
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 17 February 2025
Sec. Public Mental Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1539305
This article is part of the Research Topic The Intersection of Psychology, Healthy Behaviors, and its Outcomes View all 80 articles
Objective: Individuals vary in their perception of psychological birth trauma (PBT), with some individuals progressing to postpartum post-traumatic stress disorder (PP-PTSD). However, from both preventive and developmental perspectives, PBT and PP-PTSD have received limited attention in China. This study examines the prevalence and influencing factors of PBT among women who underwent vaginal delivery in Chongqing, China, at 3 days and 42 days postpartum, as well as the correlation between perceived PP-PTSD and PBT, aiming to enhance understanding in this field.
Methods: This questionnaire-based, cross-sectional study was conducted on women who had a vaginal delivery admitted to a grade III-A general hospital using convenience sampling between February and April of 2024. Participants were questioned using a general questionnaire, the Birth Trauma Perception Scale for Women During Vaginal Delivery (BTPS-WVD) scale, and the Postpartum Post-Traumatic Stress Disorder Scale (PP-PTSD) at 3 and 42 days postpartum. Univariate and multiple linear regression analysis was performed to identify factors associated with PBT at 42 days postpartum. Pearson correlation analysis was used to investigate the correlation between PBT and PP-PTSD in women who had a vaginal delivery.
Results: The average score of PBT at 3 and 42 days postpartum were (43.37 ± 9.46) and (51.40 ± 13.54) respectively, the difference was statistically significant (p < 0.05). There were statistically significant differences in the dimensions of medical support trauma perception, delivery pain trauma perception, family support trauma perception, and delivery outcome trauma perception (p < 0.05). The average score of PP-PTSD at 3 and 42 days postpartum were (22.38 ± 7.13) and (22.29 ± 5.77) respectively, with no statistical significance (p > 0.05). The positive rate of PP-PTSD (score ≥ 38) at 3 and 42 days postpartum were 5 and 2%, respectively. Univariate analysis showed that, feeding mode, the effect of breast swelling on mood, mother separate from the newborn, separation time between mother and newborn, place of puerperium, psychological discomfort caused by delivering with others, use of epidural anesthesia, delivery time, advise others to deliver vaginally, the effects of wound pain, time of the postnatal wound pain and who decides on abnormal delivery were independently associated with PBT (p < 0.05). Multiple linear regression analysis showed that, mother separate from the newborn, separation time between mother and newborn, place of puerperium, psychological discomfort caused by delivering with others, the effects of wound pain, time of wound pain, who decides on abnormal delivery were independently associated with PBT (p < 0.05). Pearson correlation analysis showed that, PBT and its four dimensions were positively correlated with PP-PTSD (r = 0.488, p < 0.001).
Conclusion: Women who experienced PBT during vaginal delivery reported significantly higher levels of perceived trauma at 42 days postpartum compared to 3 days postpartum. Clinical staff, family, and society should pay attention to the risk factors and take corresponding intervention measures to reduce the degree of PBT and promote maternal and child health.
Psychological Birth Trauma (PBT) refers to the painful emotional experiences that women go through during childbirth, such as intense fear, hopelessness, and a sense of losing control. This subjective experience originates in the labor process and its effects continue into the postpartum period (1). The prevalence of PBT varies from 20 to 68.6% worldwide (1, 2). PBT can lead to suicidal impulses (3), anxiety and sadness (4), and a decrease in the willingness to have another child due to fear (5). It can also increase the rate of non-medical indication cesarean sections in clinical practice, disrupt mother-baby, marital, and family relationships (6), and create postpartum mental health problems, substantially damaging the physical and mental development of the next generation (7). Approximately 3% of women develop Postpartum Post-Traumatic Stress Disorder (PP-PTSD) (8), exhibiting clinical symptoms such as traumatic memories, cognitive negativity, hypervigilance, or avoidance behaviors (9). Women with PP-PTSD are often also affected by postpartum depression (10). The Global Strategy for Women’s, Children’s, and Adolescents’ Health (2016–2030) (11) and the WHO recommendations on intrapartum care for a positive childbirth experience (12) both suggest that current and future maternal and child health services should prioritize optimizing the maternal experience throughout pregnancy and childbirth, as well as promoting maternal, fetal, and infant safety. Therefore, evaluating and monitoring PBT interventions is critical for maternal and child health, as well as family and societal development. Existing research has paid little attention to PBT itself, with only a few scholars reviewing the research on PBT (13–15).
In this study, the PBT of women who had vaginal deliveries was evaluated at 3 and 42 days postpartum, respectively, to understand the differences, explore whether the degree of PBT changes with postpartum time, and analyze its influencing factors, thereby providing a theoretical basis for effective clinical interventions.
