
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 31 March 2025
Sec. Digital Public Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1568043
This article is part of the Research TopicAssistive Technologies in Aging and DisabilityView all 5 articles
 Yujiao Shao1
Yujiao Shao1 Xiumu Yang1,2*
Xiumu Yang1,2* Qin Chen3
Qin Chen3 Hongyan Guo4
Hongyan Guo4 Xiaocui Duan1
Xiaocui Duan1 Xuejun Xu1
Xuejun Xu1 Jianxing Yue5
Jianxing Yue5 Zeyu Zhang6
Zeyu Zhang6 Shuang Zhao7
Shuang Zhao7 Shiqing Zhang1
Shiqing Zhang1Objective: This study aimed to identify the factors influencing digital health literacy in older adult patients with chronic diseases.
Methods: A descriptive qualitative approach incorporated purposive and snowball sampling methods. Semi-structured interviews were conducted with 32 older adult patients with chronic diseases from three hospitals in Anhui Province between October 2023 and May 2024. Data were coded and analyzed using Nvivo 12.0 software and content analysis.
Results: Two main themes and nine subthemes emerged: driving factors: these include the accessibility of digital health resources, perceived value and management needs, family economic and social benefits, and social network support systems. Restricting factors: These include cognitive blind spots and understanding biases, basic skills and challenges in digital adaptation, psychosocial limitations, issues with health information quality, and concerns about digital security risks.
Conclusion: The digital health literacy of older adult patients with chronic diseases is generally low, characterized by cognitive blind spots, and influenced by various personal and social factors. It is recommended to engage social forces, optimize the accessibility and applicability of digital health resources, create a supportive digital health environment, and help older adult patients improve their digital health literacy to enhance chronic disease self-management through digital health technology.
By the end of 2023, China’s population aged 60 and above reached 297 million, accounting for 21.1% of the total population. Among them, 217 million were aged 65 and above, comprising 15.4% of the total population (1). This proportion is expected to rise to 30% by 2050 (2), highlighting the deepening trend of population aging in China (3). As aging intensifies, the prevalence of chronic non-communicable diseases (NCDs) continues to grow. NCDs, characterized by high prevalence, long-term disease progression, suboptimal disease management outcomes, and substantial economic burden, pose significant threats to public health and socio-economic development. Globally, NCDs cause approximately 41 million deaths annually, accounting for 74% of all deaths (4). In China, over 80% of deaths are attributed to NCDs. Older adult individuals with NCDs often face high prevalence rates, multiple comorbidities, mental health challenges, and increased disability and mortality rates, complicating self-management.
Chronic disease self-management involves patients adopting self-management strategies under healthcare professional guidance to control disease progression. This includes preventive and therapeutic behaviors to address the physical and emotional challenges of NCDs in daily life (5). Effective chronic disease self-management can prevent disease deterioration and complications. The demand for telemedicine, health management, and personalized medical services among older adult patients with NCDs is steadily increasing. However, China continues to face significant challenges in preventing, treating, and managing NCDs (3, 6).
Amid global digitalization, the World Health Organization (WHO) published the Global Strategy on Digital Health (2020–2025), establishing digital health governance as a global priority (7). China’s healthcare services are transitioning toward digital health (8, 9). Digital health technologies enhance health management, advance personalized medicine, and facilitate health information exchange. However, as digital health technologies evolve, they create opportunities to address aging-related challenges while increasing demands on older adult patients’ self-management. Digital health literacy is the ability to obtain, assess, use, and communicate health information through digital technologies. It plays a crucial role in health promotion and disease management (10, 11).
Despite advancements in digital healthcare, access remains unequal. Digitally disadvantaged populations struggle to access these services, worsening health disparities (12, 13). International research has identified factors such as gender, age, education, technology experience, location, and health status as key influences on digital health literacy (14). Higher digital health literacy correlates with better quality of life in heart failure patients (15). Qualitative studies reveal older adult individuals’ concerns about digital health, including technological adaptability, information credibility, cost, motivation, and telemedicine feasibility (16). Recent digital health literacy research has shifted from individual skills to social and organizational influences, highlighting its role in health equity (17).
In China, digital health literacy research emerged later, initially focusing on quantitative studies and tool development (10, 18, 19). Studies have focused on students (20), the general public (21), pregnant women (22), the older adults (23–25), and chronic disease patients (26). Studies show that older adult individuals in China have low digital health literacy limited digital health adoption, and poor usage outcomes, creating barriers to healthcare integration (10, 23, 24). Limited research on digitally disadvantaged older adult chronic disease patients hinders understanding of digital health literacy influences and mechanisms. Digital health literacy determinants vary across socio-cultural contexts.
Qualitative research systematically explores individuals’ lived experiences through textual narratives. It uses an inductive approach, focusing on holism, deep understanding, individuality, and social-psychological meaning (27). The Social-Ecological Systems Theory (SET) (28, 29) posits that individual capabilities develop through interactions within environmental systems: the microsystem (personal factors), mesosystem (social support), and macrosystem (community and policy).
This study applies qualitative research within SET to examine digital health literacy determinants and mechanisms among older adult chronic disease patients in China at individual, interpersonal, and societal levels. Findings will inform evidence-based intervention strategies.
This study used purposive sampling combined with snowball sampling to recruit older adult patients with chronic diseases from three hospitals in Anhui Province between October 2023 and May 2024. The inclusion criteria were: (1) age ≥ 60 years; (2) a confirmed chronic disease diagnosis based on ICD-10 criteria; including but not limited to hypertension, diabetes mellitus, coronary artery disease, cancer, chronic obstructive pulmonary disease, and osteoarthritis; (3) own or have access to a digital device (e.g., accessing the internet via a smartphone) and be able to use it independently or with assistance from others; (4) clear consciousness and normal communication or reading abilities; (5) informed consent and willingness to participate. Exclusion criteria included: (1) severe cognitive, linguistic, auditory, or mental impairments; (2) being in an acute phase of a major illness or critical condition with severe complications; (3) extended or difficult communication issues; (4) concurrent participation in other studies. This study followed the principle of maximum variation sampling, selecting participants based on diverse factors, including age, gender, residence, education level, number of chronic diseases, perception of digital health information, and scores on the Digital Health Literacy Assessment Scale (10). This approach ensured sample representativeness and enhanced diversity.
The sample size was determined using the principles of data adequacy and information saturation, assessed through both data and theoretical saturation. Data saturation was reached when no new information emerged, interview content became repetitive, and similar responses were frequently observed, indicating that further data collection was unnecessary (30). Theoretical saturation occurred when no new themes or insights emerged, and all relevant concepts, attributes, and interrelationships had been thoroughly explored, suggesting additional data would not contribute to new theoretical understanding (31). Throughout the study, the research team continuously analyzed interview data to assess saturation. After the 30th interview, no new information or concepts emerged, confirming data saturation. To further validate this, two additional interviews were conducted. In total, 32 patients participated in the study. Data were collected through face-to-face semi-structured interviews, and participants were assigned unique identifiers (N1–N32) in accordance with privacy protection guidelines.
Detailed demographic information is provided in Table 1. Among the 32 patients, hypertension was the most common chronic disease, accounting for the highest proportion. The differences in chronic disease types were statistically significant (χ2 = 73.71, df = 10, p < 0.0001; Table 2). Smartphones were the most widely used digital devices, representing the dominant choice. The differences in the number of digital devices used were also statistically significant (χ2 = 66.71, df = 7, p < 0.0001; Table 3). The study was approved by the Ethics Committee of Bengbu Medical University (Approval No. [2023]369). All participants voluntarily participated and signed informed consent forms.
