
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 18 February 2025
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1534176
 Mohammed S. Alharthi1*
Mohammed S. Alharthi1* Abdullah A. Alshehri1
Abdullah A. Alshehri1 Fahad H. Baali1
Fahad H. Baali1 Nawaf Awd Altuwairqi1
Nawaf Awd Altuwairqi1 Meshari Hassan Altalhi1
Meshari Hassan Altalhi1 Rayan Azib Almalki1
Rayan Azib Almalki1 Meshal Khalid Aljuaid1
Meshal Khalid Aljuaid1 Majed A. Algarni1
Majed A. Algarni1 Mohmmed S. Alzahrani1
Mohmmed S. Alzahrani1 Nasser M. Alorfi2
Nasser M. Alorfi2 Wadia S. Alruqayb1
Wadia S. Alruqayb1Background: Seasonal influenza vaccination is essential for reducing the risk and impact of influenza. Makkah region in Saudi Arabia, a destination for millions of pilgrims during Hajj and Umrah, presents a unique context for this study. Therefore, this research investigates the prevalence and influencing factors of influenza vaccine uptake among the public in Makkah region, Saudi Arabia.
Method: This cross-sectional study was conducted in Saudi Arabia between February and June 2024. The main researcher developed the questionnaire, which was reviewed by five academics and then piloted with 20 individuals for validation. An online questionnaire was used, targeting residents aged 18 and over with internet access. A snowball sampling method was applied. Data were collected via Google Forms and analyzed using SPSS version 26, employing descriptive statistics such as frequencies, percentages, and means.
Results: The total number of respondents is 450 participants, with a response rate of 4.5%. Most respondents were male (71.1%) and aged between 18 and 30 years (44.5%). Education levels varied, with 57.5% holding a bachelor’s degree. Vaccination uptake showed 65.1% had received the vaccine, with 31.1% confident it is safe. Despite this, 58.8% did not get vaccinated this season. Confidence in the vaccine’s effectiveness was 59.5%, though 41.2% reported breakthrough infections. Accessibility was generally rated easy (57.7%). Social pressure (17.4%), trust in health institutions (36.9%), and COVID-19 concerns (36.7%) significantly influenced vaccination decisions. The likelihood of vaccination next season displayed polarized views.
Conclusion: This study provides significant insights about vaccine hesitancy that may inform future research endeavors and practical applications. Understanding the various factors that impact the adoption of influenza vaccines offers valuable insights for developing targeted interventions and public health policies to improve vaccination rates. This study enhances theoretical understanding and practical strategies to encourage influenza vaccination, thereby improving public health initiatives in the area and beyond.
Seasonal influenza (flu) is a significant global public health concern, contributing to annual morbidity and mortality (1). Each year, particularly during the winter, seasonal influenza affects up to one billion individuals worldwide, with most cases being mild. However, the World Health Organization (WHO) estimates that 3 to 5 million cases develop into severe illness, leading to 290,000–650,000 respiratory deaths annually (2). The burden of influenza extends beyond individual health, imposing economic and healthcare system challenges worldwide. In Saudi Arabia, the incidence of influenza-like illnesses (ILIs) and severe acute respiratory infections (SARIs) has increased significantly, with a notable spike in 2022 compared to previous years (3). The epidemiology of influenza in the Middle East and North Africa shows that influenza A and B account for 76.5 and 23.5% of cases, respectively, with influenza A being dominant in 86.8% of seasons (4). While most countries exhibit seasonality patterns similar to the Northern Hemisphere, regions such as the Arabian Peninsula experience secondary peaks, mainly due to large-scale population movements. Despite the availability of influenza vaccines, uptake remains suboptimal globally. A 2021 study examining demographic and educational influences on influenza vaccine awareness in Saudi Arabia found that 50% of surveyed adults were vaccinated. Meanwhile, 42% exhibited vaccine hesitancy due to a lack of awareness and safety concerns (5). Vaccination is widely recognized as an effective preventive measure, reducing hospitalization and mortality rates (6, 7). However, vaccination coverage varies significantly across geographic locations and demographic groups, with disparities influenced by socioeconomic status, cultural beliefs, and misinformation (8, 9). Religious and cultural perceptions further impact vaccine uptake, with some individuals considering vaccinations unnecessary or unnatural interventions (10). A global study on vaccine hesitancy identified concerns about side effects, perceived low risk of infection, and distrust in vaccine manufacturers as primary barriers to vaccine acceptance (11). In Saudi Arabia, factors such as public trust in health institutions, accessibility, and social influence have significantly affected vaccination decisions (12). Makkah presents a unique epidemiological setting, as it hosts millions of international visitors annually for Hajj and Umrah, creating an ideal environment for the rapid transmission of respiratory illnesses. Given this high-risk context, ensuring adequate influenza vaccine coverage among residents and visitors is a public health priority (13). While previous research has explored vaccine acceptance in diverse global populations, there remains a notable gap in understanding the attitudes and behaviors of individuals in Makkah regarding seasonal influenza vaccination. This cross-sectional study aims to address this gap by investigating public perceptions, uptake rates, and key factors influencing influenza vaccination in Makkah. By identifying barriers and facilitators to vaccine uptake, the findings will contribute to developing targeted public health interventions aimed at improving vaccination coverage and reducing the burden of seasonal influenza in this high-density region.
