- 1Center for Human Movement Sciences, University Medical Center Groningen, University of Groningen, Groningen, Netherlands
- 2Swiss Paraplegic Research, Nottwil, Switzerland
- 3School of Sport Exercise & Health Sciences, Peter Harrison Centre for Disability Sport, Loughborough University, Loughborough, United Kingdom
- 4Center for Rehabilitation, University Medical Center Groningen, University of Groningen, Groningen, Netherlands
- 5Amsterdam Rehabilitation Research Center Reade, Amsterdam, Netherlands
- 6Department of Human Movement Sciences, Faculty of Behavioral and Movement Sciences, Vrije Universiteit, Amsterdam, Netherlands
Wheelchair tennis players are prone to develop shoulder injuries, due to the combination of wheelchair propulsion, overhead activities and daily wheelchair activities. A methodical literature search was conducted to identify articles on shoulder complaints in wheelchair tennis, wheelchair sports and tennis. The aims were to identify (1) type of shoulder complaints; (2) possible risk factors for the development of shoulder injuries; (3) musculoskeletal adaptations in the shoulder joint in wheelchair tennis players. Fifteen papers were included in this review, five on wheelchair tennis, three on wheelchair sports and seven on tennis. Type of shoulder complaints were acromioclavicular pathology, osteoarthritic changes, joint effusion and rotator cuff tears. Possible risk factors for the development of shoulder injuries in wheelchair tennis are overhead movements, repetitive activation of the anterior muscle chain and internal rotators, as well as a higher spinal cord injury level. Muscular imbalance with higher values for the internal rotators, increase in external range of motion, decrease in internal range of motion and reduced total arc of motion were the most common proposed musculoskeletal adaptations due to an unbalanced load. These presented risk factors and musculoskeletal adaptations might help researchers, coaches and wheelchair tennis players to prevent shoulder injuries.
Introduction
Wheelchair sports participation, like wheelchair tennis, is growing in popularity and is a great opportunity for people with disabilities to get physically active (1). Wheelchair users have an elevated risk to develop various diseases due to a restricted mobility and often sedentary lifestyle, therefore, exercise is crucial to maintain health (2–4). Even though sports participation in wheelchair sports has a broad range of positive effects, it also leads to an increase in stressors on the shoulder complex in addition to the loading from daily activities (5, 6). The prevalence of shoulder problems in wheelchair athletes is reported to have a broad range, i.e., from 16% (7) up to 76% (8). This is similar to able-bodied tennis, in which the shoulder is the most common area of injury of the upper extremity (9). Shoulder pain is prevalent in 24% of the elite tennis players (12–19 years old) (10).
Becoming wheelchair dependent changes the role of the shoulder complex, from providing a great range of motion (ROM) to perform small and detailed movements, into the main source of power for mobility in daily life (11). The motion sequence of wheelchair propulsion itself puts relatively low internal joint forces on the shoulder during regular wheelchair propulsion (12, 13). However, the high frequency of performing the movement in addition to the high shoulder load during specific daily activities, such as transfers in and out of the wheelchair, result in a high exposure to the shoulder joint (12). Changes in the role of the shoulder complex, which require an increased force generation of the upper extremity might lead to imbalances of the muscular system and impact the positioning of the scapula in respect to the humerus as well as both in respect to the thorax (14). Altered conditions in the shoulder joint favor an impingement within the subacromial space and a greater abrasion of the joint (6, 15).
Wheelchair tennis is the most popular adapted racket sport but it involves a high incidence of shoulder complaints (16–19). In wheelchair tennis, the tennis racket is an additional constraint during propulsion of the wheelchair since it interferes with the hand/rim interaction (20). With the racket in one hand, which leads to unilateral power losses because of the more difficult coupling to the hand rim, greater forces need to be produced to maintain balanced power production at both sides (21, 22). As in able-bodied tennis, wheelchair tennis players have a repetitive activation of the anterior muscle chain, due to the unidirectional movements of the strokes. Furthermore, a seated position, as is the case in wheelchair tennis, leads to a modified force generation, as well as changes in shoulder alignment and trunk rotations (17, 23, 24). The core stability and sitting position in the wheelchair have a great impact on the shoulder mechanics and, therefore, on the force generation in the serve and ground strokes (23).
Wheelchair dependence and overhead activities in combination with high training intensities increase the already heavy strain on the shoulder and might be a possible risk factor for overuse injuries in wheelchair tennis athletes (22, 25). Injuries to the upper extremity or overuse symptoms not only negatively affect sport performance but also have a tremendous impact on body functions, activity, and participation in daily life (11). Therefore, it is highly important to identify possible causes and aggravating factors and avoid shoulder injuries in wheelchair tennis. The aims of this review are to: (1) identify type of shoulder complaints; (2) potential risk factors for the development of shoulder injuries in wheelchair tennis; (3) investigate potential musculoskeletal adaptations causing shoulder complaints in the shoulder joint in wheelchair tennis. Given the small number of wheelchair tennis papers, an overview will be given from a wheelchair tennis perspective, as well as a broader view from a wheelchair sports and able-bodied tennis perspective. Due to the recency of written reviews by Heyward et al. (22) on shoulder injuries in wheelchair sports and by Kekelekis et al. (26) on shoulder injuries in able-bodied tennis, these two papers were taken as central papers in the respective parts of the current review and extended with additional papers.
Materials and Methods
Search Strategy
A methodical search strategy was conducted in October 2020 using the PRISMA checklist (Supplementary Table 1) for Scoping reviews by two independent researchers (LM, TR) to identify relevant published articles on the topic of shoulder complaints in (i) wheelchair tennis, (ii) wheelchair sport and (iii) tennis. In case of discrepancies between authors, articles were discussed between the two researchers. PubMed and Web of Science were used to search for relevant articles. The PubMed search strategy shown below was adapted for the second database Web of Science.
(1) (“Wheelchairs”[Mesh])
(2) (“Sports”[Mesh])
(3) (“Tennis”[Mesh])
(4) (“Shoulder Joint”[Mesh] OR “Upper Extremity”[Mesh] OR “Shoulder”[Mesh] OR “Scapula”[Mesh] OR “Rotator Cuff”[Mesh])
(5) (“Muscle Strength”[Mesh] OR “Pain”[Mesh] OR “Musculoskeletal Pain”[Mesh] OR “Chronic Pain”[Mesh] OR “Shoulder Pain”[Mesh] OR “Wounds and Injuries”[Mesh] OR “Athletic Injuries”[Mesh] OR “Rotator Cuff Injuries”[Mesh] OR “Tendon Injuries”[Mesh] OR “Stress Disorders, Post-Traumatic”[Mesh] OR “Arm Injuries”[Mesh] OR “Shoulder Impingement Syndrome”[Mesh] OR “Shoulder Injuries”[Mesh] OR “Bursitis”[Mesh] OR “Rotator Cuff Tear Arthropathy”[Mesh] OR “Risk”[Mesh] OR “Risk Factors”[Mesh] OR “Health Risk Behaviors”[Mesh] OR “Pathology”[Mesh] OR “Syndrome”[Mesh] OR cause*[tiab] OR mechanism*[tiab] OR complaint*[tiab] OR discomfort*[tiab])
Search string – Wheelchair tennis: (1), (3), (4) and (5)
Search string – Wheelchair sports: (1), (2), (4) and (5)
Search string – Tennis: (3), (4) and (5)
Articles from the database search were first checked for duplicates, secondly the titles and abstracts were screened. Thirdly, the full text of the remaining articles was assessed and included if criteria were met.