The Unified Theory of Acceptance and Use of Technology (UTAUT) (32) posits that performance and effort expectations, social influence, and facilitating conditions shape individuals’ willingness to adopt technology, influencing adoption behavior. Additionally, age, gender, experience, and voluntariness of use moderate these relationships. In essence, individuals’ perceptions and attitudes toward digital technology affect their intention to use it, ultimately determining their actual usage. Using the UTAUT model, the research team developed a preliminary interview guide based on a literature review and brainstorming discussions. A pre-interview was conducted with three older adult patients meeting the inclusion criteria (not included in the final study sample). After discussions with clinical nursing experts, the guide was revised and finalized. During formal interviews, researchers adjusted the guide as needed to enhance depth and flexibility.
The finalized interview guide included the following questions: (1) How do you define digital health literacy? (Regardless of the interviewee’s familiarity with the concept, the researcher provided a standardized definition to ensure a shared understanding before further discussion.) (2) What channels do you typically use to obtain health information and manage your health? (3) What are the advantages or concerns of using these channels for health information or management? (4) What difficulties have you encountered in obtaining health information or managing your health through these channels? (5) What factors do you think influence digital health literacy levels? (6) Would you like to improve your digital health literacy? Why or why not? (7) If digital health literacy training were available, what content would you like to learn? Do you have suggestions for the format or content of the training? (8) Do you have any additional thoughts or comments beyond the above topics?
The study strictly followed the COREQ (Consolidated Criteria for Reporting Qualitative Research) guidelines (33). The COREQ statement for this study is shown in Table 4. Data were collected through face-to-face semi-structured in-depth interviews (34).
Before data collection, a research team was formed, consisting of two master’s students in nursing and a qualitative research expert with over 30 years of teaching experience (a professor and graduate supervisor). All team members received systematic training in qualitative research and collaborated on data collection, organization, and analysis.
Before the interviews, researchers obtained approval from the hospital department and participated in daily nursing activities to familiarize themselves with participants’ language habits and cultural backgrounds, fostering trust. They explained the study’s objectives, methods, and procedures, including recording requirements and confidentiality assurances, ensuring participants fully understood the study and provided written informed consent. Interviews were scheduled at the participants’ convenience and lasted 20–30 min. They were typically conducted in a quiet, private consultation room within the hospital to minimize disruptions.
During the interviews, researchers maintained neutrality, guided participants with open-ended questions, used probing techniques flexibly, and encouraged participants to express their genuine views, and participants’ responses were repeated or summarized for clarity. Researchers also observed and recorded participants’ facial expressions and body movements to capture meaningful non-verbal information. After each session, researchers wrote interview diaries to summarize and reflect, continuously improving the interview quality.
This study used the triangulation method to analyze data by integrating multiple sources, including research data, researchers, theoretical frameworks, and methodologies. This approach ensured cross-validation of findings, enhancing the study’s reliability and validity (35, 36). Participants were recruited from three hospitals in Anhui, ensuring a representative and diverse sample. Two nursing master’s students transcribed interview recordings within 24 h and invited participants to verify the transcripts for accuracy and authenticity. For data analysis, researchers used Nvivo 12.0 software combined with manual coding. Following the UTAUT, two nursing master’s students independently conducted a content analysis (37), repeatedly coding and comparing data to minimize omissions and bias. A qualitative research expert resolved any discrepancies through discussion, ensuring consensus before finalizing the results.
The data analysis followed these steps: (1) Researchers repeatedly listened to recordings and thoroughly reviewed transcripts, maintaining neutrality for an in-depth understanding of the data.(2) Identifying and extracting meaningful statements related to factors influencing digital health literacy as the smallest unit of analysis.(3) Performing open coding to extract concepts from meaningful statements.(4) Grouping related codes into themes and sub-themes, supported by examples to generate the research findings. The main interview results are summarized in Table 5.
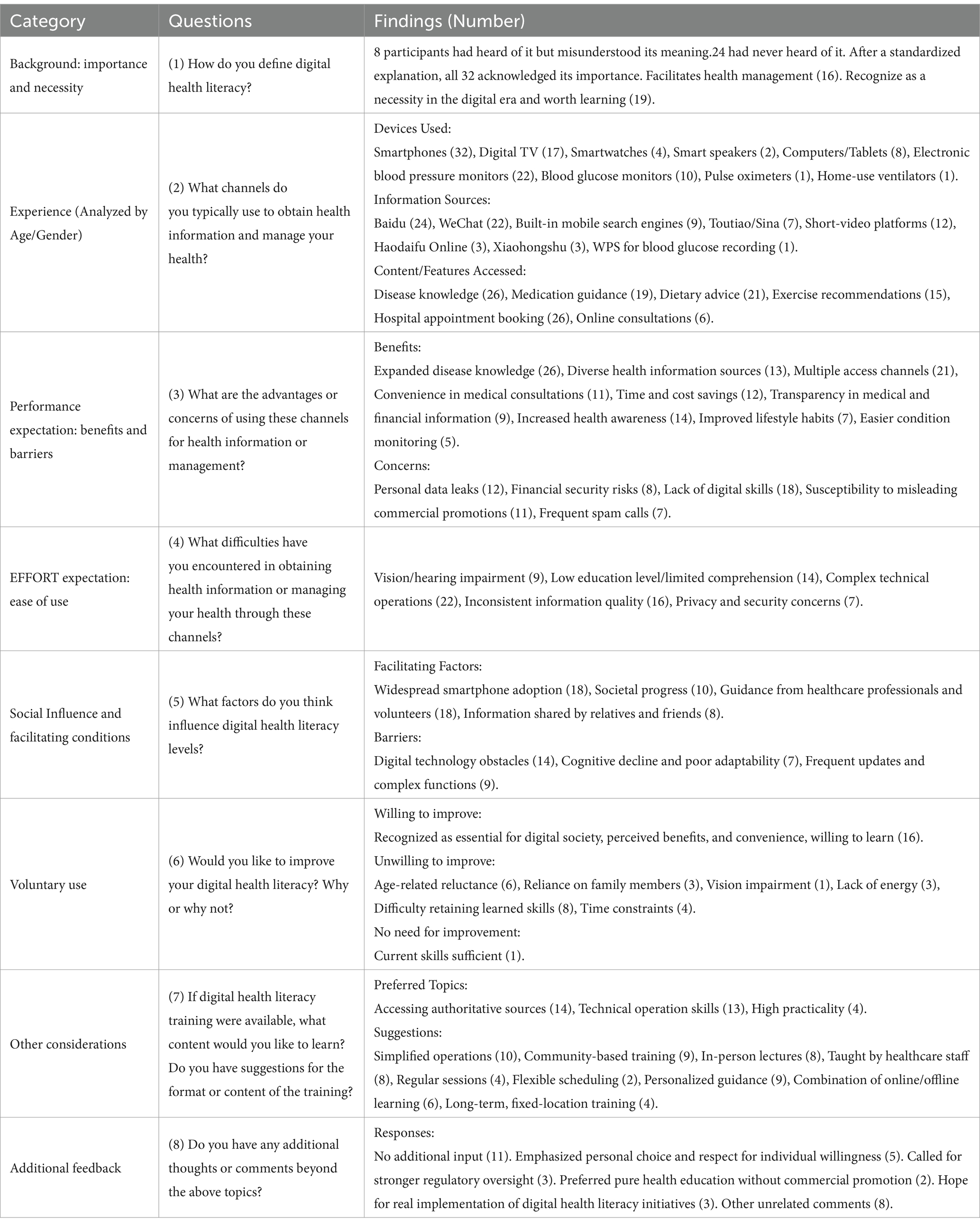
Table 5. Summary of semi-structured interview findings on digital health literacy in older adults with chronic diseases.