The study employed a cross-sectional design targeting the adult population in Makkah region of Saudi Arabia. An online questionnaire was distributed among the population. It was conducted between February 2024 and June 2024. The inclusion criteria involved males and females 18 years old and over and participants with internet access who could participate in this study. The exclusion criteria were individuals outside Makkah region, those under 18 years old, and those without internet access.
The main researcher (MA) developed the questionnaire based on the study’s aim and objectives after reviewing the literature of similar studies (14–17). Five academics critically assessed the questionnaire for accuracy, relevance, and appropriateness. The questionnaire consists of five parts with 16 closed-ended questions. These include demographics, vaccine knowledge, attitudes, vaccination practices, and factors influencing vaccine uptake. The questions cover the respondent’s demographics, knowledge about the influenza vaccine, attitudes toward its safety and effectiveness, personal vaccination practices, and factors influencing their decision to get vaccinated. The questionnaire included items assessing participants’ knowledge about the influenza vaccine, covering aspects such as its purpose, effectiveness, and recommended groups for vaccination. These items were designed to provide insight into respondents’ awareness levels. The findings related to knowledge are presented in the results section. Additionally, reliability analysis demonstrated a Cronbach’s Alpha of 0.766, reflecting an acceptable level of internal consistency. When computed based on standardized items, Cronbach’s Alpha slightly adjusted to 0.761, indicating a stable and consistent measurement scale.
The study adopted a snowballing sampling technique to maximize the number of participants. The sample size was determined using the Cochrane sample size formula: n = Z2(1 − p)/d2. Here, n is the sample size, Z is the critical value for a 95% confidence interval, p is the anticipated proportion (50%), and d is the margin of error (set at 0.05). The minimum sample size was 384, but the researchers targeted 450 respondents to account for potential non-response.
The response rate was estimated by dividing the number of completed responses by the approximate number of individuals who received or had access to the survey link. Since the survey was distributed via multiple online platforms, including social media and direct messaging, the denominator was approximated based on platform reach metrics and engagement data. The response rate was calculated as: (Response Rate = (Total Completed Responses / Estimated Recipients) × 100). Although estimating the exact number of recipients is challenging, this method reasonably approximates participation.
To ensure validity, the questionnaire was piloted with 20 individuals from diverse demographics, such as age and education level. The piloted results were not included in the final analysis. The questionnaire was distributed via social media platforms like X, WhatsApp, and Telegram.
The data was collected through an online questionnaire using Google Forms (which is compliant with the General Data Protection Regulation (GDPR)). They were entered into Statistical Package for the Social Sciences (SPSS) version 26 to analyze the basic features of the collected data. Descriptive analysis, including frequencies with percentages and means, was performed. Consent was obtained at the beginning of the questionnaire. In addition to descriptive statistics, Pearson correlation analysis was performed to examine the relationships between the likelihood of receiving the flu vaccine and influencing factors. The correlation coefficients (r) and corresponding p-values were used to assess the strength and significance of the relationships between variables. The factors analyzed included trust in vaccine safety, trust in efficacy, accessibility, peer pressure, trust in information, and awareness. These analyses aimed to identify key influencing factors associated with flu vaccine uptake within the study population.
Ethical approval was obtained from the Taif University Ethical Committee (application number 45–283). Key ethical considerations included confidentiality and informed consent. Participants were informed about the study’s purpose, procedures, risks, and benefits. Researchers ensured participants’ privacy by protecting their identity and sensitive information.
