- 1Faculty of Health and Life Sciences, School of Life Sciences, Coventry University, Coventry, United Kingdom
- 2Department of Respiratory Medicine, University Hospitals of Leicester NHS Trust, Leicester, United Kingdom
- 3Centre for Exercise and Rehabilitation Science, University Hospitals of Leicester NHS Trust, Leicester, United Kingdom
- 4Faculty of Medicine and Health Sciences, University of Nottingham, Nottingham, United Kingdom
Background: Pulmonary rehabilitation (PR) is a highly effective intervention for individuals with chronic obstructive pulmonary disease (COPD). Physical activity (PA) has been shown to increase after a centre-based programme, yet it is not clear if a home-based programme can offer the same benefit. This study aimed to evaluate the effect of home-based PR compared with the centre-based PR on the PA levels post 7 weeks of PR and 6 months follow-up.
Method: In this study, 51 participants with COPD, of them, 36 (71%) men completed physical activity monitoring with a SenseWear Armband, at three time points (baseline, 7 weeks, and 6 months). The participants were randomly assigned to either centre-based supervised PR (n = 25; 69 ± 6 years; FEV1 55 ± 20% predicted) or home-based PR (n = 26; 68 ± 7 years; FEV1 42 ± 19% predicted) programmes lasting 7 weeks. The home-based programme includes one hospital visit, a self-management manual, and two telephone calls. The PA was measured as step count, time in moderate PA (3–6 metabolic equivalent of tasks [METs]) in bouts of more than 10 min and sedentary time (<2 METs).
Results: Home-based PR increased step count significantly more than the centre-based PR after 7 weeks (mean difference 1,463 steps: 95% CI 280–2,645, p = 0.02). There was no difference in time spent in moderate PA was observed (mean difference 62 min: 95% CI −56 to 248, p = 0.24). Sedentary behaviour was also significantly different between the centre and home-based groups. The home group spent 52 min less time sedentary compared with the centre-based (CI −106 to 2, p = 0.039). However, after 6 months, the step count and time spent in moderate PA returned to baseline in both the groups.
Conclusion: This study provides an important insight into the role of home-based PR which has the potential to be offered as an alternative to the centre-based PR. Understanding who may best respond from the centre or home-based PR warrants further exploration and how to maintain these initial benefits for the long-term.
Trial Registry: ISRCTN: No.: ISRCTN81189044; URL: isrctn.com.
Introduction
The international guidelines support the effectiveness of pulmonary rehabilitation (PR) in the treatment and management of patients with chronic obstructive pulmonary disease (COPD) (1). However, few patients would benefit from receiving such treatment (2). Many individuals are unwilling or unable to attend the hospital-based programmes (3) and high dropout and low adherence rates (2) highlights the need for alternative models to the centre-based PR.
Physical activity (PA) is an important clinical outcome and has been associated with improved dyspnoea (4), exercise performance, and reduced muscle weakness (5), quality of life (6), mortality (7) and hospital admissions (8). Despite PR being highly effective at improving exercise performance (6), it has limited effect on how much patients with PA daily perform (9). Those studies which investigated PA post PR showed some improvement in the terms of step count, activity counts, and reduced sedentary time (10), whilst others did not find any significant difference (11). The challenge remains how best to change the behaviour of patients to be more physically active and maintain such behaviour long-term.
There is growing evidence that home-based PR in patients with COPD can be delivered as an alternative to the centre-based PR programme at increasing quality of life of the patients with COPD (12–16). Home-based programmes have the advantage of being easier to access. However, little is known about the impact of home-based PR on physical activity levels. Hollands et al. (15) study of home- vs. centre-based PR did show a short-term increase in moderate to vigorous physical activity (MVPA). Although 1-year later, both the groups had declined to the baseline levels. Another study also showed that home-based PR could increase daily step counts (17). However, there is a lack of more descriptive studies comparing the centre-based and home-based PR. As opposed to centre-based PR, the patients in their own home environment could more directly apply the programmes to activities of daily living and enhance the overall PA levels.
We have previously described a non-inferiority randomised trial comparing home-based rehabilitation facilitated by a manual (SPACE for COPD) vs. centre-based PR (14). A subgroup of patients from this trial was assessed for physical activity and here we describe the findings. We hypothesise that the home-based PR can effectively increase the daily physical activity in patients with COPD. This study aimed to assess the activity after 7 weeks of intervention and 6 months following up with either the centre- or home-based PR. We looked at daily step count, time spent in bouts, and time spent sedentary.
