- 1Department of Physical Therapy, Faculty of Allied Health Sciences, Thammasat University, Pathumthani, Thailand
- 2Research Unit of Physical Therapy in Respiratory and Cardiovascular Systems, Thammasat University, Pathumthani, Thailand
- 3Department of Internal Medicine, Faculty of Medicine, Thammasat University, Pathumthani, Thailand
Background: Chronic obstructive pulmonary disease (COPD) is a common, preventable, and treatable condition, characterized by persistent airflow limitation. Exercise training is a core component of pulmonary rehabilitation in people with COPD. Water-based exercise has been studied, but it remains unclear whether water-based exercise program leads to the improvement in respiratory function, muscle strength, balance ability, and exercise capacity. We aim to study the effect of an 8-week water-based exercise program on respiratory function, muscle strength, balance ability, and exercise capacity in people with COPD.
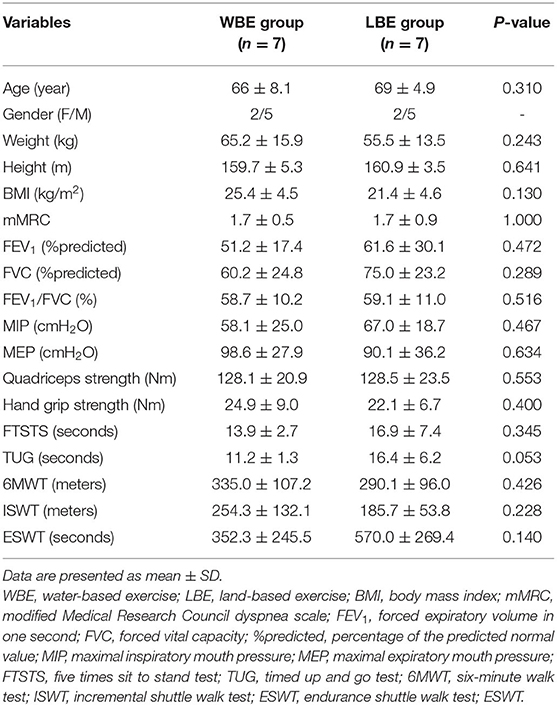
Methods: Fourteen stable COPD participants (FEV1 56.8 ± 24.6%pred) were recruited and randomized into a water-based exercise or a land-based exercise group. Both groups were trained for 8 weeks, two sessions per week. Pulmonary function, respiratory muscle strength, peripheral muscle strength, balance ability, exercise capacity [6-min walking test (6MWT), incremental shuttle walk test (ISWT), and endurance shuttle walk test (ESWT)] were assessed at baseline and at the end of the program. ANCOVA was used to conduct between-group comparisons of outcomes after adjusting for pre-intervention values.
Results: Baseline characteristics of participants were not significantly different between the two groups (p ≥ 0.05). After the 8-week training program, participants in the intervention group achieved larger gains in ESWT (Δ663.4 ± 279.5 vs. Δ45.4 ± 93.2 s, p = 0.001). In addition, maximal inspiratory pressure (MIP) was significantly increased more in the intervention group (Δ11.1 ± 7.8 vs. Δ1.1 ± 5.7 cmH2O, p = 0.026). However, no significant differences in pulmonary function, peripheral muscle strength, balance ability variables, 6MWD (p = 0.248), and ISWT (p = 0.506) were observed between the two groups.
Conclusions: The water-based exercise program could be recommended to the COPD rehabilitation program for improving the endurance exercise capacity and inspiratory muscle strength.
Clinical Trial Registration: www.thaiclinicaltrials.org, identifier: TCTR20210125005.
Introduction
The main types of NCDs are cardiovascular diseases (heart attacks and stroke), cancers, diabetes, and chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma) are responsible for most deaths worldwide (1). Chronic respiratory diseases constitute a public health problem that impose a substantial burden. Especially, chronic obstructive pulmonary disease (COPD) is a major cause of chronic morbidity and mortality. COPD is a common, preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases (1, 2). Dyspnea is the most notable exercise-limiting symptom of the disease, which leads to chronic avoidance of physical activities. As a result, low physical activity levels contribute to upper and lower limb muscle deconditioning and exercise capacity reduction, which impact negatively on health related quality of life (2, 3).