Based on the UTAUT model, factors influencing digital health literacy in older adult patients with chronic diseases were classified into two main themes and nine sub-themes, as outlined below.
Older adult patients with chronic diseases access health information through various digital platforms, including search engines, social media, news websites, and health-related mobile applications. Most respondents reported frequently using smartphones to obtain health knowledge, seek medical consultations, and manage chronic conditions. For instance, N2 and N3 stated, “WeChat, Baidu, Toutiao, Douyin, Haokan Video, and Xiaohongshu are all very convenient.” N7 and N9 added, “Now, as soon as I open my phone, I can access Sina News and Alipay—it’s very convenient.” N11 and N14 noted, “In the past, when I had a problem, I did not know who to ask. Now, I can just search on Baidu, saving me trips to the hospital.”
Some respondents also relied on health-related mobile applications for professional information and short video platforms for wellness education. For example, N13 stated, “I enjoy listening to ‘Ximalaya’ and watching Douyin.” N16 mentioned, “The nurses in my department recommended the hospital’s official WeChat account.” N21 added, “I use WPS to record my blood sugar levels.”
These findings suggest that older adults are increasingly turning to digital sources for health information. Their platform preferences are influenced by ease of use, content presentation, and specific health information needs. Short video platforms, for instance, offer accessible and easily digestible health education, reducing cognitive burden while enhancing engagement. Additionally, some respondents preferred official sources, such as hospital WeChat accounts or professional health applications, to ensure credibility.
For some older adults, limited access to offline medical services poses a challenge, whereas digital health resources help bridge this gap. Many respondents reported using online sources to obtain information on diet, exercise, and medication, as well as digital health tools (e.g., electronic blood pressure monitors and smart wristbands) to track their health. These technologies overcome traditional constraints of time and location, allowing patients to access guidance anytime, anywhere, and promoting proactive health management.
For example, N24 stated, “My home is far from the hospital, and getting there is difficult.” N30 mentioned, “Doctors from the town visit our village for check-ups, but they leave right after, making follow-ups difficult.” N7 and N31 shared, “We can check medication side effects at any time and learn how to recover after chemotherapy.” N26 demonstrated, “(Showing the device) I use a mobile app and a smart wristband to monitor my heart rate, breathing, and step count at any time.” N14 and N18 noted, “We have electronic blood pressure monitors and glucose meters at home, so we can measure them anytime—they are very practical.”
These findings underscore the value of digital health resources as a vital supplement in chronic disease management. For patients in remote areas or those with mobility limitations, online health information and digital monitoring devices enhance their ability to make informed healthcare decisions. However, individual differences in digital health literacy remain evident. While information acquisition is now more convenient, challenges persist in filtering and understanding health information, as well as in mastering digital health tools.
Most respondents believed that improving digital health literacy benefits health information access, disease awareness, and chronic disease management. Many emphasized that higher digital health literacy allows them to take a proactive approach to understanding their health, reducing uncertainty in decision-making. Some noted that lacking digital health literacy makes it difficult to independently obtain reliable information, often leading to confusion when facing health issues. For instance, N1 stated, “Improving digital health literacy is essential for better understanding one’s health.” N2 commented, “Having no digital health literacy is unacceptable… Otherwise, when problems arise, I’ll be completely lost.” N5 added, “It is crucial for chronic disease management and must be taken seriously.” These findings suggest that older adults who perceive greater benefits from digital health literacy are more likely to adopt health-related behaviors.
Illness experience drives patients to actively seek health information and prioritize health management. Several respondents reported relying on digital health resources after being diagnosed with a chronic disease to obtain information on diet, exercise, and medication management. N5 and N31 (colon cancer patients) stated, “After falling ill, I pay special attention to health information.” Some noted that when doctors provided limited guidance on dietary restrictions or medications, they supplemented their knowledge online.
Additionally, some respondents highlighted using digital tools to optimize caregiving for family members, emphasizing that digital health literacy influences both personal and family healthcare. N15 noted, “My father, over 90 years old, is frequently hospitalized… I need to learn how to care for him.” N16 stated, “My mother has been bedridden for years; I learn caregiving techniques online.” These findings indicate that older adults’ need for digital health literacy is closely linked to their health management demands.
Digital healthcare simplifies medical procedures, reducing the need for family support during visits and streamlining insurance reimbursements, thereby easing financial and time burdens. N13: “My child books appointments online, so I can go alone, letting them focus on work.”N20: “Insurance reimbursements can be processed via phone, avoiding repeated trips.” N31: “Phone-based reimbursement processes reduce my children’s worries and give them peace of mind.”
Digital health resources improve family economic efficiency by streamlining medical procedures, reducing healthcare costs, and facilitating insurance reimbursement. Many respondents reported that online appointment booking and digital insurance claims allowed them to complete medical processes independently, reducing the burden on family members. For instance, some noted that scheduling appointments via mobile phones minimized disruptions to their children’s work, while digital insurance operations reduced hospital visits and expedited reimbursements. This alleviates financial strain and enhances patient independence. N13 and N31 shared, “We book appointments on our phones and go alone, so our children can focus on work.” N20 stated, “Medical insurance claims can be processed via mobile phone, eliminating repeated hospital visits.”
Digital healthcare improves older adults’ medical experiences by reducing wait times, increasing accessibility, and enhancing transparency. Several respondents noted that registering for appointments previously required long queues, whereas online registration now minimizes wait times and enhances convenience. Additionally, online consultations provide valuable access to medical advice, particularly for those in remote areas, preventing unnecessary travel and treatment delays. N13 and N31 stated, “Online appointment booking eliminates long queues, making it very convenient.” N15 added, “I can consult specialists from other cities via mobile phone, which saves both effort and money.”
Moreover, digital healthcare has increased transparency in medical expenses. Some respondents noted that digital applications display medication records, medical tests, and cost details, allowing them to better track their spending and reducing anxiety caused by information gaps. N29 explained, “I can check my phone for medication and test records, so I know exactly where my money goes.” Others reported using online resources to clarify medication instructions, improving adherence. N26 and N32 stated, “I could not understand the doctor’s instructions, so I looked up how to take the medication online.” These findings suggest that digital healthcare enhances both the medical process and patient autonomy in decision-making.
Family plays a crucial role in older adults’ adoption of digital health tools, providing device access, technical guidance, and emotional support. Many respondents stated that their children or relatives helped them acquire and use digital health technologies. For instance, N23 said, “My children bought me a blood pressure monitor and a glucose meter and remind me to measure regularly.” This suggests that intergenerational support significantly influences digital health adoption.
Peer groups, particularly those with shared medical conditions, provide motivation and credibility in adopting digital health technologies. Many older adults noted that after observing peers successfully using digital health tools, they became more inclined to learn. Some were inspired to use mobile-based appointment booking after seeing hospital roommates navigate the system. N28 remarked, “The patient next to me is over 80 and can book appointments on a phone. I’m in my 60s—this motivated me to learn; I cannot fall behind.” These findings suggest that peer role modeling drives behavioral change.
Community hospitals, health centers, and pharmacies play a vital role in bridging digital health gaps among older adults. Some respondents reported seeking help from community healthcare providers when struggling with digital tools, such as glucose meters. N3 and N8 stated, “The community hospital and pharmacy are close, so when I have trouble using my glucose meter, I ask for help.” Additionally, some noted that outpatient volunteers and hospital staff provided guidance on online appointment booking, making digital healthcare services more accessible. N30 said, “An outpatient volunteer taught me how to book appointments online—it was very helpful.” These findings highlight the importance of institutional support in facilitating digital health adoption.
