- 1Department of Physical Therapy, University of Miami Miller School of Medicine, Miami, FL, United States
- 2Research Group on Human Aging, Department of Physical Therapy, Alagoas State University of Health Sciences, Maceió, Brazil
- 3Department of Physical Therapy, Federal University of São Carlos, São Carlos, Brazil
- 4Guttmann Brain Health Institute, Institut Universitari de Neurorehabilitació, Barcelona, Spain
- 5Hinda and Arthur Marcus Institute for Aging Research and Deanna and Sidney Wolk Center for Memory Health, Hebrew SeniorLife, Boston, MA, United States
- 6Department of Neurology, Harvard Medical School, Boston, MA, United States
- 7Linus Health, Waltham, MA, United States
- 8Federal University of Mato Grosso Do Sul, Campo Grande, Brazil
- 9Department of Neurology, University of Miami Miller School of Medicine, Miami, FL, United States
A wealth of scientific evidence supports that being physically active may prevent or delay the onset of cognitive impairment and dementia. However, a critical barrier is that while most clinicians recommend physical activity (PA) and older adults recognize its health benefits, most older adults fail to regularly practice PA. Thus, it is necessary to explore and disseminate knowledge on how to help clinicians truly partner with people and help them to change their behavior and become more active. Clinical and scientific efforts are underway to establish dose-specific PA recommendations for cognitive brain health. However, an important knowledge gap is how to develop effective strategies to increase PA adherence in aging. To better understand the perspective of older adults, we undertook a mixed-method study on sixty-five sedentary older adults at risk for cognitive decline. Participants answered a questionnaire battery related to PA engagement, and a subcohort participated in a remote focus group. Our findings revealed four main themes: First, age and aging are determinants in PA practice. Second, maintaining both an active mind and autonomy are priorities, but planned PA is not usually related as part of being “active.” Third, motivational challenges in PA engagement were noted. And fourth, they emphasized a call for tailored recommendations. Therefore, we present a multidimensional model of PA adherence to maximize brain health in older adults and suggest a tool kit and key questions to effectively screen sedentary aging adults and translate current guidelines into the needs of the individual by using behavior change strategies.
Introduction
Physical Activity and Sedentary Behavior Change Play a Crucial Role in Promoting Brain Health
Despite the important increase in human longevity (1), living longer (lifespan) has not been followed by an equal or similar increase in living healthy (health-span). As the population ages, many will develop cognitive decline and dementia, leading to substantial loss of health and quality of life (2, 3). Worldwide, there are 55 million individuals over 60 years old living with some form of dementia, and this number is estimated to nearly triple only in the next 30 years, by 2050 (4). While age is the strongest risk factor for developing cognitive decline, dementia is not an inevitable consequence of aging. Seemingly simple behaviors such as controlling hypertension and diabetes, increasing physical activity (PA), controlling one's weight, decreasing alcohol consumption, nurturing meaningful social connections, among others, can prevent or reduce the chances of progression to dementia by as much as 40% (5–8). Globally, dementia represented an annual global cost above 1.3 trillion dollars in 2019 and an expected increase up to 3 trillion by 2030 (9, 10).
Being physically active can not only delay but also mitigate the effects of cognitive impairment and dementia (5). Exercising regularly can independently revert age-related hippocampal shrinkage, and actually increase its volume by 2%−4.2%, which promotes improvement in spatial memory function (11, 12). Engaging in regular PA practice can reduce the risk of Alzheimer's Disease by 50% (13, 14). The main physiological mechanisms are linked to increased brain perfusion, synaptic neuroplasticity, increased brain volume and connectivity, and the regulation of neurotrophic factors (15–17). It is critical to appreciate that PA is a modifiable lifestyle factor, and there may be many additional reasons why this is a particularly powerful strategy to promote a healthier lifestyle in aging adults: (1) sedentary behavior is a modifiable lifestyle factor, (2) being physically active can improve important aspects of life such as functional independence, psychological wellbeing, and increase health-span (18–20), and (3) increased PA practice is a powerful cost-effective intervention to prevent and treat chronic diseases (21).
Progress Made And Remaining Challenges
Recommending Existing Universal Guidelines for Physical Activity
Numerous organizations have independently endorsed physical activity as a brain-healthy behavior for the aging population (22–26). According to the World Health Organization, a minimum of 150 min of moderate to vigorous activity per week is required for an individual to be considered active (16). Most recently, the PA Guidelines for Americans were updated and mentioned the importance of exercise for brain health and emphasized generally moving more and sitting less (22). Taking more daily steps (up to ~8,000 steps) is associated with a progressively lower risk of all-cause of mortality among adults aged 60 years and older (27).
Most healthcare providers recommend that patients increase PA levels (25, 28–31). However, this approach is unfortunately not particularly effective in helping patients to increase their PA levels over a long-term period (32). These recommendations, including step count prescription, are also associated with important limitations as it usually does not consider the singularities (including values and preferences) and environmental context of each individual. There are also limitations in achieving at least moderate intensity exercise when only step counts or a simple 'move more and sit less' are considered. Older adults spend on average 8.5 h daily on sedentary behaviors (33), and less than a third of adults accurately know and understand the PA recommended guidelines (34–37). Worldwide, approximately one-quarter (one-third in women) of this population is physically inactive, and in some countries, the pandemic increased the proportion of physically inactive up to 80% of the population (38, 39).
Lifestyle Behavior Change Models
Over the last decades, there have been great advances in the science of behavior change. This field has been focused on better understanding the process of behavior change (40). The transtheoretical model (TTM) has been developed focusing on the fact that behavior change is not a discrete task with a beginning middle and end, but a continuous and cyclical process, and is highly dependent on individuals' stage and readiness to change (41). This model can greatly help clinicians as a guide during their conversations about lifestyle change with individuals to gain a better understanding of their specific values, attitudes and needs, and readiness to change, a construct that can be measured with validated instruments (42, 43).
