
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 05 February 2025
Sec. Environmental Health and Exposome
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1526325
This article is part of the Research Topic Human Health Affected by Changing Ecological Environment in the Rapid Urbanization View all 5 articles
Background: Ambient carbon monoxide (CO) exposure has been identified as an emerging environmental risk factor contributing to the progression of pulmonary tuberculosis (PTB). However, the epidemiological evidence remains inconsistent. This study aims to investigate the short-term association between low-level CO exposure and PTB outpatient visits in a developing region.
Methods: We conducted a time-series study utilizing a distributed lag non-linear model (DLNM) combined with mediating effect analysis, based on daily CO and PTB cases from 2011 to 2020 in Ningbo, China.
Results: Among all patients with PTB, a 0.1 mg/m3 increase in CO concentration was associated with an increased risk of PTB outpatient visits in the single-pollutant model, particularly at lag days 2–6. The maximum relative risk (RR) was 1.091 (95%CI, 1.020–1.168, lag 0–2 days). Similarly, the maximum cumulative lag effect of CO exposure was 1.781 (RR = 1.781, 95%CI: 1.157–2.742, lag 0–15 days). Subgroup analysis revealed a significant effect of CO exposure in males (RR = 1.090, 95%CI: 1.009–1.777, lag 0–3 days), females (RR = 1.101, 95%CI: 1.014–1.195, lag 0–3 days), younger individuals (RR = 1.097, 95%CI: 1.022–1.178, lag 0–2 days), and during the warm season (RR = 1.012, 95%CI: 1.002–1.022, lag 0–4 days). Mediation analysis indicated that temperature had an indirect mediating effect on association between CO and PTB (−0.0065, 95%CI: −0.0130 to −0.0004), while air pressure, visibility, and humidity showed no significant mediating effects.
Conclusion: Our findings indicate that ambient CO exposure, even at low levels, has a short-term impact on PTB in developing regions. Temperature plays a partial mediating role in this relationship. Consequently, it is critical to enhance environmental monitoring and early warning systems to effectively address the prevalence of PTB and the delays in health-seeking behavior.
• Short-term and low-level air pollution in developing region has impact on the PTB.
• An increase in CO concentration is related to an increased risk of PTB at lag day 2–6.
• The effect of CO on PTB cases is partially mediated by temperature.
• Climate factors perform mediating role on air pollutants.
Tuberculosis (TB) is a chronic respiratory infectious disease that significantly impacts human health. In 2021, the global incidence of TB was reported at 133 per 100,000 individuals, accompanied by a mortality rate of 17 per 100,000. Approximately 10.6 million new TB cases and 1.3 million deaths related to TB occurred worldwide (1). Between 2015 and 2021, there was a global decline in TB incidence of approximately 10%, achieving only half of the first milestone set forth by the World Health Organization (WHO) End TB Strategy. China faces a significant burden of TB accounting for approximately 7.36% of new cases globally each year (1). In recent years, the incidence of TB in Ningbo has shown a continuous decline, reaching a rate of 32 per 100,000 in 2021. However, this rate is still far from the WHO’s goal of achieving TB-free status by the year 2035 (2). Consequently, it is imperative to control risk factors such as unhealthy lifestyles, comorbidities (e.g., diabetes and HIV), and environmental exposures to effectively reduce the risk of TB infection (3).
Ambient air pollution has recently been identified as a significant environmental risk factor, contributing to a considerable disease burden by impairing the immune system and increasing oxidative stress and inflammation (4). While most studies have focused on the long-term association between air pollution and TB risks (5), our study investigates the exposure–response relationship and mediating effects of short-term CO exposure on the incidence of PTB. Although some recent studies have explored short-term CO exposure, their findings have been inconsistent, and few have focused on low-pollution regions in developing country. For example, a nested case–control study in Northern California, a developed region, showed that CO exposure was associated with an increased risk of pulmonary TB (6). A study conducted in Shanghai, another high-incidence area in China, reported a relative risk (RR) of 1.031 (95% CI: 1.005–1.057) for a 100 μg/m3 increase in CO at an 8-day lag, with similar results observed among male participants, younger age groups, and during the warm-season (3). However, given that Shanghai is characterized by heavy pollution, its findings may be less relevant to our study’s focus on low-pollution regions. An interesting study in Urumqi revealed that PTB incidence increased following 3 months of CO exposure (7). However, two other short-term time-series studies found no significant association between CO and PTB occurrence (8, 9).
Meteorological factors have also been shown to influence the incidence of PTB, including temperature, relative humidity, wind speed, and sunshine duration (10–12). For example, a study in Brazil revealed that PTB incidence was significant correlated with climatic variables such as ultraviolet radiation exceeding 17 MJ/m2, relative humidity ranging from 31.0 to 69.0%, and temperatures between 20 and 23°C (10). A Bayesian spatio-temporal study in mainland China identified positive associations between PTB incidence and rainfall, maximum wind speed, and sunshine duration (11). Some studies have also explored the delayed effect of climate factors on PTB, such as Xiao et al.’s (12) finding that average temperature and minimum relative humidity were inversely related to PTB incidence at lag period of 2 and 3–4 months, respectively. A study conducted by Xu et al. (13) based on 22 years of continuous surveillance data from Hong Kong, identified significant associations between certain magnitudes of meteorological factors and increased risks of PTB notifications. Notably, certain meteorological factor, including temperature and humidity, were highlighted in this context (13).
However, few studies have examined the mediating effects of climate factors on the relationship between air pollutants and the incidence of PTB. The aim of this study is to examine the association between CO exposure and incident PTB through mediation analysis. We focus on the association between daily CO exposure levels and the risk of PTB in Ningbo from 2011 to 2020, while also examining the impact of climate factors (such as temperature and humidity) as potential mediators. Furthermore, we explore how variables such as gender, age, and seasonality may influence this relationship. Our findings could provide valuable insights for policymakers in designing targeted air quality standards aimed at mitigating PTB prevalence and safeguarding vulnerable populations.
