- 1Dean's Office, University of Alabama at Birmingham, Birmingham, AL, United States
- 2University of Alabama at Birmingham-Lakeshore Foundation Research Collaborative, Birmingham, AL, United States
- 3Department of Physical Medicine and Rehabilitation, University of Alabama at Birmingham, Birmingham, AL, United States
- 4Division of Pediatric Rehabilitation Medicine, Department of Pediatrics, University of Alabama at Birmingham, Birmingham, AL, United States
- 5Physical and Occupational Therapy Department, Rehabilitation Science Program, University of Alabama at Birmingham, Birmingham, AL, United States
People with spinal cord injury (SCI) experience a plethora of health conditions that hinder their health and wellness. This qualitative retrospective evaluation describes the perceptions of 14 peoples with SCI, several months after they completed an eight-week telewellness community program (MENTOR—Mindfulness, Exercise and Nutrition To Optimize Resilience). The program offered daily online classes that covered three core wellness domains (mindfulness, exercise, nutrition) and one health coaching session to introduce participants to eight other wellness domains (sleep, self-care, core values, arts & leisure, outdoor time in nature; spiritual practice, relationships, contribution to others). Qualitative analysis resulted in 4 themes related to program benefits, likes, and improvement recommendations. First, participants valued the program for the social support provided by a sense of community and relationship building with peers. Second, self-regulation was facilitated by the comprehensiveness of the program components, easy online access, and shared lifestyle goals for self-improvement among peers. Third, participants reported improved psychological wellbeing and adopted healthy behaviors that were maintained long after the program. Last, future programs should include flexible class times, post-program support, specific exercise adaptations for people with limited arm function, and supplementary in-person meetings. These preliminary findings demonstrate that MENTOR may benefit the wellbeing of people with SCI and warrant further study.
Introduction
The connection between healthcare and wellness is typically not available in conventional healthcare systems in the United States and most other parts of the world (1). With reference to the U.S., we have yet to address the societal responsibilities and barriers that prevent individuals with spinal cord injury (SCI) from leading healthy, active lives. Simply put, we have not achieved health equity. Working-age adults with SCI visit their healthcare provider and the emergency department more frequently than people without disability (2), and individuals with SCI—both recently acquired and existing for many years—are seldom exposed to wellness programs that focus on improving their quality of life and helping them prevent or manage physical and psychosocial secondary health conditions (1). The secondary conditions associated with disability, overlapping the natural course of aging, can bring an onset of new medical issues across an individual's lifespan (3–6).
Unhealthy behaviors such as a poor diet and lack of exercise can predispose people with SCI to even greater levels of adverse health consequences when they overlay such secondary conditions as pain (neuropathic and musculoskeletal) (7, 8), excess weight gain (i.e., obesity) (9–12), and deconditioning (i.e., extremely low fitness levels and high levels of sedentary behavior) (13–15). These health conditions have a profound negative impact on health and function and in the aggregate, can impose substantial limitations in rates of participation in general life activities including employment, social and community engagement and performing instrumental activities of daily living.
Expertise, support, and resources to address specific health issues or measures to prevent them are difficult to find, particularly in key areas of integrative wellness that include exercise, nutrition, mindfulness, sleep, and other less known, but important health-enhancing behaviors (16, 17). This may leave many people with SCI underprepared to return to their community and self-manage their health. The lack of continuity between the completion of rehabilitation and the initiation of wellness is clearly not helping the situation (18).
Physicians may not feel comfortable addressing certain physical or cognitive conditions associated with the disability (19), which adds to the challenge of patients with disability moving beyond medical care into self-managed wellness (3). Studies demonstrate that people with SCI experience issues with depression, anxiety, post-traumatic stress disorder, life-satisfaction, and overall quality of life (20).
People with SCI are also at increased risk for developing chronic health conditions at a much higher rate than the general population, including heart disease, obesity, and type 2 diabetes (21). These conditions may result from a lack of poor access to wellness programs that include physical activity, nutritional instruction and mind-based stress reduction (22). For these reasons, identifying and/or developing effective models for preventing and treating secondary conditions in people with SCI continues to be an important priority (23).