Attempts at appealing to older adults to PA practice have mainly been focused on “selling” the general physical health benefits that one can theoretically gain from becoming physically active. There are several other personal, behavioral, and environmental factors that have been more recently demonstrated to influence exercise adherence in older populations. Social determinants of health have an important impact on one's health, wellbeing, and quality of life (44, 45). Cognitive status and mood can give insights into one's attitudes toward exercise (46). A better understanding of motivation can empower individuals to more successfully pursue their goals (47, 48). The understanding of barriers to exercise and one's self-efficacy is also very important to helping the individuals realize the cyclic nature of behavior change, and anticipate challenges and obstacles (21, 49). Furthermore, self-regulation defined as the planning of how to address barriers can explain exercise engagement (49–51). Finally, a greater understanding surrounding exercise knowledge, tolerance, and preference are critical for setting the correct expectations from the start (52, 53).
Lifestyle interventions that incorporate the concepts discussed above have been successfully employed in helping older adults to promote PA (54), albeit in research settings. In addition, it is relevant to mention motivational interviewing (MI), a patient-centered behavioral approach that focuses on the language associated with behavior change and has been successfully applied to various settings, including increasing PA in older adults (55, 56). However, MI requires specialized training, and time, and may or may not be applicable to most clinical settings. Translation efforts are necessary to develop frameworks that incorporate these theoretical models and adapt them in a way that they can seamlessly be integrated into current workflows of clinical practice.
Thus, to better understand the perspective of the older adult population on PA engagement and adherence and provide supporting data to the proposed perspective, we designed a mixed-method study to explore the main behavioral, biological, social, and environmental factors that affect adherence to regular PA, as well as the PA perception in a sample of sedentary older adults at risk of cognitive decline. Based on this new proposed perspective and results from the mixed-method study, we aim to contrast the current model of PA prescription based mainly on the “universal guidelines,” and the new proposed multidimensional model, which focuses on implementing simple ways to effectively translate current guidelines tailored to the needs of aging individual by screening all listed factors believed to influence adherence and combining all available strategies including health education, evidence-based practice, wellness and lifestyle behavior change models, and behavioral economics and decision-making strategies. We discuss and frame our findings with practical considerations that can hopefully guide clinicians to use the science of behavior change and the concepts to improve their partnerships with their older patients who wish to pursue more active lifestyles.
Brief Methods
In this perspective study, we support our proposed multidimensional model by collecting data from a mixed-method study (1) a descriptive-exploratory analysis of a structured electronic questionnaires battery related to exercise engagement, and (2) a qualitative content analysis of the focus groups. Participants completed a battery of 11 questionnaires related to demographic characteristics and exercise engagement on the Qualtrics platform (Qualtrics, Provo, UT) (Table 1). A total of 65 (67.6 ± 5.9 years, 73% female, 49% brown race, 59% overweighed or obese, 26% high degree, 55% low-to-middle income, 72% retired, 51% hypertension) sedentary older adults (<150 min of moderate or <75 min of vigorous aerobic activity per week) completed the study.
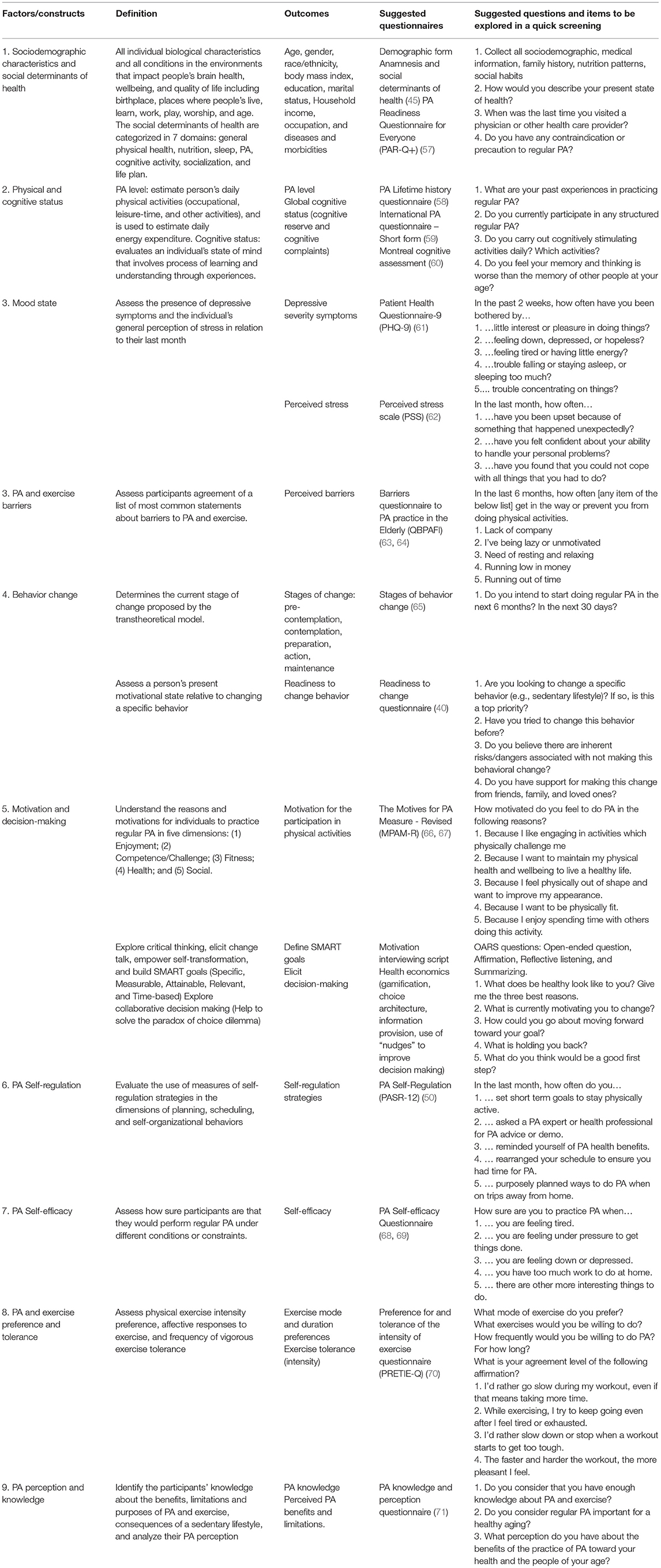
Table 1. Toolkit summary and key components for a quick assessment of physical activity adherence-related factors.