Materials and Methods
Study Design
This was a single blinded randomised controlled trial (RCT). We compared centre-based PR with a home-based PR programmed supported with the SPACE for COPD manual at 7 weeks and 6 months follow-up. The study took place between November 2007 and July 2012. All the participants gave written informed consent, and ethical approval for the study was granted by Leicestershire, Northamptonshire, and Rutland Regional Ethics Committee, reference 07/Q2501/6. Trial registration: ISRCTN81189044.
Participants
The main trial recruited participants who were referred to PR, had a medical research council dyspnoea scale (MRC) between 2 and 5 and a minimum age of 18 years. The participants excluded from the study were those who would routinely miss the PR if they had significant neurological or locomotive disorders or unstable psychiatric history, and those who had participated in PR in the previous 12 months. In addition, those with poor English language skills were also excluded due to the manual only being available in English. The participants were randomised using the random block-sized sealed envelopes, into either conventional centre-based PR or home-based PR supported by the SPACE for COPD manual. The participants in the centre-based PR group enrolled on the two times weekly supervised exercise and education programme over 7 weeks. Those in the home-based group had an initial introductory session at the hospital led by a healthcare professional trained in motivational interviewing. This session introduced them to the manual and instructed them on how to complete their exercise. This group also received two telephone calls at 2 and 4 weeks to assess the progress, support, and motivation. It was anticipated that it would take to 7 weeks to progress through the SPACE for COPD manual, although it was their decision to keep supporting lifelong lifestyle change.
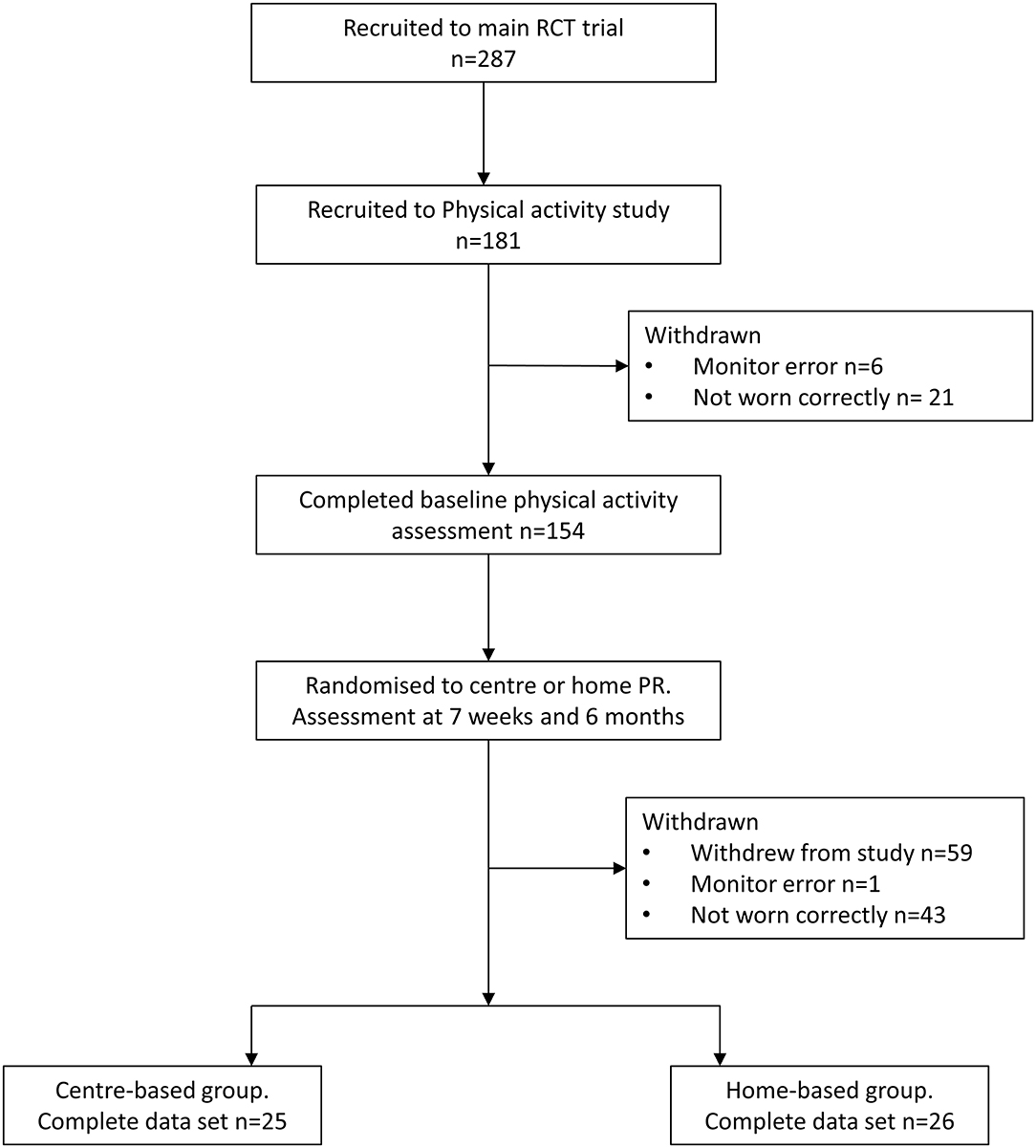
