
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 05 March 2025
Sec. Children and Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1535004
 Audrey Geoffroy1*
Audrey Geoffroy1* Wasna Sirirungsi2
Wasna Sirirungsi2 Parinya Jongpaijitsakul3
Parinya Jongpaijitsakul3 Wanna Chamjamrat4
Wanna Chamjamrat4 Chutima Ruklao5
Chutima Ruklao5 Manoosin Kongka6
Manoosin Kongka6 Usa Sukhaphan7
Usa Sukhaphan7 Somporn Sathan8
Somporn Sathan8 Sriphan Thina9
Sriphan Thina9 Tassawan Khayanchoomnoom10
Tassawan Khayanchoomnoom10 Sophie Le Coeur1,2,3 for the TEEWA Study Group
Sophie Le Coeur1,2,3 for the TEEWA Study GroupBackground: Thailand has been particularly affected by the HIV epidemic in the middle of the years 1990s. Thousands of children living with perinatal HIV have been exposed to HIV-related stigma/discrimination, but its frequency and expressions have been little studied. Our objectives were to assess, among adolescents living with perinatal HIV, the prevalence of stigma/discrimination, the factors associated with it and its expressions.
Methods: All caregivers of adolescents aged 12–19 years living with perinatal HIV and receiving antiretrovirals in 20 hospitals throughout Thailand were invited to complete a face-to-face questionnaire on their adolescent's life, and to report their adolescents' experiences of stigma/discrimination. Stigma/discrimination as perceived by the caregivers was analyzed using both quantitative and qualitative approaches.
Results: A total of 712 adolescents living with perinatal HIV and their caregivers were interviewed as part of the TEEWA study between March 2010 and November 2012. Of the 572 adolescents living in family settings, 464 had their HIV-status known in the community. Among them, the overall stigma/discrimination prevalence was 46%. The multivariable analysis showed that the risk of being stigmatized was nearly 3 times higher in the northeast region (OR: 2.93, 95%CI: 1.36–6.45) and when having a low intellectual ability (OR: 3.35, 95%CI: 1.66–7.10). It was nearly twice higher in case of conflicts with caregivers (OR: 1.81, 95%CI: 1.17–2.79) and when caregivers were members of a support group (OR: 2.28, 95%CI: 1.48–3.53), while having a BMI >18.5 was associated with a lower risk of stigma/discrimination (OR: 0.61, 95%CI: 0.37–0.98). Expressions of stigma/discrimination included bullying, social isolation, behavioral discrimination and public disclosure. Consequences of stigma/discriminations included voluntary withdrawal from school, painful awareness of HIV status, marginalization from the community, and separation of drinks and food.
Conclusion: We found that the prevalence of stigma/discrimination among adolescents living with perinatal HIV was high. Despite existing policies, stigma eradication remains necessary to normalize their life as they grow into adulthood and may face the consequences of past/current discrimination in terms of access to university studies or occupation, at work, in the community or in their romantic life.
Recognized by the United Nations General Assembly in 2006 as “a critical element in combating the global HIV/AIDS pandemic” (1), HIV-related stigma has been defined as negative beliefs, feelings and attitudes toward people living with HIV, groups associated with people living with HIV and other key populations at high risk of HIV infection (2). In addition, UNAIDS has characterized discrimination as the unfair and unjust action taken against an individual or group because of their real or perceived status or attributes, such as a health condition (e.g. HIV), socioeconomic status, gender, race, sexual identity or age (3). HIV-related stigma/discrimination is recognized as an important cause of inequality (4), leading to poorer resources, socio-emotional skills and access to prevention and healthcare (5). However, the extent of stigma/discrimination is difficult to assess because people may keep their HIV status secret for fear of being stigmatized or discriminated against.
Stigma/discriminations in perinatally infected children and adolescents has multiple characteristics. Among them, orphanhood, in affected communities, might be interpreted as the loss of parents because of AIDS and the HIV-stigma toward parents can be passed on to their children (6, 7). HIV-stigma could impede an adolescent's education and cognitive development (8, 9). A lower intellectual capacity could be a cause of stigmatization in itself and reinforce HIV-stigma (10). Poor health has been found to be a cause of stigma (4), notably when associated with visible symptoms of HIV, like lipodystrophy (11–13). Fear of stigma or discrimination can lead to poor access to HIV diagnosis (14) and reduced adherence to antiretroviral treatment, disease progression, health problems and, in turn, stigma (15). Adolescents might have a lower perception of their happiness (6, 16), and on the other hand, those who do not know their HIV status may not perceive any social isolation (17, 18). As for caregivers, their participation in support groups would enable them to be better informed about HIV and to be more sensitive to stigma and discrimination (19). Finally, the poor financial situation of the caregivers may reinforce stigma (6, 20, 21). Food accessibility has been specifically mentioned as a priority need for adolescents' caregivers, as good nutritional status would reduce the visibility of the disease (22).
Thailand was particularly affected by the HIV epidemic from the late 1980s onwards. At first, the HIV epidemic impacted intravenous drug users, then sex workers, their clients and eventually their non-sex workers girlfriends or wives, confirming the generalization of the epidemic (23). According to the Thai Ministry of Public health, in the early 2010s there were more than 12,000 HIV-infected adolescents aged 12–19 years old in the country, of whom at least 9,000 were receiving antiretroviral therapy (24). In addition, according to UNAIDS, there were ~520,000 people living with HIV in Thailand in 2021. Of these, around 2,000 were under 15 years of age (25), a dramatic reduction reflecting the success of the national Prevention of mother-to-child transmission (PMTCT) program (26).
While there is literature on HIV-related stigma in adults in Thailand (21, 27–30), little is known about the specific population of children and adolescents living with perinatally-infected HIV. To our knowledge, only one survey conducted at Chiang Mai University Hospital in northern Thailand has assessed stigma from the perspectives of caregivers (31) and adolescents (32). It shows that discriminatory attitudes were most prevalent among caregivers themselves, and that HIV-related stigma/discrimination was identified in all aspects of adolescents' lives.