Following, participants were invited to participate in a remote focus group using the Zoom Video platform. A subcohort of 16 participants, divided into two groups, participated in the focus groups. The researcher-moderator followed a pre-established script to guide the group discussion (mean duration of 96 min). The focus groups were recorded in audio and video, transcribed in full, and analyzed independently by three researchers using the content analysis proposed by Bardin (72). All participants provided electronic informed consent, and all procedures were approved by the local institutional ethics committee. Detailed methods are provided as Supplementary Material.
Results
Four major themes and their respective sub-themes emerged from the focus group analysis. We present additional supporting data from the questionnaire's battery, as well as strategies to address the concerns raised, considering the challenges and demands of the clinical setting.
Age and Aging Are Determinants in Physical Activity Practice
Among all sociodemographic and potential social determinants of health assessed, our participants listed their age and the aging process as major determinants of PA adherence. In general, the expression “at our age/my age” was mentioned by nearly all participants. Age appears as a stimulus to PA, as participants recognize the need to remain healthy and active:
...People at our age need to stay active…a lot of things are needed: physical activity, a good nutrition, occupational therapy, reading, a group of friends. That's what will make us an active person… (P8, 63)
In contrast, for some participants, aging can be a limiting factor for performing regular PA. First, more than 60% of participants “feel tired” or “low on energy” frequently or almost every day. Usually, the shared feelings and symptoms (falls, fatigue, muscle soreness, poor sleep quality, feeling down or depressive) are linked to the sedentarism's consequences. Second, this may be due to the limited perception that older adults build about themselves as fragile, a social burden, and because of cultural issues imposed by society (73):
After we retire, then we take a break, we are a little out of breath...The mind works, but the body doesn't follow along, we have to do everything in a moderate pace, with no rush... (P4, 68)
Aging makes it a little difficult because the gym I attend, there are only me and a gentleman at our age, most of them were young. Then, at your age, I think it demotivate. (P9, 69)
Physical Activity and Holistic Health: Healthy Mind, Healthy Body
A large proportion of the participants reported moderate perceived stress (92%) and depressive symptoms (40%). Surprisingly, nine out of 10 participants indicated having knowledge that regular PA can help mitigate the symptoms of depression, anxiety, and stress. Participants also recognized that the lack of regular PA can contribute to the development and worsening of depressive symptoms (74), and that directly affects work-related activities, leisure time, household activities, and getting along with people:
Physical activity is good for the human being...it is good for our body, physically as well as mentally. (P12, 81)
Maintaining both an active mind and autonomy was cited as “extremely important.” Surprisingly, however, older adults did not immediately consider planned exercise as part of being “active,” which was instead more often interpreted as maintaining an active mind, having friends, caring for their home, cognitive tasks, etc:
For me, an active older adult is an individual who knows how to solve problems by himself... who has no difficulty participating in tasks and demands [refers to household and handcraft work], on a daily basis... (P13, 75)
Motivators and Barriers to Physical Activity and Exercise Practice
Although the participants reported that practicing PA was important to them and noted that achieving this goal would represent a challenge for them, it appears that they were unprepared to deal with all aspects of behavior change. Participants mainly focused on the act of starting an exercise program but did not necessarily consider the continued motivation to remain active and develop continued habits of this practice.
With regards to internal stimulus factors, motivation and self-esteem were mentioned as a priority, including the selection of preferred activities targeting health-related issues, such as the prevention or mitigation of diseases and symptoms that affect mental health:
We must have motivation, because when you determine something and focus on what you want, then yes...you have results. (P05, 60)
We have to do what is pleasurable for you, and not just do it for the sake of doing it. What requires you participate in an activity? Enjoyment! (P09, 69)
The external stimulus factor considered most relevant for the participants was related to the social engagement with other older adults, whether it was a group of friends, a partner or family, or the guidance of an exercise professional.
I found a way to do exercise...it's creating a group of friends. One always tries to know how the other is doing and encourages the other to go when he didn't want to, right?…a family that take cares of each other. (P14, 69)
“Being lazy or unmotivated” (65%), and “lack of company” (60%) were the perceived barriers that had the greatest impact on their PA engagement. This finding reveals that older adults fail to invest more effort in an area that they most need to increase their PA levels. Among all five domains (physical, personal, beliefs, motivational, and environmental factors) of perceived barriers to PA, the motivational aspect was the most prominent. Motivation sources were related to maintaining strength and improving physical health and wellbeing. However, despite the desire to improve strength and physical health, 65% of older adults were not motivated to do physically challenging activities. This highlights two interesting findings: (1) lack of broad dissemination of cognitive benefits of being physically active; and (2) a potential opportunity for setting realistic expectations regarding strength and physical improvements (which do require physical challenge).
Participants also demonstrated low self-efficacy and a general lack of self-regulation strategies. Approximately 60%−80% of the participants reported not doing PA or being unsure if they would do it in the following circumstances: “feeling tired or under pressure,” “feeling down,” “too much work at home,” “away from home,” and “no family or friends support.” Additionally, about 70% reported that they never or rarely “rearrange their schedule to ensure they have time to exercise,” or “ask for advice or an exercise demonstration from a health professional expert.” In contrast, 80% of the individuals revealed reminding themselves of exercise health benefits. This indicates that older adults are generally unprepared to deal with the obstacles that are normal and inherent to adopting a lifestyle change (68).
