- 1School of Rehabilitation Sciences, McMaster University, Hamilton, ON, Canada
- 2CanChild Centre for Childhood Disability Research, Hamilton, ON, Canada
- 3Department of Pediatrics, McMaster University, Hamilton, ON, Canada
- 4McMaster Autism Research Team, Hamilton, ON, Canada
Clinical measures in health and rehabilitation settings are often used to examine child functioning to better support the diverse needs of children with neurodevelopmental disorders (NDD) and their families. The WHO's International Classification of Functioning, Disability, and Health (ICF) framework reflects a focus of health beyond biomedical deficits, using the concept of functioning to create opportunities for measurement development involving this construct. In the measures developed in the field of childhood NDD, it is unclear whether and how these tools measure and incorporate the ICF framework and its domains within health care contexts. Understanding how these measures utilize the ICF will enable researchers and clinicians to operationalize function-focused concepts in studies and clinical practice more effectively. This narrative review aims to identify and describe function-focused measures that are based on the ICF for children with NDD, as described in the peer-reviewed literature. This review used a systematic search strategy with multiple health-focused databases (Medline, PsycInfo, EMBASE, EMCARE), and identified 14 clinical measures that provide direct support for children (aged 0-21) with NDD in pediatric health (and other) settings. Results described the measures that were primarily developed for three main diagnostic populations [cerebral palsy, autism spectrum disorder, and communication disorders]; had varying contextual use (clinical-only or multiple settings); and for which authors had conducted psychometric tests in the measure's initial development studies, with the most common being content validity, interrater reliability, test-retest reliability. Participation (79%, n = 11) & Activities (71%, n = 10) were the most common ICF domains captured by the set of measurement tools. Overall (71%, n = 10) of the identified measures utilized multiple ICF domains, indicating that the “dynamic nature” of the interactions of the ICF domains was generally evident, and that this result differentiated from “linking rules,” commonly used in research and clinical practice. The implications of these findings suggest that clinical measures can be an effective application of the ICF's defined concepts of functioning for children with NDD.
Introduction
Neurodevelopmental disorders (NDD), as defined by the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), refer to a group of conditions that present during a child's early developmental period and are characterized by developmental deficits that may create challenges in the child's personal, social, academic, or occupational functioning (1). Common examples of NDD include autism spectrum disorder (ASD), communication and/or language disorders, attention deficit/hyperactivity disorder, motor disorders (including cerebral palsy [CP]), learning disorders, and developmental coordination disorder (1). The prevalence rate for NDD in developed countries range from 7 to 14% of all children (2). Children with NDD may experience challenges in different environments, potentially impacting their functioning within academic settings (school), daily living skills (home), and the broader community (3–7). The DSM-5 describes these challenges as a symptom of excess, deficit, or delay in key aspects of child functioning, especially when considering the achievement of expected developmental milestones (1).
Historically, biomedical models and thinking have greatly influenced clinical practice, including the field of childhood disability (8, 9). This traditional way of thinking focused on the attributes of a child's deficits and limitations, for diagnostic purposes and to treat aspects of the child's “disability” (10, 11). In 2001, the International Classification of Functioning, Disability, and Health (ICF) – a contemporary conceptual framework – challenged these practices and highlighted the paradigm shift to think beyond the biomedical model to an integrated biopsychosocial model of human functioning and disability (8). This biopsychosocial model emphasizes that individuals with disabilities have needs that extend beyond the medical scope of practice, and are often broad-based in nature within social, educational, and functional settings (12).
As shown in Figure 1, the four key domains of the ICF are: body function & structures (functioning at the level of the body); activities (functioning at the level of the individual); participation (functioning of a person as a member of society); and contextual factors (personal and environmental factors that can exist as facilitators or barriers) (8). The ICF framework defines functioning as an umbrella term to describe the interactions of these four domains, examining the positive or neutral aspects occurring between the individual's health condition(s) and their context (8). “Disability” is an alternate umbrella term used to describe the interactions of an individual's impairments, activity limitations and participation restrictions, examining the negative aspects of the interaction between the individual's health condition(s) and their context (8).
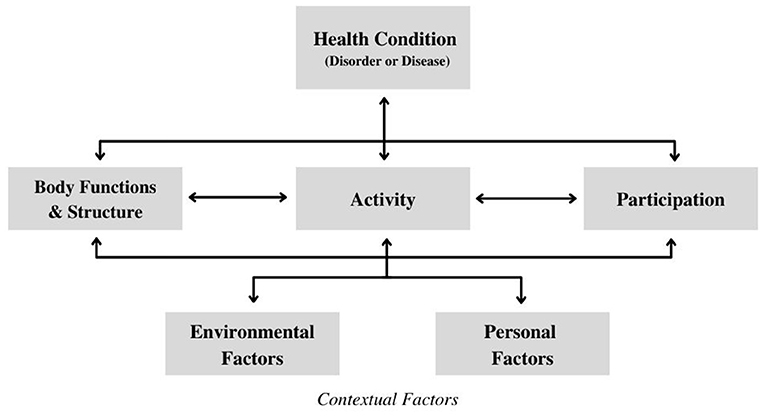
Figure 1. International classification of functioning, disability, and health framework (8).
This ICF framework depicts the interactive and non-linear nature of the core domains, establishing that these conceptual domains are not independent when examining functioning and/or disability. The framework is representative of the biopsychosocial perspective, as it recognizes how the influences of physical, psychological, and social factors within “functioning and disability” can be understood from the viewpoint of the individual with respect to their health condition (13, 14). Without focusing on single descriptors to label a child's functional abilities, this framework utilizes a holistic approach that still highlight the nuances in the interactions of the different elements that build a child's functional profile (14, 15). This framework indicates a paradigm shift in the ways that researchers and clinicians understand disability, as it provides a multidimensional perspective that both classifies functioning independently from the individual's diagnosis and views disability as product of person-environment interactions (12, 15, 16).
Children with NDD exhibit a wide range of levels of functioning within and between their diagnostic groups (17). In addition to the ICF framework, the field of NDD has seen growth in the concept of functioning that takes into consideration the heterogeneous level of abilities within diagnostic populations that extends across NDD (10). For example, within ASD literature, the concept of neurodiversity views neurological differences as inherent human variation, rather than as a disorder, and celebrates the individuality of a person – regardless of their capabilities (18, 19). This change in thinking in the field of ASD has had a great influence in promoting various abilities and child differences within ASD interventions, including the language that is being used to describe the diagnosis (19, 20).
Similar concepts of functioning started in the field of CP, in relation to interventions in pediatric rehabilitation. Rather than using the traditional approaches of CP that attempt to normalize movement patterns and minimize the development of secondary impairments, there is an increased emphasis on enabling the child to master various tasks and participate in different activities (21, 22). Over the last 20 years, in the field of CP, clinical care and research have examined child functioning as it relates to interacting contextual factors (22, 23). Although the needs and abilities of children with NDD (and their families) are heterogeneous, everyday functioning is continually regarded as an important outcome to families (24).