There is a growing body of evidence that convincingly supports the effectiveness and superiority of non-invasive wellness interventions that are consistent with contemporary lifestyle medicine in the promotion of lifelong health and wellness (16, 24). Understanding how to expand the continuum of healthcare services into the domains of wellness to allow individuals with SCI to self-manage their health and maintain adequate resilience continues to be a strong need in SCI research (5, 25–27). The SCI literature is starting to recognize the importance of resilience (20, 28, 29), which refers to the person's ability to understand, cope, adapt and strive for a positive balance between gains and losses in health and function across their lifespan.
The MENTOR program (Mindfulness, Exercise, and Nutrition To Optimize Resilience) has been offered to people with SCI and other physical disabilities across the U.S. for the past year. MENTOR is a community project (i.e., not a clinical trial) funded by the Center for Disease Control and Prevention. The purpose of this retrospective evaluation was to examine the perceptions of a subset of people with SCI who completed MENTOR, with a specific focus on program benefits and likes and dislikes related to the implementation of the program, with the intent to use these findings to refine the next iteration of MENTOR.
Methods
Design
This was a retrospective, qualitative program evaluation to understand the end users' perspective from which to make future modifications to the program. The philosophical assumptions that underpinned all phases of the research were critical realism ontological perspective (i.e., reality is multiple and subjective) and an interpretivism epistemological perspective (i.e., knowledge is socially constructed by both the participant and researcher). Put simply, the research time acknowledged that bias from participants and the team is unavoidable and should be considered throughout the study. Participants experienced different perspectives of the program, and recollections of the program could be heavily influenced by the interaction between the interviewer and analysts, as well as the presentation of the results. The team agreed upon the philosophical assumptions and aimed to incorporate only a minimal level of bias/interpretivism when conducting all aspects of the project.
MENTOR Program
The MENTOR program is an 8-week, 40-h online telewellness program created for people with SCI and other physical disabilities with the aim to provide wellness support. The program consists of 11 evidence-based wellness domains that have been proven effective for improving health (16, 30). These include exercise, diet, sleep, self-care, mindfulness, core values, arts & leisure, outdoor time in nature; spiritual practice, relationships, contribution to others. The exercise, nutrition and mindfulness classes are considered the core domains because they are offered weekly as hands-on sessions taught by qualified specialists in these respective fields. The remaining wellness domains are offered in a 1-h session, once per week, across the 8-week program. Further details of the program can be found elsewhere (31).
MENTOR Core Wellness Domains
Exercise
The exercises classes were offered 2 days a week (Tuesday/Thursday) for 1 h each day, and each class was split into 30min of exercise form and safety, followed by 30min of performing the exercise. The fitness activities were adapted based on the participants' functional level. Participants with SCI performed the exercise routines from a seated position.
Nutrition
The nutrition classes were taught once a week (Wednesday) by a registered dietitian and focused on preparing meals, learning new recipes that focused on increasing fruit and vegetable consumption, and budgeting groceries to include healthier options and reduce processed foods. All the recommended foods were approved by the Women and Infants/Children (WIC) and Supplemental Nutrition Assistance Program (SNAP) U.S. federal assistance programs.
Mindfulness
The mindfulness classes were taught once a week (Monday) by a trained instructor who emphasized various aspects of traditional mindfulness techniques that included comfortable positioning techniques for those in a wheelchair, proper breathing control, and strategies to combat negative feelings or psychological issues.
MENTOR Wellness Sub-domains
The eight sub-domains included self-care skills, core values, outdoor time in nature, sleep, contribution to others, arts and leisure, relationships, and spiritual practice. Participants practiced these domains once a week (Friday) with their assigned groups and trained health coaches, who emphasized the “high level pointers” for improving each of these domains. For example, under sleep, various suggestions were provided based on the sleep literature to improve sleep hygiene. These included use of a white or pink noise machine, maintaining an ideal room temperature (64–66 degrees), using a weighted blanket, increasing room darkness, avoiding blue light from cell phones, going to bed and waking up at a regular time, along with several other suggestions. These sessions were meant to help participants understand how to self-manage their health within these domains, and independently seek and utilize resources to improve any wellness domain that they were having difficulty with or wanting to learn more about its potential benefit for improving their health.
