- 1Directorate of Health Services, Raipur, India
- 2ESIC Medical College, Hyderabad, India
- 3Model Rural Health Research Unit, Durg, India
- 4Pt. Jawahar Lal Nehru Memorial Medical College, Raipur, India
- 5ICMR-National Institute of Reseach in Tribal Health, Jabalpur, India
Objective: The current study is a cross-sectional survey that aims to assess an association COVID-19 on mental health in rural areas of Central India.
Methods: Generalized Anxiety Disorder Assessment (GAD-7), Patient Health Questionnaire (PHQ-9), and Impact of Events Scale-Revised (IES-R) were used to evaluate the anxiety, depression, and post-traumatic stress disorder (PTSD) among families with at least one member having been affected by COVID-19 during November 2022 to December 2022 in Durg District of Chhattisgarh State.
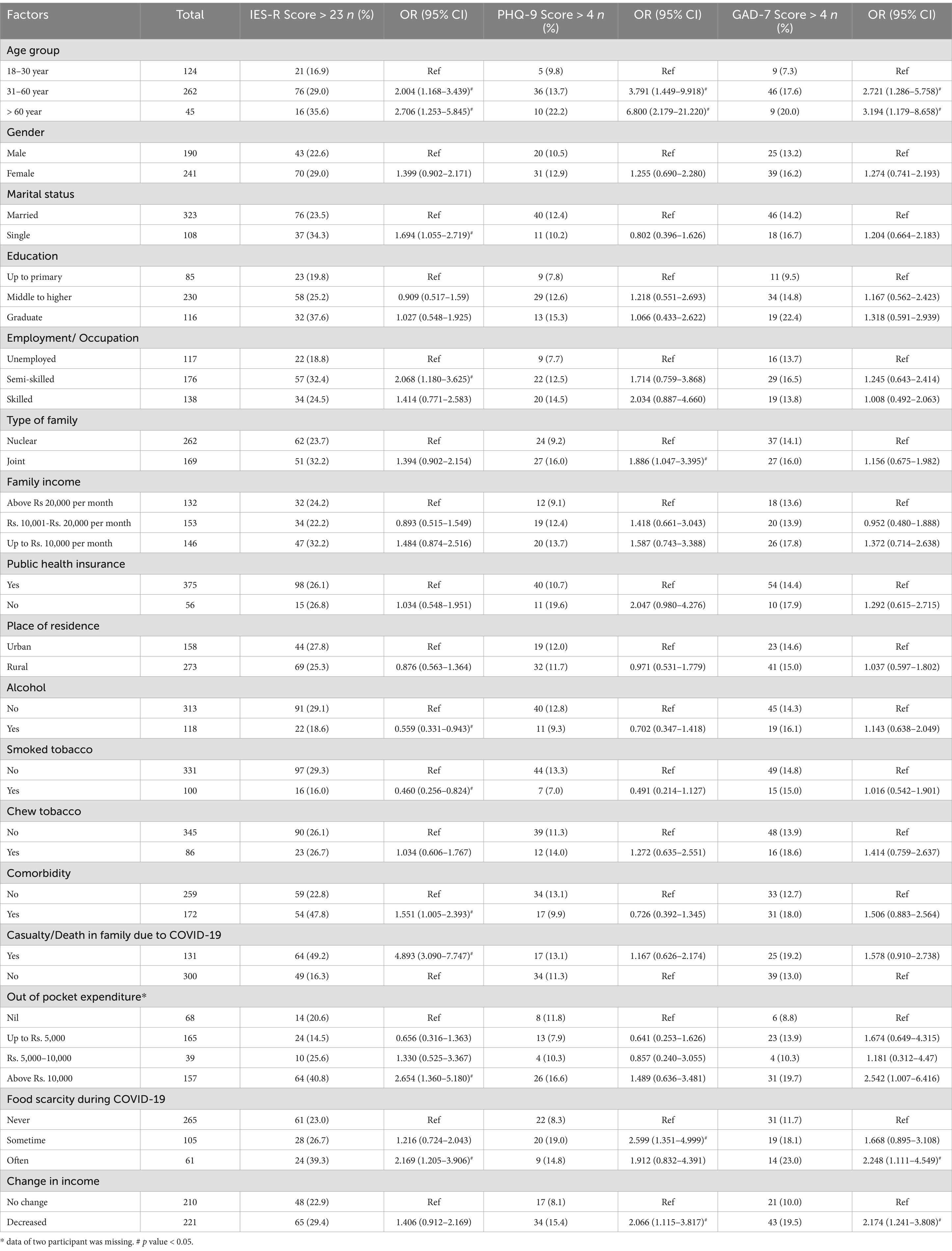
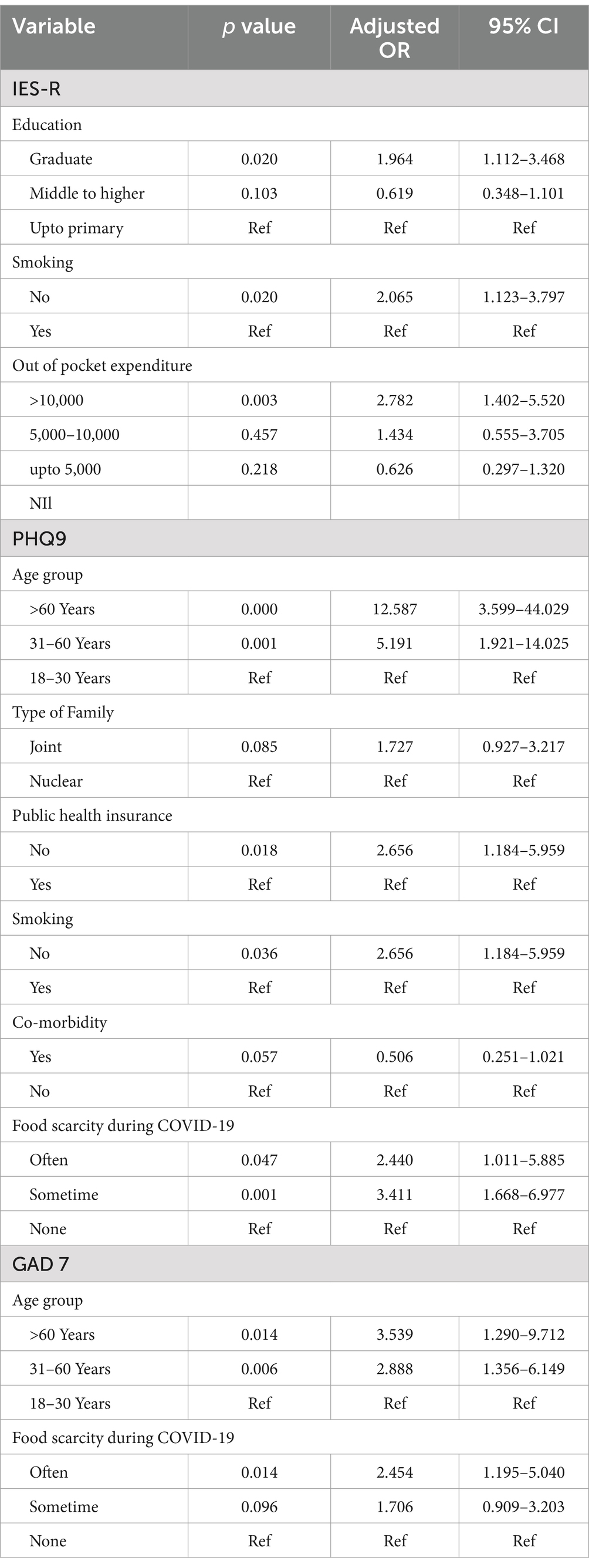
Results: A total of 431 participants were interviewed from 18 villages of Durg district of Chhattisgarh state. Symptoms of distress, anxiety and depression were observed in 26.2, 14.8 and 11.8% of participants. The death of family members due to COVID-19 and out of pocket expenditure was considerably associated with a higher risk of mental distress. A reduction in income was significantly associated with depression (p-value = 0.025, OR = 2.066, 95% CI = 1.115–3.817). Decline in income was also linked to depression among study participants (p value = 0.025, OR = 2.066, 95% CI = 1.115–3.817). Education, smoking and out of pocket expenditure was found be independently associated with occurrence of symptoms concerned with PTSD.