Inclusion Criteria
Articles in the English language that incorporated some type of shoulder complaint or assessment either in wheelchair sports, tennis or a combination of the two.
Exclusion Criteria
Papers from all categories (wheelchair tennis, wheelchair sports, tennis) were excluded if they had a treatment/ intervention program, an assessment was evaluated/tested and when it was an epidemiological study. For the able-bodied tennis and wheelchair sport papers, articles were also excluded when pain in the shoulder joint was not reported. This was not an exclusion criterion for the wheelchair tennis papers, due to the scarcity of available literature.
Data Extraction and Quality Assessment
Quality assessment was also performed by two independent researchers (LM, TR) for all included articles and was performed with a checklist of Webster et al. (27), adapted by Heyward et al. (22). This checklist was chosen because there is no standardized checklist available for this type of study. For each question a score of 1 was given for an “adequate” or “yes” response, a score of 0.5 was given for a “partial” or “limited” response; and a score of 0 was awarded for a “no”, “not stated” or “inadequate” response. A maximum score of 8 was possible. There were no minimum criteria set due to the limited number of papers that were included in the study.
Definitions of Risk Factors and Musculoskeletal Adaptations
Risk factors for complaints in this review were defined based on Hoozemans et al. (28) in which “external load” was defined using three factors: intensity, frequency and duration (Figure 1). The risk for complaints occurs if the value of one of these three factors or the combination of the factors deviates from their optimal value (28, 29). Musculoskeletal adaptions are caused by the risk factors and lead to unfavorable biomechanical conditions in the shoulder complex. An example of a risk factor could be an increased internal rotation balance ratio, due to greater activation of the anterior muscles and repetitive movements. The musculoskeletal adaptation that occurs could be a muscular imbalance. Due to the limited research in the topic, statistically proven risk factors as well as proposed risk factors were included in this review.
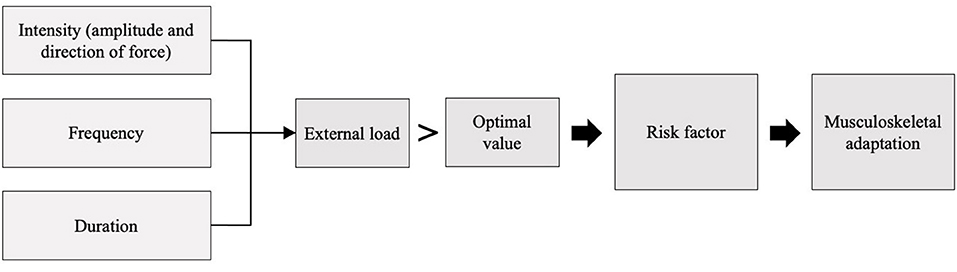
Figure 1. Conceptual model of risk factors and musculoskeletal adaptations for shoulder injuries, based on the model of Hoozemans et al. (28).
Results
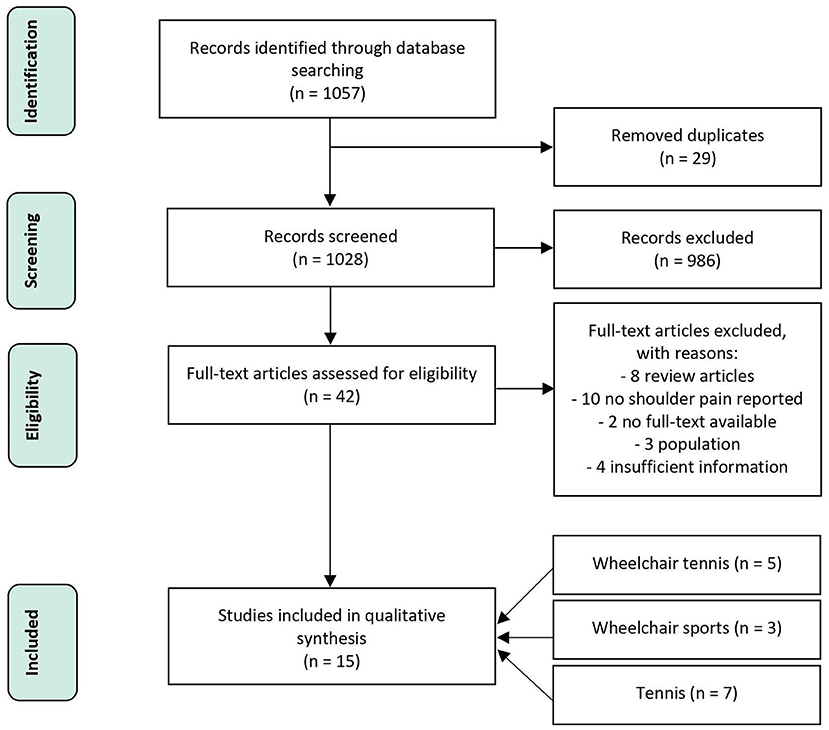
A flow chart of the selection process is shown in Figure 2. Five papers were included regarding wheelchair tennis. For wheelchair sports, an interpretation of 13 papers of the review of Heyward et al. (22) will be given, with an additional three papers selected for the current review. For the tennis papers, an interpretation of 23 papers of the review of Kekelekis et al. (26) will be given, with an additional seven papers for the current review.
In 12 of the 15 included articles shoulder problems or a history of shoulder problems were reported, of which eight included clinical testing of the shoulder complaint. A wide variety in screening of indicators for shoulder complaints were reported. Radiographic analysis was used in three articles (18, 30, 31), a strength test in six (30, 32–36), a kinematic analysis in three (5, 24, 37), a kinetic analysis in two (38, 39), the Wheelchair User's Shoulder Pain Index (WUSPI) in two (5, 31), visual analogue scale (VAS) in two (33, 34), range of motion (ROM) measurement in four (32–34, 40) and the scapular resting position (25), perceived function (25), serve speed (34) and post impact ball velocity (39) in one of the articles.
Quality of the Evidence
The results of this review should be viewed with consideration to the level of evidence (Supplementary Table 2). The quality of the articles in the review of Heyward et al. (22) were checked using the same checklist and ranged from low (3) to good (7), with a mean of around 4.5. Especially inclusion/exclusion criteria, reliability and validity were poorly described across papers. The quality of the articles in the review of Kekelekis et al. (26) were checked using a different, extensive checklist by Downs and Black (41). Due to the great number of subcategories and their specificity, the overall score average was low to moderate, with especially the internal validity lacking.
Of all 15 included papers in the current review, eight described the participants characteristics adequately (5, 18, 24, 31–34, 36). Six papers fully described inclusion and exclusion criteria (5, 25, 30, 33, 34, 40) and 13 described the limitations of the study (5, 18, 25, 30–35, 37–40). The key variables, pain, strength and injuries were measured adequately in seven of the 15 papers (5, 18, 24, 32, 34, 37, 39). Overall, the validity and reliability of the used assessments had limited description. In six of the included studies the reliability (5, 24, 30, 32, 33, 40) and in seven the validity (5, 24, 30, 31, 33, 39, 40) were adequately described. Only two papers (25, 32) adequately discussed the external validity of the results.
