
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 12 March 2025
Sec. Digital Public Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1542974
This article is part of the Research Topic Assistive Technologies in Aging and Disability View all 5 articles
 Abdulkarim M. Meraya*
Abdulkarim M. Meraya* Amani Khardali
Amani Khardali Sarfaraz Ahmad
Sarfaraz Ahmad Ahmed Z. Hoshaibari
Ahmed Z. Hoshaibari Atheer A. Alameer
Atheer A. Alameer Raed Y. Jaafari
Raed Y. Jaafari Hilal A. Thaibah†
Hilal A. Thaibah† Moaddey Alfarhan
Moaddey Alfarhan Mamoon H. Syed
Mamoon H. SyedBackground: Telehealth is a promising approach for healthcare delivery that uses telecommunication technologies to enhance accessibility by providing remote health services. This study aimed to identify psychosocial factors that best predict behavioral intention to use telehealth/telemedicine, as mediated by attitude toward use, among older adults with chronic conditions in the Jazan region of Saudi Arabia, and to compare users and non-users.
Methods: Participants were aged 60 years or above, residing in Jazan, and presenting with at least one chronic condition. This study used a quantitative research approach with a cross-sectional questionnaire survey. We stratified all analyses by telehealth use status (users or non-users).
Results: Our study sample comprised 466 participants aged 60 or above with at least one chronic condition. The most prevalent condition was diabetes (29%), followed by arthritis (23%). Among the telehealth users (n = 256), a high percentage (42%) reported that telehealth was better than in-person appointments. Among telehealth users, we found that perceived usefulness [(users: β = 0.501; p < 0.001) (non-users: β = 0.441; p < 0.001)] and facilitating conditions [(users: β = 0.768; p = 0.001) (non-users: β = 0.807; p < 0.001)] positively affected attitudes to using telehealth. Telehealth users and non-users reported dislike or fear of the service and unavailability of appointments as the most important barriers to using telehealth services.
Conclusion: The results of this study are important for designing new telehealth applications, especially for older adults in Saudi Arabia. Designers and developers must understand that the attributes and capabilities of telehealth applications should be simple and user-friendly to encourage older adults to increase their intention to use telehealth.
Telehealth is a potential approach to a healthcare delivery model that uses telecommunication technologies to enhance healthcare accessibility by providing remote health services to individuals with inadequate access to such services (1). It is the remote delivery and support of health-related services by the adoption of telecommunication and electronic information technology (2). Additionally, it could assist in making healthcare services more accessible and cheaper and maintaining continuity of care (3, 4). Analogously, virtual healthcare is a segment of telehealth involving the use of communication tools such as audio, video, and text messages to deliver care virtually rather than in person (5). The dependency and financial reliance of older adults will surge as the global population increases if older adults are not supported with the assistance they require to perform their daily activities independently (6). Research indicates that older adults' quality of life (QoL) may be significantly improved through the use of information and communication technology (ICT). This improvement could stem from increased connectivity with family, enhanced personal independence, and improved societal engagement. (6). Due to the rapid increase in the population of older adults, financial support and health maintenance have been identified as their two major concerns, and many of these individuals require specialized critical care due to age-related illness and chronic conditions (7). One-sixth of the global population is expected to be aged 60 years or older by 2030. The population of individuals aged 60 years and older is expected to increase from 1 billion in 2020 to 1.4 billion, and then to 2.1 billion by 2050, effectively doubling this age group (8). The demographic composition of the Kingdom of Saudi Arabia indicates that older adults comprise approximately 2.7% of the total population, whereas in Jazan Province, this proportion is slightly higher at 3.6% (9). As individuals grow older, they frequently encounter a range of health issues including diabetes, chronic obstructive pulmonary disease, depression, dementia, and osteoarthritis (8). A considerable proportion of the population of older adults has at least one chronic disorder requiring frequent intensive care and management (10). Self-care is a proactive means of maintaining health by observing symptoms, pursuing therapy, and assessing the effectiveness of the treatment. For more effective management, older adults should be aware of their condition and have the ability and desire to determine goals, overcome complications, and monitor therapeutic outcomes (11). For older adults residing alone, the effective application of information technology along with digital health technology (DHT) appeared most significant in mitigating health expenses and encouraging self-care management (12). Incorporating these technologies in healthcare could alleviate and improve the overall health of older adults at their residences while encouraging their autonomy through telehealth (13).
Remote patient care is facilitated through telehealth, which combines diverse communication technologies and the digital transmission of health data (14). It is not a new concept; however, its application has become common during the previous decade. Notwithstanding the various difficulties, older adults utilize telehealth services when necessary (15). Despite the demonstrated efficacy of telehealth, these technologies are frequently developed without sufficient consideration for their ease of use by patients and caregivers (8). Indeed, most of the telehealth devices in current use were created and implemented regardless of patient opinions about device usability. Usability is the degree to which a patient or caregiver believes a device is user-friendly or simple to use. Telehealth use can be facilitated by evaluating usability, which provides assistance concerning the desired psychological or physical consequences of technology on its users, expediting the practice of telehealth (16). Facilitators are features in either the older patient or the device that help obtain the desired outcome, and barriers are features that hinder its use for the patient (17). With advances in technology and digital healthcare, healthcare accessibility has shifted from a physician-centric model to a patient-oriented approach that enables remote monitoring (18). Due to social restrictions and distancing enforced by the COVID-19 pandemic, DHT has been effectively used to provide safe access to healthcare services and medical facilities (19, 20). The COVID-19 pandemic has revolutionized approaches to developing medical services and underscored the importance of remote health monitoring. Digital healthcare has become the most effective alternative to delivering healthcare to older adults, while reducing exposure to COVID-19 and overload resulting from persistent hospital visits (21). Numerous types of systems have been established to provide healthcare and services to older adults, including wearable devices, mobile health, telemedicine, and artificial intelligence. COVID-19′s impact and risks were substantially mitigated by DHT, which proved instrumental in empowering older adults to track symptoms and manage their wellbeing (22, 23). The use of mobile-health applications during the COVID-19 pandemic displayed progressive effects on the healthcare process and augmented the remote monitoring of healthcare (24).
