
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Rehabil. Sci., 06 July 2023
Sec. Disability, Rehabilitation, and Inclusion
Volume 4 - 2023 | https://doi.org/10.3389/fresc.2023.1075775
This article is part of the Research TopicEquity, Diversity, and Inclusion in Rehabilitation SciencesView all 10 articles
Objectives: Given the prevalence of discrimination experienced by racial and ethnic minorities living with disabilities, it is likely that racism experienced by Black, Indigenous, and people of color (BIPOC) is compounded by the ableism experienced by people with disabilities, widening disparities in health and healthcare outcomes. To address this, we described unmet healthcare needs of a sample of Black, non-Hispanic, and Hispanic adults with and without disabilities. The following research question was examined exploratively: Are Black and Hispanic adults with disabilities at increased risk of unmet healthcare needs compared to Black and Hispanic adults without disabilities according to the 2018 National Health Interview Survey?
Methods: Survey data was examined from the 2018 National Health Interview Survey (NHIS), a nationally representative survey of community-dwelling adults in the United States.
Results: Black and non-Hispanic adults most commonly reported mobility only disabilities. People with disabilities were significantly more likely to delay or forego care than their peers without disabilities within each racial/ethnic group. Among non-Hispanic Black and Hispanic adults, nearly 30% of people with disabilities forewent services due to cost compared to persons without disabilities.
Conclusions: Black and Hispanic adults with disabilities experience greater disparities in access to healthcare than Black and Hispanic adults without disabilities. Therefore, health disparities experienced by racial and ethnic minorities living with disabilities is likely influenced by the dual systemic factors of racism and ableism.
Recent estimates indicate that 26% of US adults experience disability (1), with higher rates of disabilities in Black, Indigenous, and people of color (BIPOC) communities. For example, compared to 26.6% of white persons with disabilities (PwD) ages 45–64, 35.5% of Black and Hispanic adults in that same age group are living with a disability in the US (2). Moreover, research shows that both BIPOC and disability communities experience disparities in the receipt of equitable care (3–5). For example, each report unmet needs for healthcare at disproportionately higher levels than their white, non-Hispanic and non-disabled counterparts, respectively (2, 6, 7). Both groups face insurance, cost, and provider-patient communication barriers to high-quality care and problems receiving culturally appropriate care.
Despite the overlap in both prevalence and similar inequities experienced by both groups, little research has examined the health and health care outcomes at the intersection of BIPOC and PwD. Given the prevalence of discrimination, it is likely that racism experienced by BIPOC is compounded by the ableism experienced by PwD, potentially amplifying disparities in health and healthcare outcomes (8–10). Studies have demonstrated in specific disability populations, namely individuals with intellectual and developmental disabilities, who belong to racial and ethnic marginalized communities have worse health and health care outcomes as compared to white individuals with intellectual and developmental disabilities (11–15). Additionally, several studies demonstrate disparities in health care utilization for women who live at the intersection of disability and race/ethnicity (16, 17). However, a dearth of evidence on the health care outcomes of the population of persons with disabilities who belong to ethnic and racial minority communities exists. To address this, we described unmet healthcare needs of a sample of Black and Hispanic adults with and without disabilities. The following research question was examined exploratively: Are Black and Hispanic adults with disabilities at increased risk of unmet healthcare needs compared to Black and Hispanic adults without disabilities according to the 2018 National Health Interview Survey?
We examined data from the 2018 National Health Interview Survey (NHIS), a nationally representative survey of community-dwelling adults in the US (18). The NHIS is a longstanding in-person federal survey of health and healthcare; it is publicly available from the National Center for Health Statistics and is, therefore, exempt from review. All persons in 30,000 households were interviewed; a single adult was randomly selected for more extensive questions on the Sample Adult file (n = 25,417). The response rate on this file was 83.9% (18).
We focus our analysis on Black, non-Hispanic adults and Hispanic adults with and without disabilities, due to the small racial/ethnic sample sizes for other BIPOC. Our retrospective cohort study includes 2 analytic samples (≥18 years old): Black, non-Hispanic adults (n = 2,822) and Hispanic adults of any race (n = 3,069).
Respondents were categorized as having a disability if they reported a lot of difficulty in any of the following areas: seeing with glasses; hearing with a hearing aid; walking or climbing steps; communicating in their “usual language”; “remembering or concentrating”; or self-care activities. Combining disability types into a single catch-all category is not ideal, because of how types of disability interact differently with the environment (19). However, the NHIS first asked these questions of all sample adults in 2018 and the sample sizes of each disability type were too small to be examined reliably. When possible, we describe some preliminary differences by disability type.