Pulmonary rehabilitation (PR) including exercise training, education, nutritional intervention, and psychosocial support is an integrated and standard care option for COPD patients (3, 4). It is the most effective non-pharmacological management to improve symptoms of dyspnea and fatigue, increase exercise capacity, improve health-related quality of life, and reduce hospital admissions (3–5). The most effective strategies for the rehabilitation of COPD is land-based exercise training. However, the general demographic of people with COPD referred to PR are of an older age, and a high proportion have physical comorbidity, such as musculoskeletal abnormalities, cerebrovascular disease, osteoarthritis, and obesity, which limit their ability to participate in land-based exercise training. There is a high drop-out rate to 66% from land-based exercise training. Therefore, performing land-based exercise training may considerably reduce the effectiveness and does not find significant differences when study in this training (6).
Even though water-based exercise has been studied (6–9), it remains unclear whether water-based exercise programs lead to an improvement in endurance exercise capacity, respiratory function, muscle strength, and balance ability. In a Cochrane review conducted in 2013, the authors concluded that there is limited quality evidence that water-based exercise training is safe and improves exercise capacity and quality of life in people with COPD immediately after training (7). Therefore, a comprehensive physical evaluation has been performed in this present study. We aimed to study the effect of an 8-week water-based exercise program on endurance exercise capacity, respiratory function, muscle strength, and balance ability in people with COPD. The second objective was to investigate the correlation between the change of primary outcome (endurance exercise capacity) and all secondary outcomes.
Materials and Methods
Study Design, Data Collection, and Randomization
Participants who had confirmed diagnosis of COPD according to the Global Initiative for Obstructive Lung Disease (GOLD) criteria, were in a stable phase age between 40 and 75 years old, and were referred for outpatient treatment at Thammasat university hospital were included in this study. The exclusion criteria were: Psychiatric disorders, cognitive disorders, progressive neurological or neuromuscular disorders, progressive musculoskeletal disorders, or severe orthopedic problems that impact in activity in daily life.
The participants gave written informed consent, answered the questionnaire, and gave personal data. This study was a randomized control trial with assessor blind (assessor and therapist would be different) due to the exercise interventions, it was not possible to blind the participants or therapist. Group allocation was performed by simple randomization using sealed opaque envelopes in random block sizes of four and six (order unknown to investigators) (10). They were divided into two groups: water-based exercise training and land-based exercise training (control group).
This study was approved by the Ethical Review Sub-Committee Board for Human Research Involving Sciences, Thammasat University, No.3 (COA No.110/2561). The clinical trial has been registered in Thai Clinical Trials Registry (the TCTR identification number is TCTR20210125005).
Measurement
Pulmonary function was assessed by spirometry using MicroLab MK8 (11). Maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) were registered at the mouth by an electronic pressure transducer (MicroRPM Micromedical, UK) (12). Peripheral muscle strength was assessed using hand-held dynamometer for quadriceps strength and hand grip dynamometer for hand grip strength (13). Postural balance was assessed by five time sits to stand (FTSTS) test and time up and go (TUG) (14). Exercise capacity was assessed by 6-min walk test (6MWT), incremental shuttle walk test (ISWT), and endurance exercise capacity was assessed by the endurance shuttle walk test (ESWT) following the recommendations of European Respiratory Society/American Thoracic Society (15, 16). The primary outcome was ESWT. The secondary outcomes were pulmonary function, respiratory muscle strength, peripheral muscle strength, postural balance, and exercise capacity. Participants have been assessed at baseline and the end of the program.
Intervention
Water-based exercise group was performed in a hydrotherapy pool with maximum of 12 participants per session under supervision, with the water temperature at 34 degree Celsius and the water level between the clavicle and xiphisternum for each participant. The exercise program was performed at moderate intensity, and before the exercise program participants were tested to find their blood pressure, respiratory rate, oxygen saturation, peak expiratory flow rate (PEFR), dyspnea and legs fatigue scale, according to modified borg scale for dyspnea, and perceived exertion at an intensity rating of three to five. Training intensity was measured three times during each exercise session. If the intensity reported was below three, participants were encouraged to increase their intensity or to add equipment to increase the resistance of the exercise program. For the land-based exercise group, at the beginning of the training course, the physiotherapist instructed participants about the correct exercise program as closely as with the water-based exercise group. Subjects in the land-based training group exercised on their own, but closely followed the instruction given at the beginning of the course and the exercise handbook. We followed up with the land-based training group by telephone call twice a week. Both training interventions were matched as closely as possible for training intensity, duration, muscles, and also the training progression. These protocols were modified from the study of McNamara et al. (8) (Table 1) and the training progression was adapted from Felcar et al. (17) (Table 2). Both groups were trained 60 min per session, 2 sessions per week for 8 weeks.
