- 1Department of Respiratory and Critical Care Medicine, Xishan People’s Hospital of Wuxi City, Wuxi, China
- 2Department of Psychiatry, First Hospital of Shanxi Medical University, Taiyuan, China
- 3Department of Respiratory and Critical Care Medicine, Third Affiliated Hospital of Soochow University, Changzhou, China
Background: Chronic lung disease (CLD) not only manifests with respiratory symptoms but is often associated with various systemic conditions that may elevate the risk of falls. This study aimed to evaluate the independent association between chronic lung disease (CLD) and fall risk among middle-aged and older adult Chinese adults.
Methods: We enrolled participants aged over 45 years from the baseline wave of the China Health and Retirement Longitudinal Study (CHARLS) conducted in 2011 and divided them into two groups based on the presence of CLD: the CLD group and the non-CLD group. Follow-up assessments were subsequently performed during the 2013, 2015, 2018, and 2020 survey waves to track longitudinal outcomes. The primary endpoint was the incidence of falls (≥1 fall event) during the entire follow-up period (2011–2020). To address potential confounding and strengthen causal inference, we employed a multivariable logistic regression model, conducted propensity score matching, and performed subgroup analyses.
Results: A total of 9,204 participants were included in the study, consisting of 940 patients with CLD and 8,264 individuals in the non-CLD group. The incidence of falls among patients with CKD was 33.5% (315/940), which was higher than the 27.5% (2,275/8264) observed in the non-CLD group (p < 0.001). After adjusting for confounding factors using logistic regression, the incidence of falls in the CLD group was found to be significantly higher compared to the non-CLD group (OR = 1.19, 95% CI: 1.02, 1.38, p = 0.02). Similar results were observed in the propensity score matching analysis and subgroup analyses.
Conclusion: Our study found that the risk of falls is significantly increased in middle-aged and older adult patients with CLD in China, highlighting the importance of fall screening and risk prevention programs for CLD patients.
Introduction
Chronic lung diseases (CLD), including chronic obstructive pulmonary disease (COPD), chronic bronchitis, and interstitial lung disease, constitute a major global health concern. Epidemiological studies indicate that approximately 5–15% of adults in industrialized countries are diagnosed with COPD based on pulmonary function testing, and by 2020, COPD had risen to rank as the fifth leading cause of death worldwide (1). Globally, it affects over 380 million individuals, with a prevalence exceeding 10% in adults aged 40 years or older (2). Characterized by irreversible decline in pulmonary function (evidenced by reduced FEV1), dyspnea, and progressive deterioration of health status, the 10-year survival rate following diagnosis is only 50% (3). In terms of pathogenesis, COPD pathophysiology involves both localized airway inflammation and structural damage to lung tissue, as well as systemic effects. This systemic inflammation disrupts skeletal muscle metabolism, leading to mitochondrial dysfunction and accelerated atrophy of type II muscle fibers—key drivers of sarcopenia. Concurrently, glucocorticoid use in exacerbation management may exacerbate muscle wasting and osteoporosis, while hypoxemia-induced neurocognitive impairment further compromises postural stability (4).
Globally, falls are the leading cause of fatal and non-fatal injuries among adults aged 65 and over, and they are associated with adverse outcomes, including trauma care, loss of independence, and reduced quality of life (5, 6). Approximately 10–19% of falls result in significant injuries such as fractures, soft tissue injuries, or traumatic brain injuries, costing over billions of dollars annually (7, 8). Growing evidence implicates COPD as an independent risk factor for falls (9, 10). While existing data predominantly stem from Western populations, China’s rapidly aging demographic faces escalating COPD prevalence. Global Burden of Disease projections suggest China will become the country with the highest number of COPD-related deaths by 2040 (11). However, the fall risk among middle-aged and older adult COPD patients remains underexplored in localized studies. Leveraging data from CHARLS, this research aims to provide critical insights into the epidemiological patterns and health outcomes of this population, offering a foundation for targeted intervention strategies.
Methods
Study population and design
The current study analyzes data from the China Health and Retirement Longitudinal Study (CHARLS), which is a nationwide cohort study.1 A multi-stage stratified probability sampling strategy was used to recruit participants from 150 counties or districts across 28 provinces in China. Surveys were conducted in 2011 (as the baseline), followed by subsequent surveys in 2013, 2015, 2018, and 2020. The study collected demographic and health-related data from middle-aged and older adults. CHARLS has been approved by the Biomedical Ethics Review Committee of Peking University (12).