To better understand the circumstances and expressions of stigma among children and adolescents living with perinatal HIV, we analyzed data from a multicenter cross-sectional study conducted among adolescents and their caregivers in Thailand (33). The aim of this analysis was to assess the prevalence of stigma/discriminations and its associated factors among children/adolescents living with perinatal HIV in Thailand, as perceived by their caregivers. We also conducted a qualitative description of the experiences of stigma/discrimination during childhood or adolescence as perceived by their caregivers.
We used the quantitative and qualitative information obtained from caregivers of adolescents living with perinatal HIV who participated in the Teens Living With Antiretrovirals (TEEWA) study (33). Briefly, the TEEWA study is a cross-sectional study conducted between January 2010 and November 2012 to examine the living conditions of adolescents living with perinatal HIV in Thailand compared with a control group from the general population. Caregivers (or legal guardians) of adolescents aged 12–19 years who were receiving antiretrovirals (ART) in 20 public hospitals across Thailand were invited to participate in the study with their adolescent child. At the hospital, the adolescents completed a detailed self-administered questionnaire about their daily lives. Because some adolescents did not know their HIV status, the adolescent questionnaire did not include questions about HIV. In a face-to-face interview conducted in the hospital, caregivers were asked about the adolescent's sociodemographic status, life and medical history, including HIV diagnosis and treatment history, experiences of stigma/discrimination, caregivers' perception of their adolescent's wellbeing, and their relationship. Clinical, virological and immunological information was extracted from medical records by the attending hospital nurse. Written informed consent and assent was obtained from caregivers and adolescents, respectively. Details regarding the TEEWA study have been published elsewhere (33).
The study was approved by the Faculty of Associated Medical Sciences of Chiang Mai University (ref: AF02-014) and by the ethics committees of the participating hospitals. All data were pseudo-anonymized using unique identifiers. Data is available upon request.
Only adolescents living in a family environment were included, as the question on stigma/discrimination was not asked for those living in orphanages. In fact, they usually live in a separate environment where they have limited interaction with the community. Moreover, these children/adolescents may not talk to orphanage staff about their experiences of stigma/discrimination. In addition, adolescents whose HIV status was not known from the community (as reported by the caregivers) were excluded from the analysis. In fact, when the HIV status was not disclosed or was kept secret from the community, adolescents were not exposed to HIV-related stigma and discrimination. Community (≪ชุมชน≫ in Thai language) includes all people present in the adolescent's environment apart from family members.
Experiences of stigma/discrimination were recorded by asking caregivers whether they knew that the adolescent in their care had ever experienced stigma or social discrimination because of their HIV status. The settings in which these experiences of stigma or discrimination had occurred were also recorded: family, friends, school, hospital, in the community. Within each setting, the frequency of occurrence was also reported.
The TEEWA questionnaire was built to assess the living situation of adolescents living with perinatal HIV, but not specifically to address the question of stigma. Characteristics obtained from the caregiver interviews included the adolescent's gender; age; region of residence (center, north, northeast, or south); orphan status, classified as at least one parent alive vs. both parents known to be dead; school delay (i.e. having repeated a grade); caregiver's perceived intellectual ability of the adolescent (good/very good, fair/low/very low); perceived adolescent's health (very good/good/fair/poor/very poor); perceived happiness (very happy/happy/fair/unhappy/very unhappy); presence of conflicts with the adolescent; caregiver's knowledge of the adolescent's awareness of his/her HIV status (yes, no or unsure); age at ART initiation; adherence to ART (very good/good/fair/poor/very poor).
Clinical characteristics of adolescents obtained from medical records included the adolescent's most recent height and weight, CD4 cell count, and HIV-1 RNA viral load. The body mass index (BMI) was calculated, and underweight was defined as < 18.5 kg/m2.
Information about the adolescent's caregiver included gender; age; relationship with the adolescent (parent, grandparent or sibling, aunt or uncle, and other); perceived financial situation (very good/good/fair/difficult/very difficult); perceived current health status (very good/good/fair/poor/very poor); and membership in a support group for people living with HIV/AIDS.
We first describe the characteristics of adolescents living in family setting overall and provide the percentages of adolescents whose HIV-status is known in the community. We then provide the percentages of adolescents reporting stigma/discrimination among those whose HIV status was known in the community. The chi-square test was used to assess differences between groups, with statistical significance set at p < 0.05.
Logistic regression was used to identify factors associated with any experience of discrimination and was carried out in two stages: Covariates with statistical significance < 0.15 in the univariable analysis were included in the multivariable analysis (34). Two additional logistic regressions were performed to assess the factors associated with “repeated stigma/discrimination,” i.e. when it was reported to occur regularly in at least one circumstance, and “diverse stigma/discrimination,” i.e. when it was reported in at least two circumstances. Statistical analyses were performed using R software (version 4.1.2).
Caregivers were also asked to describe their adolescents' experiences of stigma by answering the following question: “Is there any particular experience of stigma/discrimination concerning your child that you can tell us about.” All verbatims were recorded and translated into English by the interviewers. They were all included in the analysis. Inductive analysis was used to identify the main themes and was checked by two of the authors. Comments were classified according to these themes and their frequency were reported. The relationship between the caregiver and the child was specified when reporting verbatims. Each selected comment in the results section came from a different family.
A total of 712 adolescents living with perinatal HIV and their caregivers were interviewed as part of the TEEWA study between March 2010 and November 2012. Among the adolescents, those living in orphanages (n = 136), those not currently receiving ART (n = 3) and one with missing information on stigma were excluded, leaving a total of 572 adolescents. Figure 1 presents the study population selection.
Table 1 provides a description of the adolescents' and their caregivers' characteristics obtained from the caregivers' questionnaire. Fifty eight percent were female. Their median age was 14 years. The majority were living in the North. HIV status was more often known in the community in the North and North-East regions. Moreover, 43% were orphan from both parents, 88% were aware of their HIV status, 67% had a CD4 count >500 cells/mm3, and 82% had a viral load below 50 copies/ml.