Despite remarkable advances in DHT, older adults face challenges and barriers due to physical disabilities such as poor vision, cognitive problems, a lack of technological skills, and a lack of perceived ability and time. The digital and e-health literacy of older adults can influence their capacity to use ICT (25). Regardless of advances in healthcare technology, it is essential to assess how older adults perceive this new technology, how they feel about it, and their intention to use it. It is also crucial to identify their barriers to adopting DHT. Older adults' willingness and perspectives are also important when adopting and employing technology-based monitoring systems (26). This study primarily sought to identify which psychosocial factors best predict behavioral intention to use telehealth/telemedicine, as mediated by attitude toward use, among a sample of older adults with chronic conditions in the Jazan region of Saudi Arabia, and to conduct comparisons between users and non-users of telehealth/telemedicine.
The study participants comprised of older adults residing in the southwestern province of Jazan, Saudi Arabia. Individuals were included in this study if they were aged 60 or above and had at least one chronic condition. In order to ensure independent completion of the questionnaire, subjective judgment was used by the data-collectors to determine if there were cognitive impairment/limitations. An evaluation of cognitive functioning was not conducted via a validated scale and self- or proxy-reports (such as by a family member) of cognitive health/decline were not solicited. Prior to participation in the study, trained data collectors verbally evaluated the cognitive functions of the potential participants. By engaging in informal communication, they assessed their language skills and ability to maintain focus and coherence, followed by an evaluation of their orientation, which included inquiries about the present date, location, and recent events. This method helped build a connection with the participants in addition to identifying any communication challenges and verifying preparedness for answering the questionnaire.
We employed purposive and snowball sampling methods in order to obtain a representative sample. Recruitment of data collectors was done initially by advertising PharmD students at Jazan University's College of Pharmacy, resulting in 34 volunteers. Training was provided to these volunteers on effective communication, techniques to assess cognitive function, and ethical practices for data collection. Potential participants were sought from public places, community centers, and healthcare facilities in the region. Informed consent was obtained before the questionnaire was administered. At the end, participants were requested to suggest other individuals who were eligible for participation in the study. The recruitment process continued through this process until our desired sample size was achieved.
A cross-sectional (quantitative) questionnaire was used to evaluate the proposed model. The data collection period was from early June 2023 to mid of mid-September 2023. Both paper-based and online questionnaires were used to collect data. Qualtrics XM was used as the online survey platform. Additionally, the responses obtained through paper-based questionnaires were transferred to Qualtrics XM for analysis and storage. Assistance was provided to participants by data collectors when needed, and clarifications were offered without influencing their responses, thereby ensuring the integrity of the data. In cases where participants had difficulty reading or writing, a proxy respondent, typically a family member, was allowed to assist, given the participant's presence and consent. Completing the questionnaire took ~15–20 min.
The technology acceptance model (TAM) is a well-established and widely recognized conceptual model to study the factors influencing individuals' intentions to use telehealth (12, 27–34). The TAM is particularly suited to the older population because it accounts for the perceived usefulness (PU) and perceived ease of use (PEOU) of technology—critical factors for older adults who may be less familiar with digital platforms. Moreover, the TAM has been successfully applied in previous studies involving older adults, demonstrating its effectiveness in understanding technology acceptance in this demographic (12). As shown in Figure 1, the TAM posits that PU, PEOU, social impact, and facilitating conditions affect the attitude toward the use of a particular technology, which affects the behavioral intention to use that technology. PU indicates the extent to which older adults perceive that telehealth can augment their healthcare access, convenience, and quality. PEOU indicates the degree to which older adults perceive telehealth as user-friendly, intuitive, and easy to navigate. Additionally, social influence encompasses the impact of family, relatives, friends, and healthcare professionals in endorsing and encouraging the use of telehealth, while facilitating conditions include the availability of necessary resources, infrastructure, and technical support to facilitate telehealth adoption. Attitude toward telehealth (ATT) was characterized as positive or negative feelings about using a particular technology. Behavioral intention (BI) concerned the use of the technology influenced by one's attitude. BI refers to the extent to which an individual has consciously developed plans to perform or refrain from a specific behavior in future and indicates that a person's BI toward using technology has a positive influence on their actual use of technology. By employing the TAM framework, researchers can study and apprehend the various factors influencing individuals' intentions to use telehealth, enabling the development of effective strategies to enhance telehealth acceptance and use. Hence, we hypothesize that attitude toward using telehealth would mediate the relationship between behavioral intention to use telehealth and perceived usefulness, perceived ease of use, social impact, and facilitating conditions.
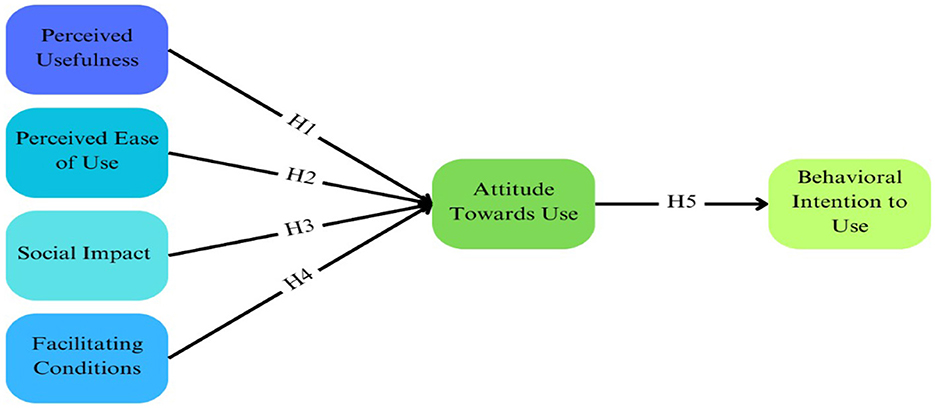
Figure 1. Structural path—technology acceptance model (12).
The survey instrument contained the following.
The variables included were sex (male or female), age in years, occupation before retirement (office worker, professional, self-employed, blue-collar, dependent, or other), education level (illiterate, high school or less, diploma, bachelor, or more), health insurance (yes or no), chronic conditions (diabetes mellitus, hypertension, heart disease, gastrointestinal complications, dyslipidemia, arthritis, mental illnesses, or other conditions).
