
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Rehabil. Sci. , 12 December 2022
Sec. Rehabilitation for Musculoskeletal Conditions
Volume 3 - 2022 | https://doi.org/10.3389/fresc.2022.983432
This article is part of the Research Topic Advances in Rehabilitation Interventions after Limb Amputation View all 5 articles
People with lower limb loss, especially of dysvascular etiology, are at substantial risk for both ipsilateral and contralateral reamputation. Additionally, while not as well documented for reamputation, there is recognition that amputation incidence is influenced by not only sociodemographic factors such as sex, race, socioeconomic status, but also by system factors such as service access. A systems strategy to address this disparity within the field of limb-loss rehabilitation is for Limb-loss Rehabilitation Programs (LRP) to partner with medical specialists, mental health professionals, and Limb Preservation Programs (LPP) to provide comprehensive limb care. While LPPs exist around the nation, design principles for such programs and their partnership role with LRPs are not well established. Using a socioecological model to incorporate hierarchical stakeholder perspectives inherent in the multidisciplinary field of limb care, this review synthesizes the latest evidence to focus on LPP design and implementation principles that can help policymakers, healthcare organizations and limb-loss rehabilitation and limb-preservation professionals to develop, implement, and sustain robust LPP programs in partnership with LRPs.
50,000–60,000 major amputations occur every year, with peripheral arterial disease (PAD) and diabetes mellitus being the most common causes (1). Rates of reamputation remain high following major amputations, with 1-year and 5-year contralateral major amputation rates being 5.7% and 11.5%, respectively. Even after minor amputations, 1-year and 5-year rates of are high, being 3.2% and 8.4% for contralateral major amputations, and 10.5% and 14.2% for ipsilateral major amputations, respectively. Risk of contralateral amputation increases with renal disease and atherosclerosis with or without diabetic neuropathy (2), with ipsilateral reamputation rates in diabetic patients being 5, 12, and 13% at 1-year, 3-year, and 5-year periods (3). 5-year mortality rates range from 29% to 69% following minor amputations, and from 52% to 80% for major amputations (4). This high risk of reamputation following limb loss, especially with dysvascular etiology, requires comprehensive limb care with not only Limb-Loss Rehabilitation Programs (LRP) to manage the complex care and comorbidities of the post limb-loss patient population, but also partnership with Limb-Preservation Programs (LPP) to minimize subsequent limb-loss. This mini-review article focuses specifically on LPPs as partners for LRPs to enable comprehensive limb care.
The overarching vision of LPPs is attainment of pain-free, functioning limbs that enable continued independence with excellent quality of life, while using limited resources optimally to maximize care delivery through coordinated multidisciplinary team care. While most robust LPP programs exist at tertiary-level academic centers (5) and within the Veterans Healthcare system (6), many of the design principles and strategies for developing and implementing such highly coordinated LPPs can be adapted by other healthcare organizations to improve overall limb-care health equity across geographic boundaries.
The authors utilize an established public health concept, the socio-ecological model (7), as a framework to present a structured hierarchical perspectives-inclusive overview of LPP design principles and implementation strategies. The article is comprised of 3 sections, describing the need for LPP services (Section “Need for limb-preservation program (LPP) services”), socioecological-level based limb care model structure focusing on partnerships between LPP and other programs (Section “Socio-ecological level-based limb care structural model”), and multilevel implementation strategies that can be adopted by healthcare organizations for LPP development (Section “Multilevel interventions and implementation strategies for LPP development”).
The goal of LPPs is early recognition of disease to facilitate preventive care and timely intervention, with individualized plans and ultimate reduction in amputation risk and rates. LPPs vary in terms of structure, and can include a combination of vascular, and limb reconstruction services.
Nonhealing wounds affect 3 to 6 million people in US with annual healthcare costs exceeding $3 billion (8). Studies have reported the occurance of foot ulcerations in as many as 85% patients needing amputation (9). Hence, dedicated wound care teams are needed to optimize clinical outcomes and cost (10).
Trans-Atlantic Inter-Society Consensus Working Group II estimates PAD-related major amputation incidence of 12–50/100,000 (11). Threefold-increase in endovascular interventions was shown to decrease amputation rates by 25% despite the increasing prevalence of diabetes in Medicare beneficiaries from 1996 to 2006 (12). However, this may not be enough, with only 68.4% undergoing arterial testing prior to amputation in 17,463 Medicare non-traumatic amputees from 2000 to 2010. Although some clinical scenarios (such as fulminant infection) preclude attempts at limb salvage, diagnosis, and treatment of limb ischemia prior to undertaking major amputation remains a key goal (13). Such decision-making and interventions require vascular services.