The total number of respondents is 450, with a response rate of 4.5%. Table 1 shows the demographic characteristics of the respondents, which indicate a higher proportion of males (71.1%) than females (28.9%). The age distribution shows that the largest group is aged 18–30 years (44.5%), followed by those aged 41–50 years (19.9%), 51–60 years (19.7%), and 31–40 years (12.3%). Educational attainment among the respondents is primarily at the bachelor’s degree level (57.5%), with 12.3% possessing postgraduate qualifications, 22.4% having completed high school or an equivalent, and 7.8% having less than a high school education. Employment status reveals that 47.2% of the respondents were employed, 32.9% were students, 12.3% were retired, and 7.4% were unemployed.
A total of 450 participants completed the questionnaire, yielding a response rate of 4.5%. While the survey was widely distributed online, participation remained limited, reflecting possible challenges in engagement and outreach effectiveness.
A pilot study was conducted with 20 participants to evaluate the questionnaire’s clarity, comprehensibility, and reliability before administering it to the main study population. The participants included 12 males (60%) and eight females (40%) aged 18 to 60. The majority (55%) were aged between 18 and 30 years. Educational backgrounds varied, with 50% holding a bachelor’s degree, 30% having completed high school, and 20% possessing postgraduate qualifications. Regarding employment status, 45% were employed, 35% were students, and 20% were unemployed. The participants provided valuable feedback regarding the wording and structure of the questionnaire. Minor adjustments were made to three questions to enhance clarity and eliminate ambiguity, ensuring a better understanding of the survey items. The pilot study results were not included in the final data analysis but were instrumental in refining the questionnaire to enhance its validity and reliability. No significant issues were reported, confirming the appropriateness of the questionnaire for the main study.
Table 2 shows that participants’ knowledge of the seasonal influenza vaccine varies. 62.5% (n = 281) correctly identified that the vaccine is recommended annually for high-risk populations, including older adults, pregnant women, and individuals with chronic diseases. However, 27.4% (n = 123) were unsure about the recommended frequency, and 10.1% (n = 46) incorrectly believed that one dose in a lifetime is sufficient. Regarding vaccine effectiveness, 64.7% (n = 291) correctly stated that the vaccine reduces, but does not entirely prevent, influenza infections. In contrast, 18.2% (n = 82) believed the vaccine completely prevents flu, while 17.1% (n = 77) were uncertain. Additionally, 55.8% (n = 251) correctly recognized that the vaccine does not cause influenza, but 28.5% (n = 128) mistakenly believed that receiving the vaccine could lead to flu infection, highlighting a common misconception.
Table 3 illustrates respondents’ attitudes toward the seasonal influenza vaccine and their vaccination practices. Most participants (65.1%) reported receiving the vaccine at least once, with 19.5% receiving it occasionally and 18.8% annually. However, a substantial proportion (58.8%) did not receive the influenza vaccine during the most recent season, indicating potential barriers to uptake despite largely positive attitudes toward vaccine safety and efficacy. Confidence in vaccine safety was generally high, with 31.1% being very confident and 24.2% somewhat confident, while 28.9% remained neutral. A smaller percentage expressed concerns about vaccine safety, with 11.2% somewhat concerned and 4.7% very concerned. These findings highlight the gap between positive perceptions of vaccine safety and actual uptake rates, suggesting that additional factors, such as accessibility, misconceptions, or external influences, may play a role in vaccination behavior.
Table 4 shows that while 59.5% of respondents are confident in the effectiveness of the seasonal influenza vaccine, 41.2% reported breakthrough infections. Among those, 27.2% gained confidence due to the rarity of such cases, 19.6% slightly lost confidence, 7.1% significantly lost confidence, and 46.2% remained unaffected.