Recruitment/Eligibility
This study aimed to recruit a convenience sample of 20 participants or recruit participants until surface-level themes were saturated (i.e., themes that appropriately and adequately address the research questions) (32). Participants with SCI who completed the MENTOR program were recruited for this study. Eligibility criteria included: (1)18–70 years of age; (2) internet access; and (3) ability to access the program materials independently.
Procedures
The entire MENTOR program was conducted remotely and included no in-person interactions. Participants were arranged in groups of 6–10 participants. The program was offered in waves, and 2 weeks prior to the start of each wave, the participant coordinator recontacted participants to confirm their interest and to provide details on their schedules, equipment, etc. Weekly check-ins were conducted with participants as reminders for upcoming classes for the week and what materials they should read or complete (i.e., a worksheet on a certain wellness domain) prior to the session. If a participant did not show up for class and did not notify their health coach in advance, he/she was called to make sure everything was ok and to document the reason for missing the class. Participants were asked to attend all of the classes through Zoom videoconference software. They were able to interact or contact their health coach or instructors prior to or after the class if they had any questions or a specific issue. They were sent a small set of inexpensive exercise equipment (e.g., hand weights, elastic bands) that was shipped to their home prior to the start of the program. They were also sent a MENTOR journal and were asked to record various activities that they did during the week that related to one or more wellness domains.
At the beginning of the program, participants were provided with program logistics, and were introduced to MENTOR's web-based commercial platform (Healthie). Because the program was completely online, there was a telelogistics support protocol in place. MENTOR components, such as online enrollment, assessment, and implementation were managed by a telelogistics support team. This was made up of four program staff and six health coaches. The local institutional reviewer board of the University granted a research exemption for this study designating it as a quality improvement evaluation study of an existing program.
Several months after completing MENTOR, participants were contacted via telephone to participate in a program evaluation interview. The interview lasted no longer than 30 min and included ~10 questions. The questions were semi-structured and asked participants about their overall thoughts of the program, likes/dislikes, potential benefits, and general questions pertaining to the 3 core components of the program (exercise, mindfulness, and nutrition). The questions also included a general ice-breaker question (asking about what the participant likes to do in their free time), and a question asking what recommendations they would have for improving the program. The interviews were conducted by three research staff who had several years of experience in wellness-related fields for people with disabilities. None of the interviewers were involved with the delivery of MENTOR. The interviewers were instructed to ask follow-up questions to clarify and expand on noteworthy topics that participants reported. Interviews were audio recorded and transcribed by a 3rd party transcription company. Participants were thanked with a $20 electronic debit card for completing the interview.
Analysis
Inductive thematic analysis (33) was used to analyze qualitative data. First, the research team transcribed and crosschecked the data for accuracy while reading the transcriptions. Next, two analysts generated initial codes that were written in the text to resemble their interpretations of short data segments. Codes were generated iteratively across each transcription. After initial coding, analysts independently searched their codes for patterns and, from these patterns, generated an initial list of sub-themes based upon internal and external homogeneity (34). The analysts then met to compare and merge their sub-themes into a single list. Sub-themes were then placed into higher-arching categories (i.e., themes). The themes were then reviewed to ensure that they adequately represented sub-themes, and that sub-themes represented codes. Analysts kept their lists of sub-themes and codes to act as an audit trail. In consideration of the small sample size of the study, the narrow aims, and the strong dialogue by interviewees, the coders aimed to generate a small number of rich themes and sub-themes to enhance the likelihood that the themes achieve informed power (35).