Examining clinical contexts in particular, there is a notable emphasis of functioning in the ICF, as this term is often used to describe abilities-focused processes – otherwise commonly referred to as function-focused care (12, 24, 25). Within this type of pediatric care planning, there are typically certain measures used with families to promote child functioning or child abilities.
Although these measures may have the appropriate psychometric testing completed to illustrate their effectiveness in clinical utility, it is also important that there is some consistency with the language that is being used with these measures (20, 26, 27). For example, the terms “function,” “functional,” and “everyday functioning,” are used synonymously in the literature, whereas the ICF's conceptualization of functioning emphasizes it as the complex interactions between the four domains (10). There are various measures that aim to assess concepts related to function, such as adaptive behavior [e.g., Vineland Adaptive Behavior Scales (28), Adaptive Behavior Assessment System (29), Behavior Assessment System for Children (30)]. However, these measures are not based on the ICF, and therefore describe everyday function differently compared to ICF-based measures.
Operationalizing the ICF framework (i.e., its domains and the interactions between them) within measurement tools can create opportunities for the ICF to be widely utilized in clinical environments for children with NDD (14). It is unclear how many measures in the field of NDD are developed using the definitions and concepts of the ICF framework. It has been demonstrated in the literature that clinical measures can be mapped on or “linked” to the ICF framework by following a set of established and standardized rules, as described by Fayed et al. (31). With NDD interventions shifting to focus more specifically on strengths and support needs, there is a need for further description of how measures that purport to be function-focused are utilized in clinical systems. The focus of this study is directed toward examining how researchers who have developed ICF-based measures conceptualized their measure, specifically with whether and how the ICF domains were utilized in pediatric clinical contexts and research.
Methods
We undertook a narrative review and synthesis of the peer-reviewed literature to understand existing function-focused, ICF-based measures that are used with children diagnosed with NDD. A narrative review summarizes and describes previously published information with an interpretation of the contents of different studies using a comprehensive, critical and objective analysis (32, 33). This study was guided by SANRA, the Scale for the Assessment of Narrative Review Articles, specifically by reviewing the six items deemed necessary for a quality review: (1) justification of the review's importance for the reader; (2) review focus/aim(s); (3) description of literature search; (4) referencing; (5) scientific reasoning; and (6) relevant and appropriate endpoint/presentation data (33).
We used a two-stage approach to review the literature. The first stage was to identify original research texts that (a) focused on children (18 and younger) diagnosed with NDD defined by DSM-5, and (b) referenced the ICF framework. Both criteria needed to be stated within the abstract of the study. Initial keywords were generated for each conceptual category of the research aim with the guidance of a trained librarian in a health sciences library to form the search strategy. Keywords were identified within three categories (NDD diagnosis, child [age range 0–18], and ICF), and were used to search the following databases: Medline, PsycInfo, EMBASE, and EMCARE. Search terms were developed and customized for each database. Abstracts were then screened to identify whether any measures were used in an intervention study and/or discussed in the literature; we also required the clinical measure to be the focus of the abstract. Searches were restricted to both English language journals and publication date (2002-April 2021), as selected papers were required to be published post-publication of the ICF in 2001. Studies were excluded if the aim was to translate the measure to explore psychometric properties within an alternate language/country/context. Measures that were used within indirect care (i.e., measures that focused on data collection and/or inter-professional collaboration) were also excluded. Lastly, secondary studies (i.e., systematic reviews, scoping reviews) as well as editorials and commentaries were excluded. The titles and abstracts of the resulting articles from the database search were exported to Covidence (34), a reference managing software. Duplicate records were then deleted using the software.
The second stage required full-text screening to identify whether select measures were ICF-based, and to identify whether the study reported the development of the measure. If a study described an ICF-based measure but was not the original paper of the measure's development, hand-searching was conducted to retrieve the original article describing its development. Hand-searching for original articles was accomplished by looking at the reference lists of the indexed articles that had described the use of these measures within their abstracts. This task was also completed using Covidence (34).
This study used a matrix to extract key details including age ranges, context(s), diagnosis sample, as well as descriptions and psychometric properties of the measures described. Details and descriptions of these measures were determined by using its original development article. After the characteristics of the included measures were extracted, the original studies of the measures were analyzed again to extract ICF-related details, specifically regarding the ICF domain(s) that were prioritized by the measure and how this framework influenced the measure's initial conception. Measures were categorized by using the definitions of the four domains of the ICF framework (body structures and function, activities, participation, and contextual factors).
Results
The initial search identified 2811 published abstracts. After duplicates were removed, 1947 papers remained. These papers were reviewed by title and abstract with the first set of inclusion criteria, resulting in 141 potentially relevant studies. For the second stage, full-text versions of these studies were obtained and reviewed to assess whether they fit the second set of inclusion criteria, at which time 97 studies were excluded. Studies were excluded mainly for having a non-relevant focus—not focused on an ICF-based measure providing direct support for children with NDD; focusing on a non-pediatric sample; or being based on secondary data. The 44 papers that remained included 9 studies that described the initial development of an ICF-based measure, and 35 articles that described the use of ICF-based measures but were not the measure's original development paper, for which hand-searching was then necessary.
From the 35 articles, five additional ICF-based measures for children with NDD were identified and included; these comprised of four additional studies (35–38), and one manual (39). In total, 14 initial development studies describing 14 individual measures were included. This information is summarized using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart in Figure 2 (40).
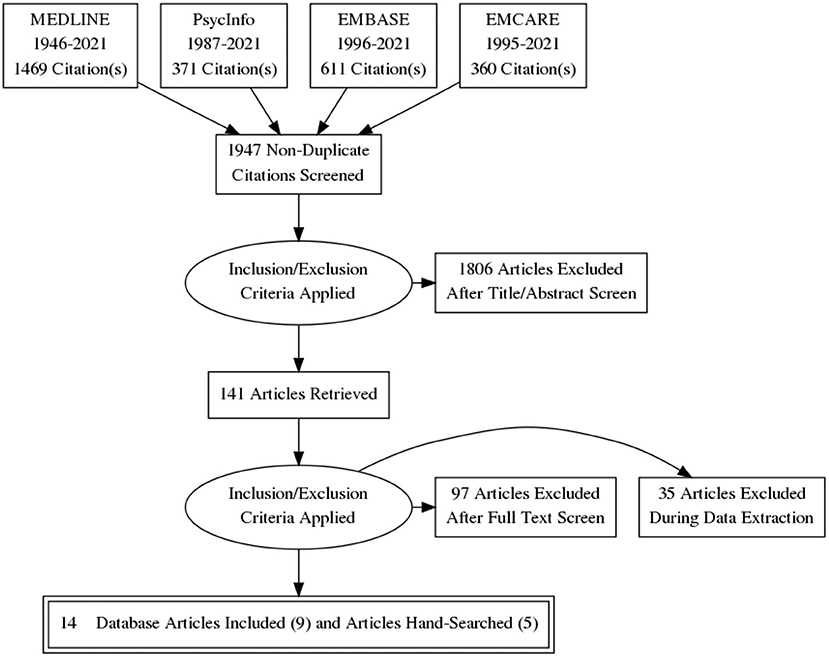
Figure 2. PRISMA (40) flowchart of search strategy.