This questionnaire-based, cross-sectional study was conducted on women who had a vaginal delivery admitted to a grade III-A general hospital using convenience sampling between February and April of 2024. The team’s previous research examined the influencing factors of postpartum trauma within 3 days post-delivery. This current study extends that investigation to explore the influencing factors of postpartum trauma at 42 days post-delivery, comparing these factors with those observed within the initial 3 days to better understand the changes in postpartum trauma over time. The inclusion criteria were: (1) vaginal delivery; (2) single birth; (3) Gestational age ≥ 36 weeks; and (4) Neonatal Apgar score ≥ 7 points. The exclusion criteria were: (1) Postpartum hemorrhage occurs after delivery; (2) Perineal degree III and IV cleft; (3) Instrument-assisted delivery; (4) women with imperfect information; and (5) Who did not complete the scale assessment twice. The sample size was determined using the 10 EPV principle (16), considering multiple factors. A total of 30 independent variables were involved in this study. When EPV = 10, the required research objects were 300, and the incidence rate of PBT reported in literature was about 60%. The total required sample size was 300÷50% ≈ 180. Considering that there is a 20% shedding rate, in order to avoid errors as much as possible, the sample size is required to be 216 cases, and the final number of included samples is 306 cases. This study received approval from the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University, China, and complied with ethical standards under ethics number K2024-082-01.
The researchers designed a questionnaire specifically for this study, comprising the following sections: (1) demographic characteristics, such as age, work situation, education. (2) Birth-related information, including whether to use epidural anesthesia, newborn sex, the time of the postnatal wound pain, etc.
This scale was developed by Lian Zerong (17) and is suitable for the cultural, reproductive, and medical backgrounds of China. The scale includes four dimensions: medical support trauma perception, delivery pain trauma perception, family support trauma perception, and delivery outcome trauma perception, with a total of 31 items. Respondents rated each item on a 5-point scale with the following criteria: “1” does not meet, “2” somewhat meets, “3” meets, “4 “is somewhat compliant, “3″ is compliant, “5″ is very compliant, and the scoring criterion: the sum of 31 items. The higher the score, the higher the level of PBT. This scale is designed for the Chinese population and has not been applied to other populations. In this study, the Cronbach’s alpha coefficient of this table was 0.875.
This scale was sinicized and applied by Yang Xiaoyun (18). The scale includes four dimensions: trauma re-experiencing symptoms, avoidance numbing symptoms, and increased alertness symptoms, with a total of 17 items. It has been widely used in clinical studies investigating maternal PP-PTSD. According to the severity of symptoms, Likert’s 5-point (1–5 points) scale was used, with a total score of 17–85 points, the higher the score, the higher the likelihood of PP-PTSD, and the total score of ≥38 points was considered to be positive for PP-PTSD.
The content of the questionnaires was designed in an electronic form using the “Sojump” website.1 Participants were provided with QR codes for direct scanning, facilitating completion through WeChat. Upon submission, questionnaires were automatically transmitted to the Wenjuanxing platform. The questionnaires were distributed by the researchers themselves, using a standardized procedure to obtain informed consent. A total of 310 questionnaires were collected, but 4 questionnaires with a completion time of less than 100 s were excluded, resulting in 306 valid questionnaires and a response rate of 98%. The specific identity information of the research object does not appear in the study, and the data is only used for this study. In order to control confounding factors, two people checked the data quality in the process, and screened out the problems such as outliers and missing values in the original data to improve the prediction effect of the model.
Data analysis was performed using SPSS 23.0 statistical software (IBM, United States). Normally distributed continuous variables are presented as mean ± standard deviation (SD) and were compared using independent sample t-tests and analysis of variance (ANOVA) for between-group comparisons. Categorical variables were presented as counts and percentages. Pearson correlation analysis explores the correlation between PBT and PP-PTSD. Perform multiple linear regression analysis on items with a p-value <0.05 in the uni-variate analysis, The significance level was set at α = 0.05.
The characteristics and demographics of the participants are shown in Table 1. A total of 306 on women who had a vaginal delivery were enrolled, with an average age of 30.14 ± 3.5 years. The average score of PBT at 3 and 42 days postpartum were (43.37 ± 9.46) and (51.40 ± 13.54) respectively, the difference was statistically significant (p < 0.05).
There were statistically significant differences in the dimensions of medical support trauma perception, labor pain trauma perception, family support trauma perception and delivery outcome trauma perception (p < 0.05). The average score of PP-PTSD at 3 and 42 days postpartum were (22.38 ± 7.13) and (22.29 ± 5.77) respectively, with no statistical significance (p > 0.05).
The positive rate of PP-PTSD (score ≥ 38) at 3 and 42 days postpartum were 5 and 2%, respectively (Table 2).
