- 1School of Physical Education and Sport, Central China Normal University, Wuhan, China
- 2School of Wushu, Wuhan Sports University, Wuhan, China
- 3School of Electronic Engineering, Xi'an University of Posts and Telecommunications, Xian, China
Purpose: Baduanjin represents an affordable and secure method of exercising both the mind and body, and has been observed to enhance balance in older adults. Nevertheless, the existing research on the impact of Baduanjin on various balance functions is still insufficient, and the optimal dosage parameters for performing Baduanjin exercises have not been studied.
Methods: To conduct a systematic review and meta-analysis, five English databases and three Chinese databases were performed. Relevant studies were searched by GOOGLE SCHOLAR, Web of Science, Cochrane, Embase, Pubmed, CNKI, SinoMed, and WangfangMed using “Baduanjin” and “balance.” Subgroup analyses were conducted to investigate the influence of different exercise parameters on the observed outcomes. Meta-regression was employed to identify potential moderating factors. The Physical Therapy Evidence Database (PEDro) scale was used for quality assessment.
Results: A total of 40 studies were included in the analysis, while the majority of studies report promising outcomes, the overall quality of these studies is relatively low. The results of the meta-analysis showed Baduanjin significantly enhanced static balance (SMD = 0.87, 95%CI: 0.69–1.05), dynamic balance (SMD = 0.85, 95%CI: 0.50–1.19), proactive balance (SMD = −1.00, 95%CI: −1.33–−0.67) and balance test battery (SMD = 1.04, 95%CI: 0.81–1.28) in older adults. Additionally, the findings indicated a notable reduction in the risk of falls (SMD = −2.19, 95%CI: −3.35–−1.04) and an improvement in fall efficacy (SMD: 0.57, 95%CI: 0.36–0.78).
Conclusion: Baduanjin has been demonstrated to improve balance and reduce the risk of falls in older adults. Studies have found that significant gains begin to be achieved with a minimum of 12 weeks of practice and that 30–49 min of practice, 5–7 times per week, works best for developing different balances. However, most of the included studies were limited by a lack of blinding and follow-up visits, and there was an insufficient number of short-term or long-term studies to establish complete optimal parameters robustly.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=548345, identifier: CRD42024548345.
1 Introduction
Falls represent a significant health concern for middle-aged and older adults, leading to fractures, bruises, and other injuries, and in severe cases, even death (1, 2). According to the World Health Organization (WHO), approximately 684,000 deaths globally are attributed to falls each year, with the majority occurring in individuals over 60 (3). Falls have become the second leading cause of accidental death globally, with the likelihood of experiencing a fall and subsequent hospitalization increasing with age (4). Annually, there are 37.3 million serious falls requiring medical attention, with older adults comprising the largest demographic among fall victims (3). Balance disorders are recognized as key internal factors contributing to falls in older adults (5). Those with poor balance are at a higher risk of future falls (6), and balance tests are often employed to predict fall occurrences (7). Balance training has emerged as an effective strategy for fall prevention, with both traditional exercises and advanced technologies like virtual reality offering diverse options for middle-aged and older adults (8). Incorporating physical activity modalities that enhance balance—like core strength training or Pilates—has proven effective in improving balance and reducing fall risk (9).
In the 5,000-year history of the Chinese nation, a diverse array of traditional physical activities has emerged, with as many as 977 documented forms (10). Among these, substantial evidence has highlighted the health benefits of practices such as Tai Chi, Qigong, and Yangko dance, particularly for older adults (11). These benefits include reduced risk of influenza (12), improved quality of life for cancer patients (13), and enhanced quality of life for individuals with essential hypertension (14). Tai Chi, recognized as a renowned method for improving balance, has been extensively studied since the early 2000s (15, 16), and encouraging evidence supports its recommendation by the Centers for Disease Control and Prevention (CDC) as a fall prevention intervention for the older adults (16, 17).
Similar to the movement form of Taijiquan, Fitness Qigong, despite having different connotations, has also attracted the attention of colleagues, who discuss its benefits for older adults balance, includes Wuqinxi, Liuzijue, Mawangdui Daoyin, etc. (18). Baduanjin is one of the most renowned forms of Qigong, It comprises eight movements that emphasize weight shifting, muscle stretching, breathing exercises, and meditative training. Characterized by its simplicity and ease of learning, Baduanjin (BDJ) is highly implementable and remarkably safe, rendering it exceedingly popular among the older population.
Recent reviews indicate that BDJ can significantly improve balance and prevent falls in individuals over 65 years old (19). Additionally, it is recognized as an effective rehabilitation modality for enhancing balance and quality of life in stroke and Parkinson's patients (20, 21). BDJ also promotes lower extremity strength, flexibility, and overall balance in older adults (22, 23). Notably, BDJ boasts a strong safety profile with a low likelihood of serious adverse events (24), making it a favorable choice for older adults, particularly those in a weakened state.
While numerous randomized controlled trials have highlighted the positive effects of BDJ on balance in older adults, there is limited evidence addressing its impact on balance specifically broad evidence synthesis. Furthermore, no studies have identified the optimal dosage of BDJ for balance improvement. Therefore, to promote the scientific practice of Baduanjin (BDJ) exercise among older adults and to inform nursing practices aimed at improving balance in this population, this study seeks to address the following questions: (1) To supplement existing evidence regarding balance enhancement and fall prevention in older adults through BDJ; (2) To analyze the moderators influencing the relationship between BDJ and balance; (3) To explore the dose-response relationship between BDJ and balance.
2 Methods
This study was planned following the Preferred reporting items for systematic review and meta-analysis (PRISMA) (25), and was registered in the center of the International Prospective Systematic Evaluation Registry database (PEOSPERO) (registration number: CRD42024548345). The specific research process developed was guided by the JBI Manual for Evidence Synthesis (26).
2.1 Eligibility criteria
The study included older adults participating in BDJ exercise without strict limitations regarding race, gender, or health status. For the definition of “older adults,” we referred to other studies, considering mean aged 60 years or older (27), with no stringent health status criteria. However, we excluded individuals with disability or special situation (such as visual impairments, vestibular injuries, etc.). In terms of intervention modalities, we included studies that specifically utilized BDJ as an intervention. Studies incorporating sit-to-stand BDJ, mixed intervention programs, or failing to highlight the independent benefits of BDJ were excluded.
There were no strict restrictions on the control group, which included various interventions such as rehabilitation, routine care, health education, and walking. However, controls with strong functional directionality, such as other forms of Qigong, resistance training, and balance training, were excluded. The primary indicators included balance-related outcomes, categorized into five areas: (I) Static Balance (e.g., Eye Closed One Leg Standing Balance, One Leg Stand Test); (II) Dynamic Balance (e.g., Five Times Sit to Stand Test, Six-Minute Walk Test); (III) Proactive Balance; (IV) Passive Balance; and (V) Balance Test Batteries (including comprehensive tests like the Berg Balance Scale). Secondary indicators included fall rates, the number of falls, assessment results (e.g., Morse Fall Assessment Scale), and safety. Only controlled trials published in English or Chinese were included in this study. The original authors were to be contacted via email for any incorrect or incomplete data; if no response was received before data analysis commenced, the study was excluded. There were no restrictions regarding randomization, allocation concealment, blinding methods, or publication date.
2.2 Information sources
To ensure a comprehensive search, we utilized the portfolio of English databases outlined in the study by Bramer et al. (28), which included, at a minimum, Embase, MEDLINE (PubMed), Web of Science, and Google Scholar (top 200 items). Additionally, we supplemented our search with the Cochrane Library (Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials). For Chinese databases, we included the China Knowledge Network, Chinese Biomedical Literature Database, and Wanfang Database. The search will remain open until May 1, 2024. To maximize the retrieval of all relevant studies, we will also review the reference lists of included studies and related systematic reviews once the initial search is complete.
2.3 Search strategy
The search terms are based on the PICO principle, and in the English databases, they include (“Old” OR “Aged” OR “older” OR “Senior”) AND (“Baduanjin” OR “Qigong” OR “Eight Section Brocades” OR “Traditional Chinese Exercise”) AND (“Balance” OR “Postural Balance” OR “Postural Stability” OR “Falling” etc.), and the search keywords in the Chinese database are slightly modified based on the English terms. The complete search strategies for different databases are provided in Appendix A.
2.4 Data selection and collection process
Once the two reviewers complete the search, the data will be imported into EndNote X9.1, with any data that cannot be imported automatically added manually. Following data collection, an automatic check for duplicates will be conducted, accompanied by a manual review. A third researcher will then review the results of this process. All data will be merged into a single dataset, with duplicate studies removed. Two independent reviewers will screen eligible articles based on pre-established criteria after reviewing the title, abstract, and full text, consulting a third reviewer in case of disagreements. Data extraction will be performed using standardized forms to capture basic information such as the title, first author, year of publication, study design, sample size, baseline characteristics, control groups, exit rate, follow-up details, outcomes, adverse events, and dosage information (duration, training frequency, intensity). In cases of data inconsistencies, a third reviewer will mediate until a unanimous agreement is reached. Any data errors will be reported to a third reviewer, who will organize an error check and exclude any literature with confirmed errors. For ambiguous or missing data, the third reviewer will contact the corresponding author via email for clarification, and if there is no response within 2 weeks, the study will be excluded.
2.5 Methodological quality assessment
This review utilized the PEDro scale to assess the methodological quality of primary studies (29). Two independent reviewers conducted the assessment, with a third reviewer facilitating discussions when disagreements arose. The PEDro scale comprises 11 items designed to evaluate the quality of studies in the Physical Therapy Evidence Database (PEDro), including one item for external validity, eight for internal validity, and two for statistical reporting. Researchers determined the quality of each study by summing the total scores, with interpretations as follows: scores <4 are considered “poor,” 4 to 5 are “fair,” 6 to 8 are “good,” and 9 to 10 are “excellent.” This approach has demonstrated reliability (30, 31).
2.6 Statistical analysis
This systematic review and meta-analysis employed a null hypothesis significance test by reporting Q. The degree of heterogeneity among the effect sizes of the studies was assessed using I2 and the heterogeneity statistic (H statistic). If a random effects model was utilized, an additional measure of absolute heterogeneity, τ2 (Tau squared), was reported. The I2 thresholds for relative heterogeneity were defined as follows: low (25%), moderate (50%), and high (75%) (32).
Considering the possible differences in magnitude of the different measures, this study combined the balance-related indicators by standardized mean deviation (SMD), collecting the sample sizes of the experimental and control groups, and the mean and the standard deviation for the calculation of the effect sizes. SMD was calculated for each study by SMD = (Mean1 − Mean2)/SDpooled, where the combined standard deviation was calculated using SDpooled = sqrt((n1 *SD12 + n2 * SD22)/(n1 + n2)). After calculating the weights for each study, SMDcombined = Σ(wi * SMDi)/Σwi was used for merging.
More conservative estimates will be made using a random effects model when heterogeneity is detected, and 95% confidence intervals for the combined effect sizes will be calculated. In contrast, a fixed effects model will be employed when heterogeneity is not present. All combined results are reported via forest plots. For studies where data merging was not feasible, narrative analysis was conducted after coding the data to engage in adding to the evidence. There may have been selective reporting of data in the included trials, with positive data being more likely to be published compared to negative data (33). If sufficient studies were available, publication bias was observed through funnel plots and the symmetry of the funnel plots was tested by Egger's test and Begg's test (34, 35).
This review used meta-regression to detect potential effects of level covariates on effect sizes. Covariates included exercise dose, control group, health status, and age. For those with significant heterogeneity, subgroup analyses were performed. Quantitative analyses were performed through the automated data analysis platform SPSSAU (version 24.0) (36), Revman 5.3 and SPSS 28.0.