For me, it's laziness, because...we're already tired from work, and still be submitted to walk a lot?! Oh, laziness! [Enthusiastically]. (P10, 65)
…although it is a medical recommendation, it makes me lazy...to do exercise, to follow an exercise routine… (P14, 69)
The most frequent external barriers were financial barriers and those related to the lack of or inadequacy of public places and facilities for the PA practice near home. This highlighted the importance of considering social determinants of health and contextual factors and providing resources that can help to guide individuals through their behavior change journeys (75).
There are many aspects that demotivate people. One aspect is financial. We lack public places to practice physical activities. (P08, 63)
Guidelines and Professional Recommendations
Clinical PA recommendations are general and did not consider older adults' preferences and values, and physical and environmental limitations (76), and this was cited as a major reason why participants did not tend to follow through with current guidelines or general exercise prescriptions. In our sample, 93% reported that had received general information from health care providers to practice PA. However, participants often mentioned their singularities and identified a lack of consideration of their differences as an obstacle to their potential engagement in PA. Thus, recognizing the singularities in each individual can be a powerful strategy for greater PA engagement. Tailored recommendations, improved knowledge and understanding, and self-perception of fitness and overall health is crucial for the correct implementation and engagement in a PA program. For instance, despite the largest majority (90%) considering regular PA important or a requisite for healthy aging, ~15% had no knowledge and 60% of older adults revealed that would like to learn more about PA and exercise:
I understand that the person by himself doesn't have…this knowledge to decide on this. I think…the competent authorities…the doctors, all the scientists, the physical therapists…whoever deals with this area is the one who should make these recommendations because all older adults do not have the same vitality...the same physical condition, so that we couldn't...generalize… (P15, 82)
A Multidimensional Model of Physical Activity Engagement
Taken together, these findings suggest that supporting lifestyle change especially related to PA requires a stronger partnership between the clinicians and patients/clients. In an ideal scenario, clinicians would learn about exercise recommendations, but also how to perform a detailed investigation of an individual's current stage of behavior change, and be proficient in the use of motivational interviewing concepts to elicit change talk toward behavior change and empower self-transformation. All these components benefit clinicians build tailored physical activity guidelines for each patient/client's functional and cognitive capacity, and maximizing exercise-related effects on motor and brain health (77). However, this may not be feasible in many clinical care settings, due to constraints in time, and the need for specialized training. For this reason, in the current manuscript, we suggest a tool kit including a clinical-meaningful script of questions that can guide all health care providers to collect valuable preliminary data about their patients, and help them to partner and build achievable goals, and provide care within the context of each patient and their family. A similar strategy of a multimodal PA education and coaching intervention was shown to be feasible, well-accepted, and effective in promoting PA participation and cognitive improvement in sedentary older adults with memory complaints (54).
Evidence-based practice highlights the importance of the integration of the knowledge and use of the best evidence, the clinical expertise/expert opinion, and respect for patients' desires and values. For instance, approximately one-third of participants revealed “no intention to change their sedentary behavior in the next 6 months,” two-thirds already failed to change their sedentary behavior, and the half sample did not consider changing behavior a high priority. Despite being screened as sedentary, 37% considered themselves physically active, which demonstrates a limitation on knowledge of exercise and PA concepts and clear recommendations. Thus, the clinician's decision making to investigate these factors and foster building a rapport for a better professional-patient relationship is crucial to elicit change talk and consequently initiate preparation for change.
We propose three concrete steps to replace the traditional model of exercise recommendation (Figure 1): (1) a multidimensional model of PA engagement, (2) a comprehensive tool kit for clinicians to assess PA adherence-related factors, and (3) a list of items and questions designed to summarize the main components for a quick assessment of PA adherence-related factors (Table 1). Importantly, frequent follow-up assessments and referrals when needed will also be crucial to minimizing relapses.