Ningbo (center: 121.5°E, 29.9°N) is a coastal city located in Zhejiang Province, China. It covers an area of 9,816 km2 and is governed by six districts and four counties, with a permanent population of 9.5 million as of 2021. The daily CO concentrations across the city were estimated by averaging data collected from eight national air monitoring stations located within the core area of Ningbo, as shown in Figure 1.
The Center for Disease Control and Prevention of Ningbo manage and report all newly diagnosed PTB cases through an online Tuberculosis Management Information System (TBIMS). For each PTB case, comprehensive information is recorded, including region, age, gender, occupation, date of initial visit, report time, address, disease type and diagnosis unit. For this study, we extracted original case data from the TBIMS for all newly reported PTB cases in Ningbo from January 1, 2011 to July 21, 2020. We included 34,154 newly diagnosed cases, excluding those of patients with relapse or extra-pulmonary tuberculosis. We calculated the daily number of cases and stratified them by age and gender.
The daily data were obtained from Ningbo China Meteorological Data Network1 and the Environmental Monitoring Center, covering the period from January 1, 2011 to July 21, 2020. The average daily concentration of PM2.5 (3, 4), NO2 (3), CO (3), SO2 (3), PM10 (4) and 8-h for O3 (3) were collected from eight national air monitoring stations. We selected daily meteorological variables, including mean temperature (°C), relative humidity (%), air pressure (Kpa), visibility (m) and wind speed (m/s),as potential mediators in our analysis.
The distributed lag non-linear model (DLNM) is used to examine the lagged effects within the exposure-response relationship (14). In this study, we applied the DLNM to evaluate the association between CO exposure and the risk of PTB outpatient visits. The lag effect in the DLMN captures changes in the outcomes occurring between exposure and subsequent time periods (15). In addition to CO, our preliminary model incorporates four meteorological factors, seasonal variation, and long-term trends (16). To account for long-term trends, we used a “Time” variable (from 1 to 3,490 days). Furthermore, to control for seasonal effects, we incorporated a “7*years” degree of freedom variable (17). A natural cubic spline (ns) function with 3 degrees of freedom was applied to adjust for climate factors, including mean wind speed (WS), temperature (MT), air pressure (AP), and relative humidity (RH) (18). “DOW” and “HOLIDAY” were included as covariates to control for the impact of weekday and holidays, respectively. The single pollutant model is shown as below:
Where t denotes the observation days. Yt refers to the observed PTB outpatient visits, and μt indicates the anticipated number of visits within t days. refers to the cross-basis function. ns means natural cubic spline function. β1 and β2 are the regression coefficients for DOW and HOLIDAY. The degrees of freedom for air climate factors are denoted as df1 to df3 (14, 19).
The analysis utilizes the 99.5th quantiles of CO concentration (specifically, 2 mg/m3) to assess the impact of CO exposure on PTB outpatient visits. The lag-specific and cumulative risks of PTB outpatient visits per 0.1-unit increase in CO concentration are represented by the Relative Risk (RR) and its corresponding 95% Confidence Interval (CI). Stratified analyses were performed to explore potential heterogeneity in the effects of air pollutants exposure across different age groups, gender, and season. Age was categorized in two groups: ≤65 years and >65 years. Seasons were classified as warm or cold, following the definition in Huang et al. (20). The warm season spans from April to September, while the cold season runs from October to March of the following year. The 95% CI of the RR estimates is calculated as follows:
Where and are the point estimates for the two subgroups, and and are the corresponding standard errors, respectively (9). “dlnm” and “splines” packages in R software (version 3.5.2) are used to conduct DNLM.
We further conducted a mediation analysis to estimate the mediating effects of meteorological factors on the association between CO and PTB cases, using 95% confidence intervals. All analysis were conducted using STATA 18.0, and the bootstrap method was applied to assess the impact of meteorological factors and other air pollutants on the relationship between CO and PTB.
A total of 34,154 new PTB cases were reported in Ningbo between January 1, 2011 and July 21, 2020, averaging 9.79 cases per day. Among these, 22,936 (67.15%) were male and 11,218 (32.85%) were female, resulting in a male-to-female ratio of 2.04:1. Of the total cases, 29,730 (87.05%) were diagnosed in individuals under 65 years of age, while 5,429 (15.90%) cases were in individuals aged 65 or older at the time of diagnosis. Additionally, 19,120 PTB cases (55.98%) were reported during the warm season, while 15,034 cases (44.02%) occurred during the cold season.
The distribution characteristics of PTB cases, air pollutants, and meteorological factors are shown in Table 1. During the study period, the mean concentration of CO was measured at 0.81 mg/m3, with values ranging from 0.02 mg/m3 to 2.80 mg/m3, which complies with China’s Ambient Air Quality Standards. The average daily incidence of PTB cases was recorded at 9.79, with a range from 0 to 42 cases per day. Supplementary Figure S1 illustrates the time series of monthly average of PTB, PM2.5, SO2, CO, NO2, O3, MT, RH, AP, WS in Ningbo from 2011 to 2020. The data reveal distinct seasonal fluctuations as well as long-term trends in the concentrations of air pollutants.
