
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 09 April 2025
Sec. Occupational Health and Safety
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1566534
Background: As the healthcare environment undergoes rapid evolution, nurses frequently confront multifaceted changes, resulting in significant change fatigue. This fatigue adversely impacts their well-being, diminishes job satisfaction, elevates turnover rates, and undermines the quality of care provided.
Aim: To comprehend the fatigue levels experienced by clinical nurses amidst environmental changes and to analyze the factors influencing this fatigue.
Methods: A survey was conducted among 451 clinical nurses at a tertiary general hospital in Nantong City, utilizing the Change Fatigue Scale, Care Perception Scale, and Emotional Intelligence Scale.
Results: The change fatigue score was 19.01 ± 3.63, indicating a moderate level of fatigue. Change fatigue was inversely correlated with emotional intelligence and care perception (all p < 0.05). Multiple linear stepwise regression analysis revealed that monthly income, professional title, years of work, number of night shifts, care perception, and emotional intelligence were significant factors influencing the change fatigue experienced by clinical nurses amidst environmental changes (all p < 0.05). These factors collectively accounted for 76.1% of the total variation.
Conclusion: Clinical nurses exhibit moderate levels of change fatigue. Therefore, it is recommended that nursing managers implement regular emotional intelligence training and reduce night shifts to actively address the rapid changes brought about by the healthcare industry and, consequently, enhance the quality of nursing care.
In the rapidly evolving medical environment, hospital relocation represents not merely the transformation of physical space but also a profound process involving workflow restructuring and the psychological adjustment of personnel (1). As a crucial component of the medical service system, the physical and mental health status of clinical nurses is intimately tied to the quality of nursing care and patient safety (2). However, the substantial changes brought about by hospital relocation often propel nurses into a psychological dilemma termed “change fatigue,” which stems not only from the rapid alterations in the working environment but also encompasses adjustments in workflow, teamwork, patient management, and other facets (3).While emotional intelligence is generally considered beneficial, recent studies suggest that the relationship between emotional intelligence and fatigue may not be linear. For instance, Partido and Owen (4) found that while emotional intelligence is linked to stress and burnout, excessive self-regulation of emotions can become a fatigue-inducing factor. Similarly, Griffin and Howard (5) proposed that individual differences in emotion regulation may lead to distinct stress patterns, such as cardiovascular reactivity, indicating that over-regulation of emotions might exacerbate fatigue rather than alleviate it.
Change fatigue is a prevalent psychological response among employees undergoing organizational change. It manifests as persistent stress, exhaustion, and fatigue. In severe cases, it may result in diminished work efficiency, increased nursing errors, and even heightened job burnout and turnover rates (6). For clinical nurses, the impact of hospital relocation is particularly pronounced, affecting not only individuals but potentially the entire nursing team.
Emotional intelligence pertains to an individual’s ability to identify, understand, express, and regulate their own and others’ emotions. It is a significant factor influencing an individual’s psychological adjustment capabilities when confronted with pressure and challenges (7). Studies have demonstrated that individuals with high emotional intelligence are better equipped to manage their emotions and maintain a positive attitude, thereby mitigating the risk of change fatigue (8). Therefore, examining the relationship between emotional intelligence and change fatigue among clinical nurses is crucial to understanding how they respond to the changes induced by hospital relocation.
Furthermore, the perception of head nurse care is another pivotal factor influencing nurses’ change fatigue. As the leader of the nursing team, the care and support provided by the head nurse play a vital role in the psychological adjustment and career development of nurses (9). When nurses perceive care and support from their head nurse, they are more inclined to maintain a positive outlook in the face of change, thereby alleviating the severity of change fatigue (10).
Consequently, this study investigated the current situation regarding clinical nurses’ change fatigue, analyzed the influencing factors, and explored their relationship with emotional intelligence and perceptions of head nurse care. The aim was to develop targeted management programs for nursing managers, enabling them to actively respond to the rapid changes in the healthcare industry and, consequently, enhance the quality of care.