Residual limb issues that limit optimal prosthetic device fitting and use, such as chronic wounds, prominent bone edges, redundant soft tissue, and neuromas (14) are some indications for review and further management with limb reconstruction services offered by specialties such as Plastic surgery and Orthopedic Surgery.
Ideally, these three services should coexist and collaborate to provide comprehensive limb preservation care, in partnership with rehabilitation, primary care, and mental health services. Depending upon resources, specialists in infectious diseases, endocrinology, cardiology, interventional radiology, plastic surgery, and pain management should be included in the program. Mental health resources can include psychologist, counselor, or psychiatrist services. Rehabilitation services provided by Physical Medicine and Rehabilitation (PM&R), occupational and physical therapy specialists should be offered to maintain a high level of functioning.
Healthcare institutions and organizations seeking to develop, expand or refine their ability to provide comprehensive limb care would benefit from using a conceptual model to comprehensively understand their current structure (Section “Socio-ecological level-based limb care structural model”), followed by determination of implementation strategies and interventions to address context-specific factors (Section “Multilevel interventions and implementation strategies for LPP development”). Both the Limb Care model structure and implementation strategies are described using the socio-ecological model to incorporate hierarchical stakeholder perspectives inherent in the multidisciplinary field of limb care.
LPPs to address diabetic foot ulcers (15) and ischemic limbs (16) provide valuable insight into program design. To further expand on how LPPs can integrate with other services to provide comprehensive limb care, the authors present a Limb Care model that illustrates LPP partnerships with LRPs and other synergistic programs (Figure 1).
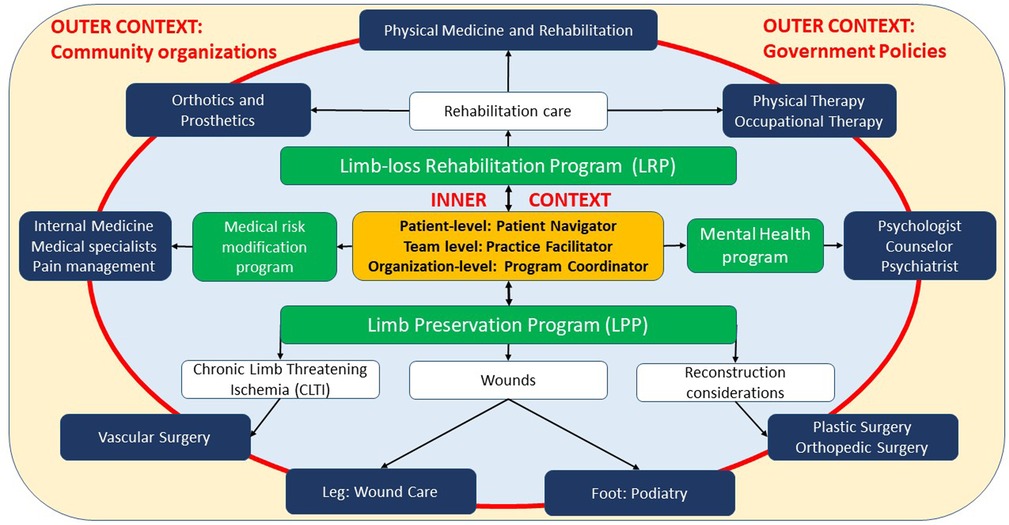
Figure 1. Model for comprehensive limb care though partnership between limb-loss rehabilitation, limb preservation, medical risk modification, and mental health programs.
The model structure includes four main constructs: context (outer yellow box and inner light blue oval, separated by a red boundary), programs (green boxes), services (dark blue boxes), and central coordination (orange box). Outer Context and Inner Context are implementation science model [e.g., EPIS (17)] constructs that reflect the ability of a program to influence factors at various socio-ecological levels. Outer Context includes system and community socio-ecological levels. Factors at these levels are entrenched and not easily influenced by a program. Implementation strategies at these levels are described in Sections “System level: understand policies and payment mechanisms” and “Community level: utilize patient resources and evidence-based guidelines”. Inner Context include patient, provider, and organization socio-ecological levels. Factors at these levels are often within a programs' sphere of influence. Implementation strategies at these levels are described in Sections “Organization level: develop processes for quality, coordination, and program sustainability”, “Provider-level principles: stay up to date with standard-of-care diagnosis and management practices” and “Patient-level principles: empower through education and navigation strategies”.
The partnership of LPPs with other programs lies within Inner Context. LPP includes four services, that are accessed based upon the specific indication for limb preservation. Vascular surgery services are utilized for limb threatening ischemia. Wound care and podiatry services are utilized based upon wound location proximal and distal to the ankle, respectively. Plastic and Orthopedic Surgery services are utilized to address reconstruction needs, as described in Section “Need for limb-preservation program (LPP) services”. Three other programs are included within inner context. LRPs include PM&R, orthotics and prosthetics and therapy services to address rehabilitation needs. Medical Risk Modification Programs include internal medicine, pain management, and other medical specialists to minimize medical risk for reamputation. Mental Health Programs can include psychologist, counselor, and psychiatry services to optimize psychological health.