Type of Shoulder Complaints
Wheelchair Tennis
An overview of the included papers can be seen in Table 1. In the wheelchair tennis papers, two (5, 18) of the five papers reported shoulder complaints by the participants. Causes of complaints in wheelchair tennis were acromioclavicular pathology in the dominant shoulder, osteoarthritic changes, joint effusion and rotator cuff tears (18) in the dominant as well as the nondominant shoulder, most commonly in the supraspinatus tendon. The paper of Warner et al. (5) reported two participants with previously experienced pain due to shoulder impingement and one participant with subacromial pain syndrome.
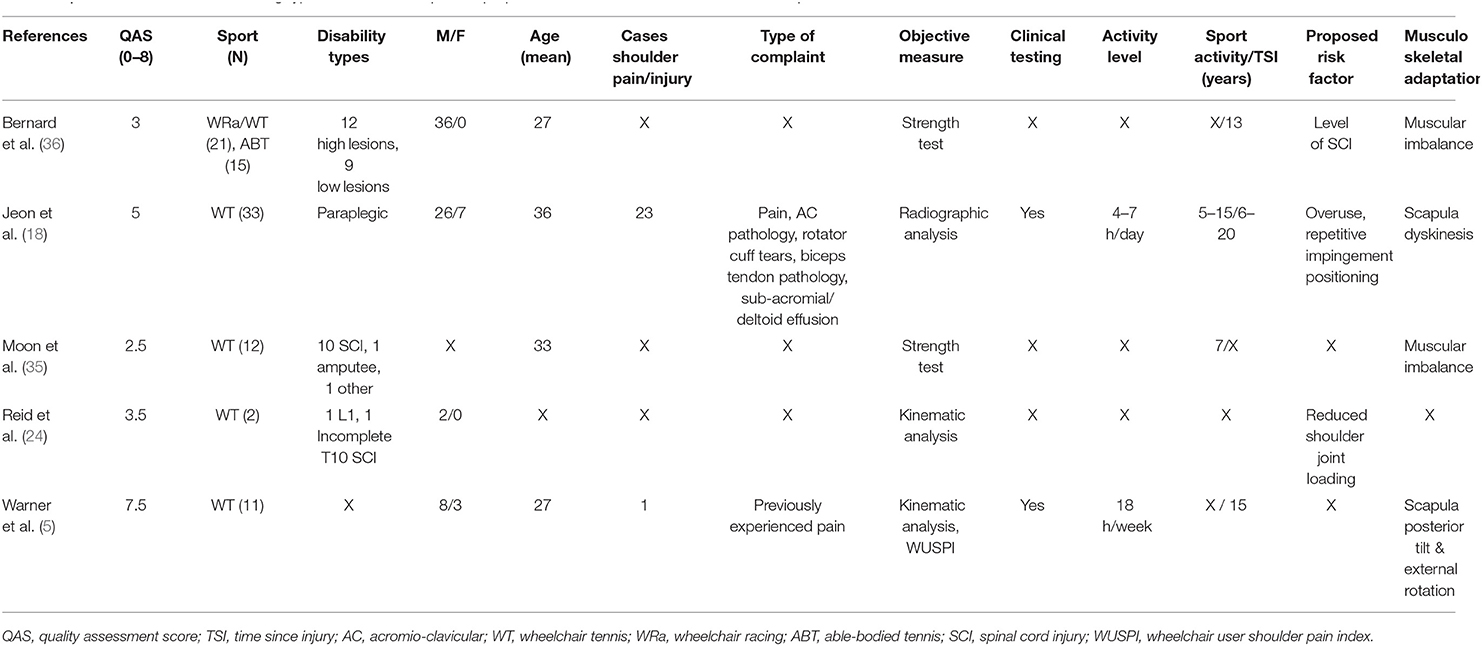
Table 1. Overview of articles describing type of shoulder complaints, proposed risk factors and musculoskeletal adaptations in wheelchair tennis.
A Broader View From Wheelchair Sports and Able-Bodied Tennis
Pain was reported as the most frequent shoulder complaint in the review of Heyward et al. (22) and the three additional selected papers (25, 31, 37) (Table 2). Other shoulder problems included rotator cuff tears, rotator cuff impingement, acromion-clavicular and bicep tendon pathology, subdeltoid and subacromial effusion, as well as non-specific shoulder issues (22). In one of the additional included papers (31) tendinopathy and bursitis were listed as other shoulder complaints. A history of shoulder problems in the selected able-bodied tennis papers and the review of Kekelekis et al. (26) were tendinosis (30), general pain (33, 34, 40, 42), rotator cuff tears or tendinopathy (38, 39, 42, 43), osteoarthritic changes (44) and labral lesion or tears (38, 42, 43).
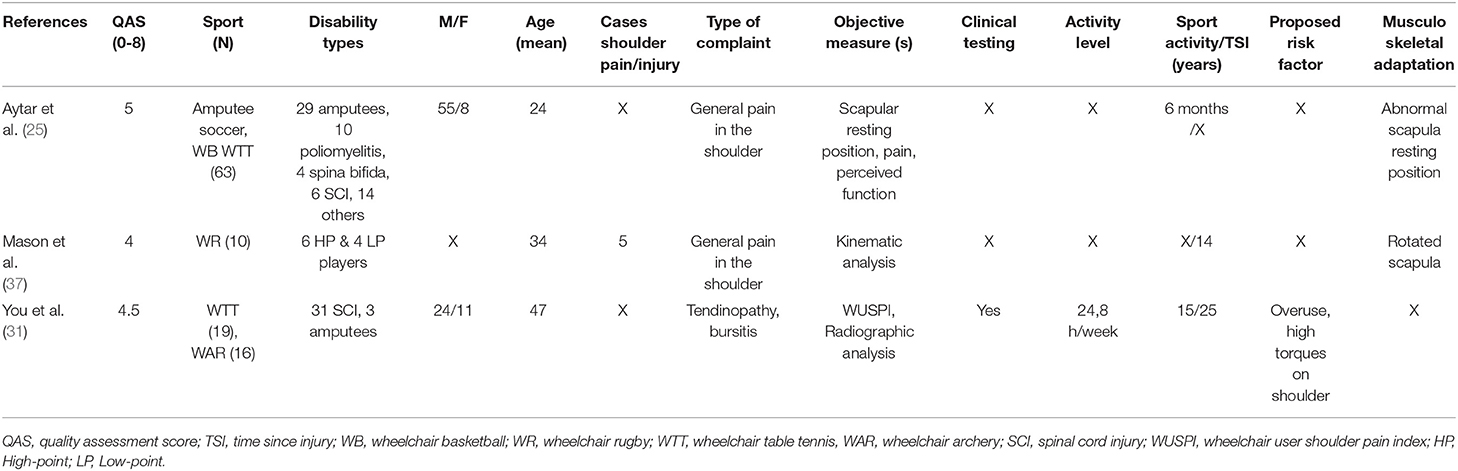
Table 2. Overview of articles describing type of shoulder complaints, proposed risk factors and musculoskeletal adaptations in wheelchair sports.