The results showed that there existed higher scores of PBT at 42 days postpartum, and in order to understand the influencing factors of PBT at 42 days postpartum, univariate analysis was conducted to analyze the influencing factors, and the results showed that, feeding mode, the effect of breast swelling on mood, mother separate from the newborn, separation time between mother and newborn, place of puerperium, psychological discomfort caused by delivering with others, use of epidural anesthesia, delivery time, advise others to deliver vaginally, the effects of wound pain, time of the postnatal wound pain and who decides on abnormal delivery were independently associated with PBT (p < 0.05) (Table 3).
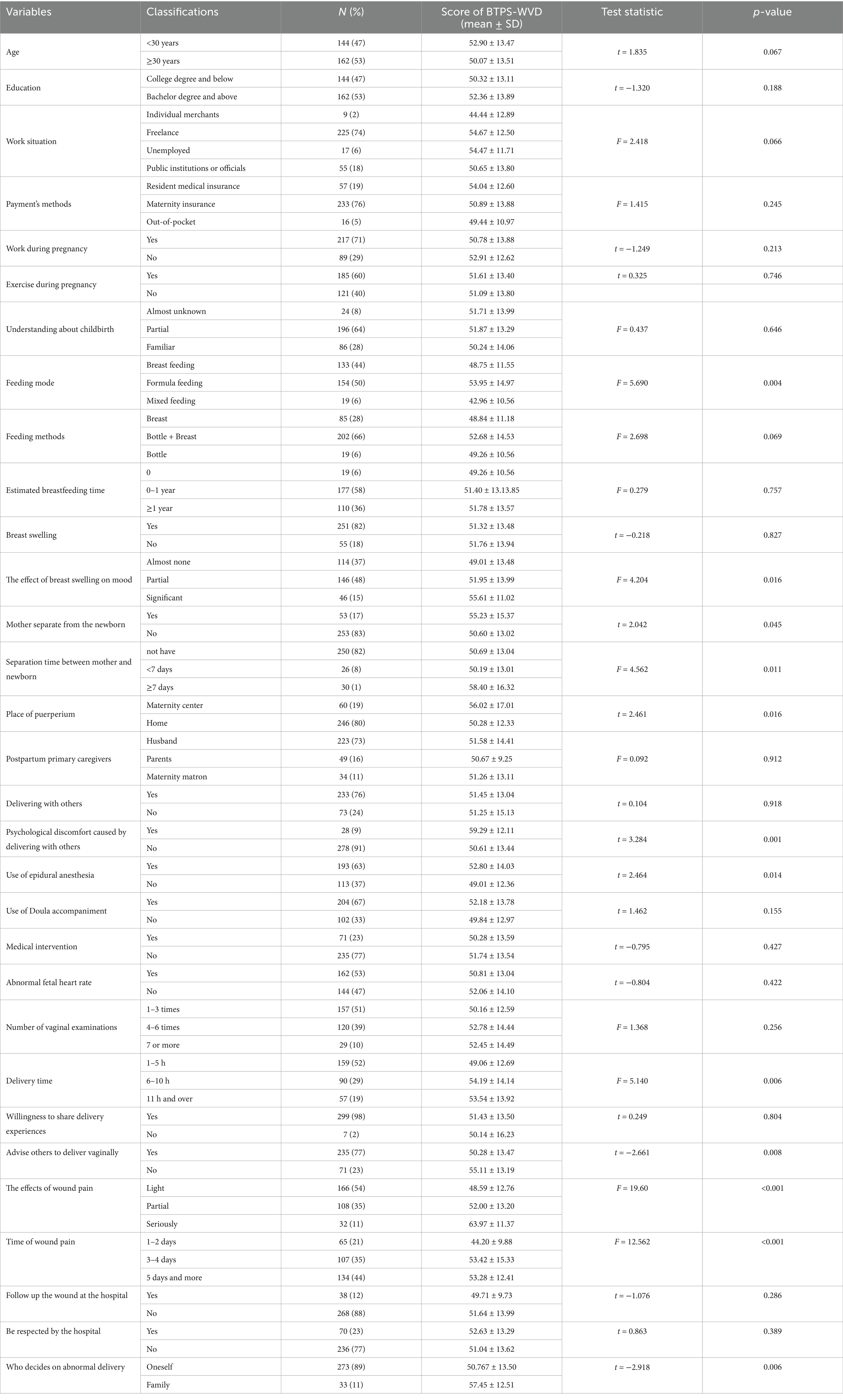
Table 3. Characteristics of the study population and univariate analysis of PBT at 42 days postpartum.