Central coordination is at the core of this model's LPPs partnerships with the other programs. Interventions for successful coordination have been described for healthcare programs such as maternal health, behavioral health, and oncology. Examples of some of these interventions that are potentially applicable for limb care program coordination are listed in the Central coordination box, and include program coordinators (18) (organization-level), practice facilitators (19) (provider-level), and patient navigators (20) (patient-level).
Once healthcare organizations have a good understanding of their limb care program structure and resources, determination of multilevel interventions and implementation strategies for LPP development and refinement is the next step. Examples of such interventions and implementation strategies corresponding to socio-ecological levels are presented in Section “Multilevel interventions and implementation strategies for LPP development” (Figure 2).
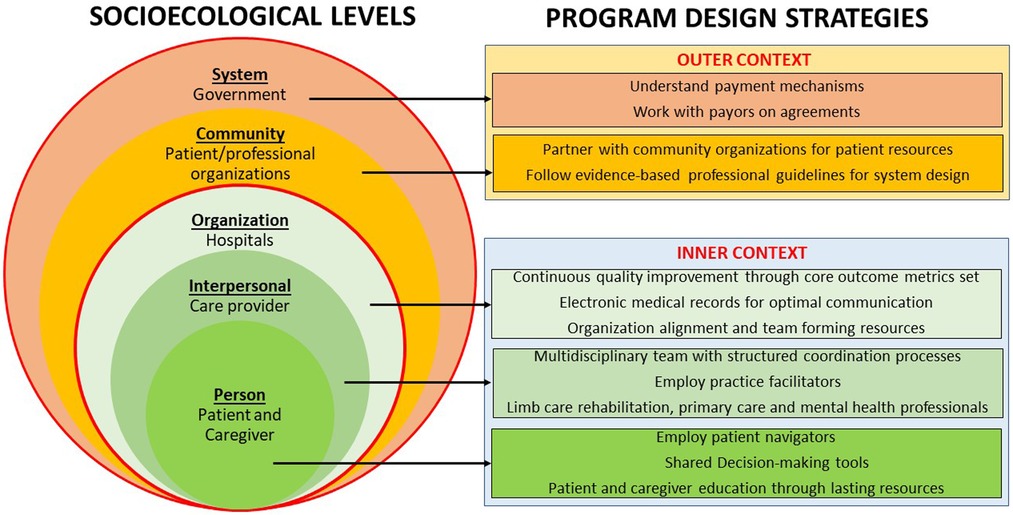
Figure 2. Socioecological level-based limb preservation program (LPP) design strategies for inner and outer context.
National health policies and payment mechanisms influence access for people seeking limb-preservation services. An example is higher amputation rates for people without insurance and with Medicaid (21). These payment mechanisms also influence provider payment and organizational reimbursement. Programs must understand their system factors and work with payors to maximize their ability to provide care.
Patient's physical and social environment (22) can limit patient access to healthcare. Appointment adherence can be addressed with interventions such as transport and appointment reminders. Home wheelchair accessibility limitations can be addressed by home assessment and modifications, which may require partnerships with community rehabilitation agencies such as vocational rehabilitation. Community mobility can be enabled by power wheelchairs/scooters. Prescription must be customized to individuals based upon potential for overuse injuries balanced with deconditioning.
Patient advocacy organizations such as Amputee Coalition (https://www.amputee-coalition.org/) and Limb Preservation Foundation (https://limbpreservation.org/) offer resources for persons with threatened limb loss such as peer mentors as well as educational resources in online and print formats, such as the First Step Manual in English (https://shop.amputee-coalition.org/first-step-p42.aspx) and Spanish (https://shop.amputee-coalition.org/first-step-en-espaol-una-gua-para-adaptarse-a-la-prdida-de-extremidades-p26.aspx). Programs should make use of these community resources for patient education.
Professional organizations are increasingly collaborating for standardization of care and quality guidelines. Evidence-based wound care guidelines by World Healing Foundation have enabled care for not only common etiologies, but also uncommon etiologies such as rheumatologic disorders with vasculitis, and dermatologic abnormalities with pyoderma (23, 24). Peripheral Academic Research Consortium has provided consensus definitions for standardization of clinical studies with Peripheral Arterial Disease/Chronic Limb Threatening Ischemia, with development of evidence-based clinical practice guidelines (25). Global Vascular Guidelines jointly released by the Society for Vascular Surgery, European Society for Vascular Surgery, and World Federation of Vascular Societies (26) incorporate wound, ischemia, and foot infection (WiFi) staging (27) and Global Anatomic Staging System (GLASS) methodology (28) for anatomic assessment and triaging into medical management and surgical intervention groups. The LEAP program developed in 1992 by HRSA (https://www.hrsa.gov/hansens-disease/leap) is a good example of wound prevention principles for people with impaired foot sensation that can be implemented by primary care. Programs should embed standard guidelines within their care programs.