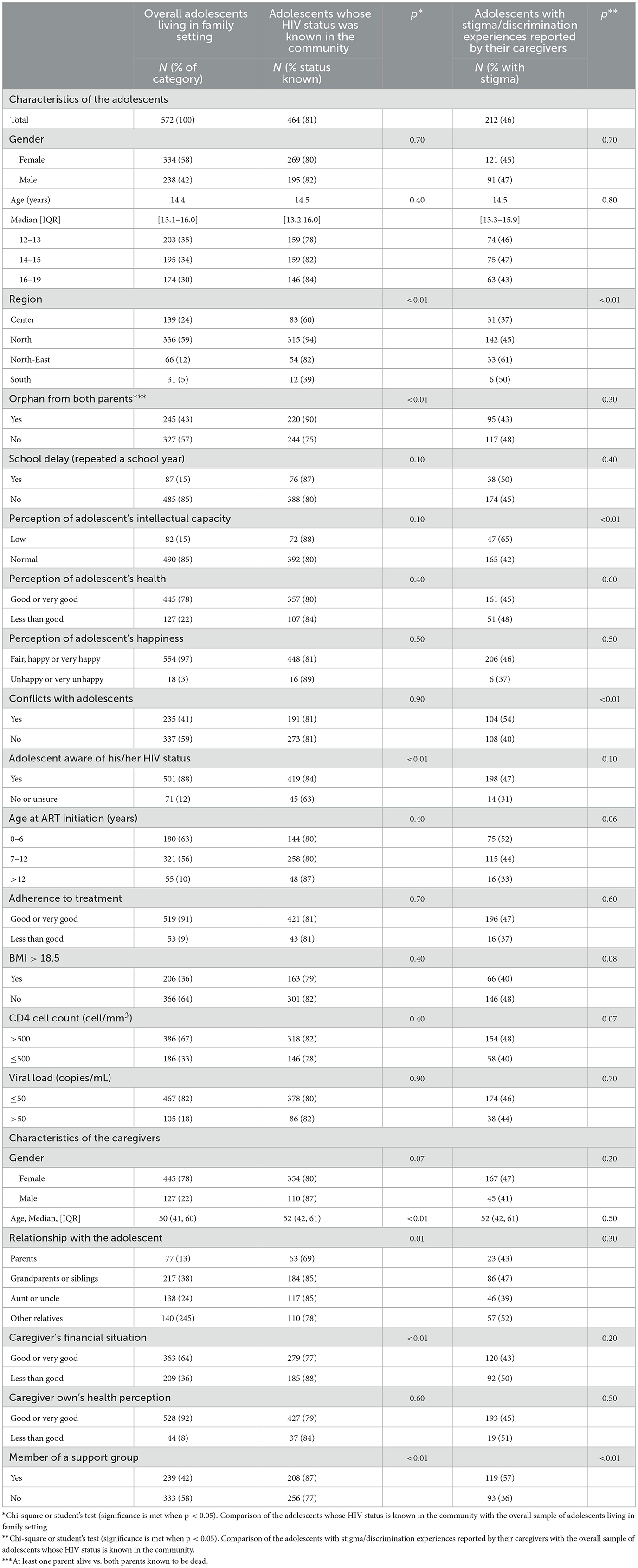
Table 1. Characteristics of adolescents living in family setting overall, percentages of adolescent's whose HIV status is known in the community, and percentages of adolescents with stigma/discrimination experiences as reported by their caregivers.
Overall, 81% of the adolescents had their HIV status known in the community (Table 1). Disclosure was significantly more frequent in the North and North-East (p < 0.01), when the adolescents were orphan from both parents (p < 0.01), when they were aware of their own HIV status (p < 0.01), when the caregivers were older (p < 0.01), when their financial situation was not good (p < 0.01) and when the caregivers were members of an HIV support group (p < 0.01).
A total of 212 (46%) caregivers reported at least one occurrence of stigma/discrimination experienced by their child/adolescent (Table 1). Stigma/discrimination was significantly more frequent among those living in the Northeast region (p < 0.01), among those perceived by the caregiver to have an intellectual disability (p < 0.01), among those in conflicts with their caregiver (p < 0.01), and among those whose caregiver was member of a support group (p < 0.01). There was no statistical association with the orphan status, but there was a trend toward more frequent stigma/discrimination among adolescents who started ART before age 7 years (p = 0.06), those who had a BMI < 18.5 (p = 0.08), and those who had CD4 count >500 cells/mm3 (p = 0.07).
Stigma/discrimination had primarily occurred at school in 64% of reports (from classmates, teachers or staff), from friends in 59% of the cases, and from family members in 10% of the cases (Table 2). Stigmatization in hospital was reported in < 1% of the cases. Twenty three percent of the caregivers reported repeated stigma/discrimination in the same context, and 24% in multiple contexts (Table 2).
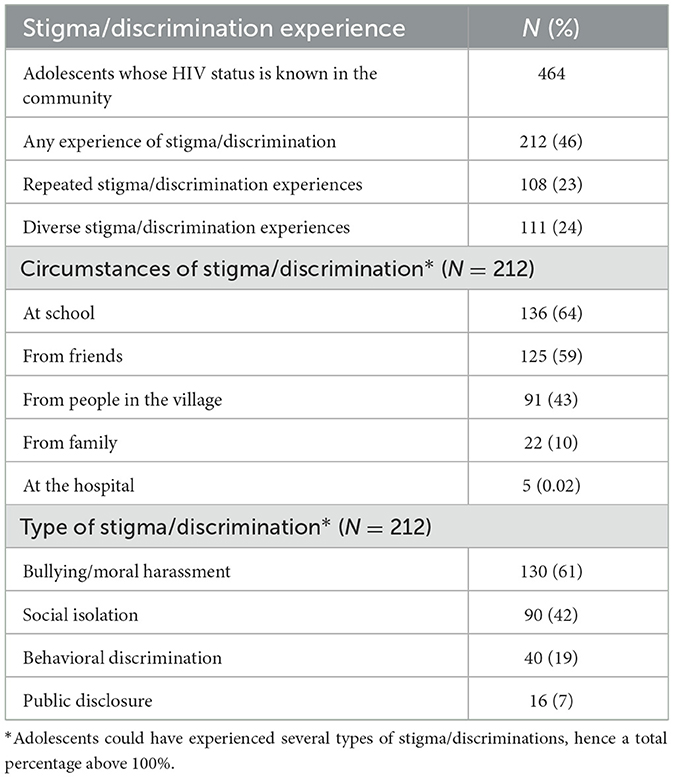
Table 2. Prevalence, context and types of stigma and discrimination experiences, as documented by the caregivers.