The survey was conducted at the People’s Hospital of Rudong County, located in Nantong City, Jiangsu Province, China. Over the past 3 years, this hospital has undergone a significant transformation and successfully attained the status of a Grade B tertiary general hospital. This remarkable change has not only enhanced the hospital’s hardware facilities and service levels but has also profoundly impacted the nursing staff, particularly by inducing a phenomenon known as “change fatigue.”
From July 2024 to August 2024, clinical nurses working in a tertiary general hospital in Nantong City were selected as the research subjects using the convenience sampling method. Inclusion criteria encompassed clinical registered nurses who had been working in clinical nursing for at least 6 months, had experienced the hospital relocation process, and provided informed consent. Exclusion criteria included training and practice nurses, as well as non-clinical workers such as administrative staff. This study was approved by the Ethics Committee of Rudong County People’s Hospital of Nantong City (Approval No. 2022001).
After obtaining approval from the hospital authority, the investigator, with the assistance of the hospital’s nursing director, explained the purpose of the study to the nurses who met the inclusion criteria and obtained their informed consent. The nurses then completed the questionnaire anonymously. On-site, the investigator verified the completeness of the questionnaire content, promptly supplemented any omissions, and confirmed and corrected any logical errors.
Gather and document the personal information of clinical nurses, which includes their age, gender, educational background, professional title, years of clinical work experience, monthly frequency of night shifts, level of job satisfaction, willingness to resign, and participation in humanistic care training, among other relevant details.
The CFS-CM was utilized to evaluate the level of care perceived by the head nurse over the past 2 weeks to 1 month (9). The scale comprises 10 items, employing the Likert 7-point scoring method, where 1 represents “very disagree” and 7 signifies “very agree.” A higher total score indicates a greater appreciation by the nurse for the role of the head nurse in nursing care. The Cronbach’s alpha coefficient for this scale was 0.961, and in the present study, it was found to be 0.983.
Yefei Wang developed the Chinese Workplace Emotional Intelligence Scale (WLEIS), which assesses the emotional intelligence of research subjects within a specific work environment (11). This scale consists of 16 items divided into four dimensions: self-emotion perception, others’ emotion perception, emotion management, and emotional application, with four items in each dimension. Utilizing the Likert 7-point scoring method, the score range is from 0 to 96 points. A higher score indicates a higher level of individual emotional intelligence. The overall Cronbach’s α coefficient for the scale was 0.860. In this study, the Cronbach’s α coefficient for the emotional intelligence scale was 0.916. Specifically, the Cronbach’s α coefficients for the self-emotion perception, others’ emotion perception, emotion management (referred to here as emotional control for clarity), and emotional application dimensions were 0.740, 0.778, 0.736, and 0.724, respectively.
As developed by Beernerth in 2011, the Six Change Fatigue Measurement Scales are designed to assess change fatigue among clinical nurses who have undergone changes in the hospital environment (2). This scale consists of 6 items, with scores ranging from 1 to 7 points, corresponding to “strongly disagree” to “strongly agree,” resulting in a total score range of 6–42 points. A higher score indicates more severe change fatigue. The Cronbach’s α coefficient for the scale was 0.85, and in this study, it was found to be 0.910.
When items within a scale were missing, a total score was calculated only if at least half of the questions were answered. For the missing items, the average score of the other items within the scale was assigned. The percentage of estimated items relative to the total sample was X%, which falls within the acceptable margin for estimation. The reliability of the scales was assessed using the Cronbach’s α internal consistency coefficient. The distribution of sample characteristics and discontent regarding change fatigue was evaluated for all study respondents. Descriptive statistics were presented in terms of frequencies, mean values, and standard deviations (SDs).