Programs should define outcome metric sets for continuous quality improvement. Examples of clinical metrics include wound healing rates, healing time exceeding 30 or 60 days, wound care/vascular technique type, and amputation rate. Example of utilization metrics include charges billed to insurance company, cost incurred to patient, and collection by the facility. Examples of functioning and rehabilitation metrics include pain control (impairment), distance and speed of ambulation (activity) and return to work (participation). Patient reported outcome measures (PROMs) including satisfaction with care are useful to understand patient perspective.
Programs should employ electronic medical records (EMR) for optimal information sharing and care coordination. Given the heterogeneity in patient characteristics, wound-care diagnostic protocols and therapies (29, 30), scientific evidence for using EMR data for a precision medicine approach, matching patients with best therapies for best clinical outcomes and resource utilization is a work in progress.
While effective multi-disciplinary teams are effective in decreasing amputation prevalence (31), dedicated support from the organizations that invest in education and team-forming resources is vital. The role of organizational champions cannot be overstated (32). Practice facilitators may play an integral role in team-forming as well.
A comprehensive history should elucidate information on potential risk factors for wounds and vascular disease such as injury, diabetes, neuropathy, ill-fitting shoes, smoking, and sedentary lifestyle. Physical exams should include a detailed evaluation for changes related to vascular insufficiency, neuropathy, and foot architecture. Diagnostic testing should be guided by the history and exam as well as resources available. This can range from simple screens such as Semmes-Weinstein monofilament exam, to digital photography and vascular lab studies, to even more sophisticated tests such as tissue concentration of oxygen, and near infra-red photography (33). Comprehensive holistic evaluation should be accompanied by realistic expectation setting (34, 35).
Fifty percent reduction in wound area by 30 days (36) is a clinically accepted goal. Delay in wound healing should prompt evaluation for contributory factors and consideration for more advanced diagnostic and management techniques. Early debridement can be both diagnostic and therapeutic. Chronic ulcerations often need serial debridement and biopsies, and abnormal bony architecture may need correction, combined with off-loading positioning education, mattress overlays, shoes, and sometimes total contact casting (37). Inflammatory, nutritional, or collagen-based deficiencies hampering wound healing should be addressed as well. Once a clean wound bed is obtained, further support can be provided by re-epithelialization techniques from grafting to cultured skin grafts and other biological implants, to skin and tissue scaffolds. Advanced modalities include hyperbaric oxygen to stimulate neo-angiogenesis (38, 39), e-stimulation and ultrasound (40), complex angiosomal reconstruction and negative pressure either alone or in combinations with skin grafting options, pro-healing scaffolds, biologically stimulating dressings, and pluri-potent cell lines. Classification of wounds, appropriate diagnosis and intervention strategy selection should be based upon the latest clinical practice guidelines (41), available resources, and shared decision making with patients and their caregivers.
Interventions can range from vein bypasses and open aortobifemoral reconstructions to endovascular interventions such as drug delivery to limit restenosis, lithotripsy of calcified lesions, pedal loop interventions, and deep venous arterialization for desert foot. Hybrid interventions that combine open and endovascular options responsive to individual factors such as anatomy, disease burden and co-morbidities have been steadily increasing [6.1% in 2010 to 32% in 2017 (42)]. Efforts should focus on the restoration of inline flow to the wound-specific angiosome, which results in the best chance of wound healing. Surgical intervention recommendation for claudicants depend upon anatomic location, with better chances of symptom improvement with aortoiliac and common femoral segment who fail medical treatment alone. Interestingly, vascular interventions in claudicants have not shown a reduction in progression to limb-threatening ischemia and amputation (43). Regenerative medicine approaches like gene and cell therapy for CLTI should be restricted to randomized controlled trials.
Contemporary thought emphasizes that amputation surgery itself be considered a reconstructive surgery (44). Reconstruction of a functional residual limb is the goal, and this should include surgical measures to prevent chronic pain and biomechanical or soft tissue deformities that make ambulation with a prosthesis difficult. Residual limb issues that limit prosthetic device fitting and use, such as chronic wounds, neuromas, prominent anatomy, and redundant tissue are indications for review and further management with limb reconstruction services offered by specialties such as Plastic surgery and Orthopedic Surgery. Recent innovations in peripheral nerve surgery such as targeted muscle reinnervation (TMR) (45–47) and regenerative peripheral nerve interface (RPNI) (48) techniques have improved our ability to surgically treat painful neuromas and phantom pain. Osseointegration interfaces for prosthetics are now FDA approved for transfemoral amputation and increasingly available. For appropriate patients, they offer the advantages of improved skeletal alignment with the prosthesis, subsequent reduction in energy expenditure, simplified donning and doffing, and improvement in quality of life (49). Adoption may be slow related to surgical expertise as well insurance issues.