A multiple linear regression analysis was conducted on the influencing factors of PBT in women, with the total score of PBT as the dependent variable and statistically significant indicators in uni-variate analysis as independent variables. The specific assigned values are shown in Table 4. The factors that were ultimately included in the regression equation include mother separate from the newborn, separation time between mother and newborn, place of puerperium, psychological discomfort caused by delivering with others, the effects of wound pain, time of wound pain, who decides on abnormal delivery. The adjustment determination coefficient R2 of the fitting model is 0.297, indicating that the fitting model can analyze 29.7% of the variability. The overall test of the fitting model is p < 0.05, indicating that the fitting effect of the model is good, as shown in Table 5.
Pearson correlation analysis showed that, PBT and its four dimensions were positively correlated with PP-PTSD (r = 0.488, p < 0.001) (Figure 1; Table 6).
Psychological birth trauma and childbirth-related posttraumatic stress disorder represent a substantial burden of disease with 6.6 million mothers and 1.7 million fathers or co-parents affected by childbirth-related posttraumatic stress disorder worldwide each year (19). The main risk factors and causes of PBT are as follows, During pregnancy, risk factors most strongly associated were depression, fear of childbirth, poor health or complications of pregnancy, history of trauma, or previous psychological therapy for pregnancy or birth-related problems. During birth, risk factors most strongly associated were negative subjective birth experiences, operative birth (assisted vaginal delivery or cesarean delivery), and dissociation (including depersonalization, derealization, and emotional numbness) (20). Considering the harm of PBT, this study further investigated the risk factors of PBT in Chinese population.
This study examined the incidence of postpartum trauma at 3 and 42 days postpartum using the BTPS-WVD scale. The findings indicated that the severity of PBT increased over time following childbirth, suggesting the need for extended care to monitor maternal mental health during this critical period. Hospitals should implement comprehensive follow-up programs, families should maintain continuous support for maternal well-being, and society should increase its involvement in providing resources and assistance. Additionally, integrating psychologists into home-based support systems can help mothers navigate this challenging period characterized by elevated PBT levels. The median PBT scores in this study were 41 and 44 at 3 and 42 days postpartum respectively, and the number of people with PBT above the median at 3 and 42 days postpartum were 55 and 61%, respectively. Due to the lack of objective diagnostic criteria at present, the incidence of PBT varies substantially among studies (21), ranging from 9 to 44%. The differences in outcomes could be attributed to the following subjective and objective factors, medical intervention, maternal and newborn safety/separation, environment, delivery expectation, loss of control, doctor-patient communication and support (22). Murphy et al. (23) interviewed 4 women with PBT experience after their first delivery through narrative research method, and the results showed that early family planning with medical staff was a protective factor to avoid reoccurrence of trauma. Greenfield et al. (24) investigated 9 pregnant women who had undergone PBT and had a second pregnancy using longitudinal grounding theory and discovered that they had a strong desire to avoid suffering PBT again. They agreed that having access to credible information from specialists and collaborating with professionals to create and confirm pregnancy and family planning in the early stages of pregnancy were helpful approaches to avoid additional trauma.
The average score of PP-PTSD at 3 and 42 days postpartum was no statistical significance, with positive rates of 5 and 2%, respectively. In the UK and Australia, the prevalence of PP-PTSD in large-sample studies ranges from 1 to 6% (25, 26), Wang Meifang (27) conducted PP-PTSD surveys at 1–3, 4–6, and 7–12 months postpartum. The results showed that the positive rates of PP-PTSD were 10.8%, 12.6%, and 15.1%, respectively. The differences in positive PP-PTSD rates over the three periods were not statistically significant, implying that postpartum women’s PP-PTSD status remained rather consistent over the course of a year. However, the findings of this study suggest the incidence of post-traumatic stress disorder steadily falls after delivery, indicating that the severity of post-traumatic stress disorder decreases over time. Possible reasons include the body’s recuperation following childbirth, which enables it to adequately care for both itself and the newborn. As a result, it is critical to aid postpartum women in recuperating physically and mentally throughout the postpartum period in order to reduce the detrimental influence of the traumatic event during childbirth on their psychological health. This study found that the four components of the BTPS-WVD Scale, namely medical support, labor pain, family support, and delivery outcome, are all positively connected with post-traumatic stress disorder (PTSD). The ERTAN (8) study also indicated that birth trauma is a risk factor for postpartum traumatic stress disorder, which is in line with the findings of this study. As a result, all four dimensions of birth trauma deserve account, and interventions before and after labor can be based on these four components.