Outcome measures included self-reported usual source of care (USC) for sick and routine care. Respondents reported 4 separate measures of unmet need: (1 and 2) delayed/forewent care due to cost, (3) delayed care due to availability (e.g., could not get through on the phone, wait was too long), and (4) forewent services (e.g., prescription medication, mental healthcare) due to cost.
Pearson's χ2 and multivariate logistic regression were used to examine outcomes by disability within each race/ethnicity group, controlling for age, sex, marital status, employment, education, imputed poverty status, health insurance, and number of chronic conditions. We report predicted proportions and odds ratios (95% confidence intervals) from regression. Analyses were conducted in Stata 15, accounting for NHIS weights and complex sampling design. We used p < 0.017 to account for the examination of multiple outcomes within each racial/ethnic group (20).
Sociodemographic characteristics of our sample are contained in Table 1. Fifty percent of adults were ages 35–64 and female; most had private health insurance, graduated high school or earned a GED, and were employed. Approximately 20% of adults reported living in poverty. Most had no chronic conditions.
Approximately 11.5% (n = 402) of Black, non-Hispanic adults reported a disability; the most common disabilities were mobility only disabilities [4.7% (n = 197)] and multiple disabilities, including mobility disability [3.0% (n = 100)]. Among Hispanic adults, 8.1% reported a disability, most commonly mobility only disabilities [2.8% (n = 119)].
The predicted proportions of access to care outcomes by race/ethnicity and disability are shown in Figure 1. Within each racial/ethnic group, PwD were significantly more likely to delay or forego care than their peers without disabilities. Nearly 30% of PwD forewent services due to cost (Black, non-Hispanic: 28.2%; Hispanic: 26.5%) compared to persons without disabilities (Black, non-Hispanic: 17.1%; Hispanic: 15.7%, both p < 0.001). There were no significant differences in access to usual source of care by disability group for either racial/ethnic group or for delaying care due to cost among Black, non-Hispanic adults.
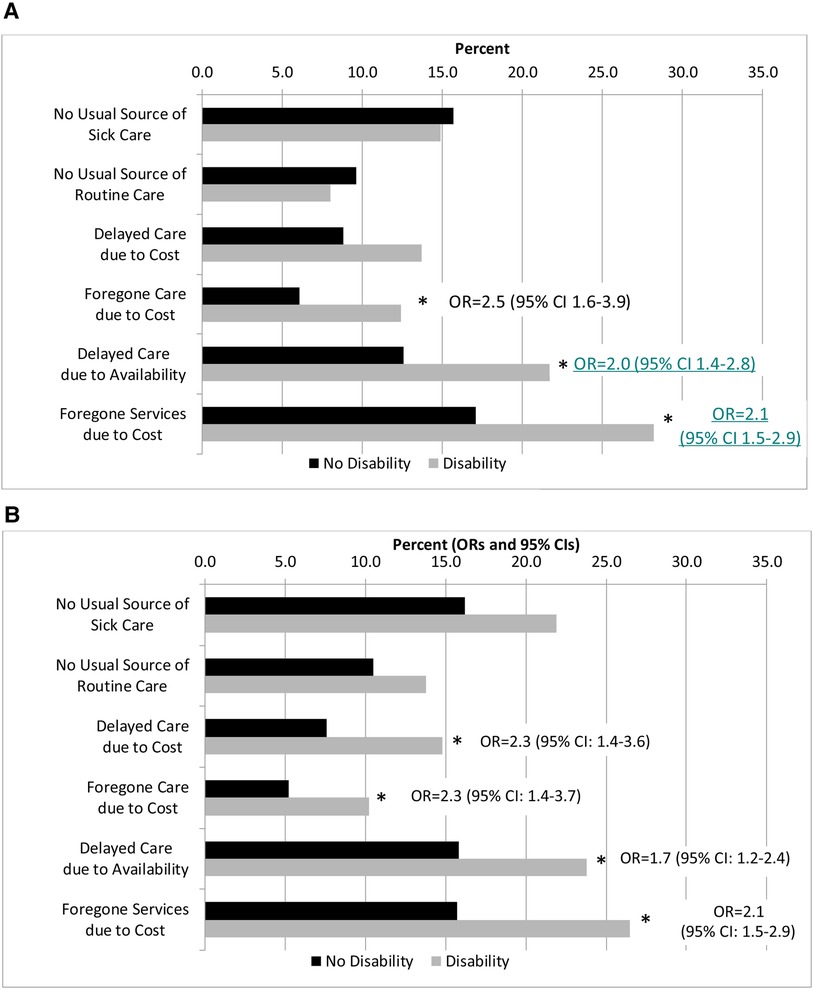
Figure 1. Predicted probabilities of access to healthcare by race/ethnicity and disability Status. (A) Black, non-Hispanic Adults. (B) Hispanic Adults. *p < 0.017, Indicates that the Odds ratios (OR) and 95% confidence intervals (CI) from logistic regression controlling for age, sex, marital status, employment status, educational attainment, poverty ratio, chronic conditions, and health insurance type. The ORs represent the disability group in reference to the no disability group.