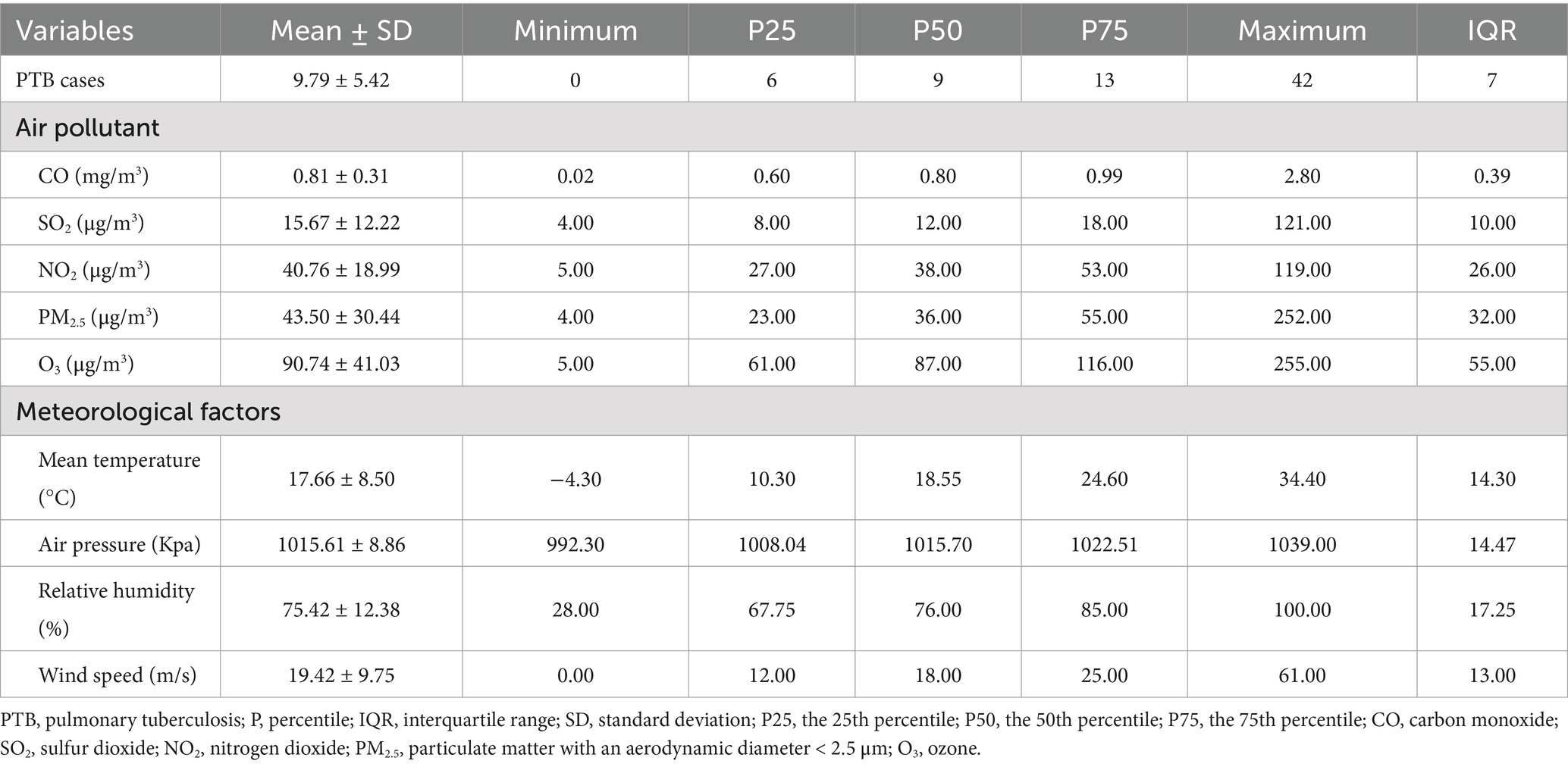
Table 1. Descriptive statistics of daily tuberculosis cases, air pollutants concentration and meteorological factors in Ningbo from January 1st 2011 to April 30th 2020.
Table 2 showed the result of Spearman rank correlation coefficients. CO was negatively correlated with daily PTB cases (r = −0.027, p < 0.05). Additionally, air pressure and temperature were also found to be negatively correlated (r = −0.885, p < 0.05).
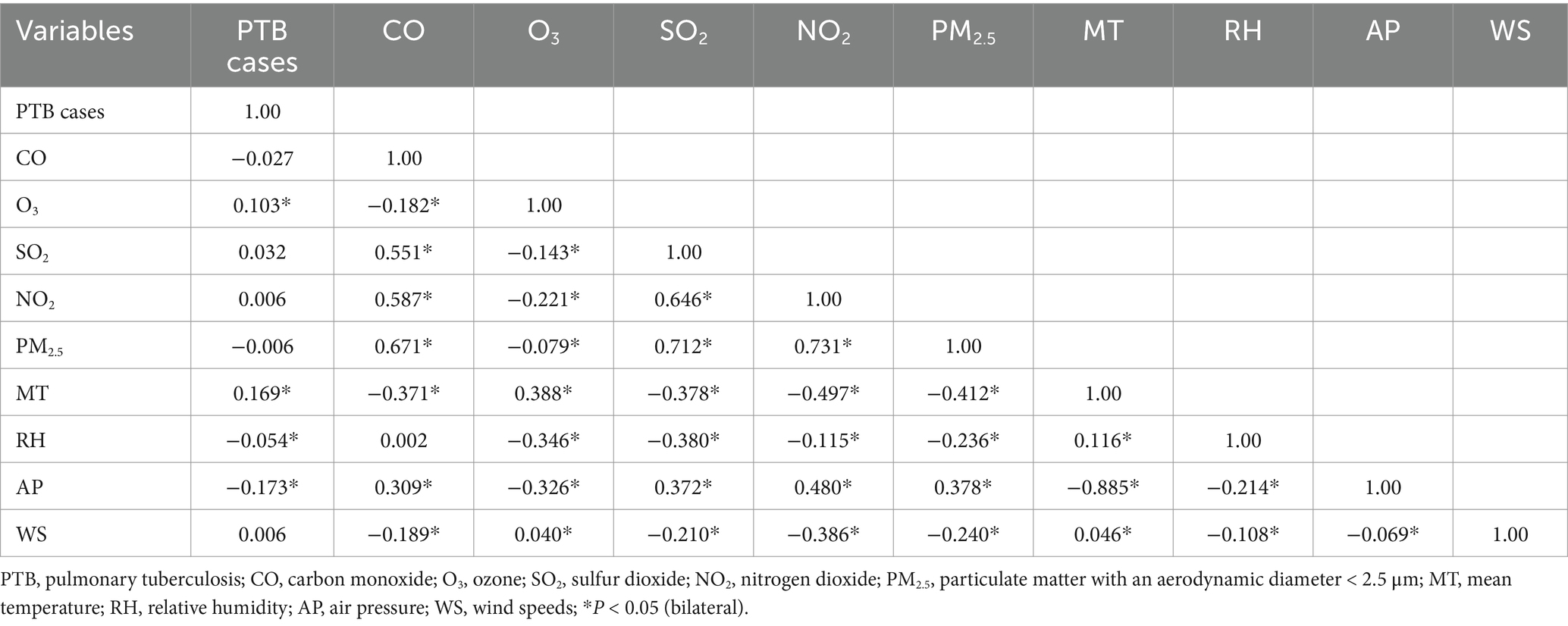
Table 2. Spearman rank correlation coefficients between daily pulmonary tuberculosis cases, air pollutant concentrations and meteorological factors in Ningbo, 2011 to 2020.