3 Results
3.1 Literature search results
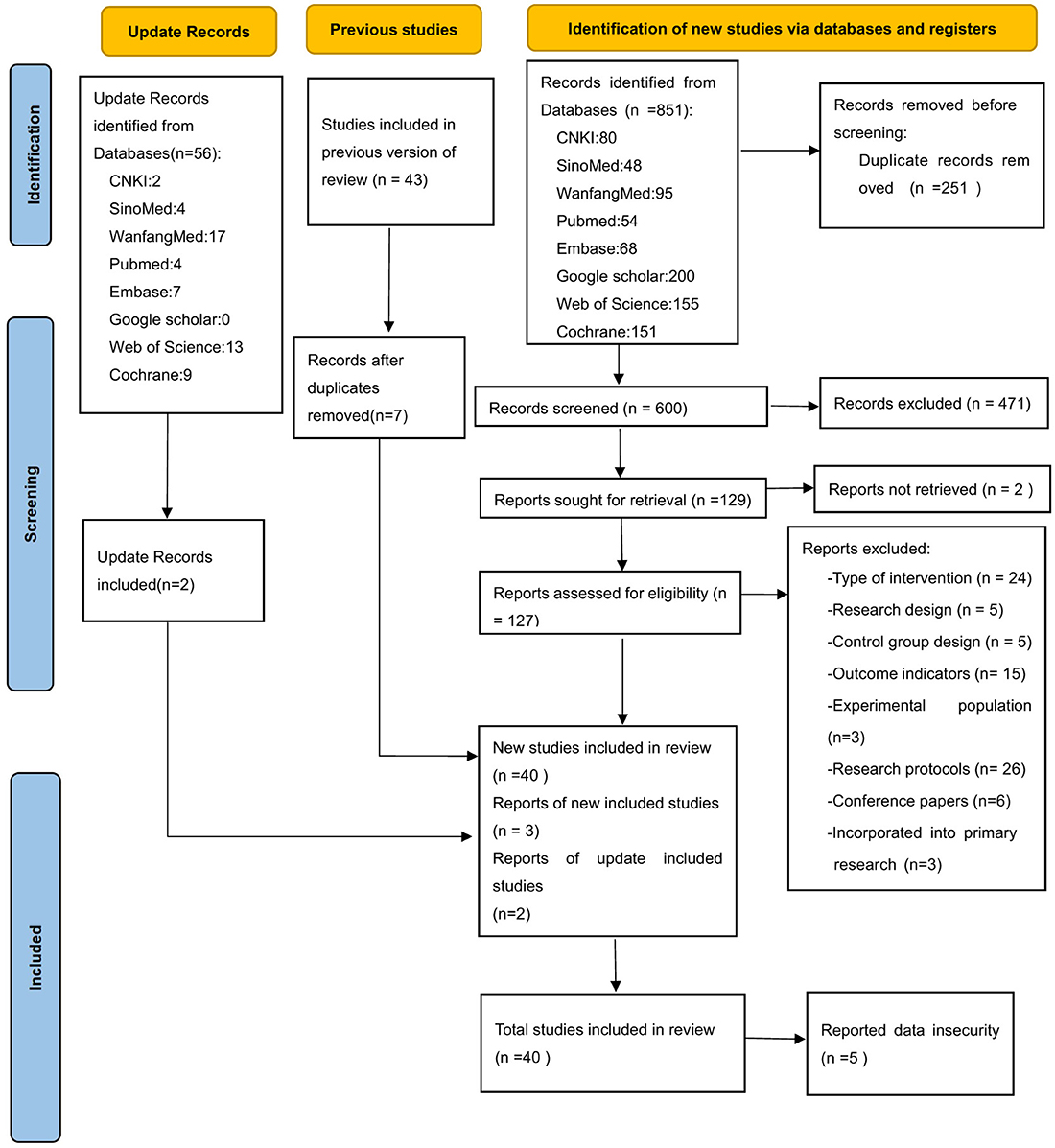
Figure 1 illustrates the process of literature inclusion, and total of 851 records were retrieved from 8 distinct databases. After two rounds of deduplication, 600 records remained. Upon reviewing the abstracts and titles, we incorporated 127 studies into our analysis. However, following a thorough examination of the complete articles, we excluded 87 studies. The primary reasons for exclusion were mismatched intervention methods, absence of relevant outcome indicators, research protocols, and conference proceedings. Additionally, three studies were incorporated by reviewing previous versions of the systematic review. During the data extraction phase, data security concerns were identified in five studies from the same institutions, reducing the final sample to 38 studies (37–74). The search was updated on January 22, 2025, resulting in 55 revised records. Following the screening process, 2 additional studies were included (75, 76). In the aggregate, a total of 40 studies were incorporated into the analysis in two successive phases.
3.2 Study characteristics
A detailed summary of the characteristics of these studies is provided in Appendix B. The mean age of participants ranged from 60 to 75 years across 35 studies (37, 39, 43–57, 59–64, 66–76), and from 75 to 85 years in 5 studies (40–42, 58, 65). The dataset comprised 30 journal articles (37, 38, 41, 43, 45, 46, 48, 50–54, 57, 59–75) and 10 theses (39, 40, 42, 44, 47, 49, 55, 56, 58, 76), with two studies were conducted in Spain (67) and Singapore (75), and the remainder in China. Participants were categorized by health status as either generally healthy or incompletely healthy. “Generally healthy” was defined as the absence of mobility or psychological disorders, normal cognitive function, basic balance ability, and no serious acute illnesses or diseases affecting balance. Of the total, 16 studies (37–39, 42, 46, 47, 49, 52, 55–57, 62, 67–69, 76) involved generally healthy participants, 23 studies (40, 41, 43, 44, 48, 50, 51, 53, 54, 58–61, 63–66, 70–75) included incompletely healthy participants, and one study (45) did not report the health status of participants.
In alignment with the definitions of balance ability indicators outlined in previous studies (77, 78), the outcome measures in this review encompass static balance indicators (SBT, including the single-leg standing test and related kinematic measures), dynamic balance indicators (DBT, including the 6-min walk test), proactive balance indicators (PBT, including the timed up and go test), the balance test batteries (BTB, including the mountain balance test), and passive balance. Among the studies included in the review, 22 reported on SBT (37–40, 42, 45, 49, 50, 52, 54–56, 62, 64, 67–72, 74), 16 on DBT (37–40, 45, 48–50, 53, 58, 63, 65, 66, 72, 75, 76), 20 on PBT (38, 40, 42, 43, 45, 49, 50, 52–54, 56, 58, 59, 64, 68–70, 72, 75, 76), and 21 on BTB (38, 39, 41, 43, 44, 51, 52, 54–56, 58–61, 64, 66, 68–70, 73, 76). Additionally, 14 studies included fall-related indicators (40, 43, 46, 47, 49, 50, 54, 57, 59, 64, 66, 68, 72, 75).
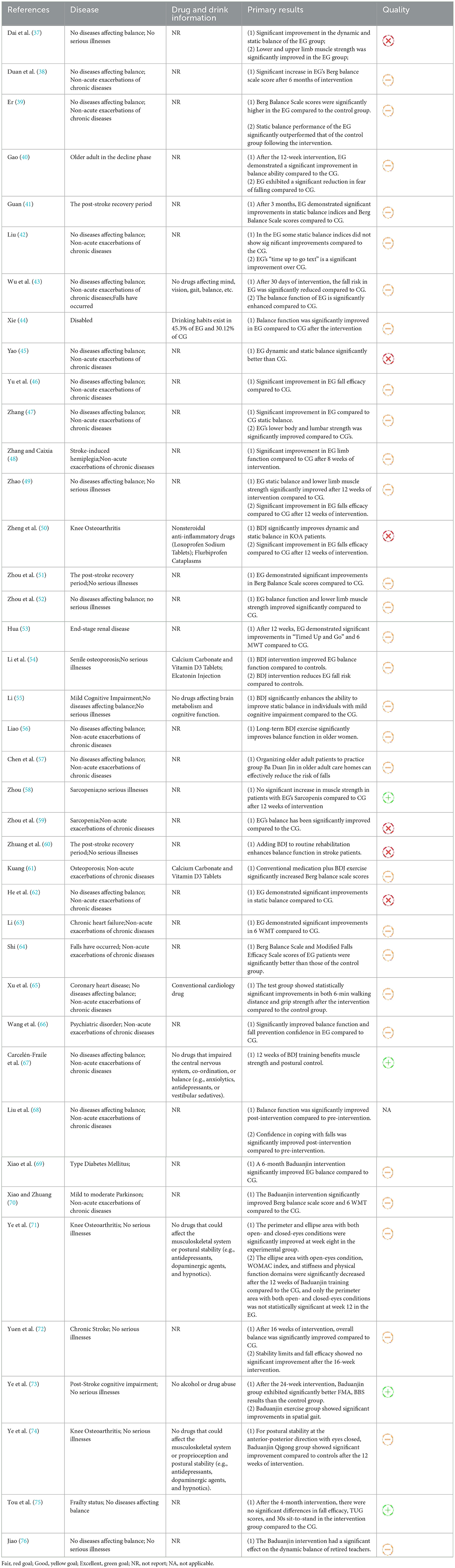
Table 1 summarizes the primary outcomes, participant characteristics, and information on drug and alcohol consumption of the included studies. While the majority of studies reported positive outcomes, the high-quality study by Tou et al. (75) found no significant differences in balance measures or fall efficacy between the intervention and control groups following a 4-month intervention. Discrepancies in findings have also emerged regarding static balance assessments utilizing force plates or plantar pressure sensors, with some studies reporting less favorable outcomes. Nevertheless, the majority of studies demonstrated significant improvements in test items such as the Timed Up and Go (TUG) test, 6-Min Walk Test (6WMT), and Five Times Sit to Stand Test (FTSST), etc. The primary results included in the study are (1) Balance test batteries, (2) Proactive balancing, (3) Steady-state balancing (dynamic/static), and (4) Fall efficiency and risk.
3.3 Methodological quality of included studies
A quasi-experimental study was excluded from the quality assessment (68). The remaining 39 studies underwent quality evaluation, with 6 rated as fair (37, 45, 50, 59, 60, 62), 29 as good (38–44, 46–49, 51–57, 61, 63–66, 69–72, 74, 76), and 4 classified as excellent (58, 67, 73, 75). Overall, the majority of the included literature was of good quality. The detailed results of the quality assessment are provided in Appendix C.