We found that Black and Hispanic adults with disabilities were significantly more likely to forego or delay care due to reasons such as cost as compared to Black and Hispanic adults without disabilities. This suggests that BIPOC with disabilities experience greater disparities in access to healthcare than those without disabilities. This may reflect the systemic economic barriers experience by both BIPOC and disability communities, as well as those who experience intersectionality (10, 21). Policies and programs are needed to reduce costs whenever possible to ensure that BIPOC with disabilities (and BIPOC and PwD more generally) receive timely access to appropriate healthcare.
We found that across both Black and Hispanic populations, there was no difference in reporting a usual source of care by disability status. This is similar to the findings of a study using Medicare Expenditure Panel Survey data from 2002 to 2010 (22). This study found that Hispanics with basic activity limitations were the only group to be more likely to report lacking a usual source of care, as compared to other disability groups who are Hispanic.
Racism and ableism are often thought of as parallel systems of oppression that work separately, yet this notion ignores experiences at the intersection of BIPOC and PwD (8, 9). Our findings bring together separate bodies of scholarship that show that PwD and racial/ethnic minority populations experience disparities compared to their non-disabled and non-Hispanic white peers. Moreover, our findings highlight the need to account for the intersection of these identities in future analyses to appropriately tailor programs and policies. The health care disparities experienced by racial and ethnic minorities living with disabilities is likely influenced by systemic racism and systemic ableism factors.
There are limitations to our findings. We focused our analysis on Black, non-Hispanic adults and Hispanic adults with and without disabilities. Additional research should be conducted to investigate Asian and Indigenous populations. Additionally, due to sample size, we collapsed disability types. Differences may exist based on type of disability. Another limitation is the fact the findings are descriptive and do not consider longitudinal data or related contextual factors. Health disparities research is often examined through risk and not indicative of a strength-based approach. Finally, the term BIPOC does not account for or reflect the breadth of diversity among BIPOC individuals. More research should be done to acknowledge and examine the diversity across and within BIPOC PwD.
Future research should examine the intersection of social stressors such as racism and ableism and how they uniquely impact the health outcomes of BIPOC individuals. The disparity at the intersection of BIPOC and disability suggests disability access issues faced by BIPOC with disabilities cannot be solved without systemic reform of the healthcare delivery system. With respect to systemic challenges faced by BIPOC PwD and in line with other initiatives and recommendations to increase health equity for other marginalized groups, it is likely that systemic changes such as reducing costs associated with quality health care, increasing accessibility to health care, and building provider competency in the unique needs of racial and ethnic minority PwD may meaningfully improve health outcomes for this community. However, further qualitative examination of health needs from the perspective of members of this community is needed.
Meeting the health needs of BIPOC with disabilities is a matter of quality as much as it is equity. BIPOC with disabilities are likely to experience additional barriers such as racism, compounded by what is often an urgent or chronic need to maintain frequent consistent use of the healthcare system. Understanding health outcomes experienced by those who are members of both groups is critical to developing successful interventions aimed at improving health outcomes for this marginalized group.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://www.cdc.gov/nchs/nhis/nhis_2018_data_release.htm.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
The authors confirm contribution to the paper as follows: study conception and design: BD and MM; data collection: MS; analysis and interpretation of results: BD, ND and MS; draft manuscript preparation: all authors. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Varadaraj V, Deal JA, Campanile J, Reed NS, Swenor BK. National prevalence of disability and disability types among adults in the US, 2019. JAMA Netw Open. (2021) 4(10):e2130358. doi: 10.1001/jamanetworkopen.2021.30358
2. Okoro CA, Hollis ND, Cyrus AC, Griffin-Blake S. Prevalence of disabilities and health care access by disability Status and type among adults—United States, 2016. MMWR Morb Mortal Wkly Rep. (2018) 67(32):882–7. doi: 10.15585/mmwr.mm6732a3
3. Fiscella K, Sanders MR. Racial and ethnic disparities in the quality of health care. Annu Rev Public Health. (2016) 37:375–94. doi: 10.1146/annurev-publhealth-032315-021439
4. Institute of medicine committee on understanding eliminating racial ethnic disparities in health care. In: Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press (US) (2003).