Conclusion: The study points to the significance of socioeconomic factors like food security, and income stability during COVID-19 in mental health outcomes even after 1 year of pandemic. Increasing access to mental health resources and support for those affected by financial and food insecurities can help individuals cope with stress and maintain mental well-being.
Introduction
Individuals affected by COVID-19 have experienced a range of mental health problems, including depression, anxiety disorders, panic attacks, irrational anger, impulsivity, sleep disorders, emotional disturbance, post-traumatic stress disorder (PTSD), and suicidal tendencies (1, 2). The global prevalence of anxiety and depression was increased by 25% in the first year of the COVID-19 pandemic (3). Further, during initial phase of the pandemic high prevalence of symptoms of anxiety (6.33–50.9%), depression (14.6–48.3%), post-traumatic stress disorder (7–53.8%) and psychological distress (34.43–38%) were reported in the general population during the COVID-19 pandemic across the world (4). While studies were indeed conducted during the onset of pandemic, to understand the immediate impact on mental health among various populations, it is crucial to continue studying the long-term effects and recovery, particularly in underrepresented areas such as rural communities. The mental health impacts of a crisis like a pandemic can extend far beyond the immediate crisis period.
Chhattisgarh, a state in India, has one of the highest suicide rates, with 28.2% compared to the national average of 12.4% (5). The state was also among the most affected by the COVID-19 pandemic, ranking twelfth in India (6). While numerous studies have been conducted on specific populations in India, very few have focused on the general population of rural settings. Therefore, a cross-sectional study was conducted in rural areas to determine the prevalence of depression, anxiety, and PTSD like symptoms among those affected with COVID-19 in the past 3 years and to identify the associated risk factors.
Materials and methods
A community-based survey was conducted among rural and urban blocks of Durg district, Chhattisgarh, from November 2022 to December 2022. The demographic details of COVID-19 affected individuals were sought from the district hospital. Individuals who were affected from COVID-19 or individuals whose close family member was affected by COVID-19 or died due to COVID-19 in period between October to December 2021 were recruited from 18 villages. These 18 villages were selected conveniently from five blocks of the district for the study. For selecting participants, farthest house from the village was selected and then household were interviewed sequentially. Data was gathered from households that fulfilled the eligibility criteria.
Sample size estimation
With a confidence level of 95%, assuming 50% prevalence from studies cited above, the sample size estimated was 384. Considering the non-response rate of 10%, the sample size estimated was 422. To achieve the sample size, 25 individuals were approached from each village.
Data collection
Written informed consent was taken from each participant before the interview. The survey instrument consisted of two schedules. The first schedule was on sociodemographic data of the participant and his/ her family and medical history of the one affected with COVID-19, relevant personal history, hospital admissions or home isolation, presence of complications and health problems related to the disease etc. Those with preexisting mental illness (diagnosed before March 2020) were excluded from the study. The second schedule consisted of psychometric assessment scales, namely the Generalized Anxiety Disorder Assessment (GAD-7), Patient Health Questionnaire (PHQ)-9 and Impact of Event Scale-Revised (IES-R) scale. The GAD-7 schedule consists of seven items that are designed to identifying symptoms consistent with generalized anxiety disorder (GAD) (7). In order to complete the assessment, an individual is asked to rate the severity of their symptoms over the past 2 weeks. The PHQ-9 is the nine-item depression scale helpful in screening depression in primary care (8). It consists of nine questions that evaluate symptoms over the past 2 weeks. Each item is scored from 0 (not at all) to 3 (nearly every day), resulting in a total score ranging from 0 to 27. Higher scores indicate greater depression severity. Whereas IES-R is a self-report measure comprising 22 items; commonly used to symptoms related to subjective distress level related to traumatic event (9). The respondents are required to identify a specific stress-inducing life event and rank their level (scale 0–4) of distress or discomfort for each difficulty listed based on the past 7 days.
A cutoff score of >4 of PHQ9, >4 of GAD 7, and >23 for the IES-R scale was used to determine the presence of symptoms of depression, anxiety and PTSD, respectively.