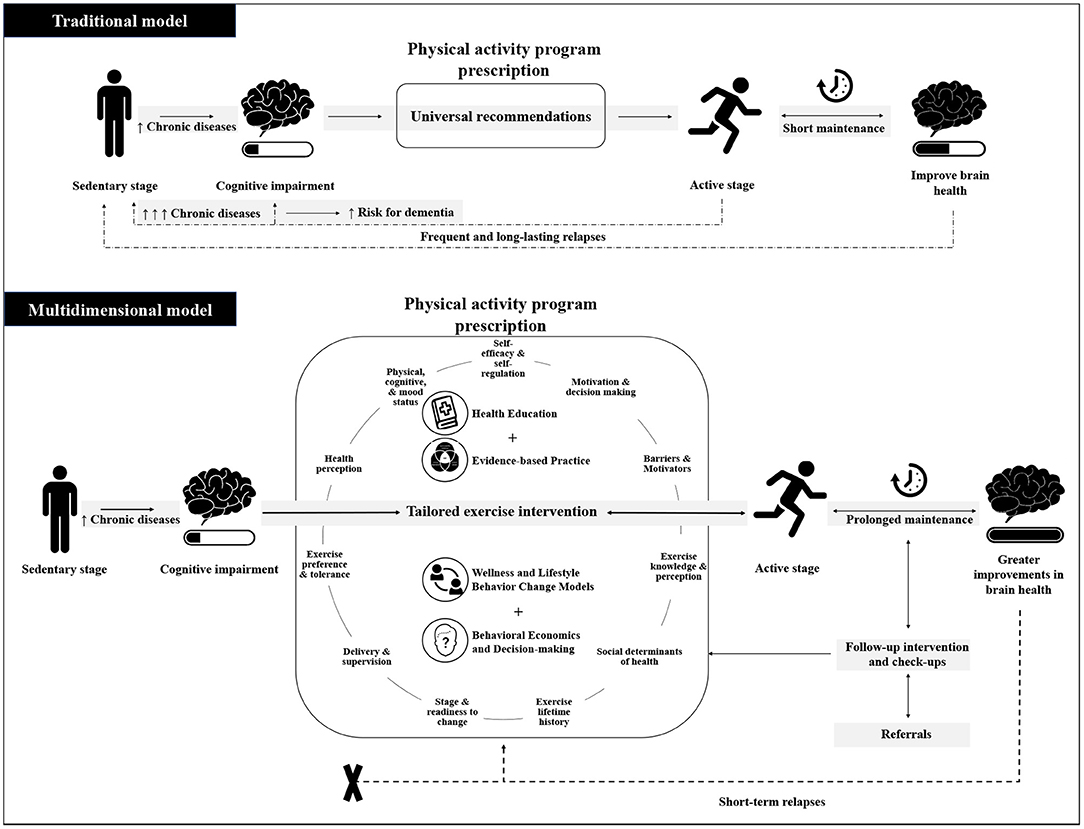
Figure 1. Schematic illustration of traditional model vs. multidimensional model. The traditional model emphasizes universal physical activity recommendations as the main component of an exercise program. The multidimensional model focus on implementing simple ways to effectively translate current guidelines tailored to the needs of the aging individual by screening all listed factors believed to influence adherence and combining all available strategies including health education, evidence-based practice, wellness and lifestyle behavior change models, and behavioral economics and decision-making strategies. The successful assessment and intervention prescription will affect expected prolonged maintenance in a physically active stage and greater improvements in brain health.
Toolkit and a Screening Questionnaire for Clinicians: What Do They Need to Assess?
In Table 1, we propose a list of instruments, questionnaires, and behavior change models that are crucial for clinicians to have a comprehensive understanding and assessment of their patients before prescribing a PA program (Table 1), including specific questions that should be explored by clinicians for a quick screening participant's profile. This screening will also help direct the interview with active listening, build rapport with the patient/client, and gather all necessary information before listing goals and interventions in partnership with the individual.
Future studies will implement the proposed screening targeting older adults at risk for cognitive decline aiming at evaluating validity, reliability, and responsiveness to a multimodal intervention targeting long-term PA participation.
Conclusion
Our findings suggested four main themes linked to PA adherence in sedentary older adults. First, older adults believe that aging is a limiting factor for PA engagement. Second, maintaining both an active mind and autonomy are priorities, but older adults did not immediately consider planned exercise as part of being “active,” which was instead more often interpreted as maintaining an active mind, having friends, caring for their home, etc. Third, motivational challenges in PA engagement were noted. And fourth, clinical PA recommendations were general and did not consider their physical and contextual limitations, and thus, they do not tend to follow through with them. We presented a multidimensional model of PA adherence to maximize brain health in older adults and suggest a tool kit and key questions to effectively screen sedentary aging adults and translate current guidelines into the needs of the individual by using behavior change strategies.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Alagoas State University of Health Science institutional Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
DC: study concept, design, data collection, data analysis, data interpretation, and manuscript preparation, writing, editing, and submission. VS: data collection, data processing, data interpretation, and manuscript editing and review. MS, GL, and AM: data collection, data interpretation, and manuscript review. LC and AP-L: critical revision of manuscript for intellectual content. AB: study design, data analysis, and manuscript editing. AO and JG-O: study concept, design, supervisor of study, manuscript writing and editing, and critical revision of manuscript for intellectual content. All authors contributed to the article and approved the submitted version.
Funding
AO, GL, and AM were supported by the National Council for Scientific and Technological Development and Alagoas State University of Health Science (Brazil).
Conflict of Interest
JG-O works as Director of Interventional Therapy at Linus Health and AP-L is a co-founder of Linus Health and TI Solutions AG.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to acknowledge the contributions of the members of Research Group on Human Aging of the Alagoas State University of Health Sciences: Adélia Sampaio, Bruna Pereira, Camila Mayara, Emanuelle Rocha, Lucas Lisboa, and Rayane Claudino.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2022.923221/full#supplementary-material
References
1. United Nations, Department of Economic and Social Affairs PD. World Population Aging 2020 Highlights: Living arrangements of older persons. New York, NY: United Nations (2021). doi: 10.18356/9789210051934
2. Murman D. The impact of age on cognition. Semin Hear. (2015) 36:111–21. doi: 10.1055/s-0035-1555115
3. National Institute on Aging World Health Organization. Global Health and Aging. NIH. Geneva: NIH Publication; World Health Organization (2011).
4. World Health Organization. Risk Reduction of Cognitive Decline and Dementia: WHO Guidelines. Geneva: World Health Organization (2019). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK542796/
5. Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet. (2020) 396:413–46. doi: 10.1016/S0140-6736(20)30367-6
6. Liang JH, Lu L, Li JY, Qu XY, Li J, Qian S, et al. Contributions of modifiable risk factors to dementia incidence: a Bayesian network analysis. J Am Med Dir Assoc. (2020) 21:1592–9.e13. doi: 10.1016/j.jamda.2020.04.006
7. Dhana K, Evans DA, Rajan KB, Bennett DA, Morris MC. Healthy lifestyle and the risk of Alzheimer's dementia: findings from 2 longitudinal studies. Neurology. (2020) 95:E374–83. doi: 10.1212/WNL.0000000000009816
8. Yu JT, Xu W, Tan CC, Andrieu S, Suckling J, Evangelou E, et al. Evidence-based prevention of Alzheimer's disease: systematic review and meta-analysis of 243 observational prospective studies and 153 randomized controlled trials. J Neurol Neurosurg Psychiatry. (2020) 91:1201–9. doi: 10.1136/jnnp-2019-321913
9. World Health Organization. Global Status Report on the Public Health Response to Dementia: Executive Summary. Geneva: World Health Organization (2021).