Risk Factors
The interpretation of the possible relationships between risk factors and musculoskeletal adaptions are schematically represented using the previous defined model of Hoozemans (Figure 3). Due to the low number of articles in wheelchair tennis describing risk factors and musculoskeletal adaptations, a broader view from wheelchair sports and able-bodied tennis is presented as well. Firstly, the risk factors will be described, secondly the musculoskeletal adaptation. These summarizing results will be further interpreted in the discussion part.
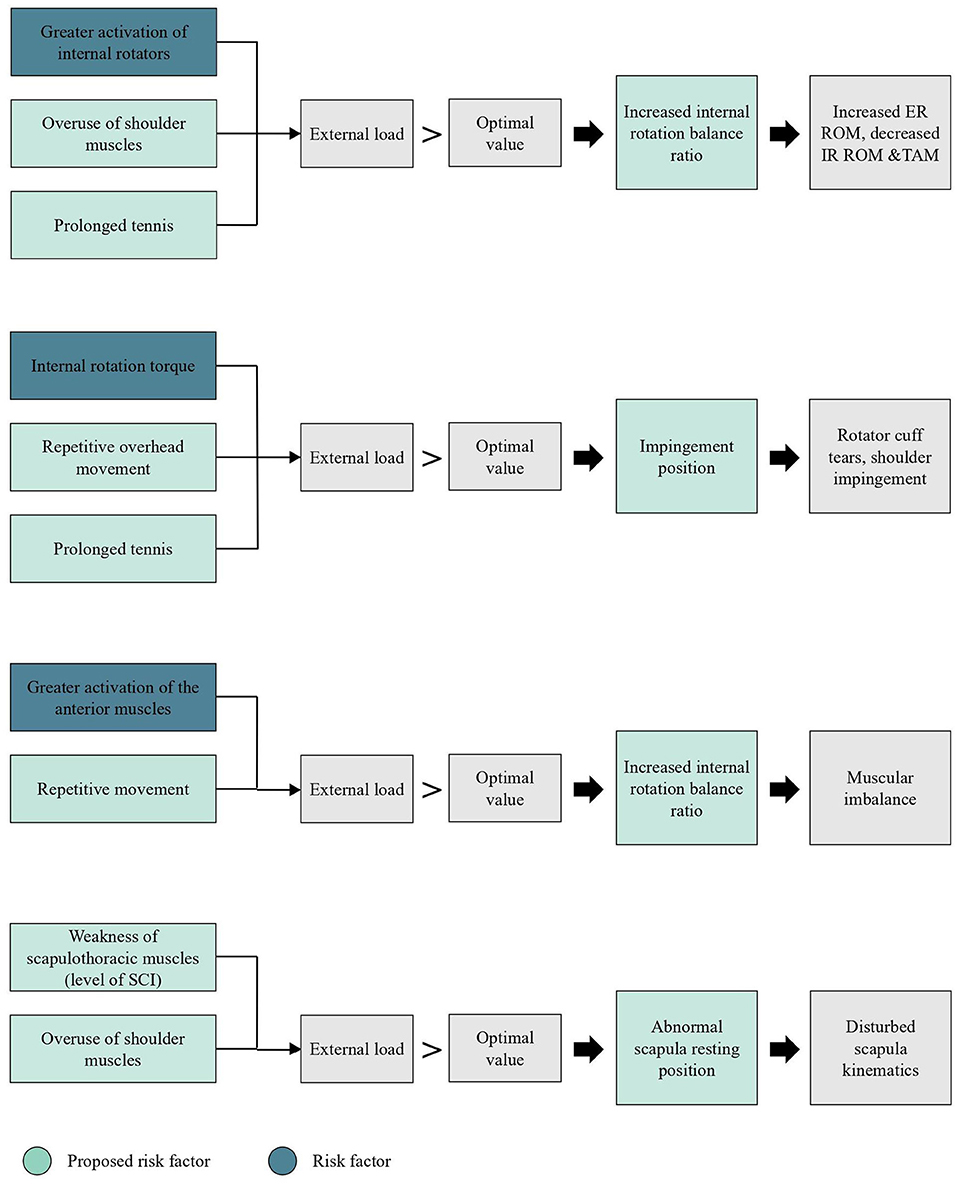
Figure 3. Schematic representation of (potential) risk factors and musculoskeletal adaptations for shoulder injuries in wheelchair tennis, based on the conceptual model of Hoozemans et al. (28). ER = external rotation, IR = internal rotation, ROM = range of motion, TAM = total arc of motion, SCI = spinal cord injury.
Wheelchair Tennis
A proposed risk factor for shoulder problems in wheelchair tennis, especially in the dominant shoulder, is overuse, caused by wheelchair propulsion, transfers in and out of the wheelchair and playing tennis (18). The repetitive impingement positioning during the play can lead to rotator cuff tears, especially the supraspinatus muscle, and high compressive forces on the acromioclavicular joint (18). The risk for overuse increases when the internal rotation balance ratio is higher compared to the normal range (35). Another proposed risk factor is the level of spinal cord injury (SCI) (36). Higher values of torque and power for internal and external muscles were observed in athletes with a low level SCI (T11-L3) in comparison with athletes with a higher level SCI (T5-T8) (36). The level of lesion does not necessarily influence the rotator balance ratio in the shoulder by the activation of internal rotator muscles but by the participation of the external rotators (36). Age, training time per day, duration of wheelchair usage and wheelchair tennis career did not present as risk factors (18).
A Broader View From Wheelchair Sports and Able-Bodied Tennis
Participating in wheelchair sports bears several risk factors for shoulder problems, which are multifactorial (22). Proposed risk factors were overuse of the shoulder muscles and less trunk control. Performing overhead sports in a wheelchair increases the risk for rotator cuff tears due to overhead motion and the recurrent microtrauma (8). Repetitive shoulder movements with a great internal rotation torque can lead to the occurrence of a mechanical shoulder impingement and are a proposed risk factor for shoulder overuse injuries (31). No associations were observed between age, wheelchair usage duration, training load and the amount of pain due to shoulder problems (31).
Prolonged tennis exposure was identified as the most common proposed risk factor for able-bodied tennis players in the review of Kekelekis et al. (26), due to its negative effect on muscle performance, serve maximal angular velocities and joint kinetics (26, 45). Furthermore, skill level and technique of the player were identified as risk factors. Less shoulder joint load with a lower risk for the development of injuries was observed in professional tennis players (43). Additional risk factors were a prolonged abduction during the external rotation phase of the serve (46) and scapula dyskinesia (47). Proposed risk factors were a stiffer racket (48), racket with a higher polar moment of inertia (49) and previous injuries (46, 50).
The additional selected papers in this review showed that repetitive overhead movements (42) and overuse due to rigorous training schedules (32) seem to be related to shoulder injuries (Table 3). During the serve and smash, the dominant arm is in an abducted position with full external rotation and extension which leads to structural lesions of the rotator cuff and superior labral lesions (42). The overhead motion causes repetitive microtraumas to the capsule and a posterior capsule tightness in tennis players with shoulder pain can be observed (33). Additionally, serve variations like the waiter's serve (39) as well as improper techniques (38) are risk factors for the development of overuse injuries, since alterations in timing of trunk and shoulder rotation in the serve can lead to higher shoulder joint loads. Lastly, a strong upper trapezius in both sides (32) was listed as a proposed risk factor for the development of shoulder injuries in tennis players.