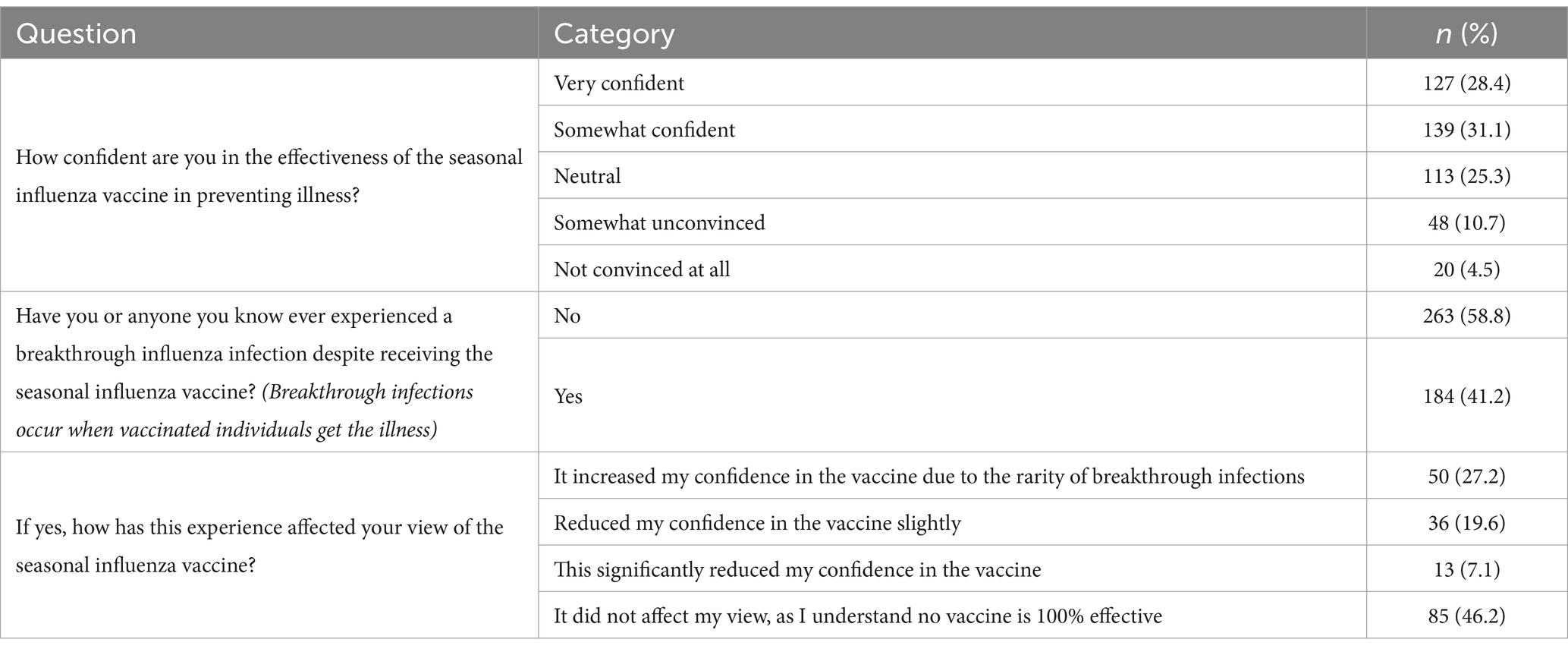
Table 4. Respondents’ responses on confidence and experiences with seasonal influenza vaccine effectiveness.
The accessibility and convenience of seasonal influenza vaccination services in the community vary among respondents. A majority, 258 (57.7%), find the services easy to access. In contrast, 4 (0.9%) respondents consider them very difficult to access, and 1 (0.2%) is unaware of the method to access these services. Additionally, 47 (10.5%) respondents feel neutral about the accessibility, while 21 (4.7%) find it somewhat difficult, and 116 (26%) believe the services are slightly accessible.
Table 5 shows a multifaceted influence on attitudes toward the seasonal influenza vaccine. Social pressure from peers is varied, with the highest proportion of respondents (30%) feeling neutral, 17.4% experiencing strong encouragement, and 14.5% encountering strong discouragement. Trust in health institution-provided information is significant, with 36.9% expressing complete trust and 32% moderate trust. Awareness regarding the vaccine’s importance is high, with 36.7% being very aware and 33.6% somewhat aware. The COVID-19 pandemic has notably impacted vaccination intentions, with 36.7% of respondents reporting an increased desire to vaccinate due to exposure concerns, while 36.2% indicated their decision was not significantly affected.
The chart below illustrates the respondents’ intentions on a scale from 1 to 10. The data reveals a significant inclination toward both extremes, with 20.4% of respondents being very unlikely (1) and 23% being very likely (10) to get the vaccine. Intermediate levels show varying degrees of uncertainty or moderate likelihood, with notable peaks at 5 (14.1%) and lower percentages for other values. This distribution highlights an attitude toward vaccination, with a considerable portion of the population either strongly favoring or against receiving the influenza vaccine next season (Figure 1).
Table 6 demonstrates significant positive correlations between the likelihood of receiving the flu vaccine and factors such as trust in safety, trust in efficacy, peer pressure; trust in information, and awareness, with all associated p-values indicating statistical significance (p < 0.001). Conversely, accessibility did not exhibit a statistically significant relationship with vaccine uptake. p-value for the likelihood of receiving the flu vaccine is “N/A” because it represents the dependent variable, which inherently correlates perfectly (r = 1.0) with itself, rendering a significance test inapplicable. These results underscore the importance of trust and awareness as key influencing factors associated with flu vaccine uptake.