As part of the larger RCT comparing, the centre-, and home-based PR data were collected on the physical activity levels in a subgroup of the participants. Due to the limited number of activity monitors, the participants were recruited for this study based on the monitor availability. In total, 287 participants consented to the main trial and 154 provided the baseline physical activity data. The complete datasets, including baseline, 7 weeks, and 6 months, were available from 51 participants (Table 1). The flow of participants through the trial is presented in Figure 1.
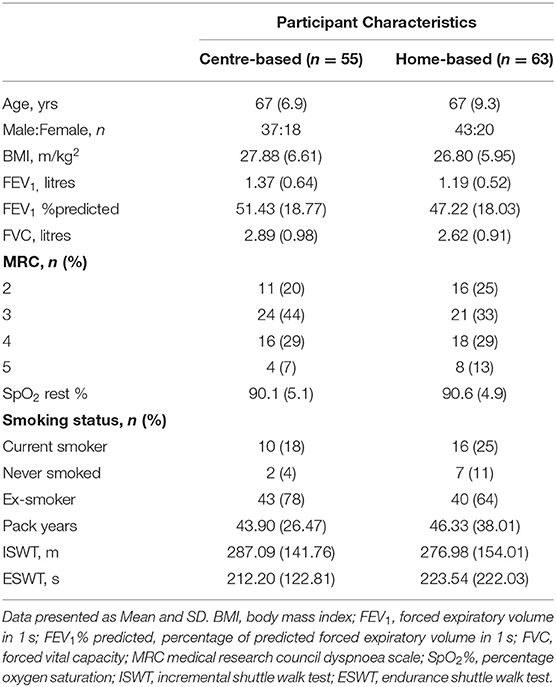
Table 1. Mean (SD) characteristics of the centre-based and home-based groups who participated in the physical activity monitoring study.
Outcome Measures and Intervention
The physical activity was measured using the SenseWear armband (SWM; BodyMedia, Pittsburgh, PA, USA) and the participants were asked to wear the monitor for 5 days (including 2 weekend days) for all waking hours, apart from whilst bathing, showering, or swimming. The data from the SWM were downloaded using the InnerView™ software. The outcome measures at 7 weeks and 6 months were daily stepping count, time spent in moderate physical activity (>3 metabolic equivalent of tasks [METs]) in ≥10 min bouts, and time spent sedentary. The outcome measures at the baseline level were step count and time in moderate physical activity (>3 METs) in ≥10 min bouts.
The data were excluded from the analysis for the following reasons: if an error message occurred when downloading the SWM data, days where the data were <12 h, or if the monitor was worn for fewer than 3 days.
Data Analysis
The data were analysed for normality. The paired t-test was used to analyse within the group differences from the baseline to 7 weeks and an independent t-test to determine the differences between the groups. Between group differences over time to 6 months were analysed using an ANOVA. The data processing and analysis were undertaken using IBM SPSS statistics 20.