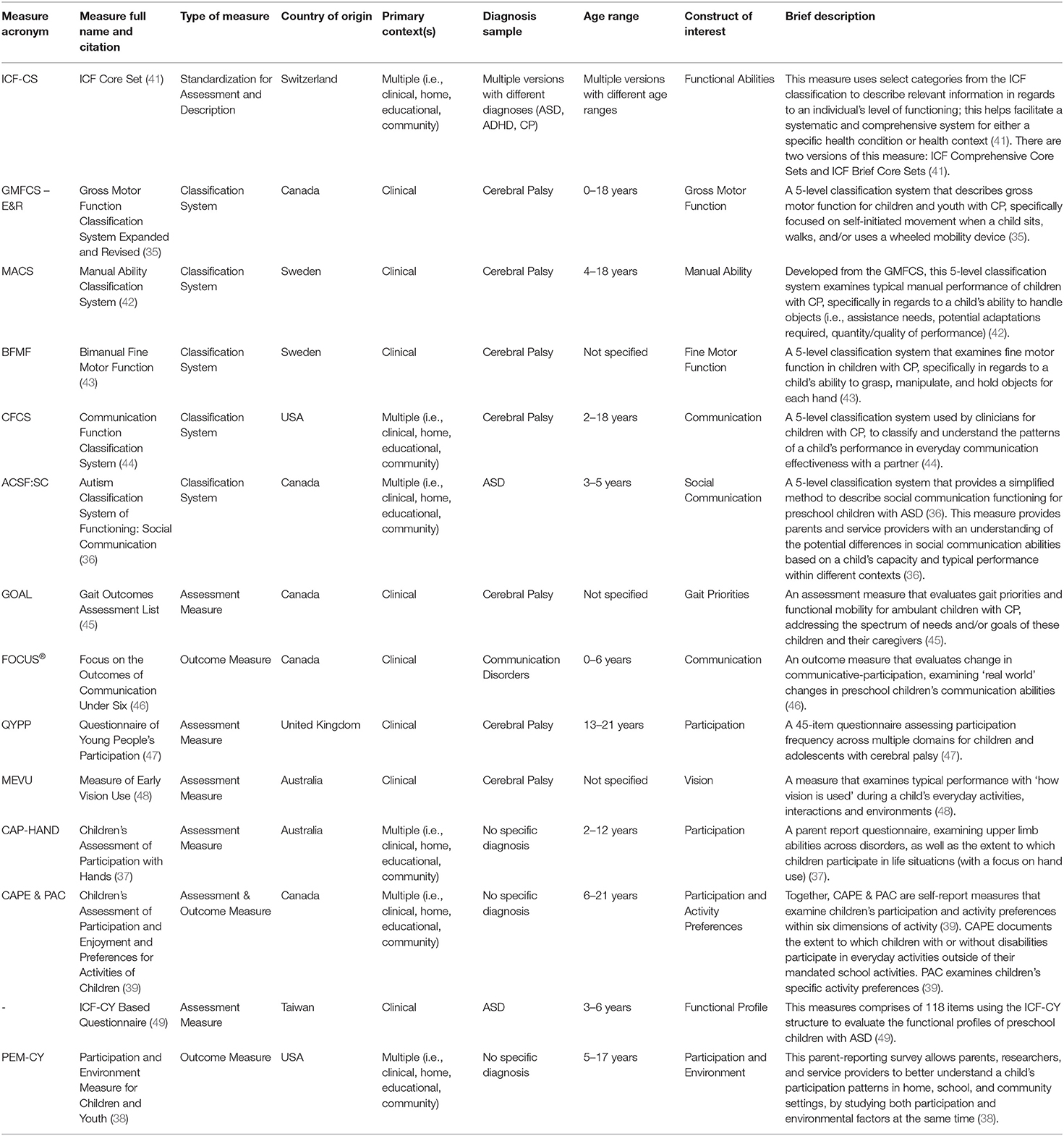
The 14 measures originated in seven countries including Canada, US, UK, Australia, Sweden, Switzerland, and Taiwan. These measures were predominately described as either assessment and/or outcome measures (64%, n = 9) or classification systems (36%, n = 5), and could be utilized in various contexts including home, community, educational, and clinical environments. The most common diagnosis was CP (50%, n = 7), followed by non-diagnostic/multiple diagnoses (29%, n = 4), ASD (14%, n = 2), and communication disorders (7%, n = 1). Age applicability of these measures ranged from 0 to 21 years. The diagnosis sample, age groups, and brief descriptions are reported in Table 1. The common characteristics of these measures are also described.
Assessment (and Outcome) Measures
The following nine ICF-based measures have a primary focus on the assessment of a specific construct of interest: ICF Core Sets (ICF-CS) (41), Gait Outcomes Assessment List (GOAL) (45), Focus on the Outcomes of Communication Under Six (FOCUS®) (46), Questionnaire of Young People's Participation (QYPP) (47), Measure of Early Vision Use (MEVU) (48), Children's Assessment of Participation with Hands (CAP-HAND) (37), Children's Assessment of Participation and Enjoyment & Preferences for Activities of Children (CAPE & PAC) (39), the ICF-CY Based Questionnaire (49), and the Participation and Environment Measure for Children and Youth (PEM-CY) (38). These types of measures describe details of functioning, can observe and evaluate a child's abilities and limitations within the construct of interest (otherwise referred to as outcome measures—a subset of assessment measures), and in some cases, it may be used to predict within-person change over time (26). These assessments can be completed by various individuals that are familiar with and/or are knowledgeable about the child's competencies within their daily routines, including caregivers, clinicians, and teachers (39). With the conceptual grounding of the ICF, these measures can provide a comprehensive and clinically useful understanding of a specific phenomenon, which can then be used for various applications within research and practice (39).
Classification Systems
The remaining five ICF-based measures are classification systems that can be used for children with NDD: Gross Motor Function Classification System Expanded & Revised (GMFCS-ER) (35), Manual Ability Classification System (MACS) (42), Bimanual Fine Motor Function (BFMF) (43), Communication Function Classification System (CFCS) (44), and Autism Classification System of Functioning: Social Communication (ACSF:SC) (36). The GMFCS-ER (35), MACS (42), BFMF (43), and CFCS (44) each individually describe functioning in children with CP based on specific constructs (i.e., gross motor function, manual ability, fine motor function, and communication), and the ACSF:SC (36) describes social communication functioning in children diagnosed with ASD. In these classification systems, level I typically describes child functioning with the highest level of ability in that aspect of functioning, whereas levels IV-V typically describe child functioning with more significant limitations (43). The five levels in these systems are ordinal, describing different levels of a child's abilities for a specific construct (36). It is important to note that the differences between these levels are not equal, as these systems provide a simplified guide for families and clinicians to communicate level of functioning within the clinical process (43).
