- 1Wolfson Institute of Preventative Medicine, Queen Mary University of London, London, United Kingdom
- 2Department of Health Sciences, Brunel University London, London, United Kingdom
People with multiple sclerosis (MS) report lower physical activity levels and are at a risk of becoming sedentary. As such, they are at an increased risk of developing secondary health conditions associated with inactivity. This is of major public health concern. Attempts to improve the physical activity levels in people with MS remain a challenge for health professionals. One key reason might be the lack of understanding about the meanings people with MS ascribe to exercise and physical activity. This paper draws on the key findings of a three-phased interconnected mixed methods sequential explanatory study to examine the meanings of exercise and physical activity from the perspectives of people with MS and health professionals. Phase 1 used a four-round Delphi questionnaire to scope and determine the consensus of priorities for exercise and physical activity and the reasons why people with MS (N = 101) engaged in these activities. Phase 2 used face-to-face semistructured interviews of people with MS (N = 16) to explore the meanings ascribed to exercise and physical activity. Phase 3 explored the perceptions of physiotherapists (N = 14) about exercise and physical activity using three focus groups. Using the International Classification of Functioning, Disability, and Health as a theoretical framework to underpin this study, the authors discuss the key factors, for example, emphasis on the contextual factors, that drive decision making around exercise and physical activity participation in people with MS and explore the clinical implications to health professionals.
Introduction
Multiple sclerosis (MS) is a progressive neurological condition of the central nervous system characterized by inflammation, demyelination, and neurodegeneration. Symptoms experienced by people with MS are varied and differ between individuals. Commonly reported symptoms include, but are not limited to, reduced mobility, fatigue, difficulty with performing activities of daily living, and reduced community participation (1–3). These symptoms are often associated with barriers to engaging in exercise and physical activity within the home and community (4, 5). For purposes of this paper, physical activity is defined as “any bodily movement produced by skeletal muscles that results in energy expenditure” [(6), p. 126] and would include domestic, occupational, and sports-related activities. Exercise is defined as “a subset of physical activity that is planned, structured and repetitive” [(6), p. 126].
In the absence of a cure and with the limitations of disease-modifying therapies to stem disability accrual (7), exercise and physical activity remain a key strategy to manage the symptoms and consequences of MS. There is strong evidence that consistently demonstrates the safety (8, 9) and beneficial effects of exercise and physical activity (8). Examples include increased strength (8, 10), balance (8, 10), mood (8), mobility (8, 11), quality of life (8, 10, 12, 13), and fatigue (14). These effects have been shown to help people with MS manage MS symptoms and cope over time with the condition (15). However, despite the well-rehearsed safety and beneficial effects of exercise and physical activity, people with MS report lower levels of physical activity (16) and are reported as being sedentary (17–19).
Many different approaches have been developed to encourage more physical activity such as, “Blue prescription” (a physiotherapy approach designed to enhance adherence with physical activity in MS) (20–22), behavioral approaches (23–25), and self-management strategies (26). Although these have shown some promise in clinical trials, they have had limited impact on sustaining physical activity levels in people with MS. This highlights a potential mismatch between the evidence base and the reality of implementation for people with MS and the health (and other) professionals who work with them. As such, there is a need to reconsider the development of programmes and strategies to not only increase but also sustain physical activity levels in people with MS. That is, creating space for a multimodal approach that on one hand understands and addresses the drivers of physical activity from the lived experience while taking into account the framework and theoretical lens through which health professionals work.
Therefore, the aim of this paper is to demonstrate the interplay of a theoretical model widely used in clinical practice to gain further insight into exercise and physical activity. The authors draw on a series of studies (15, 27, 28) carried out sequentially using a mixed methods approach to provide additional insight into the lived experiences of people with MS and using the International Classification of Functioning, Disability, and Health (ICF) (29) as a conduit to discuss the key factors that drive decision making around exercise and physical activity in community-dwelling people with MS and its implications for health professionals. Following a brief overview of the ICF, three studies unpacking the meaning of exercise and physical activity will be summarized, followed by a discussion of the key findings framed within the ICF.
The Clinical Utility of the ICF
The ICF is a global measure that is used to understand the health and health-related status of an individual (see Figure 1) (29). It consists of two key areas, namely, functioning and disability, and contextual factors. Functioning and disability include three domains, namely, body functions and structures, activity, and participation. The contextual factors include environmental and personal factors. This model recognizes the dynamic interactions that exist between the different domains of the ICF; for example, the influence the contextual factors (environmental and personal) might have on the outcomes of an intervention (5, 30, 31).
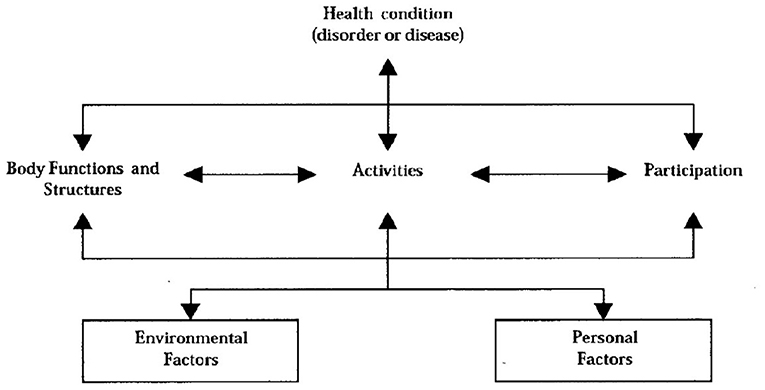
Figure 1. Representation of the International Classification of Functioning, Disability, and Health (29).