As shown in Figure 2A, a 0.1 mg/m3 increase in CO concentration was significantly associated with an increase in outpatient visits for PTB from lag days 2 to 6, as demonstrated by the single-pollutant model (RR = 1.091, 95%CI: 1.020–1.168, lag 2 day). The maximum cumulative lag effect of CO exposure was statistically significant over a period of 0–15 days (RR = 1.781, 95%CI: 1.157–2.742, lag 0–15 days) (see Figure 2B). The 15-day cumulative association between a rise of 0.1 mg/m3 in CO concentration and the increased risk of PTB outpatient visits is graphically presented in Figure 2C. The RR value reaches its minimum when CO concentration is at 1.2 mg/m3, however, RR values were statistically significant when the CO concentrations were equal to or greater than 1.6 mg/m3.
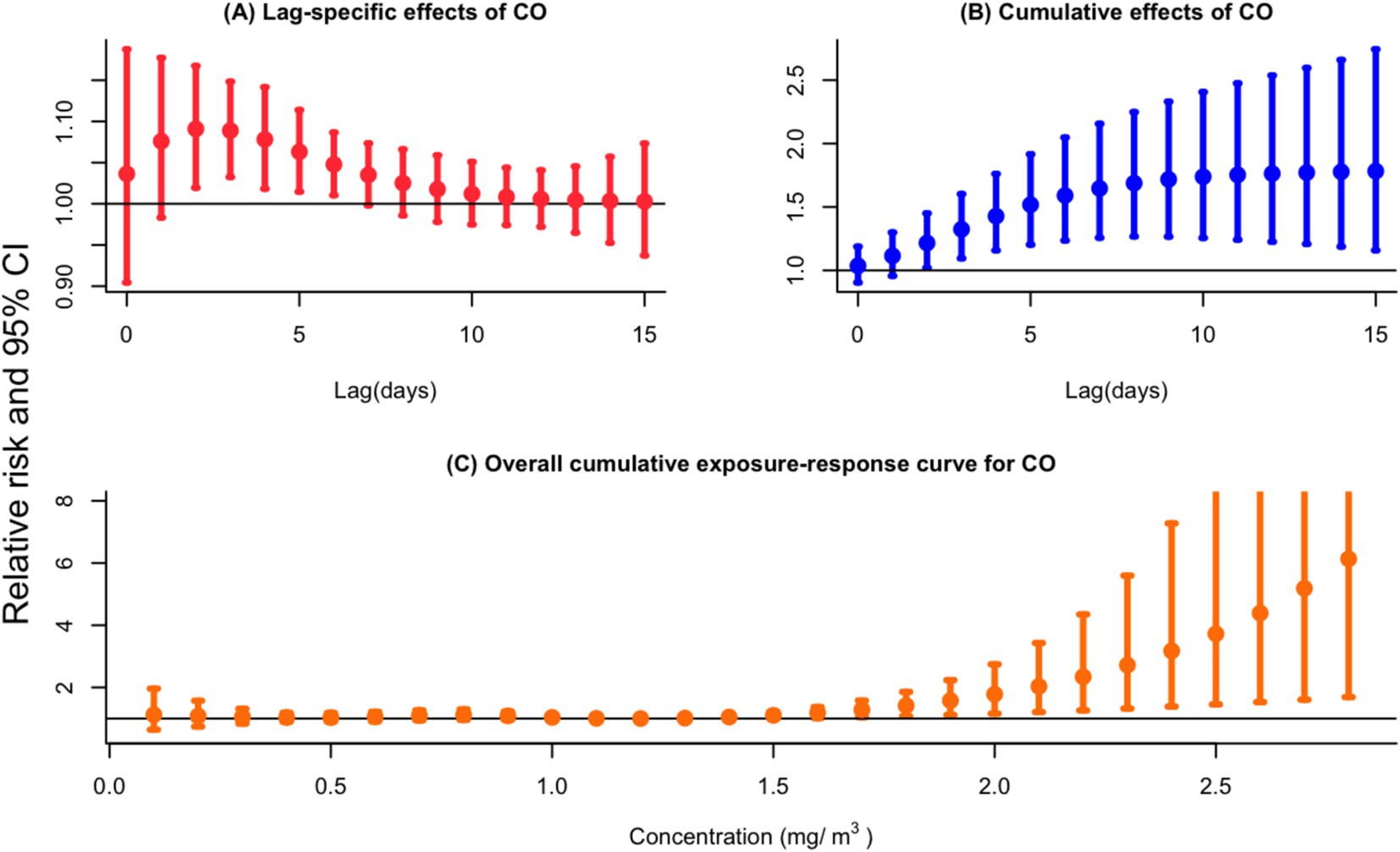
Figure 2. (A) Lag-specific relative risks (%) and (B) cumulative risks (%) in total outpatient visits for PTB per 0.1 mg/m3 increase in daily mean concentrations of CO in the single-pollutant model. (C) Overall exposure-response relationships between CO (lag 0–15 day) and the risk of PTB outpatient visits.
In Figure 3, the subgroup analysis indicates that the impact of CO exposure was statistically significant in several groups: among male (RR = 1.090, 95%CI: 1.009–1.777, lag 3 day), females (RR = 1.101, 95%CI: 1.014–1.195, lag 3 day), younger individuals (RR = 1.097, 95%CI: 1.022–1.178, lag 2 day), and during the warm season (RR = 1.012, 95%CI: 1.002–1.022, lag 4 day) (Supplementary Table S1).
