015) 35(4):225–30. doi: 10.1097/HCR.0000000000000101
34. Vanhees L, McGee HM, Dugmore LD, Schepers D, van Daele P. Carinex working group CRIE. A representative study of cardiac rehabilitation activities in European union member states: the carinex survey. J Cardiopulm Rehabil. (2002) 22(4):264–72. doi: 10.1097/00008483-200207000-00009
35. Ho PM, Spertus JA, Masoudi FA, Reid KJ, Peterson ED, Magid DJ, et al. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med. (2006) 166(17):1842–7. doi: 10.1001/archinte.166.17.1842
36. Bjarnason-Wehrens B, McGee H, Zwisler AD, Piepoli MF, Benzer W, Schmid JP, et al. Cardiac rehabilitation in Europe: results from the European cardiac rehabilitation inventory survey. Eur J Cardiovasc Prev Rehabil. (2010) 17(4):410–8. doi: 10.1097/HJR.0b013e328334f42d
37. Korenfeld Y, Mendoza-Bastidas C, Saavedra L, Montero-Gomez A, Perez-Terzic C, Thomas RJ, et al. Current status of cardiac rehabilitation in Latin America and the Caribbean. Am Heart J. (2009) 158(3):480–7. doi: 10.1016/j.ahj.2009.06.020
38. Herber OR, Smith K, White M, Jones MC. ‘Just not for me’—contributing factors to nonattendance/noncompletion at phase III cardiac rehabilitation in acute coronary syndrome patients: a qualitative enquiry. J Clin Nurs. (2017) 26(21-22):3529–42. doi: 10.1111/jocn.13722
39. Neubeck L, Freedman SB, Clark AM, Briffa T, Bauman A, Redfern J. Participating in cardiac rehabilitation: a systematic review and meta-synthesis of qualitative data. Eur J Prev Cardiol. (2012) 19(3):494–503. doi: 10.1177/1741826711409326
40. Dunlay SM, Pack QR, Thomas RJ, Killian JM, Roger VL. Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am J Med. (2014) 127(6):538–46. doi: 10.1016/j.amjmed.2014.02.008
41. Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. (2007) 116(15):1653–62. doi: 10.1161/CIRCULATIONAHA.107.701466
42. Bush M, Simpson RJ Jr., Kucharska-Newton A, Fang G, Sturmer T, Brookhart MA. Approaches to address premature death of patients when assessing patterns of use of health care services after an Index event. Med Care. (2018) 56(7):619–25. doi: 10.1097/MLR.0000000000000923
43. Elderon L, Smolderen KG, Na B, Whooley MA. Accuracy and prognostic value of American heart association: recommended depression screening in patients with coronary heart disease: data from the heart and soul study. Circ Cardiovasc Qual Outcomes. (2011) 4(5):533–40. doi: 10.1161/CIRCOUTCOMES.110.960302
44. Thombs BD, Roseman M, Coyne JC, de Jonge P, Delisle VC, Arthurs E, et al. Does evidence support the American heart association's recommendation to screen patients for depression in cardiovascular care? An updated systematic review. PLoS One. (2013) 8(1):e52654. doi: 10.1371/journal.pone.0052654
45. Lichtman JH, Bigger JT Jr., Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American heart association prevention committee of the council on cardiovascular nursing, council on clinical cardiology, council on epidemiology and prevention, and interdisciplinary council on quality of care and outcomes research: endorsed by the American psychiatric association. Circulation. (2008) 118(17):1768–75. doi: 10.1161/CIRCULATIONAHA.108.190769
46. Aylward A, Evenson KR, Kucharska-Newton A, Bush M. Outpatient cardiac rehabilitation services, participants and workforce in North Carolina: results of a 2019 survey of cardiac rehabilitation program directors. N C Med J. (2022) 83(2):134–41. doi: 10.18043/ncm.83.2.134
47. Grazier KL, Smiley ML, Bondalapati KS. Overcoming barriers to integrating behavioral health and primary care services. J Prim Care Community Health. (2016) 7(4):242–8. doi: 10.1177/2150131916656455
Keywords: mental health assessments, barriers and facilitative factors, post-myocardial infarction care, patient beliefs and attitudes, cardiac rehabilitation
Citation: Bush M, Evenson KR, Aylward A, Cyr JM and Kucharska-Newton A (2023) Psychosocial services provided by licensed cardiac rehabilitation programs. Front. Rehabil. Sci. 4:1093086. doi: 10.3389/fresc.2023.1093086
Received: 8 November 2022; Accepted: 3 March 2023;
Published: 30 March 2023.
Edited by:
Błażej Cieślik, Jan Długosz University, PolandReviewed by:
Barbara Murphy, Australian Centre for Heart Health, Australia© 2023 Bush, Evenson, Aylward, Cyr and Kucharska-Newton. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Montika Bush bWJ1c2g4QHVuYy5lZHU=
Specialty Section: This article was submitted to Strengthening Rehabilitation in Health Systems, a section of the journal Frontiers in Rehabilitation Sciences
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.