After adjustment for age and gender, the following covariates were included in the multivariable analysis: region, awareness of HIV status, perception of adolescent's intellectual abilities, conflicts with caregivers, age at ART initiation, BMI, CD4 count and caregivers' being membership of support groups. Factors independently associated with an experience of stigma/discrimination are presented in Table 3. The risk of being stigmatized, as perceived by the caregivers, was nearly three times higher in the northeast region (OR: 2.93, 95%CI: 1.36–6.45) and when having a low intellectual ability (OR: 3.35, 95%CI: 1.66–7.10). It was twice as high in case of conflicts with caregivers (OR: 1.81, 95%CI: 1.17–2.79), and when caregivers were members of a support group (OR: 2.28, 95%CI: 1.48–3.53). In contrast, having a BMI >18.5 was associated with a lower risk of stigma/discrimination (OR: 0.61, 95%CI: 0.37–0.98).
Sensitivity analyses were conducted to assess the factors that remained associated with “repeated stigma/discrimination” and with “diverse stigma/discrimination” are shown in Table 3. Awareness of the adolescent's own HIV status (OR: 3.55, 95%CI: 1.30–12.6) was also associated with experience of “diverse stigma/discrimination.”
All caregivers who reported experiences of stigma/discrimination toward their adolescents (N = 212) provided comments. In addition, 5 caregivers provided comments related to the fear of discrimination without having experienced it, and finally 9 caregivers reported discrimination from siblings (a category not considered separately in the questionnaire).
Inductive analysis of the verbatims identified four main themes of stigma: bullying or moral harassment was reported in 61% of cases, social isolation in 42% of cases, behavioral discrimination in 19% of cases, and public disclosure in 7% of cases (Table 2).
School was the main setting for bullying, where children/adolescents were mistreated by administrative staff teachers or friends. One of the most common forms of bullying was calling children “Pen AIDS,” i.e. “you have AIDS.” Such bullying sometimes led to temporary or permanent voluntary withdrawal from school. For three children who didn't know their HIV status, this was a way of finding out they were HIV-positive. Sometimes the bullying was also related to the health or HIV status of the parents.
Grand-father: “The child said that her friends often bullied her, “Pen AIDS,” so that she refused to go to school for one year.”
Aunt: “When the child was young, his friends always teased him that his parents got HIV and died from AIDS and that it will be the same for him. He came to me and asked what is AIDS?”
Bullying also occurred when children showed visible physical symptoms.
Aunt: “My niece could not go to school because the director said the other parents don't want a child who has skin wounds on her body.
Another major issue raised by caregivers was the social isolation resulting from the children's HIV status. This isolation occurred at school, in the community and even within the family. The main reason given was the fear of infection.
Grand-mother: “The teacher didn't pay attention when my grand-daughter was asking permission to go out of the classroom in order to take her medication. Also when she was sick at school, she had to manage to call home on her own”
Mother: “The school director refused to enroll my son, because in that year, his own child was attending the school and he feared that they may be close”
Mother: “In kinder-garden, nobody dare to sit near my daughter”
In the community, parents of other children or neighbors also tended to forbid their children from playing with children who were known to be living with HIV.
Grand-mother: “My grand-daughter was always told that as having AIDS she was not allowed to play with other children at school and in the community”
Finally, in the family context, some comments were made about discrimination due to fear of contamination.
Aunt: “Some cousins were disgusted and feared that my niece might transmit the disease to other children. They warned her not to get close to other children”
Another common discrimination behavior was to avoid sharing the same food or water with children living with HIV, whether at school, in the children's home or in any other place where the children might be invited.
Grand-mother: “My grand-daughter went to other people's house and ask them to drink water, but they refused”
Beyond not sharing food or water, some children were unable to access services or help because of their status.
Grand-mother: “Between age 8 and 9 years, when my grand-son was going for a haircut, the barber refused to do”
Some caregivers commented on how the child's HIV status was disclosed to the community.
Father: “I was angry at the teacher because she (the teacher) told the students that my child had HIV infection in front of the whole classroom”
Aunt: “The neighbor said that my niece had AIDS, and asked why she wasn't dying already. We both felt angry”
Our study showed that, from the perspective of their caregivers, almost half of adolescents living with perinatal HIV had experienced stigma or discrimination. This occurred mainly at school, more often in the north-east region, was more likely to affect those perceived as having an intellectual disability, those in conflict with their caregivers, those with a BMI < 18.5, and those whose caregivers were members of support groups. It was not significantly associated with other factors such as gender, age, orphan status, health status including virological or immunological status, self-awareness of HIV status, or adherence to ART.
In our study, 19% of caregivers reported that their child's HIV status was not known to the community. In the Northern Thailand study of adolescents living with perinatal HIV followed in Chiang Mai University hospital, about 40% of caregivers reported keeping their adolescent's HIV status secret, a percentage twice as high as in our study (31). The lack of disclosure in the community is likely related to anticipated stigma (35), as caregivers or adolescents may have chosen not to disclose their status (36). However, they are not always in a position to choose disclosure, as for example, the HIV status of orphans is generally known in the community, with parental deaths suspected to be HIV-related. In addition, people living with HIV who are in the most precarious situation are more likely to apply to the dedicated financial support from the government. As registration is often not confidential, the HIV status is then known in the community. It is difficult to compare our findings with those of other studies conducted in Thailand, as the populations and approaches used to study stigma/discrimination against adolescents are different. Similar to our study, a qualitative study conducted in Bangkok among 33 adolescents and young adults 15–24 years (more than half of whom were infected perinatally) indicates that the educational context was the main setting in which they encountered stigma/discrimination (37). In contrast with the study in Chiang Mai University hospital, where almost half of the caregivers had discrimination attitudes toward their adolescents (31), caregivers in our study reported relatively few (10%) experiences of stigma/discrimination in the family context. It is possible that this frequency is underestimated, as specific questions about discriminatory attitudes in the family were not asked, and that caregivers may not consider these attitudes to be discriminatory. In neighbor Cambodia, similar frequencies of HIV stigma/discrimination were measured, ranging from 32.0 (38) to 43.2% (39). Finally, experiences of stigma/discrimination in the health care setting were almost never reported (< 1%). This contrasts with the situation in the United States, where a study of adolescents and young adults found that 38% had experienced HIV-related stigma/discrimination when accessing sexual health services, particularly women (40).