Programs should address risk factor modification and medical optimization for reducing long-term risks such as cardiovascular mortality and morbidity, by managing conditions such as diabetes, chronic kidney disease and hypertension, and smoking cessation. Antiplatelet therapy with aspirin or clopidogrel reduces the risk of myocardial infarction, stroke, and death in these patients (50). High potency statin therapy reduces risk of cardiovascular mortality and amputation risk in PAD patients (51, 52). Aspirin with low dose rivaroxaban has major cardiovascular benefit and reduced need for revascularization compared with revascularization alone per the VOYAGER PAD trial (53).
Both prior mental health concerns and new concerns that arise with major surgeries such as amputations (54) should be addressed by including mental health professionals such as psychologists, counselors, and psychiatrists in the care provider team. Peer-mentors offer a valuable resource for mental health as well.
Programs should include PM&R guided therapy, medical equipment, assistive devices (e.g., wheelchair, walker, cane) and orthotic determination, presurgical planning, postsurgical rehabilitation care, and care coordination with community resources such as peer support, vocational, recreational, and driving rehabilitation. The value to prehabilitation for improving postoperative outcome such as mobility is a promising area of study (55).
Program should include patient education strategies, with the goal of maximizing patient understanding, participation in decision making and realistic goal setting (56). Patient navigation resources help patients to navigate complicated care-delivery systems. Examples of outcomes that can be measured include self -foot exams, adherence to medical and rehabilitation management recommendations, appointment no-shows, and quality of life metrics.
Surgical decision making should be guided by patient's expectations and health conditions.
Inability to adhere to recommendations for medical (e.g., oncologic) and other reasons may be better served with earlier tissue resection and closures rather than prolonged attempts at healing. This is because the latter can lead to potential secondary complications such as immobility-related cardio-respiratory functional decline, and long-term antibiotics-related worsening renal function. Where wounds represent a terminal condition such as those seen in cancer or Kennedy terminal ulcerations, palliative or custodial wound care may be presented as option.
Limb care is an inter-disciplinary field. Comprehensive programs should be partnerships between LRP and LPP that address not only limb health, but also medical risk factors, mental health, and functioning, with the goal of optimizing long-term outcomes and quality of life. A multilevel approach that includes system, community, organization, provider, and patient perspectives should guide comprehensive LPP design. Major strategies should include realistic goal setting and adherence promotion with patient empowerment, multidisciplinary team-based approach that incorporates standard-of-care practices, focus on process improvement and EMRs for efficient communication, utilization of evidence-based guidelines and established patient resources, and working with payors to maximize impact.
VK, JPK, PG, JF and PG contributed substantially to discussions for the manuscript and abstract. VK, JPK, PG, and PG contributed substantially to manuscript text. VK, PG, and PG contributed substantially to figures. All authors contributed to the article and approved the submitted version.
Prateek Grover’s potential non-financial, non-commercial COIs include service as a member of the Amputee Coalition Scientific and Medical Advisory Committee, and chair of the American Congress of Rehabilitation Medicine Limb Care Networking Group.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Nowygrod R, Egorova N, Greco G, Anderson P, Gelijns A, Moskowitz A, et al. Trends, complications, and mortality in peripheral vascular surgery. J Vasc Surg. (2006) 43(2):205–16. doi: 10.1016/j.jvs.2005.11.002
2. Glaser JD, Bensley RP, Hurks R, Dahlberg S, Hamdan AD, Wyers MC, et al. Fate of the contralateral limb after lower extremity amputation. J Vasc Surg. (2013) 58(6):1571–1577.e1. doi: 10.1016/j.jvs.2013.06.055
3. Izumi Y, Satterfield K, Lee S, Harkless LB. Risk of reamputation in diabetic patients stratified by limb and level of amputation: a 10-year observation. Diabetes Care. (2006) 29(3):566–70. doi: 10.2337/diacare.29.03.06.dc05-1992
4. Cascini S, Agabiti N, Davoli M, Uccioli L, Meloni M, Giurato L, et al. Survival and factors predicting mortality after major and minor lower-extremity amputations among patients with diabetes: a population-based study using health information systems. BMJ Open Diabetes Res Care. (2020) 8(1):e001355. doi: 10.1136/bmjdrc-2020-001355
5. Sobti N, Park A, Crandell D, Smith FA, Valerio I, Lozano-Calderon SA, et al. Interdisciplinary care for amputees network: a novel approach to the management of amputee patient populations. Plast Reconstr Surg Glob Open. (2021) 9(2):e3384. doi: 10.1097/GOX.0000000000003384
6. Webster JB, Poorman CE, Cifu DX. Guest editorial: department of veterans affairs amputations system of care: 5 years of accomplishments and outcomes. J Rehabil Res Dev. (2014) 51(4):vii–xvi. doi: 10.1682/JRRD.2014.01.0024
7. Dahlberg LL, Krug EG. Violence: A global public health problem. In: Krug E, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. World report on violence and health. Geneva, Switzerland: World Health Organization (2002). p. 1–21.