5. Iezzoni LI. Eliminating health and health care disparities among the growing population of people with disabilities. Health Aff (Millwood). (2011) 30(10):1947–54. doi: 10.1377/hlthaff.2011.0613
6. Manuel JI. Racial/ethnic and gender disparities in health care use and access. Health Serv Res. (2018) 53(3):1407–29. doi: 10.1111/1475-6773.12705
7. Stransky M, Jensen K, Morris MA. Adults with communication disabilities experience poorer health and healthcare outcomes compared to people without communication disabilities. J Gen Intern Med. (2018) 33(12):2147–55. doi: 10.1007/s11606-018-4625-1
9. Bailey M, Mobley IA. Work in the intersections: a black feminist disability framework. Gend Soc. (2019) 33(1):19–40. doi: 10.1177/0891243218801523
10. Courtney-Long EA, Romano SD, Carroll DD, Fox MH. Socioeconomic factors at the intersection of race and ethnicity influencing health risks for people with disabilities. J Racial Ethn Health Disparities. (2017) 4(2):213–22. doi: 10.1007/s40615-016-0220-5
11. Arana E, Carroll-Scott A, Massey PM, Lee NL, Klassen AC, Yudell M. Racial/ethnic disparities in mammogram frequency among women with intellectual disability. Intellect Dev Disabil. (2019) 57(3):177–87. doi: 10.1352/1934-9556-57.3.177
12. Landes SD, Wilmoth JM, McDonald KE, Smith AN. Racial-ethnic inequities in age at death among adults with/without intellectual and developmental disability in the United States. Prev Med. (2022) 156:106985. doi: 10.1016/j.ypmed.2022.106985
13. Li H, Parish SL, Magaña S, Morales MA. Racial and ethnic disparities in perceived barriers to health care among U.S. adults with intellectual and developmental disabilities. Intellect Dev Disabil. (2021) 59(1):84–94. doi: 10.1352/1934-9556-59.1.84
14. Magaña S, Parish S, Morales MA, Li H, Fujiura G. Racial and ethnic health disparities among people with intellectual and developmental disabilities. Intellect Dev Disabil. (2016) 54(3):161–72. doi: 10.1352/1934-9556-54.3.161
15. Scott HM, Havercamp SM. Race and health disparities in adults with intellectual and developmental disabilities living in the United States. Intellect Dev Disabil. (2014) 52(6):409–18. doi: 10.1352/1934-9556-52.6.409
16. Horner-Johnson W, Akobirshoev I, Amutah-Onukagha NN, Slaughter-Acey JC, Mitra M. Preconception health risks among U.S. women: disparities at the intersection of disability and race or ethnicity. Womens Health Issues. (2021) 31(1):65–74. doi: 10.1016/j.whi.2020.10.001
17. Parish SL, Swaine JG, Son E, Luken K. Receipt of mammography among women with intellectual disabilities: medical record data indicate substantial disparities for African American women. Disabil Health J. (2013) 6(1):36–42. doi: 10.1016/j.dhjo.2012.08.004
18. National Center for Health Statistics. Health, United States. Health, United States, 2018. Hyattsville, MD: National Center for Health Statistics (US) (2019).
19. Reichard A, Stransky M, Phillips K, Drum C, McClain M. Does type of disability matter to public health policy and practice? Calif I Health Promot. (2015) 13(2):25–36. doi: 10.32398/chp.v1312.1821
20. Sedgwick P. Multiple significance tests: the Bonferroni correction. Br Med J. (2012) 344:e509. doi: 10.1136/bmj.e509
21. Institute ND. Race, Ethnicity and Disability: The Financial Impact of Systemic Inequality and Intersectionality. Available at: https://www.nationaldisabilityinstitute.org/webinars/april-28-race-ethnicity-and-disability-the-financial-impact-of-systemic-inequality-and-intersectionality/ (Accessed June 1, 2022).
Keywords: disability, discrimination, BIPOC, disparities (health, racial), survey data
Citation: Dorsey Holliman B, Stransky M, Dieujuste N and Morris M (2023) Disability doesn’t discriminate: health inequities at the intersection of race and disability. Front. Rehabil. Sci. 4:1075775. doi: 10.3389/fresc.2023.1075775
Received: 20 October 2022; Accepted: 2 June 2023;
Published: 6 July 2023.
Edited by:
Adria Quigley, Dalhousie University, CanadaReviewed by:
Kara Ayers, Cincinnati Children’s Hospital Medical Center, United States© 2023 Dorsey Holliman, Stransky, Dieujuste and Morris. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brooke Dorsey Holliman YnJvb2tlLmRvcnNleWhvbGxpbWFuQGN1YW5zY2h1dHouZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.