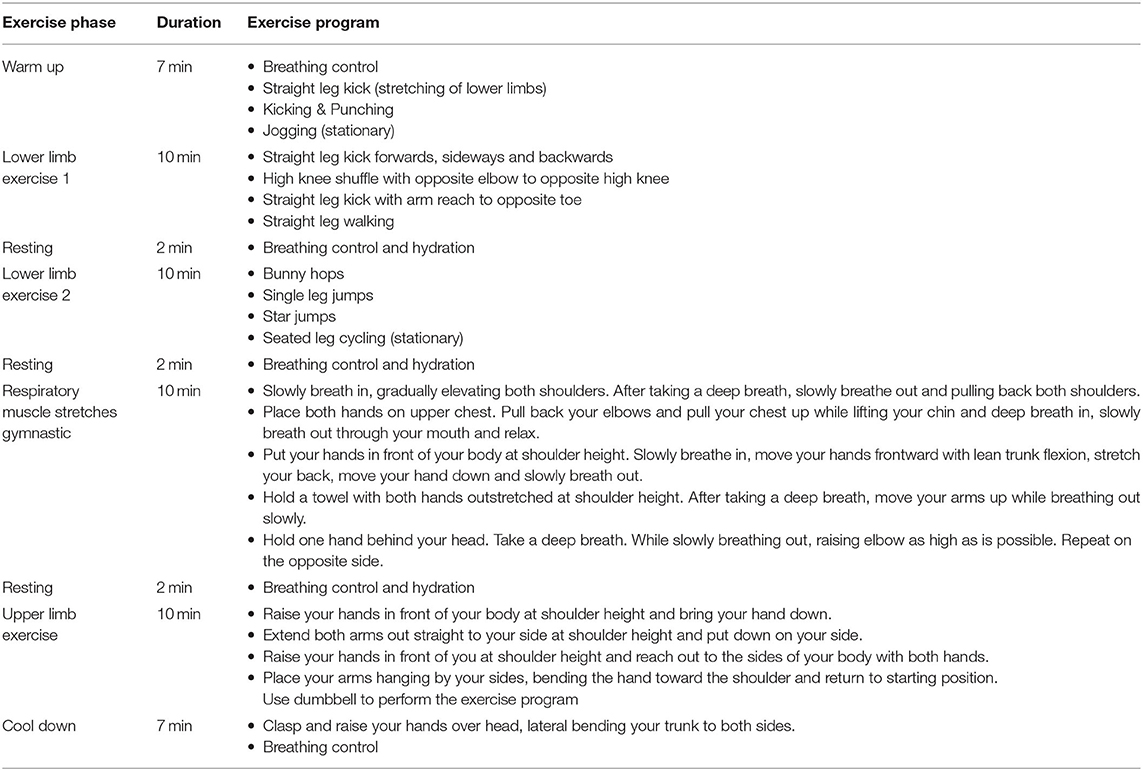
Table 1. Land-based and water-based exercise program (8).