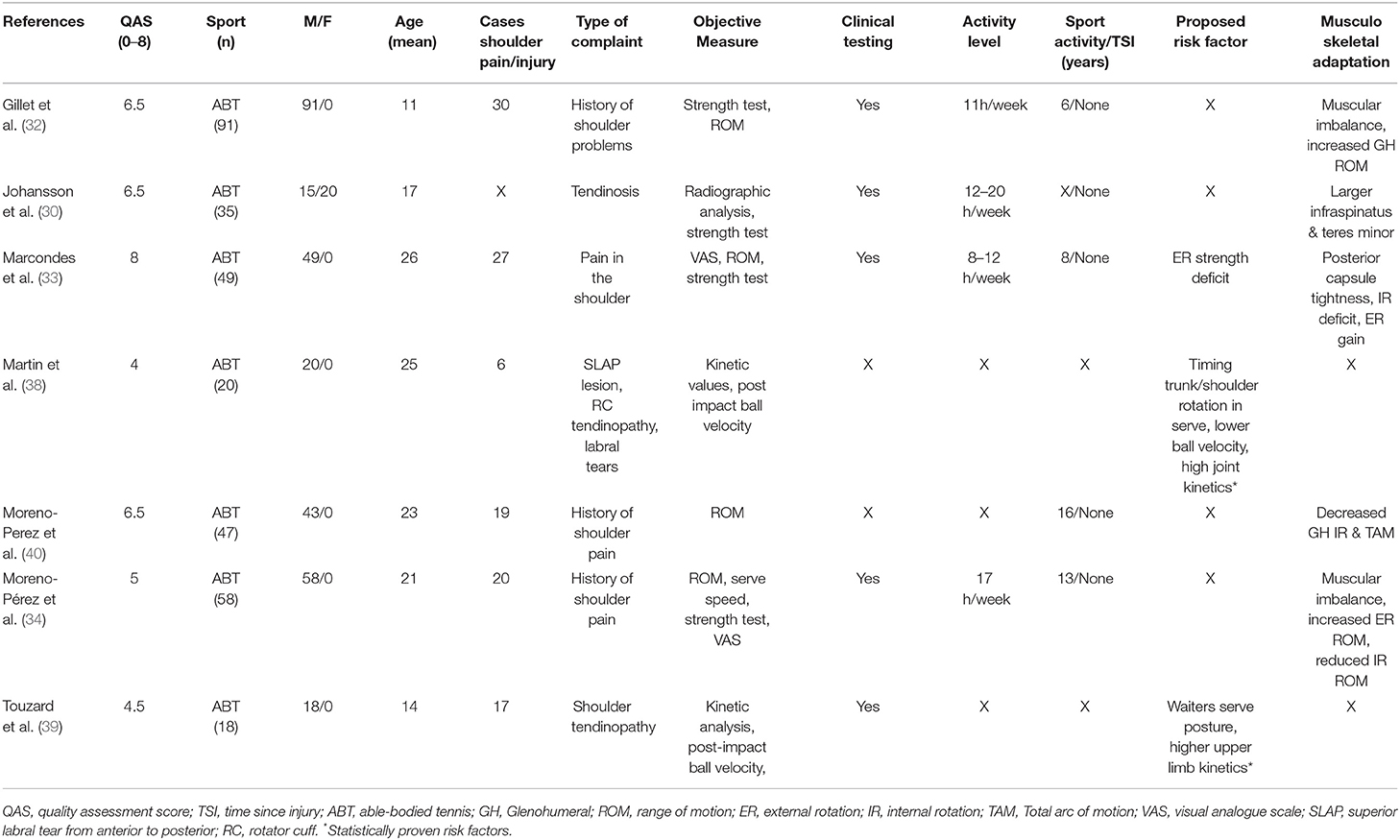
Table 3. Overview of articles describing type of shoulder complaints, proposed risk factors and musculoskeletal adaptations in able-bodied tennis.
Musculoskeletal Adaptations
Wheelchair Tennis
In wheelchair tennis, the supposed musculoskeletal adaptations in shoulder problems are multifactorial. Three of the five papers (18, 35, 36) mentioned a muscular imbalance as alteration in the shoulder girdle, but only one (18) connected it with the occurrence of shoulder problems. Two papers (35, 36) described a muscular imbalance with a higher extension than flexion strength and higher values for internal than external rotator muscles, especially on the dominant side. Differences between the dominant and non-dominant side for scapula posterior tilt were observed, with a more posteriorly tilted scapula on the dominant side (5). The upwardly rotated scapula of the dominant arm in wheelchair tennis players was higher compared to able-bodied participants with shoulder impingement (5).
A Broader View From Wheelchair Sports and Able-Bodied Tennis
Musculoskeletal adaptations associated with shoulder pain in wheelchair sports were difficult to identify. In the review of Heyward et al. (22) it was suggested that shoulder pain was connected to weaknesses in the internal/external rotation, as well as adduction of the shoulder. In one of the additional included papers (25) it was discussed that a weakness of scapula thoracic muscles due to participation in wheelchair sports potentially leads to an abnormal positioning of the scapula. As a consequence, disturbances in the scapula humeral rhythm and general shoulder dysfunction might be observed (25). Scapula position in bilateral shoulder pain in symptomatic individuals had less upward rotation than symptomatic individuals with unilateral pain (37). During the push phase, the scapula moves towards a more internally, upwardly rotated and less anterior position. During the recovery phase the scapula maintained an upward rotated position (37).
Muscular imbalance in the shoulder joint was the most frequent proposed musculoskeletal adaptations in shoulder problems in able-bodied tennis players (30, 32, 34). The studies describe an unbalanced ratio between internal and external rotators in tennis players, especially in the dominant arm. Increases in internal rotators strength are favored due to the demand during tennis strokes (30, 32, 34). A deficit in external rotation strength in the dominant arm in tennis players with shoulder pain has been observed in the study of Marcondes et al. (33). With an imbalance of the muscular system, a change of ROM often takes place, which can be associated with shoulder problems. Four papers (32–34, 40) describe an increase in external ROM, a decrease in internal ROM and a reduced total arc of motion (TAM) in the glenohumeral joint of the dominant arm of tennis players with a history of shoulder pain. The TAM, is defined as the sum of internal rotation ROM and external rotation ROM (32).
Discussion
The aim of the current review was to identify type of shoulder complaints and potential risk factors for the development of shoulder injuries in wheelchair tennis and investigate potential musculoskeletal adaptations in the shoulder joint in wheelchair tennis players. In the course of this review, risk factors and musculoskeletal adaptations in wheelchair tennis, wheelchair sports and able-bodied tennis were presented (Figure 3). There was a scarcity of literature in all three areas, but by connecting available literature, implications for future research and practice were derived.
Overhead activity with the shoulder joint in an impingement position was proposed as a risk factor for shoulder problems in wheelchair tennis (18), wheelchair sports with an overhead movement (8) and able-bodied tennis (42). Overhead activities, like the service or smash in tennis, repeatedly decrease the subacromial cavity by an elevation of the upper arm and lead to an impingement position (42). The supraspinatus tendon passes laterally beneath the cover of the acromion and the bursa subacromialis in the subacromial cavity, therefore it can be damaged due to the repetitive mechanical impingement (51). That could explain the high prevalence of supraspinatus pathology and bursitis in the dominant arm in athletes performing overhead activities (8, 18, 31, 42).