3.4 The effect of Baduanjin on balanced performance
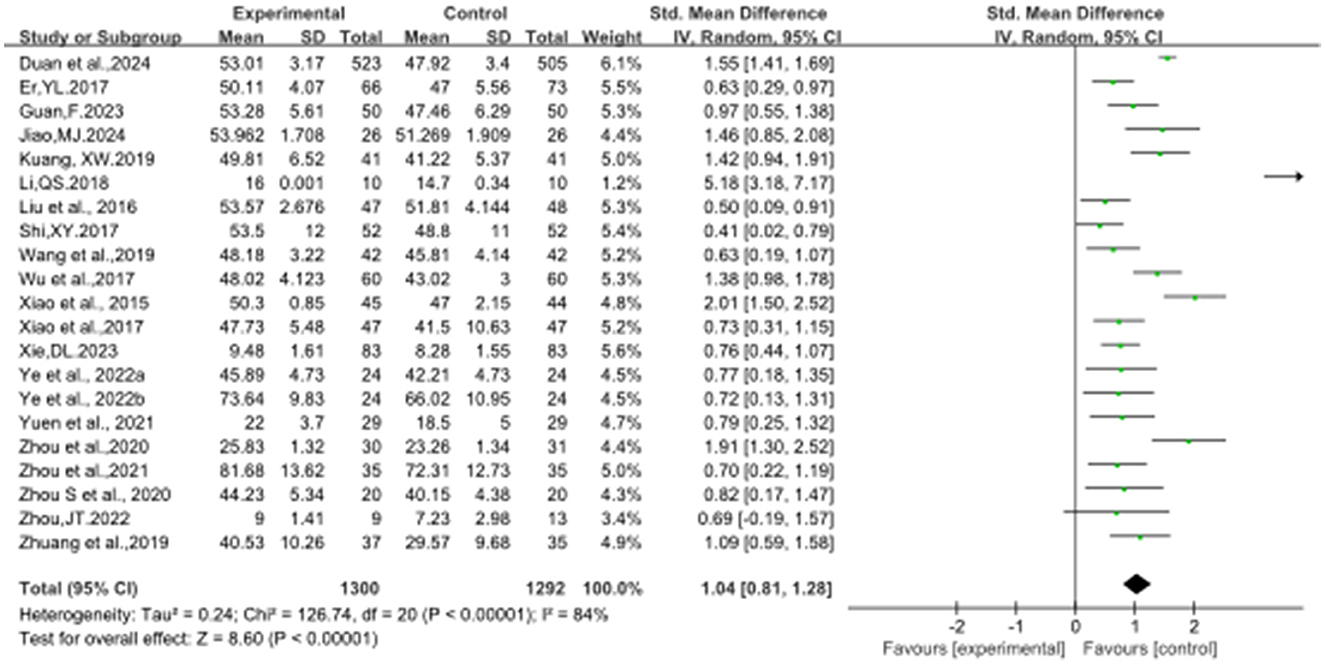
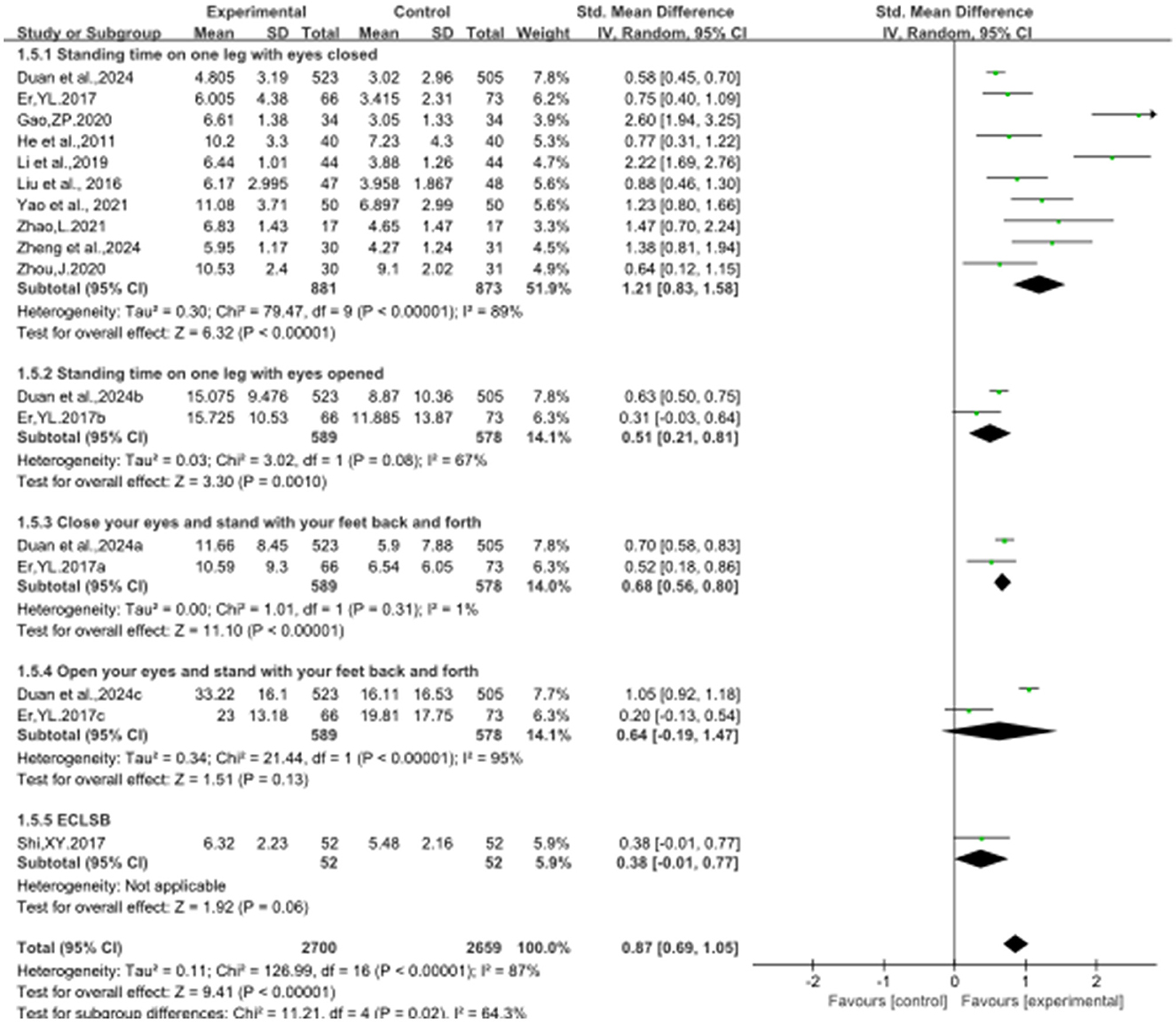
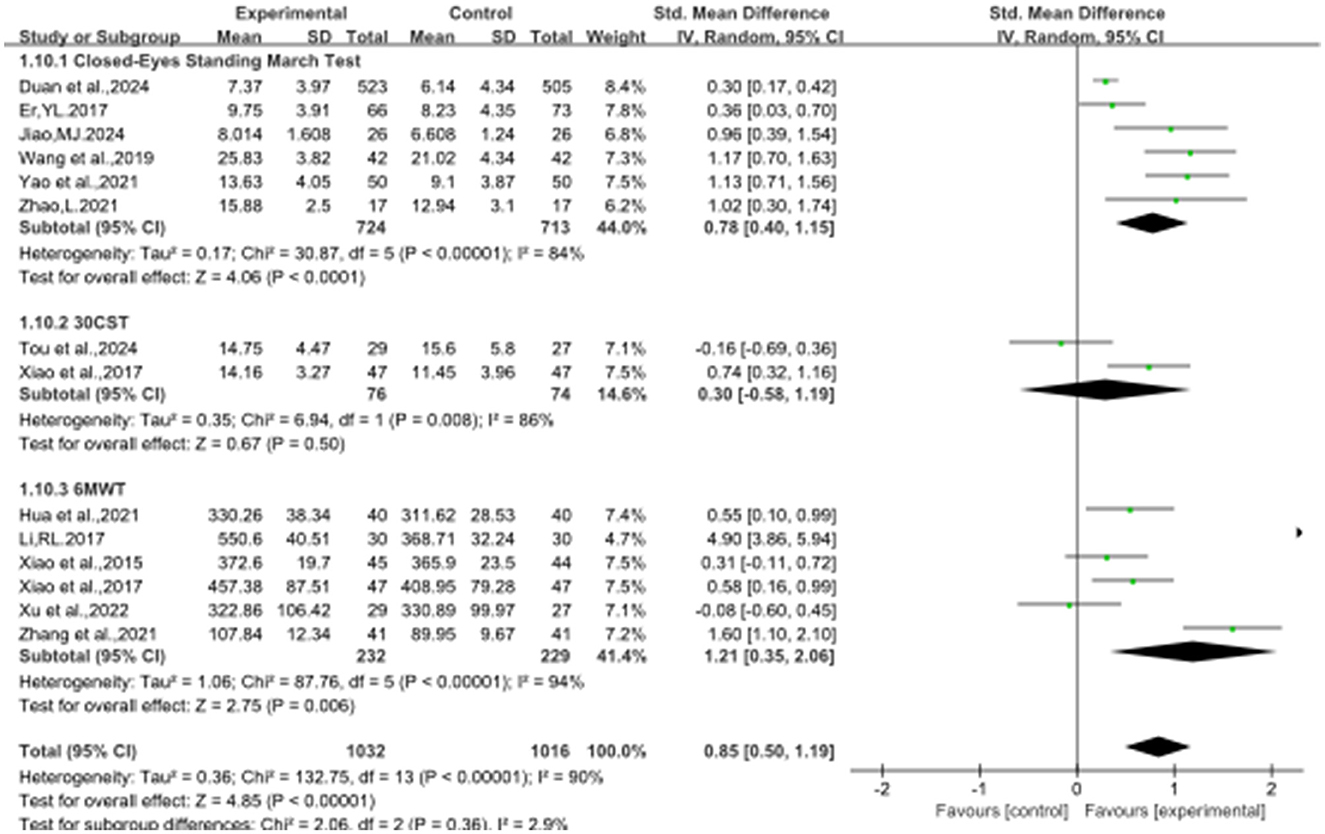
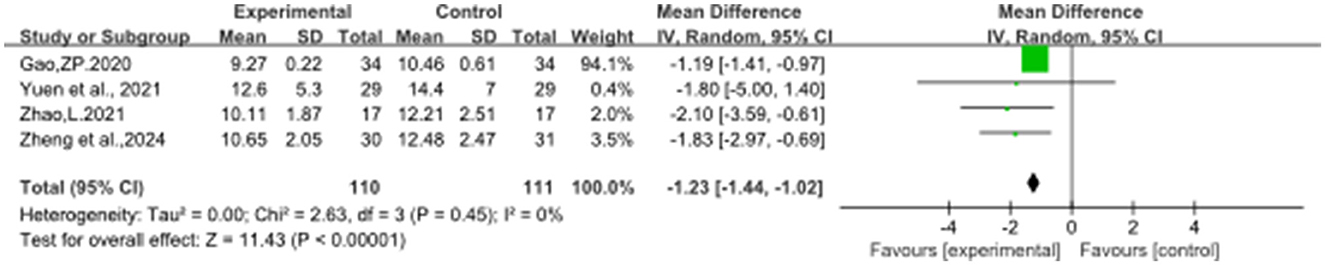
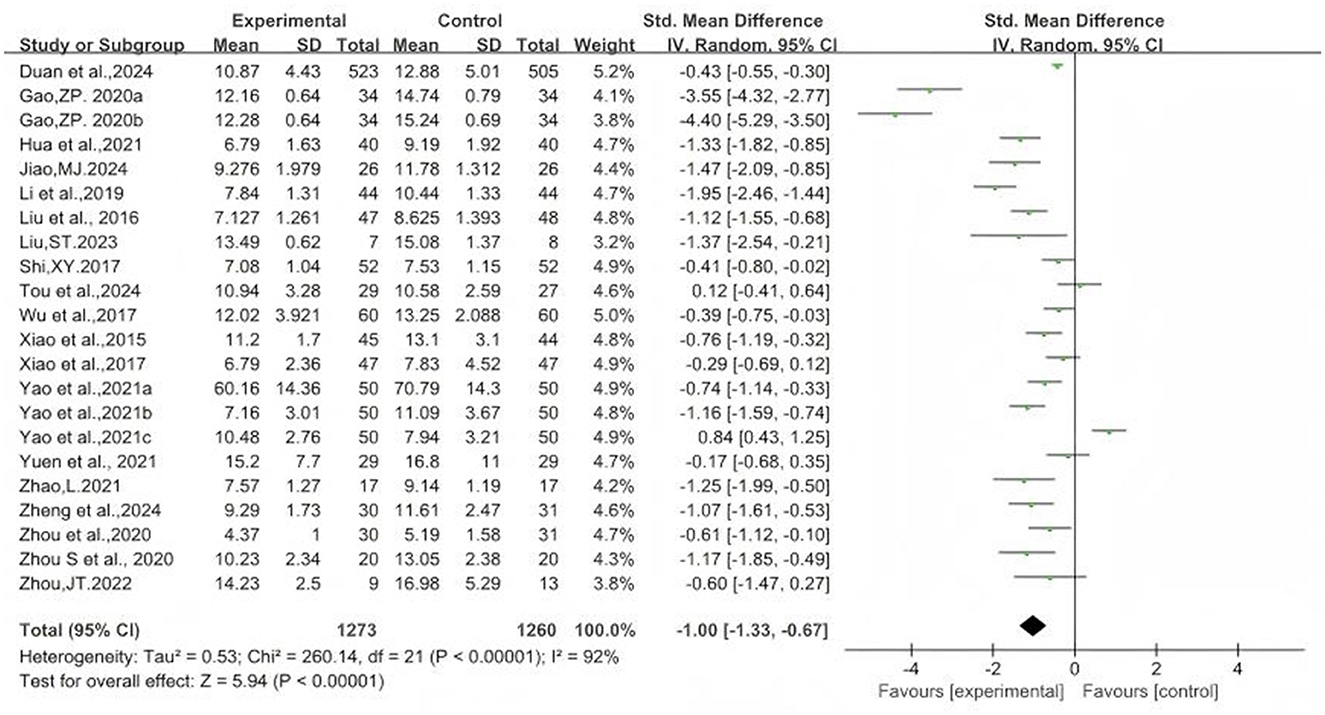
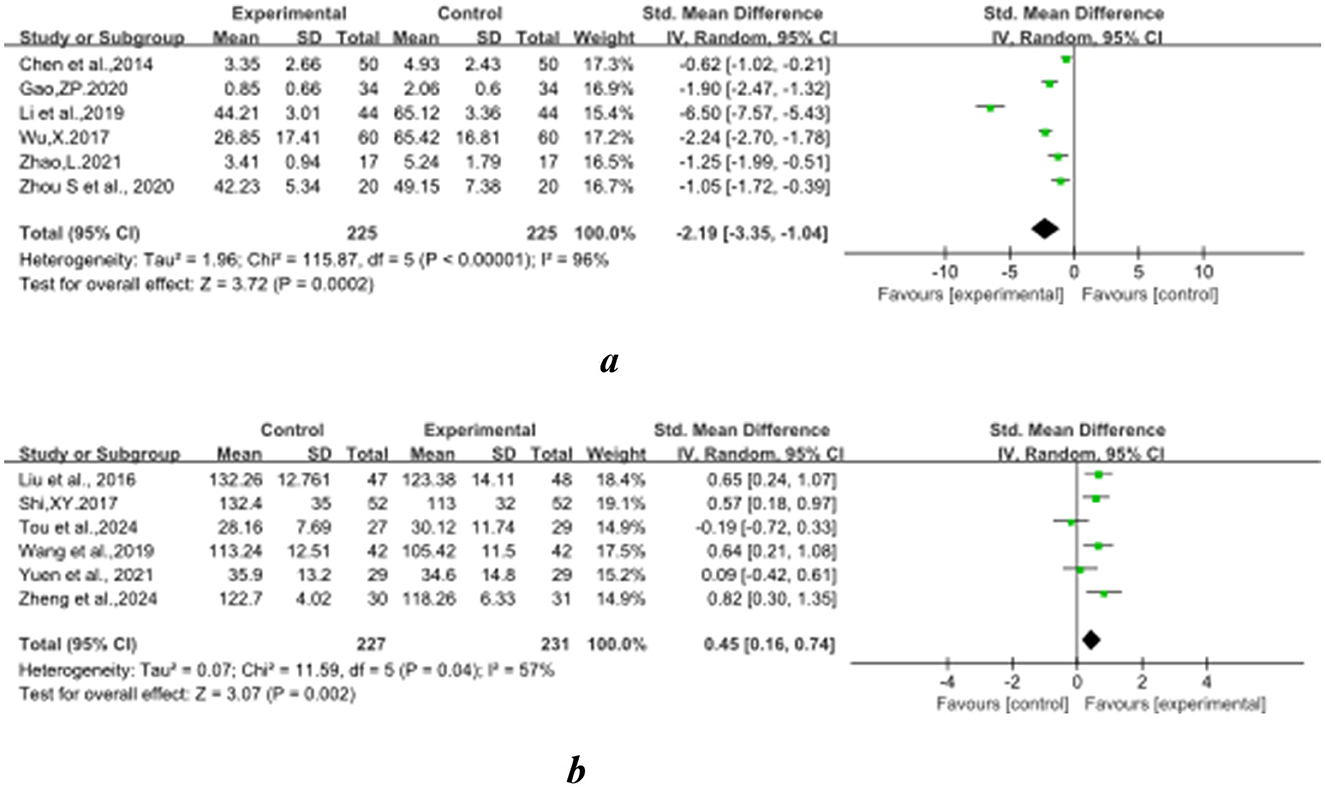
Figures 2–8 illustrate the effects of BDJ on balance performance and fall risk among older adults. The results indicated that BDJ had a significant positive effect on static balance compared to the control group (SMD = 0.87, 95% CI: 0.69–1.05, P < 0.01, df = 16), with substantial improvements in one-legged standing [eyes open (OE): SMD = 1.21, 95% CI: 0.83–1.58, P < 0.01, df = 9; eyes closed (CE): SMD = 0.51, 95% CI: 0.21–0.81, P = 0.001, df = 1] and anterior-posterior standing with CE (SMD = 0.68, 95% CI: 0.56–0.80, P < 0.01, df = 1). However, no significant improvement was observed in anterior-posterior standing with OE. The analysis of static balance parameters revealed a significant reduction in COP displacement distance (left-right: SMD = −0.99, 95% CI: −1.69–−0.28, P < 0.01, df = 7; anterior-posterior: SMD = −1.40, 95% CI:−2.41–−0.40, P < 0.01, df = 6), although COP trajectory length and COP ellipse area did not show significant changes. BDJ also significantly improved dynamic balance (SMD = 0.85, 95% CI: 0.50−1.19, P < 0.01, df = 13). Specifically, a fixed-effects model analysis of five sit-to-stand