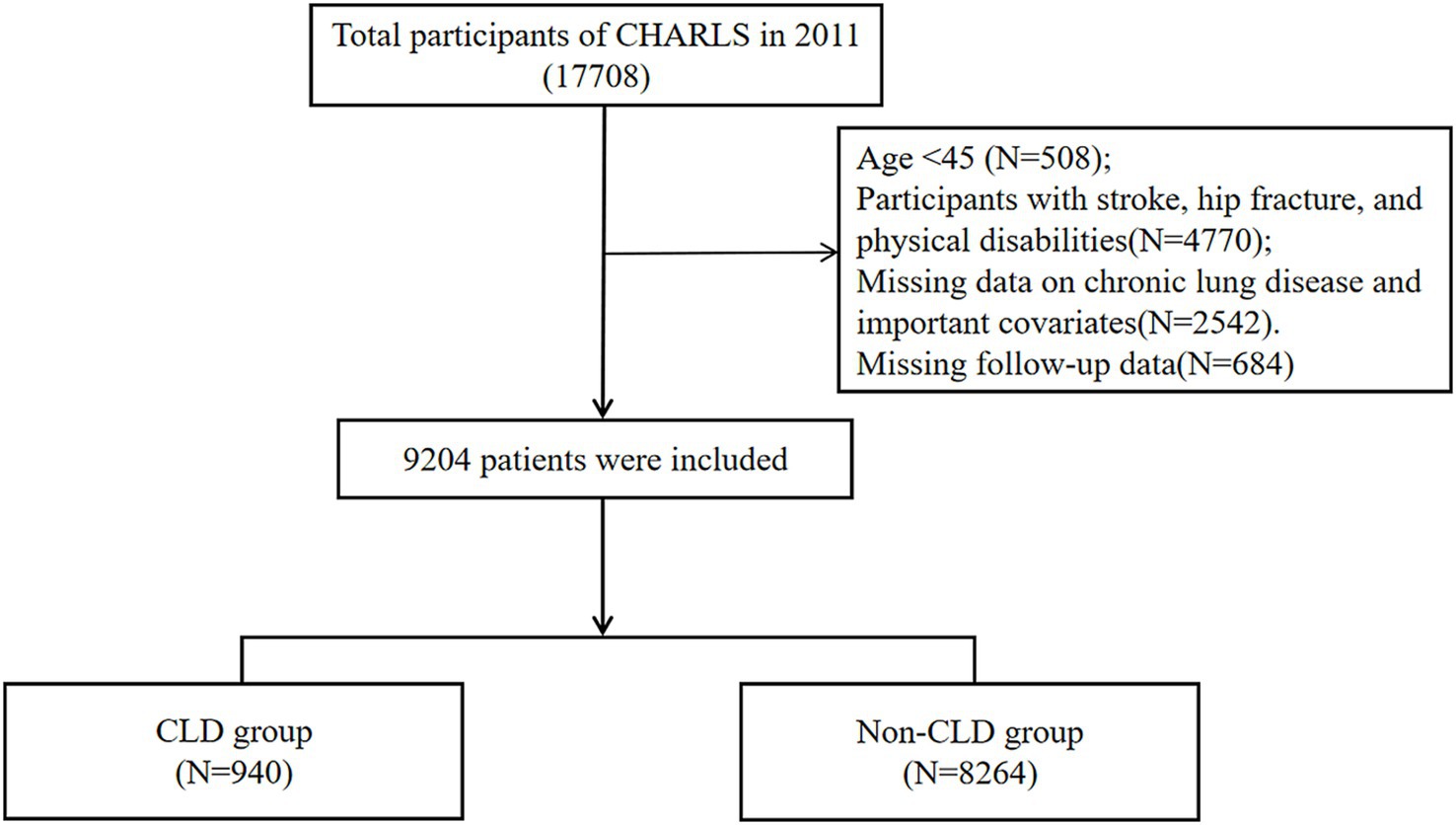
This study utilized a retrospective cohort design based on data from CHARLS. Baseline data (2011) were linked with follow-up surveys (2013, 2015, 2018, 2020) to assess incident falls. Participants were limited to those aged 45 or older. We excluded participants with a history of stroke, disability, or hip fracture at baseline, as well as those with missing potential covariates. Additionally, participants without fall information in the subsequent follow-up surveys were also excluded. The final study cohort included 9,204 participants (Figure 1).
CLD
The diagnosis of CLD was determined based on the information provided by participants at baseline regarding their doctor’s diagnosis, including COPD, chronic bronchitis, emphysema, pulmonary heart disease, and asthma.
Fall accidents
Fall events were defined as a binary outcome (yes/no) based on self-reported responses to the question: “Have you experienced any falls since your last visit?” during follow-up surveys. Participants reporting ≥1 fall in any follow-up were classified as “fallers.” Additionally, participants without fall information in the subsequent follow-up surveys were also excluded.
Covariates
Demographics: Age, gender, education level (categorized as no formal education, elementary school, middle school, or higher), marital status (married vs. unmarried), and residence (urban vs. rural). Behavioral Factors: Smoking status (current smoker vs. non-smoker), alcohol consumption (current drinker vs. non-drinker). Clinical Comorbidities: Hypertension, diabetes, depression (CES-D-10 score ≥10), memory-related diseases (dementia, brain atrophy, Parkinson’s), and mental health disorders. Cognitive Function: Composite score derived from episodic memory and mental integrity tests (range: 0–21).
Depression
The Center for Epidemiologic Studies Depression Scale Short Form (CES-D) was used to assess depression. This is a widely used self-report measure for evaluating depression in the general population (13). The CES-D-10 consists of 10 items, with a total score ranging from 0 to 30. A higher score indicates more severe depressive symptoms. We used a cutoff of ≥10 to distinguish between patients with depression and those who are relatively free of depression (14).
Cognitive function
Cognitive function was assessed using the CHARLS questionnaire, covering two domains: episodic memory and mental integrity. Episodic memory consists of immediate recall and delayed recall. Participants were asked to immediately recall a list of words in any order, and after 4 min, the score was defined as the average of the two components, with a range of 0–10 points. The mental integrity domain, derived from the Telephone Interview for Cognitive Status (TICS), measures orientation, calculation, and visuospatial abilities. Respondents were asked, “Please tell me today’s date, the day of the week, and what season it is?” Additionally, participants were asked to subtract 7 from 100 repeatedly and to draw two overlapping pictures. The score range for this domain is 0–11 points. The overall cognitive score is the sum of the scores from these two domains, with a score range from 0 to 21 points.