Most respondents were unaware of digital health literacy, demonstrating low recognition and delayed comprehension. Many stated they had never heard of it or hesitated when asked related questions. For example: N8: “I do not understand. I cannot comprehend it.”N10, N14: “Um… (pause) Not very clear.” N21: “I do not know about it. This is the first time I’ve heard of it.” N26: “(Pause, thinking) … No (never heard of it).”
This lack of awareness may stem from the rapid advancement of digital technology, making it difficult for older adults to keep up. Traditional health education has mainly focused on disease management, with little emphasis on digital skills. Additionally, some older adults resist new technologies or have low self-efficacy.
Some respondents (8 individuals) had heard of “digital health literacy” but misunderstood it, often associating it with smartphone proficiency, online shopping, or artificial intelligence. Many equated it with mobile phone usage and accessing health information, overlooking its core aspects, such as evaluating digital health information and making informed decisions. These misconceptions may arise from limited information sources and the lack of targeted health education. Additionally, personal experiences and social environments shape learning and cognition. Older adults mainly exposed to digital services in daily life are more likely to equate digital health literacy with general tech skills. For example: N29: “It’s just about using your phone well and caring about health knowledge.” N23: “Isn’t it artificial intelligence and robots making life easier for older adults?” N18 (a rural-to-urban migrant living in Guangzhou for over 10 years): “The gap in digital development between small towns and big cities is too large.”
Many older adults struggle to interpret health information due to low education levels, limited literacy, and a lack of medical knowledge. Some relied on voice or video content because they were illiterate or unfamiliar with input methods. Those without formal education found complex medical terminology difficult to understand or remember, even when doctors provided detailed explanations. For example: N8: “I do not know how to type. I just watch videos and send voice messages.” N20: “I’m from the countryside. I had many siblings… I dropped out of school early and have little education.” N26: “I cannot understand or remember the professional content explained by doctors.”
Limited exposure to digital media and technology further contributed to unfamiliarity, leading to anxiety and avoidance. Some respondents mentioned that frequent updates in smart devices made adaptation challenging, triggering resistance. Physiological decline, such as deteriorating vision, hearing loss, and cognitive decline, further exacerbated difficulties, reducing willingness to use digital tools. N2: “There are too many functions. Before I learn one, it updates again. It’s frustrating.” N22: “I’m too old to learn and do not want to anymore.” N6, N10: “My eyesight is poor, and I worry about relying too much on smartphones.” N13: “I cannot use smartphones as well as children. I feel outdated.”N17, N25: “My memory is poor. I forget what I learned—I’m old.”
Due to weak digital skills, older adults face multiple obstacles when accessing health information, particularly when using self-service machines, booking appointments online, or searching for health content. Many struggle with complex digital healthcare processes and feel overwhelmed. Rural residents, in particular, have limited exposure to digital technology, leading to a lack of confidence. Fearing errors or damaging devices, they often avoid usage altogether, exacerbating health information inequality. N13, N19: “I cannot use self-service machines or figure out how to book an appointment on my phone.” N14: “WeChat appointment booking and online consultations are too complicated. I cannot find the right section.”N22: “I do not know how to search for health information. If I cannot find it, I just give up.”N24, N30: “We do not have these devices in rural areas. I do not dare use them—I’m afraid of breaking them.”
Older adults often struggle with digitalized healthcare procedures, negatively impacting their medical experience. Some reported difficulties with online appointment booking and digital payments, sometimes resulting in financial losses. However, after guidance from medical staff or family members, some gradually adapted and were able to book appointments independently. N14: “I messed up online booking and lost money.”N24: “At first, I did not know how to use it, but after a nurse taught me, I could book my own follow-ups.”N30: “I had never seen it before and could not figure it out. A nurse had to help me.”
Many older adults distrust online consultations, as they lack the sense of reality and personal connection of face-to-face interactions. Most respondents felt that online consultations could not replace in-person visits, particularly when choosing a doctor. They preferred recommendations from acquaintances or existing doctor-patient relationships over online information. Additionally, some doubted the credibility of online doctors, believing digital platforms could not accurately assess medical professionals’ expertise, reinforcing their preference for in-person visits. N8, N22: “You cannot see the doctor online, so it does not feel reassuring.”N11: “How do I know who’s really on the other side? My home is near the hospital, and I trust Dr. X because I know him personally. If I need a referral, I’d rather have him recommend someone.”N21: “I check doctors’ credentials online, but I still prefer visiting the hospital—it feels more reliable.”
Adaptability to digital health tools varies depending on their complexity. Older adults could easily use simple devices like electronic blood pressure monitors and smart wristbands but found more complex tools, such as blood glucose monitors, difficult to operate. This reduced their willingness to use them. Additionally, some questioned the accuracy and reliability of digital health devices, further limiting their use. N1: “With an electronic blood pressure monitor, you just strap it on and press a button. It tells you if your pressure is too high or low, and you adjust your medication accordingly.”N2: “I can use wrist and arm blood pressure monitors, but I cannot handle the blood glucose monitor.”N4, N11: “Once the wristband is set up, it works fine—no issues.”N5: “I often check my blood pressure digitally, but I find blood glucose monitors too troublesome. I feel they are inaccurate and unreliable.”N17: “There’s nothing difficult about using an electronic blood pressure monitor.”
Older adult patients must balance family responsibilities, social activities, and health management, which reduces their willingness and capacity to engage in digital health management. Many interviewees reported that caring for grandchildren, older adult parents, or managing household duties made it difficult to invest time in learning digital health skills. Some prioritized their children’s or grandchildren’s education at the expense of their health. N8: “My grandson is taking the college entrance exam next year. Everything revolves around him, and I have no time to focus on my minor ailments.”N15: “I live with my 90-year-old father and have to take care of him.” N20: “I have cared for my younger siblings, my children, and now my grandchildren.” N22: “I care for my 80-year-old mother, do the grocery shopping, cook, and manage house renovations. My child is at work and cannot help.” Additionally, some respondents indicated that active participation in social activities, such as attending senior university courses or community events, reduced their opportunities to access digital health resources. N3: “I take classes at a senior university and often attend gatherings.” This phenomenon suggests that many older adult patients voluntarily assume intergenerational responsibilities, prioritizing family obligations over personal health management. A strong sense of familial duty may limit their willingness to engage with digital health tools.
When obtaining and sharing digital health information, older adult patients exhibit heightened sensitivity to their social image, making them cautious about sharing health-related content. Some fear that sharing unverified information could mislead others, cause misunderstandings, or damage their reputation. N3: “I tried kudzu root powder (a health supplement) and found it effective, so I shared it on social media. However, I hesitated to actively recommend it, fearing others might think I was selling medicine.” This self-restraint reflects their desire to maintain social harmony and avoid being perceived as having commercial motives.
Moreover, family members’ interventions influence their behavior. Some respondents noted that after purchasing health products online, they wanted to recommend them to friends but were discouraged by their children, who feared potential risks. N10: “I bought medicine for back pain on ‘Kuaishou’ (a short video platform) and found it helpful. I shared it in my social media groups, but my child advised against recommending it, fearing allergic reactions or unintended consequences.” Such external constraints reinforce older adult patients’ reluctance to share health information, reducing their participation in digital health discussions.
Some older adult patients deliberately avoid health information to reduce anxiety and emotional distress. This avoidance manifests in both emotional and social dimensions. At the emotional level, some interviewees felt that excessive focus on health issues increased their anxiety, prompting them to avoid health-related content. N22: “I do not want to look at these things. The more I see, the more annoyed I feel.” At the social level, health discussions are sometimes seen as taboo among older adult social circles. Some respondents reported receiving negative reactions when sharing health information. N26: “I shared health information with a friend, and they said I was cursing them. They joked that I was ‘afraid of dying,’ so I stopped bringing it up.” This suggests that in some social contexts, discussing health matters may be culturally sensitive, leading older adult patients to avoid digital health interactions.