tests demonstrated a notable reduction in time (MD = −1.23, 95% CI: −1.44–−1.02, P < 0.001, df = 3). Proactive balance also showed significant improvement compared to the control group (SMD = −1.00, 95% CI: −1.33–−0.67, P < 0.001, df = 21). In addition, the study analyzed fall-related outcomes. Following the BDJ intervention, participants exhibited significant reductions in fall risk (SMD = −2.19, 95% CI: −3.35 to −1.04, P < 0.001, df = 5) and improvements in fall efficacy (SMD = 0.45, 95% CI: 0.16–0.74, P < 0.001, df = 5).
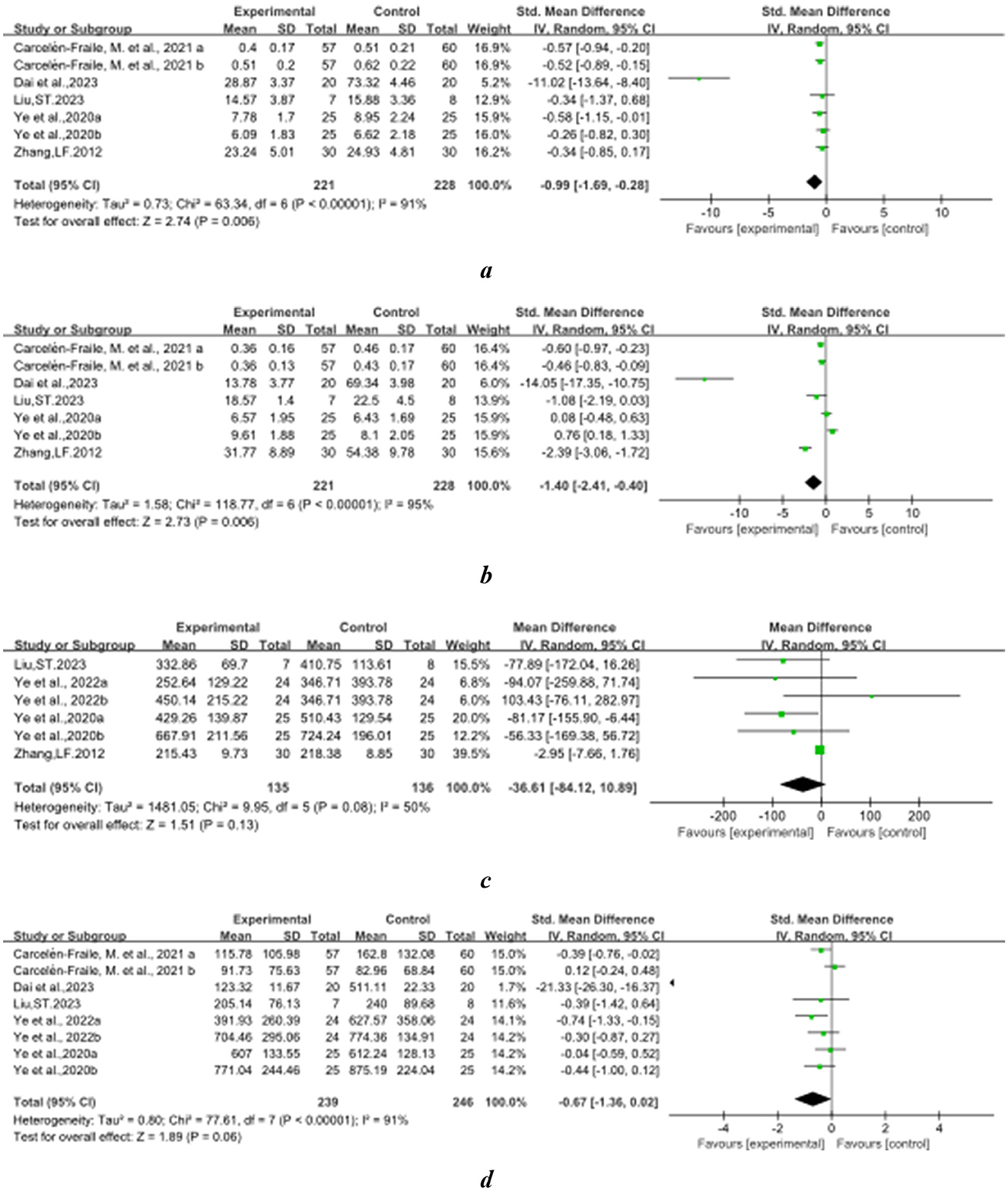
Figure 4. SBT related parameters. (A) Displacement distance in the left and right directions of the cop; (B) displacement distance in front and back direction of cop; (C) cop track length; (D) area of the cop encircling ellipse.
Furthermore, the impact of BDJ in comparison to various control groups was evaluated (Appendix D), demonstrating that BDJ exhibited a significant superiority over health education, routine care or rehabilitation, regular activities, and walking for diverse balance abilities in older. Despite the observation of no significant advantage of BDJ over routine care or rehabilitation in static balance (SMD = 0.69, 95%CI: −0.23–1.61, P = 0.14, df = 2), the overall evidence suggests that BDJ practice outside of essential activities significantly enhances balance in older adults and is more efficacious than walking.