To distinguish between users and non-users of telehealth services, we asked the question, “Have you had a telemedicine/telehealth appointment (appointment with your health provider by video or phone instead of an in-person appointment)?” We also asked the users, “How did your telemedicine/telehealth visit compare to a traditional in-person medical visit?” with a response scale (better than, just as good as, worse than a traditional visit, and not sure).
The TAM constructs were measured using scales adapted from previous studies that demonstrated good reliability and validity in similar contexts (12, 27–34).
• The PU was evaluated using a 3-item scale: (i) Healthcare using telehealth will help me manage my health. (ii) I believe that using telehealth will make my daily life safer. (iii) Using telehealth will improve my quality of life.
• PEOU also was measured using a 3-item scale: (i) I think using telehealth would be simple. (ii) Learning to use telehealth applications will be easy. (iii) Telehealth-healthcare will be convenient to use.
• Social impact was measured with the following items: (i) Family will approve of my use of telehealth. (ii) Acquaintances will recommend that I use telehealth. (iii) Acquaintances will approve of me using telehealth.
• Facilitating conditions were measured with the following items: (i) I will know how to use telehealth. (ii) If I encounter difficulties using your telehealth, I think someone will be able to help. (iii) I have sufficient resources to use telehealth.
• ATT was measured using a 3-item scale, which included the following statements: (i) Using telehealth will have a positive impact on my life. (ii) Using telehealth will benefit my health. (iii) I have positive thoughts about telehealth.
• BI to use was measured with the following items: (i) I would use telehealth if given the opportunity. (ii) I will use telehealth for my healthcare. (iii) I will use telehealth to change my life for the better.
Participants responded to these questions using a Likert-type scale ranging from “strongly disagree” to “strongly agree.” The instrument was reviewed by experts to ensure content validity. A pilot study with 30 participants was conducted to assess the clarity and reliability of the scales. Cronbach's alpha coefficients for the constructs were >0.70, indicating acceptable internal consistency.
Prior to description of the specific facilitators used in our study, it is crucial to distinguish between facilitating conditions and facilitators to using telehealth. Facilitating conditions assess existing support and resources, including users' perceived ability to use telehealth, access to assistance, and resource availability. In contrast, facilitators to using telehealth address design features and improvements to enhance telehealth acceptance, especially for older users, such as simplified interfaces, guidance systems, and age-appropriate visuals. While facilitating conditions evaluate current support for telehealth use, facilitators to using telehealth explore enhancements for wider adoption. This distinction helps assess present readiness for telehealth and strategies for improving accessibility and acceptance. In this study, facilitators to using telehealth were measured using a 3-item scale, which included the following statements: (i) Devices that use fewer buttons could be a factor that aids in the acceptance of telehealth. (ii) Providing visual and audio guidance could be factors that aid in the acceptance of telehealth. (iii) User-friendly images appropriate for older adults could be factors that aid in the acceptance of telehealth. Participants responded to these questions using a Likert-type scale ranging from “strongly disagree” to “strongly agree.” These items specifically address design features and improvements that could enhance telehealth acceptance, particularly for older users, aligning with the concept of facilitators to using telehealth as described earlier.
Participants were asked for their agreement or disagreement on a five-point Likert scale to determine whether the following were barriers to accessing telehealth: (i) The reason that I could not access a telehealth service is that I do not have internet. (ii) The reason that I could not access a telehealth service was dislike or fear of the service. (iii) The reason that I could not access a telehealth service was that an appointment was not available when required. (iv) The reason that I could not access a telehealth service was that it was not available from my general practitioner or other health professional.
The questionnaire was developed based on earlier studies that employed the TAM (12, 27–34) and adapted to the cultural context of the older population in Saudi Arabia. Prior validation studies have shown these scales to be reliable and valid in assessing technology acceptance. Adjustments were made to language and content to ensure relevance and comprehension. The pilot testing helped refine the questionnaire for clarity and cultural appropriateness.
This study was approved by the Institutional Review Board and Ethics Committee at Jazan University, Saudi Arabia (reference number: REC44/10/653). The study was performed in accordance with the principles of the Declaration of Helsinki. Each participant provided an informed consent prior to participation. Those who participated in the online survey through Qualtrics XM were provided with detailed information about purpose and procedures of the study and were required to review the consent form and indicate their agreement before proceeding with the questionnaire. The voluntary nature of participation, confidentiality, and anonymity of the responses were emphasized. Participants were also informed of their right to withdraw at any time by simply exiting the survey, without any consequences.
For participants completing the paper-based survey, data collectors elucidated study's purpose and procedures before obtaining signed informed consent. Participants were assured of confidentiality and anonymity of their responses and were notified that their participation was voluntary and that they exit the survey at any time with no consequences. In cases where participants had reading difficulties, consent forms were read aloud, and verbal consent was documented with the participant's approval.
Descriptive statistics were generated to summarize participant characteristics. Frequencies and percentages were derived for categorical variables and presented in tables and graphs. Continuous variables were summarized using means and standard deviations. Chi-square tests were performed to examine differences in demographic categorical variables between users and non-users. To evaluate differences in continuous demographic variables between the two groups, t-tests were employed. For every scale employed in the present study, an exploratory factor was determined through principal component extraction analysis. For assessing the data suitability for factor analysis, we employed Bartlett's test whereas sampling adequacy was checked by Kaiser-Meyer-Olkin test (35). To ascertain the number of components, Velicer's test was utilized (36). Relationships between independent variables and outcomes in the TAM were estimated using SEM because of its appropriateness for examining theoretical frameworks, such as the TAM. SEM allows for the concurrent examination of multiple relationships between latent and observed variables (37). In the SEM, the maximum likelihood was employed as an estimator due to its suitability. To assess the model's goodness of fit, we used several indicators such as the chi-square statistic, root mean square error of approximation (RMSEA), comparative fit index (CFI), and Tucker-Lewis index (TLI). The model was considered to have an acceptable fit if it met the following benchmarks: RMSEA value of 0.08 or less, CFI of at least 0.90, and TLI of 0.90 or above. The analysis was stratified by telehealth use status (users and non-users) to explore potential differences in the factors influencing telehealth acceptance between these groups. Stratification enables a better understanding of how prior experience with telehealth may impact the relationships proposed in the TAM and helps identify tailored strategies to increase telehealth adoption. A statistical significance of p ≤ 0.05 was used to identify any differences and associations between variables. STATA version 18 was used for data analysis.