In tennis players with a history of shoulder problems, a reduced glenohumeral TAM was observed (32). Tennis players appear to evolve an increase in external ROM due to osseus alterations, a decrease in internal ROM due to stiffening of the posterior capsule and a loss of TAM in the dominant arm (32, 34). A loss of internal ROM and TAM in the dominant arm compared to the non-dominant arm is a common adaptation in shoulder injuries (32, 34). The rotator cuff muscles have to compensate for the integrity of the shoulder if the ROM and flexibility increases which could then lead to an overuse of the rotator cuff muscles (32, 34).
The combination of being wheelchair-bound and being an overhead athlete can cause alterations in the position of the shoulder joint and scapula which leads to unfavorable biomechanical conditions in the shoulder complex. Wheelchair tennis consists of short intermittent sprints, that demand a constant acceleration and deceleration with changes in direction, as well as the generation of powerful serves and groundstrokes (11, 22). Due to the seated position and lower ball velocities during the serve, wheelchair tennis players reported less load on the shoulder compared to able-bodied tennis players (24). Wheelchair propulsion as well as playing tennis lead to an unbalanced ratio in the dominant arm in tennis players between internal/external rotators due to a high demand of internal rotators during strokes (34, 36). Comparing wheelchair tennis players with able-bodied tennis players, even higher values for internal rotation were observed (36), which suggests a greater muscular imbalance in wheelchair tennis players.
A higher risk of muscular imbalance and shoulder problems seems to occur in wheelchair tennis athletes who have a higher level of SCI and, as a consequence, less trunk control (36). This is in line with the findings of Heyward et al. (22) in which wheelchair athletes with low trunk control had more shoulder complaints compared to athletes with high trunk control. The lack of muscular control and stabilization in the trunk limits the power generation in the kinematic chain (7). Therefore, the upper body has to compensate for the lack of power, which can overload the shoulder joint and increases the stress on the joint (22). In addition, Bernard et al. (36) suggest that a higher level of SCI influences the internal and external rotator ratio by the preferential development of flexor, internal rotator, and adductor muscles. A muscular imbalance oftentimes alters the scapula position to a more upward and internal rotated position (37). In this abnormal position, the impingement within the subacromial space in the shoulder joint is favored and a greater abrasion of the joint occurs, which is suggested to be one of the reasons for shoulder injuries (5, 35).
Given the above-stated factors, wheelchair tennis players are expected to be prone to develop a muscular imbalance which leads to alterations in the joint positioning. This is supported by a study of Aytar et al. (25) that showed that a high percentage of abnormal scapular resting positions was prevalent in wheelchair sports players, which was associated with pain as well as bad perceived shoulder function. In contrary to this hypothesis, Warner et al. (5) reported that the scapula was more posterior tilted and externally rotated on the dominant than the non-dominant side and only one of the wheelchair tennis players reported pain. Postural abnormalities of the scapula, with a protraction of the scapula are associated with decreasing the subacromial space and the prevalence of shoulder impingement (52). The absence of shoulder pain might be related to the posterior tilt of the scapula. A reduced upward rotation, external rotation and posterior tilt of the scapula are increasing the sub-acromial space, which leads to less abrasion in the shoulder joint (52). The connection between an upwardly rotated scapula and a higher prevalence of pain, was also described by Warner et al. (5). It was suggested that an absence of shoulder pain occurred due to a posterior tilted and externally rotated scapula in the dominant arm. The low prevalence of shoulder pain reported in this sample may be explained by a protective benefit due to a specific training program or sports participation, that prevents a protraction and internal rotation of the scapula (5).
Future Research
Further research should be directed toward more specific wheelchair tennis research focused on the load of the shoulder, risk factors and musculoskeletal adaptations. Shoulder load was never assessed in wheelchair tennis, only the influence of the racket and a different hand rim were investigated (20, 21, 53, 54). First the influence of the racket on shoulder load should be investigated, afterwards wheelchair tennis players with and without shoulder complaints could be compared to identify differences. Further investigation of identified risk factors and musculoskeletal adaptations in the course of this review, such as muscular imbalance and alterations in ROM, can give valuable insight for the development of preventive training and exercise programs for wheelchair tennis players.
Limitations
Overall, the lack of publications and research in the wheelchair tennis field brought a limited number of papers out of the literature search that investigated shoulder joint injuries in wheelchair tennis. Due to the lack of high-quality literature on wheelchair tennis to be included in this review, it was necessary to combine it with papers about shoulder complaints in other wheelchair sports and able-bodied tennis. This review is a first attempt to gain insight into potential risk factors for shoulder injuries in wheelchair tennis and their musculoskeletal adaptations by comparing and connecting the available information with outcomes of tennis and other wheelchair sports papers.
Additionally, it is important to mention that the included articles about wheelchair sports in general had a relatively low number of participants, which is a common problem in wheelchair sport literature (55). Several papers did not directly investigate risk factors and musculoskeletal adaptations but proposed multiple potential reasons based on their findings, which makes wheelchair tennis focused research even more important. Furthermore, the studies oftentimes did not specify which type of shoulder complaint was the cause and differentiated in the objective measurement tools, which made it challenging to compare the outcomes and draw conclusions.
Conclusion
Risk factors and musculoskeletal adaptations in wheelchair tennis can only be described from a broader wheelchair sports and tennis perspective. Possible risk factors for the development of shoulder injuries in wheelchair tennis are overhead movements, repetitive activation of the anterior muscle chain and internal rotators, as well as a higher SCI level. Muscular imbalance with higher values for the internal rotators, increase in external ROM, decreased internal ROM and reduced TAM were the most common proposed musculoskeletal adaptations due to an unbalanced load. In the future, these risk factors and musculoskeletal adaptations should be investigated in a more wheelchair tennis focused research.