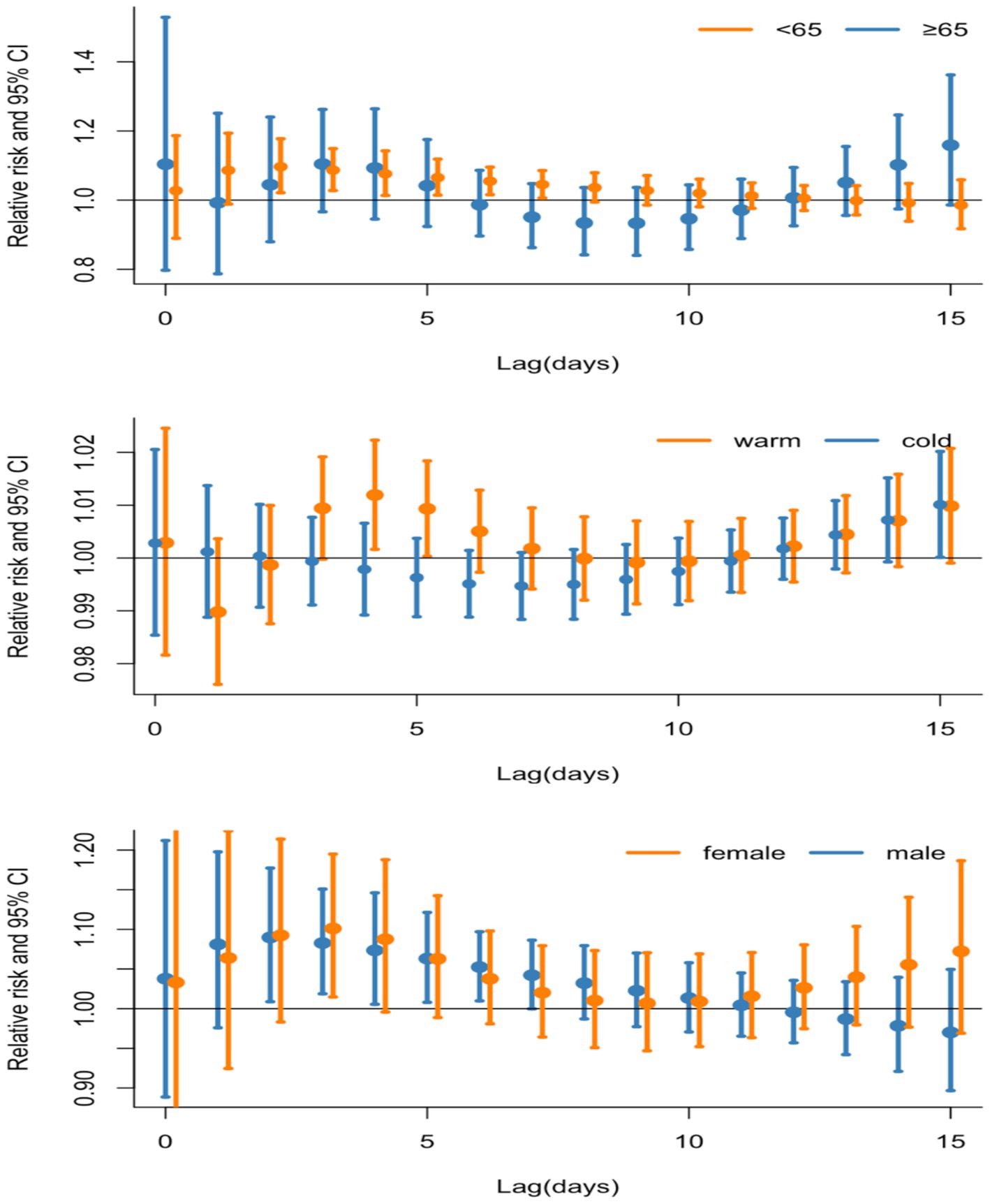
Figure 3. Lag-specific relative risks (95% CI) for outpatient visits to PTB per 0.1 mg/m3 increase in daily air pollution concentrations analyzed through single-pollutant models and stratified by age, gender, and season.
This study found that temperature had a mediating effect on the association between CO and PTB −14.35% (95%CI: −0.5, −90.34%) (see Supplementary Figure S2). As other air pollutants did not show a significant association with PTB cases, we further investigated the mediation effects of meteorological factors on the relationship between other air pollutants and PTB cases. Supplementary Table S2 shows that temperature, pressure and humidity all had mediating effects on the association between PM2.5, NO2 and PTB, respectively. For the association between SO2, PM2.5 and PTB, temperature and humidity had a mediating effect. For the association between O3 and PTB, pressure and humidity had a mediating effect. As the association between SO2, PM2.5, NO2, O3, and PTB was influenced by more than one mediator, we further conducted parallel mediation testing to ascertain the cumulative parallel mediation effect for each air pollutant, respectively. The results showed that total parallel mediation effect on each air pollutant ranged from 40.01 to 90.44% (see Figure 4 and Supplementary Table S3).