This study found that risk factors for PBT include delivering with others and who decides the abnormal delivery mode. The higher the PBT score, the more significant the psychological impact on parturients. In addition, women who experienced higher levels of trauma during vaginal delivery were less likely to recommend the same delivery to others. Dai Ling (28) conducted a study in which pregnant women observed other pregnant women’s poor birthing experiences and emergency. They experience emotional breakdowns and lose psychological resilience as a result of the tight atmosphere and fear of encountering the same situation. Beck (29) and Meyer (30) et al. argue that the loss of dignity is a key aspect in delivery trauma, and disrespect during labor can have an influence on a woman’s mental health. According to a study, during delivery, pregnant women have low levels of awareness and lack decision-making power, which can make them feel helpless. The study also found that the sense of losing control in decision-making and the lack of sufficient information are predictors of childbirth trauma (31). A Spanish study (32) revealed that unexpected birth, severe pain, lack of informed consent, and lack of social support are factors that give rise to PBT. Iranian researchers Taghizadeh et al. (33) carried out semi-structured interviews with 23 women ranging from 3 days postpartum to 32 years postpartum and discovered that the absence of delivery education, unfamiliar delivery environment, mother and child threatened, poor doctor-patient communication, and insufficient family support were significant risk factors for PBT. In the review carried out by Watson et al. (34), all interviewees disclosed having PBT experience. The study discovered that inappropriate care delivered by healthcare personnel, such as medical staff negligence, excessive medical intervention, etc., the loss of control and decision-making power during delivery, and insufficient social support were associated with PBT. Therefore, it is recommended that clinical medical staff pay heed to the PBT’s parturition factors, enhance delivery management, respect the demands of pregnant women, improve the medical experience, and promote the physical and mental health of pregnant women.
Among postpartum factors, formula feeding, separation time from newborn for at least 7 days, time of wound pain for at least 5 days, place of puerperium was Maternity center, the effect of Breast swelling on mood was significant had higher PBT scores. Chan (35) et al. also pointed out that the mother’s PBT is associated with the baby’s attachment, and being separated from the baby after delivery is a cold and dreadful experience that can make her feel lonely and sorrowful. Li Tao’s (2) research also referred that the lack of maternal–infant relationships after delivery and the transfer of the newborn to the NICU can make the mother feel lonely and ignored, thereby affecting her mental health.
Several studies (32, 36) have demonstrated that breastfeeding serves as a protective factor against PBT, which had the same findings as in this study. As breastfeeding may stimulate the secretion of hormones in women in vaginal delivery, it leads to more positive emotions and less stress (37). It is crucial to offer breastfeeding guidance during the prenatal, intrapartum and postpartum phases for women who have undergone maternal–infant separation.
Maternity centers are staffed by nutritionists, obstetricians, pediatricians, and postpartum therapists, so women in vaginal delivery and their families generally believe that maternity centers are more conducive to maternal recovery than at home. However, this study actually discovered that the postpartum period spent in a maternity center was ineffective in helping women reduce their PBT. This could reverse women’s perception of the postpartum care method. The absence of family support constitutes a detrimental factor that influences the mental health of women in vaginal delivery (38). A lack of supportive, listening and supportive communication from a partner can increase a woman’s negative experience of delivery (39). It is more beneficial to reduce the PBT for women in vaginal delivery by encouraging family members to offer greater support and encouragement to them and creating a warm and supportive family environment after delivery. This study reveals that the 42 days postpartum is associated with a higher PBT. Hence, healthcare workers should pay greater attention to this stage and collaborate with families and society to mitigate the impact of risk factors and facilitate women in vaginal delivery faster physical and mental recovery.
The research on PBT can be traced back to as early as 1996, according to a study (5). Furthermore, there has been a consistent increase in the number of papers published in this field over the past 3 years, indicating an enduring scholarly interest in maternal psychology. The impact of PBT extends beyond the physical and mental health of the women, encompassing her family, marital relationship, and even society itself. Therefore, it is imperative to address this global public health issue (22). The identification of the factors that contribute to PBT during delivery can enable the early identification of high-risk groups, the formulation of intervention strategies, the improvement of maternal mental health management, and the advancement of the health of both mothers and infants. The interventions referred to in the previous literature are as follows: Enlarging prenatal education to enhance maternal knowledge and improve psychological resilience, thereby lowering the incidence of PBT during delivery (30). Strengthening maternal family support and medical assistance, providing spouses with intimate physical contact and continuous support (40), can contribute to mitigating the degree of PBT. Previous meta-analyses demonstrate that proactive and early psychological intervention implemented by healthcare providers within 72 h postpartum proves effective in alleviating PBT symptoms in women during the 4–6 weeks postpartum period (41). Iranian scholar Hajarian Abhari et al. (42) offered Gamble psychological counseling at 35, 36, 37 weeks, and 4–12 h postpartum. Each session centered on: establishing a therapeutic relationship with women in vaginal delivery, introducing prenatal and postpartum problems, supporting the expression of emotions, facilitating the establishment of a connection between behavior, emotions, and delivery, and encouraging the sharing of the delivery. The results demonstrated that Gamble psychological counseling could effectively reduce the incidence of PBT after delivery. Taheri et al. (43) undertook semi-structured interviews with pregnant women, spouses, and healthcare professionals to summarize the prevention strategies for PBT, which comprise, intensifying prenatal training, providing a conducive delivery environment, appropriate care measures, such as pain alleviation and avoidance of excessive manipulation, and creating a favorable working atmosphere for midwives to elevate the quality of midwifery care. At present, the intervention measures remain in the development stage. Larossa et al. (44) explored the neurobiology and attachment implications of early tactile experience and discussed the importance of early postpartum experience in mitigating birth-related trauma. According to the results of the previous study, the research team conducted a continuous study on the intervention of labor trauma in women with vaginal delivery, and the specific intervention method was to improve the PBT level through the postpartum Internet-based care integrated with extended support services. In future studies, we propose extending the follow-up periods for assessing PBT status to 3 months, 6 months, and 1 year postpartum. This will provide a more comprehensive understanding of the changes in postpartum PBT among women who have undergone vaginal delivery. This will provide theoretical underpinnings for the prevention of postpartum PBT.