Author Contributions
LM, TR, and RV: conceptualization, investigation, and methodology. LM and TR: formal analysis and writing—original draft. RV, LvdW, SdG, and WdV: supervision. LM, TR, RV, LvdW, SdG, and WdV: writing—review & editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank Leda Maffei and Rowie Janssen for their help in the initial phase of the manuscript and also thank Frontiers in Rehabilitation Sciences for granting a fee waiver to publish this article.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2022.862233/full#supplementary-material
References
1. Fagher K, Lexell J. Sports-related injuries in athletes with disabilities. Scand J Med Sci Sport. (2014) 24:e320–31. doi: 10.1111/sms.12175
2. Blauwet C, Willick SE. The paralympic movement: using sports to promote health, disability rights, and social integration for athletes with disabilities. PM R. (2012) 4:851–6. doi: 10.1016/j.pmrj.2012.08.015
3. Sánchez-Pay A, Sanz-Rivas D. Competitive evolution of professional wheelchair tennis from the paralympic games in Athens 2004 to rio 2016: an observational study. Int J Environ Res Public Health. (2021) 18:1–10. doi: 10.3390/ijerph18063157
4. Flank P, Wahman K, Levi R, Fahlström M. Preval ence of risk factors for cardiovascular dis easestratified by body mas index cat egories in pati ents with wheelchair-dependent parapl egia after spinal cord injury. J Rehabil Med. (2012) 44:440–3. doi: 10.2340/16501977-0964
5. Warner MB, Wilson D, Heller MO, Wood D, Worsley P, Mottram S, et al. Scapular kinematics in professional wheelchair tennis players. Clin Biomech. (2018) 53:7–13. doi: 10.1016/j.clinbiomech.2018.01.022
6. Burnham RS, May L, Nelson E, Steadward R, Reid DC. Shoulder pain in wheelchair athletes: The role of muscle imbalance. Am J Sports Med. (1993) 21:238–42. doi: 10.1177/036354659302100213
7. Chung WM, Yeung S, Wong AYL, Lam IF, Tse PTF, Daswani D, et al. Musculoskeletal injuries in elite able-bodied and wheelchair foil fencers-a pilot study. Clin J Sport Med. (2012) 22:278–80. doi: 10.1097/JSM.0b013e31824a577e
8. Akbar M, Brunner M, Ewerbeck V, Wiedenhöfer B, Grieser T, Bruckner T, et al. Do overhead sports increase risk for rotator cuff tears in wheelchair users? Arch Phys Med Rehabil. (2015) 96:484–8. doi: 10.1016/j.apmr.2014.09.032
9. Gescheit DT, Cormack SJ, Duffield R, Kovalchik S, Wood TO, Ornizzolo M, et al. multi-year injury epidemiology analysis of an elite national junior tennis program. J Sci Med Sport. (2019) 22:11–5. doi: 10.1016/j.jsams.2018.06.006
10. Silva RT, Gracitelli GC, Saccol MF, de Souza Laurino CF, Silva AC, Braga-Silva JL. Shoulder strength profile in elite junior tennis players: horizontal adduction and abduction isokinetic evaluation. Br J Sports Med. (2006) 40:513–7. doi: 10.1136/bjsm.2005.023408
11. Churton E, Keogh JWL. Constraints influencing sports wheelchair propulsion performance and injury risk. BMC Sports Sci Med Rehabil. (2013) 5:1. doi: 10.1186/2052-1847-5-3
12. Van Drongelen S, Van Der Woude LHV, Janssen TW, Angenot EL, Chadwick EK, Veeger HEJ. Mechanical load on the upper extremity during wheelchair activities. Arch Phys Med Rehabil. (2005) 86:1214–20. doi: 10.1016/j.apmr.2004.09.023
13. Briley SJ, Vegter RJK, Goosey-Tolfrey VL, Mason BS. Scapular kinematic variability during wheelchair propulsion is associated with shoulder pain in wheelchair users. J Biomech. (2020) 113:110099. doi: 10.1016/j.jbiomech.2020.110099
14. Ballinger DA, Rintala DH, Hart KA. The relation of shoulder pain and range-of-motion problems to functional limitations, disability, and perceived health of men with spinal cord injury: a multifaceted longitudinal study. Arch Phys Med Rehabil. (2000) 81:1575–81. doi: 10.1053/apmr.2000.18216
15. Van Der Hoeven H, Kibler WB. Shoulder injuries in tennis players. Br J Sports Med. (2006) 40:435–40. doi: 10.1136/bjsm.2005.023218
16. Sánchez-Pay A, Torres-Luque G, Sanz-Rivas D. Activity patterns in male and female wheelchair tennis matches. Kinesiology. (2017) 49:41–6. doi: 10.26582/k.49.1.10
17. Chung KC, Lark ME. Upper Extremity Injuries in Tennis Players: Diagnosis, Treatment, and Management. Hand Clin. (2017) 33:175–86. doi: 10.1016/j.hcl.2016.08.009
18. Jeon IH, Kochhar H, Lee JM, Kyung HS, Min WK, Cho HS, et al. Ultrasonographic Evaluation of the Shoulder in Elite Wheelchair Tennis Players. J Sport Rehabil. (2010) 19:161–72. doi: 10.1123/jsr.19.2.161
19. Matsuwaka ST, Latzka EW. Summer adaptive sports technology, equipment, and injuries. Sport Med Anrthrosc Rev. (2019) 27:48–55. doi: 10.1097/JSA.0000000000000231
20. Goosey-Tolfrey VL, Moss AD. Wheelchair velocity of tennis players during propulsion with and without the use of racquets. Adapt Phys Act Q. (2005) 22:291–301. doi: 10.1123/apaq.22.3.291
21. De Groot S, Bos F, Koopman J, Hoekstra AE, Vegter RJK. Effect of holding a racket on propulsion technique of wheelchair tennis players. Scand J Med Sci Sport. (2017) 27:918–24. doi: 10.1111/sms.12701
22. Heyward OW, Vegter RJK, De Groot S, Van der Woude LHV. Shoulder complaints in wheelchair athletes: a systematic review. PLoS ONE. (2017) 12:e0188410. doi: 10.1371/journal.pone.0188410
23. Fairbairn JR, Bliven KCH. Incidence of shoulder injury in elite wheelchair athletes differ between sports: a critically appraised topic. J Sport Rehabil. (2019) 28:294–8. doi: 10.1123/jsr.2017-0360
24. Reid M, Elliott B, Alderson J. Shoulder joint kinetics of the elite wheelchair tennis serve. Br J Sports Med. (2007) 41:739–44. doi: 10.1136/bjsm.2007.036145
25. Aytar A, Zeybek A, Pekyavas NO, Tigli AA, Ergun N. Scapular resting position, shoulder pain and function in disabled athletes. Prosthet Orthot Int. (2015) 39:390–6. doi: 10.1177/0309364614534295
26. Kekelekis A, Nikolaidis PT, Moore IS, Rosemann T, Knechtle B. Risk factors for upper limb injury in tennis players: a systematic review. Int J Environ Res Public Health. (2020) 17:2744. doi: 10.3390/ijerph17082744
27. Webster MJ, Morris ME, Galna B. Shoulder pain in water polo: a systematic review of the literature. J Sci Med Sport. (2009) 12:3–11. doi: 10.1016/j.jsams.2007.05.014
28. Hoozemans MJM, Van Der Beek AJ, Frings-Dresen MHW, Van Dijk FH, Van der Woude LHV. Pushing and pulling in relation to musculoskeletal disorders: A review of risk factors. Ergonomics. (1998) 41:757–81. doi: 10.1080/001401398186621
29. Winkel J, Mathiassen SE. Assessment of physical work load in epidemiologic studies: concepts, issues and operational considerations. Ergonomics. (1994) 37:979–88. doi: 10.1080/00140139408963711