Results
In this study, 154 patients took part in baseline PA monitoring, 59 withdrew from the main trial, and the findings from 43 monitors were discarded as they were not worn for at least 12 h on at least 3 days. One set of data was discarded due to an error message on the SWM. This left 51 subjects with a minimum of 3 days of 12 h data at each of the time points (baseline, 7 weeks, and 6 months). Therefore, 25 patients were analysed in the centre-based group, 26 patients were analysed in the home-based group. A significant difference in the percentage of predicted FEV1 was detected at the baseline between the groups, but no other significant differences (Table 1).
Intervention Effects
The results show that at 7 weeks, there were significant differences between the centre-based and home-based groups in the number of steps and time spent over 3 METs in bouts (Table 2). With a between-group difference of 1,463 steps (95% CI 280–2,645, p = 0.020) and 32 min longer time spent over 3 METS in the bouts (95% CI 11–54, p = 0.006), respectively, in favour of the home-based group. Within a home-based group, step count and time over 3 METs in the bouts increased significantly from the baseline by 1,074 steps (95% CI 289–1,708, p < 0.008) and by 28 min (95% CI 9–48, p < 0.008), respectively. No significant change was found in the PR group (Figures 2A,B). However, at 6 months, there was no significant difference between the centre-based group and home-based group even though time over 3 METs in the bouts remained improved in the home-based group. At 6 months, the home-based group spent 15 min more in time over 3 METs in the bouts (p = 0.037) whilst centre-based patients only 5 min (Figure 2B). In terms of step count, intergroup difference of 185 steps (95% CI 1,004–1,374) was not significant, and it went back to baseline within the groups (Figure 2B).
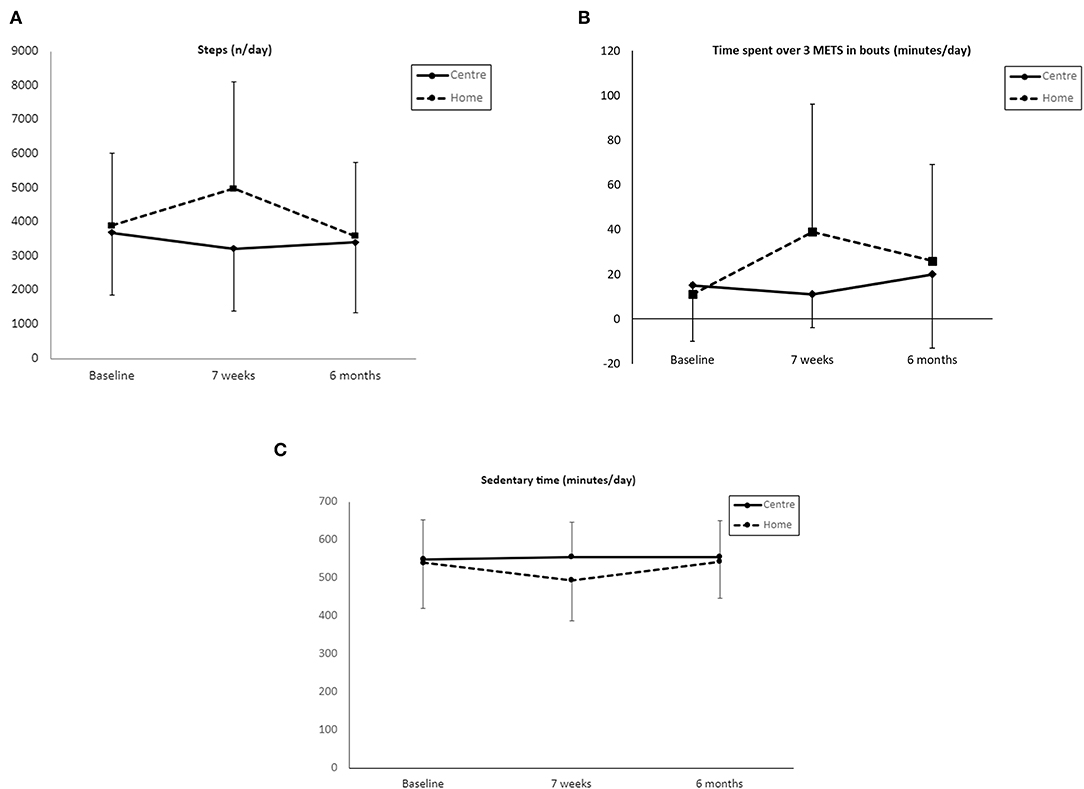
Figure 2. Baseline, after 7-week intervention and 6 months mean scores (± SD) in, (A) step count; (B) time spent over 3 METS in bouts; (C) sedentary time.