In conclusion, women who experienced PBT during vaginal delivery reported significantly higher levels of perceived trauma at 42 days postpartum compared to 3 days postpartum. Mother separate from the newborn, separation time between mother and newborn, place of puerperium, psychological discomfort caused by delivering with others, the effects of wound pain, time of wound pain, who decides on abnormal delivery were its risk factors. Healthcare workers, families, and society are obligated to implement targeted and individualized nursing strategies for high-risk groups so as to diminish the perceived extent of PBT among women who had a vaginal delivery and ensure the mental well-being of women during the perinatal period. However, the study exhibited several limitations that warrant consideration. The sample was derived from a single center, and the use of convenience sampling may introduce biases, including but not limited to geographical and age distribution biases. The study did not conduct a comparative analysis between populations with high and low PBT levels. The number of factors considered in the analysis was limited, which could be expanded in future research to address these limitations more comprehensively. Lastly, The BTPS-WVD scale has only been validated in the Chinese population, suggesting the need for further research on global applicability.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the First Affiliated Hospital of Chongqing Medical University, China. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
HQ: Data curation, Writing – original draft, Writing – review & editing. WW: Investigation, Methodology, Writing – review & editing. XF: Methodology, Writing – review & editing. XY: Project administration, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sun, X, Fan, X, Cong, S, Wang, R, Sha, L, Xie, H, et al. Psychological birth trauma: a concept analysis. Front Psychol. (2023) 13:1065612. doi: 10.3389/fpsyg.2022.1065612
2. Li, T, Guo, X, and Han, T. Investigation of maternal birth trauma after cesarean section and analysis of influencing factors. Chin J Fam Plan. (2024) 5:995–1001. doi: 10.3969/j.issn.1004-8189.2024.05.004
3. Pidd, D, Newton, M, Wilson, I, and East, C. Optimising maternity care for a subsequent pregnancy after a psychologically traumatic birth: a scoping review. Women Birth. (2023) 36:e471–80. doi: 10.1016/j.wombi.2023.03.006
4. Barut, S, Uçar, T, and Yılmaz, AN. Comparison of pregnant women's anxiety, depression and birth satisfaction based, on their traumatic childbirth perceptions. J Obstet Gynaecol. (2022) 42:2729–37. doi: 10.1080/01443615.2022.2106832
5. Wen, Y, Sun, H, and Li, T. Co-word cluster analysis of research hotspots in childbirth trauma. Chin Nurs Educ. (2024) 4:492–8.
6. Van Sieleghem, S, Danckaerts, M, Rieken, R, Okkerse, JM, de Jonge, E, Bramer, WM, et al. Childbirth related PTSD and its association with infant outcome: a systematic review. Early Hum Dev. (2022) 174:105667. doi: 10.1016/j.earlhumdev.2022.105667
7. Sun, X, Fan, X, Cong, S, Wang, R, Feng, J, Sha, L, et al. Effect of psychological interventions on mental health, personal relationships and quality of life of women who have subjectively experienced traumatic childbirth. J Affect Disord. (2023) 339:706–16. doi: 10.1016/j.jad.2023.07.085
8. Ertan, D, Hingray, C, Burlacu, E, Sterlé, A, and El-Hage, W. Post-traumatic stress disorder following childbirth. BMC Psychiatry. (2021) 21:155. Published 2021 Mar 16. doi: 10.1186/s12888-021-03158-6
9. James, S. Women's experiences of symptoms of posttraumatic stress disorder (PTSD) after traumatic childbirth: a review and critical appraisal. Arch Womens Ment Health. (2015) 18:761–71. doi: 10.1007/s00737-015-0560-x
10. Bayri Bingol, F, and Demirgoz, BM. The risk factors for postpartum posttraumatic stress disorder and depression. Perspect Psychiatr Care. (2020) 56:851–7. doi: 10.1111/ppc.12501
11. Nations S G O T. Global strategy for women's, children's and adolescent's health (2016–2030). (2015). Available at: https://www.who.int/lifecourse/p (accessed Mar 15, 2022).