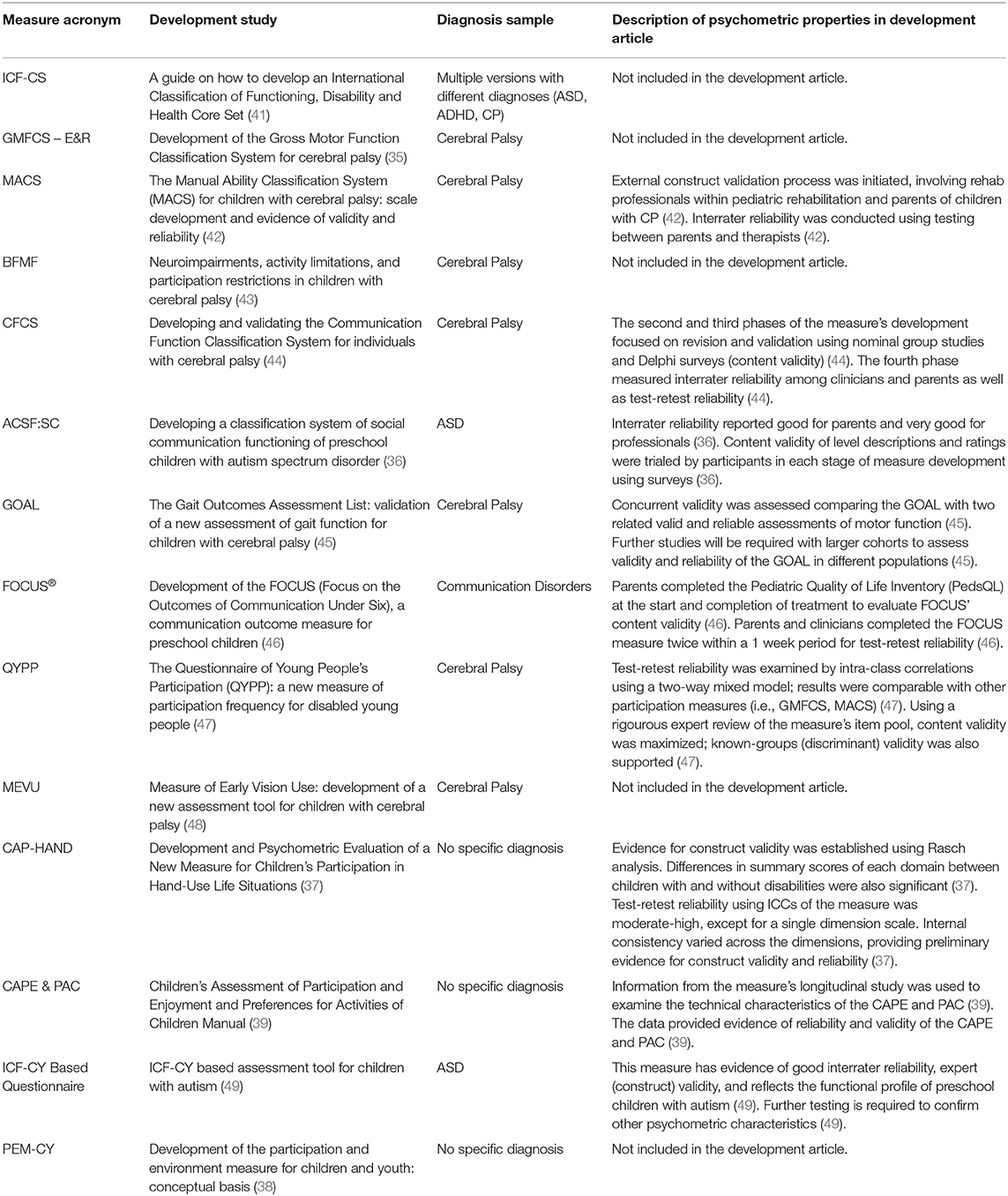
Psychometric Properties of Development Studies
The studies in which these measures were first established were published between 2002 and 2021. Almost all measures were initially published in journal articles (93%, n = 13), with one measure [CAPE & PAC (39)] described in a manual format. Most studies of these measures (64%, n = 9) provided some psychometric testing information during the measure's development. The most common forms of testing include content validity, interrater reliability, and test-retest reliability (29%, n = 4). Other types of psychometric testing include various types of construct validity testing, such as discriminant validity, expert validity, and concurrent validity (each 7%, n = 1) or were generally described as construct validity (14%, n = 2). The CAPE & PAC (39). Manual did not specify the type of reliability and validity results (see Table 2).
ICF Domains of Measures
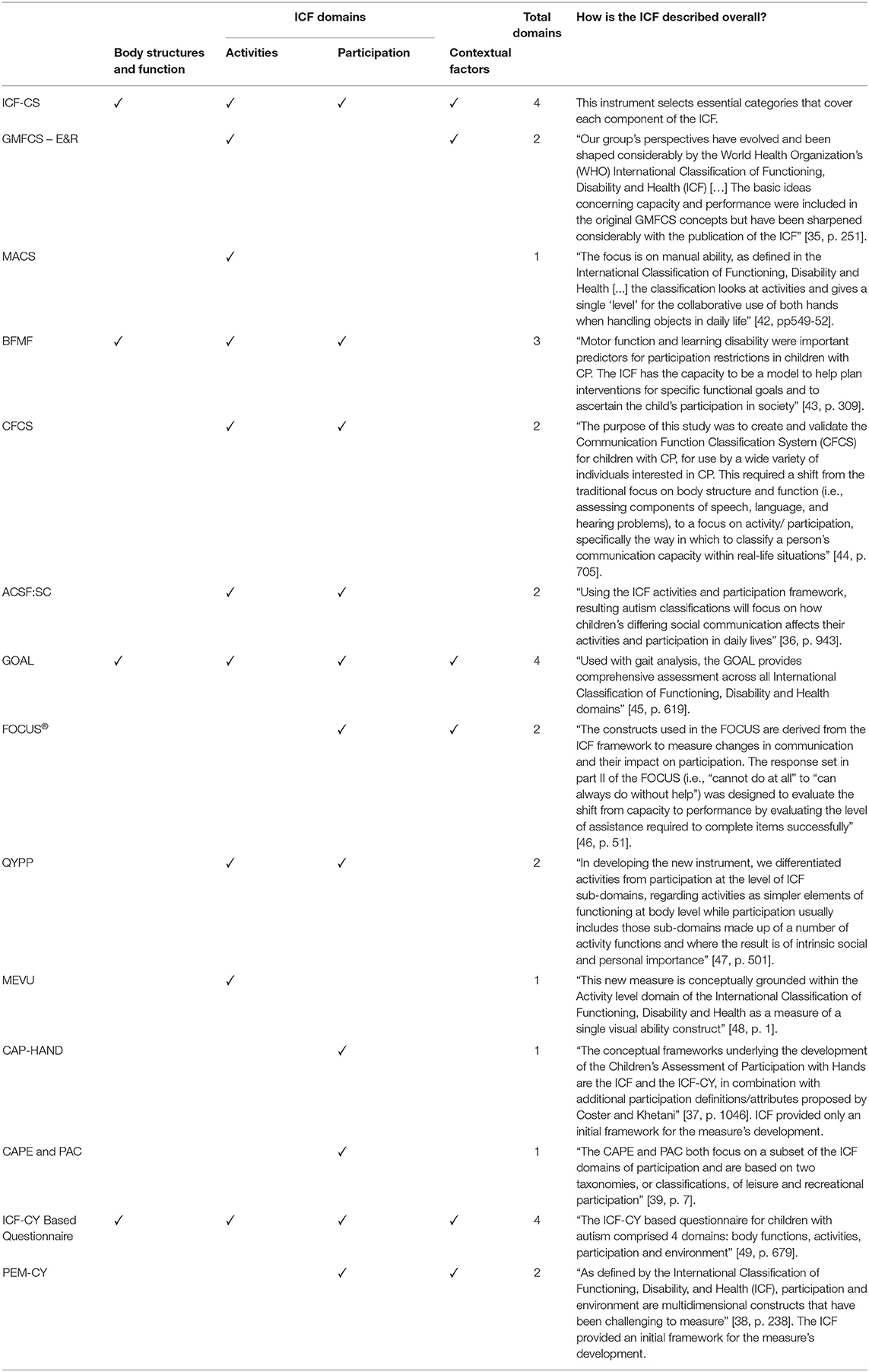
To understand the role of the ICF framework in the conception of these clinical measures, it was important to analyze what ICF domain(s) were prioritized, and the specific foundational concepts from the ICF framework during the initial development process (see Table 3). All listed measures included at least one domain of interest, and the ICF-CS (41), GOAL (45), and ICF-CY Based Questionnaire (49) using all four ICF domains. The most common domain across measures was Participation (79%, n = 11), followed by Activities (71%, n = 10), Contextual Factors (43%, n = 6), and Body Structures and Function (29%, n = 4). Seventy one percent of the measures (n = 10) used more than one domain of the ICF.
Discussion
This study is the first of which we are aware to identify ICF-based clinical measures for children with NDD. We have reported the psychometric properties and characteristics of 14 measures that are grounded in the ICF framework, using the information gathered from the initial development studies. We also identified the prominent ICF conceptual domain(s) that these measures represent, and the extent to which the framework was captured, including its interactive nature. There may be more ICF-based measures for this population that exist outside the clinical context (i.e., educational-based measures) and some of these tools may be applicable to other settings; however, the intent of this study was to examine how ICF-based clinical measures were operationalized in practice. Therefore, only health-focused databases were consulted.
The initial development studies for the selected measures included varying levels and types of psychometric properties conducted and described. Some studies [ICF-CS (41), GMFCS-ER (35), BFMF (43), MEVU (48), and PEM-CY (38)] placed emphasis on the process that the research team experienced when developing the measure, rather than describing specific psychometric characteristics of their measure. These studies had concurrent publications that described the conceptual processes and psychometric testing separately. The remaining studies combined psychometric testing with the measure's development process. The most common psychometric tests that were completed were interrater and test-retest reliability as well as content validity. It is important for clinical instruments to demonstrate good psychometric properties (27), and 64% of the measures were introduced with some form of psychometric testing conducted. These results provide a descriptive overview of the function-focused tools developed in the field of childhood NDD, but since potential subsequent psychometric studies were not included in this study, it is difficult to provide comment on the overall rigor of the state of function-focused tools in this field. Future research should examine levels of rigor found in the psychometric properties of the listed tools.