The correlation analysis was performed using Pearson’s correlation coefficient to assess the relationships between change fatigue, care perception, and emotional intelligence. A p-value of less than 0.05 was considered statistically significant. Logistic regression analysis was employed to identify the characteristics of those who exhibited high discontent with their change fatigue. Results were deemed statistically significant at a p-value of less than 0.05, using two-tailed tests. Statistical analyses were conducted using SPSS version 26.0.
In this study, a total of 451 questionnaires were distributed, and all 451 were collected as valid responses, resulting in an effective recovery rate of 100%. The demographic information is presented in Table 1.
The change fatigue score of clinical nurses was 19.01 ± 3.63, indicating a moderate level of fatigue. Change fatigue was inversely correlated with emotional intelligence and care perception (all p < 0.05) (Table 2).
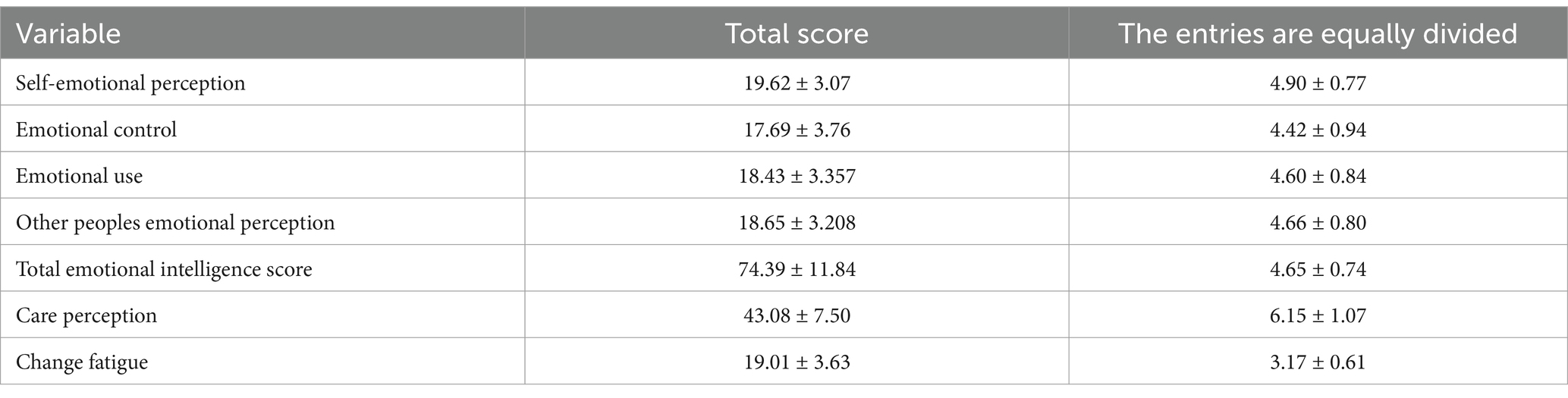
Table 2. Change fatigue, care perception, and emotional intelligence scores of clinical nurses (n = 451).
Multiple linear stepwise regression analysis revealed that monthly income, professional title, years of work, number of night shifts, care perception, and emotional intelligence were significant factors influencing the change fatigue experienced by clinical nurses amidst environmental changes (all p < 0.05). These factors collectively accounted for 77.6% of the total variation (Table 3).
The results of the correlation analysis revealed significant negative correlations between change fatigue and emotional intelligence (r = −0.666, p < 0.001) as well as care perception (r = −0.765, p < 0.001), indicating that higher levels of emotional intelligence and care perception are associated with lower levels of change fatigue (Table 4).