12. WHO. WHO recommendations: intrapartum care for a positive childbirth experience. (2018). Available at: https://pubmed.ncbi.nlm.nih.gov/30070803/.
13. Dai, L, Zeng, T, and Yuan, M. Research progress of female labor trauma. Chin J Nurs. (2019) 2:311–5. doi: 10.3761/j.issn.0254-1769.2019.02.030
14. Yuan, M, Zeng, T, and Dai, L. Progress of research on labor trauma in women. Nurs Res. (2019) 12:2069–73.
15. Liu, Y, Guo, N, and Zhang,. Progress in the study of women's labor trauma and its impact assessment tools. China Nurs Manag. (2020) 8:1253–7. doi: 10.3969/j.issn.1672-1756.2020.08.029
16. Riley, RD, Ensor, J, Snell, KIE, Harrell, FE Jr, Martin, GP, Reitsma, JB, et al. Calculating the sample size required for developing a clinical prediction model. BMJ. (2020) 368:m441. doi: 10.1136/bmj.m441
17. Lian, Z. Development and application of an assessment tool for labor trauma perception of women in transvaginal delivery Nanchang University (2023).
18. Yang, X. An experimental study on the generation, attribution and intervention of post-traumatic stress disorder in medical college students Liaoning Normal University (2007).
19. Horsch, A, Garthus-Niegel, S, Ayers, S, Chandra, P, Hartmann, K, Vaisbuch, E, et al. Childbirth-related posttraumatic stress disorder: definition, risk factors, pathophysiology, diagnosis, prevention, and treatment. Am J Obstet Gynecol. (2024) 230:S1116–27. doi: 10.1016/j.ajog.2023.09.089
20. Gankanda, WI, Gunathilake, IAGMP, Kahawala, NL, and Ranaweera, AKP. Prevalence and associated factors of post-traumatic stress disorder (PTSD) among a cohort of Srilankan post-partum mothers: a cross-sectional study. BMC Pregnancy Childbirth. (2021) 21:626. doi: 10.1186/s12884-021-04058-z
21. De Graaff, LF, Honig, A, van Pampus, MG, and Stramrood, CAI. Preventing post-traumatic stress disorder following childbirth and traumatic birth experiences: a systematic review. Acta Obstet Gynecol Scand. (2018) 97:648–56. doi: 10.1111/aogs.13291
22. Fan, X, Pu, C, Zhang, A, Zhou, C, and Zhu, Z. Progress of research on maternal trauma in labor and delivery. Chin J Nurs. (2022) 10:1256–62. doi: 10.3761/j.issn.0254-1769.2022.10.016
23. Murphy, H, and Strong, J. Just another ordinary bad birth? A narrative analysis of first time mothers' traumatic birth experiences. Health Care Women Int. (2018) 39:619–43. doi: 10.1080/07399332.2018.1442838
24. Greenfield, M, Jomeen, J, and Glover, L. "it Can't be like last time" – choices made in early pregnancy by women who have previously experienced a traumatic birth. Front Psychol. (2019) 10:56. Published 2019 Jan 25. doi: 10.3389/fpsyg.2019.00056
25. Ayers, S, and Pickering, AD. Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth. (2001) 28:111–8. doi: 10.1046/j.1523-536x.2001.00111.x
26. Creedy, DK, Shochet, IM, and Horsfall, J. Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth. (2000) 27:104–11. doi: 10.1046/j.1523-536x.2000.00104.x
27. Wang, M, Wang, X, Zheng, W, Liang, Z, Du, J, and Yang, X. Analysis of the current status of maternal stress disorder and its influencing factors in different postpartum periods. Chin J Mod Nurs. (2022) 14:1902–7. doi: 10.3760/cma.j.cn115682-20210927-04404
28. Dai, L. Research on the experience of labor trauma and its influencing factors Huazhong University of Science and Technology (2019).