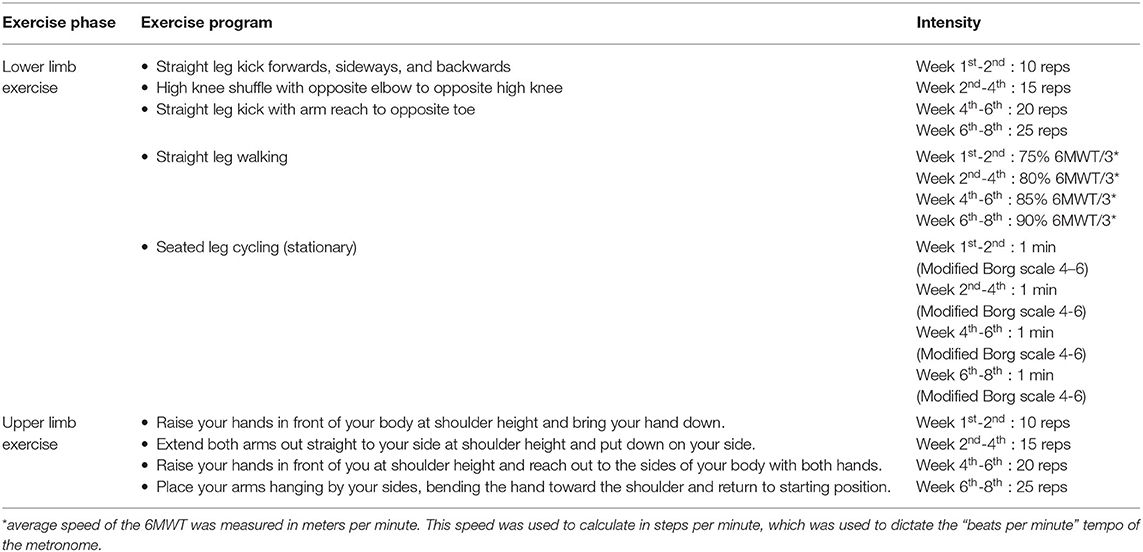
Table 2. Progression of exercise program for land-based and water-based exercise group (12).
Compliance with the training protocol was assessed by physiotherapist during the training sessions in the water-based exercise group and by telephone call in the land-based exercise group.
Statistical Analysis
Statistical analysis was performed using SPSS Version 21 and G-Power version 3.1.9.2 was used to calculate the sample size based on our pilot study and the study of McNamara et al. (8). To detect a minimally clinically important difference between groups of 203 m in the ESWT distance, with a degree of certainty (statistical power) of 80% and a risk for a type 1 error (α) <5%, a total of 14 participants (7 per group) were required to complete the study. Baseline data was verified using the descriptive statistics. Analysis of covariance (ANCOVA) was used to conduct between-group comparisons of outcomes. Pearson correlation was used to analyze the correlation between outcomes. Statistical significance was set as P < 0.05.
Results
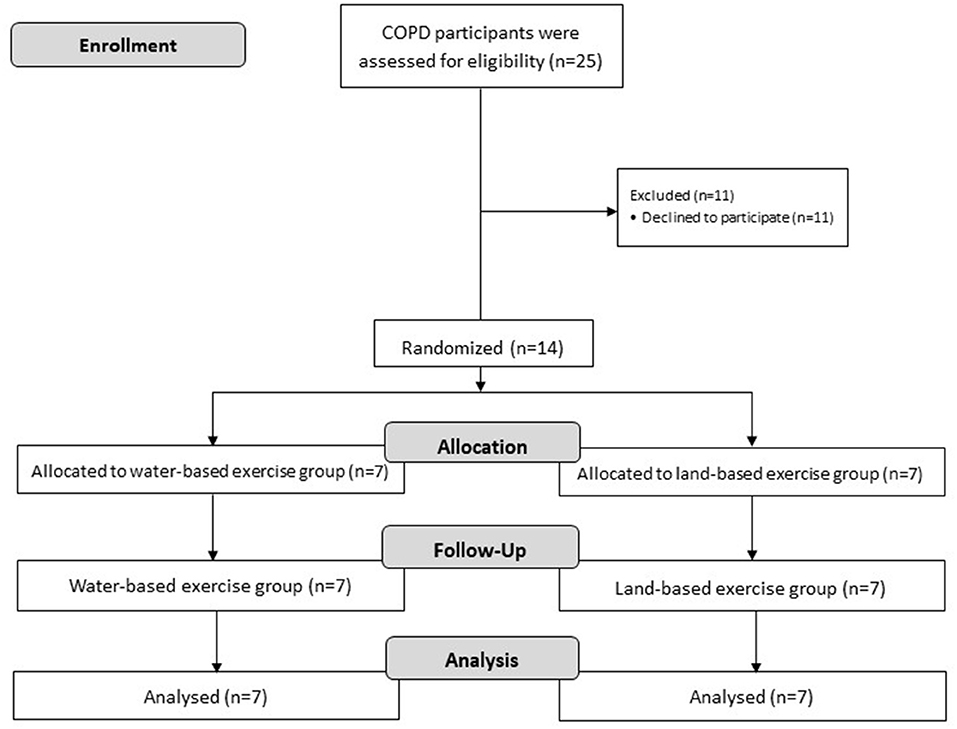
Between January 2019 and October 2020, 25 patients were screened for study participation. A diagram summarizing the flow of participants through the study is presented in Figure 1. The most frequent reason for non-eligibility was declined to participate (n = 11). Baseline characteristics of included patients were not significantly different between the two groups (Table 3).