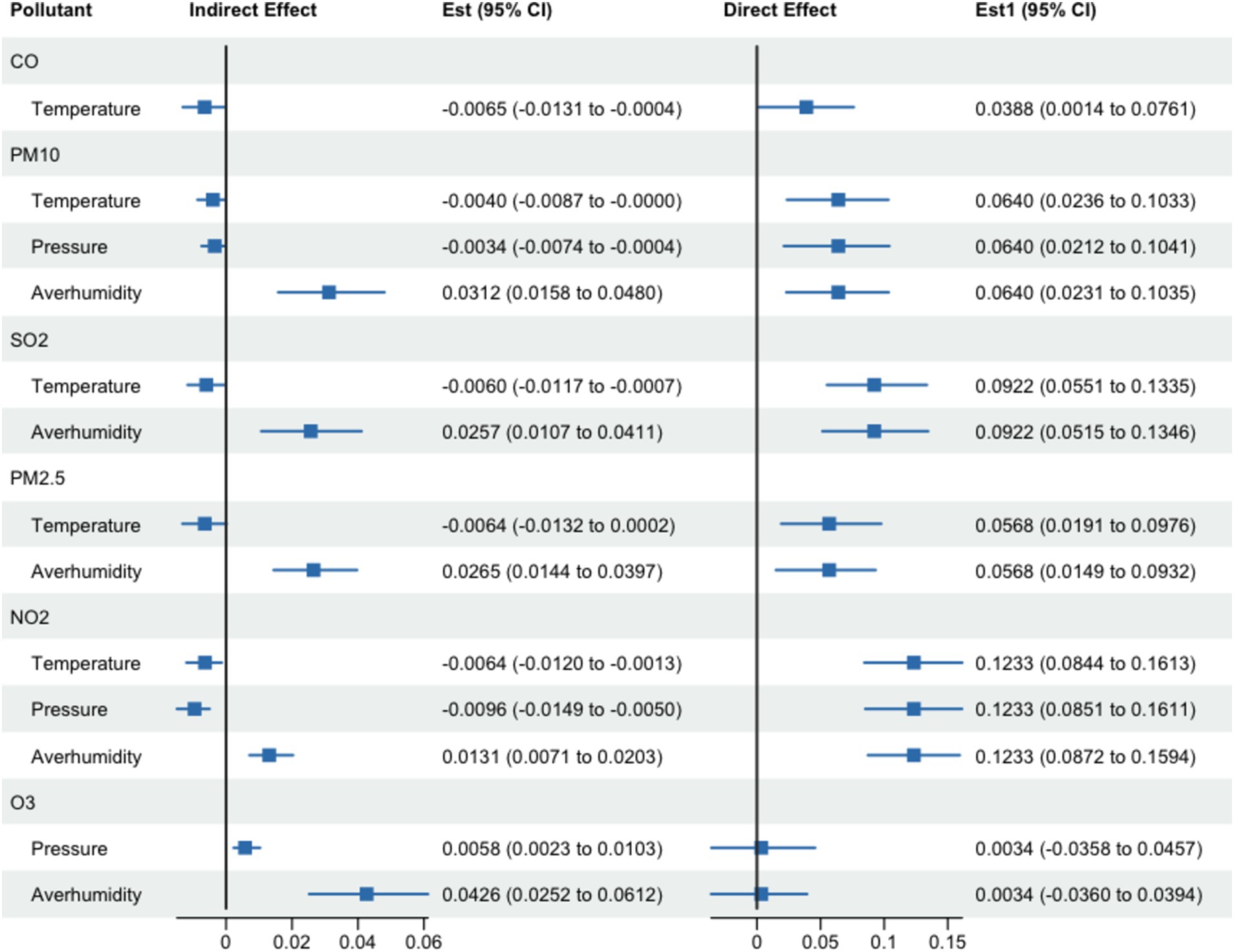
Figure 4. The result of mediating effect of meteorological factors on the association between CO, PM10, SO2, PM2.5, NO2, O3 exposure and PTB incidence.
To assess the robustness of our findings, we employed a double air pollutants model incorporating CO alongside other ambient air pollutants, including PM2.5, SO2, O3 and NO2. Table 3 shows that the RR value for CO exhibits minimal variation across the four double-pollutant models, notably, an increase of 0.1 mg/m3 in CO concentration is association with an increased risk of PTB outpatient visits from lag period of 2–6 days. Similarly, the RR value for all four double pollution exposure reached their peak at a lag time of 2 days.

Table 3. Lag-specific relative risks for active PTB cases per 0.1 mg/m3 increase in the daily concentrations of CO over lagged 15 days in the multi-pollutant model.
Numerous sensitivity analyses were conducted to assess the resilience and validity of our primary findings, exploring various scenarios and conditions: (1) fitting two-pollutant models, (2) changing the length of maximum lag days to 7 and 30 days in the DLNM, (3) using 7 df and 4 df in the splines on time and climate factors, (4) examining the influence of missing data on our DLNM results (i.e., excluding participants with missing meteorological covariates), (5) examining the influence of missing data on our mediation effect results by similarly excluding participants with absent meteorological covariates. While alterations were observed within specific subgroups or pollutants, the primary outcomes remained largely consistent across models involving two pollutants (Supplementary Table S4). This consistency was also evident when modifying maximum lags (Supplementary Figure S3), adjusting degrees of freedom for smoother time and climate factors (Supplementary Figure S4), examining different methods for addressing missing data in relation to DLNM results (Supplementary Figure S5), as well as when examining the influence of missing data on the mediation effect results (Supplementary Tables S4-1–S4-3).
Our findings indicate that the average daily concentration of CO, SO2, NO2, PM2.5 and O3 in Ningbo from lag 0–15 days were 0.81 mg/m3, 15.67 μg/m3, 40.76 μg/m3, 43.50 μg/m3 and 90.74 μg/m3, respectively. The lag-specific associations between the 97.5th percentiles of CO and the number of PTB cases notified were observed at lag 2–6 days. This association was partially mediating by temperature, with a mediating effect of −14.35% (95% CI: −0.5, −90.34%). The exposure–response curves showed that cumulative risks of PTB cases increased as CO concentrations rose over lags of 2–6 days. This result aligns with a short-term exposure study conducted in Shanghai (3). However, while the precise biological mechanism underlying this association remains unclear, some toxicological studies suggest that CO exposure beyond a certain threshold may impair immune resistance to Mycobacterium tuberculosis (M. tuberculosis), thereby increasing vulnerability to infection (21). Furthermore, M. tuberculosis is the only known organism capable of altering its gene expression in response to varying CO concentrations. When host macrophages produce CO, M. tuberculosis activates its CO resistance genes, allowing it to thrive in the presence of CO, unlike other pathogens (22).
Our study found that the 95th percentiles of CO was associated with an increased numbers of PTB cases, consistent with findings from a few studies that reported significant associations between short-term CO exposure and PTB risk (3, 6, 23). For example, a study in Shandong province found a significantly link between short-term outdoor CO exposure and PTB risk (23), and similar results were observed in time-series study in China and case–control studies in the United States (3, 6). However, a study in Wuhan found no significant association between CO and PTB risk in the overall population (8), and similar results were reported from a time-series study in Wuhan based on Kriged Data (9). Despite these conflicting results, our study adds to the growing body of evidence suggesting that short-term exposure to lower CO concentrations may increase the risk for PTB.