Statistical analysis
In this study, continuous variables did not follow a normal distribution; therefore, they are presented as median and interquartile range (IQR) values. Differences between the two groups were tested using the Mann–Whitney U test. For categorical variables, data are expressed as frequencies or percentages and analyzed using the chi-square test or Fisher’s exact test. Logistic regression models were employed to estimate the association between chronic lung disease and falls. In Model 1, no adjustment was made for covariates. Model II was adjusted for age and gender as confounding factors. Model III was further adjusted for age, gender, marital status, educational level, smoking history, drinking history, living area, hypertension, diabetes, depression, memory related disease, mental related disease, cognitive Function. To address potential confounding by baseline characteristics, we performed 1:1 propensity score matching (PSM) between CLD and non-CLD groups. The propensity score was estimated via a logistic regression model including all baseline covariates listed in Table 1. Matching was conducted using nearest-neighbor algorithm with a caliper width of 0.05 standard deviations (SD) of the logit propensity score (15). All data were analyzed using R software (version 4.2.2) and SPSS version 23.0 (IBM Corp., Armonk, NY, United States). A p-value < 0.05 was considered statistically significant.
Results
Baseline characteristics
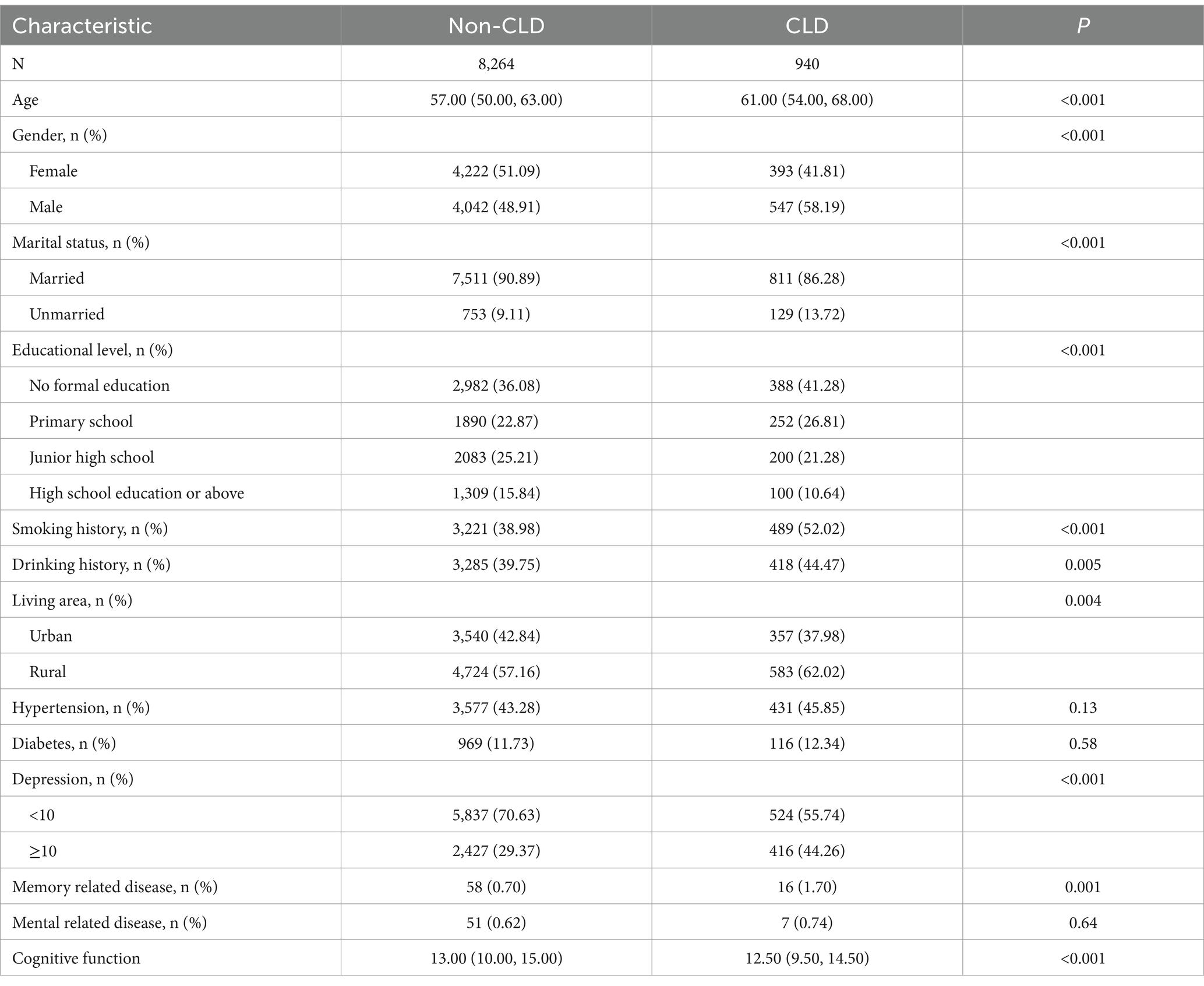
A total of 9,204 participants (CLD: n = 940; non-CLD: n = 8,264) were included in the analysis. As shown in Table 1, participants with CLD were significantly older (median [IQR]: 61.0 [54.0–68.0] vs. 57.0 [50.0–63.0] years; p < 0.001) and more likely to be male (58.2% vs. 48.9%; p < 0.001). The CLD group also had higher rates of smoking (52.0% vs. 39.0%; p < 0.001), alcohol consumption (44.5% vs. 39.8%; p = 0.005), and depression (44.3% vs. 29.4%; p < 0.001). Cognitive function scores were lower in the CLD group (median [IQR]: 12.5 [9.5–14.5] vs. 13.0 [10.0–15.0]; p < 0.001), while hypertension (p = 0.13) and diabetes prevalence (p = 0.58) did not differ significantly between groups.
Longitudinal association between CLD and fall
During the follow-up period, the incidence of falls in non-CLD patients was 27.5% (2,275/8264), while the incidence in CLD patients was 33.5% (315/940). Notably, CLD patients demonstrated a significantly higher incidence of falls (Chi-square test: p < 0.001).