The 14 measures varied in their constructs of interest, age ranges, and diagnoses. These constructs ranged from very specific functional skills [i.e., BFMF: bimanual fine motor function (43)] to broader areas of interest [i.e., ICF-CY-Based Questionnaire: building a functional profile for children diagnosed with ASD (49)]. For age applicability, two measures [CAP-HAND (37) and CAPE & PAC (39)] had expanded upper-age ranges to 21 years old. Many measures focused on specific diagnoses: CP, ASD, and communication disorders. With the broad spectrum of diagnoses involved in DSM-5's definition of NDD, this highlights the need for great representation in other NDD populations. To fill these gaps, measures like the ICF-CS have been continually adapted with subsequent publications to explore the clinical utility of this measure in multiple communities within disability research and practice, including within NDD (50). These diagnosis-based populations include ASD, CP, and ADHD, but the outreach in these diagnosis populations continue to grow today (50, 51).
Furthermore, these results indicated that measures such as the CAP-HAND (37), CAPE & PAC (39), and PEM-CY (38) could be potentially used with any child or youth, regardless of whether they are diagnosed with any condition of NDD, as these measures are not diagnosis-specific. In addition, although a key population of the users of FOCUS® (46) is young children with communication disorders, this tool is designed to address communication needs across all young children with or without disabilities. These findings are important, as they illustrate function-focused measures that examine abilities across diagnoses/conditions – an emerging trend (15). With the various diagnoses categorized within NDD, these measures have a wider scope in reaching different communities, thus creating more opportunities to utilize the concepts of the ICF in clinical and research settings. It is important to note that the ICF is still considered a contemporary framework, and that measures are continuing to be developed, such as the MEVU (48) that was published 1 month prior to conducting the database search for this narrative review.
With the heterogeneity of functional abilities within NDD, and the emerging measures that are being developed without a focus on any specific diagnosis, non-diagnostic ICF-based measures create opportunities for further examination of the continuum of abilities across diagnoses. By doing so, the goal of these measures shifts toward capturing profiles of individual abilities as well as unique differences among children (12). Furthermore, there is some evidence in today's literature that indicates that neurological similarities (i.e., brain structure/activity) that may affect an individual's social communication abilities may exist across diagnoses such as autism and attention deficit hyperactivity disorder; this shows that a child's overall abilities may also overlap across diagnoses (52). This example can be used to challenge the ways in which we can define, diagnose, and “treat” NDD, specifically with how we approach functional perspectives for these populations (53). Measurement tools may still involve neurophysiological processes in their design, but by focusing on a more individualistic foundation, this shift in thinking may better suit the cultural direction of how function-focused care is understood with today's ideas (12). By utilizing these measures across the populations of NDD, we better understand the diversity in the needs of children within their communities. These needs may exist beyond the core domains (i.e., addressing participation needs), and can potentially extend to how we can utilize these measures to improve the overall quality of life of children with NDD (13, 27, 28). As the ICF promotes this understanding that these four domains can build a unique functional profile of a child, the ICF can be seen as a supporting resource within the use of family-centered care to support a child's individualized needs. When this type of care continues to play prominent roles in the design and development of intervention plans for these individuals with disabilities, this may need to be more apparent in the tools that we develop as well. This approach utilizes the biopsychosocial model and will be a more relevant application of the ICF. Furthermore, with children receiving school supports that are often integrated with health services, exploring function-focused measures that are applicable in educational settings, such as the Functional Abilities Classification Tool (54), is also important to examine in future work.