Changes in Pulmonary Function, Respiratory and Peripheral Muscles Function, Balance Ability, and Functional Exercise Capacity Outcomes
Patients in the water-based exercise group exhibited significantly larger improvements in inspiratory (Δ11.1 ± 7.8 vs. Δ1.1 ± 5.7 cmH2O, p = 0.026), but not expiratory muscle strength in comparison to the land-based exercise group (p = 0.071) (Table 4). There were no statistically significant changes in pulmonary function and other muscle strength variables between the two groups. FTSTS and TUG were both improved within both groups after training with no statistically significant between-group differences. The water-based exercise group exhibited significantly larger improvements in ESWT (Δ663.4 ± 279.5 vs. Δ45.4 ± 93.2 s, p = 0.001), but not 6MWT and ISWT (p = 0.248 and p = 0.506, respectively). Moreover, there was a trend of reduction in dyspnea symptom after the ISWT and ESWT in both groups. Furthermore, ESWT was not significantly correlated with all pulmonary function, respiratory and peripheral muscles function, balance ability variables.
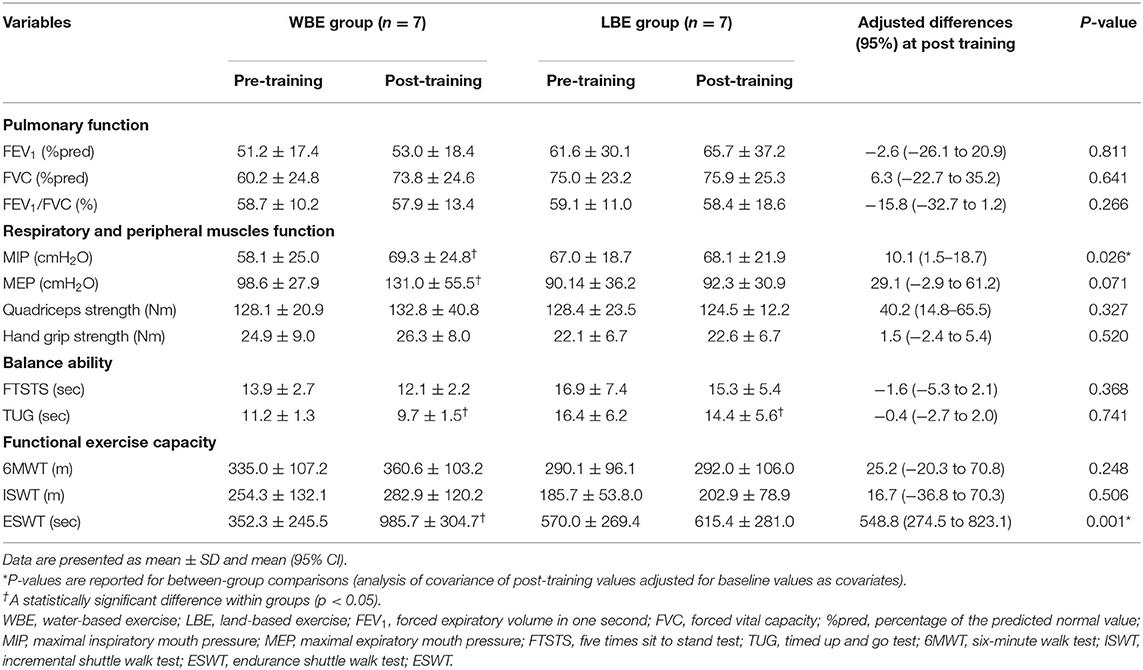
Table 4. Changes in pulmonary function, respiratory and peripheral muscles function, balance ability, and functional exercise capacity outcomes.
Both groups had a high and similar training adherence. The water-based exercise group completed 73.4 ± 17.2% of all training sessions while the land-based exercise group completed 71.7 ± 21.6% of all sessions. In addition, there was a trend of reduction in average dyspnea scale after each training sessions in both water-based exercise and land-based exercise group (-0.4 ± 0.2 vs.−0.2 ± 0.35, respectively).