Results
Interviews were stopped upon interviewing a total of 14 people, because the analysts determined that the surface-level themes achieved informed power. The mean age of the sample was 50 ± 16 years and there were 6 males (42.9%) and 8 (57.1%) females. Regarding race, 6 self-identified as Caucasian; 5 African American, 1 American Indian/Alaskan Native, and 2 were Unknown. Participants were from several different cities across the U.S including Birmingham, AL, Boston, MA, Chicago IL, Denver, CO, and New York, New York.
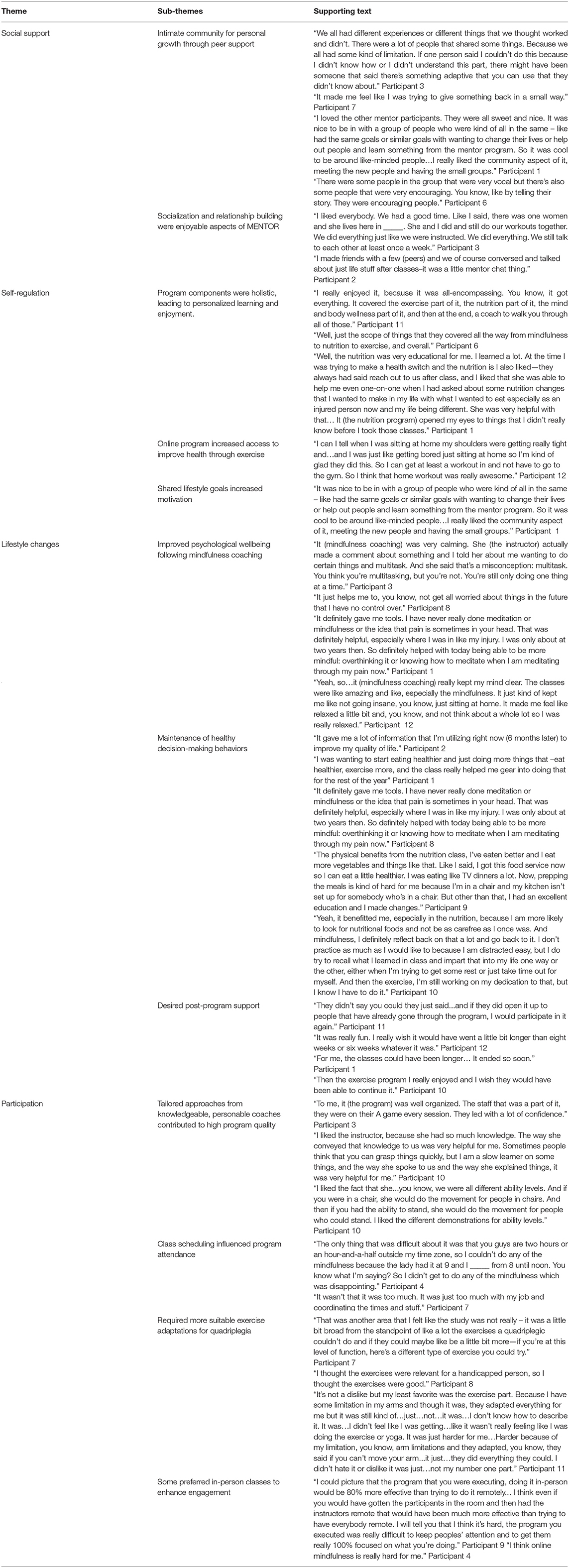
Themes
The resultant themes incorporated rich participant feedback related to social support, self-regulation motivational factors, lifestyle changes, and factors that affected participation. These themes are described below and presented with their supporting sub-themes and codes in Table 1.
Social support was an enjoyable component of MENTOR. Participants reported that the group-based classes provided a valuably intimate sense of community with other members. Value was created by either receiving or providing verbal support. Examples of these interactions included recommending adaptations for various activities or overcoming other physical or emotional life challenges. Small groups fostered in-depth communication and relationship building, which led to some participants creating peer friendships and bonds outside of the class after the program ended. Groups were balanced by participants who were vocal and others who were less conversive.