The ICF is underpinned by the principles of the biopsychosocial approach to understanding disability. Within this context, the ICF views disability as an interaction between the biological and social aspects of life (29). It is widely used to provide a common language amongst clinicians, researchers, and people with disability, including people with MS, to describe disability and contextual factors that might have an impact on their lives (30, 32–35). Therefore, given the ethos of the ICF, which focuses on bridging the clinical and experiential gap, it is used in this study as a useful tool through which physical activity can be examined.
The Meaning of Exercise and Physical Activity: Perspective Matters
Unpacking the meaning of exercise and physical activity is a complex issue that lends itself to an examination from different perspectives.
A three-phase mixed methods sequential explanatory design was used to determine the meanings people with MS ascribe to exercise and physical activity and its clinical implications (15, 27, 28). These studies have been published elsewhere but will be summarized here.
Phase 1: A Day in the Life of People With MS: the Delphi Method
A four-round Delphi questionnaire scoped and determined consensus of priorities for the top 10 exercise and physical activities and the reasons people with MS were engaged in these activities (27).
A purposive sample was recruited via a series of targeted strategies aimed at people who had the ability to complete questionnaires, who were diagnosed with MS, and who were living in the community (N = 101). Data were analyzed using content analysis, descriptive statistics, and non-parametric tests.
Findings from this study provided a snapshot view of exercise and physical activity. Table 1 shows the top 10 prioritized exercise and physical activity practices and the reasons people with MS (N = 70) engaged in these activities. The consensus was achieved for the exercise and physical activities using Kendall's coefficient of concordance (36) (W = 0.744, p < 0.0001) and for the reasons they engaged in exercise and physical activity (W = 0.723, p < 0.0001). Overall, the exercise and physical activity practices and the reasons people with MS engaged in exercise and physical activity were diverse and highlighted the physical, psychological, and social benefits. Results indicated that unstructured activities that focused on maintaining everyday function were prioritized and had a significant impact on the identity of people with MS.
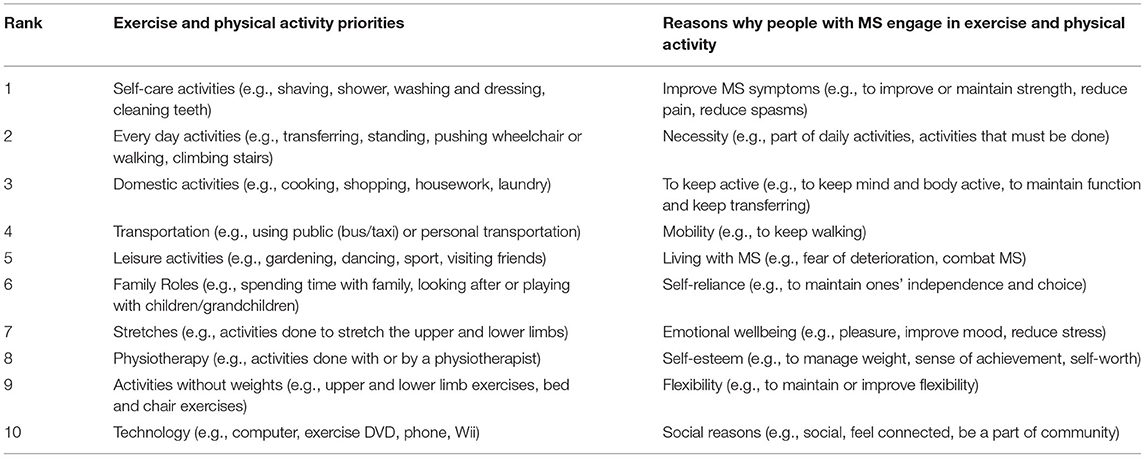