Discussion
This pilot study investigated the effects of water-based exercise on respiratory function, muscle strength, balance ability, and exercise capacity in people with chronic obstructive pulmonary disease. The outcome of the water-based exercise program has not been well-characterized and not widely reported. In this study, we address this relevant topic and provide the evidence showing the benefits of the water-based exercise on the COPD patients. We include a comprehensive physical evaluation of the patients and perform the randomized control trial to strengthen our study approaches. The main findings of this study are two profound improvements in endurance exercise capacity assessed by the ESWT (primary outcome) and in the inspiratory muscle strength in the COPD patients (n = 7) who engaged in the water-based exercise program for 8 weeks. Significant differences in pulmonary function, peripheral muscle strength, balance ability variables, the 6MWD, and the ISWT were not found between the two groups. Moreover, the correlations between the improvement in ESWT and the secondary outcomes were not found in this study.
First, the endurance exercise capacity which was measured by the ESWT was dramatically enhanced in favor of the water-based exercise group. This result could be explained by the buoyancy properties of water which supports the body weight, water resistance which increases exercise intensity, and the proposed effects of warm water (34 degrees Celsius) on muscle blood flow (18). These may allow the COPD patients to exercise at a higher intensity with a likelihood of dyspnea to be reduced. Felcar et al. previously found that patients with moderate-to-severe COPD who participated in a high-intensity exercise training in water generates results similar to our findings. After 6 months of training, significant improvements were seen in inspiratory, expiratory, and peripheral muscle strength; maximal and submaximal exercise capacity; quality of life and functional status (17). Moreover, other studies reported that the water-based exercise was more effective in improving endurance exercise capacity than the land-based exercise (6, 8).
Next, the participants in the intervention group achieved a larger gain in the inspiratory muscle strength, as indicated by a significant elevation of the MIP in the water-based exercise group compared to the control group (11 vs. 1 cmH2O) after training for 8 weeks. One of the explanations could be that the hydrostatic pressure placed on the chest wall while immersing in water, which adds load to the inspiratory muscles (8), may act as a training stimulus and may increase the work of breathing. Similar to the previous study, the water-based exercise can improve respiratory muscle strength and peripheral muscle strength in patients with COPD (19).
This pilot study encounters limitations which include the small sample size and the difference between the supervised and unsupervised training sessions between the two groups. Further studies should be conducted with a larger sample size under the same supervised training sessions between the water-based and land-based exercise groups. Different changes in the outcomes at the end of the program may be more pronounced in a study with a larger number of the patients. We noticed that the results related to balance and exercise capacity at the baseline showed better values in the water-based exercise group relative to the land-based exercise group. We also noted that the probability of these variables to be intensified at the end of the program is high in the water-based exercise group. Whether or not a high deviation in these variables underlies a non-significant difference between the two exercise groups at the baseline could be addressed by increasing the study sample size.
In conclusion, this pilot study shows the beneficial consequence of the water-based exercise program in COPD patients and suggests that this training program could potentially be incorporated to the COPD rehabilitation program to improve the endurance exercise capacity and inspiratory muscle strength. These findings could be further supported by studies that include a larger sample size under the same supervised training sessions between the water-based and land-based exercise groups.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethical Review Sub-Committee Board for Human Research Involving Sciences, Thammasat University, No.3 (COA No.110/2561). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
NC, TS, KP, KY, PN, JL, and PK contributed substantially to the literature search and study design. NC, KP, KY, PN, and JL provided data collection. NC contributed to the data analysis, interpretation, and manuscript preparation. All authors critically reviewed the manuscript.
Funding
The financial support provided by Thammasat University Research Fund under TU Research Scholar, Contract No.2/8/2562.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to acknowledge the physiotherapists from Physical Therapy and Hydrotherapy center, Thammasat University for performing the exercise program and all measurements of included patients as blinded outcome assessors.
References
1. World Health Organization. World Health Organization (WHO) Website. (2020). Available online at: http://www.who.int (accessed January 26, 2019).
2. From the global strategy for the diagnosis management and prevention of COPD Global Initiative for chronic obstructive lung disease (GOLD) (2020). Available online at: http://goldcopd.org
3. Spruit MA, Singh SJ, Garvey C, Zuwallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. (2013) 188:e13–64. doi: 10.1164/rccm.201309-1634ST
4. Spruit MA, Nici L. Current concepts and definitions. In: Clini E, editor. Textbook of Pulmonary Rehabilitation. Cham: Springer (2018). p. 19–22.