Many interviewees found the vast quantity and inconsistent quality of online health information overwhelming. Some noted that complex webpage layouts and excessive advertisements made it difficult to focus. N9: “There’s too much text, the font is too small, and there are too many ads. I do not want to look at it.” N29: “Online health information is chaotic and disorganized. It’s hard to distinguish truth from falsehood.” Additionally, some content prioritizes marketing over education, promoting medications rather than providing reliable health knowledge. N20, N24: “The information is superficial. In the end, it’s all about selling medicine rather than educating people.” Information overload increases cognitive burden, making it harder for older adult patients to filter and evaluate content, ultimately limiting their access to valuable health information.
Many respondents were skeptical about the authenticity of digital health information, particularly when different sources provided contradictory explanations for the same issue. N11: “For the same question, some sources say one thing, others say the opposite. I do not know which to trust.” Inconsistent information led to distrust, with some interviewees criticizing self-proclaimed experts who spread exaggerated or misleading health claims. N6: “There’s so much information online, some even claim to cure cancer—what nonsense.” N13: “Many fake experts read a few books and start spreading misinformation. In the end, it’s all about selling medicine.”
Some respondents observed that digital health content was repetitive, leading to a perception that it lacked novelty or in-depth guidance, which diminished their interest over time. N5: “It’s all the same repetitive content. I cannot find what I need.” N21: “I used to read it often, but eventually realized that everything is superficial and repetitive, so I lost interest.” Content homogeneity discourages continued engagement and hinders digital health literacy. Enhancing personalization, relevance, and depth of health information may improve user engagement.
Although older adult patients are generally aware of privacy and financial security risks, their limited digital skills and knowledge of online security constrain their ability to protect themselves. Instead, they rely on personal experience and trusted acquaintances to manage risks. Some interviewees avoided unfamiliar links and only trusted information shared by relatives and friends. N15: “I only read content shared by people I know. I do not trust unfamiliar links.” Some adopted a “minimalist” approach, such as not linking bank cards or using only small amounts for mobile payments to minimize potential losses. N22: “I’m not worried. I do not link my bank card—I just use the few hundred yuan my child transfers to me via WeChat.”
However, heightened risk perception affected their online interactions. Some expressed willingness to share illness experiences but refrained from online discussions due to privacy concerns. N5: “I will not post online. I’m worried about malicious websites collecting my data.” N13, N28: “I generally do not participate online, leave comments, or forward posts.”N15: “I do not engage with links or voting activities from strangers.”N24: “I accidentally clicked on something before, and my phone number was leaked. Now I get marketing calls every day.”N29, N31: “I do not dare to grant permissions. My WeChat is linked to my salary account, and my pension is there. I’m afraid of being scammed.” Overall, high sensitivity to data security risks discourages older adult patients from engaging with digital health resources, limiting their ability to obtain and share health knowledge, and ultimately hindering digital health literacy development.
This study found that older adult patients have cognitive blind spots and misunderstandings regarding digital health literacy. They often equate it solely with browsing health information on smart devices while neglecting key competencies such as information filtering, decision-making, and digital chronic disease management. This may stem from the fact that digital health literacy, as an emerging concept, has yet to gain widespread recognition in China. Additionally, older adult patients primarily use digital devices for socialization and entertainment, paying little attention to health-related functions. Consequently, their ability to utilize digital health services remains significantly limited (38, 39).
From the microsystem perspective of the social-ecological system theory, aging and chronic disease progression lead to physiological and cognitive decline, further restricting older adult patients’ access to the internet and digital health skills. When attempting to learn these skills, low self-efficacy and prior failures often result in resistance and negative attitudes, with some believing they “cannot learn” or “do not want to learn.” Others hold pessimistic views such as “I will not live much longer” or “Digital technology is for young people.” Consistent with previous studies (24, 40), negative aging attitudes not only heighten social isolation and loneliness but also exacerbate anxiety about digital technology, hindering its adoption. Conversely, research indicates that older adult patients with higher self-efficacy and positive attitudes toward aging are more inclined to explore and learn digital health skills, thereby enhancing their digital health literacy (41, 42). To address this, health education should guide older adult patients in developing a correct understanding of aging, boosting their confidence and adaptability in digital environments to improve digital health literacy.
Moreover, this study found that some older adult patients have limited medical knowledge. Due to differences in doctor-patient perspectives and constrained consultation time, they often struggle to fully comprehend medical advice. As a result, they turn to digital platforms for supplementary information. This aligns with previous research, which suggests that the complex needs of chronic disease management drive patients to actively seek digital health resources, improving their digital health literacy (43). Medical institutions should offer personalized health education and continuously assess older adult patients’ physical and mental conditions to enhance their acceptance and application of digital health services.
This study found that older adult patients generally lack awareness of digital security risks when using digital health services, consistent with previous research (44). Some have experienced online fraud or misinformation, leading to distrust or even rejection of digital health platforms in favor of traditional offline methods. Others oversimplify cybersecurity, believing that avoiding unfamiliar links or not linking their bank accounts is sufficient protection while overlooking more complex threats, particularly those arising from social interactions with acquaintances.
From the microsystem perspective of the Socio-Technical Environment (SET) theory, older adult patients’ risk perception and decision-making abilities are shaped by cognitive capacity, education, and past experiences. Many lack digital security education and struggle to assess health information credibility. Previous studies suggest that digital risk assessment skills directly influence the acceptance and frequency of digital health service use among older adult patients (10). To mitigate these risks, targeted digital security education is essential. Strengthening critical thinking and risk-avoidance skills can enhance trust in digital health services, ensuring safer and more effective engagement with digital platforms.
This study found that some older adult patients passively receive health information, often encountering it incidentally on smartphones rather than actively seeking it. Some prioritize authoritative sources and validate information through personal experience, peer verification, and cross-referencing multiple channels. However, cognitive limitations, technology acceptance, and information accessibility constrain their ability to acquire digital health information (44, 45). Research suggests that diverse information sources significantly enhance health literacy (46, 47). Nevertheless, some older adult patients overly rely on hospital-affiliated public accounts while dismissing alternative sources, limiting their information intake.
Additionally, older adult patients with multiple chronic diseases are more prone to health information avoidance, deliberately evading disease-related content to reduce psychological stress. This aligns with previous findings (48, 49), which indicate that concerns about disease progression or a lack of coping strategies drive such avoidance. However, avoiding health information diminishes motivation to acquire health knowledge, ultimately compromising disease management.
Furthermore, China’s digital health sector lacks unified regulatory standards. Some search engines and short-video platforms engage in “paid ranking” practices, resulting in inconsistent information quality and making it difficult for users to identify reliable sources. This study found that older adult patients with limited medical knowledge often disregard complex health information rather than translate it into practical chronic disease management strategies. To address these challenges, regulatory authorities should strengthen oversight of digital health content, optimize information presentation, and provide evidence-based training. Enhancing older adult patients’ ability to discern credible information will enable them to translate health knowledge into effective chronic disease management behaviors.
In the social-ecological systems theory, the interpersonal level emphasizes the interaction between individuals and their family and social support networks in shaping digital health literacy. This includes family and social support as well as the reciprocal effect of digital technology.
In modern society, older adult patients often assume multiple roles, including chronic disease managers, family caregivers, and social participants. In traditional Chinese family values, older adult patients regard maintaining their health as part of their familial responsibilities. To avoid becoming a burden on their children, they actively learn digital technologies to better manage chronic diseases, thereby enhancing their self-efficacy and sense of value. Additionally, some older adult patients, when acting as caregivers, actively seek and apply health information to meet caregiving needs.