3.5 Optimal parameters for balanced performance in Baduanjin
Subgroup analyses were conducted to examine dose-related parameters, revealing a reduction in heterogeneity to varying degrees. The relevant data metrics are provided in Appendix E. Figure 9 displays the effect sizes and 95% confidence intervals for data points demonstrating significant effects.
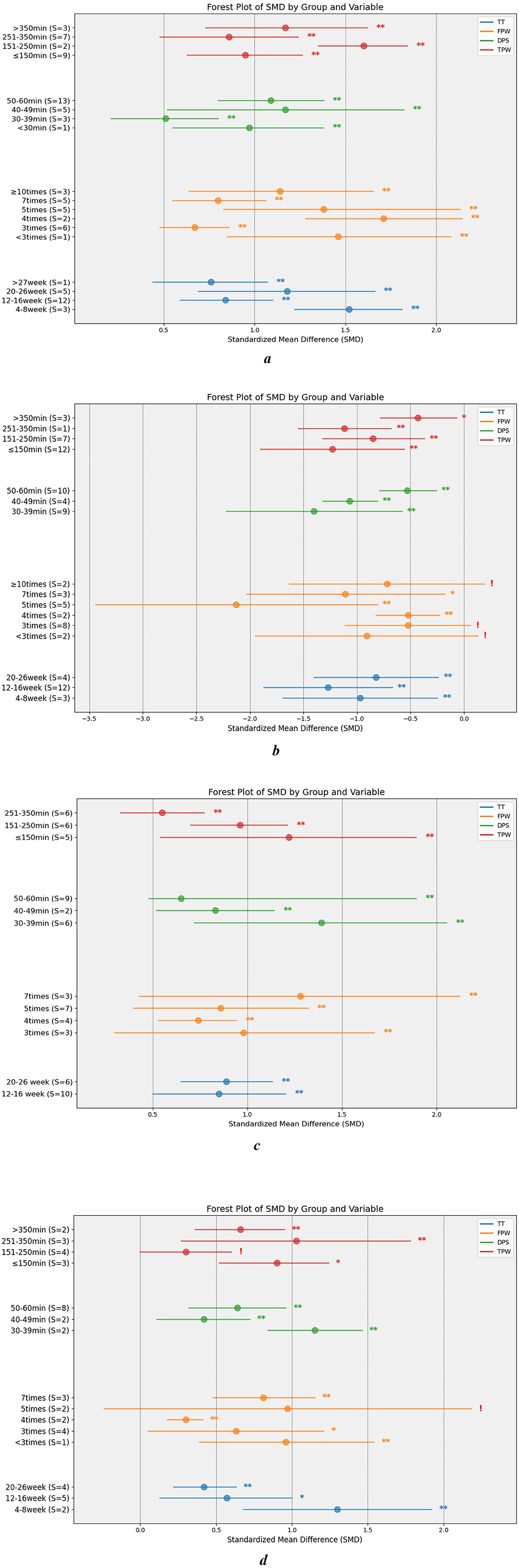
Figure 9. Dose subgroup results. BTB, static balance indicators; PBT, Proactive balancing indicators; SBT, static balance indicators; DBT, dynamic balance indicators; TT, The total number of weeks during which the subject engaged in physical exercise; FPW, The number of times per week that subjects participated in physical activity; DPS, Time duration during which subjects were engaged in physical activity; TPW, Total time spent by subjects in physical activity per week; S, sample size. **P < 0.01; *P < 0.05; !P ≥ 0.05. (A) BTB. (B) PBT. (C) SBT. (D) DBT.
3.5.1 Total training time
Subgroup analyses revealed that the optimal timeframe for DBT was 4–8 weeks (SMD = 1.30, 95%CI: 0.68–1.92, P < 0.01, df = 1), during which its effects were most pronounced. Notably, the efficacy observed at 12–16 weeks was comparable to that seen at 20–26 weeks. For SBT, training during weeks 20–26 (SMD = 0.89, 95% CI: 0.65–1.13, P < 0.001, df = 5) yielded only marginally better results than weeks 12–16 (SMD = 0.85, 95% CI: 0.50–1.20, P < 0.001, df = 9). PBT showed its highest improvement during weeks 12–16 (SMD = −1.27, 95% CI: −1.87–−0.67, P < 0.001, df = 11), with a decline in effectiveness observed by weeks 20–26. The BTB showed the greatest gains during weeks 4–8 (SMD = 1.52, 95% CI: 1.22–1.81, P < 0.001, df = 2). An upward trend in BTB effectiveness was noted from weeks 12–16 (SMD = 0.84, 95% CI: 0.59–1.10, P < 0.001, df = 12) to weeks 20–26 (SMD = 1.18, 95% CI: 0.69–1.66, P < 0.001, df = 4).
3.5.2 Training frequency
Interventions administered seven times per week (SMD = 1.28, 95% CI: 0.43–2.12, P < 0.001, df = 2) yielded the most significant improvements in SBT, while no substantial differences were observed between 3, 4, and 5 weekly sessions. For DBT, seven training sessions per week (SMD = 0.81, 95% CI: 0.48–1.15, P < 0.001, df = 2) produced the best results, with three sessions being slightly less effective. Optimal performance in PBT was achieved with 5 weekly sessions (SMD = −2.13, 95% CI: −3.44–−0.81, P < 0.01, df = 4), with effectiveness declining at seven sessions per week. BTB results were most favorable with 4 weekly sessions (SMD = 1.71, 95% CI: 1.28–2.14, P < 0.01, df = 1), although this finding was based on only two studies. The second-highest gains were observed with 5 weekly sessions (SMD = 1.38, 95% CI: 0.63–2.13, P < 0.01, df = 4).
3.5.3 Duration of training per time
The greatest improvements in SBT (SMD = 1.39, 95% CI: 0.72–2.05, P < 0.001, df = 5) and PBT (SMD = −1.40, 95% CI: −2.22–−0.58, P < 0.001, df = 8) were observed with training sessions lasting 30–39 min, with a gradual decline in effectiveness as session duration increased. For DBT, the optimal results were achieved with 50–60 min sessions (SMD = 0.64, 95% CI: 0.32−0.96, P < 0.001, df = 7), while BTB saw the highest benefits with 40–49 min sessions (SMD = 1.17, 95% CI: 0.52−1.82, P < 0.001, df = 4). Training sessions lasting 50–60 min (SMD = 1.09, 95% CI: 0.80–1.38, P < 0.001, df = 12) provided slightly lower gains in BTB compared to the 40–49 min range.
3.5.4 Training duration per week
The maximum improvements in SBT (SMD = 1.22, 95% CI: 0.54–1.89, P < 0.001, df = 4) and proactive balance (PB) performance (SMD = −1.23, 95% CI: −1.90–−0.56, P < 0.001, df = 10) were achieved with a relatively low total training time (≤150 min). In contrast, optimal performance in dynamic balance training (DBT) was observed with weekly training totals in the range of 251–350 min (SMD = 1.03, 95% CI: 0.27–1.78, P < 0.001, df = 2). For the balance test battery (BTB), the most effective training time was between 151 and 250 min (SMD = 1.60, 95% CI: 1.35–1.84, P < 0.001, df = 2), reflecting significant gains across both time periods.
3.6 Moderator analysis
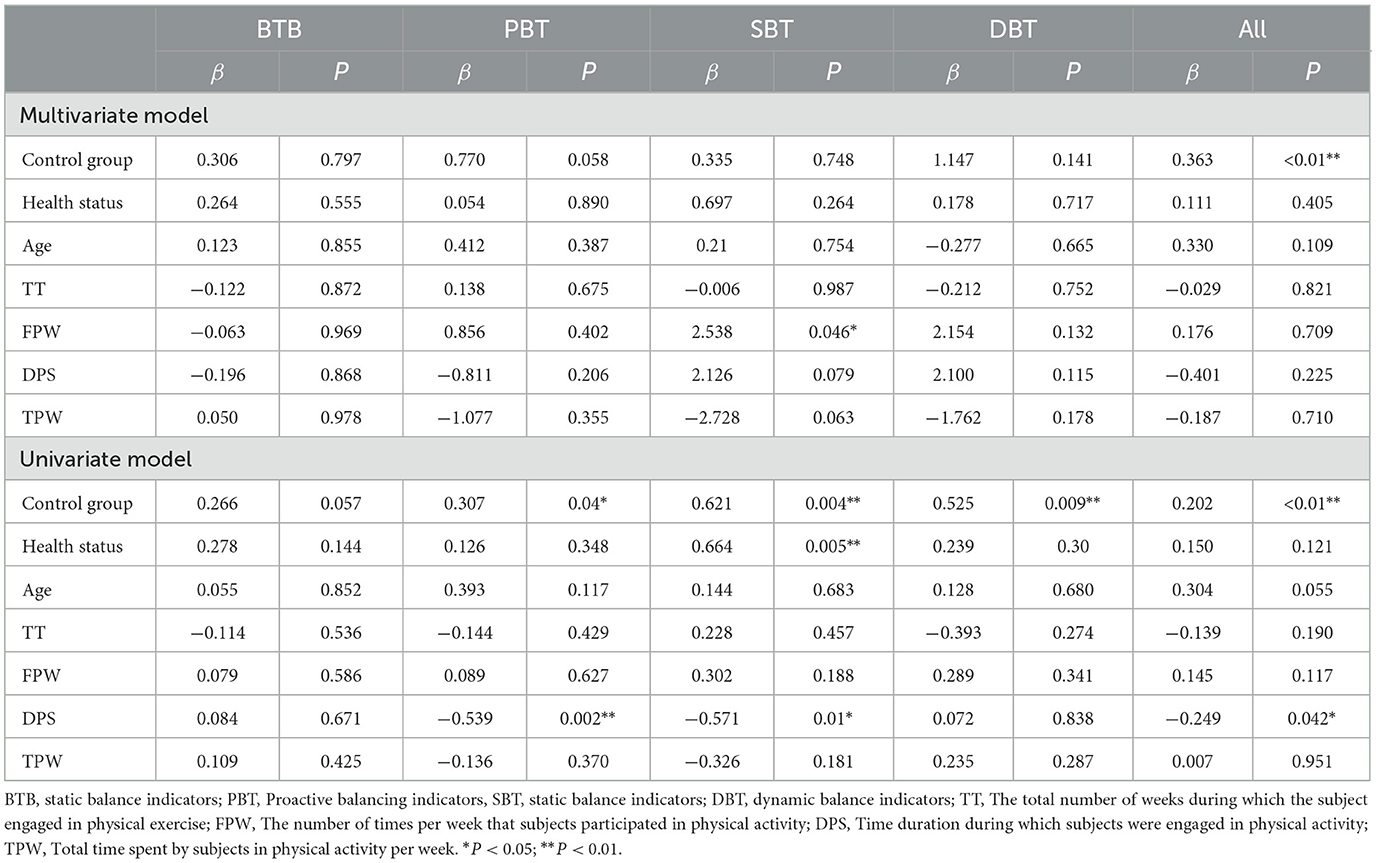
The study underwent moderated factor analysis (Table 2), incorporating covariates such as the control group, health status, age, and dose-related parameters. Two studies were excluded from the regression analysis due to the lack of dose parameters (45, 63). The results of the multivariate modeling indicated that the frequency of exercise sessions per week significantly moderated the positive effects on SBT (β = 2.538, P = 0.046). Additionally, the type of control group demonstrated a significant overall moderating effect (β = 0.363, P < 0.01). Univariate modeling revealed potential moderating effects of the control group on PBT, SBT, DBT, and overall balance outcomes. Health status was found to significantly moderate SBT (β = 0.664, P = 0.005). Furthermore, the duration of each training session significantly influenced PBT (β = −0.539, P = 0.002), SBT (β = −0.571, P = 0.01), and overall balance (β = −0.249, P = 0.042).