Descriptive statistics of the sample by telehealth use status are displayed in Table 1. Of the study sample (n = 466), 256 (55%) older adults used telehealth in the Jazan region of Saudi Arabia. A significant relationship existed between occupation status before retirement and telehealth use. Higher percentages of older adults with office-based occupations (62% vs. 38%), professional occupations (79% vs. 21%), and self-employed status (60% vs. 40%) were telehealth users. Additionally, a significant relationship was found between education level and telehealth use status, indicating that education influences telehealth adoption among older adults. Specifically, a higher percentage of illiterate older adults were telehealth non-users (55% vs. 45%), which may be attributed to lower technological literacy and discomfort with using digital platforms. However, a higher percentage of older adults with a college degree or higher were telehealth users (59% vs. 41%), possibly due to greater familiarity with technology and a better understanding of the advantages offered by telehealth services. Furthermore, a higher percentage of older adults with health insurance were telehealth users (80% vs. 20%) than those without health insurance. This indicates that health insurance may be crucial in facilitating access to telehealth services.
Among telehealth users (n = 256), a high percentage (42%) reported that telehealth was better than in-person appointments. Furthermore, more than a quarter reported no difference between telehealth and traditional visits (26%). Conversely, 15% reported that telehealth was worse than traditional visits. Twelve percent of the older adults reported that they were unsure about the difference between telehealth and traditional in-person visits.
The factor loading and reliability tests for all scales in this study are presented in Appendix 1. Internal reliability of the items was confirmed by values of Cronbach's alpha exceeding 0.7. SEM's goodness-of-fit measures are shown in Table 2, indicating an acceptable fit to the data. A significant chi-square result was observed [χ2(124) = 328.836, p < 0.001]. Borderline acceptable fit was indicated by RMSEA value of 0.080 (90% CI: 0.070–0.091). The results of CFI (0.952) and TLI (0.941) both suggest a good to excellent fit. SEM results of telehealth users are displayed in Table 3 which indicate that PU had a significant positive effect on ATT (β = 0.501 [95% CI = 0.252–0.749]; p < 0.001). Facilitating conditions (β = 0.768 [95% CI = 0.324 −1.212]; p = 0.001) had a significant positive effect on ATT among telehealth users. Among telehealth users, ATT had a significant effect on BI to use telemedicine (β = 0.875 [95% CI = 0.780–0.971]; p < 0.001). The results suggest that ATT fully mediates the relationship between PU and BI. Specifically, PU had a significant indirect effect on BI through ATT (Î2 = 0.438, 95% CI [0.220, 0.656], p < 0.001). The total effect of PU on BI is identical to the indirect effect, indicating that PU influences BI entirely through its impact on ATT. The direct effect of PU on BI is negligible, supporting the hypothesis of full mediation. Similarly, the relationship between FC and BI is also fully mediated by ATT. FC has a significant indirect effect on BI through ATT, with the total effect of FC on BI being identical to its indirect effect.
The factor loading and reliability tests for all scales used in this study are presented in Appendix 2. The variables were internally reliable, as the Cronbach's alpha values were higher than 0.7. The goodness-of-fit measures for SEM, as presented in Table 4, indicate that the model is an overall good fit. Table 5 displays the results of the SEM model for telehealth nonusers. The results indicate that PU had a significant positive effect on ATT (β = 0.441 [95% CI = 0.230–0.651]; p < 0.001). Conversely, PEOU and social impact had no significant effect on ATT. Nevertheless, facilitating conditions positively affected the ATT (β = 0.807 [95% CI = 0.388 −1.226]; p < 0.001). Among telehealth non-users, ATT had a significant effect on the BI to use telemedicine (β = 0.902 [95% CI = 0.793–0.948]; p < 0.001). The results indicate that the relationship between PU and BI is fully mediated by ATT. Specifically, PU had a significant indirect effect on BI through ATT, indicating that PU influences BI entirely through its impact on ATT. The direct effect of PU on BI was negligible, supporting the hypothesis of full mediation. Similarly, the relationship between FC and BI is fully mediated by ATT. FC has a significant indirect effect on BI through ATT, with the total effect of FC on BI identical to its indirect effect. This finding indicates that FC influences BI entirely through its impact on ATT, with no meaningful direct effect, further supporting the hypothesis of full mediation.
Figure 2 shows the results regarding facilitators of telehealth use for users and non-users. Among telehealth users, a significant majority (83%) expressed either agreement or strong agreement regarding the incorporation of user-friendly images appropriate for older adults, which could enhance the acceptance of telehealth.” This suggests that visual simplicity and age-appropriate graphics are crucial in enhancing usability for older adults, who may have visual impairments or reduced familiarity with digital interfaces. Furthermore, 85% of the users agreed or strongly agreed that telehealth acceptance could be enhanced if the devices used fewer buttons and provided both audio and visual guidance. These findings indicate that simplifying device interfaces and offering multimodal guidance can significantly reduce technological barriers. For older adults, who may experience cognitive decline or physical limitations such as reduced fine motor skills, fewer buttons and clear instructions make technology more accessible and less intimidating.
Similarly, among non-users, 85% either agreed or strongly agreed with the importance of “user-friendly images” and “devices that use fewer buttons” in aiding the acceptance of telehealth. This reflects a shared recognition across both groups that simplicity and ease of use are key factors in adopting telehealth services. The high agreement among non-users highlights potential areas to focus on to increase telehealth adoption in this group.