5. Wouters EF, Posthuma R, Koopman M, Liu WY, Sillen MJ, Hajian B, et al. An update on pulmonary rehabilitation techniques for patients with chronic obstructive pulmonary disease. Expert Rev Respir Med. (2020) 14:149–61. doi: 10.1080/17476348.2020.1700796
6. Wadell K. Water-based exercise is more effective than land-based exercise in people with COPD physical comorbidities: critically appraised papers. J Physiotherapy. (2014) 60:57. doi: 10.1016/j.jphys.2013.12.011
7. McNamara RJ, McKeough ZJ, McKenzie DK, Alison JA. Water-based exercise training for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. (2013) 12:CD008290. doi: 10.1002/14651858.CD008290.pub2
8. McNamara RJ, McKeough ZJ, McKenzie DK, Alison JA. Water-based exercise in COPD with physical comorbidities: a randomized controlled trial. Eur Respir J. (2013) 41:1284–91. doi: 10.1183/09031936.00034312
9. Lotshaw AM, Thompson M, Sadowsky HS, Hart MK, Millard MW. Quality of life and physical performance in land- and water-based pulmonary rehabilitation. J Cardiopulm Rehabil Prev. (2007) 27:247–51. doi: 10.1097/01.HCR.0000281772.28394.30
10. Doig GS, Simpson F. Randomization and allocation concealment: a practical guide for researchers. J.Crit Care. (2005) 20:187–91. doi: 10.1016/j.jcrc.2005.04.005
11. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. (2005) 26:319–38. doi: 10.1183/09031936.05.00034805
12. Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis. (1969) 99:696–702.
13. Mathiowetz V, Dove M, Kashman N, Rogers S. Grip and pinch strength: normative data for adults. Arch Phys Med Rehabil. (1985)66:69–72.
14. Jones SE, Kon SS, Canavan JL, Patel MS, Clark AL, Nolan CM, et al. The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax. (2013) 68:1015–20. doi: 10.1136/thoraxjnl-2013-203576
15. Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. (2014) 44:1428–46. doi: 10.1183/09031936.00150314
16. Singh SJ, Puhan MA, Andrianopoulos V, Hernandes NA, Mitchell KE, Hill CJ, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J. (2014) 44:1447–78. doi: 10.1183/09031936.00150414
17. Felcar JM, Probst VS, de Carvalho DR, Merli MF, Mesquita R, Vidotto LS, et al. Effects of exercise training in water and on land in patients with COPD: a randomised clinical trial. Physiotherapy. (2018) 104:408–16. doi: 10.1016/j.physio.2017.10.009
18. Becker BE. Aquatic therapy: scientific foundations and clinical rehabilitation applications. PM R. (2009) 1:859–72. doi: 10.1016/j.pmrj.2009.05.017
Keywords: water-based exercise, chronic obstructive pulmonary disease, pulmonary rehabilitation, exercise capacity, inspiratory muscle strength
Citation: Charususin N, Sricharoenchai T, Pongpanit K, Yuenyongchaiwat K, Namdaeng P, Laosiripisan J and Keawutan P (2021) Beneficial Effect of Water-Based Exercise Training on Exercise Capacity in COPD Patients—a Pilot Study. Front. Rehabilit. Sci. 2:728973. doi: 10.3389/fresc.2021.728973
Received: 22 June 2021; Accepted: 21 October 2021;
Published: 17 November 2021.
Edited by:
Cristina Jácome, Universidade do Porto, PortugalReviewed by:
Elena Gimeno-Santos, Instituto Salud Global Barcelona (ISGlobal), SpainJoana Cruz, Polytechnic Institute of Leiria, Portugal
Copyright © 2021 Charususin, Sricharoenchai, Pongpanit, Yuenyongchaiwat, Namdaeng, Laosiripisan and Keawutan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Noppawan Charususin, bm9wcGF3YW4uY0BhbGxpZWQudHUuYWMudGg=
 Noppawan Charususin
Noppawan Charususin Thiti Sricharoenchai
Thiti Sricharoenchai Karan Pongpanit
Karan Pongpanit Kornanong Yuenyongchaiwat1,2
Kornanong Yuenyongchaiwat1,2 Phuwarin Namdaeng
Phuwarin Namdaeng