3.7 Sensitivity analysis
The study conducted a sensitivity analysis on the combined data, and the results remained robust after sequentially presenting each study, confirming the robustness of the findings. The details of the sensitivity analysis are provided in Appendix F.
3.8 Publication bias and correction
The funnel plot indicated the presence of publication bias in groups with combined data of seven or more studies (Appendix G). The funnel plots for DBT and BTB appeared less symmetrical; however, only Egger's test indicated significant asymmetry for DBT (P = 0.027), and Begg's test (P = 0.090 and P = 0.053) indicated no significant asymmetry. In contrast, the funnel plots for SBT showed significant asymmetry, as suggested by Egger's test (P = 0.215), while Begg's test (P = 0.003) indicated potential publication bias. To address this, we corrected the effect size for static balance using the Trim and Fill method proposed by Duval and Tweedie (79), resulting in a Hedges' g of 0.731 (95% CI: 0.526–0.936). The funnel plot for PBT exhibited slight asymmetry, as confirmed by Egger's test (P = 0.022) and Begg's test (P = 0.022), suggesting possible publication bias. This adjustment added seven data points, resulting in a corrected effect size of Hedges' g = −0.495 (95% CI: −0.850–−0.139).
4 Discussion
The present study reviewed the effects of BDJ on balance and fall-related indices in older adults, highlighting the impact of training parameters across different balance abilities. The findings indicate that: (1) BDJ significantly enhances overall balance in older adults, with proactive balance training yielding greater improvements compared to homeostatic balance (both dynamic and static); (2) Notable benefits begin to emerge after a minimum of 12 weeks of training, with 5–7 practice sessions per week lasting 30–49 min identified as the optimal training duration; (3) BDJ training significantly reduces fall risk and improves fall efficacy, thereby increasing older adults' confidence in managing potential falls.
4.1 Effect of Baduanjin on balanced performance
BDJ was associated with significant improvements in homeostatic balance, proactive balance, and balance test battery performance among older adults. However, no passive balance-related metrics were available for analysis. Previous research has established that balance is an idiosyncratic task (80), with one study noting a lack of strong correlation between different balance abilities in middle-aged and older adults (81). This indicates that comprehensively improving balance ability is crucial for non-specific exercise tasks. BDJ exercise is a mind-body practice akin to Tai Chi, incorporating stretching and frequent shifts of the center of gravity in various directions. Unlike idiosyncratic balance training, the enhancements achieved through BDJ are rooted in its kinematic characteristics. Both approaches to improving balance are based on the interplay between training adaptations and neural plasticity, with exercises promoting task-specific neural adaptations (82). Balance is primarily maintained through the synergy of the proprioceptive, visual, and vestibular systems (80). However, age-related degenerative changes in these systems lead to declines in sensory, central nervous, and skeletal musculature functions, resulting in reduced balance ability, irrespective of pathological dysfunction (83).
Prior research has shown that Baduanjin enhances proprioception in muscles and joints, particularly in the lower extremities, contributing to improved postural control and balance stability (21, 74). Proprioception plays a crucial role in postural control, especially during postural orientation, by providing the central nervous system with feedback about the position and movement of the body in space (84). BDJ strengthens proprioception by shifting the center of gravity across the horizontal, coronal, and sagittal planes at high frequencies, with a particular emphasis on the alignment of body and mind, which is employed to perceive the movement of forces in diverse directions, as well as the folding and rotation of bodily components. This aligns with the objectives of proprioceptive training, which aims to enhance sensory perceptions such as positional awareness and movement sensation (85). This type of slow-moving physical activity, which integrates both physical and mental exercise, has significantly improved balance in older adults (86). Additionally, certain movements challenge the visual and vestibular systems, enhancing their functions through habituation exercises. For instance, in the fifth form, “Shaking the Head and Swinging the Tail to Eliminate the Heart Fire,” the head is lowered while the center of gravity shifts, requiring rotation around the central axis via the neck muscles. This movement increases the difficulty for the vestibular system in spatial perception and balance maintenance. Approximating perturbation training has improved control of disturbed balance and reorganize feedback responses (87). It is possible that such training leads to increased adaptations in the spinal cord and cerebral cortex, potentially enhancing the automation of postural control (82). Furthermore, performing BDJ involves repetitive movements guided by musical instructions, along with synchronized breathing to enhance mental focus. The multiple perturbation strategy, which has optimized sensory integration, has significantly facilitated the development of balance, especially in the realm of proactive balance, among older adult (88). This likely accounts for the superior effects of BDJ on active balance compared to homeostatic balance, as greater gains are observed in dynamically complex tasks. However, it is important to note that publication bias exists in the PBT, with an adjusted effect size indicating a suboptimal result. Caution is warranted when interpreting these findings.
4.2 Optimal training parameters for Baduanjin
A study by Wang et al. demonstrated that the optimal dose of 24-Style Simplified Tai Chi Chuan (24-STC) for improving balance in older adults was 45–60 min, four times per week, over a minimum of 8 weeks (78). This aligns with the findings of our study, as BDJ and Tai Chi share similar kinesiological principles and cultural roots. However, in terms of session duration and training weeks, our study found that BDJ requires less time per session but longer overall training duration, suggesting that high-frequency and extended BDJ practice may offer greater benefits for balance in older adults. While both BDJ and 24-STC are mind-body exercises, BDJ engages more sensory systems. For instance, certain movements where the head is positioned below waist level (e.g., in the 5th and 6th forms) are more challenging than comparable Tai Chi movements. This is consistent with our findings, where improvements in static balance with eyes closed were superior to those with eyes open, likely due to the enhanced activation of motor-sensory systems.
The intensity of BDJ exercise for healthy adults aged 18–64 has been estimated at 3.2 MET, classifying it as moderate-intensity activity according to the Chinese Society of Sports Science (89). The U.S. Centers for Disease Control and Prevention recommends that older adults engage in at least 150 min of moderate-intensity activity per week, which 30 min per day, 5 days per week. Our study builds on this by finding that BDJ may require an even higher frequency of exercise to optimize balance improvements. Specifically, we observed balanced improvements in different balance abilities after 12 weeks of training. However, our data is limited by the small number of short-term (n ≤ 2) and long-term studies. In terms of weekly training frequency, 5–7 sessions per week yielded the most balanced development across different balance skills, though our study lacked data on higher frequencies (n ≥ 10), so we cannot exclude the possibility of additional benefits at higher frequencies. Interestingly, no significant moderating effect of training frequency on balance improvements was identified. Regarding the number of weeks, both 12–16 weeks and 20–26 weeks of training showed improvements across various balance metrics, with only slight differences between the two periods. However, improvements in proactive balance (PB) and dynamic balance (DB) were not significant in the 4–8 week range, although only two trials were included in this analysis.
This study examined the effect of exercise duration on outcomes, finding that optimal results were achieved with session lengths of 30–49 min, while a decline in proactive balance (PB) performance was observed at 50–60 min. Given the greater impact of BDJ on PB, it may not be advisable to extend practice sessions to 50–60 min. According to video tutorials published by the General Administration of Sport of China (GASPC), a standard BDJ session lasts approximately 12 min. Intervention protocols that incorporate 2–3 BDJ cycles after a preparatory activity appear to yield higher balance gains. Unfortunately, only one study included an intervention session shorter than 30 min (a single 15-min practice session), yet even this shorter session showed significant post-intervention improvements in the Berg Balance Scale (BBS) compared to both pre-intervention levels and the control group (41).
4.3 Effect of moderator factors on balance performance
The findings of this systematic review and meta-analysis indicate that neither the number of weeks of exercise nor the weekly duration significantly moderated the effect on balance outcomes. However, as previously mentioned, high-frequency exercise was recommended, and regression analysis results confirmed that the frequency of weekly training sessions and the type of control group had a significant impact on effect size. The control group's role may stem from incorporating participants' daily activities (e.g., walking) or essential tasks (e.g., routine care of sick individuals), which could influence balance performance. However, subgroup analyses revealed that BDJ outperformed the majority of control interventions across various balance abilities. After adjusting for variables, factors such as age, health status, and session duration significantly moderated balance outcomes. These findings align with prior research, suggesting that high-frequency training combined with appropriate session durations enhances the benefits, especially when considering total intervention time (22). Nevertheless, our study underscores the importance of carefully regulating the duration of each session. Prolonged sensory integration may lead to partial sensory deprivation, potentially causing sensory overload (90), as the continuous processing of sensory information can induce physical and mental fatigue earlier (91). Adverse effects such as dizziness, fatigue, palpitations, and chest tightness have been documented in safety checks related to BDJ practice (24). A key study that examined this phenomenon involved 90-min sessions in patients with chronic fatigue syndrome, where the extended duration may have contributed to adverse effects (92). This suggests that excessively long BDJ sessions could act as a trigger for such negative outcomes.
4.4 Research gap
While the outcomes of the majority of the included studies and the findings of this review are indeed encouraging, the overall quality of the research leaves something to be desired. The current body of work on Baduanjin (BDJ) and its impact on balance function has primarily concentrated on interventions spanning from 12 to 26 weeks. However, there is a notable absence of studies focusing on acute interventions and those with a long-term perspective. Additionally, the sustainability of the benefits post-intervention is an area that requires further investigation, yet only a few studies have conducted follow-up assessments. Regarding the outcomes, although most functional tests have yielded favorable results, there is an urgent need to enhance the precision of balance measurements. For instance, incorporating the use of pressure transducers to capture parameters of postural control is crucial, as the current data in this regard are less than optimal. In summary, underscore the imperative for future investigations to concentrate on several key areas: (1) enhancing the methodological rigor of research, (2) extending follow-up periods to discern the lasting impacts of BDJ on balance, (3) refining the accuracy of balance metrics, and (4) undertaking both long-term observational studies and acute intervention trials among specific populations.
5 Limitations
It is important to acknowledge several limitations of this study: (1) During the subgroup analyses, the absence of short-term and long-term studies limited the ability to assess short-term benefits and reduced the reliability of long-term outcomes. (2) Heterogeneity was observed among some subgroups. While potential sources of heterogeneity were explored, focusing solely on dose likely diminished the precision of the analysis. (3) Some balance metrics exhibited potential publication bias, and although adjustments were made, this may have affected the interpretation of the findings. Additionally, the study lacked a sufficient number of high-quality studies to establish a more solid basis for its conclusions. (4) The moderated effects analysis faced challenges, including data loss and difficulties in accurately categorizing health status due to incomplete information in the primary studies. Moreover, most studies did not provide the mean age for the entire sample, requiring the use of weighted conversions, which introduced some level of imprecision. (5) The lack of proactive balance data further limited the ability to draw comprehensive conclusions regarding overall balance outcomes.
6 Conclusions
In conclusion, this systematic review and meta-analysis suggest that BDJ is an effective intervention for enhancing balance and preventing falls in older adults that could be more beneficial than routine care, walking or regular activities for improving balance and reducing the risk of falls in older adults. For optimal balance outcomes, it is recommended to engage in a minimum of 12 weeks of training, consisting of five to seven sessions of 30 to 39 min each week. This dosage has been shown to yield significant improvements across various balance metrics, a finding that is consistently supported by the majority of studies included in this review.