Sedentary behaviour was also significantly different between the centre and home-based groups. The home group spent 52 min less time sedentary compared with the centre-based (95% CI −106 to 2, p = 0.039; Figure 2C). Within group difference following home-based PR at 7 weeks was 46 min less time spent sedentary (95% CI −86 to −11, p = 0.013), whilst centre-based PR spent only 6 min less time sedentary. Time spent sedentary was replaced by light PA and MVPA activity at 7 weeks. However, despite this numerical improvement, the latter two parameters did not reach statistical significance.
At 6 months, both the centre-and home-based groups' sedentary behaviour went back to the baseline and the intergroup difference was not significant.
Discussion
There is a paucity of data exploring the home-based PR on PA. Compared with the previous studies, this data demonstrates the importance of group differences. It identified that home based programme was superior to usual centre-based PR at 7 weeks for increasing the step count exceeding the MCID proposed by Demeyer et al. (18) of 600–1,100 steps, time spent over 3 METs and reducing sedentary time. However, at 6 months postintervention, there was no significant difference in change between the two groups, even though the home-based patients with PR had significantly increased time spent over 3 METs and reduced sedentary time whilst the centre-based patients with PR did not. This suggests that the highly structured workbook and support from healthcare practitioners can produce a meaningful change.
We did not detect any improvement in the physical activity levels in the PR group. There is variability in the reports from other studies with an overall small increase in PA. Some authors suggested a longer time is required (9). PR focuses on the completion of bouts of walking, thus it is surprising that the patients did not improve on this aspect. On the other hand, it is possible that those in the PR group abdicated responsibility for their health to the healthcare team and relied purely on their supervised exercise sessions. Therefore, they did not perform more exercise at home.
At 6 months after the centre-based and home-based PR activity levels returned to baseline. The lack of long-term effects post PR was an expected finding: it is an established problem (19), and this study shows that home-based PR is not superior in this respect. We anticipated that within their home environment, the patients were more likely to maintain exercise behaviour. On the other hand, even though the differences were not significant between the two programmes, 6 months post home-based PR time spent over 3 METS was significantly higher compared with the baseline. This positive trend could be explored further. The optimal duration of the programmes is still not clear (6). It has been previously demonstrated that a 6-month programme is required to alter the free-living activity levels of the patients (10).
The focus of PR has conventionally been to improve exercise capacity (1, 20). However, there is an increasing focus on PA as an outcome measure for PR which depend on how PA is reported may not directly align with the aims of PR. PR has the explicit aim of increasing MVPA, which may not be reflected in steps. It is interesting that the home-based intervention seems to produce greater improvements in both the MVPA and steps at 7 weeks. In addition, the intervention produced important changes in the exercise capacity and health-related quality of life exceeding reported MCIDs for the Chronic Respiratory Disease Questionnaire (CRQ)-dyspnoea score and the endurance shuttle walk test (ESWT), suggesting an effective alternative to conventional PR.
Effing reported that their home-based trial which measured PA showed that over 11-month intervention, there was a mean improvement of 1,190 steps per day (17). This is comparable with our home-based programme after 7 weeks. In a similar study, Holland et al. (15) demonstrated an 8-week improvement in the time spent in MVPA, with no differences identified in any other physical activity parameter and no difference between the groups. Compare with our data that found an increase in step count in the home-based group of 1,074 steps, which was significantly higher than the centre-based group and met the MCID (18). The PA data from our trial are more descriptive in determining the patterns and intensities of PA whilst step count provides limited information and therefore makes it difficult to determine if the guidelines have been met. Sedentary behaviour is a problem of its own (21), thus the reduction in time sedentary is an important achievement too. It was replaced by light physical activity which might be a more realistic target in the patients with COPD rather than vigorous activity. Although at 6 months overall PA levels have returned to the baseline, an increase in time spent in continuous bouts of the exercise was maintained.