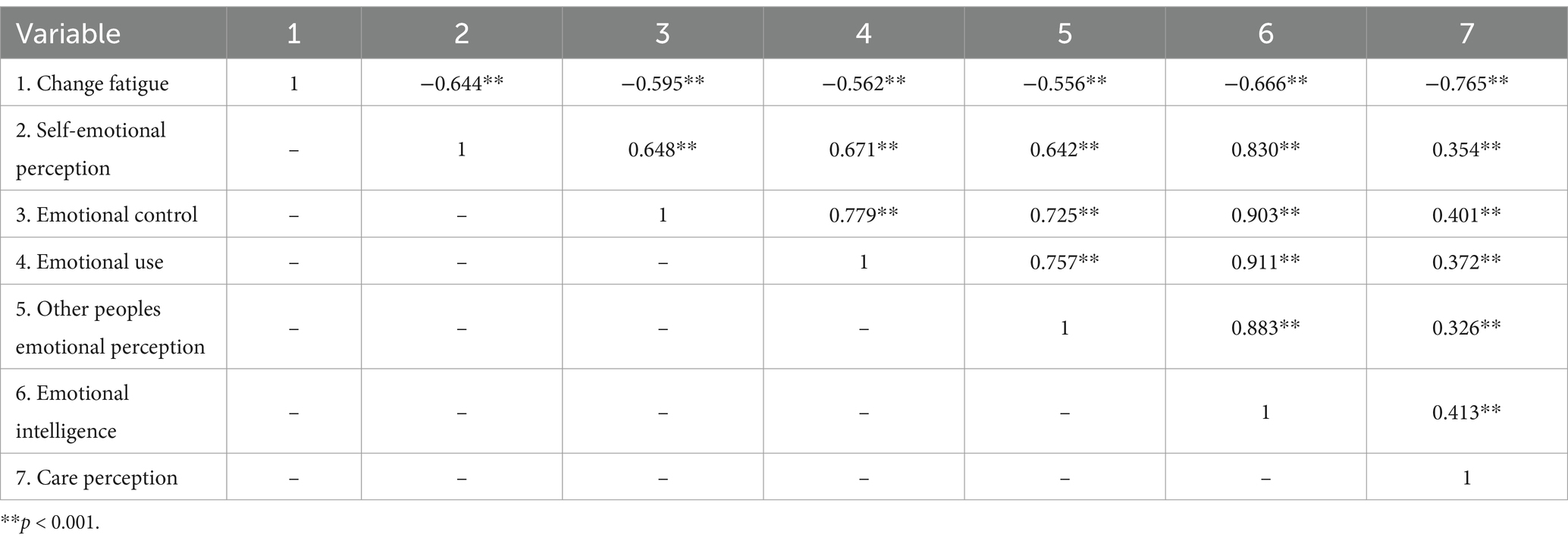
Table 4. Correlation coefficient of change fatigue and care perception and emotional intelligence among clinical nurses.
Multiple linear regression analysis was conducted with the clinical nurses’ change fatigue score serving as the dependent variable, and variables that exhibited statistically significant differences in the univariate analysis were included as independent variables. The results of the collinearity diagnosis revealed that the variance inflation factor ranged from 1.310 to 2.413, indicating the absence of multicollinearity among the variables. The outcomes of the multiple linear regression analysis showed that monthly income, professional title, years of work experience, number of night shifts, care perception, and emotional intelligence were the primary factors influencing change fatigue among clinical nurses (all p < 0.05). These factors collectively accounted for 77.6% of the total variation (Table 5).
The change fatigue score of clinical nurses in this study, who experienced environmental changes, was 19.01 ± 3.63, which was higher than the moderate level found in a study by Fernemark et al. (12) among Swedish doctors. This difference may be attributed to the distinct populations of the study subjects. Research indicates that nurses tend to experience change fatigue three times more frequently in the healthcare system (13). In the healthcare system, nurses, as the primary group in direct contact with patients, not only bear the burden of heavy nursing tasks but also need to constantly adapt to new workflows, technological updates, and information system changes.
To alleviate change fatigue among nurses, medical institutions should rationally arrange change plans, provide training and support, strengthen communication, and prioritize the physical and mental health of nurses (6). A review by Brown on the relationship between resilience training and nurse change fatigue suggests that resilience can be a key measure to mitigate change fatigue (14). Additionally, the change diary (a tool for tracking organizational changes), serving as a preventive and predictive tool, can effectively reduce the occurrence of nurse change fatigue by using a weekly timeline to count, evaluate, and coordinate various changes within the organization. This aims to proactively assess and arrange the organization’s change process (14).