The primary findings from this cross-sectional study reveal significant insights into the public perception and uptake of the seasonal influenza vaccine in Makkah region of Saudi Arabia. The study highlights a notable male dominance among respondents, with the majority being young adults. Despite a generally positive attitude toward the influenza vaccine, a significant portion of respondents did not receive the vaccine this season, indicating potential barriers to vaccine uptake. These barriers may include misconceptions about vaccine effectiveness and concerns about breakthrough infections, which many participants reported. The study underscores the importance of addressing these barriers through targeted public health interventions and educational campaigns. Furthermore, the study identifies key factors influencing vaccination decisions, such as social pressure, trust in health institutions, and concerns related to the COVID-19 pandemic. Social influence from peers and family, along with trust in the information provided by health institutions, plays a crucial role in shaping individuals’ attitudes toward vaccination. The heightened awareness and increased desire to vaccinate due to COVID-19 concerns present an opportunity to leverage this awareness for promoting influenza vaccination. These findings suggest that enhancing trust and leveraging social networks can significantly improve vaccination rates. Public health strategies should focus on clear communication about vaccine safety and efficacy and improving the accessibility of vaccination services to address the population’s diverse needs in Makkah region.
The findings from this cross-sectional study provide a comprehensive understanding of the demographic characteristics and attitudes toward influenza vaccination in Makkah region. The age distribution, with a significant proportion of respondents aged 18–30 years (44.5%), suggests that younger adults are more engaged in health questionnaires, possibly due to higher levels of education or greater access to digital platforms. Educational attainment plays a crucial role in health behavior, and the high percentage of respondents holding a bachelor’s degree (57.5%) indicates that educated individuals may be more aware of the benefits of vaccination. However, the finding that 58.8% of respondents did not receive the influenza vaccine this season despite a generally positive attitude toward its safety and effectiveness highlights the presence of barriers to vaccination that go beyond education and awareness. One of the key insights from this study is the moderate level of confidence in the vaccine’s effectiveness (59.5%) and the significant number of breakthrough infections reported (41.2%). This suggests that while there is general trust in the vaccine, experiences of breakthrough infections may undermine confidence. An important consideration is that these infections are often self-diagnosed, making it difficult to prove their validity, as most people need help distinguishing between the common cold and influenza. Public health campaigns need to address these concerns by providing precise and accurate information about the expected efficacy of the vaccine and the normalcy of breakthrough infections due to the virus’s mutability. Social pressure and trust in health institutions emerged as significant factors influencing vaccination decisions. This underscores the importance of community and familial influence on health behaviors. Public health initiatives should consider involving community leaders and trusted figures to advocate for vaccination, thereby leveraging social networks to improve vaccine uptake. Trust in health institutions (with 36.9% expressing complete trust) indicates that efforts to enhance transparency and communication from these bodies can positively influence vaccination rates. Another critical finding is the influence of the COVID-19 pandemic on vaccination decisions. The increased desire to vaccinate due to COVID-19 (36.7%) indicates that the pandemic has raised awareness about the importance of vaccination in preventing respiratory illnesses. This raised awareness can be harnessed to promote influenza vaccination and other routine immunizations that may have been neglected during the pandemic. This result is aligned with a systematic review published in 2022, which reported that the COVID-19 pandemic has significantly boosted the intention to vaccinate against influenza worldwide. Analysis of 27 studies with 39,193 participants revealed a 50% increase in vaccination intention for the 2020/21 season compared to pre-COVID-19 rates. This trend was consistent across age, gender, and occupation. Key factors driving this increase include historical vaccine acceptance and perceptions of influenza severity and vaccine safety. The pandemic presents a unique opportunity to promote influenza vaccination and reduce vaccine hesitancy (18). A study among healthcare workers in Saudi Arabia found that those who perceived a greater negative impact from the COVID-19 pandemic were 40% more likely to receive the influenza vaccine (19). Additionally, research in Jeddah, Saudi Arabia, indicated that the COVID-19 pandemic had little effect on individuals’ decisions to receive the influenza vaccine, suggesting that other factors may play a more significant role in vaccination uptake (20). Accessibility to vaccination services was generally rated as easy (57.7%), yet a significant portion of the population did not find it easy to access these services. This indicates a need for more widespread and convenient vaccination locations and enhanced communication about where and how to get vaccinated. This study’s findings on influenza vaccine uptake and hesitancy align with