8. Mathieu D, Linke JC, Wattel F. Non-Healing wounds. In: Mathieu D, editors. Handbook on hyperbaric medicine. Dordrecht: Springer (2006). doi: 10.1007/1-4020-4448-8_20
9. Reiber GE, Boyko EJ, Smith DG. Chapter 18: Lower extremity foot ulcers and amputations in diabetes. In: Diabetes in America. 2nd ed: National Diabetes Data Group, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. p. 409–28.
10. Ennis WJ. Wound care specialization: the current Status and future plans to move wound care into the medical community. Adv Wound Care (New Rochelle). (2012) 1(5):184–8. doi: 10.1089/wound.2011.0346
11. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG. TASC II working group. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. (2007) 45(Suppl S):S5–67. doi: 10.1016/j.jvs.2006.12.037
12. Goodney PP, Beck AW, Nagle J, Welch HG, Zwolak RM. National trends in lower extremity bypass surgery, endovascular interventions, and major amputations. J Vasc Surg. (2009) 50(1):54–60. doi: 10.1016/j.jvs.2009.01.035
13. Vemulapalli S, Greiner MA, Jones WS, Patel MR, Hernandez AF, Curtis LH. Peripheral arterial testing before lower extremity amputation among medicare beneficiaries, 2000 to 2010. Circ Cardiovasc Qual Outcomes. (2014) 7(1):142–50. doi: 10.1161/CIRCOUTCOMES.113.000376
14. Mioton LM, Dumanian GA, Shah N, Qiu CS, Ertl WJ, Potter BK, et al. Targeted muscle reinnervation improves residual limb pain, phantom limb pain, and limb function: a prospective study of 33 major limb amputees. Clin Orthop Relat Res. (2020) 478(9):2161–7. doi: 10.1097/CORR.0000000000001323
15. Khan T, Shin L, Woelfel S, Rowe V, Wilson BL, Armstrong DG. Building a scalable diabetic limb preservation program: four steps to success. Diabet Foot Ankle. (2018) 9(1):1452513. doi: 10.1080/2000625X.2018.1452513
16. Neville RF, Kayssi A. Development of a limb-preservation program. Blood Purif. (2017) 43(1-3):218–25. doi: 10.1159/000452746
17. Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA. Systematic review of the exploration, preparation, implementation, sustainment (EPIS) framework. Implement Sci. (2019) 14(1):1. doi: 10.1186/s13012-018-0842-6
18. Cordasco KM, Katzburg JR, Katon JG, Zephyrin LC, Chrystal JG, Yano EM. Care coordination for pregnant veterans: VA's Maternity care coordinator telephone care program. Transl Behav Med. (2018) 8(3):419–28. doi: 10.1093/tbm/ibx081
19. Siantz E, Redline B, Henwood B. Practice facilitation in integrated behavioral health, and primary care settings: a scoping review. J Behav Health Serv Res. (2021) 48(1):133–55. doi: 10.1007/s11414-020-09709-1
20. Cantril C, Haylock PJ. Patient navigation in the oncology care setting. Semin Oncol Nurs. (2013) 29(2):76–90. doi: 10.1016/j.soncn.2013.02.003
21. Hughes K, Mota L, Nunez M, Sehgal N, Ortega G. The effect of income and insurance on the likelihood of major leg amputation. J Vasc Surg. (2019) 70(2):580–7. doi: 10.1016/j.jvs.2018.11.028
22. ICF Checklist Version 2.1a. Clinician Form for International Classification of Functioning, Disability and Health. Available at: https://cdn.who.int/media/docs/default-source/classification/icf/icfchecklist.pdf?sfvrsn=b7ff99e9_4&download=true
23. Sibbald RG, Woo K, Ayello EA. Increased bacterial burden and infection: the story of NERDS and STONES. Adv Skin Wound Care. (2006) 19(8):447–61; quiz 461–3. doi: 10.1097/00129334-200610000-00012
24. Ansert E, Tickner A, Cohen D, Murry W, Gorelik S. Understanding the zebras of wound care: an overview of atypical wounds. Wounds. (2022) 34(5):124–34. doi: 10.25270/wnds/2022.124134
25. Patel MR, Conte MS, Cutlip DE, Dib N, Geraghty P, Gray W, et al. Evaluation and treatment of patients with lower extremity peripheral artery disease: consensus definitions from peripheral academic research consortium (PARC). J Am Coll Cardiol. (2015) 65(9):931–41. doi: 10.1016/j.jacc.2014.12.036; Erratum in: J Am Coll Cardiol. (2015) 65(23):2578–9.25744011
26. Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, et al. GVG Writing group. Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg. (2019) 69(6S):3S–125S.e40. doi: 10.1016/j.jvs.2019.02.016; Erratum in: J Vasc Surg. (2019) 70(2):662.31159978
27. Mills JL Sr, Conte MS, Armstrong DG, Pomposelli FB, Schanzer A, Sidawy AN, et al. Society for vascular surgery lower extremity guidelines committee. The society for vascular surgery lower extremity threatened limb classification system: risk stratification based on wound, ischemia, and foot infection (WIfI). J Vasc Surg. (2014) 59(1):220–34.e1-2. doi: 10.1016/j.jvs.2013.08.003
28. Wijnand JGJ, Zarkowsky D, Wu B, van Haelst STW, Vonken EPA, Sorrentino TA, et al. The global limb anatomic staging system (GLASS) for CLTI: improving inter-observer agreement. J Clin Med. (2021) 10(16):3454. doi: 10.3390/jcm10163454
29. Jones CM, Rothermel AT, Mackay DR. Evidence-Based medicine: wound management. Plast Reconstr Surg. (2017) 140(1):201e–16e. doi: 10.1097/PRS.0000000000003486
30. Welsh L. Wound care evidence, knowledge and education amongst nurses: a semi-systematic literature review. Int Wound J. (2018) 15(1):53–61. doi: 10.1111/iwj.12822
31. Flores AM, Mell MW, Dalman RL, Chandra V. Benefit of multidisciplinary wound care center on the volume and outcomes of a vascular surgery practice. J Vasc Surg. (2019) 70(5):1612–9. doi: 10.1016/j.jvs.2019.01.087
32. Hendy J, Barlow J. The role of the organizational champion in achieving health system change. Soc Sci Med. (2012) 74(3):348–55. doi: 10.1016/j.socscimed.2011.02.009
33. Armstrong DG, Meyr AJ. Basic Principles of Wound Management, © 2022 UpToDate, Inc. Available at: https://www.uptodate.com/contents/basic-principles-of-wound-management (June 09, 2022).
34. Ubbink DT, Brölmann FE, Go PM, Vermeulen H. Evidence-Based care of acute wounds: a perspective. Adv Wound Care (New Rochelle). (2015) 4(5):286–94. doi: 10.1089/wound.2014.0592
35. Werdin F, Tennenhaus M, Schaller HE, Rennekampff HO. Evidence-based management strategies for treatment of chronic wounds. Eplasty. (2009) 9:e19. PMID: 19578487; PMCID: PMC269164519578487
36. Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care (New Rochelle). (2015) 4(9):560–82. doi: 10.1089/wound.2015.0635
37. Messenger G, Masoetsa R, Hussain I. A narrative review of the benefits and risks of total contact casts in the management of diabetic foot ulcers. J Am Coll Clin Wound Spec. (2018) 9(1–3):19–23. doi: 10.1016/j.jccw.2018.05.002
38. Huang E. Adjunctive hyperbaric oxygen therapy for diabetic foot ulcers: an editorial perspective. Undersea Hyperb Med. (2015) 42(3):177–81. PMID: 2615210126152101
39. Kirby JP. Hyperbaric oxygen indications: diabetic foot ulcers and intractable management. Mo Med. (2019) 116(3):188–91. PMID: 31527938; PMCID: PMC669029931527938
40. Ennis WJ, Lee C, Gellada K, Corbiere TF, Koh TJ. Advanced technologies to improve wound healing: electrical stimulation, vibration therapy, and ultrasound-what is the evidence? Plast Reconstr Surg. (2016) 138(3 Suppl):94S–104S. doi: 10.1097/PRS.0000000000002680
41. World Union of Wound Healing Societies. Evidence in wound care. London: Wounds International (2020). Available at: www.woundsinternational.com
42. Fereydooni A, Zhou B, Xu Y, Deng Y, Dardik A, Ochoa Chaar CI. Rapid increase in hybrid surgery for the treatment of peripheral artery disease in the vascular quality initiative database. J Vasc Surg. (2020) 72(3):977–986.e1. doi: 10.1016/j.jvs.2019.11.041
43. Fatima J, Scali S, Neal D, Vallabhaneni R, Han SM, Ochoa C, et al. VESS17. Amputation after peripheral vascular intervention and bypass for claudication in the vascular quality initiative (VQI). J Vasc Surg. (2016) 63(6):27S–8S. doi: 10.1016/j.jvs.2016.03.208