Table 1. Prioritised exercise and physical activity and reasons why people with MS engage in exercise and physical activity.
Phase 2: The Meaning of Exercise and Physical Activity in People With MS: Interview Method
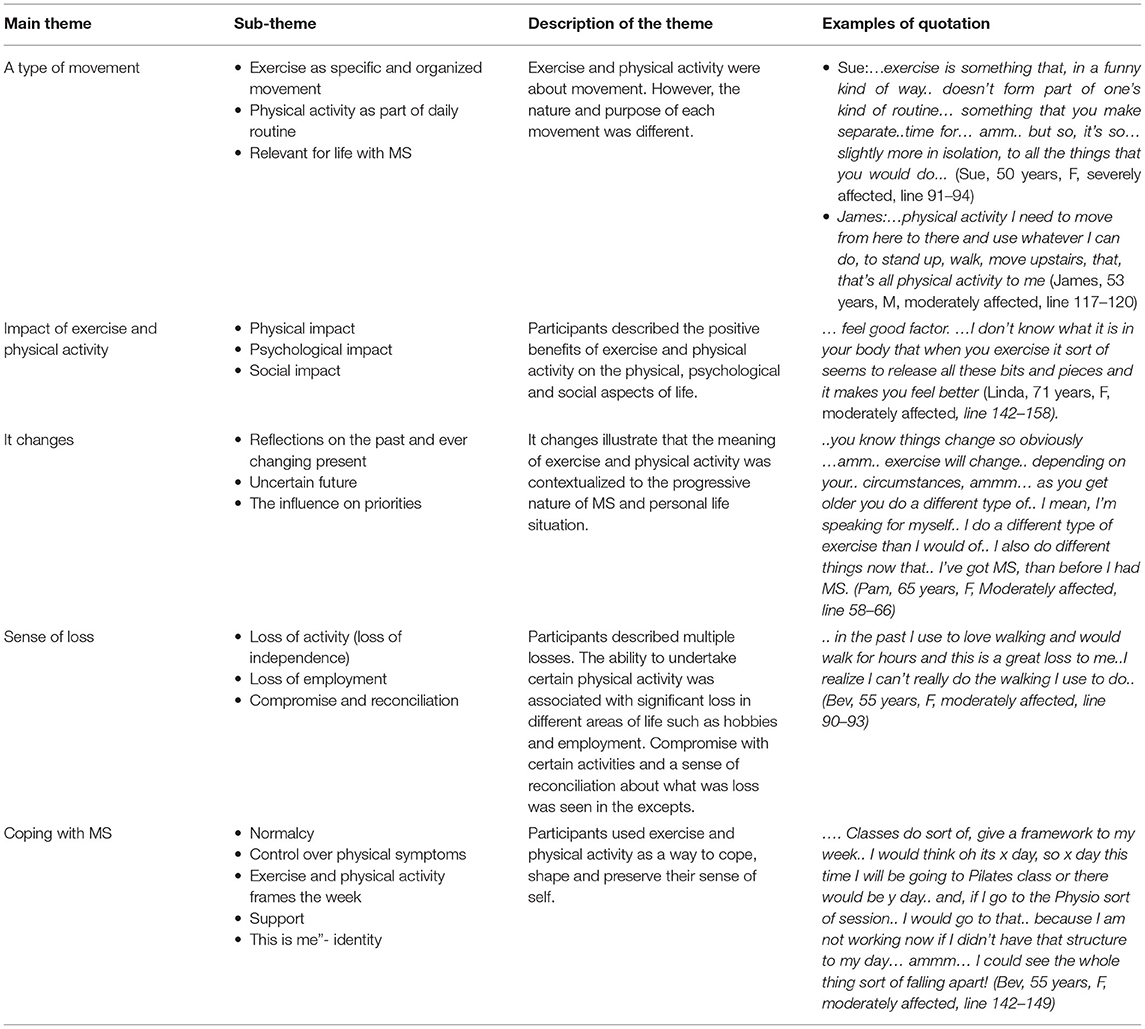
The meaning of exercise and physical activity was explored using in-depth semistructured, face-to-face interviews (N = 16; 12 women and four men). Data were analyzed using framework analysis (37). Details of the methods have been published elsewhere (15). To summarize the findings, five major themes were developed, namely, type of movement, impact of exercise and physical activity, “it changes”, sense of loss, and coping with MS. Table 2 provides a brief description of each theme. Overall, the study highlights views from the experiential perspective suggesting that people with MS took a multidimensional view of exercise and physical activity. This view of exercise and physical activity extended beyond movement; it was about using these activities as a way to cope, preserve their identity, and live life with a progressive neurological condition. Nonetheless, it was the contextual factors, such as, sense of loss and the fluctuating nature of priorities, energy demands, and choice that were dominant influences that dictated engagement or participation in exercise and physical activity.
Phase 3: Perceptions of Physiotherapists About Exercise and Physical Activity: FOCUS Group Method
Three focus groups were used to explore the understandings of physiotherapists about exercise and physical activity in light of the Delphi results and their relevance to clinical practice (28). Physiotherapists (N = 14; 12 women/2 men) with experience working with people with MS in the community were included. The focus groups were analyzed using the principles of framework analysis (37). Four themes were developed, namely, blurred terminologies, influencing factors for the meaning of exercise and physical activity, when professional expertise meets experiential expertise, and the resolve. Table 3 shows the themes and a brief description of each theme. Overall, the findings highlight the perspective of professionals that was largely shaped by training and models of practice. Physiotherapists expressed that the use of exercise is embedded into clinical practice, but physical whilst activity considered is less routine in clinical practice.
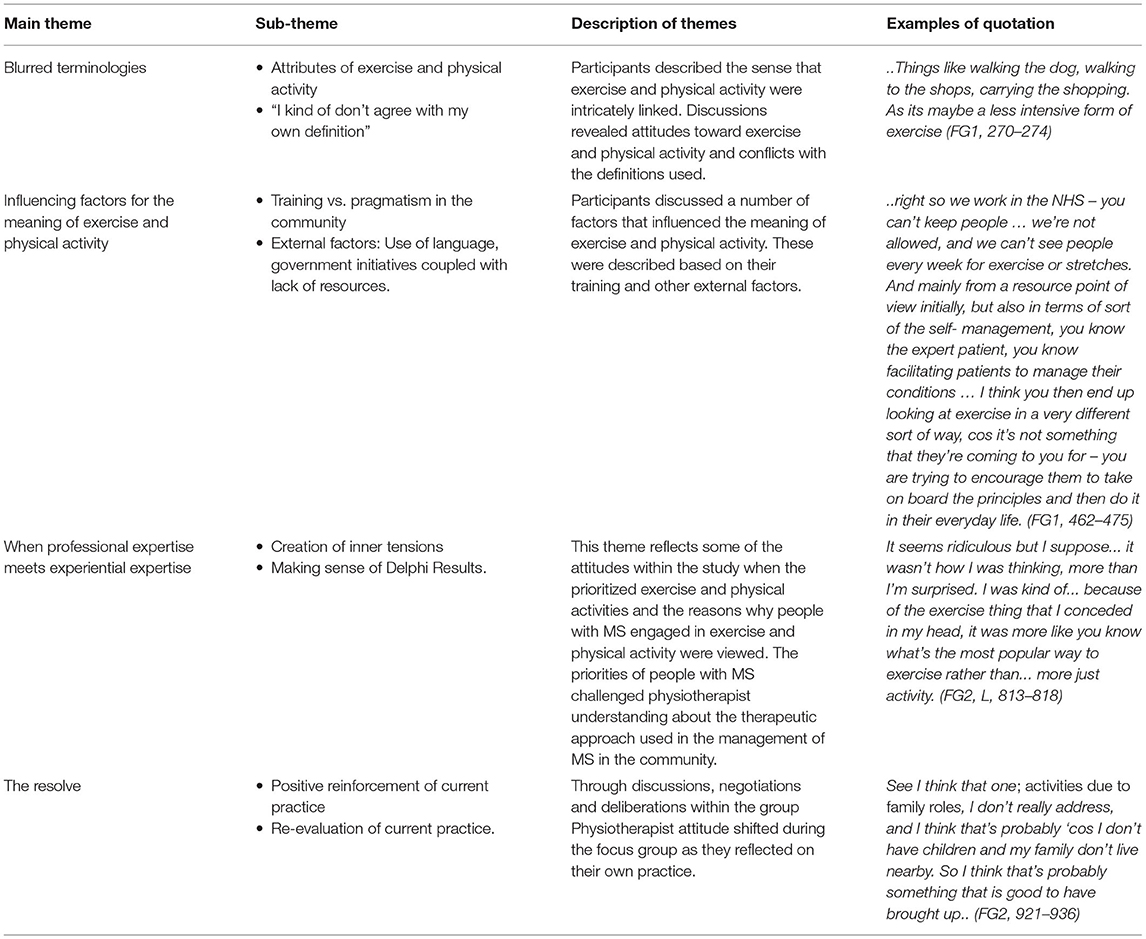
Table 3. Major themes and subthemes for perceptions of physiotherapists of exercise and physical activity.