trends in Saudi Arabia and the broader Middle East. Prior research in Riyadh has reported similar vaccination rates and hesitancy levels, influenced by misconceptions about vaccine safety, perceived effectiveness, and social influence (21). Studies in other Gulf countries, including the UAE, Kuwait, and Oman, have reported varying vaccination rates among healthcare workers, with 24.7% in the UAE, 67.2% in Kuwait, and 46.4% in Oman. The primary motivator for vaccination was self-protection (59%), while the most common barrier was a lack of time (31.8%). Other factors influencing vaccine hesitancy included unawareness of vaccine availability (29.4%), vaccine unavailability (25.4%), doubts about efficacy (24.9%), lack of information about importance (20.1%), and concerns about side effects (17.3%) (22). Educational attainment is crucial in health behavior, particularly regarding vaccine acceptance. A 2013 study in Bangkok found that health education significantly increased influenza vaccine acceptance among older adults, particularly those with lower education levels and no prior vaccination history. After targeted educational interventions, acceptance rates rose from 83.3 to 92.6% (23). However, this trend was not observed in our study, likely due to Makkah’s unique demographic and cultural context, where a substantial proportion of the population is already aware of the potential spread of influenza during Hajj and Umrah. While the Bangkok study was referenced due to its structured health education intervention, it is essential to acknowledge that more regionally relevant studies should also be compared. The findings in Makkah emphasize the importance of addressing vaccine misconceptions and enhancing public trust. Given the region’s large influx of visitors during Hajj and Umrah, targeted vaccination campaigns focusing on high-risk populations and leveraging healthcare professionals as trusted sources of information may improve uptake. Comparative analysis with global trends underscores the need for more structured awareness programs, integrating lessons from countries with successful vaccination strategies (13). Given the region’s large influx of visitors during Hajj (pilgrim) and Umrah, Makkah presents a unique context where high population density and international travel increase the risk of influenza transmission. This reinforces the importance of vaccination campaigns in reducing disease burden in such an environment. The unique setting of Makkah requires targeted public health strategies that prioritize accessibility, education, and vaccine advocacy, particularly for high-risk populations such as older adult individuals, those with chronic illnesses, and healthcare workers. Trust in vaccine safety and efficacy emerged as key influencing factors, suggesting that individuals who perceive the vaccine as safe and effective are more likely to receive it. Similarly, the significant associations with peer pressure and trust in information indicate that social influences and reliable communication sources play pivotal roles in shaping vaccination decisions. Awareness was also significantly correlated, highlighting the importance of educational campaigns in improving vaccine uptake. In contrast, accessibility did not show a significant relationship, potentially reflecting that structural barriers to vaccine access may be less pronounced in the studied population or that trust, and awareness exert stronger influences. These findings collectively underscore the need for targeted interventions focusing on building trust, enhancing awareness, and leveraging social influences to improve flu vaccination rates. Overall, the study highlights several areas for intervention to improve influenza vaccination rates in Makkah region. Efforts should focus on addressing misconceptions about vaccine effectiveness, leveraging social and community influences, enhancing trust in health institutions, and improving the accessibility of vaccination services. By addressing these factors and considering the unique dynamics of Makkah region, public health initiatives can more effectively increase vaccination uptake and thereby reduce the prevalence of influenza and its associated complications in Makkah region.
One limitation of the study is the use of a snowballing sampling technique, which may introduce selection bias and limit the generalizability of the findings. Additionally, the reliance on self-reported data could result in response bias. The study’s cross-sectional nature limits the ability to establish causality between the identified factors and vaccination uptake. Moreover, the study did not account for potential confounders such as socioeconomic status, underlying health conditions, and previous vaccination history, which could influence vaccination behavior. The sample size of 450 respondents, while sufficient for meaningful statistical analysis, is relatively smaller compared to other studies conducted on similar topics in Saudi Arabia, where sample sizes often about 1,000 participants (24). While the sample size may limit broader generalizability, it still provides valuable insights into vaccine hesitancy and uptake trends within Makkah region. Future research with a more prominent and representative sample would help strengthen the findings and allow for greater external validity. Despite these limitations, the study comprehensively analyses multiple factors influencing vaccination decisions, offering valuable insights for targeted interventions. Additionally, the focus on Makkah region, with its unique demographic and cultural characteristics, adds a significant contextual understanding to the factors influencing vaccination uptake in this area with a high visitor population.