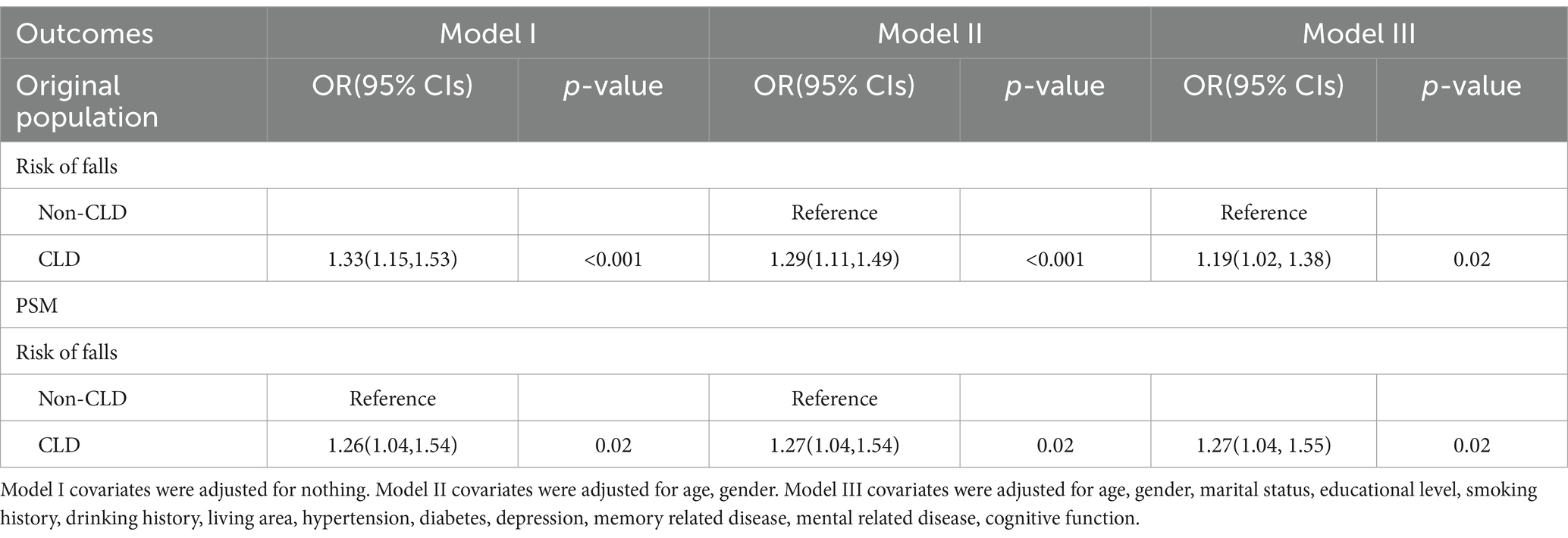
Table 2 presents the results of the logistic regression analysis for the incidence of falls. The original model (Model I), which did not adjust for any variables, showed a significantly higher incidence of falls in the CLD group compared to the non-CLD group during the follow-up period. Model II, adjusted for gender and age, still indicated that CLD was associated with an increased incidence of falls. In Model III, after adjusting for confounding factors, the OR (95% confidence interval) for falls in the CLD group was 1.19 (1.02, 1.38), suggesting that the incidence of falls was 1.19 times higher than that in the non-CLD group.
Propensity score matching
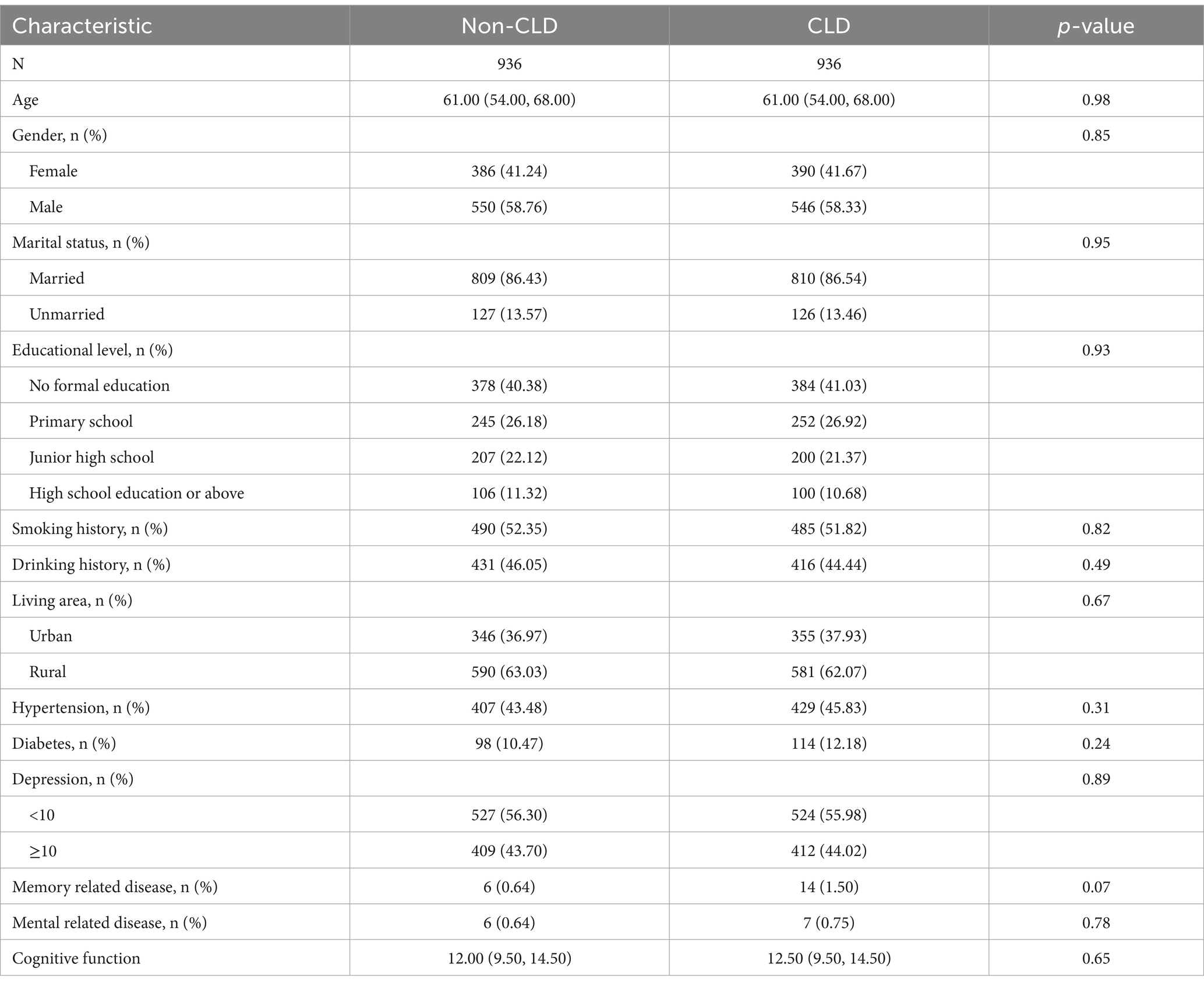