The Interplay of Theory and Physical Activity Using the ICF
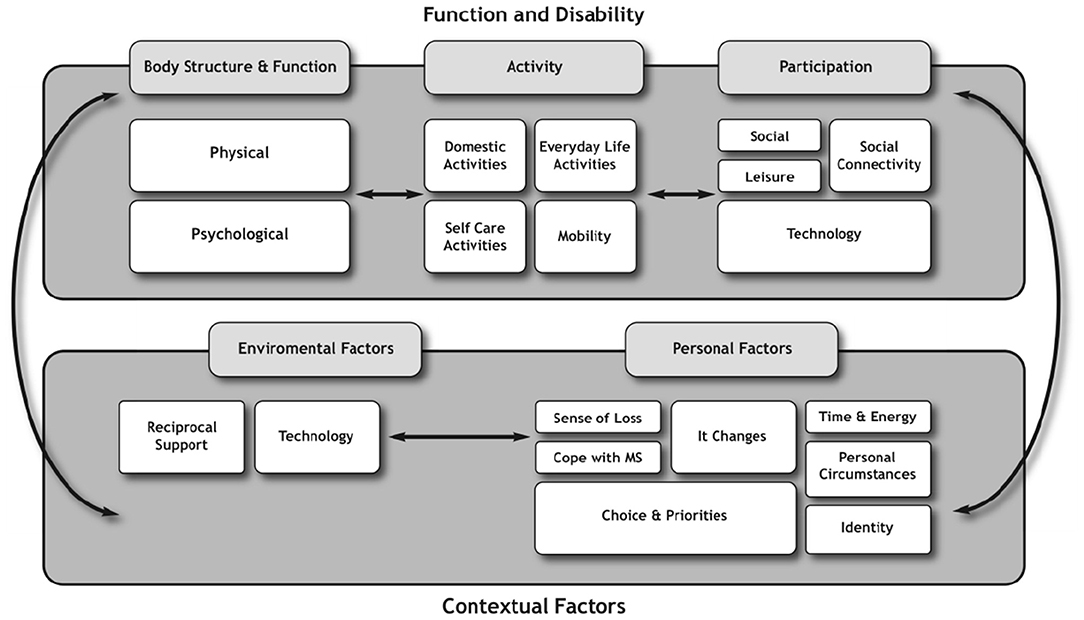
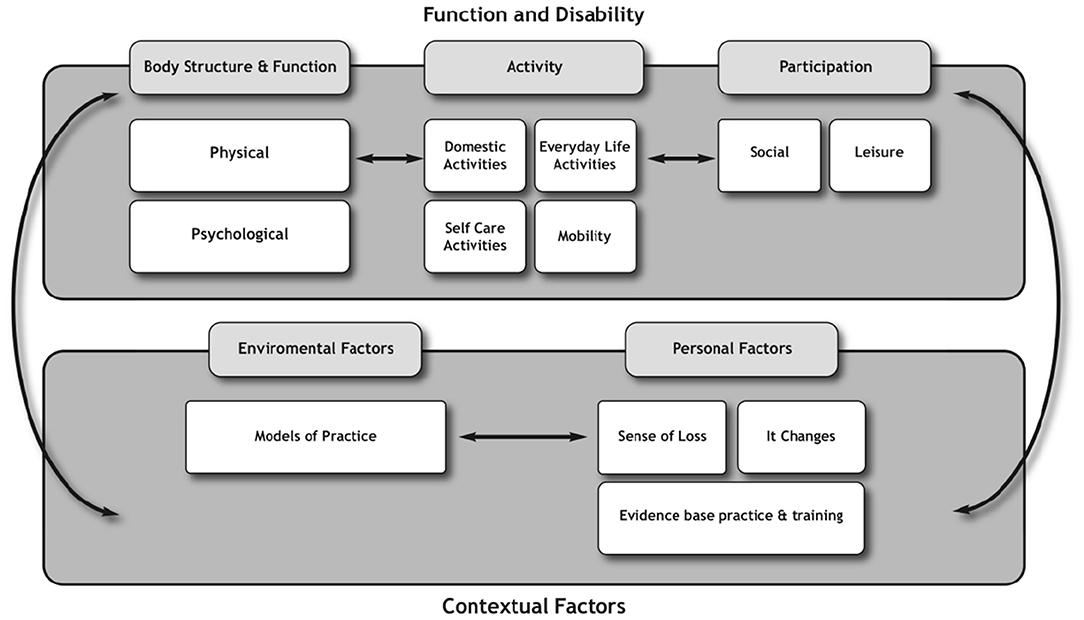
To explore the interplay of physical activity from the lived experience and the experience of professionals and how they interact with the theory, the key findings were mapped onto the domains of the ICF (29). The findings from the perspectives of people with MS (Phase 1 and 2) (see Figure 2) were mapped separately to those of the health professionals (see Figure 3).