However, the rapid updates of digital devices and their operational complexity require significant time and effort to learn, while traditional family values compel older adult patients to prioritize family needs over their chronic disease management. This role conflict and resource constraint limit their ability to improve digital health literacy. This study found that in multigenerational households, older adult patients often bear responsibilities such as household chores and caring for grandchildren, restricting their time for acquiring digital health skills. In contrast, those in relatively independent family structures tend to have greater autonomy in digital health management.
Therefore, healthcare professionals should encourage older adult patients to enhance their proactive health awareness, promote family communication, and leverage community support to help them balance family responsibilities with personal health management. Additionally, regular and multi-level digital skills training should be conducted to improve their digital health competencies, reducing the social stigma associated with learning and ultimately enhancing their digital health literacy.
The trust relationships that older adult patients establish within peer groups or among fellow patients facilitate the acceptance and sharing of health information. Health information shared within familiar social circles is perceived as filtered and validated, aiding comprehension and communication. Such interactions provide demonstrative and motivational effects. However, the prevalence of online fraud has heightened older adult patients’ concerns about data privacy and financial security, reinforcing their reliance on trusted social circles.
Older adult patients’ interactions on social platforms (e.g., WeChat) not only serve as important channels for obtaining health information but also promote information sharing. Social support networks help bridge the information gap for older adult patients, aligning with previous research findings that emotional, informational, and instrumental support within social networks alleviate stress and improve physical and mental well-being (50). These networks are thus key factors influencing digital health literacy (41).
Additionally, older adult patients’ sensitivity to social image makes them cautious about publicly sharing health information, particularly regarding disease privacy and health-related decisions. While some older adult patients wish to share health information or disease experiences to help others, they fear providing inaccurate information that might mislead others or be misinterpreted as promotional activity. Consequently, they adopt an avoidant attitude toward health information sharing. Furthermore, within the context of traditional Chinese culture, health issues are often considered sensitive or private topics. Discussing health information may be perceived as inauspicious or as touching upon life-and-death matters, potentially disrupting social harmony and hindering health information exchange and dissemination.
This study found that emotional support and practical assistance from family members—such as guidance in accessing and interpreting health information—enhance older adult patients’ confidence and ability to use digital health technologies. Older adult patients lacking family emotional and technological support are prone to experiencing “digital loneliness” and technology-related anxiety. Previous research suggests that younger generations teaching older adult patients digital skills, known as “digital reciprocity,” is a crucial measure for bridging the digital divide (51). This process fulfills older adult patients’ desire for digital learning and helps alleviate their digital technology anxiety (52).
However, disparities arise due to variations in family structures, children’s educational backgrounds, and digital competencies. Similar to previous findings (51), harmonious intergenerational relationships, higher family education levels, and better economic conditions improve the effectiveness of digital reciprocity. Positive intergenerational interactions also enhance emotional communication within families, strengthening older adult patients’ sense of belonging and security, fostering their enthusiasm for learning, and improving their ability to assimilate knowledge. This facilitates their adaptation to digital transformation and access to accurate and efficient health information. Nevertheless, this study also found that some older adult patients overly rely on family members, leading to information biases or excessive dependence, thereby reducing their ability to independently obtain and evaluate digital health information. This aligns with prior research indicating that most older adult patients are passive recipients of digital health information (10).
While family support can enhance older adult patients’ acceptance of digital health tools, the long-term effectiveness of “digital reciprocity” is limited due to the time and energy constraints of younger generations. Consistent with previous findings (51), the support provided by younger generations tends to be intermittent, fragmented, and sporadic, making it difficult to meet older adult patients’ needs for continuous and systematic learning. Therefore, social forces should be mobilized to encourage community and healthcare institutions to offer sustained and structured training programs to supplement the gaps in family education.
This study found that older adult patients in rural or remote areas have relatively low levels of digital health literacy, which aligns with previous findings that low-income older adult groups often face significant digital health disparities due to economic and technological limitations (53). The disparity in social and economic development between urban and rural areas, uneven digital infrastructure, and imbalanced healthcare resource allocation restrict older adult patients’ ability to access high-quality digital health services (54).
In recent years, driven by policy support, technological advancements, and increasing social demand, China’s digital healthcare market has expanded rapidly. To enhance the accessibility of digital healthcare resources and improve patient experiences, China has been actively promoting the development of digital hospitals, upgrading primary healthcare digitalization, advancing internet hospitals, and implementing digital health insurance management initiatives (55).
Compared to traditional health information acquisition methods (such as advice from relatives and friends, television, and newspapers), digital health resources, with their open and shared characteristics, transcend time and space limitations, making information dissemination more diversified, personalized, and interactive. Older adult patients can independently search for health resources based on their needs, reducing acquisition costs and enhancing their health management capabilities (56). This study found that older adult patients’ perceived usefulness and ease of use of digital health information positively influence their willingness to accept and utilize digital health resources, consistent with prior research (57). The adoption of digital health resources can improve health lifestyles and self-management of chronic diseases.
However, although older adult patients tend to trust digital health information provided by peers, their limited communication range may lead to inconsistent information quality, potentially affecting health decisions. At the societal level, national policies and healthcare institutions are actively promoting digital healthcare transformation while improving the accessibility and age-friendliness of digital health services. Therefore, it is recommended that healthcare professionals integrate both online and offline approaches to provide systematic guidance for older adult patients, enhancing their ability to filter and evaluate health information.
This study was conducted in three tertiary hospitals in Anhui Province, where access to digital medical resources is greater than in community or rural healthcare settings. This may limit the generalizability of the findings to older adults in under-resourced areas. Future research should adopt a multi-center approach, including primary care and rural hospitals, to better capture variations in digital health literacy across different healthcare settings.
Additionally, participants were required to own or have access to digital devices and use them independently or with assistance. While this ensured relevance to the study’s focus, it may have excluded individuals with very low digital literacy or those unwilling to engage with digital tools, introducing potential selection bias. Future research should examine the perspectives of digitally excluded older adults to provide a more comprehensive understanding of digital health disparities.
This study used a mixed-methods approach, combining qualitative interviews with quantitative demographic analysis and digital health literacy scale scores. Although this offered some degree of triangulation, the reliance on self-reported interview data may have introduced social desirability bias. Moreover, researchers’ prior knowledge and assumptions could have influenced data interpretation. To strengthen research credibility, future studies should expand quantitative components, such as longitudinal tracking of digital literacy trends or large-scale surveys. Incorporating additional qualitative perspectives from family members and healthcare providers, along with expert review and multiple coding strategies, could further enhance analytical rigor.
Digital health literacy is essential for managing health in the digital age. This study found that older adult patients with chronic diseases generally have low digital health literacy, characterized by cognitive gaps, comprehension difficulties, and limited ability to acquire, evaluate, and apply digital health information. These challenges stem from multiple factors, including physical and mental health conditions and social support systems.
To address this issue, healthcare professionals should enhance education and awareness programs, regularly assess patients’ physical and mental well-being, and encourage the use of digital tools for chronic disease management. Broader societal efforts are needed to develop a supportive “digital feedback” system, improve access to digital health resources, and foster an inclusive digital health environment. Through collective action, older adult patients can better utilize digital health technologies, ultimately improving health outcomes and quality of life.
The datasets presented in this article are not readily available because the datasets presented in this article are not readily available because the dataset generated and analyzed during the current study contains personal health information from older adult patients with chronic diseases, and its use is subject to strict confidentiality agreements. Due to privacy and ethical concerns, the data cannot be made publicly available. Access to the dataset is restricted and available only upon reasonable request, with approval from the ethics committee of the participating institutions, in compliance with applicable data protection regulations. Requests to access the datasets should be directed to XY, MDcwMDAxM0BiYm11LmVkdS5jbg==.