Figure 3 displays the results for barriers to using telehealth for users and non-users. Among telehealth users, 70% agreed that they could not access telehealth services because appointments were unavailable when required. This indicates that even those familiar with telehealth face systemic issues such as scheduling difficulties, possibly due to the limited availability of healthcare providers offering telehealth services in their area. Additionally, 68% of users agreed that “dislike or fear of the service” was a barrier. This suggests that despite using telehealth, a significant proportion of older users may still harbor apprehensions about the technology, potentially stemming from generational gaps in technology adoption or concerns about the quality of remote consultations. Furthermore, 67% of the users agreed that not having the Internet was the reason they could not access a telehealth service. This highlights the digital divide affecting even current users, where unreliable internet connectivity or lack of digital literacy can impede consistent access to telehealth services.
Among telehealth non-users, 64% agreed that “dislike or fear of the service” prevented them from accessing telehealth. This reflects a cultural preference for traditional in-person healthcare interactions and possible distrust of virtual platforms among the older adults. Similarly, 63% agreed that appointments not being available when required was a barrier, indicating that access issues are a common challenge regardless of telehealth use status.
This study aimed to identify which key psychosocial factors best predict individuals' behavioral intention to use telehealth services, as mediated by attitude toward use, among older adults with chronic health conditions in Saudi Arabia's Jazan region and to conduct comparisons between its users and non-users. Our research findings support our hypothesis that attitude toward using telehealth would mediate the relationship between behavioral intention to use telehealth and perceived usefulness and facilitating conditions. However, our findings did not support the hypothesis that attitude toward using telehealth would mediate the relationship between behavioral intention to use telehealth and perceived ease of use and social impact. PU had a significant effect on ATT among both users and non-users. Previous studies have confirmed that PU significantly affects adoption of telehealth (38, 39). Another study reported that both PU and PEOU positively affect intention to use telehealth, with PU having a stronger influence on telehealth adoption (40).
Facilitating conditions significantly influenced the attitudes of both users and non-users toward using telehealth services. Cimperman et al., demonstrated that FC directly influenced BI of older adults to use Home Telehealth Services (41). Woo and Dowding highlighted that the availability of clinical/technical support (facilitating conditions) was associated with telehealth initiation (42). Additionally, our findings suggest that, among users and non-users, ATT significantly mediated BI to use telehealth services. This finding of positive mediation of attitude on BI is supported by another study in which participants had a positive attitude toward using telehealth and was correlated with the BI toward use of telehealth in the future (43). Kohnke et al. included attitude as a moderator in their structural equation modeling (SEM) for predicting BI to use telehealth (44).
The findings of this research show that PU has a significantly beneficial impact on the BI (mediated by ATT) to use telehealth among the Saudi older population. Comparable results were found by Cimperman et al., where performance expectancy (which is closely related to PU) had a direct impact on the BI to use home telehealth services (41). Another Chinese study on the adoption of telehealth indicated that PU significantly and positively affected BI among older adults (45). However, a study from the Philippines reported that effort expectancy has a more significant influence on BI to use telehealth than other factors (46). Previous studies have also identified other factors, such as social impact (47) and system self-efficacy (48), which may have considerable influence on the adoption of telehealth.
Our findings underscore the importance of telehealth services being perceived as useful in managing health conditions, especially among those already using telehealth. Thus, enhancing the PU of telehealth services is essential for widespread acceptance. Intuitive design and clear demonstration of benefits can influence perceptions about the usefulness of telehealth systems. The practical implications of these findings suggest that healthcare providers should actively promote the benefits of telehealth to older patients, highlighting how it can improve health management and access to care. Providers can address training needs by offering practical demonstrations, informational materials, and personalized support to increase patients' familiarity and comfort with telehealth technologies. It is suggested that technology designers integrate user-friendly interfaces tailored to the capabilities of older adults. Simplifying technology interfaces using larger fonts, clear icons, and straightforward navigation, as well as providing visual and audio guidance, can make telehealth platforms more accessible. Improvements should be implemented in telehealth-related technologies, such as bio-physiological data monitoring tools, integration of data with electronic medical records, and connection of data with multiple sources to enhance functionality and appeal to users and potential users.
Policymakers have a crucial role in addressing barriers to telehealth adoption among older adults. Although Saudi Arabia has made significant strides in expanding internet infrastructure as part of Vision 2030—achieving 100% mobile-cellular network coverage and high percentages for 3G and 4G coverage even in rural areas (49)—the high percentage of participants citing lack of internet access as a barrier suggests that challenges remain. These challenges may not stem solely from infrastructural deficiencies but could include factors such as the affordability of internet services, lack of access to suitable devices, or digital literacy gaps among the older population. Therefore, policymakers should not just focus on maintaining and enhancing infrastructure but also work toward affordability and accessibility of internet services and devices to the older adults. The provision of training programs for older adults are an important initiative that can improve digital literacy. These initiatives are in line with the country's long-term plan (Vision 2030), which aims to achieve digital transformation, inclusivity, and transformation of the healthcare sector. Implementation of these strategies could substantially enhance the adoption of telehealth among older adults and ensure the inclusion of all segments of society.
The research was conducted in Saudi Arabia's Jazan region, the country's second-smallest region, with 40% of its population living in rural settings (50). The results reveal that technological obstacles, such as insufficient internet connectivity, and personal factors, including fear or dislike of telehealth services, significantly affect older adults' use of telehealth. The high proportion of poor internet access (67% of users and 60% of non-users) highlights the digital gap in rural areas, where challenging terrain and scattered populations limit the technological infrastructure. Cultural elements, such as resistance to change and preference for in-person interactions (68% of users and 64% of non-users expressing fear or dislike of telehealth services), exacerbate these challenges. The older generation, which has grown without modern technology, is less comfortable with complex digital platforms and finds it challenging to navigate.