In our study, the most common expression of stigma/discrimination against children was teasing or bullying, reported by about a quarter of all caregivers. In the Chiang Mai study, 23% of caregivers reported that their adolescents had been teased and 11% bullied at school (31), a similar percentage to our findings. In our study, social isolation was mentioned by almost a fifth of all caregivers and was reinforced in case of physical symptoms. The word “rangkiat,” meaning “disgust,” was often used by caregivers to express how HIV-infected people were perceived by others.
We found that the prevalence of stigma/discrimination was highest in the Northeast region. This is consistent with the results of successive surveys on stigmatizing attitudes toward people living with HIV among the Thai adult population (29, 30), and highlights the need to prioritize this region for interventions.
Our study also shows a strong association between stigma/discrimination and lower intellectual ability among adolescents. In a previous analysis, it was found that adolescents who had experienced stigmatization at school were almost twice as likely to have a disrupted academic trajectory (10). However, it is difficult to distinguish between HIV-related stigma and stigma associated with mental disability. Negative consequences of stigma on mental health have also been documented (41–44). Finally, we found that reports of stigma/discrimination were more frequent when caregivers were members of an HIV support group. Through their participation in these groups, caregivers are better informed about HIV and may be more sensitive to stigma and discrimination. Also, the association between stigma/discrimination, and conflicts with caregivers might indicate resentment toward parents who transmitted the virus perinatally, or toward caregivers who may view them as a burden (45).
We found no difference in the experience of stigma/discrimination according to gender. This is in contrast to findings in adults, where women were more likely to experience stigma/discrimination than men (27). Similarly, unlike in adults, HIV-related stigma/discrimination was not associated with poor adherence (15). In fact, during childhood, adherence depends primarily on the caregivers who provide ART and directly observe its intake (46, 47). There was also no association between stigma/discrimination and the viral load level or CD4 count. It should be noted that the virological and immunological response to ART was very good in both groups. As encouraging results in medical settings are found both in our population and other populations (48), stigma remains a factor that can facilitate the spread of HIV (49). The transition to adulthood remains complex and should be managed in a multidisciplinary way, including psychosocial support (50).
Thailand has developed several interventions to prevent HIV stigmatization based on three building blocks: policy, measurement and implementation (50). Among the results, reducing stigma and discrimination was mentioned as a goal in the National AIDS Strategic Plan (2014–2016) and was high on Thailand priority agenda. In addition, surveillance data was obtained from the general population, healthcare professionals and key-populations. Moreover, participatory interventions and training took place in healthcare facilities. Finally, the United Nations has created a mobile telephone application enabling people to contact HIV services in Bangkok to report stigma or discrimination events and monitor them (51).
Our findings may not be representative of the situation in the country, as most adolescents were recruited from the northern region and were living in family settings. Adolescents living in orphanages may have a different experience of stigma and discrimination. However, our study was conducted on a relatively large sample of adolescents living with perinatal HIV, recruited from 20 hospitals of different sizes across Thailand.
The study was carried out more than 10 years ago, and it is known that, in adults, stigma and discrimination have decreased as a consequence of the widespread use of ART (52). However, the level of stigma/discrimination in perinatally-infected children and adolescents were, to our knowledge, not measured in the last years. In the 5th and 6th Thai National Health Examination Surveys, which measured stigmatizing attitudes toward people living with HIV among adults in the general population, one-fourth and one-fifth, respectively, believed that HIV-infected children should be separate from other children at school (29, 30). However, in the Thailand National Strategic Plan 2017–2030, documented interventions do not mention schools or other settings involving this specific population. Therefore, although the data was collected relatively long ago, describing stigma/discrimination experiences of adolescents born with HIV remains essential to highlighting their specific needs, which must be addressed in Thailand and other contexts, particularly in Africa.
The 46% prevalence of stigma/discrimination obtained from interviews with caregivers is likely to be an underestimate, as children/adolescents do not always report their experiences to their caregivers, and direct testimonies from adolescents were not available. Also, given the frequent change in caregivers due to parental separation or death, the caregiver at the time of the interview may not be aware of past experiences of child stigma or discrimination. However, our approach of interviewing caregivers rather than the adolescents themselves, while reducing the number of reports of stigma/discrimination, respected the fact that some adolescents had not been informed of their HIV status and prevented them from recalling painful events in their lives. Nonetheless, the fact that information was collected from the caregivers might lead to an information bias. This is indicated by the higher odds of perceived stigma when caregivers were members of a support group. The age of the children/adolescents at the time of HIV disclosure in the community and when their stigma/discrimination experiences occurred, as well as internalized self-stigma were not available. A specific Thai internalized HIV-stigma scale for adults was developed in 2023 (53). However, the mixed methods used, with a life-history approach in which the adolescent's life was reconstructed by the caregiver, alongside a qualitative questioning, enabled us to obtain detailed information about stigma/discrimination experiences in childhood and adolescence.
Thanks to the successful implementation of PMTCT, the number of adolescents living with perinatal HIV is decreasing significantly (54) and may no longer be considered a key population. However, as they reach adulthood, they may face the consequences of past discrimination in terms of access to university studies or certain jobs, and may face discrimination at work, in the community or in their romantic life (55). We are currently conducting a follow-up study, TEEWA-2, in which the same young people will be asked directly about their current experiences of stigma/discrimination, as young adults (56).
In its National Strategy to End AIDS 2017–2030, Thailand has committed to reducing HIV-related discrimination by 90% (57), and has outlined measures to promote awareness of HIV, human rights, and sexuality in healthcare settings, the media, and the workplace. However, the strategy does not directly address children and adolescents born with HIV, or include specific interventions in schools or settings involving this population. While Thailand can be considered a success story in its fight against HIV/AIDS, in terms of prevention of sexual transmission, PMTCT, scaling up ART and combating stigma/discrimination among adults (58), our study highlights the vulnerability of children and adolescents for whom community-based and school-based interventions should be targeted.