Statistical analysis
Data was presented as number and percentage for discrete values and mean ± SD for continuous variables. The Fisher exact test was applied to see the univariate association of different dependent variables with presence of symptoms of depression, anxiety and PTSD. Odds ratio (OR) with 95% confidence interval was also calculated to determine the strength of association. Multinomial logistic regression with backward elimination model was applied to see the independent risk factors for the symptoms of depression, anxiety and PTSD. A p-value of less than 0.05 was considered statistically significant. All the statistical analyses were conducted using IBM SPSS version 26 software for windows.
Results
During the study, a total of 435 participants were recruited from 18 villages of Durg district and interviewed. Out of which, some information related to mental health was missing for four individuals and was excluded from the analysis. Therefore, analysis of the results was performed among 431 responses. The mean age of participants was 41 ± 14 years. There were 190 (44.1%) male and 241 (55.9%) female. Of these 431 participants, 157 (36.4%) have mental health issues (at least one of the three scales).
A total of 113 (26.2%, 43 males (22.6%) and 70 (29.0%) females) participants had symptoms concerned with PTSD. The mean IES-R scale score was 24.25 ± 6.98. Forty-four (10.2%) had moderate to severe symptoms (IES-R scores ≥33) (Supplementary Table 1). As expected, older peoples have higher occurrence of symptoms of PTSD than younger (Table 1). High prevalence of PTSD symptoms was observed in single participants as compared to married participants (p = 0.032, OR = 1.694, 95% CI = 1.055–2.719). Symptoms of PTSD was found in lesser number of participants in alcoholic and smokers’ groups as compared than non-alcoholic (p value = 0.028, OR = 0.559, 95% CI = 0.331–0.943) and non-smokers (p value = 0.009, OR = 0.460, 95% CI = 0.256–0.824) groups, respectively. The presence of comorbidity (p value = 0.048, OR = 1.551, 95% CI = 1.005–2.393) and death in the family due to COVID-19 (p < 0.001, OR = 4.893, 95% CI = 3.090–7.747) were associated with the symptoms of traumatic distress (Table 1). Out-of-pocket expenditure for medical expenses and shortage of food were also found to be associated with high PTSD in studied participants (Table 1). After applying multivariate logistic regression analysis Education, smoking and out of pocket expenditure was found be independently associated with occurrence of symptoms concerned with PTSD (Table 2).
The mean PHQ score was 1.32 ± 2.70. As per PHQ-9 score, total 51 (11.8%) participants were having symptoms of depression (Supplementary Table 1). Out of these, 45 participants had mild symptoms and four had moderate and one had severe depression. Older individuals were more likely of facing depression (Table 1). The occurrence of depression-like symptoms was higher in joint families compared to nuclear families (p value = 0.046, OR = 1.886, 95% CI = 1.047–3.395). Decrease in income was also found to be significantly associated with depression like symptoms (p value = 0.025, OR = 2.066, 95% CI = 1.115–3.817) (Table 1). Older age group, absence of public health insurance, smoking and scarcity of food during Covid-19 were the independent risk variables for the occurrence symptoms of depression in studied participants (Table 2).
A total 64 (14.8%) participants were found to have anxiety like symptoms as per GAD7 score. Fifty-three had mild anxiety symptoms (GAD7 score 5–9), seven had moderate symptoms (GAD7 score 10–14) and four had severe anxiety symptoms (GAD7 score > 15) (Supplementary Table 1). The mean score for GAD7 was 1.78 ± 3.04. The occurrence of anxiety symptoms was found higher in older age groups as compared to lower age group (Table 1). Participants who have shortage of foods during pandemic were more anxious (p value = 0.0371, OR = 2.248, 95% CI = 1.111–4.549). Further decrease in income was also found to be associated with anxiety symptoms (p value = 0.007, OR = 2.174, 95% CI = 1.241–3.808) (Table 1). Older age group and food scarcity was identified as independent risk factors for high GAD7 score (Table 2).