However, exceeding this duration in a single session may diminish the observed benefits. Caution is advised in interpreting these results due to limitations related to heterogeneity, study quality, and the overall number of studies included.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
YY: Conceptualization, Methodology, Software, Validation, Visualization, Writing – original draft. EL: Conceptualization, Data curation, Supervision, Writing – review & editing. ZG: Data curation, Methodology, Writing – original draft. MT: Data curation, Validation, Writing – review & editing. ZZhao: Data curation, Methodology, Writing – review & editing. ZZhan: Data curation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1541170/full#supplementary-material
References
1. Institute of Medicine (US) Division of Health Promotion and Disease Prevention, editors. The Second Fifty Years: Promoting Health and Preventing Disability. Washington (DC): National Academies Press (1992). p. 15.
2. Terroso M, Rosa N, Torres MA, Simoes R. Physical consequences of falls in the elderly: a literature review from 1995 to 2010. Eur Rev Aging Phys Act. (2014) 11:51–9. doi: 10.1007/s11556-013-0134-8
3. World Health Organization. Falls. Geneva: World Health Organization (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/falls (accessed May 13, 2024).
4. Peel NM, Kassulke DJ, McClure RJ. Population based study of hospitalised fall related injuries in older people. Inj Prev. (2002) 8:280–3. doi: 10.1136/ip.8.4.280
5. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. (2006) 35(Suppl 2):ii37–41. doi: 10.1093/ageing/afl084
6. Garbin AJ, Fisher BE. The interplay between fear of falling, balance performance, and future falls: data from the national health and aging trends study. J Geriatr Phys Ther. (2023) 46:110–5. doi: 10.1519/JPT.0000000000000324
7. Jalali MM, Gerami H, Heidarzadeh A, Soleimani R. Balance performance in older adults and its relationship with falling. Aging Clin Exp Res. (2015) 27:287–96. doi: 10.1007/s40520-014-0273-4
8. Phu S, Vogrin S, Saedi AA, et al. Balance training using virtual reality improves balance and physical performance in older adults at high risk of falls. Clin Interv Aging. (2019) 14:1567–77. doi: 10.2147/CIA.S220890
9. Granacher U, Gollhofer A, Hortobágyi T, Kressig RW, Muehlbauer T. The importance of trunk muscle strength for balance, functional performance, and fall prevention in seniors: a systematic review. Sports Med. (2013) 43:627–41. doi: 10.1007/s40279-013-0041-1
10. Dai GB. Introduction to Traditional National Sports. 2nd ed Beijing: Higher Education Press (2015).
11. Guo Y, Shi H, Yu D, Qiu P. Health benefits of traditional Chinese sports and physical activity for older adults: a systematic review of evidence. J Sport Health Sci. (2016) 5:270–80. doi: 10.1016/j.jshs.2016.07.002
12. Song Y, Ren F, Sun D, Wang M, Baker JS, István B, et al. Benefits of exercise on influenza or pneumonia in older adults: a systematic review. Int J Environ Res Public Health. (2020) 17:2655. doi: 10.3390/ijerph17082655
13. Song Y, Sun D, István B, Thirupathi A, Liang M, Teo EC, et al. Current evidence on traditional Chinese exercise for cancers: a systematic review of randomized controlled trials. Int J Environ Res Public Health. (2020) 17:5011. doi: 10.3390/ijerph17145011
14. Song Y, Li J, István B, Xuan R, Wei S, Zhong G, et al. Current evidence on traditional Chinese exercises for quality of life in patients with essential hypertension: a systematic review and meta-analysis. Front Cardiovasc Med. (2021) 7:627518. doi: 10.3389/fcvm.2020.627518
15. Li F, Harmer PJ, Fisher KJ, McAuley E, Chaumeton N, Eckstrom E, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. (2005) 60:187–94. doi: 10.1093/gerona/60.2.187
16. Maciaszek J, Osiński W. The effects of Tai Chi on body balance in elderly people—A review of studies from the early 21st century. Am J Chin Med. (2010) 38:219–29. doi: 10.1142/S0192415X10007798
17. Burns E, Kakara R, Moreland B. A CDC Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. 4th ed Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (2022).
18. Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot. (2010) 24:e1–e25. doi: 10.4278/ajhp.081013-LIT-248
19. Jones C, Qi M, Xie Z, Moyle W, Weeks B, Li P. Baduanjin exercise for adults aged 65 years and older: a systematic review and meta-analysis of randomized controlled studies. J Appl Gerontol. (2022) 41:1244–56. doi: 10.1177/07334648211059324
20. Zou L, Wang C, Chen X, Wang H. Baduanjin exercise for stroke rehabilitation: a systematic review with meta-analysis of randomized controlled trials. Int J Environ Res Public Health. (2018) 15:600. doi: 10.3390/ijerph15040600
21. Lai J, Cai Y, Yang L, Xia M, Cheng X, Chen Y. Effects of Baduanjin exercise on motor function, balance and gait in Parkinson's disease: a systematic review and meta-analysis. BMJ Open. (2022) 12:e067280. doi: 10.1136/bmjopen-2022-067280
22. Guo L, Liu Z, Yuan W. The effect of Baduanjin on the balancing ability of older adults: a systematic review and meta-analysis. Front Med (Lausanne). (2022) 9:995577. doi: 10.3389/fmed.2022.995577
23. Lin H, Wan M, Ye Y, Zheng G. Effects of Baduanjin exercise on the physical function of middle-aged and elderly people: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Med Ther. (2023) 23:38. doi: 10.1186/s12906-023-03866-4
24. Fang J, Zhang L, Wu F, Ye J, Cai S, Lian X. The safety of Baduanjin exercise: a systematic review. Evid Based Complement Alternat Med. (2021) 2021:8867098. doi: 10.1155/2021/8867098
25. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
26. Aromataris E, Lockwood C, Porritt K, Pilla B, Jordan Z. JBI Manual for Evidence Synthesis. Adelaide: JBI (2024). doi: 10.46658/JBIMES-24-01
27. Navarrete-Villanueva D, Gómez-Cabello A, Marín-Puyalto J, Moreno LA, Vicente-Rodríguez G, Casajús JA. Frailty and physical fitness in elderly people: a systematic review and meta-analysis. Sports Med. (2021) 51:143–60. doi: 10.1007/s40279-020-01361-1
28. Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. (2017) 6:245. doi: 10.1186/s13643-017-0644-y
29. Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Bouter LM, et al. The Delphi List: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. (1998) 51:1235–41. doi: 10.1016/S0895-4356(98)00131-0
30. Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. (2003) 83:713–21. doi: 10.1093/ptj/83.8.713
31. Cashin AG, McAuley JH. Clinimetrics: physiotherapy Evidence Database (PEDro) scale. J Physiother. (2020) 66:59. doi: 10.1016/j.jphys.2019.08.005
32. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
33. Thornton A, Lee P. Publication bias in meta-analysis: its causes and consequences. J Clin Epidemiol. (2000) 53:207–16. doi: 10.1016/S0895-4356(99)00161-4
34. Irwig L, Macaskill P, Berry G, Glasziou P. Bias in meta-analysis detected by a simple, graphical test. Graphical test is itself biased. BMJ. (1998) 316:470–1. doi: 10.1136/bmj.316.7129.469
35. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
36. SPSSAU project. SPSSAU. Version 24.0. (2024). Available at: https://www.spssau.com (accessed June 28, 2024).
37. Dai X, Lu Y, Zheng Z, Jiang Q, Sha W, Zhu W, et al. Effects of Baduanjin and fitness walking on stability and muscle strength of middle-aged and old women. Chin J Rehab Med. (2023) 38:319–24. doi: 10.3969/j.issn.1001-1242.2023.03.006
38. Duan LL, Zhao YB, Er YL, Ye PP, Wang W, Gao X, et al. The effect of Ba Duan Jin on the balance of community-dwelling older adults: a cluster randomized control trial. Chinese J Epidemiol. (2024) 45:250–6. doi: 10.3760/cma.j.cn112338-20230506-00283
39. Er YL. A study on the short-term effects of Baduanjin exercise on the balance function of community-dwelling elderly women. Doctoral dissertation. China CDC (2017).
40. Gao Z. Rehabilitation effect of Baduanjin on frailty status and lower extremity motor function on pre-frail elderly people. Master's thesis. North China University of Science and Technology (2020).
41. Guan F. Application effects of Baduanjin in elderly patients during the recovery period of stroke. China's Naturop. (2023) 31:3–6.
42. Liu S. The influence of Health Qigong-Baduanjin exercise on the balance of the elderly. Master's thesis. Shanghai University of Sport (2018). Available at: https://kns.cnki.net/kcms2/article/abstract?v=MuRVhOLgpmtQ6f1mr5SInd2TDd-ffnL_eV1WDLyETJ07qlxFTHdsc4-zkkFDCLxMDPDMfolbNiTfoayfwoXIlER6Zlnht6WCKSwI2EvgSoJaVcr2PKJG6VNQ4K1nfg5LgZnSKK7xH3gZdXI-WzhDINOP84Re7tTi&uniplatform=NZKPT&language=CHS (accessed July 12, 2024).
43. Wu X, Xue W, Fang J, Wang J, Fan X, Ma H, et al. Baduanjin of movements on the risk of falls in community elderly people for 60 cases. Chinese Med Mod Dist Educ China. (2017) 15:106–9. doi: 10.3969/j.issn.1672-2779.2017.03.047
44. Xie D. Study on factors related to mildly impaired physical function in elderly people at risk of disability and the effect of Baduanjin intervention. Master's thesis. School of Public Health, Shantou University Medical College (2023). Available at: http://d-wanfangdata-com-cn.vpn2.sjlib.cn/thesis/ChJUaGVzaXNOZXdTMjAyNDAxMDkSCFk0MDkwNDA3GghkODR4Zm9vNA%3D%3D (accessed July 12, 2024).
45. Yao Y. Analysis of the effect of Baduanjin exercise on improving balance ability in the elderly. Health Must-Read Mag. (2021) 242:242–3.
46. Yu Y, Yang C, Su Y, Duan L, Er Y, Ye P, et al. The effect of Baduanjin exercise on fall efficacy in the elderly: evaluation and analysis of potential category heterogeneity. Chinese J Health Stat. (2020) 37:715–20. doi: 10.3969/j.issn.1002-3674.2020.05.019
47. Zhang LF. The influence of Baduanjin exercise on seniors' balance ability. Master's thesis. Capital Sports University (2010). Available at: https://kns.cnki.net/kcms2/article/abstract?v=MuRVhOLgpmvS4mPw6ez1NkcWBEcaWoktqr6BQ0KGQuHu8yIpb-TKhAGG144oepesB6kawOu4GTpxBBAfQzxUbWmBeOUGOQm3wLxgIBFqLCDofrnMyDtPkxwHfs2jCM72SFVCH7uScP9F33qOtdYJsHcetH-XSctE&uniplatform=NZKPT&language=CHS (accessed July 12, 2024).
48. Zhang L, Caixia H. The effect of Baduanjin rehabilitation training on limb motor function, daily living and quality of life in elderly stroke hemiplegic patients. Chinese J Gerontol. (2021) 41:4620–2. doi: 10.3969/j.issn.1005-9202.2021.21.006
49. Zhao L. Fitness Qigong Baduanjin and fall risk and self-efficacy in community elderly people. Master's thesis. Shanghai Normal University (2023).