Self-regulation motivational factors were attributed to the holistic nature of the program, the accessible online platform, and shared lifestyle goals. The program offered a variety of opportunities for participants to self-select classes or certain components that they felt best fit their personal needs. Some participants found themselves enjoying and attending all the classes across the 8-week program, which was a substantial time investment (5 hr/week for 8 weeks). Some participants reported that nutrition was the most helpful toward improving their lifestyle, while others reported that the mindfulness component was most beneficial. Since MENTOR was provided through an online platform, participants appreciated that the classes could be conveniently attended without requiring transportation to an onsite facility. Moreover, self-improvement goals were often shared by other members, which strengthened their motivation to attend the classes.
Lifestyle changes were a positive benefit of participation in MENTOR. Participants reported that they adopted healthy behaviors and sustained these behaviors long after the program ended. Participants made valuable changes to their nutritional behaviors to eat healthier. Nutritional guidance was provided to participants at a depth they had not expected or previously received. Mindfulness strategies were novel to most participants and helped them cope with pain and other life stressors. Most importantly, nutrition and mindfulness strategies were sustained after the program ended.
Participation was affected by several factors. Regarding facilitating factors, participants reported that the program content was perceived to be of high quality, which was attributed to the professional and knowledgeable coaches. Coaches were perceived as prompt, knowledgeable of disability, helpful, and confident. Additionally, participants reported that exercises were generally well tailored to their functional and cognitive abilities. Regarding barriers to participation, some participants with more severe functional impairment (e.g., quadriplegia) reported that exercises were not suitable to their functional ability. Specifically, people with tetraplegia desired more in-depth adaptations for their arms that would increase the ease of difficulty with performing similar movements as others in the class, while also exhibiting sufficient effort or work to provide a physiologic health benefit. Additionally, some participants reported that they would like the option to attend in-person classes. These participants did not feel engaged through telecommunication. Some participants' ability to attend the classes was restricted by their availability (e.g., worked a full-time job or had family responsibilities). To remedy this, participants recommended more options for class times. Even though the daily class regime was provided to participants as a way of allowing them to choose various components that could fit into their daily routine, participants were disappointed by having to miss class components.
Discussion
This retrospective evaluation of a holistic, community-based program found that people with SCI value comprehensive online wellness for providing a sense of peer-support and promoting sustainable, health-enhancing behaviors. Participants also reported improved psychological well-being. This finding is similar with benefits reported in a scoping review of 20 qualitative clinical studies examining wellness interventions for people with SCI (36). Of note, the scoping review recommended that clinical studies of wellness should include a broad understanding of well-being and be more accessible to people with SCI, traits inherent in the MENTOR program. Most of the previous studies were conducted in clinical settings or required in-person supervision or visitation. MENTOR provided a fully remote, no-cost program across the nation for people with SCI who had internet access. The program included daily classes that participants could choose and prioritize based on their needs and interests, and the group-based structure and one-on-one coaching promoted peer-supported mentoring.
Quantitative, evidence-based wellness programs for people with SCI are sparse. One study published in 2017 descriptively reported that a wellness program for 45 people with SCI may have improved pain management, depression levels, and exercise behavior, with reductions in time spent watching television (37). Another study demonstrated that 23 people with SCI who participated in a wellness program had statistically significant improvements in health behaviors and self-efficacy, as well as fewer and less severe secondary health condition compared to a control group (n = 20). One study published in 2016 found that a more medically focused wellness intervention improved function, mood, and quality of life (38). The study further suggested that a wellness program could potentially produce a financial return on investment over a 2-year period (38). MENTOR demonstrated quantitative improvements to exercise behavior, nutrition, sleep, core values, self-care, hobbies, and contribution to society/community, relationships, and overall wellness with a general cohort of people with physical disabilities (31). However, further evidence is needed to confirm these benefits among specific subgroups, such as people with SCI.
Of note, qualitative findings demonstrated that three components, namely, peer-support and relationship building, comprehensive wellness options, and expert coaches, were well received by people with SCI. Peer-support is a strong facilitator of wellness programs (36) and is even a strongly desired trait of exercise only programs (39). Future programs should aim to produce more inclusive class times, provide specific exercise adaptations for people with limited arm function, and provide in-person options for attendance (e.g., peer meetings with remote instructors).