Discussion
According to the current study, 26.2% of participants showed signs of PTSD, while 11.8% have depression, and 14.8% have anxiety symptoms after the COVID-19 pandemic. A systematic review and meta-analysis reported the pooled prevalence of anxiety 23.5% (95% CI: 17.4–29.6%) and 20.2% (95% CI: 17.2–23.2%) prevalence of depressive symptoms among general population of India during COVID-19 pandemic (10). Furthermore, a previous study conducted in urban Slum in North India observed the lower prevalence of depression (3.5, 95% CI = 0.95–6.05) and anxiety (2.5, 95% CI = 0.34–4.66) (11). Similarly, during the onset of the pandemic, there have been reports of relatively high rates of symptoms of anxiety, depression, and PTSD in various other countries (China, Denmark, Nepal, Spain, Italy, Iran, the US and Turkey) around the world during the COVID-19 pandemic. These symptoms have been reported with rates ranging from 6.33 to 50.9% for anxiety, 14.6 to 48.3% for depression, and 7 to 53.8% for post-traumatic stress disorder (2, 4, 12–16). Chronic disease patients, quarantined persons, and COVID-19 patients were at an increased risk of anxiety and depression than other populations (12).
Several risk factors associated with PTSD, depression and anxiety have been identified in various studies (17–24). Based on our study, it was found that the old age group was more likely to have symptoms of PTSD, depression and anxiety. In contrast, some studies have found the young population more prone to mental distress (13, 14), while reports on age as a risk factor were varying in other studies (17). Recently study conducted in central India showed the 7.83% prevalence of depression, 12.2% prevalence of anxiety and 5.2% prevalence of stress among older participants (25). In the current study, sex was not a significant risk factor. Other studies have found females to suffer more during the pandemic due to increased household responsibilities and domestic violence during the lockdown (18, 19, 22–24).
Food insecurity is a serious issue that can lead to significant stress and depression. Not knowing status of next meal creates a constant state of worry and anxiety, which can deeply affect mental health. In current study, food insecurity was found to be associated with depressed state. Previous studies have also shown that food insecurity is strongly associated with increased risks of depression, anxiety, and stress (26–28). For example, one study found that food insecurity was linked to a 257% higher risk of anxiety and a 253% higher risk of depression (28). However, all these studies were conducted in early days of pandemic. Public health strategies should focus on offering direct subsidies for food purchases to impoverished families and decreasing the stigma surrounding charitable food assistance.
The unpredictability and financial pressure can take a significant toll on mental well-being. Decrease in income was also found to be associated with depression and traumatic stress like symptoms in current study. Previous studies have also shown that individuals facing financial difficulties during the pandemic reported higher levels of psychosocial distress (29, 30). Another study reported that more than one-third of low-income adults screened positive for depression, anxiety, and high stress during the early days of the pandemic (27). Public health measures should focus on providing financial support and mental health resources to those affected by income loss. Previous studies also show that direct COVID-19 infection may not be the leading cause of long-term psychological distress. Instead, it appears that psychosocial factors related to the pandemic may be contributing to the increased prevalence of anxiety, depression and PTSD. Addressing the indirect effects of COVID-19 in long term (31) is crucial in mental health treatment and policy. The current study results provide important insights for mental health professionals and policymakers in developing strategies to prevent and treat PTSD.
Our study acknowledges some limitations, such as the self-reported information regarding co-morbidities. We did not analyze the association between the intensity or severity of mental health issues and the closeness or friendliness of the relative who succumbed to the pandemic. Additionally, we did not elicit the impact of severity of disease, such as hospitalization, ventilator usage, and near-death experiences, on mental status. We also did not capture social factors that may have influenced mental health status, such as income, financial or economic burden, food scarcity, and stigma, in detail through any standard tool. The effect of other variables such as social support, utilization of digital tools, access to healthcare which may impact the depression, anxiety and PTSD was not studied.
It is imperative to emphasize the significance of family focused therapy and community-based interventions such as providing mental health education to family and community members. Families play a crucial role in mental health treatment as supportive family relationships can enhance emotional well-being. Family-focused psychotherapeutic interventions can be applied to improve the mental health and well-being of individuals during these pandemic situations (32). Such measures are vital in creating a supportive environment, and we should continue striving to achieve these goals. To effectively address mental health during future pandemics, the healthcare system should incorporate mental health services into pandemic response plans, provide training to healthcare workers in psychological first aid, and establishing telehealth infrastructure (33) for remote mental health support. Family focused therapy, building social support networks and involving community leaders in promoting mental health awareness (34) can be vital steps in overcoming the challenges related to mental health. Furthermore, increasing mental health research and preparedness funding can help inform evidence-based strategies for future pandemics.