This study found that the monthly income of clinical nurses was negatively correlated with their change fatigue (β = −0.428, p < 0.05), indicating that nurses with higher monthly incomes experienced relatively less change fatigue. This result suggests that economic factors play a significant role in nurses’ responses to job changes, and that a higher income may assist nurses in better coping with the stress associated with change and reducing fatigue. Income serves not only as a primary motivator for nurses in their work but also as a reflection of their work value and family economy. The income level directly influences the quality of life of nurses (15). It is recommended that managers optimize the nurse compensation system and increase income to mitigate change fatigue. Additionally, strengthening psychological support and communication is crucial to encourage nurses’ active participation in change decision-making.
The results of this study demonstrated that the professional title of clinical nurses affects their change fatigue (β = −0.98, p < 0.05). Specifically, nurses with higher professional titles experienced less change fatigue, which is attributed to their advantages of higher income, attention to career development, rich experience, and strong adaptability. Nurses holding high professional titles typically earn higher incomes, prioritize their career development, possess extensive work experience, and demonstrate robust adaptability, enabling them to more effectively address the challenges posed by job changes. Furthermore, they may possess a more mature psychological state and more efficient coping mechanisms, allowing them to better maintain psychological balance and reduce the stress, fatigue, and burnout associated with change. It is recommended that managers focus on the professional title promotion system, provide nurses with more career development opportunities, and strengthen psychological support to assist nurses at all levels in effectively responding to reforms and maintaining psychological balance.
The results of this study indicate that the working years of clinical nurses impact their change fatigue (β = −0.268, p < 0.05). Contrary to what might be expected, a longer working life is associated with heavier change fatigue. This can be attributed to several factors: the accumulation of physical and mental fatigue due to prolonged adaptation to ever-changing work environments, technologies, and processes (16); the increased family responsibilities and personal pressures that accompany the accumulation of work experience, which hinder their ability to adapt to change; long-term intensive work leading to job burnout, thereby diminishing their acceptance and responsiveness to change; and finally, deficiencies in the management and support system during times of change, such as the absence of clear change goals, strategies, and effective communication mechanisms, which further exacerbate nurses’ change fatigue (17). Consequently, managers must implement corresponding measures, such as providing necessary support and resources, optimizing change plans, and enhancing communication mechanisms, to alleviate nurses’ change fatigue.
The results of this study revealed that the number of clinical nurses affects their change fatigue (β = 0.255, p < 0.05). Similarly, a study by Sarıgül and Uğurluoğlu (13) demonstrated comparable findings, showing that an increase in monthly night shifts leads to heightened fatigue. This may be attributed to night shift work disrupting the normal biological clock, thereby increasing work stress and physiological burden, and making nurses more susceptible to feelings of fatigue and burnout when confronted with job changes. Considering this, the study suggests that hospitals should optimize the night shift system by reducing the number of night shifts, strengthening health management and psychological support, and enhancing the work environment and resource support to alleviate nurses’ change fatigue.
The results of this study indicated that clinical nurses perceived head nurse care items as generally moderate (6.15 ± 1.07), which aligns with previous survey findings among psychiatric nurses in this group [8]. This similarity suggests potential commonalities in nurses’ perceptions of care across different departments or nursing fields. The change fatigue of clinical nurses was negatively correlated with the perceived level of care (r = −0.765, p < 0.001) and was significantly affected by the level of perceived head nurse care (β = −0.243, p < 0.001), indicating that as the level of care provided by head nurses increased, clinical nurses experienced lower levels of fatigue.