This study had several limitations. First, the evaluation was conducted retrospectively. Some participants completed the program long after others (durations ranging from 5 to 18 months), which could have affected their ability to recall specific aspects or benefits of the program. Second, the sample included a slightly larger number of females than males, which may not be representative of SCI, which generally has a higher incidence among males (40). Third, we were not able to report the lesion levels of participants. Fourth, participants were required to have access to the internet which may not be feasible for some people with SCI. Fifth, given the small sample size, the study findings are not generalizable but, instead, should be transferable to similar settings and traits of those involved.
Conclusion
The need among people with SCI to improve health and prevent/manage secondary conditions can be greatly enhanced by increasing their access to the social determinants of wellness. As a government-sponsored program, MENTOR has the capacity over the next 5 years to reach more and more people with SCI across the U.S. in an effort to provide quality programs and services to this underserved population. The social determinants of wellness can have a profound effect on improving health and reducing the risk of age-associated chronic diseases in people with SCI.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by University of Alabama at Birmingham Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
RY, MC, and CL were responsible for conducting the interviews. BL and MC analyzed the data. TS, JR, and BL created the initial draft of the manuscript. H-JY and JW created the second manuscript draft. All authors contributed to the final manuscript draft.
Funding
Funding for this study was provided by the Centers for Disease Control and Prevention (CDC), Division of Birth Defects and Developmental Disabilities (NCBDDD), Disability and Health Promotion Branch, Grant #NU27DD000022.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to give special thanks to the MENTOR participants who volunteered their time and effort to assist with testing this online quality improvement program.
References
1. Carroll N, Hall AG, Feldman S, Thirumalai M, Wade JT, Rimmer JH. Enhancing transitions from rehabilitation patient to wellness participant for people with disabilities: an opportunity for hospital community benefit. Front Pub Health. (2020) 8:105. doi: 10.3389/fpubh.2020.00105
2. Kennedy J, Wood EG. Disability-Based Disparities in Social Determinants of Health Among Working-Age Adults: Evidence From the 2018 National Health Interview Surveys. Spokane: Collaborative on Health Reform and Independent Living (2020).
3. Rimmer J H, Chen M-D, Hsieh K. A conceptual model for identifying, preventing and treating secondary conditions in people with disabilities. Phys Ther. (2011) 91:1728–38. doi: 10.2522/ptj.20100410
4. Brinkhof M, Al-Khodairy A, Eriks-Hoogland I, Fedete C, Hinrichs T, Hund-Georgiadis M, et al. Health conditions in people with spinal cord injury: contemporary evidence from a population-based community survey in Switzerland. J Rehabil Med. (2016) 48:197–209. doi: 10.2340/16501977-2039
5. Heinemann A, Steeves JD, Boninger M, Groah S, Sherwood AM. State of the science in spinal cord injury rehabilitation 2011: informing a new research agenda. Spinal Cord. (2012) 50:390–7. doi: 10.1038/sc.2012.12
6. Krause J. Secondary conditions and spinal cord injury: a model for prediction and prevention. Top Spinal Cord Inj Rehabil. (1996) 2:58–70. doi: 10.1310/sci1901-15
7. Burke D, Fullen BM, Stokes D, Lennon O. Neuropathic pain prevalence following spinal cord injury: a systematic review and meta-analysis. Eur J Pain. (2017) 21:29–44. doi: 10.1002/ejp.905