44. Pinzur MS. Outcomes-oriented amputation surgery. Plast Reconstr Surg. (2011) 127:241S–7S. doi: 10.1097/prs.0b013e318200a409
45. Dumanian GA, Potter BK, Mioton LM, Ko JH, Cheesborough JE, Souza JM, et al. Targeted muscle reinnervation treats neuroma and phantom pain in Major limb amputees: a randomized clinical trial. Ann Surg. (2019) 270(2):238–46. doi: 10.1097/SLA.0000000000003088
46. Souza JM, Cheesborough JE, Ko JH, Cho MS, Kuiken TA, Dumanian GA. Targeted muscle reinnervation: a novel approach to postamputation neuroma pain. Clin Orthop Relat Res. (2014) 472(10):2984–90. doi: 10.1007/s11999-014-3528-7
47. Valerio IL, Dumanian GA, Jordan SW, Mioton LM, Bowen JB, West JM, et al. Preemptive treatment of phantom and residual limb pain with targeted muscle reinnervation at the time of Major limb amputation. J Am Coll Surg. (2019) 228(3):217–26. doi: 10.1016/j.jamcollsurg.2018.12.015
48. Kubiak CA, Kung TA, Brown DL, Cederna PS, Kemp SWP. State-of-the-Art techniques in treating peripheral nerve injury. Plast Reconstr Surg. (2018) 141(3):702–10. doi: 10.1097/PRS.0000000000004121
49. Souza JM, Mioton LM, Harrington CJ, Potter BK, Forsberg JA. Osseointegration of extremity prostheses: a primer for the plastic surgeon. Plast Reconstr Surg. (2020) 146(6):1394–403. doi: 10.1097/PRS.0000000000007364
50. 2011 Writing Group Members; 2005 Writing Committee Members; ACCF/AHA Task Force Members. 2011 ACCF/AHA focused update of the guideline for the management of patients with peripheral artery disease (updating the 2005 guideline): a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation. (2011) 124(18):2020–45. doi: 10.1161/CIR.0b013e31822e80c3
51. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. (2019) 139(25):e1082–143. doi: 10.1161/CIR.0000000000000625; Erratum in: Circulation. (2019) 139(25):e1182–6.30586774
52. Foley TR, Singh GD, Kokkinidis DG, Choy HK, Pham T, Amsterdam EA, et al. High-Intensity statin therapy is associated with improved survival in patients with peripheral artery disease. J Am Heart Assoc. (2017) 6(7):e005699. doi: 10.1161/JAHA.117.005699; Erratum in: J Am Heart Assoc. (2019) 8(10):e002305.28711864
53. Bonaca MP, Bauersachs RM, Anand SS, Debus ES, Nehler MR, Patel MR, et al. Rivaroxaban in peripheral artery disease after revascularization. N Engl J Med. (2020) 382(21):1994–2004. doi: 10.1056/NEJMoa2000052.32222135
54. Şimsek N, Öztürk GK, Nahya ZN. The mental health of individuals with post-traumatic lower limb amputation: a qualitative study. J Patient Exp. (2020) 7(6):1665–70. doi: 10.1177/2374373520932451
55. Hijmans JM, Dekker R, Geertzen JHB. Pre-operative rehabilitation in lower-limb amputation patients and its effect on post-operative outcomes. Med Hypotheses. (2020) 143:110134. doi: 10.1016/j.mehy.2020.110134
Keywords: amputation, lower limb, program development, rehabilitation, reconstructive surgery, socioecological model of health, vascular surgical procedure, wound healing
Citation: Khetarpaul V, Kirby JP, Geraghty P, Felder J and Grover P (2022) Socioecological model-based design and implementation principles of lower limb preservation programs as partners for limb-loss rehabilitation programs— A mini-review. Front. Rehabilit. Sci. 3:983432. doi: 10.3389/fresc.2022.983432
Received: 1 July 2022; Accepted: 18 October 2022;
Published: 12 December 2022.
Edited by:
David Crandell, Spaulding Rehabilitation Hospital, United StatesReviewed by:
Katherine M. Martinez, Northwestern University, United States© 2022 Khetarpaul, Kirby, Geraghty, Felder and Grover. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Prateek Grover cGdyb3Zlci5kckBob3RtYWlsLmNvbQ==
Specialty section: This article was submitted to Rehabilitation for Musculoskeletal Conditions, a section of the journal Frontiers in Rehabilitation Sciences
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.