Conceptually, the diagram highlights that the exercise and physical activity practices, and the meanings people with MS ascribed to exercise and physical activity fit within the ICF model multiple times across all of the domains of function, disability, and contextual factors. This supports the applicability of the ICF to the lived experience of people with MS in relation to exercise and physical activity.
The findings from the perspective of professionals were also mapped onto the ICF conceptually to ascertain how their views about exercise and physical activity fit within this model (see Figure 3). The representation of the perspective of physiotherapists highlights less focus on the participation and contextual factors domains. Of note, there were double the number of factors within the function and disability domain compared with the contextual domain. Indeed, the contextual factors reported by physiotherapists were less than half expressed by people with MS.
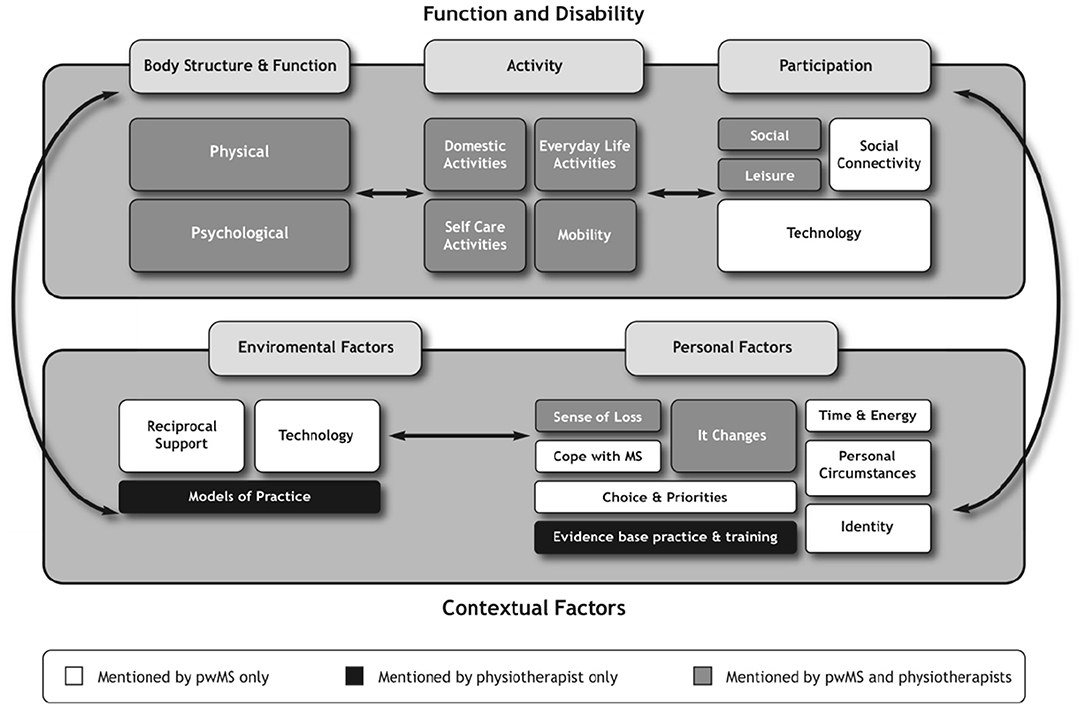
Both perspectives were then merged to compare and contrast the views of people with MS and physiotherapists (see Figure 4). It illustrates each domain and highlights that certain domains of the ICF had a greater influence on how people with MS and physiotherapists ascribed meaning to exercise and physical activity. These influences will be discussed to highlight areas of overlap and areas of dominance.
The findings from the experiential perspective demonstrated that people with MS adopted a participatory mind set, as their discussions focused on social and leisure-type activities as well as the use of technologies that enabled access to these activities. As such, they were more likely to engage in activities that connected with other people. This was in contrast to physiotherapists whose concerns revolved around whether the activities people with MS prioritized would have a direct impact on their physical performance. These findings would suggest that for physiotherapists, greater weighting and higher priority were given to the body structure, function, and activity domains rather than participation domains of the ICF in ascribing meaning to exercise and physical activity.
In contrast, the functioning and disability domains reflected a different weight of influence for people with MS compared with physiotherapists. For example, the perceptions of people with MS about exercise and physical activity were dynamic and diverse and could be reflected across all the domains of the ICF. This was exemplified by the inclusion of certain categories such as transportation and activities involving technology, which were prioritized by people with MS in the Delphi study (27). The inclusion of technology was interesting and traversed the participation and environmental domains. For example, people with MS described technology as a form of activity to facilitate higher education, as well as the use of technology as a communicative device necessary for organizing daily routines. These were not mentioned by physiotherapists, and signify the expansive views of people with MS in relation to exercise and physical activity.
Furthermore, the findings from the interviews revealed that in ascribing meaning to exercise and physical activity, people with MS were influenced predominantly by the participation and contextual factors domains; more specifically the personal factors. These contextual factors, which included the environmental and, specifically, the personal factors, shaped the perspectives of people with MS (see Figure 2), for example, “coping with MS,” “identity,” “energy demands and availability,” “time constraints,” “personal choice and priorities.” These findings concur with other researchers who have also identified that contextual factors play a significant role in influencing the other domains such as functioning and disability in people with MS as well as in people living with other forms of disability (31, 33, 35, 38). Therefore, understanding the influence contextual factors play in people with MS is important especially to health professionals who use exercise and physical activity as treatment strategies. Lack of understanding and insight into these contextual issues render people with MS seemingly inactive to the view of professionals, whereas the findings from the experiential perspective portray a different picture where people with MS are active on other priorities in other contexts.