29. Beck, CT. Middle range theory of traumatic childbirth: the ever-widening ripple effect. Glob Qual. Nurs Res. (2015) 2:2333393615575313. doi: 10.1177/2333393615575313
30. Meyer, S, Cignacco, E, Monteverde, S, Trachsel, M, Raio, L, and Oelhafen, S. “We felt like part of a production system”: a qualitative study on women's experiences of mistreatment during childbirth in Switzerland. PLoS One. (2022) 17:e0264119. Published 2022 Feb 18. doi: 10.1371/journal.pone.0264119
31. Soet, JE, Brack, GA, and DiIorio, C. Prevalence and predictors of women's experience of psychological trauma during childbirth. Birth. (2003) 30:36–46. doi: 10.1046/j.1523-536x.2003.00215.x
32. Rodríguez-Almagro, J, Hernández-Martínez, A, Rodríguez-Almagro, D, Quirós-García, JM, Martínez-Galiano, JM, and Gómez-Salgado, J. Women's perceptions of living a traumatic childbirth experience and factors related to a birth experience. Int J Environ Res Public Health. (2019) 16:1654. doi: 10.3390/ijerph16091654
33. Taghizadeh, Z, Irajpour, A, Nedjat, S, Arbabi, M, and Lopez, V. Iranian mothers' perception of the psychological birth trauma: a qualitative study. Iran J Psychiatry. (2014) 9:31–6. Available at: https://pubmed.ncbi.nlm.nih.gov/25561946
34. Watson, K, White, C, Hall, H, and Hewitt, A. Women's experiences of birth trauma: a scoping review. Women Birth. (2021) 34:417–24. doi: 10.1016/j.wombi.2020.09.016
35. Chan, SJ, Ein-Dor, T, Mayopoulos, PA, Mesa, MM, Sunda, RM, McCarthy, BF, et al. Risk factors for developing posttraumatic stress disorder following childbirth. Psychiatry Res. (2020) 290:113090. doi: 10.1016/j.psychres.2020.113090
36. Hernández-Martínez, A, Rodríguez-Almagro, J, Molina-Alarcón, M, Infante-Torres, N, Donate Manzanares, M, and Martínez-Galiano, JM. Postpartum post-traumatic stress disorder: associated perinatal factors and quality of life. J Affect Disord. (2019) 249:143–50. doi: 10.1016/j.jad.2019.01.042
37. Diez-Sampedro, A, Flowers, M, Olenick, M, Maltseva, T, and Valdes, G. Women's choice regarding breastfeeding and its effect on well-being. Nurs Womens Health. (2019) 23:383–9. doi: 10.1016/j.nwh.2019.08.002
38. Huang, D, Dai, L, Zeng, T, Huang, H, Wu, M, Yuan, M, et al. Exploring contributing factors to psychological traumatic childbirth from the perspective of midwives: a qualitative study. Asian Nurs Res (Korean Soc Nurs Sci). (2019) 13:270–6. doi: 10.1016/j.anr.2019.10.002
39. Simon, RM, Johnson, KM, and Liddell, J. Amount, source, and quality of support as predictors of Women's birth evaluations. Birth. (2016) 43:226–32. doi: 10.1111/birt.12227
40. Hodnett, ED, Gates, S, Hofmeyr, GJ, and Sakala, C. Continuous support for women during childbirth. Cochrane Database Syst Rev. (2007) 3:CD003766. doi: 10.1002/14651858.CD003766.pub2
41. Taylor Miller, PG, Sinclair, M, Gillen, P, McCullough, JEM, Miller, PW, Farrell, DP, et al. Early psychological interventions for prevention and treatment of post-traumatic stress disorder (PTSD) and post-traumatic stress symptoms in post-partum women: a systematic review and meta-analysis. PLoS One. (2021) 16:e0258170. doi: 10.1371/journal.pone.0258170
42. Hajarian Abhari, Z, Karimi, FZ, Taghizdeh, Z, Mazloum, SR, and Asghari Nekah, SM. Effects of counseling based on Gamble's approach on psychological birth trauma in primiparous women: a randomized clinical trial. J Matern Fetal Neonatal Med. (2022) 35:668–76. doi: 10.1080/14767058.2020.1730799
43. Taheri, M, Taghizadeh, Z, Jafari, N, and Takian, A. Perceived strategies to reduce traumatic childbirth amongst Iranian childbearing women: a qualitative study. BMC Pregnancy Childbirth. (2020) 20:350. doi: 10.1186/s12884-020-03045-0
Keywords: puerperium, psychological birth trauma, postpartum post-traumatic stress disorder, vaginal delivery, influencing factors
Citation: Qin H, Wei W, Feng X and Yang X (2025) The current status of psychological birth trauma in women who had a vaginal delivery and associated factors: a questionnaire-based, cross-sectional study. Front. Public Health. 13:1539305. doi: 10.3389/fpubh.2025.1539305
Received: 04 December 2024; Accepted: 29 January 2025;
Published: 17 February 2025.
Edited by:
Yibo Wu, Peking University, ChinaReviewed by:
Elena Commodari, University of Catania, ItalyCopyright © 2025 Qin, Wei, Feng and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiwei Wei, NDIzNTgzMjZAcXEuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.