To reduce confounding bias in baseline data, we performed PSM based on the presence or absence of CLD. A total of 936 pairs of patients were successfully matched. After matching, there were no significant differences in baseline characteristics between the two groups (Table 3). Similar to the original population, we also conducted logistic regression analysis on the matched population. Following multivariate logistic regression, the odds ratio (OR, with 95% confidence interval) for the incidence of falls in the CLD group was 1.27(1.04, 1.55) among the PSM population (Table 2).
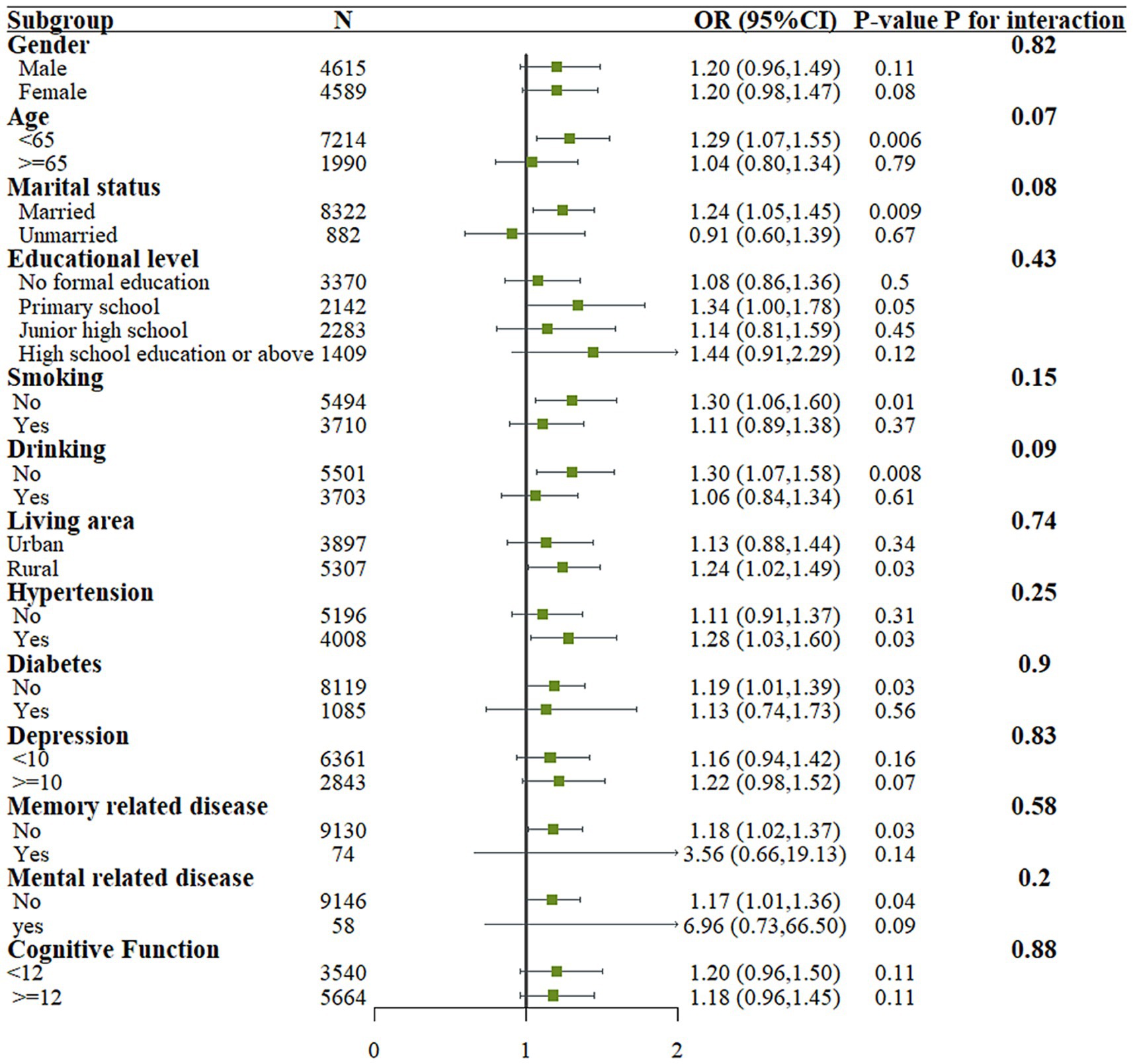
Subgroup analysis
Figure 2 shows the results of stratified analysis based on age, gender, education level, marital status, residence, smoking status, alcohol consumption, cognitive ability, and underlying diseases. The results indicate that no significant interactions were observed in any of the stratified groups (P for interaction > 0.05).