The development studies demonstrated variability in how ICF concepts were foundational within their measures. Some studies explicitly stated that their measure was conceptually based in the ICF whereas others used the ICF to develop their measure's items or constructs. Both the Participation and Activities domains were predominately represented throughout all measures whereas Contextual Factors and Body Structures and Function were not as prominent. The ICF-CS (41) and ICF-CY-Based Questionnaire (49) utilized a holistic approach of the framework rather than focusing on specific domains, and this is evident simply looking at the naming of these tools. Other measures utilize the ICF combined with other frameworks, such as the CAP-HAND (37), that uses the definitions provided by both the framework and what is described by the authors of the PEM-CY (38) to configure a definition for participation that is suitable for the needs of CAP-HAND (37). These results align with the literature, specifically regarding the shift in thinking the ICF proposes: this framework has motivated health service providers to focus beyond “body structures and functions” to include the other roles (i.e., activities, participation) that can impact a child's level of functioning and health (55, 56).
There are different ways that tools and measures interact with the components of the ICF, and some measures can still utilize this framework without using it for its conceptual basis. It is here that the use of the ICF linking rules may become more relevant, as the rules provides an effective method to link meaningful “concepts” of non-ICF-based measures to the most precise category(s) in the ICF framework (57). These concepts could describe health condition, functional activities or any of the contextual factors (31, 57). This “linking process” differentiates from what is being studied in this narrative review, in that we are examining the extent to which ICF-based measures involve the domains of the framework, and the dynamic interactions they capture. This review focused on identifying measures that used the ICF for the initial conception, rather than the measures that have only considered the ICF post-publication or in an “after-the-fact” exploration. With the linking process, the developers of non-ICF based measures undergo the steps required in understanding the ICF to link certain items of their measure to the most relevant domains of the framework (58). However, the use of linking individual concepts of a measure to the ICF framework may not be as effective in demonstrating the interaction between the concepts, especially between activities/participation and contextual factors (59). Of the identified measures, 71% utilized more than one domain of the ICF, often highlighting the various ways in which the nuanced interactions influenced the development of the tool. For example, the PEM-CY (38) evaluates both participation and environmental factors in different settings, and can provide problem-solving strategies to adjust contextual factors within these settings to support further participation (38). As described earlier, the dynamic nature of the interaction of these non-linear domains is one of the most easily identifiable components of the framework. Although there is variability with how these interactions are explicitly described, when a measure is ICF-based and correctly utilizes the framework as a core component, the interactions of the domains are more likely to be inherently captured within the use of the measure.
Limitations
There are a couple of limitations to report about this study. To begin, there were varying levels of psychometric data that emerged across the initial development studies of the selected measures. While psychometric testing of measures is an ongoing process, we recognize that the original development manuscripts would only have captured psychometric testing at its initial development, and that subsequent studies could have tested additional properties, potentially with other populations of children. We also recognize that the contributors of the development studies may have differed from the original developers of the measure. The aim of this review was to provide an overview of the current ICF-based measures developed for children with NDD, in which we focused on using the development studies as the main sources for this work.
A second limitation relates to study screening process. We selected measures that explicitly used the ICF in the screening of study abstracts in the identified health databases, either in the development study, or in a subsequent published study of the measure that was used to locate the original manuscript. Although there is the potential for other measures to incorporate the ICF framework in some capacity in the development and/or design of their measure, the focus of this work was to identify the measures that explicitly used the ICF and its domains as a foundational element in its work.
Conclusion
This narrative review can serve as a potential resource for clinicians/researchers looking to use measures grounded in the ICF framework for children with NDD. These 14 measures can play important roles in creating effective applications of the ICF for exploring child functioning in both research and practice (15, 54, 60). As measures are continuing to be developed using the ICF framework at their foundation, this emerging knowledge can help inform function-focused care. By understanding how function-focused care is operationalized within the measures that we create, we are also able to better understand functioning in clinical care for children with NDD, and whether there are gaps in what is measured. These gaps are also evident in NDD populations where these ICF-based tools are not applied. Future research can explore the expansion of existing ICF-based measures across NDD populations and ages (i.e., adults), in addition to examining measures that impact functioning in other childhood contexts (e.g., home and educational settings).
Author Contributions
KS completed the search and wrote the manuscript with support from BD, PR, and MZ. BD supervised the project, with help from PR and MZ as part of the supervising committee. PR, MZ, and BD conceived the original idea. All authors reviewed the results and contributed ideas to the final manuscript.
Funding
Funding support for this study was provided by the following: Hamilton Health Science Research Early Career Award (ECA) for BD (2018–2021), and the Innovation Fund of the Alternative Funding Plan for the Hamilton Academic Health Sciences Organization (HAHSO).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Laura Banfield and Dr. Stephen Gentles for their insight and guidance for helping build and advance this study.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Publishing (2013). doi: 10.1176/appi.books.9780890425596
2. Miller A, Shen J, Mâsse LC. Child Functional Characteristics Explain Child and Family Outcomes Better Than Diagnosis: Population-Based Study of Children with Autism or Other Neurodevelopmental Disorders/Disabilities. (2016). Available online at: https://www150.statcan.gc.ca/n1/pub/82-003-x/2016006/article/14635-eng.htm (accessed May 7, 2021).
3. Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, et al. Trends in the prevalence of developmental disabilities in US children. Pediatrics. (2011) 127:1034–42. doi: 10.1542/peds.2010-2989
4. Halfon N, Houtrow A, Larson K, Newacheck PW. The changing landscape of disability in childhood. Future Child. (2012) 22:13–42. doi: 10.1353/foc.2012.0004
5. Allard A, Fellowes A, Shilling V, Janssens A, Beresford B, Morris C. Key health outcomes for children and young people with neurodisability: qualitative research with young people and parents. BMJ Open. (2014) 4:e004611. doi: 10.1136/bmjopen-2013-004611
6. Anaby D, Hand C, Bradley L, Di Rezze B, Forhan M, DiGiacomo A, et al. The effect of the environment on participation of children and youth with disabilities: a scoping review. Disabil Rehabil. (2013) 35:1589–98. doi: 10.3109/09638288.2012.748840
7. King G, Law M, King S, Rosenbaum P, Kertoy MK, Young NL. A conceptual model of the factors affecting the recreation and leisure participation of children with disabilities. Phys Occup Pediatr. (2003) 23:63–90. doi: 10.1080/J006v23n01_05
8. World Health Organization. International Classification of Functioning, Disability and Health: ICF (2001). Available online at: https://apps.who.int/iris/handle/10665/42407 (accessed March 7, 2021).