The responses of physiotherapists did not fit neatly into the ICF framework. For example, physiotherapists shared aspects of the themes “sense of loss” and “it changes,” which represents the personal factors of people with MS. This finding suggests that physiotherapists do consider some aspects of the personal factors identified by people with MS. However, physiotherapists did not make the link as to how these personal factors might influence engagement in exercise and physical activity beyond the physical aspects of the life of individuals. In addition, the findings from the perspectives of physiotherapists highlight that their views about exercise and physical activity were also shaped by their own contextual factors, which were external to people with MS but influenced decisions around their management in the community. These factors included their professional knowledge based on evidence-based practice and training (personal factors) as well as models of practice, which could be represented under environmental factors.
The current interpretation of the ICF implies that the contextual factors interact with the functional and disability domains (29). Although this is true, this study extended this view to also suggest that for community-dwelling people with MS, the contextual factors did not only influence the functional and disability domains but dictated what happened at the functional and disability domains. Indeed, the orientation of priority was challenged by people with MS. Having considered the views put forward by people with MS, the importance of how these views were expressed, and the heavier weight attributed by the contextual factors, the authors reconsidered the orientation of the ICF by 180°. This flip suggests that the contextual factors played a more major role than previously thought in relation to the exercise and physical activity practices, and the meanings people with MS ascribed to these practices (see Figure 5).
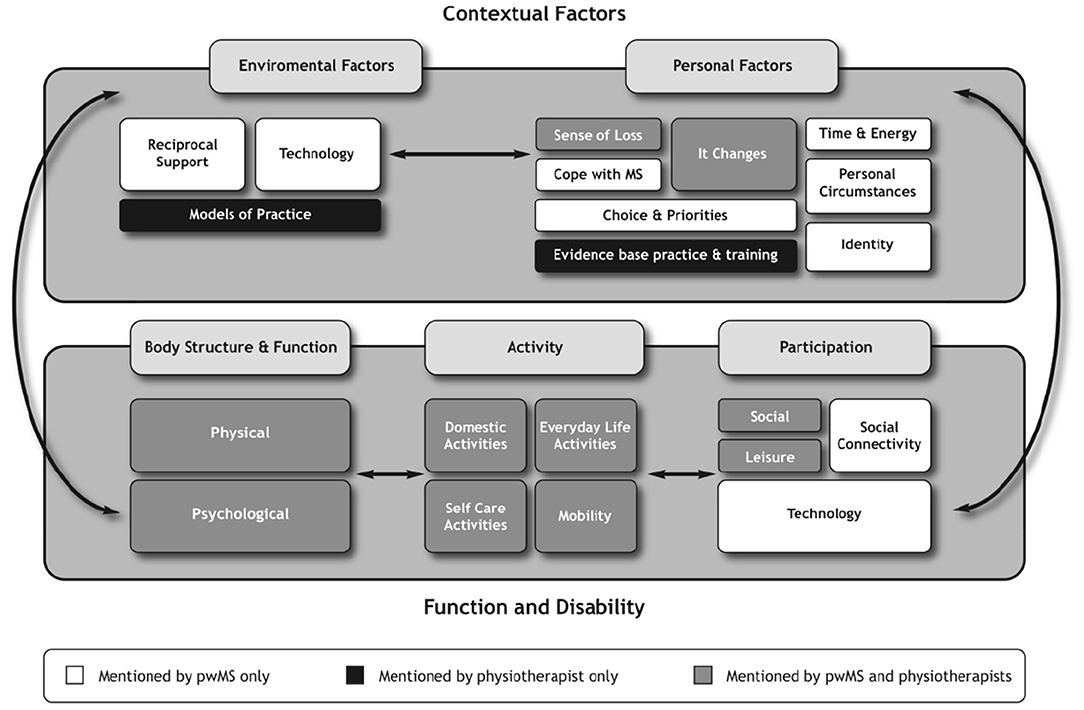
Figure 5. Reorientation of the ICF based on the experiential and perspective of the professionals of exercise and physical activity.
Implications For Future Thinking on Physical Activity in People With MS
Reconceptualising the interactions between the contextual factors and the function and disability domains, not only as influences to be considered but also as factors having the capacity to dictate decisions about exercise and physical activity, should be central to the thinking behind engagement strategies in community-dwelling people with MS. As such, physiotherapists and other exercise professionals working in the community should give more focused attention to these domains when designing and implementing rehabilitation strategies or programs for people with MS living in the community as a way to engage and sustain exercise and physical activity in this population.
This study provided some insights about exercise and physical activity based on two sources of information, one extracted from the experiential perspective of people with MS and the other from the perspective of professionals. Exploring both sources of information suggests a “rethink” about how exercise and physical activity are viewed by health professionals and points toward taking a more person-centered approach to reflect the preferences and priorities of community-dwelling people with MS.
The key findings from the experiential perspective have not only identified the exercise and physical activity preferences and priorities of people with MS but also what these activities mean to people with MS. Having an understanding of these activities and their meanings provides some insight into the way health professionals, specifically, physiotherapists might approach exercise and physical activity in people with MS living in the community. For example, people with MS preferred engaging in exercise and physical activity practices that they valued and considered meaningful for living life with MS. This suggests that exercise and physical activity for community-dwelling people with MS were more than managing MS symptoms and also about the importance of participating in life activities, how they coped with life and maintained a sense of self. Therefore, it is now time to create more opportunities and design interventions that reflect the participatory aspect of exercise and physical activity and develop tools to monitor such interventions with a participatory focus.