The baseline data revealed significant differences in the bout and non-bout activity: when measured in bouts percentage who met guidelines drops to 18% from 67%. However, Donaire-Gonzalez (22) in a study, found that 61% of the patients fulfilled the recommended PA guidelines by performing moderate to vigorous (METs >2.6 and >3) activity in bouts. The discrepancy between our findings and Donaire-Gonzalez is difficult to explain since our study populations were similar in age and disease severity. Spanish population performs the same amount of exercise as the British population (23). It could be explained by seasonal differences as described previously (24). With more severe disease, the patients reduced duration and frequency of bouts (22).
The main limitation of this study is a limited sample size. Regarding the baseline PA analysis, data from the current study may not truly reflect whether guidelines have been met as SWM was not worn for a full week thus it might be difficult to assess compliance with the guidelines which are set for 5 days. The data were collected only for 12 h a day which might have missed periods of significant activity. The participants in the home group had a significantly lower FEV1% predicted which may also be considered a limitation to the study.
Conclusion
This study provides an important insight into a structured home-based PR programme effect on the physical activity levels. It is an important finding since physical activity plays a key role in the management of COPD. The challenge remains in sustaining positive PA and exercise behaviour in this population.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Leicestershire, Northamptonshire, and Rutland Regional Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
EH, LS, and SS designed the study and intervention. EH, LS, and KM completed the intervention and data collection. EH and CN analysed the data. EH, JR, and SS wrote the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to acknowledge the pulmonary rehabilitation team at Glenfield Hospital, Leicester NHS trust who recruited the participants. We are grateful to all the participants for their involvement in this study.
References
1. Rochester CL, Vogiatzis I, Holland AE, Lareau SC, Marciniuk DD, Puhan MA, et al. ATS/ERS task force on policy in pulmonary rehabilitation. An official american thoracic society/european respiratory society policy statement: enhancing implementation, use, and delivery of pulmonary rehabilitation. Am J Respir Crit Care Med. (2015) 192:1373–86. doi: 10.1164/rccm.201510-1966ST
2. Steiner M, McMillan V, Lowe D, Holzhauer-Barrie J, Mortier K, Riordan J, et al. Pulmonary Rehabilitation: An Exercise in Improvement. National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme: Clinical and Organisational Audits of Pulmonary Rehabilitation Services in England and Wales 2017. National Report. London: RCP (2018).
3. Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chronic Respir Dis. (2011) 2011:89–99. doi: 10.1177/1479972310393756
4. Watz H, Waschki B, Meyer T, Magnussen H. 'Physical activity in patients with COPD'. Europ Respir J. (2009) 33:262–72. doi: 10.1183/09031936.00024608
5. Pitta F, Troosters T, Spruit MA, Probst VS, Decramer M, Gosselink R. 'Characteristics of physical activities in daily life in chronic obstructive pulmonary disease'. Am J Respir Critic Care Med. (2005) 171:972–7. doi: 10.1164/rccm.200407-855OC
6. McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. (2015) CD003793. doi: 10.1002/14651858.CD003793.pub3
7. Waschki B, Kirsten A, Holz O, Müller KC, Meyer T, Watz H, et al. Physical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort study. Chest. (2011) 140:331–42. doi: 10.1378/chest.10-2521
8. Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Antó JM. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax. (2006) 61:772–8. doi: 10.1136/thx.2006.060145
9. Cindy Ng LW, Mackney J, Jenkins S, Hill K. Does exercise training change physical activity in people with COPD? A systematic review and meta-analysis. Chron. Respir. Dis. (2012) 9:17–26. doi: 10.1177/1479972311430335