Discussion
This nationally representative, community-based CHARLS study (2011–2020) found that participants with middle-aged and older adult CLD exhibited a significantly higher risk rate of falls compared to those non-CLD. The same results were obtained in the PSM population, and this association remained consistent in the subgroup analysis.
In our study, patients with CLD were older than the general population, and advanced age is a recognized key risk factor for falls. Falls among older adults are often associated with adverse outcomes such as fractures and reduced quality of life. Several studies suggest that older adults exhibit more balance deficits than younger individuals (16, 17). Aging can lead to abnormalities in the sensory system and alterations in muscle activation, resulting in impaired balance among the older adult. When it comes to avoiding falls, older adults tend to maintain higher stability while walking, unlike younger individuals who may adjust their step length or speed. Additionally, patients with CLD often exhibit a range of comorbidities that may amplify their vulnerability to falls (18). Studies have indicated that patients with chronic lung diseases often experience cognitive decline (19, 20), which is consistent with our findings. This decline in cognitive function may lead to impaired balance, thereby increasing the risk of falls. Some research suggests that dementia is a common comorbidity among patients who fall. Patients with dementia are 2–3 times more likely to fall compared to those without dementia (21, 22). In our study, we also found that patients with CLD and concomitant memory-related diseases were more numerous than in the control group. When cognitive abilities decline, gait control is negatively impacted, leading to falls. Additionally, studies have shown that patients who fall are more likely to be receiving treatment with anticonvulsants, antipsychotics, atypical antidepressants, and tricyclic antidepressants. These medications are commonly used to treat pain, insomnia, and depression (23, 24). Therefore, when possible, COPD patients should be encouraged to use non-pharmacological alternatives to these medications or reduce their usage to lower the risk of falls.
During the follow-up process, the proportion of falls among patients with CLD was significantly higher compared to non-CLD participants (33.5% for CLD and 27.5% for non-CLD). A recent two-year follow-up study from the English Longitudinal Study of Aging also reported a higher proportion of falls among patients with COPD compared to healthy controls (33% in COPD and 15% in healthy older adults) (25). In contrast, a cross-sectional study in Canada reported a 1-year fall incidence rate of 46% among COPD patients, which is higher than that observed in our study. This difference may be attributed to the small sample size in the Canadian study (only 39 patients), leading to a potential skew in the results (26).Currently, most studies indicate that the fall incidence rate among older adult COPD patients ranges from 31.7 to 40%, which is similar to our findings (27, 28).Interestingly, a 12-month prospective follow-up study found that the annual fall rate in COPD patients was 1.17 falls per person per year (29) Our study found that after adjusting for factors such as gender, age, and comorbidities, the risk of falls in patients with CLD was 1.19 times higher than in those without CLD. A similar finding was reported in a study using the UK primary care database, where COX regression analysis showed that, compared to non-COPD patients, the fall risk in COPD patients was increased by 1.55 times (30).
Observational studies have identified lower limb weakness, gait disturbances, and balance impairments as common non-respiratory manifestations of COPD, which are key risk factors for falls (31, 32). Balance impairments in COPD patients are independent of lung function, and their presence and impact are not only common but also clinically significant. Compared to controls, COPD patients perform worse on tests assessing risk of falls, such as the Berg Balance Scale, although the relationship with the severity of COPD is variable (33).A previous study on acute exacerbations of COPD found that hospitalization due to acute exacerbations is associated with an increased risk of falls in the 12 months following discharge (29). Bed rest can contribute to balance dysfunction and decreased strength, affecting gait and thereby increasing the risk of falls (34). The incidence of falls is highest within the first 2 weeks after hospital discharge, particularly among patients with pre-existing anxiety, depression, or impairments in activities of daily living (ADL) (35, 36).Current research suggests that COPD induces muscle atrophy through the synergistic effects of chronic systemic inflammation, oxidative stress, and hypoxia. Elevated proinflammatory cytokines, such as TNF-α and IL-6, activate proteolytic pathways including the ubiquitin-proteasome system, accelerating muscle protein degradation (37). Additionally, reactive oxygen species (ROS) impair mitochondrial function, reducing energy production in skeletal muscles (38). Factors like physical inactivity commonly associated with COPD patients may also contribute to muscle atrophy. This muscular degeneration directly leads to postural instability, thereby increasing the risk of falls (39, 40).
This study has several limitations. Firstly, fall prevalence relied on self-reported data, which may underestimate minor falls or overestimate events due to recall bias. Future studies should integrate objective measures (e.g., accelerometers) to improve accuracy. Additionally, the lack of COPD severity data (e.g., GOLD stages) limits our ability to analyze dose–response relationships between disease progression and fall risk. Secondly, although we adjusted for various confounding factors, some unconsidered confounders may require further investigation. Thirdly, there was a lack of information regarding CLD treatment, preventing a comparison of fall incidence between participants who received treatment and those who did not.
Conclusion
This study demonstrates that the risk of falls among middle-aged and older adult patients with chronic lung disease (CLD) in China increases significantly by 19% (adjusted OR = 1.19, 95% CI: 1.02–1.38). This association is further strengthened by propensity score matching analysis (OR = 1.27). These findings underscore CLD as a key factor contributing to the risk of falls. It also highlights the importance of addressing falls among the chronic lung disease population and implementing preventive measures to minimize their occurrence.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: details of the CHARLS data are available from http://charls.pku.edu.cn/pages/data/111/zh-cn.html.