The studies involving humans were approved by the study was approved by the Ethics Committee of Bengbu Medical University (Approval No. [2023]369). All participants voluntarily participated and signed informed consent forms. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
YS: Data curation, Writing – original draft, Writing – review & editing, Conceptualization. XY: Data curation, Writing – review & editing, Conceptualization. QC: Investigation, Writing – review & editing. HG: Investigation, Writing – review & editing. XD: Investigation, Writing – review & editing. XX: Investigation, Writing – review & editing. JY: Data curation, Writing – review & editing. ZZ: Data curation, Writing – review & editing. ShuZ: Data curation, Writing – review & editing. ShiZ: Investigation, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Anhui Provincial Philosophy and Social Science Research Planning Project (AHSKY2023D048), the Major Philosophy and Social Sciences Project of the Anhui Provincial Department of Education (2024AH040341), the 2023 Medical Education Research Project of the Chinese Medical Association and the National Medical Education Development Center (2023B014), the Quality Engineering Projects of the Anhui Provincial Department of Education (2022msgzs034, 2023zyxwjxalk139, 2023kcszsf146, and 2023jyxm0635), the National Social Science Fund Incubation Projects of Bengbu Medical University (2023byfy142sk and 2023byzd166sk), the Natural Science Foundation of Bengbu Medical University (2023byzd047) and the Longhu Talent Project of Bengbu Medical University (LH250201001).
We thank all participants in this study for their sincere cooperation and the hospital’s clinical staff for their help and support. We also sincerely appreciate the valuable comments and suggestions from the reviewers.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. National Bureau of Statistics of China. Statistical Communiqué of the People's Republic of China on the 2023 National Economic and Social Development [Eb/Ol]. Available online at: https://www.stats.gov.cn/sj/zxfb/202402/t20240228_1947915.html (Accessed July 8, 2024).
2. United Nations Department of Economic and Social Affairs, Population Division. World Population Prospects 2022: summary of results [Eb/Ol]. (2022). Available online at: https://www.un.org/development/desa/pd/content/World-Population-Prospects-2022 (Accessed November 15, 2022).
3. National Health Commission and 15 other departments jointly issued. "14th Five-Year Plan for Healthy Aging" [Eb/Ol]. Available online at: https://www.gov.cn/zhengce/zhengceku/2022-03/01/content_5676342.htm (Accessed February 7, 2022).
4. World Health Organization. Noncommunicable diseases [Eb/Ol]. Available online at: https://www.who.int/zh/news-room/fact-sheets/detail/noncommunicable-diseases (Accessed October 8, 2023).
5. Dongbo, F, and Hua, F. Chronic disease self-management. Chin J Prev Control Chronic Dis. (2002) 2:93–5. doi: 10.3969/j.issn.1004-6194.2002.02.030
6. Xue, L, Cai, M, Liu, Q, Ying, X, and Wu, S. Trends and regional variations in chronic diseases and their risk factors in China: an observational study based on National Health Service Surveys. Int J Equity Health. (2023) 22:120. doi: 10.1186/s12939-023-01910-w
7. World Health Organization. Global strategy on digital health2020-2025 [Eb/Ol]. Available online at: https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf (Accessed October 8, 2023).
8. General Office of the State Council. Notice on the Implementation Plan to Effectively solve the Difficulties of the Older adult using intelligent Technology [Eb/Ol]. Available online at: https://www.gov.cn/zhengce/content/2020-11/24/content_5563804.htm (Accessed November 24, 2020).
9. General Office of the National Health Commission Office of the State Administration of Traditional Chinese Medicine. Notice on the issuance of the "Guidelines for Public Hospital Operation and Management Information Function" [Eb/Ol]. Available online at: http://www.nhc.gov.cn/caiwusi/s7785t/202204/8b32aad2325f4ed290c2ed6acf19fe3b.shtml (Accessed April 19, 2022).
10. Siqi, L. Development and empirical research on the digital health literacy assessment scale for community older adult under the background of active aging. Chongqing: Army Medical University (2022).
11. Bittlingmayer, UH, Dadaczynski, K, Sahrai, D, van den Broucke, S, and Okan, O. Digital health literacy-conceptual contextualization, measurement, and promotion. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2020) 63:176–84. doi: 10.1007/s00103-019-03087-6
12. Farahani, M, and Ghasemi, G. Artificial intelligence and inequality: Challenges and opportunities. [J]. Int J Innov Educ. (2024). 9:78–99.
13. World Health Organization. Ageism in artificial intelligence for health [Eb/Ol]. Available online at: https://www.who.int/publications/i/item/9789240040793 (Accesses June 28, 2024).
14. Van Kessel, R, Wong, BLH, Clemens, T, and Brand, H. Digital health literacy as a super determinant of health: more than simply the sum of its parts. Internet Interv. (2022) 27:100500. doi: 10.1016/j.invent.2022.100500
15. Rodríguez Parrado, IY, and Achury Saldaña, DM. Digital health literacy in patients with heart failure in times of pandemic. Comput Inform Nurs. (2022) 40:754–62. doi: 10.1097/CIN.0000000000000883
16. Leong, QY, Lee, VV, Ng, WY, Vijayakumar, S, Lau, NY, Mauritzon, I, et al. Older adults' perspectives and experiences with digital health in Singapore: qualitative study. JMIR Hum Factors. (2024) 11:e58641. doi: 10.2196/58641
17. Yelton, B, Sakhuja, M, Kavarana, S, Schaurer, L, Arent, MA, Donelle, L, et al. How has health literacy and digital health literacy scholarship evolved? A global, qualitative study. Health Promot Int. (2024) 39:daae123. doi: 10.1093/heapro/daae123
18. Zhao, B, Xu, Q, Wang, X, Huang, L, Zhang, Y, and Hu, R. The sinicization of the digital health literacy instrument and the test of its reliability and validity. Chin J Nurs Educ. (2024) 21:89–95. doi: 10.3761/j.issn.1672-9234.2024.01.015
19. Zong, M, Huang, Y, Fang, Y, Zhang, C, Dong, R, and Fu, W. Development of digital health literacy assessment questionnaire for stroke patients and its reliability and validity. China Health Stand Manag. (2024) 15:136–9. doi: 10.3969/j.issn.1674-9316.2024.07.032
20. Luo, L, Yuan, J, and Li, C. Influential mechanism of digital health quality on university students’ sports practice based on Ttm theory. J Phys Educ. (2021) 37:72–78+95. doi: 10.16419/j.cnki.42-1684/g8.2021.04.012
21. Zhao, X. Research on the measurement and improvement strategies of Residents' digital health literacy. Hangzhou Normal University. (2022).
22. Xia, H, Fulei, W, Huang, Q, Zong, X, and Yuan, C. Research progress on digital health literacy of pregnant women under the digital empowerment background. J Nurs Train. (2022) 37:1478–82. doi: 10.16821/j.cnki.hsjx.2022.16.007
23. Yang, Q, Xin, X, Yang, J, Cao, J, Liu, C, Li, X, et al. The mediating effect of digital health literacy on the aging expectations and healthy aging of rural empty nest older adult. Modern. Prev Med. (2024) 51:2780–4. doi: 10.20043/j.cnki.MPM.202403037
24. Yang, Q, Xin, X, Li, X, and Zhang, L. The mediating effect of self-perceived aging between digital health literacy and technology anxiety in rural older adult. Mod Prev Med. (2024) 51:471–5. doi: 10.20043/j.cnki.MPM.202309424
25. Wan, H, Peng, J, Wen, H, Zhang, Y, Xu, Y, Gu, C, et al. Analysis of current situation and influencing factors of digital health literacy of the older adult in Shanghai. J Med Inform. (2024) 45:53–8. doi: 10.3969/j.issn.1673-6036.2024.10.010
26. Tang, Y, Zhang, J, Zhou, M, Feng, S, Gao, F, and Shi, L. The status quo and influencing factors of digital health literacy in patients with rheumatoid arthritis. China Med Pharm. (2023) 13:16–19+29.