We also observed that both male and female patients exposed to low levels of CO had an increased risk of initial PTB; though male patients exhibited a higher risk. These findings are consistent with a population-based case–control study in Northern California (6) and a long-term study in Jinan, China (24). Interestingly, the Jinan study did not identify any association between short-term CO exposure and PTB risk for either gender, highlighting a gap that our study addresses. The heightened sensitivity of males to PTB risk when exposed to lower levels of CO may be attributed to factors such as smoking and occupation exposures. For instance, the prevalence of smoking is significantly higher among men (68.2%) compared to women (11.7%) (25), and it is well-established that smoking increases the risk of PTB (26). Furthermore, males are more likely than females to work in environments such as chemical plants, coal mines, and roads where exposure to air pollutants is higher (27). We also identified a significant positive association between increased CO levels and the risk of PTB during the warm season, despite an inverse mediation effect attributed to temperature. This finding contrasts with studies conducted in Wuhan and Jinan, where air pollution levels, including CO concentrations, were observed to be higher during the cold season than in the warm season (8, 23). However, Ningbo, being a low-level air pollution region, individuals tend to spend more time outdoors during the warm season, this increased outdoor activity may elevate cardiopulmonary load, respiratory rate, and inhalation volume, thereby contributing to greater CO intake (3). Furthermore, younger patients were more likely to be affected by low-level CO exposure.
A key strength of this study is our use of daily time-serious data combined with mediation analysis to explore the association between low-level CO exposure and PTB cases. This approach helps to better understand the impacts of low-levels CO exposure on PTB cases over a 15-day period. Mediation analysis also sheds light on how climate factors may mediate the association between CO exposure and PTB incidence. However, several limitations must be acknowledged. First, our study was limited to a coastal city with relatively low air pollution and specific meteorological characteristics, which may limit the generalizability of our findings to other regions. Given Ningbo’s characteristic, our study may be more representative of other cities in developing regions with low air pollution levels, but larger studies involving more low level air pollution cities are needed. Second, we lacked individual-level data, and the air pollution data used were primarily obtained from fixed monitoring stations, which may not accurately reflect individual exposure. In future studies, wearable devices could be used to collect more accurate air pollution exposure data (28).
Our findings indicate that low-level exposure to CO is associated with an increased risk of PTB outpatient visits in the short-term. Temperature partially mediates this association. Both male and female, as well as younger individuals, were found to be more susceptible to be effects of low-level CO exposure. Additionally, all patients were more vulnerable to CO exposure during the warm season. These findings highlight the urgent need to establish a comprehensive environmental monitoring and early warning system, with a focus on controlling environmental risk factors, in order to prevent tuberculosis and reduce delays in health-seeking behavior.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Institutional Review Board of Ningbo Municipal CDC. The studies were conducted in accordance with the local legislation and institutional requirements.
TH: Conceptualization, Formal analysis, Funding acquisition, Resources, Writing – original draft. XQ: Data curation, Formal analysis, Writing – review & editing. JH: Data curation, Formal analysis, Methodology, Writing – review & editing. GL: Data curation, Formal analysis, Methodology, Writing – review & editing. XG: Project administration, Supervision, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by Medical Technology and Education of Zhejiang Province of China (CN) (No. 2021KY334), Zhejiang Province Public Welfare Technology Application Research Project (CN) (Nos. LGF19H260010 and LGF22H260003), Natural Science Foundation of Ningbo Municipality (Nos. 2022J173 and 2023Z174), and Ningbo Top Medical and Health Research Program (No. 2023020713).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1526325/full#supplementary-material
CO, carbon monoxide; TB, Tuberculosis; PTB, pulmonary tuberculosis; DLNM, distributed lag non-linear model; RR, relative risk; CI, Confidence interval; WHO, World Health Organization; TBIMS, Tuberculosis Management Information System; PM2.5, particulate matter with an aerodynamic diameter < 2.5 μm; NO2, Nitrogen dioxide; SO2, Sulfur dioxide; PM10, particulate matter with an aerodynamic diameter < 10 μm.
3. Xiong, Y, Yang, M, Wang, Z, Jiang, H, Xu, N, Tong, Y, et al. (2022). Association of Daily Exposure to air pollutants with the risk of tuberculosis in Xuhui District of Shanghai, China. Int J Environ Res Public Health 19:6085. doi: 10.3390/ijerph19106085
4. Zhu, S, Wu, Y, Wang, Q, Gao, L, Chen, L, Zeng, F, et al. (2022). Long-term exposure to ambient air pollution and greenness in relation to pulmonary tuberculosis in China: a nationwide modelling study. Environ Res 214:114100. doi: 10.1016/j.envres.2022.114100
5. Xiang, K, Xu, Z, Hu, YQ, He, YS, Dan, YL, Wu, Q, et al. (2021). Association between ambient air pollution and tuberculosis risk: a systematic review and meta-analysis. Chemosphere 277:130342. doi: 10.1016/j.chemosphere.2021.130342