Ethics statement
The data used in this study have been approved by the Biomedical Ethics Review Committee of Peking University. All participants provided written informed consent. The ethics approval number is IRB00001052-11015. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ML: Writing – original draft, Investigation, Methodology, Supervision. XJ: Supervision, Formal analysis, Validation, Writing – review & editing. QH: Writing – review & editing, Conceptualization, Funding acquisition, Software, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Changzhou Health and Youth Talent Training Project (grant no. CZQM2023001) and Changzhou Sci&Tech Program (grant no. CJ20230056).
Acknowledgments
We would like to thank the China Health and Retirement Longitudinal Study (CHARLS) team for providing high-quality data from the Chinese population, which made our research possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Andreassen, H, and Vestbo, J. Chronic obstructive pulmonary disease as a systemic disease: an epidemiological perspective. Eur Respir J Suppl. (2003) 46:2s–4s. doi: 10.1183/09031936.03.00000203
2. GBD. 2019 chronic respiratory diseases collaborators. Global burden of chronic respiratory diseases and risk factors, 1990-2019: an update from the global burden of disease study 2019. EClinicalMedicine. (2023) 59:101936. doi: 10.1016/j.eclinm.2023.101936
3. Ruvuna, L, and Sood, A. Epidemiology of chronic obstructive pulmonary disease. Clin Chest Med. (2020) 41:315–27. doi: 10.1016/j.ccm.2020.05.002
4. Barnes, PJ, and Celli, BR. Systemic manifestations and comorbidities of COPD. Eur Respir J. (2009) 33:1165–85. doi: 10.1183/09031936.00128008
5. Ye, P, Er, Y, Wang, H, Fang, L, Li, B, Ivers, R, et al. Burden of falls among people aged 60 years and older in mainland China, 1990-2019: findings from the global burden of disease study 2019. Lancet Public Health. (2021) 6:e907–18. doi: 10.1016/S2468-2667(21)00231-0
6. Rubenstein, LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. (2006) 35:ii37–41. doi: 10.1093/ageing/afl084
7. Florence, CS, Bergen, G, Atherly, A, Burns, E, Stevens, J, and Drake, C. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. (2018) 66:693–8. doi: 10.1111/jgs.15304
8. Burns, ER, Stevens, JA, and Lee, R. The direct costs of fatal and non-fatal falls among older adults - United States. J Saf Res. (2016) 58:99–103. doi: 10.1016/j.jsr.2016.05.001
9. Tarasconi, M, Oliva, FM, Ambrosino, N, Sotgiu, G, Saderi, L, Zampogna, E, et al. Pulmonary rehabilitation and risk of fall in elderly with chronic obstructive pulmonary disease. Panminerva Med. (2024) 66:10–7. doi: 10.23736/S0031-0808.23.04892-9
10. Chauvin, S, Durocher, E, Richardson, J, and Beauchamp, MK. Experiences of a home-based fall prevention exercise program among older adults with chronic lung disease. Disabil Rehabil. (2022) 44:5513–9. doi: 10.1080/09638288.2021.1938246
11. Fang, L, Gao, P, Bao, H, Tang, X, Wang, B, Feng, Y, et al. Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med. (2018) 6:421–30. doi: 10.1016/S2213-2600(18)30103-6
12. Zhao, Y, Hu, Y, Smith, JP, Strauss, J, and Yang, G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
13. Li, M, Yang, Y, Pang, L, Wu, M, Wang, Z, Fu, Y, et al. Gender-specific associations between activities of daily living disability and depressive symptoms among older adults in China: evidence from the China health and retirement longitudinal study. Arch Psychiatr Nurs. (2019) 33:160–6. doi: 10.1016/j.apnu.2019.08.010
14. Ren, X, Wang, S, He, Y, Lian, J, Lu, Q, Gao, Y, et al. Chronic lung diseases and the risk of depressive symptoms based on the China health and retirement longitudinal study: a prospective cohort study. Front Psychol. (2021) 12:585597. doi: 10.3389/fpsyg.2021.585597
15. Austin, PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multiv Behav Res. (2011) 46:399–424. doi: 10.1080/00273171.2011.568786
16. Riva, D, Mamo, C, Fanì, M, Saccavino, P, Rocca, F, Momenté, M, et al. Single stance stability and proprioceptive control in older adults living at home: gender and age differences. J Aging Res. (2013) 2013:561695. doi: 10.1155/2013/561695
17. Alsubheen, SA, Beauchamp, M, Ellerton, C, Goldstein, R, Alison, J, Dechman, G, et al. Age and sex differences in balance outcomes among individuals with chronic obstructive pulmonary disease (COPD) at risk of falls. COPD. (2022) 19:166–73. doi: 10.1080/15412555.2022.2038120
18. Oliveira, CC, Lee, AL, McGinley, J, Anderson, GP, Clark, RA, Thompson, M, et al. Balance and falls in acute exacerbation of chronic obstructive pulmonary disease: a prospective study. COPD. (2017) 14:518–25. doi: 10.1080/15412555.2017.1342232
19. Liang, S, Han, X, Diao, S, and Li, H. COPD, dietary Fiber intake, and cognitive performance in older adults: a cross-sectional study from NHANES 2011-2014. Exp Aging Res. (2023) 51:92–102. doi: 10.1080/0361073X.2023.2286874