8. Adriaansen J., Post MWM, Brinkhof MWG, deGroot S, van Asbeck FWA, et al. Secondary health conditions in persons with spinal cord injury: a longitudinal study from one to five years post-discharge. J Rehabil Med. (2016) 45:1016–22. doi: 10.2340/16501977-1207
9. Laughton G, Buchholz AC, Martin Ginis KA, Goy RE. Lowering body mass index cutoffs better identifies obese persons with spinal cord injury. Spinal Cord. (2009) 47:757–62. doi: 10.1038/sc.2009.33
10. Gorgey A, Gater DR. Prevalence of obesity after spinal cord injury. Top Spinal Cord Inj Rehabil. (2007) 12:1–7. doi: 10.1310/sci1204-1
11. Tian W, Hsieh C-H, DeJong G, Backus D, Groah S, Ballard PH. Role of body weight in therapy participation and rehabilitation outcomes among individuals with traumatic spinal cord injury. Arch Phy Med Rehabil. (2013) 94:S125–36. doi: 10.1016/j.apmr.2012.10.039
12. Rajan S, McNeely MJ, Warms C, Goldstein B. Clinical assessment and management of obesity in individuals with spinal cord injury: a review. J Spinal Cord Med. (2008) 31:361–72. doi: 10.1080/10790268.2008.11760738
13. Latimer A, Martin Ginis KA, Craven B, Hicks A. The physical activity recall assessment for people with spinal cord injury: validity. Med Sci Sports Exerc. (2006) 38:208–16. doi: 10.1249/01.mss.0000183851.94261.d2
14. Martin Ginis K, Latimer AE, Arbour-Nicitopoulos KP, Bucholz AC, Bray SR, Craven C. Leisure time physical activity in a population-based sample of people with spinal cord injury Part I: demographic and injury-related correlates. Arch Phy Med Rehabil. (2010) 91:722–8. doi: 10.1016/j.apmr.2009.12.027
15. Martin Ginis KA, Hicks AL. Exercise research issues in the spinal cord injured population. Exerc Sport Sci Rev. (2005) 33:49–53.
17. Bodai B, Nakata TE, Wong WT, Clark DR, Lawenda S, Tsou C, et al. Lifestyle medicine: a brief review of its dramatic impact on health and survival. Perm J. (2018) 22:17–025. doi: 10.7812/TPP/17-025
18. Rimmer JHHK. Building the crossroad between inpatient/outpatient rehabilitation and lifelong community-based fitness for people with neurologic disability. JNPT. (2013) 37:72–7. doi: 10.1097/NPT.0b013e318291bbf6
19. Iezzoni L, Rao SR, Ressalam J, Bolcis-Jankovic D, Agaronnik ND, Donelan K et al. Physicians' perceptions of people with disability and their health care. Health Aff. (2021) 40:296–306. doi: 10.1377/hlthaff.2020.01452
20. Post MWM, van Leeuwen CMC. Psychosocial issues in spinal cord injury: a review. Spinal Cord. (2012) 50:382–9. doi: 10.1038/sc.2011.182
21. Nash M, Tractenberg RE, Mendez AJ, David M, Ljungberg IH, Tinsley EA, et al. Cardiometabolic syndrome in people with spinal cord injury/disease: guideline-derived and nonguideline risk components in a pooled sample. Arch Phy Med Rehabil. (2016) 97:1696–705. doi: 10.1016/j.apmr.2016.07.002
22. Burkell JA, Wolfe DL, Potter PJ, Jutai JW. Information needs and information sources of individuals living with spinal cord injury. Health Info Libr J. (2006) 23:257–65. doi: 10.1111/j.1471-1842.2006.00686.x
23. Geyh S, Kunz S, Muller R, Peter C. SwiSCI Study Group. Describing functioning and health after spinal cord injury in the light of psychological-personal factors. J Rehabil Med. (2016) 48:219–34. doi: 10.2340/16501977-2027
24. Winett R, Davy BM, Marinik E, Savla J, Winett SG, Phillips SM, et al. Developing a new treatment paradigm for disease prevention and healthy aging. Trans Behav. Med. (2014) 4:117–23. doi: 10.1007/s13142-013-0225-0
25. Munce S, Webster F, Fehlings MG, Straus SE, Jang E, Jaglal SB. Meaning of self-management from the perspective of individuals with traumatic spinal cord injury, their caregivers, and acute care and rehabilitation managers: an opportunity for improved care delivery. BMC Neurol. (2016) 16:1–9. doi: 10.1186/s12883-016-0534-2