10. Alzheimer's Disease International. World Alzheimer's Report 2019: Attitudes to Dementia. London: Alzheimer's Disease International (2019).
11. Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci USA. (2011) 108:3017–22. doi: 10.1073/pnas.1015950108
12. Niemann C, Godde B, Voelcker-Rehage C. Not only cardiovascular, but also coordinative exercise increases hippocampal volume in older adults. Front Aging Neurosci. (2014) 6:1–24. doi: 10.3389/fnagi.2014.00170
13. De la Rosa A, Olaso-Gonzalez G, Arc-Chagnaud C, Millan F, Salvador-Pascual A, García-Lucerga C, et al. Physical exercise in the prevention and treatment of Alzheimer's disease. J Sport Health Sci. (2020) 9:394–404. doi: 10.1016/j.jshs.2020.01.004
14. Beckett MW, Ardern CI, Rotondi MA. A meta-analysis of prospective studies on the role of physical activity and the prevention of Alzheimer's disease in older adults. BMC Geriatr. (2015) 15:9. doi: 10.1186/s12877-015-0007-2
15. Cabral DF, Rice J, Morris TP, Rundek T, Pascual-Leone A, Gomes-Osman J. Exercise for brain health: an investigation into the underlying mechanisms guided by dose. Neurotherapeutics. (2019) 16:580–99. doi: 10.1007/s13311-019-00749-w
16. Gligoroska JP, Manchevska S. The effect of physical activity on cognition – physiological mechanisms. Mater Socio Med. (2012) 24:198. doi: 10.5455/msm.2012.24.198-202
17. Mandolesi L, Polverino A, Montuori S, Foti F, Ferraioli G, Sorrentino P, et al. Effects of physical exercise on cognitive functioning and wellbeing: biological and psychological benefits. Front Psychol. (2018) 9:509. doi: 10.3389/fpsyg.2018.00509
18. Blazer DG, Yaffe K, Liverman CT. Cognitive aging: Progress in Understanding and Opportunities for Action. Washington, DC: National Academies Press (2015). p. 1–330. doi: 10.17226/21693
19. Holm AL, Severinsson E. A qualitative systematic review of older persons' perceptions of health, ill health, and their community health care needs. Nurs Res Pract. (2013) 2013:1–12. doi: 10.1155/2013/672702
20. Strout K, Ahmed F, Sporer K, Howard EP, Sassatelli E, Mcfadden K. What are older adults wellness priorities? A qualitative analysis of priorities within multiple domains of wellness. Healthy Aging Res. (2018) 7:e21. doi: 10.1097/HXR.0000000000000021
21. Groessl EJ, Kaplan RM, Castro Sweet CM, Church T, Espeland MA, Gill TM, et al. Cost-effectiveness of the LIFE physical activity intervention for older adults at increased risk for mobility disability. J Gerontol A Biol Sci Med Sci. (2016) 71:656–62. doi: 10.1093/gerona/glw001
22. Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. (2018) 320:2020–8. doi: 10.1001/jama.2018.14854
23. Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behavior. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
24. Ministry of Health of Brazil. Physical Activity Guidelines for the Brazilian Population. (2021). Available online at: http://bvsms.saude.gov.br/bvs/publicacoes/guia_atividade_fisica_populacao_brasileira.pdf (accessed April 15, 2022).
25. Lobelo F, Stoutenberg M, Hutber A. The exercise is medicine global health initiative: a 2014 update. Br J Sports Med. (2014) 48:1627–33. doi: 10.1136/bjsports-2013-093080
26. Blazer DG, Yaffe K, Karlawish J. Cognitive aging: a report from the institute of medicine. JAMA. (2015) 313:2121–2. doi: 10.1001/jama.2015.4380
27. Paluch AE, Bajpai S, Bassett DR, Carnethon MR, Ekelund U, Evenson KR, et al. Daily steps and all-cause mortality: a meta-analysis of 15 international cohorts. Lancet Public Health. (2022) 7:e219–28. doi: 10.1016/S2468-2667(21)00302-9
28. ISPAH International Society for Physical Activity and Health. The Bangkok declaration on physical activity for global health and sustainable development. Br J Sports Med. (2017) 51:1389–91. doi: 10.1136/bjsports-2017-098063
29. Institute of Medicine of the National Academics. Cognitive aging: progress in understanding and opportunities for action. Mil Med. (2015) 180:1111–3. doi: 10.7205/MILMED-D-15-00292
30. World Health Organization. Global action plan for the prevention and control of non-communicable diseases 2013–2020. Societies. Geneva: WHO Press (2013).
31. U.S. National Academy of Medicine. Healthy Longevity Global Grand Challenge. Available online at: https://nam.edu/initiatives/grand-challenge-healthy-longevity/ (accessed February 1, 2020).