Strengths and Limitations
Using the key findings from a mixed methods study, this paper provided some insights into the intricacies associated with exercise and physical activity from the perspectives of people with MS and its clinical applicability to health care professionals. It also highlights the types of personal factors and their relevance to dictate and influence engagement in physical activity in people with MS. However, the findings must be examined, reflected on, and interpreted within the context and rigor of each study. As such, the findings might not be generalisable beyond the participants and context of the studies highlighted in this paper. Nonetheless, further research could explore the theoretical underpinnings and concepts highlighted in this study in other long-term conditions and contexts.
Conclusions
This paper demonstrates the interplay between theory and physical activity in people with MS using the ICF model to guide discussions. The model illustrates the interaction of the ICF domains in relation to the meanings ascribed to exercise and physical activity based on the perspectives of people with MS and physiotherapists. It highlights that although people with MS were predominately influenced by participation and personal factors, physiotherapists were predominately influenced by the function and disability domains, albeit with less reference to participation. In addition, this paper adds to the existing evidence in relation to exercise and physical activity and provides evidence that the perception of exercise and physical activity in people with MS is not static and limited to any one domain within the ICF model. Instead, it highlights a complex concept, which is dynamic in nature, traversing between functioning and disability and contextual factors (personal and environmental) with personal factors having a greater influence on decisions made about exercise and physical activity in people with MS.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by School of Health Sciences and Social Care, Brunel University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors read and contributed to the manuscript development and revision of this paper.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Einarsson U, Gottberg K, Fredrikson S, von Koch L, Holmqvist LW. Activities of daily living and social activities in people with multiple sclerosis in Stockholm County. Clin Rehabil. (2006) 20:543–51. doi: 10.1191/0269215506cr953oa
2. Krupp LB. Fatigue in multiple sclerosis: definition, pathophysiology and treatment. CNS Drugs. (2003) 17:225–34. doi: 10.2165/00023210-200317040-00002
3. Freeman JA. Improving mobility and functional independence in persons with multiple sclerosis. J Neurol. (2001) 248:255–9. doi: 10.1007/s004150170198
4. Asano M, Duquette P, Andersen R, Lapierre Y, Mayo NE. Exercise barriers and preferences among women and men with multiple sclerosis. Disabil Rehabil. (2013) 35:353–61. doi: 10.3109/09638288.2012.742574
5. Kayes NM, McPherson KM, Taylor D, Schlüter PJ, Kolt GS. Facilitators and barriers to engagement in physical activity for people with multiple sclerosis: a qualitative investigation. Disabil Rehabil. (2011) 33:625–42. doi: 10.3109/09638288.2010.505992
6. Caspersen CJ, Powell KE, Christenson G. Physical activity, exercise and physical fitness: definitions and distinctions for health-related research. Publ Health Rep. (1985) 100:126–31.
7. Merkel B, Butzkueven H, Traboulsee AL, Havrdova E, Kalincik T. Timing of high-efficacy therapy in relapsing-remitting multiple sclerosis: a systematic review. Autoimmun Rev. (2017) 16:658–65. doi: 10.1016/j.autrev.2017.04.010
8. Rietberg MB, Brooks D, Uitdehaag BM, Kwakkel G. Exercise therapy for multiple sclerosis. Cochr Database Syst Rev. (2004) 3:CD003980. doi: 10.1002/14651858.CD003980
9. Pilutti LA, Platta ME, Motl RW, Latimer-Cheung AE. The safety of exercise training in multiple sclerosis: a systematic review. J Neurol Sci. (2014) 343:3–7. doi: 10.1016/j.jns.2014.05.016
10. Sá MJ. Exercise therapy and multiple sclerosis: a systematic review. J Neurol. (2013) 261:1651–61. doi: 10.1007/s00415-013-7183-9
11. Snook EM, Motl RW. Effect of exercise training on walking mobility in multiple sclerosis: a meta-analysis. Neurorehabil Neural Repair. (2009) 23:108–16. doi: 10.1177/1545968308320641
12. Motl R, Gosney J. Effect of exercise training on quality of life in multiple sclerosis: a meta-analysis. Multiple Sclerosis. (2008) 14:129–35. doi: 10.1177/1352458507080464
13. Anthony W, Gidugu V. Systematic Review of the Effects of Exercise and Physical Activity on Psychological and Quality of Life Outcomes for Individuals with Multiple Sclerosis, 1996-2011. Boston: Boston University, Sargent College, Center for Psychiatric Rehabilitation. (2012).