This study contributes significantly to understanding the factors associated with influenza vaccine uptake in Makkah region. The findings highlight the need for targeted public health initiatives to address barriers to vaccination and reinforce positive attitudes toward the influenza vaccine. In practice, these insights can inform the development of tailored public health campaigns that address specific concerns and leverage social influences and trust in health institutions. For research, this study provides a foundation for further exploration into the factors affecting vaccine uptake in different demographic and geographic contexts. Future research could investigate interventions to improve vaccine confidence and uptake, mainly focusing on addressing breakthrough infections and enhancing communication strategies about vaccine effectiveness.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval was obtained from the Taif university ethical Committee (application number 45-283). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
MAlh: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. FB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Writing – original draft, Writing – review & editing. NAA: Data curation, Formal analysis, Funding acquisition, Resources, Writing – original draft, Writing – review & editing. MHA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Software, Writing – original draft, Writing – review & editing. RA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Software, Writing – original draft, Writing – review & editing. MKA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Software, Writing – original draft, Writing – review & editing. MAA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing. MAlz: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing. NMA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing. WA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was funded by Taif University, Saudi Arabia, Project No. (TU-DSPP-2024-175).
The authors extend their appreciation to Taif University, Saudi Arabia, for supporting this work through project number (TU-DSPP-2024-175).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Dunning, J, Thwaites, RS, and Openshaw, PJM. Seasonal and pandemic influenza: 100 years of progress, still much to learn. Mucosal Immunol. (2020) 13:566–73. doi: 10.1038/s41385-020-0287-5
2. World Health Organization. (2024). The burden of influenza. Available at: https://www.who.int/news-room/feature-stories/detail/the-burden-of-influenza (Accessed (August 08, 2024).
3. Alshahrani, SM, and Zahrani, Y. Prevalence and predictors of seasonal influenza vaccine uptake in Saudi Arabia post COVID-19: a web-based online cross-sectional study. Vaccines. (2023) 11:353. doi: 10.3390/vaccines11020353
4. Caini, S, El-Guerche Séblain, C, Ciblak, MA, and Paget, J. Epidemiology of seasonal influenza in the Middle East and North Africa regions, 2010-2016: circulating influenza A and B viruses and spatial timing of epidemics. Influenza Other Respir Viruses. (2018) 12:344–52. doi: 10.1111/irv.12544
5. Alzeer, AA, Alfantoukh, LA, Theneyan, A, Bin Eid, F, Almangour, TA, Alshememry, AK, et al. The influence of demographics on influenza vaccine awareness and hesitancy among adults visiting educational hospital in Saudi Arabia. Saudi Pharm J. (2021) 29:188–93. doi: 10.1016/j.jsps.2021.01.001
6. Osterholm, MT, Kelley, NS, Sommer, A, and Belongia, EA. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis. (2012) 12:36–44. doi: 10.1016/S1473-3099(11)70295-X
7. Cox, RJ, Brokstad, KA, and Ogra, P. Influenza virus: immunity and vaccination strategies. Comparison of the immune response to inactivated and live, attenuated influenza vaccines. Scand J Immunol. (2004) 59:1–15. doi: 10.1111/j.0300-9475.2004.01382.x
8. Kini, A, Morgan, R, Kuo, H, Shea, P, Shapiro, J, Leng, SX, et al. Differences and disparities in seasonal influenza vaccine, acceptance, adverse reactions, and coverage by age, sex, gender, and race. Vaccine. (2022) 40:1643–54. doi: 10.1016/j.vaccine.2021.04.013
9. Nagata, JM, Hernández-Ramos, I, Kurup, AS, Albrecht, D, Vivas-Torrealba, C, and Franco-Paredes, C. Social determinants of health and seasonal influenza vaccination in adults ≥65 years: a systematic review of qualitative and quantitative data. BMC Public Health. (2013) 13:388. doi: 10.1186/1471-2458-13-388