32. Wanigatunga AA, Tudor-Locke C, Axtell RS, Glynn NW, King AC, McDermott MM, et al. Effects of a long-term physical activity program on activity patterns in older adults. Med Sci Sports Exerc. (2017) 49:2167–75. doi: 10.1249/MSS.0000000000001340
33. Harvey JA, Chastin SFM, Skelton DA. Prevalence of sedentary behavior in older adults: a systematic review. Int J Environ Res Public. (2013) 10:6645–61. doi: 10.3390/ijerph10126645
34. Knox ECL, Musson H, Adams EJ. Knowledge of physical activity recommendations in adults employed in england: associations with individual and workplace-related predictors. Int J Behav Nutr Phys Act. (2015) 12:1–8. doi: 10.1186/s12966-015-0231-3
35. Kay MC, Carroll DD, Carlson SA, Fulton JE. Awareness and knowledge of the 2008 physical activity guidelines for Americans. J Phys Act Health. (2014) 11:693–8. doi: 10.1123/jpah.2012-0171
36. Vaara JP, Vasankari T, Koski HJ, Kyröläinen H. Awareness and knowledge of physical activity recommendations in young adult men. Front Public Health. (2019) 7:310. doi: 10.3389/fpubh.2019.00310
37. Fredriksson SV, Alley SJ, Rebar AL, Hayman M, Vandelanotte C, Schoeppe S. How are different levels of knowledge about physical activity associated with physical activity behavior in Australian adults? PLoS ONE. (2018) 13:e0207003. doi: 10.1371/journal.pone.0207003
38. Guthold R, Stevens GA, Riley LM, Bull FC. Articles Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. (2018) 6:e1077–86. doi: 10.1016/S2214-109X(18)30357-7
39. Amini H, Habibi S, Islamoglu AH, Isanejad E, Uz C, Daniyari H. COVID-19 pandemic-induced physical inactivity: the necessity of updating the global action plan on physical activity 2018–2030. Environ Health Prev Med. (2021) 26:1–3. doi: 10.1186/s12199-021-00955-z
40. American Council on Exercise. The Professional's Guide to Health and Wellness Coaching. San Diego, CA: ACE (2019).
41. Gourlan M, Bernard P, Bortolon C, Romain AJ, Lareyre O, Carayol M, et al. Efficacy of theory-based interventions to promote physical activity. A meta-analysis of randomized controlled trials. Health Psychol Rev. (2016) 10:50–66. doi: 10.1080/17437199.2014.981777
42. Dumith SC, Gigante DP, Domingues MR. Stages of change for physical activity in adults from Southern Brazil: a population-based survey. Int J Behav Nutr Phys Act. (2007) 4:25. doi: 10.1186/1479-5868-4-25
43. Gonzalez-Ramirez LP, De La Roca-Chiapas JM, Colunga-Rodriguez C, Preciado-Serrano MDL, Daneri-Navarro A, Pedroza-Cabrera FJ, et al. Validation of health behavior and stages of change questionnaire. Breast Cancer. (2017) 9:199. doi: 10.2147/BCTT.S129855
44. Mattos MK, Burke LE, Baernholdt M, Hu L, Nilsen ML, Lingler JH. Perceived social determinants of health among older, rural-dwelling adults with early-stage cognitive impairment. Dementia. (2019) 18:920–35. doi: 10.1177/1471301217694250
45. Cattaneo G, Bartrés-Faz D, Morris TP, Sánchez JS, Macià D, Tarrero C, et al. The Barcelona brain health initiative: a cohort study to define and promote determinants of brain health. Front Aging Neurosci. (2018) 10:321. doi: 10.3389/fnagi.2018.00321
46. Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B. Physical activity and depression: toward understanding the antidepressant mechanisms of physical activity. Neurosci Biobehav Rev. (2019) 107:525–39. doi: 10.1016/j.neubiorev.2019.09.040
47. Stathi A, Withall J, Thompson JL, Davis MG, Gray S, De Koning J, et al. Feasibility trial evaluation of a peer volunteering active aging intervention: ACE (Active, Connected, Engaged). Gerontologist. (2020) 60:571–82. doi: 10.1093/geront/gnz003
48. O'Neil-Pirozzi TM, Cattaneo G, Solana-Sánchez J, Gomes-Osman J, Pascual-Leone A. The importance of motivation to older adult physical and cognitive exercise program development, initiation, and adherence. Front Aging. (2022) 3:773944. doi: 10.3389/fragi.2022.773944
49. Olson EA, McAuley E, Olson EA. Impact of a brief intervention on self-regulation, self-efficacy and physical activity in older adults with type 2 diabetes HHS public access. J Behav Med. (2015) 38:886–98. doi: 10.1007/s10865-015-9660-3
50. Umstattd MR, Motl R, Wilcox S, Saunders R, Watford M. Measuring physical activity self-regulation strategies in older adults. J Phys Act Health. (2009) 6(s1):S105–12. doi: 10.1123/jpah.6.s1.s105
51. Rhodes RE, Pfaeffli LA. Mediators of physical activity behavior change among adult non-clinical populations: a review update. Int J Behav Nutr Phys Act. (2010) 7:37. doi: 10.1186/1479-5868-7-37
52. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. (2011) 43:1334–59. doi: 10.1249/MSS.0b013e318213fefb
53. Parfitt G, Alrumh A, Rowlands AV. Affect-regulated exercise intensity: does training at an intensity that feels ‘good’ improve physical health? J Sci Med Sport. (2012) 15:548–53. doi: 10.1016/j.jsams.2012.01.005
54. Cabral DF, Santos VS, Pereira OTT, Silva MJ, Pascual-Leone A, Rundek T, et al. Feasibility and preliminary efficacy of a multimodal approach to increase physical activity in older adults with memory complaints: the education for action study. J Aging Phys Act. (2021) 30:1–13. doi: 10.1123/japa.2020-0484
55. Miller W, Rollnick S. Motivational Interviewing: Preparing People to Change. New York, NY: Guilford Press. (2013).
56. Stewart EE, Fox C. Encouraging Patients to Change Unhealthy Behaviors with Motivational Interviewing. Family Practice Management. (2011). Available online at: www.aafp.org/fpm (accessed November 5, 2020).