20. Chen, X, Song, H, Liu, J, He, Y, Wei, L, Deng, M, et al. The impact of cognitive impairment on patient activation and their value in self-management among COPD patients. Patient Educ Couns. (2024) 129:108397. doi: 10.1016/j.pec.2024.108397
21. Racey, M, Markle-Reid, M, Fitzpatrick-Lewis, D, Ali, MU, Gagne, H, Hunter, S, et al. Fall prevention in community-dwelling adults with mild to moderate cognitive impairment: a systematic review and meta-analysis. BMC Geriatr. (2021) 21:689. doi: 10.1186/s12877-021-02641-9
22. Peek, K, Bryant, J, Carey, M, Dodd, N, Freund, M, Lawson, S, et al. Reducing falls among people living with dementia: a systematic review. Dementia. (2020) 19:1621–40. doi: 10.1177/1471301218803201
23. Currow, DC, and Agar, MR. Benzodiazepine prescribing in people with chronic obstructive pulmonary disease: clinical considerations. Drugs Aging. (2020) 37:263–70. doi: 10.1007/s40266-020-00756-z
24. McDermott, CL, Feemster, LC, Engelberg, RA, Spece, LJ, Donovan, LM, and Curtis, JR. Fall risk and medication use near end of life among adults with chronic obstructive pulmonary disease. Chronic Obstr Pulm Dis. (2024) 11:604–10. doi: 10.15326/jcopdf.2024.0551
25. Loughran, KJ, Tough, D, Ryan, CG, Wellburn, S, Martin, D, Dixon, J, et al. The Association of Pain with incident falls in people with chronic obstructive pulmonary disease: evidence from the English longitudinal study of ageing. Int J Environ Res Public Health. (2023) 20:6236. doi: 10.3390/ijerph20136236
26. Beauchamp, MK, Hill, K, Goldstein, RS, Janaudis-Ferreira, T, and Brooks, D. Impairments in balance discriminate fallers from non-fallers in COPD. Respir Med. (2009) 103:1885–91. doi: 10.1016/j.rmed.2009.06.008
27. Roig, M, Eng, JJ, MacIntyre, DL, Road, JD, FitzGerald, JM, Burns, J, et al. Falls in people with chronic obstructive pulmonary disease: an observational cohort study. Respir Med. (2011) 105:461–9. doi: 10.1016/j.rmed.2010.08.015
28. Oliveira, CC, McGinley, J, Lee, AL, Irving, LB, and Denehy, L. Fear of falling in people with chronic obstructive pulmonary disease. Respir Med. (2015) 109:483–9. doi: 10.1016/j.rmed.2015.02.003
29. Oliveira, CC, Lee, AL, McGinley, J, Thompson, M, Irving, LB, Anderson, GP, et al. Falls by individuals with chronic obstructive pulmonary disease: a preliminary 12-month prospective cohort study. Respirology. (2015) 20:1096–101. doi: 10.1111/resp.12600
30. Hakamy, A, Bolton, CE, Gibson, JE, and McKeever, TM. Risk of fall in patients with COPD. Thorax. (2018) 73:1079–80. doi: 10.1136/thoraxjnl-2017-211008
31. Smith, MD, Chang, AT, Seale, HE, Walsh, JR, and Hodges, PW. Balance is impaired in people with chronic obstructive pulmonary disease. Gait Posture. (2010) 31:456–60. doi: 10.1016/j.gaitpost.2010.01.022
32. Beauchamp, MK, Sibley, KM, Lakhani, B, Romano, J, Mathur, S, Goldstein, RS, et al. Impairments in systems underlying control of balance in COPD. Chest. (2012) 141:1496–503. doi: 10.1378/chest.11-1708
33. Loughran, KJ, Atkinson, G, Beauchamp, MK, Dixon, J, Martin, D, Rahim, S, et al. Balance impairment in individuals with COPD: a systematic review with meta-analysis. Thorax. (2020) 75:539–46. doi: 10.1136/thoraxjnl-2019-213608
34. Ritchey, KC, Yohannes, AM, Locke, ER, Chen, S, Simpson, T, Battaglia, C, et al. Association between self-reported falling risk and risk of hospitalization for patients with chronic obstructive pulmonary disease. Respir Med. (2023) 220:107466. doi: 10.1016/j.rmed.2023.107466
35. Mahoney, JE, Palta, M, Johnson, J, Jalaluddin, M, Gray, S, Park, S, et al. Temporal association between hospitalization and rate of falls after discharge. Arch Intern Med. (2000) 160:2788–95. doi: 10.1001/archinte.160.18.2788
36. Qian, XX, Chen, Z, Fong, D, Ho, M, and Chau, PH. Post-hospital falls incidence and risk factors among older adults: a systematic review and meta-analysis. Age Ageing. (2022) 51:afab209. doi: 10.1093/ageing/afab209
37. Ji, Y, Li, M, Chang, M, Liu, R, Qiu, J, Wang, K, et al. Inflammation: roles in skeletal muscle atrophy. Antioxidants. (2022) 11:11. doi: 10.3390/antiox11091686
38. Tidball, JG. Inflammatory processes in muscle injury and repair. Am J Physiol Regul Integr Comp Physiol. (2005) 288:R345–53. doi: 10.1152/ajpregu.00454.2004
39. Ma, K, Huang, F, Qiao, R, and Miao, L. Pathogenesis of sarcopenia in chronic obstructive pulmonary disease. Front Physiol. (2022) 13:850964. doi: 10.3389/fphys.2022.850964
Keywords: chronic lung disease, fall, risk, China Health and Retirement Longitudinal Study, logistic regression
Citation: Li M, Jing X and He Q (2025) Risk of fall in middle-aged and older adult patients with chronic lung disease: evidence from the China Health and Retirement Longitudinal Study. Front. Public Health. 13:1547006. doi: 10.3389/fpubh.2025.1547006
Edited by:
Edwin van Teijlingen, Bournemouth University, United KingdomReviewed by:
Marco Bilucaglia, IULM University, ItalyTania Maria Abril Mera, Universidad Católica de Santiago de Guayaquil, Ecuador
Copyright © 2025 Li, Jing and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qian He, NTMyMDMxMzgzQHFxLmNvbQ==
 Min Li1
Min Li1 Xushu Jing
Xushu Jing Qian He
Qian He