10. al-Jayyousi, G, Sherbash, MAM, Ali, LAM, el-Heneidy, A, Alhussaini, NWZ, Elhassan, MEA, et al. Factors influencing public attitudes towards COVID-19 vaccination: a scoping review informed by the socio-ecological model. Vaccine. (2021) 9:548. doi: 10.3390/vaccines9060548
11. Nuwarda, RF, Ramzan, I, Weekes, L, and Kayser, V. Vaccine hesitancy: contemporary issues and historical background. Vaccine. (2022) 10:1595. doi: 10.3390/vaccines10101595
12. Al-Tawfiq, JA, Gautret, P, and Memish, ZA. Expected immunizations and health protection for hajj and Umrah 2018 —an overview. Travel Med Infect Dis. (2017) 19:2–7. doi: 10.1016/j.tmaid.2017.10.005
13. Larson, HJ, Jarrett, C, Eckersberger, E, Smith, DMD, and Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. (2014) 32:2150–9. doi: 10.1016/j.vaccine.2014.01.081
14. Delgado-Gallegos, JL, Padilla-Rivas, GR, Zúñiga-Violante, E, Avilés-Rodríguez, G, Arellanos-Soto, D, Gastelum-Arias, LJ, et al. Determinants of COVID-19 vaccine hesitancy: a cross-sectional study on a Mexican population using an online questionnaire (COV-AHQ). Front Public Health. (2021) 9:728690. doi: 10.3389/fpubh.2021.728690/full
15. Shapiro, GK, Tatar, O, Dube, E, Amsel, R, Knauper, B, Naz, A, et al. The vaccine hesitancy scale: psychometric properties and validation. Vaccine. (2018) 36:660–7. doi: 10.1016/j.vaccine.2017.12.043
16. Noronha, V, Abraham, G, Bondili, S, Rajpurohit, A, Menon, R, Gattani, S, et al. COVID-19 vaccine uptake and vaccine hesitancy in Indian patients with cancer: a questionnaire-based survey. Cancer Res Stat Treat. (2021) 4:211–8. doi: 10.4103/crst.crst_138_21
17. Guay, M, Gosselin, V, Petit, G, Baron, G, and Gagneur, A. Determinants of vaccine hesitancy in Quebec: a large population-based survey. Hum Vaccin Immunother. (2019) 15:2527–33. doi: 10.1080/21645515.2019.1603563
18. Kong, G, Lim, NA, Chin, YH, Ng, YPM, and Amin, Z. Effect of COVID-19 pandemic on influenza vaccination intention: a Meta-analysis and systematic review. Vaccines. (2022) 10:606. doi: 10.3390/vaccines10040606
19. Alshagrawi, S. Impact of COVID-19 pandemic on influenza vaccination rate among health care workers. Hum Vaccin Immunother. (2024) 20:284. doi: 10.1080/21645515.2024.2426284
20. Alaa, M, Yasin, HM, Alharbi, HA, Barry, M, and Qashqary, M. The attitude regarding the uptake of influenza vaccine in the COVID-19 era in Jeddah City, Saudi Arabia. J Pure Appl Microbiol. (2024) 18:703–10. doi: 10.22207/JPAM.18.1.60
21. Alhatim, N, Al-Bashaireh, AM, and Alqudah, O. Knowledge, attitude, and practice of seasonal influenza and influenza vaccine immunization among people visiting primary healthcare centers in Riyadh, Saudi Arabia. PLoS One. (2022) 17:e0266440. doi: 10.1371/journal.pone.0266440
22. Abu-Gharbieh, E, Fahmy, S, Rasool, BA, and Khan, S. Influenza vaccination: healthcare workers attitude in three Middle East countries. Int J Med Sci. (2010) 7:319–25. doi: 10.7150/ijms.7.319
23. Worasathit, R, Wattana, W, Okanurak, K, Songthap, A, Dhitavat, J, and Pitisuttithum, P. Health education and factors influencing acceptance of and willingness to pay for influenza vaccination among older adults. BMC Geriatr. (2015) 15:136. doi: 10.1186/s12877-015-0137-6
24. Fayed, AA, al, A, Almanea, LT, Alsweed, NI, Almarzoug, LM, Almuwallad, RI, et al. Willingness to receive the COVID-19 and seasonal influenza vaccines among the Saudi population and vaccine uptake during the initial stage of the National Vaccination Campaign: a cross-sectional survey. Vaccine. (2021) 9:765. doi: 10.3390/vaccines9070765
Keywords: seasonal influenza vaccine, influenza, hesitancy, public, Makkah region, Saudi Arabia
Citation: Alharthi MS, Alshehri AA, Baali FH, Altuwairqi NA, Altalhi MH, Almalki RA, Aljuaid MK, Algarni MA, Alzahrani MS, Alorfi NM and Alruqayb WS (2025) Public perceptions and influencing factors of seasonal influenza vaccine uptake in Makkah region, Saudi Arabia: a cross-sectional study. Front. Public Health. 13:1534176. doi: 10.3389/fpubh.2025.1534176
Received: 28 November 2024; Accepted: 07 February 2025;
Published: 18 February 2025.
Edited by:
Italo F. Angelillo, University of Campania Luigi Vanvitelli, ItalyReviewed by:
ChengChing Liu, Michigan State University, United StatesCopyright © 2025 Alharthi, Alshehri, Baali, Altuwairqi, Altalhi, Almalki, Aljuaid, Algarni, Alzahrani, Alorfi and Alruqayb. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed S. Alharthi, TXMuaGFydGhpQHR1LmVkdS5zYQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.