6. Smith, GS, Van Den Eeden, SK, Garcia, C, Shan, J, Baxter, R, Herring, AH, et al. (2016). Air pollution and pulmonary tuberculosis: a nested case-control study among members of a northern California health plan. Environ Health Perspect 124:761–8. doi: 10.1289/ehp.1408166
7. Yang, J, Zhang, M, Chen, Y, Ma, L, Yadikaer, R, Lu, Y, et al. (2020). A study on the relationship between air pollution and pulmonary tuberculosis based on the general additive model in Wulumuqi, China. Int J Infect Dis 96:42–7. doi: 10.1016/j.ijid.2020.03.032
8. Xu, M, Liao, J, Yin, P, Hou, J, Zhou, Y, Huang, J, et al. (2019). Association of air pollution with the risk of initial outpatient visits for tuberculosis in Wuhan, China. Occup Environ Med 76:560–6. doi: 10.1136/oemed-2018-105532
9. Huang, S, Xiang, H, Yang, W, Zhu, Z, Tian, L, Deng, S, et al. (2020). Short-term effect of air pollution on tuberculosis based on Kriged data: a time-series analysis. Int J Environ Res Public Health 17:1522. doi: 10.3390/ijerph17051522
10. Fernandes, FMC, Martins, ES, Pedrosa, DMAS, and Evangelista, MDSN (2017). Relationship between climatic factors and air quality with tuberculosis in the Federal District, Brazil, 2003-2012. Braz J Infect Dis 21:369–75. doi: 10.1016/j.bjid.2017.03.017
11. Li, Q, Liu, M, Zhang, Y, Wu, S, Yang, Y, Liu, Y, et al. (2019). The spatio-temporal analysis of the incidence of tuberculosis and the associated factors in mainland China, 2009–2015. Infect Genet Evol 75:103949. doi: 10.1016/j.meegid.2019.103949
12. Xiao, Y, He, L, Chen, Y, Wang, Q, Meng, Q, Chang, W, et al. (2018). The influence of meteorological factors on tuberculosis incidence in Southwest China from 2006 to 2015. Sci Rep 8:10053. doi: 10.1038/s41598-018-28426-6
13. Xu, M, Li, Y, Liu, B, Chen, R, Sheng, L, Yan, S, et al. (2021). Temperature and humidity associated with increases in tuberculosis notifications: a time-series study in Hong Kong. Epidemiol Infect 149:e8. doi: 10.1017/S0950268820003040
14. Gasparrini, A (2014). Modeling exposure-lag-response associations with distributed lag non-linear models. Stat Med 33:881–99. doi: 10.1002/sim.5963
15. Gasparrini, A, Armstrong, B, and Kenward, MG (2010). Distributed lag non-linear models. Stat Med 29:2224–34. doi: 10.1002/sim.3940
16. Bhaskaran, K, Gasparrini, A, Hajat, S, Smeeth, L, and Armstrong, B (2013). Time series regression studies in environmental epidemiology. Int J Epidemiol 42:1187–95. doi: 10.1093/ije/dyt092
17. Peng, RD, Dominici, F, and Louis, TA (2006). Model choice in time series studies of air pollution and mortality. J R Stat Soc A Stat Soc 169:179–203. doi: 10.1111/j.1467-985X.2006.00410.x
18. Zhu, S, Xia, L, Wu, J, Chen, S, Chen, F, Zeng, F, et al. (2018). Ambient air pollutants are associated with newly diagnosed tuberculosis: a time-series study in Chengdu, China. Sci Total Environ 631-632:47–55. doi: 10.1016/j.scitotenv.2018.03.017
19. Liu, H, Tian, Y, Xu, Y, Huang, Z, Huang, C, Hu, Y, et al. (2017). Association between ambient air pollution and hospitalization for ischemic and hemorrhagic stroke in China: a multicity case-crossover study. Environ Pollut 230:234–41. doi: 10.1016/j.envpol.2017.06.057
20. Huang, K, Ding, K, Yang, X-J, Hu, C-Y, Jiang, W, Hua, X-G, et al. (2020). Association between short-term exposure to ambient air pollutants and the risk of tuberculosis outpatient visits: a time-series study in Hefei, China. Environ Res 184:109343. doi: 10.1016/j.envres.2020.109343
21. Sarkar, S, Song, Y, Sarkar, S, Kipen, HM, Laumbach, RJ, Zhang, J, et al. (2012). Suppression of the NF-kappa B pathway by diesel exhaust particles impairs human antimycobacterial immunity. J Immunol 188:2778–93. doi: 10.4049/jimmunol.1101380
22. Zacharia, VM, and Shiloh, MU (2012). Effect of carbon monoxide on Mycobacterium tuberculosis pathogenesis. Med Gas Res 2:30–7. doi: 10.1186/2045-9912-2-30
23. Liu, Y, Zhao, S, Li, Y, Song, W, Yu, C, Gao, L, et al. (2021). Effect of ambient air pollution on tuberculosis risks and mortality in Shandong, China: a multi-city modeling study of the short-and long-term effects of pollutants. Environ Sci Pollut Res 28:27757–68. doi: 10.1007/s11356-021-12621-6
24. Liu, Y, Cui, L, Hou, L, Yu, C, Tao, N, Liu, J, et al. (2018). Ambient air pollution exposures and newly diagnosed pulmonary tuberculosis in Jinan, China: a time series study. Sci Rep 8:17411. doi: 10.1038/s41598-018-35411-6
25. Hao, W, Li, LJ, Xiao, SY, Yang, DS, Tu, J, Cao, HG, et al. (1994). The gender differences and related factors in drinking and smoking behaviors among general population of two communities in Hunan Province. Chin J Clin Psych 2:90–4.
26. Rao, VG, Gopi, PG, Bhat, J, Yadav, R, Selvakumar, N, and Wares, DF (2012). Selected risk factors associated with pulmonary tuberculosis among Saharia tribe of Madhya Pradesh, Central India. Eur J Pub Health 22:271–3. doi: 10.1093/eurpub/ckr009
27. Locke, SJ, Colt, JS, Stewart, PA, Armenti, KR, Baris, D, Blair, A, et al. (2014). Identifying gender differences in reported occupational information from three US population-based case-control studies. Occup Environ Med 71:855–64. doi: 10.1136/oemed-2013-101801
Keywords: tuberculosis, carbon monoxide, short-term exposure, mediation analysis, health
Citation: He T, Qian X, Huang J, Li G and Guo X (2025) A mediation analysis of meteorological factors on the association between ambient carbon monoxide and tuberculosis outpatients visits. Front. Public Health. 13:1526325. doi: 10.3389/fpubh.2025.1526325
Received: 11 November 2024; Accepted: 03 January 2025;
Published: 05 February 2025.
Edited by:
Yunhui Zhang, Southwest Jiaotong University, ChinaReviewed by:
Jian Lei, Xi’an Jiaotong University, ChinaCopyright © 2025 He, Qian, Huang, Li and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinbiao Guo, Z3VveGJAYmptdS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.