26. Simpson L, Eng JJ, Hsieh JTC, Wolfe DL. Spinal cord injury rehabilitation evidence research team. The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma. (2012) 29:1548–55. doi: 10.1089/neu.2011.2226
27. Rubinelli S, Glassel A, Brach M. From the person's perspective: perceived problems in functioning among individuals with spinal cord injury in Switzerland. J Rehabil Med. (2016) 48:235–43. doi: 10.2340/16501977-2060
28. Bonanno G, Kennedy P, Galatzer-Levy IR, Lude P, Elfstrom ML. Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehab Psych. (2012) 57:236–47. doi: 10.1037/a0029256
29. Monden, Trost Z, Catalano D, Garner AN, Symcox J, Driver S, et al. Resilience following spinal cord injury: a phenomenological view. Spinal Cord. (2014) 52:197–201. doi: 10.1038/sc.2013.159
30. Bertozzi B, Tosti V, Fontana L. Beyond calories: An integrated approach to promote health, longevity, and well-being. Geront. (2017) 63:13–9. doi: 10.1159/000446346
31. Rimmer JH, Wilroy J, Galea P, Jeter A, Lai BW. Retrospective evaluation of a pilot eHealth/mHealth telewellness program for people with disabilities: mindfulness, exercise, and nutrition to optimize resilience (MENTOR). mHealth. (2022) 8:15. doi: 10.21037/mhealth-21-34
32. Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. (2006) 18:59–82. doi: 10.1177/1525822X05279903
33. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Pyshcol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
35. Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. (2016) 26:1753–60. doi: 10.1177/1049732315617444
36. Simpson B, Villeneuve M, Clifton S. The experience and perspective of people with spinal cord injury about well-being interventions: a systematic review of qualitative studies. Disabil Rehabil. (2020) 1–15. doi: 10.1080/09638288.2020.1864668
37. Crane DA, Hoffman JM, Reyes MR. Benefits of an exercise wellness program after spinal cord injury. J Spinal Cord Med. (2017) 40:154–8. doi: 10.1179/2045772315Y.0000000038
38. Dicianno BE, Lovelace J, Peele P, Fassinger C, Houck P, Bursic A, et al. Effectiveness of a wellness program for individuals with spina bifida and spinal cord injury within an integrated delivery system. Arch Phys Med Rehabil. (2016) 97:1969–78. doi: 10.1016/j.apmr.2016.05.014
39. Lai BW, Rimmer JH, Yates A, Jeter A, Young H-J, Thirumalai M, et al. Critical factors influencing the decision to enroll in a physical activity intervention among a predominant group of adults with spinal cord injury: a grounded theory study. Spinal Cord. (2021) 59:17–25. doi: 10.1038/s41393-020-0530-7
Keywords: wellness, disability, exercise, nutrition, lifestyle program, telehealth
Citation: Rimmer JH, Wilroy J, Young H-J, Young R, Sinha T, Currie M, Lima CR and Lai B (2022) Qualitative Evaluation of a Comprehensive Online Wellness Program (MENTOR) Among People With Spinal Cord Injury. Front. Rehabilit. Sci. 3:917898. doi: 10.3389/fresc.2022.917898
Received: 11 April 2022; Accepted: 16 May 2022;
Published: 10 June 2022.
Edited by:
Kristin Musselman, University of Toronto, CanadaReviewed by:
Zhuoying Qiu, China Rehabilitation Research Center/WHO Collaborating Center for Family International Classifications, ChinaGabriel Ronen, McMaster University, Canada
Verna Stavric, Auckland University of Technology, New Zealand
Copyright © 2022 Rimmer, Wilroy, Young, Young, Sinha, Currie, Lima and Lai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Byron Lai, YmxhaUB1YWJtYy5lZHU=
 James H. Rimmer
James H. Rimmer Jereme Wilroy
Jereme Wilroy Hui-Ju Young1,2
Hui-Ju Young1,2 Madison Currie
Madison Currie Carla Rigo Lima
Carla Rigo Lima Byron Lai
Byron Lai