From a demographic perspective, older adults frequently encounter difficulties such as declining eyesight, hearing loss, and decline in motor skills, making user-friendly designs critical for the adoption of telehealth systems. This is underscored by 83%−85% of both users and non-users expressing their agreement on preferring easy-to-understand visuals and devices with minimal buttons on telehealth platforms. Additionally, telehealth interfaces should be simplified and include audio and visual support to enhance usability and acceptance among older adults. Focused public health awareness campaigns should be undertaken to educate older adults regarding the benefits of telehealth and address their fears regarding its use. To address these challenges and capitalize on facilitators, a holistic and culturally aware strategy tailored to specific demographic requirements is necessary, which should aim to improve the technological infrastructure, boost digital literacy, and build confidence in older adults with regard to the use of telehealth services. Steps should be taken to improve internet access in rural areas, and community programs should be implemented to train older adults to use digital devices and improve their digital literacy. Health technology companies should design customized interfaces based on the preferences of older adults, obtain extensive feedback from users, and undergo evaluation by healthcare providers to ensure mapping of the needs and telehealth solutions. Health authorities should provide training programs to health care professionals on the use of telehealth services and strategies to provide support to older adults. Special training should be provided to health care professionals when dealing with older adults with visual or hearing disabilities. From the healthcare providers' perspective, identifying the training needs is crucial to understanding the gaps and providing hands-on demonstrations to the older adults to build their confidence and mitigate their apprehensions associated with the use of telehealth.
A potential limitation of this study is that it was conducted only in the Jazan region, which may limit the generalizability of the findings to other regions of Saudi Arabia. The cultural, infrastructural, and socioeconomic characteristics of Jazan may differ from those of other areas, impacting telehealth acceptance differently. Additionally, the use of snowball sampling might introduce selection bias, as participants may refer others with similar characteristics or ATT. This method may not capture a fully representative sample of the older population. Our study lacked data on the frequency of telehealth utilization among participants, preventing us from distinguishing between one-time users and those who had multiple or ongoing sessions, which may vary considerably. Future investigations should include this variable to offer a more detailed understanding of telehealth experiences at different usage levels. Another limitation of our study is the analysis of facilitators and barriers to the use of telehealth services. We employed a descriptive approach that restricted the deeper insights provided by the inclusion of a qualitative approach. Participants were asked to select only from the options provided instead of expressing their own views through open-ended questions. Employing a mixed-methods approach combining both qualitative and quantitative techniques could benefit future studies by gaining a more comprehensive understanding of telehealth usage in lieu of facilitators and barriers. An additional limitation was the potential lack of clarity of certain survey items, as they were not tailored to capture specific information. Our questionnaire was aimed at gathering broader perceptions and attitudes toward the use of telehealth, permitting a broad understanding of the factors that influence the adoption and use of telehealth.
The Technology Acceptance Model (TAM) was applied as the conceptual model for this study as it has been widely applied across various information technology domains, which demonstrates its generalizability to some extent. Nevertheless, the generalizability of the TAM is not without limitations or contradictions. Some studies have found inconsistencies in the TAM's applicability, especially when applied to specific user groups or technologies. For example, in the healthcare sector, perceived ease of use did not predict intention to use online health applications by physicians (51). Similarly, regarding electronic collaboration technology, perceived usefulness was found to have a negative association with system usage, thereby contradicting the typical findings of the TAM (52). In view of such inconsistencies, the generalizability of TAM may vary depending on the specific technology and the user group under study, and caution should be exercised when extrapolating our findings to a larger scale.
To improve the applicability of findings on a larger scale, future studies should be conducted across various regions in Saudi Arabia. This approach would allow for a comparison of results and to identify the regional differences in the acceptance of telehealth services. Expanding the research to include younger populations or different demographic groups could provide comparative insights into telehealth acceptance across age groups. Additionally, longitudinal studies examining changes in attitudes and use over time would be valuable, especially as technology evolves and becomes more integrated into healthcare services. Investigating other adoption models beyond the TAM could also offer a deeper understanding of factors influencing telehealth acceptance. This study has significance for guiding future research, as well as for Saudi Arabian healthcare policymakers.
This study examined the factors influencing ATT and BI to use telehealth among older adults with chronic conditions in the Jazan region of Saudi Arabia. Key findings indicate that PU and facilitating conditions positively affect ATT among both users and non-users. Barriers such as lack of internet access and fear or dislike of telehealth services hinder use, whereas facilitators such as user-friendly interfaces and simplified devices enhance acceptance. These findings have important practical implications. For healthcare providers, a need exists to address training and support for older patients by offering education on how to use telehealth technologies and emphasizing their benefits. Policymakers should focus on improving internet infrastructure in rural areas, subsidizing internet access and devices for older adults, and developing policies encouraging telehealth adoption. Telehealth application developers should design interfaces that meet the needs of older adults users, incorporating simplified navigation, clear visual aids, and multimodal guidance to enhance usability.
Altogether, this study advances the understanding of telehealth by highlighting the key factors that influence the adoption of telehealth among older adults in Saudi Arabia. The study findings can aid healthcare providers and policymakers in understanding the barriers in existing support systems and taking steps to address them. They can also use facilitators to improve the accessibility of healthcare technology, promote independence, and enhance the quality of life of older adults through tailored telehealth educational programs, thereby leading to better health outcomes and supporting the healthcare transformation of Saudi Arabia.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Institutional Review Board and Ethics Committee of Jazan University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
AM: Conceptualization, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. AK: Methodology, Writing – original draft. SA: Methodology, Software, Writing – original draft. AH: Data curation, Writing – original draft. AA: Data curation, Writing – original draft. RJ: Data curation, Writing – original draft. HT: Data curation, Supervision, Writing – original draft. MA: Data curation, Writing – original draft. MS: Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research and/or publication of this article.
The authors would like to extend their profound gratitude to the College of Pharmacy at Jazan University, Saudi Arabia, and special thanks to our colleagues for their continuous encouragement.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1542974/full#supplementary-material
TAM, Technology Acceptance Model; PU, Perceived usefulness; PEOU, Perceived ease of use; ATT, Attitudinal factors; BI, Behavioral Intention; ICT, Information and communication technology: QoL, Quality of life; IRB, Institutional review board; EC, Ethical committee; SEM, Structured equation modeling.