The raw data supporting this study will be made available upon reasonable request, contingent upon approval by the authors.
This study involving human subjects was approved by the Faculty of Associated Medical Sciences of Chiang Mai University (ref: AF02-014) and by the ethics committees of the participating hospitals when available. The study was conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin and written informed ascent was provided by the adolescents.
• Bhumibol Adulyadej Hospital
• Chiang Dao Hospital
• Chiang Kham Hospital
• Chomthong Hospital
• Hat Yai Hospital
• Kalasin Hospital
• Mae Chan Hospital
• Mae Sai Hospital
• Mahasarakam Hospital
• Nong Khai Hospital
• Phan Hospital
• Phayao Provincial Hospital
• Prapokklao Hospital
• Rayong Hospital
• Samutsakhorn Hospital
• Sanpatong Hospital
AG: Formal analysis, Writing – original draft, Writing – review & editing. WS: Investigation, Writing – review & editing. PJ: Investigation, Writing – review & editing. WC: Investigation, Writing – review & editing. CR: Investigation, Writing – review & editing. MK: Investigation, Writing – review & editing. US: Investigation, Writing – review & editing. SS: Investigation, Writing – review & editing. ST: Investigation, Writing – review & editing. TK: Investigation, Writing – review & editing. SL: Conceptualization, Funding acquisition, Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Sidaction, Grant AI22-1/01855 and OXFAM Great Britain, Grant THAA51, the National Institute for Demographic Studies (Ined), and the Agence Régionale de Santé Ile-de-France (ARS). The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
We would like to thank Julie Pannetier, Aurore Camier, Marc Lallemant and Aboubakari Nambiema for reviewing and providing valuable suggestions to the manuscript. A preprint has been published in July 2024 in preprints.org (59).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. United Nations General Assembly. Political Declaration on HIV/AIDS (Resolution 60/262). (2006). Available at: https://www.unaids.org/sites/default/files/sub_landing/files/20060615_hlm_politicaldeclaration_ares60262_en.pdf (accessed February 26, 2024).
2. UNAIDS. Evidence for eliminating HIV-related stigma and discrimination. (2020). Available at: https://www.unaids.org/sites/default/files/media_asset/eliminating-discrimination-guidance_en.pdf (accessed February 26, 2024).
3. United Nations Agency for International Development (UNAIDS). Protocol for identification of discrimination against people living with HIV. (2000). Available at: https://data.unaids.org/publications/irc-pub01/jc295-protocol_en.pdf (accessed February 26, 2024).
4. Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. (2013) 103:813–21. doi: 10.2105/AJPH.2012.301069
5. Relf MV, L Holzemer W, Holt L, Nyblade L, Ellis Caiola C. A review of the state of the science of HIV and stigma: context, conceptualization, measurement, interventions, gaps, and future priorities. J Assoc Nurses AIDS Care. (2021) 32:392–407. doi: 10.1097/JNC.0000000000000237
6. Cluver L, Orkin M. Cumulative risk and AIDS-orphanhood: interactions of stigma, bullying and poverty on child mental health in South Africa. Soc Sci Med. (2009) 69:1186–93. doi: 10.1016/j.socscimed.2009.07.033
7. Chen C, Wu Q, Zhao J, Zhao G, Li X, Du H, et al. Enacted stigma influences bereavement coping among children orphaned by parental AIDS: a longitudinal study with network analysis. Psychol Res Behav Manag. (2023) 16:4949–58. doi: 10.2147/PRBM.S423707
8. Horsakulchai W, Sermprasartkul T, Sumetchoengprachya P, Chummaneekul P, Rungruang N, Uthis P, et al. Factors associated with internalized HIV-related stigma among people living with HIV in Thailand. AIDS Care. (2024) 10:1452–61. doi: 10.1080/09540121.2024.2308742
9. Lowther K, Selman L, Harding R, Higginson IJ. Experience of persistent psychological symptoms and perceived stigma among people with HIV on antiretroviral therapy (ART): a systematic review. Int J Nurs Stud. (2014) 51:1171–89. doi: 10.1016/j.ijnurstu.2014.01.015
10. Merville O, Puangmala P, Suksawas P, Kliangpiboon W, Keawvilai W, Tunkam C, et al. School trajectory disruption among adolescents living with perinatal HIV receiving antiretroviral treatments: a case-control study in Thailand. BMC Public Health. (2021) 21:189. doi: 10.1186/s12889-021-10189-x
11. Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. (2009) 21:742–53. doi: 10.1080/09540120802511877
12. Kimera E, Vindevogel S, Reynaert D, Justice KM, Rubaihayo J, De Maeyer J, et al. Experiences and effects of HIV-related stigma among youth living with HIV/AIDS in Western Uganda: a photovoice study. PLoS ONE. (2020) 15:e0232359. doi: 10.1371/journal.pone.0232359
13. Brener L, Callander D, Slavin S, de Wit J. Experiences of HIV stigma: the role of visible symptoms, HIV centrality and community attachment for people living with HIV. AIDS Care. (2013) 25:1166–73. doi: 10.1080/09540121.2012.752784
14. Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. (2013) 16(3 Suppl 2):18640. doi: 10.7448/IAS.16.3.18640
15. Xu L, Munir K, Kanabkaew C, Le Coeur S. Factors influencing antiretroviral treatment suboptimal adherence among perinatally HIV-infected adolescents in Thailand. PLoS ONE. (2017) 12:e0172392. doi: 10.1371/journal.pone.0172392
16. Amuri M, Mitchell S, Cockcroft A, Andersson N. Socio-economic status and HIV/AIDS stigma in Tanzania. AIDS Care. (2011) 23:378–82. doi: 10.1080/09540121.2010.507739
17. Wiener LS, Battles HB, Heilman N, Sigelman CK, Pizzo PA. Factors associated with disclosure of diagnosis to children with HIV/AIDS. Pediatr AIDS HIV Infect. (1996) 7:310–24.