30. Johansson FR, Skillgate E, Adolfsson A, Jenner G, DeBri E, Swärdh L, et al. Asymptomatic Elite Adolescent Tennis Players' Signs of Tendinosis in Their Dominant Shoulder Compared With Their Nondominant Shoulder. J Athl Train. (2015) 50:1299–305. doi: 10.4085/1062-6050-51.1.07
31. You BC, Lee WJ, Lee SH, Jang S, Lee HS. Shoulder disease patterns of the wheelchair athletes of table-tennis and archery: a pilot study. Ann Rehabil Med. (2016) 40:702–9. doi: 10.5535/arm.2016.40.4.702
32. Gillet B, Begon M, Diger M, Berger-Vachon C, Rogowski I. Shoulder range of motion and strength in young competitive tennis players with and without history of shoulder problems. Phys Ther Sport. (2018) 31:22–8. doi: 10.1016/j.ptsp.2018.01.005
33. Marcondes FB, de Jesus JF, Bryk FF, de Vasconcelos RA, Fukuda TY. Posterior shoulder tightness and rotator cuff strength assessments in painful shoulders of amateur tennis players. Braz J Phys Ther. (2013) 17:185–94. doi: 10.1590/S1413-35552012005000079
34. Moreno-Pérez V, Elvira JLL, Fernandez-Fernandez J, Vera-Garcia FJ. A comparative study of passive shoulder rotation range of motion, isometric rotation strength and serve speed between elite tennis players with and without history of shoulder pain. Int J Sports Phys Ther. (2018) 13:39–49. doi: 10.26603/ijspt20180039
35. Moon H, Park S, Kim A, Jang J. Characteristics of upper limb muscular strength in male wheelchair tennis players. J Exerc Rehabil. (2013) 9:375–80. doi: 10.12965/jer.130051
36. Bernard PLL, Codine P, Minier J. Isokinetic shoulder rotator muscles in wheelchair athletes. Spinal Cord. (2004) 42:222–9. doi: 10.1038/sj.sc.3101556
37. Mason BS, Vegter RJK, Paulson TAW, Morrissey D, van der Scheer JW, Goosey-Tolfrey VL. Bilateral scapular kinematics, asymmetries and shoulder pain in wheelchair athletes. Gait Posture. (2018) 65:151–6. doi: 10.1016/j.gaitpost.2018.07.170
38. Martin C, Bideau B, Bideau N, Nicolas G, Delamarche P, Kulpa R. Energy flow analysis during the tennis serve: comparison between injured and noninjured tennis players. Am J Sports Med. (2014) 42:2751–60. doi: 10.1177/0363546514547173
39. Touzard P, Kulpa R, Bideau B, Montalvan B, Martin C. Biomechanical analysis of the “waiter's serve” on upper limb loads in young elite tennis players. Eur J Sport Sci. (2019) 19:765–73. doi: 10.1080/17461391.2018.1539527
40. Moreno-Pérez V, Moreside J, Barbado D, Vera-Garcia FJ. Comparison of shoulder rotation range of motion in professional tennis players with and without history of shoulder pain. Man Ther. (2015) 20:313–8. doi: 10.1016/j.math.2014.10.008
41. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. (1998) 52:377–84. doi: 10.1136/jech.52.6.377
42. Lädermann A, Chagué S, Kolo FC, Charbonnier C. Kinematics of the shoulder joint in tennis players. J Sci Med Sport. (2016) 19:56–63. doi: 10.1016/j.jsams.2014.11.009
43. Martin C, Kulpa R, Ropars M, Delamarche P, Bideau B. Identification of temporal pathomechanical factors during the tennis serve. Med Sci Sports Exerc. (2013) 45:2113–9. doi: 10.1249/MSS.0b013e318299ae3b
44. Maquirriain J, Ghisi JP, Amato S. Is tennis a predisposing factor for degenerative shoulder disease? A controlled study in former elite players. Br J Sports Med. (2006) 40:447–50. doi: 10.1136/bjsm.2005.023382
45. Martin C, Kulpa R, Ezanno F, Delamarche P, Bideau B. Influence of playing a prolonged tennis match on shoulder internal range of motion. Am J Sports Med. (2016) 44:2147–51. doi: 10.1177/0363546516645542
46. Martin C, Bideau B, Ropars M, Delamarche P, Kulpa R. Upper limb joint kinetic analysis during tennis serve: assessment of competitive level on efficiency and injury risks. Scand J Med Sci Sports. (2014) 24:700–7. doi: 10.1111/sms.12043
47. Rich RL, Struminger AH, Tucker WS, Munkasy BA, Joyner AB, Buckley TA. Scapular upward-rotation deficits after acute fatigue in tennis players. J Athl Train. (2016) 51:474–9. doi: 10.4085/1062-6050-51.7.05
48. Hennig EM. Influence of racket properties on injuries and performance in tennis. Exerc Sport Sci Rev. (2007) 35:62–6. doi: 10.1249/JES.0b013e31803ec43e
49. Rogowski I, Creveaux T, Cheze L, Dumas R. Scapulothoracic kinematics during tennis forehand drive. Sport Biomech. (2014) 13:166–75. doi: 10.1080/14763141.2014.885073
50. Hjelm N, Werner S, Renstrom P. Injury profile in junior tennis players: a prospective two year study. Knee Surg Sport Traumatol Arthrosc. (2010) 18:845–50. doi: 10.1007/s00167-010-1094-4
51. Sein ML, Walton J, Linklater J, Appleyard R, Kirkbride B, Kuah D, et al. Shoulder pain in elite swimmers: Primarily due to swim-volume-induced supraspinatus tendinopathy. Br J Sports Med. (2010) 44:105–13. doi: 10.1136/bjsm.2008.047282
52. Hbert LJ, Moffet H, McFadyen BJ, Dionne CE. Scapular behavior in shoulder impingement syndrome. Arch Phys Med Rehabil. (2002) 83:60–9. doi: 10.1053/apmr.2002.27471
53. De Groot S, Bos F, Koopman J, Hoekstra AE, Vegter RJK. The effect of a novel square-profile hand rim on propulsion technique of wheelchair tennis players. Appl Ergon. (2018) 71:38–44. doi: 10.1016/j.apergo.2018.04.001
54. Rietveld T, Vegter RJK, Van der Woude LHV, De Groot S. The interaction between wheelchair configuration and wheeling performance in wheelchair tennis: a narrative review. Sport Biomech. (2021) 1−22. doi: 10.1080/14763141.2020.1840617
Keywords: wheelchairs, shoulder injuries, physical activity, wheelchair tennis, adapted sports
Citation: Mayrhuber L, Rietveld T, de Vries W, van der Woude LHV, de Groot S and Vegter RJK (2022) A Scoping Review on Shoulder Injuries of Wheelchair Tennis Players: Potential Risk-Factors and Musculoskeletal Adaptations. Front. Rehabilit. Sci. 3:862233. doi: 10.3389/fresc.2022.862233
Received: 25 January 2022; Accepted: 07 March 2022;
Published: 07 April 2022.
Edited by:
Areerat Suputtitada, Chulalongkorn University, ThailandReviewed by:
Massimiliano Murgia, G. Brotzu Hospital, ItalyTugba Kuru Çolak, Marmara University, Turkey
Copyright © 2022 Mayrhuber, Rietveld, de Vries, van der Woude, de Groot and Vegter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thomas Rietveld, dC5yaWV0dmVsZEB1bWNnLm5s
†These authors have contributed equally to this work and share first authorship
 Laura Mayrhuber
Laura Mayrhuber Thomas Rietveld
Thomas Rietveld Wiebe de Vries
Wiebe de Vries Lucas H. V. van der Woude
Lucas H. V. van der Woude Sonja de Groot
Sonja de Groot Riemer J. K. Vegter
Riemer J. K. Vegter