10. Pitta F, Troosters T, Probst VS, Langer D, Decramer M, Gosselink R. Are patients with COPD more active after pulmonary rehabilitation? Chest. (2008) 134:273–80. doi: 10.1378/chest.07-2655
11. Egan C, Deering BM, Blake C, Fullen BM, McCormack NM, Spruit MA, et al. Short term and long term effects of pulmonary rehabilitation on physical activity in COPD. Respir. Med. (2012) 106:1671–9. doi: 10.1016/j.rmed.2012.08.016
12. Mitchell KE, Johnson-Warrington V, Apps LD, Bankart J, Sewell L, Williams JE, et al. A self-management programme for COPD: a randomised controlled trial. Eur Respir J. (2014) 44:1538–47. doi: 10.1183/09031936.00047814
13. Bourbeau J. Making pulmonary rehabilitation a success in COPD. Swiss Med Wkly. (2010) 140:w13067. doi: 10.4414/smw.2010.13067
14. Horton EJ, Mitchell KE, Johnson-Warrington V, Apps LD, Sewell L, Morgan M, et al. Comparison of a structured home-based rehabilitation programme with conventional supervised pulmonary rehabilitation: a randomised non-inferiority trial. Thorax. (2018) 73:29–36. doi: 10.1136/thoraxjnl-2016-208506
15. Holland AE, Mahal A, Hill CJ, Lee AL, Burge AT, Cox NS, et al. Home-based rehabilitation for COPD using minimal resources: a randomised, controlled equivalence trial. Thorax. (2017) 72:57–65. doi: 10.1136/thoraxjnl-2016-208514
16. Hansen H, Bieler T, Beyer N, Kallemose T, Wilcke JT, Østergaard LM, et al. Supervised pulmonary tele-rehabilitation versus pulmonary rehabilitation in severe COPD: a randomised multicentre trial. Thorax. (2020) 75:413–21. doi: 10.1136/thoraxjnl-2019-214246
17. Effing T, Zielhuis G, Kerstjens H, van der Valk P, van der Palen J. Community based physiotherapeutic exercise in COPD self-management: a randomised controlled trial. Respir Med. (2011) 105:418–26. doi: 10.1016/j.rmed.2010.09.017
18. Demeyer H, Burtin C, Hornikx M, Camillo CA, Van Remoortel H, Langer D, et al. The minimal important difference in physical activity in patients with COPD. PLoS ONE. (2016) 11:e0154587. doi: 10.1371/journal.pone.0154587
19. Griffiths TL, Burr ML, Campbell IA, Lewis-Jenkins V, Mullins J, Shiels K, et al. Results at 1 year of outpatient multidisciplinary pulmonary rehabilitation: a randomised controlled trial. Lancet. (2000) 355:362–8. doi: 10.1016/S0140-6736(99)07042-7
20. Bolton CE, Bevan-Smith E, Blakey JD, Crowe P, Elkin SL, Garrod R, et al. 'British thoracic society guideline on pulmonary rehabilitation in adults'. Thorax. (2013) 68(Suppl. 2):ii1–30. doi: 10.1136/thoraxjnl-2013-203809
21. Hill K, Gardiner PA, Cavalheri V, Jenkins SC, Healy GN. Physical activity and sedentary behaviour: applying lessons to chronic obstructive pulmonary disease. Intern Med J. (2015) 45:474–82. doi: 10.1111/imj.12570
22. Donaire-Gonzalez D, Gimeno-Santos E, Balcells E, Rodríguez DA, Farrero E, de Batlle J, et al. Physical activity in COPD patients: patterns and bouts. Eur Respir J. (2013) 42:993–1002. doi: 10.1183/09031936.00101512
23. British Heart Foundation (2012). Physical Activity Statistics 2012: British Heart Foundation Health Promotion Research Group.
Keywords: pulmonary rehabilitation, physical activity, chronic obstructive pulmonary disease (COPD), exercise, step count, sedentary time
Citation: Horton EJ, Ruksenaite J, Mitchell K, Sewell L, Newby C and Singh SJ (2021) A Comparison of Physical Activity Between Home-Based and Centre-Based Pulmonary Rehabilitation: A Randomised Controlled Secondary Analysis. Front. Rehabilit. Sci. 2:743441. doi: 10.3389/fresc.2021.743441
Received: 18 July 2021; Accepted: 22 September 2021;
Published: 26 October 2021.
Edited by:
Guido Vagheggini, Azienda USL Toscana Nord Ovest, ItalyReviewed by:
Francesca Marzetti, University of Pisa, ItalyDewi Nurul Makhabah, Sebelas Maret University, Indonesia
Copyright © 2021 Horton, Ruksenaite, Mitchell, Sewell, Newby and Singh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elizabeth J. Horton, ZS5ob3J0b25AY292ZW50cnkuYWMudWs=
 Elizabeth J. Horton
Elizabeth J. Horton Justina Ruksenaite2
Justina Ruksenaite2 Louise Sewell
Louise Sewell Sally J. Singh
Sally J. Singh