18. Robinson A, Cooney A, Fassbender C, McGovern DP. Examining the relationship between HIV-related stigma and the health and wellbeing of children and adolescents living with HIV: a systematic review. AIDS Behav. (2023) 27:3133–49. doi: 10.1007/s10461-023-04034-y
19. Kalichman SC, Sikkema KJ, Somlai A. People living with HIV infection who attend and do not attend support groups: a pilot study of needs, characteristics and experiences. AIDS Care. (1996) 8:589–600. doi: 10.1080/09540129650125542
20. Tzemis D, Forrest JI, Puskas CM, Zhang W, Orchard TR, Palmer AK, et al. Identifying self-perceived HIV-related stigma in a population accessing antiretroviral therapy. AIDS Care. (2013) 25:95–102. doi: 10.1080/09540121.2012.687809
21. Rayanakorn A, Ong-Artborirak P, Ademi Z, Chariyalertsak S. Predictors of stigma and health-related quality of life among people living with HIV in Northern Thailand. AIDS Patient Care STDS. (2022) 36:186–93. doi: 10.1089/apc.2022.0035
22. Chem ED, Ferry A, Seeley J, Weiss HA, Simms V. Health-related needs reported by adolescents living with HIV and receiving antiretroviral therapy in sub-Saharan Africa: a systematic literature review. J Int AIDS Soc. (2022) 25:e25921. doi: 10.1002/jia2.25921
23. Weniger BG, Limpakarnjanarat K, Ungchusak K, Thanprasertsuk S, Choopanya K, Vanichseni S, et al. The epidemiology of HIV infection and AIDS in Thailand. AIDS. (1991) 5(Suppl 2):S71–85. Erratum in: AIDS (1993) 7:following 147. doi: 10.1097/00002030-199101001-00011
24. National Health Statistical Office (NHSO). National Statistical Office (NSO) the 2010 Population and Housing Census (2010).
25. UNAIDS. Thailand country factsheet. (2022). Available at: https://www.unaids.org/en/regionscountries/countries/thailand (accessed February 26, 2024).
26. Lolekha R, Boonsuk S, Plipat T, Martin M, Tonputsa C, Punsuwan N, et al. Elimination of mother-to-child transmission of HIV - Thailand. MMWR Morb Mortal Wkly Rep. (2016) 65:562–6. doi: 10.15585/mmwr.mm6522a2
27. Pannetier J, Lelièvre E, Le Cœur S. HIV-related stigma experiences: understanding gender disparities in Thailand. AIDS Care. (2016) 28:170–8. doi: 10.1080/09540121.2015.1096888
28. Zhang H. Intersectional stigma and coping strategies of single mothers living with HIV in Thailand. Cult Health Sex. (2023) 25:336–51. doi: 10.1080/13691058.2022.2042393
29. Srithanaviboonchai K, Chariyalertsak S, Nontarak J, Assanangkornchai S, Kessomboon P, Putwatana P, et al. Stigmatizing attitudes toward people living with HIV among general adult Thai population: results from the 5th Thai National Health Examination Survey (NHES). PLoS ONE. (2017) 12:e0187231. doi: 10.1371/journal.pone.0187231
30. Chautrakarn S, Ong-Artborirak P, Naksen W, Thongprachum A, Wungrath J, Chariyalertsak S, et al. Stigmatizing and discriminatory attitudes toward people living with HIV/AIDS (PLWHA) among general adult population: the results from the 6th Thai National Health Examination Survey (NHES VI). J Glob Health. (2023) 13:04006. doi: 10.7189/jogh.13.04006
31. Washington CH, Oberdorfer P. Perceived and experienced stigma and discrimination among caregivers of perinatally HIV-infected adolescents in Thailand. J Ther Manag HIV Infect. (2013) 1:63–8. doi: 10.12970/2309-0529.2013.01.02.5
32. Washington CH, Oberdorfer P. Stigma and discrimination among perinatally HIV-infected adolescents receiving HAART in Thailand. Int J Sociol Study. (2014) 2:33–41. Available at: https://www.academia.edu/27933803/Stigma_and_Discrimination_among_Perinatally_HIV_Infected_Adolescents_Receiving_HAART_in_Thailand
33. Le Coeur S, Lelièvre E, Kanabkaew C, Sirirungsi W. A survey of adolescents born with HIV: the TEEWA project in Thailand. Population. (2017) 72:333–56. doi: 10.3917/popu.1702.0343
34. Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. (2008) 3:17. doi: 10.1186/1751-0473-3-17
35. Aurpibul L, Tangmunkongvorakul A, Detsakunathiwatchara C, Masurin S, Srita A, Meeart P, et al. Social effects of HIV disclosure, an ongoing challenge in young adults living with perinatal HIV: a qualitative study. Front Public Health. (2023) 11:1150419. doi: 10.3389/fpubh.2023.1150419
36. Hogwood J, Campbell T, Butler S. I wish I could tell you but I can't: adolescents with perinatally acquired HIV and their dilemmas around self-disclosure. Clin Child Psychol Psychiatry. (2013) 18:44–60. doi: 10.1177/1359104511433195
37. Mathew RS, Boonsuk P, Dandu M, Sohn AH. Experiences with stigma and discrimination among adolescents and young adults living with HIV in Bangkok, Thailand. AIDS Care. (2019) 32:530–5. doi: 10.1080/09540121.2019.1679707
38. Toth G, Mburu G, Tuot S, Khol V, Ngin C, Chhoun P, et al. Social-support needs among adolescents living with HIV in transition from pediatric to adult care in Cambodia: findings from a cross-sectional study. AIDS Res Ther. (2018) 15:8. doi: 10.1186/s12981-018-0195-x
39. Barennes H, Tat S, Reinharz D, Vibol U. Perceived stigma by children on antiretroviral treatment in Cambodia. BMC Pediatr. (2014) 14:300. doi: 10.1186/s12887-014-0300-9
40. Fair CD, Berk M. Provider perceptions of stigma and discrimination experienced by adolescents and young adults with pHiV while accessing sexual and reproductive health care. AIDS Care. (2018) 30:178–81. doi: 10.1080/09540121.2017.1344349