Conclusion
Around one fourth of the studied participant have PTSD, even after waning of the COVID-19 pandemic. Social factors such as decrease in income and food scarcity influenced mental health issues during a pandemic. Hence, it is imperative to consider social factors such as income and food stability when addressing mental health issues during a pandemic.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
This study was conducted in line with the principles of the Declaration of Helsinki. It was given approval by the Ethics Committee of Pandit JNM Medical College, Raipur (Letter no./MC/Ethics/2022/118 dated 2/5/22) and ICMR-National Institute of Research in Tribal Health, Jabalpur. Written informed consent was taken from each participant before the interview. The studies were conducted in accordance with the local legislation and institutional requirements.
Author contributions
DG: Conceptualization, Data curation, Methodology, Writing – original draft. SD: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. AM: Data curation, Methodology, Writing – original draft. SC: Data curation, Formal analysis, Investigation, Writing – review & editing. BS: Conceptualization, Writing – review & editing. MS: Supervision, Writing – review & editing. RK: Conceptualization, Formal analysis, Project administration, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The study was financially supported under the intramural research scheme of Model Rural Health Research Unit of Department of Health Research, New Delhi, Government of India (letter no V.25011/140/2014-HR).
Acknowledgments
The authors acknowledge Secretary, Department of Health Research and Director General, ICMR, New Delhi for providing facilities. Authors are thankful to Dr Aparup Das, Former Director, ICMR-NIRTH, Jabalpur for guidance and kind support to carry out this research. We also acknowledge the cooperation of the participants and the support of the field functionaries of the Health and the Women & Child Welfare departments in facilitating the interviews. We thank the support staff of MRHRU, Jheet and Statistician (Mr Shubham Mishra) for support in data cleaning and analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1526300/full#supplementary-material
References
1. Hossain, MM, Tasnim, S, Sultana, A, Faizah, F, Mazumder, H, Zou, L, et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. (2020) 9:636. doi: 10.12688/f1000research.24457.1
2. Chen, J, Zhang, SX, Yin, A, and Yanez, JA. Mental health symptoms during the COVID-19 pandemic in developing countries: a systematic review and meta-analysis. J Glob Health. (2022) 12:05011. doi: 10.7189/jogh.12.05011
3. World Health Organisation. (2022) COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. Available online at https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide (Accessed on 26 Feb 2025).
4. Xiong, J, Lipsitz, O, Nasri, F, Lui, LMW, Gill, H, Phan, L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
5. National Crime Records Bureau. (2020) Ministry of home affairs Gov of India. Accidental deaths & suicides in India. Available online at: http://ncrb.gov.in/ (Accessed on 25 Feb 2025).
6. Agarwala, P, Bhargava, A, Gahwai, DK, Negi, SS, Shukla, P, and Dayama, S. Epidemiological characteristics of the COVID-19 pandemic during the first and second waves in Chhattisgarh, Central India: a comparative analysis. Cureus. (2022) 14:e24131. doi: 10.7759/cureus.24131
7. Löwe, B, Decker, O, Müller, S, Brähler, E, Schellberg, D, Herzog, W, et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
8. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9. Validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
9. Horowitz, M, Wilner, N, and Alvarez, W. Impact of event scale: a measure of subjective stress. Psychosom Med. (1979) 41:209–18. doi: 10.1097/00006842-197905000-00004
10. Sharma, SK, Joseph, J, Varkey, BP, Dhandapani, M, Varghese, A, Sharma, S, et al. Prevalence of anxiety and depressive symptoms during COVID-19 pandemic among the general population in India: a systematic review and meta-analysis. J Neurosci Rural Pract. (2022) 13:608–17. doi: 10.25259/JNRP-2022-1-21-R3-(2324)