57. Warburton DER, Jamnik VK, Bredin SSD, Gledhill N. The physical activity readiness questionnaire for everyone (PAR-Q+) and electronic physical activity readiness medical examination (ePARmed-X+). Health Fitness J Canada. (2011) 4:3–17. doi: 10.14288/HFJC.V4I2.103
58. Chasan-Taber L, Erickson JB, McBride JW, Nasca PC, Chasan-Taber S, Freedson PS. Reproducibility of a self-administered lifetime physical activity questionnaire among female college alumnae. Am J Epidemiol. (2002) 155:282–9. doi: 10.1093/aje/155.3.282
59. Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-Country reliability and validity. Med Sci Sports Exerc. (2003) 35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB
60. Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. (2005) 53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x
61. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
62. Chan SF, La Greca AM. Perceived stress scale (PSS). In: Encyclopedia of Behavioral Medicine. New York, NY: Springer New York (2013). p. 1454–5. doi: 10.1007/978-1-4419-1005-9_773
63. Hirayama M. [Physical Activity and Parkinson's Disease: Behavior Change, Self-Efficacy and Perceived Barriers]. Aleph. Rio Claro: Universidade Estadual Paulista (2006).
64. Booth ML, Owen N, Bauman A, Clavisi O, Leslie E. Social-cognitive and perceived environment influences associated with physical activity in older Australians. Prev Med. (2000) 31:15–22. doi: 10.1006/pmed.2000.0661
65. Dumith S de C, Domingues MR, Gigante DP. [Stages of change toward physical activity: a review of literature]. Rev Bras de Cineantropometriae Desempenho Hum. (2008) 10:301–7. doi: 10.5007/1980-0037.2008v10n3p301
66. Ryan RM, Frederick CM, Lepes D, Rubio N, Sheldon KM. Intrinsic motivation and exercise adherence. Int J Sport Psychol. (1997) 335–54.
67. Albuquerque MR, Lopes MC, de Paula JJ, Faria LO, Pereira ET, da Costa VT. Cross-cultural adaptation and validation of the MPAM-R to Brazilian Portuguese and proposal of a new method to calculate factor scores. Front Psychol. (2017) 8:1–9. doi: 10.3389/fpsyg.2017.00261
68. Neupert SD, Lachman ME, Whitbourne SB. Exercise self-efficacy and control beliefs: effects on exercise behavior after an exercise intervention for older adults. J Aging Phys Act. (2009) 17:1–16. doi: 10.1123/japa.17.1.1
69. Borges RA, Rech CR, Meurer ST, Benedetti TRB. [Validity and reliability of a scale to assess self-efficacy for physical activity in elderly]. Cad Saude Publica. (2015) 31:701–8. doi: 10.1590/0102-311X00081414
70. Smirmaul BPC, Ekkekakis P, Teixeira IP, Nakamura PM, Kokubun E. Preference for and tolerance of the intensity of exercise questionnaire: Brazilian portuguese version. Rev Bras de Cineantropometriae Desempenho Hum. (2015) 17:550–64. doi: 10.5007/1980-0037.2015v17n5p550
71. Domingues MR, Araújo CLP. [Knowledge and perceptions of physical exercise in an adult urban population in Southern Brazil]. Cad Saude Publica. (2004) 20:204–15. doi: 10.1590/S0102-311X2004000100037
73. Richeson JA, Shelton JN. A social psychological perspective on the stigmatization of older adults. In: Carstensen LL, Hartel CR, editors. National Research Council (US) Committee on Aging Frontiers in Social Psychology, Personality, and Adult Developmental Psychology; When I'm 64. Washington, DC: National Academies Press (US) (2006). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK83758/
74. Maynou L, Hernández-Pizarro HM, Errea Rodríguez M. The association of physical (in)Activity with Mental Health. Differences between elder and younger populations: a systematic literature review. Int J Environ Res Pub Health. (2021) 18:4771. doi: 10.3390/ijerph18094771
75. Short SE, Mollborn S. Social determinants and health behaviors: conceptual frames and empirical advances. Curr Opin Psychol. (2015) 5:78. doi: 10.1016/j.copsyc.2015.05.002
76. Bethancourt HJ, Rosenberg DE, Beatty T, Arterburn DE. Barriers to and facilitators of physical activity program use among older adults. Clin Med Res. (2014) 12:10–20. doi: 10.3121/cmr.2013.1171
Keywords: exercise engagement, physical activity, sedentary behavior, exercise guidelines, lifestyle behavior, behavior change, cognitive decline, brain health
Citation: Cabral DF, Santos VS, Silva MJG, Leite GF, Mesquita APB, Pascual-Leone A, Cahalin LP, Batiston AP, Oliveira ACA and Gomes-Osman J (2022) Recommending Physical Activity to Your Aging Patients? What Clinicians Need to Know to Increase Adherence From the Older Adult Perspective. Front. Rehabilit. Sci. 3:923221. doi: 10.3389/fresc.2022.923221
Received: 19 April 2022; Accepted: 17 June 2022;
Published: 08 July 2022.
Edited by:
Javier Güeita-Rodriguez, Rey Juan Carlos University, SpainReviewed by:
Ladislav Batalik, University Hospital Brno, CzechiaGaryfallia Pepera, University of Thessaly, Lamia, Greece
Copyright © 2022 Cabral, Santos, Silva, Leite, Mesquita, Pascual-Leone, Cahalin, Batiston, Oliveira and Gomes-Osman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joyce Gomes-Osman, amdvbWVzQGxpbnVzLmhlYWx0aA==
†These authors have contributed equally to this work and share last authorship
 Danylo F. Cabral
Danylo F. Cabral Vinicius S. Santos
Vinicius S. Santos Maria Jasmine G. Silva
Maria Jasmine G. Silva Gabriela F. Leite
Gabriela F. Leite Ana Paula B. Mesquita
Ana Paula B. Mesquita Alvaro Pascual-Leone
Alvaro Pascual-Leone Lawrence P. Cahalin
Lawrence P. Cahalin Adriane P. Batiston
Adriane P. Batiston Augusto C. A. Oliveira
Augusto C. A. Oliveira Joyce Gomes-Osman
Joyce Gomes-Osman