41. Thai TT, Tran VB, Thi Nguyen NB, Bui HHT. HIV-related stigma, symptoms of depression and their association with suicidal ideation among people living with HIV in Ho Chi Minh City, Vietnam. Psychol Health Med. (2023) 28:1263–74. doi: 10.1080/13548506.2022.2067342
42. Aurpibul L, Kosalaraksa P, Kawichai S, Lumbiganon P, Ounchanum P, Natalie Songtaweesin W, et al. Alcohol use, suicidality and virologic non-suppression among young adults with perinatally acquired HIV in Thailand: a cross-sectional study. J Int AIDS Soc. (2023) 26:e26064. doi: 10.1002/jia2.26064
43. Lewis JV, Abramowitz S, Koenig LJ, Chandwani S, Orban L. Negative life events and depression in adolescents with HIV: a stress and coping analysis. AIDS Care. (2015) 27:1265–74. doi: 10.1080/09540121.2015.1050984
44. Aurpibul L, Sophonphan J, Malee K, Kerr SJ, Sun LP, Ounchanum P, et al. PREDICT Resilience study. HIV-related enacted stigma and increase frequency of depressive symptoms among Thai and Cambodian adolescents and young adults with perinatal HIV. Int J STD AIDS. (2021) 32:246–56. doi: 10.1177/0956462420960602
45. Rutakumwa R, Zalwango F, Richards E, Seeley J. Exploring the care relationship between grandparents/older carers and children infected with HIV in South-Western Uganda: implications for care for both the children and their older carers. Int J Environ Res Public Health. (2015) 12:2120–34. doi: 10.3390/ijerph120202120
46. Aurpibul L, Detsakunathiwatchara C, Khampun R, Wongnum N, Chotecharoentanan T, Sudjaritruk T. Quality of life and HIV adherence self-efficacy in adolescents and young adults living with perinatal HIV in Chiang Mai, Thailand. AIDS Care. (2023) 35:406–10. doi: 10.1080/09540121.2022.2075537
47. Fair CD, Jutras A. “I have hope, but I'm worried”: perspectives on parenting adolescents and young adults living with perinatally-acquired HIV. Fam Syst Health. (2022) 40:232–8. doi: 10.1037/fsh0000676
48. Peretti-Watel P, Spire B, Obadia Y, Moatti JP, VESPA Group. Discrimination against HIV-infected people and the spread of HIV: some evidence from France. PLoS ONE. (2007) 2:e411. doi: 10.1371/journal.pone.0000411
49. Mofenson LM, Cotton MF. The challenges of success: adolescents with perinatal HIV infection. J Int AIDS Soc. (2013) 16:18650. doi: 10.7448/IAS.16.1.18650
50. Siraprapasiri T, Srithanaviboonchai K, Chantcharas P, Suwanphatthana N, Ongwandee S, Khemngern P, et al. Integration and scale-up of efforts to measure and reduce HIV-related stigma: the experience of Thailand. AIDS. (2020) 34 Suppl 1:S103–14. doi: 10.1097/QAD.0000000000002586
51. UN Sustainable Development Group. An app to monitor HIV services in Bangkok. Action 2030 Blog (2015). Available at: https://unsdg.un.org/latest/blog/app-monitor-hiv-services-bangkok (accessed September 11, 2024).
52. Dollfus C, Le Chenadec J, Faye A, Blanche S, Briand N, Rouzioux C, et al. Long-Term outcomes in adolescents perinatally infected with HIV-1 and followed up since birth in the French Perinatal Cohort (EPF/ANRS CO10). Clin Infect Dis. (2010) 51:214–24. doi: 10.1086/653674
53. Uthis P, Suktrakul S, Wiwatwongwana R, Tangmunkongvorakul A, Sripan P, Srithanaviboonchai K. The Thai Internalized HIV-related stigma scale. Front Psychol. (2023) 14:1134648. doi: 10.3389/fpsyg.2023.1134648
54. Desmonde S, Lolekha R, Costantini S, Siraprapasiri T, Frank S, Bakkali T, et al. A focused multi-state model to estimate the pediatric and adolescent HIV epidemic in Thailand, 2005-2025. PLoS ONE. (2022) 17:e0276330. doi: 10.1371/journal.pone.0276330
55. Fernet M, Wong K, Richard ME, Otis J, Lévy JJ, Lapointe N, et al. Romantic relationships and sexual activities of the first generation of youth living with HIV since birth. AIDS Care. (2011) 23:393–400. doi: 10.1080/09540121.2010.516332
56. Le Coeur S, Hoang Ngoc Minh P, Sriphetcharawut S, Jongpaijitsakul P, Lallemant M, Puangmala P. The Teens Living with Antiretrovirals (TEEWA) study group. Mortality among adolescents living with perinatal HIV (APHIV) receiving antiretroviral therapy (ART): the Teens Living with Antiretrovirals (TEEWA) study in Thailand. In: 23rd Intl AIDS Conference (Aids 2020), 6-10 July 2020. San Francisco, CA (2020).
57. National Committee for the Prevention and Response to AIDS. Thailand National Strategy to End AIDS 2017-2030. (2017).
58. Harris J, Thaiprayoon S. Common factors in HIV/AIDS prevention success: lessons from Thailand. BMC Health Serv Res. (2022) 22:1487. doi: 10.1186/s12913-022-08786-6
Keywords: perinatal HIV, stigmatization, discrimination, Thailand, bullying, adolescent
Citation: Geoffroy A, Sirirungsi W, Jongpaijitsakul P, Chamjamrat W, Ruklao C, Kongka M, Sukhaphan U, Sathan S, Thina S, Khayanchoomnoom T and Le Coeur S (2025) Stigma and discrimination against adolescents living with perinatal HIV in Thailand: caregivers' perceptions. Front. Public Health 13:1535004. doi: 10.3389/fpubh.2025.1535004
Received: 26 November 2024; Accepted: 06 February 2025;
Published: 05 March 2025.
Edited by:
Renaud Becquet, Bordeaux Population Health Research Centre (Inserm, IRD, Bordeaux University), FranceReviewed by:
Philippe Msellati, PACCI, Côte d'IvoireCopyright © 2025 Geoffroy, Sirirungsi, Jongpaijitsakul, Chamjamrat, Ruklao, Kongka, Sukhaphan, Sathan, Thina, Khayanchoomnoom and Le Coeur. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Audrey Geoffroy, YXVkcmV5anVsaWEuZ2VvZmZyb3lAeWFob28uY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.