Watson, a theorist of human nature and care (18), noted that care is infectious to both participants and observers. By offering care and support, head nurses can foster a more harmonious and supportive working atmosphere, effectively assisting nurses in coping with the pressures of change and reducing their sense of fatigue (19). To mitigate potential harm, management should strengthen communication with frontline nurses. Additionally, timely assistance during critical moments is essential. In addition to establishing a solid, long-term communication bridge, management should actively engage in organizational change, comprehensively control the pace of change, rationally allocate tasks, and have a keen insight into the key stages of fatigue during the change process, allowing for the deployment of preventive measures in advance (20).
Additionally, an extreme case of head nurse support style is micromanagement, which refers to excessive attention to detail and constant oversight. Micromanagement can undermine nurses’ autonomy and well-being, potentially leading to increased work stress and burnout (21). Therefore, while head nurse support is crucial, it is equally important to avoid micromanagement to ensure a supportive and empowering work environment.
Furthermore, management should be vigilant about nurses’ overtime behavior during organizational change and avoid blindly praising such behavior, as this could inadvertently promote the spread of a “super nurse” culture (22).
The results of this study revealed that clinical nurses’ emotional intelligence scores were at a medium level (4.65 ± 0.74) (9). This similarity further verifies the stability and universality of emotional intelligence across different studies and samples. Emotional intelligence, defined as an individual’s ability to identify, understand, utilize, and manage their own and others’ emotions, is particularly crucial for nurses, a profession that necessitates frequent interaction with patients and their families (23).
The study found that clinical nurses’ change fatigue was negatively correlated with their emotional intelligence level (r = −0.666, p < 0.001) and was significantly affected by it (β = −0.123, p < 0.001). Specifically, for each unit increase in emotional intelligence level, the degree of change fatigue was notably reduced. This further underscores the vital role of emotional intelligence in mitigating change fatigue. Emotional intelligence not only aids nurses in better understanding and regulating their emotions but also facilitates effective communication with colleagues, patients, and their families, thereby reducing the negative emotions and stress associated with change (24).
Furthermore, the potential fatigue-inducing effects of emotional self-regulation should not be overlooked. While emotional intelligence aids in managing stress, excessive regulation of emotions may lead to increased fatigue (4). Additionally, the negative impact of micromanagement on nurses’ autonomy and well-being highlights the importance of balancing support with empowerment in leadership styles (21).
In response to this phenomenon, the study offers the following recommendations: Firstly, organizations should conduct targeted emotional intelligence training to enhance nurses’ emotional recognition, regulation, and social skills. Secondly, they should establish and improve psychological support systems to provide professional psychological counseling and guidance for nurses with lower emotional intelligence (15). Lastly, management should consider nurses’ emotional intelligence levels and adopt more detailed and humanized change management strategies (25).
Based on the findings of this study, we recommend that clinical nurses engage in emotional intelligence training to enhance their ability to manage stress and adapt to change (26). Additionally, nursing managers should avoid micromanagement and instead focus on providing supportive and empowering leadership to improve nurses’ job satisfaction and well-being (10).
In this study, clinical nurses exhibited moderate levels of change fatigue, with influencing factors encompassing monthly income, professional title, years of experience, number of monthly night shifts, care perception, and emotional intelligence. However, due to constraints related to manpower and time, the impact of varying times on clinical nurses’ change fatigue was not explored. Furthermore, the study only included nurses from a single tertiary hospital, resulting in an underrepresented sample. Additionally, the influencing factors considered may have been inadequate. It is hoped that future studies will expand the sample size and dynamically analyze potential predictors of change fatigue to develop more effective interventions.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study has been approved by the Ethics Committee of County People’s Hospital in Nantong, Jiangsu Province, China (No. 2022001).
MY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JJ: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. DK: Conceptualization, Writing – original draft, Writing – review & editing. DG: Formal analysis, Writing – original draft, Writing – review & editing. XY: Methodology, Writing – original draft, Writing – review & editing. SC: Conceptualization, Writing – original draft, Writing – review & editing. RG: Data curation, Methodology, Writing – original draft, Writing – review & editing. LJ: Conceptualization, Writing – original draft, Writing – review & editing, Methodology.