1. Bokolo AJ. Application of telemedicine and eHealth technology for clinical services in response to COVID-19 pandemic. Health Technol. (2021) 11:359–66. doi: 10.1007/s12553-020-00516-4
2. Wijesooriya NR, Mishra V, Brand PL, Rubin BK. COVID-19 and telehealth, education, and research adaptations. Paediatr Respir Rev. (2020) 35:38–42. doi: 10.1016/j.prrv.2020.06.009
3. Valentino LA, Skinner MW, Pipe SW. The role of telemedicine in the delivery of health care in the COVID-19 pandemic. Haemophilia. (2020) 26:e230. doi: 10.1111/hae.14044
4. Gajarawala SN, Pelkowski JN. Telehealth benefits and barriers. JNP. (2021) 17:218–21. doi: 10.1016/j.nurpra.2020.09.013
5. Jang-Jaccard J, Nepal S, Celler B, Yan B. WebRTC-based video conferencing service for telehealth. Computing. (2016) 98:169–93. doi: 10.1007/s00607-014-0429-2
6. Guner H, Acarturk C. The use and acceptance of ICT by senior citizens: a comparison of technology acceptance model (TAM) for elderly and young adults. Univ Access Inf Soc. (2020) 19:311–30. doi: 10.1007/s10209-018-0642-4
7. Vegda K, Nie JX, Wang L, Tracy CS, Moineddin R, Upshur RE. Trends in health services utilization, medication use, and health conditions among older adults: a 2-year retrospective chart review in a primary care practice. BMC Health Serv Res. (2009) 9:217 doi: 10.1186/1472-6963-9-217
8. World Health Organization. Ageing and Health. Geneva: World Health Organization. (2024). Available online at: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed November 8, 2024).
9. Census S. Population by Age Group. Available online at: https://portal.saudicensus.sa/portal/public/1/17/44?type=DASHBOARD (accessed November 8, 2024).
10. Stellefson M, Chaney B, Barry AE, Chavarria E, Tennant B, Walsh-Childers K, et al. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res. (2013) 15:e35. doi: 10.2196/jmir.2439
11. Clark NM, Becker MH, Janz NK, Lorig K, Rakowski W, Anderson L. Self-management of chronic disease by older adults: a review and questions for research. J Aging Health. (1919) 3:3–27. doi: 10.1177/089826439100300101
12. Zin KS, Kim S, Kim HS, Feyissa IF. A study on technology acceptance of digital healthcare among older Korean adults using extended tam (extended technology acceptance model). Adm Sci. (2023) 13:42. doi: 10.3390/admsci13020042
13. Kaplan B, Litewka S. Ethical challenges of telemedicine and telehealth. Camb Q Healthc Ethics. (2008) 17:401–16. doi: 10.1017/S0963180108080535
14. Haimi M, Sergienko R. Adoption and use of telemedicine and digital health services among older adults in light of the COVID-19 pandemic: repeated cross-sectional analysis. JMIR Aging. (2024) 7:e52317. doi: 10.2196/52317
15. Riva G. From telehealth to e-health: internet and distributed virtual reality in health care. Cyberpsychol Behav. (2000) 3:989–98. doi: 10.1089/109493100452255
16. Coughlin JF, D'Ambrosio LA, Reimer B, Pratt MR. Older adult perceptions of smart home technologies: implications for research, policy & market innovations in healthcare. In: 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. Lyon: IEEE. (2007). p. 1810–1815.
17. Vegesna A, Tran M, Angelaccio M, Arcona S. Remote patient monitoring via non-invasive digital technologies: a systematic review. Telemed e-Health. (2017) 23:3–17. doi: 10.1089/tmj.2016.0051
18. Bowles KH, Baugh AC. Applying research evidence to optimize telehomecare. J Cardiovasc Nurs. (2007) 22:5–15. doi: 10.1097/00005082-200701000-00002
19. Zaman SB, Khan RK, Evans RG, Thrift AG, Maddison R, Islam SM. Exploring barriers to and enablers of the adoption of information and communication technology for the care of older adults with chronic diseases: scoping review. JMIR Aging. (2022) 5:e25251. doi: 10.2196/25251
20. Demiris G, Thompson H, Boquet J, Le T, Chaudhuri S, Chung J. Older adults' acceptance of a community-based telehealth wellness system. Inform Health Soc Care. (2012) 38:27–36. doi: 10.3109/17538157.2011.647938
21. Doukas C, Maglogiannis I. Bringing IoT and cloud computing towards pervasive healthcare. In: 2012 Sixth International Conference on Innovative Mobile and Internet Services in Ubiquitous Computing. Palermo: IEEE. (2012). p. 922–926.
22. Cerchione R, Centobelli P, Riccio E, Abbate S, Oropallo E. Blockchain's coming to hospital to digitalize healthcare services: designing a distributed electronic health record ecosystem. Technovation. (2023) 120:102480. doi: 10.1016/j.technovation.2022.102480
23. Jeddi Z, Bohr A. Remote patient monitoring using artificial intelligence. In: Artificial Intelligence in Healthcare. Cambridge, MA: Academic Press. (2020). p. 203–234.
24. Asadzadeh A, Kalankesh LR. A scope of mobile health solutions in COVID-19 pandemics. Inform Med Unlock. (2021) 23:100558. doi: 10.1016/j.imu.2021.100558
25. Istepanian RS. Mobile health (m-Health) in retrospect: the known unknowns. Int J Environ Res Public Health. (2022) 19:3747. doi: 10.3390/ijerph19073747
26. Sivathanu B. Adoption of internet of things (IOT) based wearables for healthcare of older adults–a behavioural reasoning theory (BRT) approach. J Enabling Technol. (2018) 12:169–85. doi: 10.1108/JET-12-2017-0048
27. Chan ZY, Lim CF, Leow JL, Chium FY, Lim SW, Tong CH, et al. Using the technology acceptance model to examine acceptance of telemedicine by cancer patients in an ambulatory care setting. In: Proceedings of Singapore Healthcare. (2022). p. 31.