14. Andreasen AK, Stenager E, Dalgas U. The effect of exercise therapy on fatigue in multiple sclerosis. Multiple Sclerosis. (2011) 17:1041–54. doi: 10.1177/1352458511401120
15. Stennett A, De Souza L, Norris M. The meaning of exercise and physical activity in community dwelling people with multiple sclerosis. Disabil Rehabil. (2020) 42:317–23. doi: 10.1080/09638288.2018.1497715
16. Motl RW, McAuley E, Snook EM. Physical activity and multiple sclerosis: a meta-analysis. Multiple Sclerosis. (2005) 11:459–63. doi: 10.1191/1352458505ms1188oa
17. Sandroff BM, Dlugonski D, Weikert M, Suh Y, Balantrapu S, Motl RW. Physical activity and multiple sclerosis: new insights regarding inactivity. Acta Neurol Scand. (2012) 126:256–62. doi: 10.1111/j.1600-0404.2011.01634.x
18. Veldhuijzen van Zanten JJ, Pilutti LA, Duda JL, Motl RW. Sedentary behaviour in people with multiple sclerosis: is it time to stand up against MS? Mult Scler. (2016) 22:1250–6 doi: 10.1177/1352458516644340
19. Brenda J, Sasaki JE, Cederberg KL, Motl RW. Sociodemographic and clinical correlates of device-measured sedentary behaviour in multiple sclerosis. Disabil Rehabil. (2021) 43:42–8. doi: 10.1080/09638288.2019.1614683
20. Mulligan H, Treharne GJ, Hale LA, Smith C. Combining self-help and professional help to minimize barriers to physical activity in persons with multiple sclerosis: a trial of the “Blue prescription” approach in New Zealand. J Neurol Phys Ther. (2013) 37:51–7. doi: 10.1097/NPT.0b013e318292799e
21. Smith CM, Hale LA, Mulligan HF, Treharne GJ. Participant perceptions of a novel physiotherapy approach (“Blue Prescription”) for increasing levels of physical activity in people with multiple sclerosis: a qualitative study following intervention. Disabil Rehabil. (2013) 35:1174–81. doi: 10.3109/09638288.2012.723792
22. Hale LA, Smith C, Mulligan H, Treharne GJ. Tell me what you want, what you really really want.: Asking people with multiple sclerosis about enhancing their participation in physical activity. Disabil Rehabil. (2012) 34:1887–93. doi: 10.3109/09638288.2012.670037
23. Plow MA, Resnik L, Allen SM. Exploring physical activity behaviour of persons with multiple sclerosis: a qualitative pilot study. Disabil Rehabil. (2009) 31:1652–65. doi: 10.1080/09638280902738375
24. McAuley E, Motl RW, Morris KS, Hu L, Doeksen SE, Elavsky S, et al. Enhancing physical activity adherence and well-being in multiple sclerosis: a randomised controlled trial. Multiple Sclerosis. (2007) 13:652–9. doi: 10.1177/1352458506072188
25. Ryan JM, Fortune J, Stennett A, Kilbride C, Lavelle G, Hendrie W, et al. Safety, feasibility, acceptability and effects of a behaviour-change intervention to change physical activity behaviour among people with multiple sclerosis: results from the iStep-MS randomised controlled trial. Mult Scler. (2020) 26:1907–18. doi: 10.1177/1352458519886231
26. Barlow J, Edwards R, Turner A. The experience of attending a lay-led, chronic disease self-management programme from the perspective of participants with multiple sclerosis. Psychol Health. (2009) 24:1167–80. doi: 10.1080/08870440802040277
27. Stennett A, De Souza L, Norris M. Physical activity and exercise priorities in community dwelling people with multiple sclerosis: a Delphi study. Disabil Rehabil. (2018) 40:1686–93. doi: 10.1080/09638288.2017.1309464
28. Stennett A, De Souza L, Norris M. A qualitative exploration of physiotherapists' perceptions about exercise and physical activity: reflections on the results from a Delphi Study. Disabil Rehabil. (2020) 42:3142–51. doi: 10.1080/09638288.2019.1585969
29. World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva: World Health Organization (2001).
30. Rimmer JH. Use of the ICF in identifying factors that impact participation in physical activity/rehabilitation among people with disabilities. Disabil Rehabil. (2006) 28:1087–95. doi: 10.1080/09638280500493860
31. Van Der Ploeg HP, Van Der Beek AJ, Van Der Woude LHV, Van Mechelen W. Physical activity for people with a disability: a conceptual model. Sports Med. (2004) 34:639–49. doi: 10.2165/00007256-200434100-00002
32. Karhula ME, Kanelisto KJ, Ruutiainen J, Hämäläinen PI, Salminen A. The activities and participation categories of the ICF Core Sets for multiple sclerosis from the patient perspective. Disabil Rehabil. (2013) 35:492–7. doi: 10.3109/09638288.2012.702845
33. Hamed R, Tariah H, Hawamdeh Z. Personal factors affecting the daily functioning and well-being of patients with multiple sclerosis using the international classification of functioning model. Int J Mental Health. (2012) 41:47–61. doi: 10.2753/IMH0020-7411410404
34. Coenen M, Basedow-Rajwich B, König N, Kesselring J, Cieza A. Functioning and disability in multiple sclerosis from the patient perspective. Chronic Illness. (2011) 7:291–310. doi: 10.1177/1742395311410613
35. Khan F, Pallant JF. Use of international classification of functioning, disability and health (ICF) to describe patient-reported disability in multiple sclerosis and identification of relevant environmental factors. J Rehabil Med. (2007) 39:63–70. doi: 10.2340/16501977-0002
36. Schmidt RC. Managing Delphi surveys using nonparametric statistical techniques. Decision Sci. (1997) 28:763–74. doi: 10.1111/j.1540-5915.1997.tb01330.x
37. Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In Bryman and Burgess, editors, Analysing Qualitative Data. London: Routledge (1994). p. 173–94. doi: 10.4324/9780203413081_chapter_9
Keywords: exercise, physical activity, priorities, ICF (international classification of functioning disability and health), physiotherapy, multiple sclerosis
Citation: Stennett AM, De Souza LH and Norris M (2021) Flipping the ICF: Exploring the Interplay of Theory and the Lived Experience to Reconsider Physical Activity in Community-Dwelling People With Multiple Sclerosis. Front. Rehabilit. Sci. 2:710618. doi: 10.3389/fresc.2021.710618
Received: 16 May 2021; Accepted: 16 August 2021;
Published: 01 October 2021.
Edited by:
Mats Granlund, Jönköping University, SwedenReviewed by:
Leigh Hale, University of Otago, New ZealandLisa Bunn, University of Plymouth, United Kingdom
Copyright © 2021 Stennett, De Souza and Norris. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrea Marjorie Stennett, YS5zdGVubmV0dEBxbXVsLmFjLnVr
 Andrea Marjorie Stennett
Andrea Marjorie Stennett Lorraine H. De Souza2
Lorraine H. De Souza2 Meriel Norris
Meriel Norris