50. Zheng LW, Zou LY, Lu AH, Xiu ZB, Wang RM, Lin CX, et al. Effect of Baduanjin on knee joint and balance ability in middle-aged and elderly patients with knee osteoarthritis. Tradit Chin Med Rehab. (2024) 1:28–37. doi: 10.19787/j.issn.2097-3128.2024.02.006
51. Zhou H, Wu Y, Wu C. Effects of Eight Trigrams Boxing combined with rehabilitation training in the treatment of elderly patients with convalescent cerebral vascular accident. Geriatric Health Care. (2021) 27:1191–4. doi: 10.3969/j.issn.1008-8296.2021.06.017
52. Zhou J, Zhao Y, Wei M. The effects of Baduanjin on balance ability, fall risk, and lower limb surface electromyography in the elderly. Lishizhen Med Mater Med Res. (2020) 31:124–7. doi: 10.3969/j.issn.1008-0805.2020.01.040
53. Hua Q. Effects of Baduanjin exercise on the microinflammatory state and exercise capacity of elderly patients with peritoneal dialysis. Chinese J Conval Med. (2021) 30:700–3. doi: 10.13517/j.cnki.ccm.2021.07.010
54. Li Z, Deng Q, Zhang Y, Peng R, Li J, Chen W, et al. Clinical observation on Eight-Section Brocade in improving balance ability and fall risk of senile osteoporosis. Western J Trad Chin Med. (2019) 32:62–5. doi: 10.3969/j.issn.1004-6852.2019.09.017
55. Li Q. The effects of Baduanjin Health Qigong on executive function and physical function in patients with mild cognitive impairment. Master's thesis. Shenyang Sport University (2018).
56. Liao Y. The epidemiological characteristics of falls in elderly people in Guangzhou city and the community intervention study of ‘Baduanjin' to improve balance function. Master's thesis. Southern Medical University (2018).
57. Chen CF, Xu H, Gu QL, Wu JF. Study on the impact of group Baduanjin practice on the risk of falls and quality of life in elderly patients. Chinese Commun Phys. (2016) 28:170–2. doi: 10.3969/j.issn.1007-614x.2016.28.106
58. Zhou J. A study on the intervention effect of eight-Duanjin on old age sarcopenia. Master's Thesis. Hunan University of Science and Technology, Sports College (2022).
59. Zhou S, Zou Y, Sun X, Xu Q. Research on Baduanjin for preventing falls in elderly patients with sarcopenia. Sport Sci Technol. (2020) 41:27–30. doi: 10.14038/j.cnki.tykj.2020.06.010
60. Zhuang K, Xu Y, Shen Z, Chen M, Jia J. The effect of Baduanjin on lower limb balance function and gait in elderly patients undergoing stroke rehabilitation. J Modern Med Health. (2019) 35:3352–3354. doi: 10.3969/j.issn.1009-5519.2019.21.036
61. Kuang XW. Observational study on the effect of simplified standing Ba Duan Jin on preventing and improving primary osteoporosis in the elderly. Chinese Commun Doctors. (2019) 35:186–188. doi: 10.3969/j.issn.1007-614x.2019.28.126
62. He JH, Yao L, Chang Z, Liu GN. The influence of the newly compiled Baduanjin exercise on the physiological functions of elderly female soldiers. Acta Acad Med Sinicae Vigil. (2011) 20:1–3. doi: 10.3969/j.issn.1008-5041.2011.01.004
63. Li R. Observation on the improvement of heart function and quality of life of elderly patients with chronic heart failure by Baduanjin. Massage Rehab Med. (2017) 24:23–5. doi: 10.3969/j.issn.1008-1879.2017.24.009
64. Shi XY. Research on the effect of Baduanjin exercise therapy in preventing falls in the elderly. Modern Diagn Treatm. (2017) 28:222–3. doi: 10.3969/j.issn.1001-8174.2017.02.015
65. Xu ZM, Zhang L, Qian Y, Chen MQ. Effects of Baduanjin combined with conventional exercise rehabilitation on exercise function in elderly patients with coronary heart disease. Chinese J Conval Med. (2022) 31:704–7. doi: 10.13517/j.cnki.ccm.2022.07.009
66. Wang C, Han F, Li LY, Liu CX, Peng MC. Application of Baduanjin exercise therapy in preventing falls in elderly psychiatric inpatients. Integr Tradit Chin Western Nurs. (2019) 5:68–71. doi: 10.11997/nitcwm.201909016
67. Carcelén-Fraile MdC, Aibar-Almazán A, Martínez-Amat A, Brandão-Loureiro V, Jiménez-García JD, Castellote-Caballero Y, et al. Qigong for muscle strength and static postural control in middle-aged and older postmenopausal women: a randomized controlled trial. Front Med. (2021) 8:784320. doi: 10.3389/fmed.2021.784320
68. Liu XY, Gao J, Yin BX, Yang XY, Bai DX. Efficacy of Ba Duan Jin in improving balance: a study in Chinese community-dwelling older adults. J Gerontol Nurs. (2016) 42:38–46. doi: 10.3928/00989134-20160201-03
69. Xiao CM, Zhuang YC, Kang Y. Effects of Ba Duan Jin Qigong on balance and fitness ability in older adults with type 2 diabetes mellitus. J Tradit Med Clin Naturop. (2017) 6:206. doi: 10.4172/2573-4555.1000206
70. Xiao CM, Zhuang YC. Effect of health Baduanjin Qigong for mild to moderate Parkinson's disease. Geriatr Gerontol Int. (2016) 16:911–9. doi: 10.1111/ggi.12571
71. Ye J, Zheng Q, Zou L, Yu Q, Veronese N, Grabovac I, et al. Mindful exercise (Baduanjin) as an adjuvant treatment for older adults (60 years old and over) of knee osteoarthritis: a randomized controlled trial. Evidence-Based Compl Altern Med. (2020) 2020:9869161. doi: 10.1155/2020/9869161
72. Yuen M, Ouyang HX, Miller T, Pang MYC. Baduanjin Qigong improves balance, leg strength, and mobility in individuals with chronic stroke: a randomized controlled study. Neurorehabil Neural Repair. (2021) 35:444–56. doi: 10.1177/15459683211005020
73. Ye M, Zheng Y, Xiong Z, Ye B, Zheng G. Baduanjin exercise ameliorates motor function in patients with post-stroke cognitive impairment: a randomized controlled trial. Complement Ther Clin Pract. (2022) 46:101506. doi: 10.1016/j.ctcp.2021.101506
74. Ye J, Simpson MW, Liu Y, Lin W, Zhong W, Cai S, et al. The effects of Baduanjin Qigong on postural stability, proprioception, and symptoms of patients with knee osteoarthritis: a randomized controlled trial. Front Med. (2020) 6:307. doi: 10.3389/fmed.2019.00307
75. Tou NX, Goh SF, Harding S, Tsao MA, Ng TP, Wee SL. Effectiveness of community-based Baduanjin exercise intervention for older adults with varying frailty status: a randomized controlled trial. Eur Rev Aging Phys Act. (2024) 21:28. doi: 10.1186/s11556-024-00363-6
76. Jiao MJ. Biomechanical analysis of the impact of ba duan jin on the balance ability of retired teachers. Unpublished master's thesis. Henan University, Kaifeng, China (2024).
77. Lesinski M, Hortobágyi T, Muehlbauer T, Gollhofer A, Granacher U. Effects of balance training on balance performance in healthy older adults: a systematic review and meta-analysis. Sports Med. (2015) 45:1721–38. doi: 10.1007/s40279-015-0375-y
78. Wang LC, Ye MZ, Xiong J, Wang XQ, Wu JW, Zheng GH. Optimal exercise parameters of Tai Chi for balance performance in older adults: a meta-analysis. J Am Geriatr Soc. (2021) 69:2000–10. doi: 10.1111/jgs.17094
79. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000) 56:455–63. doi: 10.1111/j.0006-341X.2000.00455.x
80. Dunsky A, Zeev A, Netz Y. Balance performance is task specific in older adults. BioMed Res Int. (2017) 2017:6987017. doi: 10.1155/2017/6987017
81. Kiss R, Schedler S, Muehlbauer T. Associations between types of balance performance in healthy individuals across the lifespan: a systematic review and meta-analysis. Front Physiol. (2018) 9:1366. doi: 10.3389/fphys.2018.01366
82. Taube W, Gruber M, Gollhofer A. Spinal and supraspinal adaptations associated with balance training and their functional relevance. Acta Physiol. (2008) 193:101–16. doi: 10.1111/j.1748-1716.2008.01850.x
83. Wang J, Li Y, Yang GY, Jin K. Age-related dysfunction in balance: a comprehensive review of causes, consequences, and interventions. Aging Dis. (2024). doi: 10.14336/AD.2024.0124-1
84. Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing. (2006) 35:ii7–ii11. doi: 10.1093/ageing/afl077
85. Allum JH, Honegger F. Interactions between vestibular and proprioceptive inputs triggering and modulating human balance-correcting responses differ across muscles. Exp Brain Res. (1998) 121:478–94. doi: 10.1007/s002210050484
86. Chen S, Zhang Y, Wang YT, Liu XL. Traditional Chinese mind and body exercises for promoting balance ability of old adults: a systematic review and meta-analysis. Evid Based Compl Alternat Med. (2016) 2016:7137362. doi: 10.1155/2016/7137362
87. Alizadehsaravi L, Bruijn SM, van Dieën JH. Balance training improves feedback control of perturbed balance in older adults. bioRxiv. (2021). doi: 10.1101/2021.03.31.437824
88. Gerards MHG, McCrum C, Mansfield A, Meijer K. Perturbation-based balance training for falls reduction among older adults: current evidence and implications for clinical practice. Geriatr Gerontol Int. (2017) 17:2294–303. doi: 10.1111/ggi.13082
89. Qiu J, Yang J, Lu M, Xu C, Yi L, Guo X, et al. Physical Activity Energy Expenditure Reference Value of Healthy Adults. T/CSSS 002–2023. Beijing: China Sports Science Society (2023).
90. Scheydt S, Müller Staub M, Frauenfelder F, Nielsen GH, Behrens J, Needham I. Sensory overload: a concept analysis. Int J Ment Health Nurs. (2017) 26:110–20. doi: 10.1111/inm.12303
91. Allen HA. Sensory loss, change, and its relationship to cognition in the brain. In: Reference Module in Neuroscience and Biobehavioral Psychology. Elsevier (2023). p. 1–10.
92. Chan JSM, Ho RTH, Chung K-F, Wang C-W, Yao T-J, Ng S-M, et al. Qigong exercise alleviates fatigue, anxiety, and depressive symptoms, improves sleep quality, and shortens sleep latency in persons with chronic fatigue syndrome-like illness. Evid Based Compl Alter Med. (2014) 2014:106048. doi: 10.1155/2014/106048
Keywords: dosages, balance, Baduanjin, Qigong, traditional exercise
Citation: Yang Y, Li E, Gong Z, Tualaulelei M, Zhao Z and Zhang Z (2025) Optimal exercise parameters of Baduanjin for balance in older adults: a systematic review and meta-analysis. Front. Public Health 13:1541170. doi: 10.3389/fpubh.2025.1541170
Received: 07 December 2024; Accepted: 11 February 2025;
Published: 19 March 2025.
Edited by:
Matthew Lee Smith, Texas A and M University, United StatesReviewed by:
Yang Song, Óbuda University, HungaryJames David Adams, Independent Researcher, Benicia, CA, United States
Copyright © 2025 Yang, Li, Gong, Tualaulelei, Zhao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Enjing Li, bGVlZWpAY2NudS5lZHUuY24=
 Yikun Yang
Yikun Yang Enjing Li1*
Enjing Li1* Zixin Gong
Zixin Gong