The author(s) declare that no financial support was received for the research and/or publication of this article.
The authors would like to thank all the employees who participated in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Chen, AJ, Richards, MR, and Shriver, R. Fitting in? Physician practice style after forced relocation. Health Serv Res. (2024) 59:e14340. doi: 10.1111/1475-6773.14340
2. Beaulieu, L, Seneviratne, C, and Nowell, L. Change fatigue in nursing: an integrative review. J Adv Nurs. (2023) 79:454–70. doi: 10.1111/jan.15546
3. McMillan, K, and Perron, A. Change fatigue in nurses: a qualitative study. J Adv Nurs. (2020) 76:2627–36. doi: 10.1111/jan.14454
4. Partido, BB, and Owen, J. Relationship between emotional intelligence, stress, and burnout among dental hygiene students. J Dent Educ. (2020) 84:864–70. doi: 10.1002/jdd.12172
5. Griffin, SM, and Howard, S. Individual differences in emotion regulation and cardiovascular responding to stress. Emotion. (2022) 22:331–45. doi: 10.1037/emo0001037
6. Kwiecień-Jaguś, K, and Wujtewicz, M. Multifactorial analysis of fatigue scale among nurses in Poland. Open Med. (2016) 11:593–604. doi: 10.1515/med-2016-0097
7. Saif, N, Amelia, GGGG, Rubin, A, Shaheen, I, and Murtaza, M. Influence of transformational leadership on innovative work behavior and task performance of individuals: the mediating role of knowledge sharing. Heliyon. (2024) 10:e32280. doi: 10.1016/j.heliyon.2024.e32280
8. Kasemy, ZA, Sharif, AF, Bahgat, NM, Abdelsattar, S, and Abdel Latif, AA. Emotional intelligence, workplace conflict and job burn-out among critical care physicians: a mediation analysis with a cross-sectional study design in Egypt. BMJ Open. (2023) 13:e074645. doi: 10.1136/bmjopen-2023-074645
9. Yu, M, Wang, H, Wu, Y, Zhang, Q, Du, X, Huang, X, et al. The influence of emotional intelligence on psychiatric Nurses' Care behavior, and the chain mediating role of compassion fatigue and perception of management. J Psychosoc Nurs Ment Health Serv. (2025) 63:35–43. doi: 10.3928/02793695-20241101-02
10. Wang, Y, Han, T, Han, G, and Zheng, Y. The relationship among nurse Leaders' humanistic care behavior, Nurses' professional identity, and psychological security. Am J Health Behav. (2023) 47:321–36. doi: 10.5993/AJHB.47.2.12
11. Ma, J, Peng, W, and Pan, J. Investigation into the correlation between humanistic care ability and emotional intelligence of hospital staff. BMC Health Serv Res. (2022) 22:839. doi: 10.1186/s12913-022-08227-4
12. Fernemark, H, Karlsson, N, Skagerström, J, Seing, I, Karlsson, E, Brulin, E, et al. Psychosocial work environment in Swedish primary healthcare: a cross-sectional survey of physicians' job satisfaction, turnover intention, social support, leadership climate and change fatigue. Hum Resour Health. (2024) 22:70. doi: 10.1186/s12960-024-00955-4
13. Sarıgül, SS, and Uğurluoğlu, Ö. Examination of the relationships between change fatigue and perceived organizational culture, burnout, turnover intention, and organizational commitment in nurses. Res Theory Nurs Pract. (2023) 37:311–32. doi: 10.1891/RTNP-2023-0018
14. Brown, R, and Abuatiq, A. Resilience as a strategy to survive organizational change. Nurs Manag. (2020) 51:16–21. doi: 10.1097/01.NUMA.0000651180.42231.ef