9. Stucki G, Cieza A, Ewert T, Kostanjsek N, Chatterji S, Ustün TB. Application of the international classification of functioning, disability and health (ICF) in clinical practice. Disabil Rehabil. (2002) 24:281–2. doi: 10.1080/09638280110105222
10. Miller AR, Rosenbaum P. Perspectives on “disease” and “disability” in child health: the case of childhood neurodisability. Front Public Health. (2016) 4:226. doi: 10.3389/fpubh.2016.00226
11. Lee AM. Using the ICF-CY to organise characteristics of children's functioning. Disabil Rehabil. (2011) 33:605–16. doi: 10.3109/09638288.2010.505993
12. Simeonsson RJ, Leonardi M, Lollar D, Bjorck-Akesson E, Hollenweger J, Martinuzzi A. Applying the international classification of functioning, disability and health (ICF) to measure childhood disability. Disabil Rehabil. (2003) 25:602–10. doi: 10.1080/0963828031000137117
13. McDougall J, Wright V, Rosenbaum P. The ICF model of functioning and disability: incorporating quality of life and human development. Dev Neurorehabil. (2010) 13:204–11. doi: 10.3109/17518421003620525
14. Miller A, Shen J, Mâsse LC. Child functional characteristics explain child and family outcomes better than diagnosis: population-based study of children with autism or other neurodevelopmental disorders/disabilities. Health Rep. (2016) 27:9–18. Available online at: https://www150.statcan.gc.ca/n1/pub/82-003-x/2016006/article/14635-eng.pdf
15. Castro S, Ferreira T, Dababnah S, Pinto AI. Linking autism measures with the ICF-CY: functionality beyond the borders of diagnosis and interrater agreement issues. Dev Neurorehabil. (2013) 16:321–31. doi: 10.3109/17518423.2012.733438
16. Simeonsson RJ. ICF-CY: a universal tool for documentation of disability. J Policy Pract Intellect Disabil. (2009) 6:70–2. doi: 10.1111/j.1741-1130.2009.00215.x
17. Dajani DR, Llabre MM, Nebel MB, Mostofsky SH, Uddin LQ. Heterogeneity of executive functions among comorbid neurodevelopmental disorders. Sci Rep. (2016) 6:36566. doi: 10.1038/srep36566
18. Kapp SK, Gillespie-Lynch K, Sherman LE, Hutman T. Deficit, difference, or both? Autism and neurodiversity. Dev Psychol. (2013) 49:59–71. doi: 10.1037/a0028353
19. Bumiller K. Quirky citizens: autism, gender, and reimagining disability. Signs J Women Cult Soc. (2008) 33:967–91. doi: 10.1086/528848
20. Baron-Cohen S. Editorial perspective: neurodiversity - a revolutionary concept for autism and psychiatry. J Child Psychol Psychiatry. (2017) 58:744–7. doi: 10.1111/jcpp.12703
21. Darrah J, Law MC, Pollock N, Wilson B, Russell DJ, Walter SD, et al. Context therapy: a new intervention approach for children with cerebral palsy. Dev Med Child Neurol. (2011) 53:615–20. doi: 10.1111/j.1469-8749.2011.03959.x
22. Ostensjø S, Carlberg EB, Vøllestad NK. Everyday functioning in young children with cerebral palsy: functional skills, caregiver assistance, and modifications of the environment. Dev Med Child Neurol. (2003) 45:603–12. doi: 10.1111/j.1469-8749.2003.tb00964.x
23. Ketelaar M, Vermeer A, Helders PJ. Functional motor abilities of children with cerebral palsy: a systematic literature review of assessment measures. Clin Rehabil. (1998) 12:369–80. doi: 10.1191/026921598673571117
24. McConachie H, Parr JR, Glod M, Hanratty J, Livingstone N, Oono IP, et al. Systematic review of tools to measure outcomes for young children with autism spectrum disorder. Health Technol Assess. (2015) 19:1–506. doi: 10.3310/hta19410
25. Resnick B, Galik E, Boltz M. Function focused care approaches: literature review of progress and future possibilities. J Am Med Dir Assoc. (2013) 14:313–8. doi: 10.1016/j.jamda.2012.10.019
26. Rosenbaum P. The ABC s of clinical measures. Dev Med Child Neurol. (2015) 57:496. doi: 10.1111/dmcn.12735
27. Waters E, Davis E, Ronen GM, Rosenbaum P, Livingston M, Saigal S. Quality of life instruments for children and adolescents with neurodisabilities: how to choose the appropriate instrument. Dev Med Child Neurol. (2009) 51:660–90. doi: 10.1111/j.1469-8749.2009.03324.x
28. Sparrow SS, Cicchetti DV, Saulnier CA. Vineland Adaptive Behavior Scales. Third Edition (Vineland-3) San Antonio: Pearson (2016).
29. Harrison P, Oakland T. Adaptive Behavior Assessment System (ABAS-3). San Antonio: The Psychological Corporation (2015).
30. Reynolds CR, Kamphaus RW. Behavior Assessment System for Children. 3rd ed. Bloomington: Pearson (2015).
31. Fayed N, Cieza A, Bickenbach JE. Linking health and health-related information to the ICF: a systematic review of the literature from 2001 to 2008. Disabil Rehabil. (2011) 33:1941–51. doi: 10.3109/09638288.2011.553704
32. Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. (2006) 5:101–17. doi: 10.1016/S0899-3467(07)60142-6
33. Baethge C, Goldbeck-Wood S, Mertens S. SANRA—a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. (2019) 4:5. doi: 10.1186/s41073-019-0064-8
34. Veritas Health Innovation. Covidence Systematic Review Software. (2021). Available online at: www.covidence.org (accessed March 27, 2021).
35. Rosenbaum PL, Palisano RJ, Bartlett DJ, Galuppi BE, Russell DJ. Development of the gross motor function classification system for cerebral palsy. Dev Med Child Neurol. (2008) 50:249–53. doi: 10.1111/j.1469-8749.2008.02045.x
36. Di Rezze B, Rosenbaum P, Zwaigenbaum L, Hidecker MJ, Stratford P, Cousins M, et al. Developing a classification system of social communication functioning of preschool children with autism spectrum disorder. Dev Med Child Neurol. (2016) 58:942–8. doi: 10.1111/dmcn.13152
37. Chien CW, Rodger S, Copley J. Development and psychometric evaluation of a new measure for children's participation in hand-use life situations. Arch Phys Med Rehabil. (2015) 96:574–83. doi: 10.1016/j.apmr.2014.11.013
38. Coster W, Law M, Bedell G, Khetani M, Cousins M, Teplicky R. Development of the participation and environment measure for children and youth: conceptual basis. Disabil Rehabil. (2012) 34:238–46. doi: 10.3109/09638288.2011.603017
39. King G, Law M, King S, Hurley P, Hanna S, Kertoy M, et al. Children's Assessment of Participation and Enjoyment (CAPE) and Preferences for Activities of Children (PAC). San Antonio: Harcourt Assessment Inc (2004).