28. Holtz B, Mitchell K, Hirko K, Ford S. Using the technology acceptance model to characterize barriers and opportunities of telemedicine in rural populations: survey and interview study. JMIR Form Res. (2022) 6:e35130. doi: 10.2196/35130
29. Venkatesh V, Davis FD. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Manage Sci. (2000) 46:186–204. doi: 10.1287/mnsc.46.2.186.11926
30. Venkatesh V, Thong JY, Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Quart. (2012) 1:157–78. doi: 10.2307/41410412
31. Ahmad A, Rasul T, Yousaf A, Zaman U. Understanding factors influencing elderly diabetic patients' continuance intention to use digital health wearables: extending the technology acceptance model (TAM). J Open Innovat. (2020) 6:81. doi: 10.3390/joitmc6030081
32. Chakraborty M, Al Rashdi S., Venkatesh, et al. 's unified theory of acceptance and use of technology (UTAUT). In: Technology adoption and social issues: Concepts, Methodologies, Tools, and Applications. Pennsylvania: IGI Global. (2018). p. 1657–1674.
33. Liu D, Li Q, Han S. Using extended technology acceptance model to assess the adopt intention of a proposed IoT-based health management tool. Sensors. (2022) 22:6092. doi: 10.3390/s22166092
34. Ajzen I. Belief, Attitude, Intention and Behaviour: An Introduction to Theory and Research. Boston: Addison-Wesley. (2015).
35. Dziuban CD, Shirkey EC. When is a correlation matrix appropriate for factor analysis? Some decision rules. Psychol Bull. (1974) 81:358361. doi: 10.1037/h0036316
36. VelicerWF. Determining the number of components from the matrix of partial correlations. Psychometrika. (1976) 41:321–327. doi: 10.1007/BF02293557
37. Rahimi B, Nadri H, Afshar HL, Timpka T. A systematic review of the technology acceptance model in health informatics. Appl Clini Inform. (2018) 9:604–34. doi: 10.1055/s-0038-1668091
38. Almazroi AA, Mohammed F, Al-Kumaim NH, Hoque MR. An empirical study of factors influencing e-health services adoption among public in Saudi Arabia. J Health Inform. (2022) 28:2316. doi: 10.1177/14604582221102316
39. Tsai J-M, Cheng M-J, Tsai H-H, Hung S-W, Chen Y-L. Acceptance and resistance of telehealth: the perspective of dual-factor concepts in technology adoption. Int J Inform Managem. 49:34–44. doi: 10.1016/j.ijinfomgt.2019.03.003
40. Su Y-Y, Huang S-T, Chen C-M, Wu Y-H. Factors affecting patients' acceptance of and satisfaction with cloud-based telehealth for chronic disease management: a case study in the workplace. Appl Clini Inform. (2020) 11:286–94. doi: 10.1055/s-0040-1708838
41. Cimperman M, Makovec Brenčič M, Trkman P. Analyzing older users' home telehealth services acceptance behavior—applying an Extended UTAUT model. Int J Med Inform. (2016) 90:22–31. doi: 10.1016/j.ijmedinf.2016.03.002
42. Woo K, Dowding DW. Decision-making factors associated with telehealth adoption by patients with heart failure at home: a qualitative study. Comp Inform Nurs. (2020) 38:204–14. doi: 10.1097/CIN.0000000000000589
43. Wang H, Liu J, Yu L, Tsui K-L, Zwetsloot IM, Zhao Y, et al. Personalized health monitoring system for community-dwelling elderly people in Hong Kong: design, implementation, and evaluation study. J Med Internet Res. (2020) 22:e19223. doi: 10.2196/19223
44. Kohnke A, Cole ML, Bush R. Incorporating UTAUT predictors for understanding home care patients' and clinician's acceptance of healthcare telemedicine equipment. J Technol Managem Innovat. (2014) 9:29–41. doi: 10.4067/S0718-27242014000200003
45. Li W, Guo J, Liu W, Tu J, Tang Q. Effect of older adults willingness on telemedicine usage: an integrated approach based on technology acceptance and decomposed theory of planned behavior model. BMC Geriat. (2024) 24:1. doi: 10.1186/s12877-024-05361-y
46. Diño MJS, De Guzman AB. Using partial least squares (PLS) in predicting behavioral intention for telehealth use among filipino elderly. Educ Gerontol. (2014) 41:53–68. doi: 10.1080/03601277.2014.917236
47. Li X, Zhou Y, Liu Y, Wang X, Yuen KF. Psychological antecedents of telehealth acceptance: A technology readiness perspective. Int J Disast Risk Reduct. (2023) 91:103688. doi: 10.1016/j.ijdrr.2023.103688
48. Tsai C-H. Integrating social capital theory, social cognitive theory, and the technology acceptance model to explore a behavioral model of telehealth systems. Int J Environm Res Public Health. (2014) 11:4905–25. doi: 10.3390/ijerph110504905
49. National Platform GOV.SA. Digital Inclusion. (2024). Available online at: https://www.my.gov.sa/wps/portal/snp/careaboutyou/digitalinclusion/?lang=en (accessed November 8, 2024).
50. Mahfouz MS, Rahim BE, Solan YM, Makeen AM, Alsanosy RM. Khat chewing habits in the population of the Jazan region, Saudi Arabia: prevalence and associated factors. PLoS ONE. (2015) 10:e0134545. doi: 10.1371/journal.pone.0134545
51. Chismar WG, Wiley-Patton S. Does the Extended Technology Acceptance Model Apply to Physicians. Piscataway, NJ: Institute of Electrical Electronics Engineers. (2003).
Keywords: telehealth, technology acceptance model, perceived ease of use, older adults, chronic conditions
Citation: Meraya AM, Khardali A, Ahmad S, Hoshaibari AZ, Alameer AA, Jaafari RY, Thaibah HA, Alfarhan M and Syed MH (2025) Telehealth perceptions and associated factors among older adults with chronic conditions in Saudi Arabia: a comparative study of users and non-users. Front. Public Health 13:1542974. doi: 10.3389/fpubh.2025.1542974
Received: 10 December 2024; Accepted: 24 February 2025;
Published: 12 March 2025.
Edited by:
Hasheem Mannan, University College Dublin, IrelandReviewed by:
Joanne McVeigh, Maynooth University, IrelandCopyright © 2025 Meraya, Khardali, Ahmad, Hoshaibari, Alameer, Jaafari, Thaibah, Alfarhan and Syed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdulkarim M. Meraya, YW1lcmF5YUBqYXphbnUuZWR1LnNh
†ORCID: Hilal A. Thaibah orcid.org/0000-0002-0793-5445
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.