15. Chen, X, Chen, M, Zheng, H, Wang, C, Chen, H, Wu, Q, et al. Effects of psychological intervention on empathy fatigue in nurses: a meta-analysis. Front Public Health. (2022) 10:952932. doi: 10.3389/fpubh.2022.952932
16. Damen, LJ, Van Tuyl, LHD, Korevaar, JC, Knottnerus, BJ, and De Jong, JD. Citizens' perspectives on relocating care: a scoping review. BMC Health Serv Res. (2024) 24:202. doi: 10.1186/s12913-024-10671-3
17. Damen, LJ, Van Tuyl, LHD, Knottnerus, BJ, and De Jong, JD. General practitioners' perspectives on relocating care: a Dutch interview study. BMC Prim Care. (2024) 25:186. doi: 10.1186/s12875-024-02425-1
18. Akbari, A, and Nasiri, A. A concept analysis of Watson's nursing caritas process. Nurs Forum. (2022) 57:1465–71. doi: 10.1111/nuf.12771
19. Compton, RM, Hubbard Murdoch, N, Press, MM, Lowe, ME, Ottley, KM, Barlow, M, et al. Capacity of nurses working in long-term care: a systematic review qualitative synthesis. J Clin Nurs. (2023) 32:1642–61. doi: 10.1111/jocn.16144
20. Chachula, KM, and Varley, E. Perceptions and experiences of psychological trauma in nursing and psychiatric nursing students: a small scale qualitative case study. PLoS One. (2022) 17:e0277195. doi: 10.1371/journal.pone.0277195
21. Lee, J, Ahn, S, Henning, MA, van de Ridder, JMM, and Rajput, V. Micromanagement in clinical supervision: a scoping review. BMC Med Educ. (2023) 23:563. doi: 10.1186/s12909-023-04543-3
22. Venturato, L, Horner, B, and Etherton-Beer, C. Development and evaluation of an organisational culture change intervention in residential aged care facilities. Australas J Ageing. (2020) 39:56–63. doi: 10.1111/ajag.12667
23. Urtubia-Herrera, V, Navarta-Sánchez, MV, Palmar-Santos, AM, Pedraz-Marcos, A, García-Gomez, A, Luis, EO, et al. The relationship between sense of coherence and emotional intelligence as individual health assets for mental health promotion in students and healthcare professionals: a scoping review. Front Public Health. (2024) 12:1304310. doi: 10.3389/fpubh.2024.1304310
24. Richards, AE, Curley, KL, Zhang, N, Bendok, BR, Zimmerman, RS, Patel, NP, et al. Burnout and emotional intelligence in neurosurgical advanced practice providers across the United States: a cross-sectional analysis. World Neurosurg. (2021) 155:e335–44. doi: 10.1016/j.wneu.2021.08.066
25. Awe, AO, David-Olawade, AC, Ayodele-Awe, I, Feng, H, Odetayo, A, Afolalu, TD, et al. Predictors and influencing factors of emotional intelligence among nurses in the north East England, United Kingdom. J Educ Health Promot. (2023) 12:236. doi: 10.4103/jehp.jehp_1656_22
Keywords: clinical nurse, change fatigue, emotional intelligence, care perception, influencing factors
Citation: Yu M, Ji J, Kan D, Gu D, Yin X, Cai S, Geng R and Jiang L (2025) Analysis of the current situation and influencing factors of nurse change fatigue. Front. Public Health. 13:1566534. doi: 10.3389/fpubh.2025.1566534
Received: 25 January 2025; Accepted: 18 March 2025;
Published: 09 April 2025.
Edited byw:
Suresh M., Amrita Vishwa Vidyapeetham University, IndiaReviewed by:
Luis Felipe Llanos, Universidad Anáhuac México, North Campus, MexicoCopyright © 2025 Yu, Ji, Kan, Gu, Yin, Cai, Geng and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lingling Jiang, eW1yZHJ5QDE2My5jb20=; Ronghui Geng, cmRyeWhsYkAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.