40. Page MJ, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
41. Selb M, Escorpizo R, Kostanjsek N, Stucki G, Üstün B, Cieza A. A guide on how to develop an international classification of functioning, disability and health core set. Euro J Phys Rehabil Med. (2015) 51:105–17. Available online at: https://www.minervamedica.it/en/journals/europa-medicophysica/article.php?cod=R33Y2015N01A0105
42. Eliasson AC, Krumlinde-Sundholm L, Rösblad B, Beckung E, Arner M, Ohrvall AM, et al. The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol. (2006) 48:549–54. doi: 10.1111/j.1469-8749.2006.tb01313.x
43. Beckung E, Hagberg G. Neuroimpairments, activity limitations, and participation restrictions in children with cerebral palsy. Dev Med Child Neurol. (2002) 44:309–16. doi: 10.1111/j.1469-8749.2002.tb00816.x
44. Hidecker MJ, Paneth N, Rosenbaum PL, Kent RD, Lillie J, Eulenberg JB, et al. Developing and validating the communication function classification system for individuals with cerebral palsy. Dev Med Child Neurol. (2011) 53:704–10. doi: 10.1111/j.1469-8749.2011.03996.x
45. Thomason P, Tan A, Donnan A, Rodda J, Graham HK, Narayanan U. The gait outcomes assessment list (GOAL): validation of a new assessment of gait function for children with cerebral palsy. Dev Med Child Neurol. (2018) 60:618–23. doi: 10.1111/dmcn.13722
46. Thomas-Stonell NL, Oddson B, Robertson B, Rosenbaum PL. Development of the FOCUS (Focus on the outcomes of communication under six), a communication outcome measure for preschool children. Dev Med Child Neurol. (2010) 52:47–53. doi: 10.1111/j.1469-8749.2009.03410.x
47. Tuffrey C, Bateman BJ, Colver AC. The questionnaire of young people's participation (QYPP): a new measure of participation frequency for disabled young people. Child Care Health Dev. (2013) 39:500–11. doi: 10.1111/cch.12060
48. Deramore Denver B, Froude E, Rosenbaum P, Imms C. Measure of early vision use: development of a new assessment tool for children with cerebral palsy. Disabil Rehabil. (2021) 1–11. doi: 10.1080/09638288.2021.1890241
49. Gan SM, Tung LC, Yeh CY, Wang CH. ICF-CY based assessment tool for children with autism. Disabil Rehabil. (2013) 35:678–85. doi: 10.3109/09638288.2012.705946
50. Schiariti V, Mahdi S, Bölte S. International classification of functioning, disability and health core sets for cerebral palsy, autism spectrum disorder, and attention-deficit-hyperactivity disorder. Dev Med Child Neurol. (2018) 60:933–41. doi: 10.1111/dmcn.13922
51. Bölte S, de Schipper E, Robison JE, Wong VC, Selb M, Singhal N, et al. Classification of functioning and impairment: the development of ICF core sets for autism spectrum disorder. Autism Res. (2014) 7:167–72. doi: 10.1002/aur.1335
52. Kushki A, Anagnostou E, Hammill C, Duez P, Brian J, Iaboni A, et al. Examining overlap and homogeneity in ASD, ADHD, and OCD: a data-driven, diagnosis-agnostic approach. Transl Psychiatry. (2019) 9:318. doi: 10.1038/s41398-019-0631-2
53. Baribeau DA, Dupuis A, Paton TA, Hammill C, Scherer SW, Schachar RJ, et al. Structural neuroimaging correlates of social deficits are similar in autism spectrum disorder and attention-deficit/hyperactivity disorder: analysis from the POND network. Transl Psychiatry. (2019) 9:72. doi: 10.1038/s41398-019-0382-0
54. Klein B, Kraus de Camargo. A proposed functional abilities classification tool for developmental disorders affecting learning and behaviour. Front Educ. (2018) 3:2. doi: 10.3389/feduc.2018.00002
55. Cunningham BJ, Washington KN, Binns A, Rolfe K, Robertson B, Rosenbaum P. Current methods of evaluating speech-language outcomes for preschoolers with communication disorders: a scoping review using the ICF-CY. J Speech Lang Hear Res. (2017) 60:447–64. doi: 10.1044/2016_JSLHR-L-15-0329
56. McLeod S, Threats TT. The ICF-CY and children with communication disabilities. Int J Speech Lang Pathol. (2008) 10:92–109. doi: 10.1080/17549500701834690
57. Cieza A, Fayed N, Bickenbach J, Prodinger B. Refinements of the ICF linking rules to strengthen their potential for establishing comparability of health information. Disabil Rehabil. (2019) 41:574–83. doi: 10.3109/09638288.2016.1145258
58. Cerniauskaite M, Quintas RUI, Boldt C, Raggi A, Cieza A, Bickenbach JE, et al. Systematic literature review on ICF from 2001 to 2009: its use, implementation and operationalisation. Disabil Rehabil. (2011) 33:281–309. doi: 10.3109/09638288.2010.529235
59. Ballert CS, Hopfe M, Kus S, Mader L, Prodinger B. Using the refined ICF linking rules to compare the content of existing instruments and assessments: a systematic review and exemplary analysis of instruments measuring participation. Disabil Rehabil. (2019) 41:584–600. doi: 10.1080/09638288.2016.1198433
60. Moran M, Bickford J, Barradell S, Scholten I. Embedding the international classification of functioning, disability and health in health professions curricula to enable interprofessional education and collaborative practice. J Med Educ Curric Dev. (2020) 7:2382120520933855. doi: 10.1177/2382120520933855
Keywords: children, neurodevelopmental disabilities, clinical measures, ICF, NDD
Citation: Shanmugarajah K, Rosenbaum P, Zubairi M and Di Rezze B (2021) A Narrative Review of Function-Focused Measures for Children With Neurodevelopmental Disorders. Front. Rehabilit. Sci. 2:709978. doi: 10.3389/fresc.2021.709978
Received: 14 May 2021; Accepted: 02 July 2021;
Published: 29 July 2021.
Edited by:
Liane Simon, Medical School Hamburg, GermanyReviewed by:
Julia Schuchard, Children's Hospital of Philadelphia, United StatesPatricia Welch Saleeby, Bradley University, United States
Copyright © 2021 Shanmugarajah, Rosenbaum, Zubairi and Di Rezze. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kajaani Shanmugarajah, c2hhbm11Z2tAbWNtYXN0ZXIuY2E=
†Senior author
 Kajaani Shanmugarajah
Kajaani Shanmugarajah Peter Rosenbaum
Peter Rosenbaum Mohammad Zubairi
Mohammad Zubairi Briano Di Rezze
Briano Di Rezze