27. Li, Z, and Liu, Y. Nursing research methods. 2nd ed. Beijing: People's Medical Publishing House (2018).
28. Bronfenbrenner, U. The ecology of human development: experiments by nature and design. Harvard university press, (1979).
29. Bronfenbrenner, U, and Ceci, SJ. Nature-nurture reconceptualized in developmental perspective: a bioecological model. Psychol Rev. (1994) 101:568–86. doi: 10.1037/0033-295X.101.4.568
30. Jackson, M, Harrison, P, Swinburn, B, and Lawrence, M. Using a qualitative vignette to explore a complex public health issue. Qual Health Res. (2015) 25:1395–409. doi: 10.1177/1049732315570119
31. Saunders, B, Sim, J, Kingstone, T, Baker, S, Waterfield, J, Bartlam, B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. (2018) 52:1893–907. doi: 10.1007/s11135-017-0574-8
32. Venkatesh, V, Morris, MG, Davis, GB, and Davis, FD. User acceptance of information technology: toward a unified view. MIS Q. (2003) 27:425–78. doi: 10.2307/30036540
33. Tong, A, Sainsbury, P, and Craig, J. Consolidated criteria for reporting qualitative research (Coreq): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
34. Guest, G, Namey, E, and Chen, M. A simple method to assess and report thematic saturation in qualitative research. PLoS One. (2020) 15:e0232076. doi: 10.1371/journal.pone.0232076
35. Denzin, NK. The research act: A theoretical introduction to sociological methods. 2nd ed. New York: McGraw-Hill (1978).
36. Carter, N, Bryant-Lukosius, D, Dicenso, A, Blythe, J, and Neville, AJ. The use of triangulation in qualitative research. Oncol Nurs Forum. (2014) 41:545–7. doi: 10.1188/14.ONF.545-547
37. Elo, S, and Kyngäs, H. The qualitative content analysis process. J Adv Nurs. (2008) 62:107–15. doi: 10.1111/j.1365-2648.2007.04569.x
38. Dunn, P, and Conard, S. Digital health literacy in cardiovascular research. Int J Cardiol. (2018) 269:274–5. doi: 10.1016/j.ijcard.2018.07.011
39. Mahmood, A, Kedia, S, Wyant, DK, Ahn, SN, and Bhuyan, SS. Use of mobile health applications for health-promoting behavior among individuals with chronic medical conditions. Digit Health. (2019) 5:2181. doi: 10.1177/2055207619882181
40. Xi, W, Zhang, X, and Ayalon, L. The framing effect of intergenerational comparison of technologies on technophobia among older adults. J Gerontol B Psychol Sci Soc Sci. (2022) 77:1179–85. doi: 10.1093/geronb/gbab199
41. Yang, Q, Xin, X, Wang, Y, Peng, D, and Tian, J. The impact of social support networks and self-efficacy on digital health literacy among urban and rural older adult. Bus Inf. (2022) 12:0136–8.
42. Wang, X, and Luan, W. Research progress on digital health literacy of older adults: a scoping review. Front Public Health. (2022) 10:906089. doi: 10.3389/fpubh.2022.906089
43. Chuttur, Mohammad. Overview of the technology acceptance model: origins, developments and future directions. All Sprouts Content, (2009), 9. https://aisel.aisnet.org/sprouts_all/290
44. Meng, H, and Huijie, X. Research on the online health information seeking behavior of older adult patients with chronic diseases based on grounded theory. Chin Clin Nurs. (2020) 12:388–92. doi: 10.3969/j.issn.1674-3768.2020.05.002
45. Xiong, S, Lu, H, Peoples, N, Duman, EK, Najarro, A, Ni, Z, et al. Digital health interventions for non-communicable disease management in primary health care in low-and middle-income countries. NPJ Digit Med. (2023) 6:12. doi: 10.1038/s41746-023-00764-4
46. Cutilli, CC, Simko, LC, Colbert, AM, and Bennett, IM. Health literacy, health disparities, and sources of health information in U.S. older adults. Orthop Nurs. (2018) 37:54–65. doi: 10.1097/NOR.0000000000000418
47. Li, C, Liu, M, Zhou, J, Zhang, M, Liu, H, Wu, Y, et al. Do health information sources influence health literacy among older adults: a cross-sectional study in the urban areas of Western China. Int J Environ Res Public Health. (2022) 19:13106. doi: 10.3390/ijerph192013106
48. Barbour, JB, Rintamaki, LS, Ramsey, JA, and Brashers, DE. Avoiding health information. J Health Commun. (2012) 17:212–29. doi: 10.1080/10810730.2011.585691
49. Xinran, T. The study of the influence factors of the health information of the patients with hypertension. Hebei University (2024).
50. Shin, H, and Park, C. Social support and psychological well-being in younger and older adults: the mediating effects of basic psychological need satisfaction. Front Psychol. (2022) 13:1051968. doi: 10.3389/fpsyg.2022.1051968
51. Zhuoran, W. Digital feedback: the old people are not left behind. Family Life Guide. (2024) 40:60–1.
52. Ministry of Civil Affairs. Basic Data Bulletin of the Fifth Sampling Survey on the Living conditions of the Older adult in Urban and rural areas of China [Eb/Ol]. Available online at: https://www.mca.gov.cn/n152/n165/c1662004999980001877/part/19971.pdf (Accessed October 24, 2024).
53. Alkureishi, MA, Choo, ZY, Rahman, A, Ho, K, Benning-Shorb, J, Lenti, G, et al. Digitally disconnected: qualitative study of patient perspectives on the digital divide and potential solutions. JMIR Hum Factors. (2021) 8:e33364. doi: 10.2196/33364
54. Fei, S, Xiang, Y, Wang, Y, Mei, H, and Sun, Y. Study on acceptance situation of we-media health information in older adult chronic patients. Front Social Sci. (2023) 12:2319–25. doi: 10.12677/ass.2023.125314
55. National Health Commission National Administration of Traditional Chinese Medicine" Notice on the theme activity of improving medical experience and enhancing patient experience" [Eb/Ol]. Available online at: https://www.gov.cn/zhengce/zhengceku/202305/content_6883385.htm (Accessed May 23, 2023).
56. Chengbo, L, and Xue, G. The status of online access to health information and its influence factors among older urban adults in West China. Popul Dev. (2019) 25:111–118+128.
Keywords: older adult, chronic diseases, digital health literacy, determinants, qualitative research
Citation: Shao Y, Yang X, Chen Q, Guo H, Duan X, Xu X, Yue J, Zhang Z, Zhao S and Zhang S (2025) Determinants of digital health literacy among older adult patients with chronic diseases: a qualitative study. Front. Public Health. 13:1568043. doi: 10.3389/fpubh.2025.1568043
Received: 28 January 2025; Accepted: 11 March 2025;
Published: 31 March 2025.
Edited by:
Suraj Singh Senjam, All India Institute of Medical Sciences, IndiaReviewed by:
Gergő Túri, Semmelweis University, HungaryCopyright © 2025 Shao, Yang, Chen, Guo, Duan, Xu, Yue, Zhang, Zhao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiumu Yang, MDcwMDAxM0BiYm11LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.