11. Rehman, T, Singh, T, Sharma, S, Kumar, J, Govindan, D, and Singh, SM. Prevalence of depression and anxiety during the COVID-19 pandemic among the residents of an urban slum in North India. J Neurosci Rural Pract. (2021) 12:153–8. doi: 10.1055/s-0040-1721623
12. Wu, T, Jia, X, Shi, H, Niu, J, Yin, X, Xie, J, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. (2021) 281:91–8. doi: 10.1016/j.jad.2020.11.117
13. Anand, V, Verma, L, Aggarwal, A, Nanjundappa, P, and Rai, H. COVID-19 and psychological distress: lessons for India. PLoS One. (2021) 16:e0255683. doi: 10.1371/journal.pone.0255683
14. Rodriguez-Rey, R, Garrido-Hernansaiz, H, and Collado, S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front Psychol. (2020) 11:1540. doi: 10.3389/fpsyg.2020.01540
15. Mazza, C, Ricci, E, Biondi, S, Colasanti, M, Ferracuti, S, Napoli, C, et al. A Nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. (2020) 17:3165. doi: 10.3390/ijerph17093165
16. Gao, J, Zheng, P, Jia, Y, Chen, H, Mao, Y, Chen, S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. (2020) 15:e0231924. doi: 10.1371/journal.pone.0231924
17. Na, L, Yang, L, Mezo, PG, and Liu, R. Age disparities in mental health during the COVID19 pandemic: the roles of resilience and coping. Soc Sci Med. (2022) 305:115031. doi: 10.1016/j.socscimed.2022.115031
18. Marzo, RR, Vinay, V, Bahari, R, Chauhan, S, Ming, DAF, Nelson Fernandez, SFA, et al. Depression and anxiety in Malaysian population during third wave of the COVID-19 pandemic. Clin Epidemiol Glob Health. (2021) 12:100868. doi: 10.1016/j.cegh.2021.100868
19. Liu, N, Zhang, F, Wei, C, Jia, Y, Shang, Z, Sun, L, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. (2020) 287:112921. doi: 10.1016/j.psychres.2020.112921
20. Cao, W, Fang, Z, Hou, G, Han, M, Xu, X, Dong, J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
21. Wang, Y, Di, Y, Ye, J, and Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. (2021) 26:13–22. doi: 10.1080/13548506.2020.1746817
22. Joaquim, RM, Pinto, ALCB, Guatimosim, RF, de Paula, JJ, Souza Costa, D, Diaz, AP, et al. Bereavement and psychological distress during COVID-19 pandemics: the impact of death experience on mental health. Curr Res Behav Sci. (2021) 2:100019. doi: 10.1016/j.crbeha.2021.100019
23. Vindegaard, N, and Benros, ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
24. Du, J, Dong, L, Wang, T, Yuan, C, Fu, R, Zhang, L, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. (2020) 67:144–5. doi: 10.1016/j.genhosppsych.2020.03.011
25. Malhotra, V, Javed, D, Bharshankar, R, Singh, V, Gautam, N, Mishra, S, et al. Prevalence and predictors of depression, anxiety and stress among elderly during COVID-19: a cross-sectional study from Central India. Mymensingh Med J. (2023) 32:556–66.
26. Sundermeir, SM, Wolfson, JA, Bertoldo, J, Gibson, DG, Agarwal, S, and Labrique, AB. Food insecurity is adversely associated with psychological distress, anxiety and depression during the COVID-19 pandemic. Prev Med Rep. (2021) 24:101547. doi: 10.1016/j.pmedr.2021.101547
27. Wolfson, JA, Garcia, T, and Leung, CW. Food insecurity is associated with depression, anxiety, and stress: evidence from the early days of the COVID-19 pandemic in the United States. Health Equity. (2021) 5:64–71. doi: 10.1089/heq.2020.0059
28. Fang, D, Thomsen, MR, and Nayga, RM. The association between food insecurity and mental health during the COVID-19 pandemic. BMC Public Health. (2021) 21:607. doi: 10.1186/s12889-021-10631-0
29. Allen, J, Smith-Carrier, T, Smye, V, Gewurtz, R, Isard, R, Goldszmidt, R, et al. Experiences of mental health and poverty in high-income countries during COVID-19: a systematic review and meta-aggregation. PLOS Ment Health. (2024) 1:e0000059. doi: 10.1371/journal.pmen.0000059
30. Adise, S, West, AE, Rezvan, PH, Marshall, AT, Betts, S, Kan, E, et al. Socioeconomic disadvantage and youth mental health during the COVID-19 pandemic lockdown. JAMA Netw Open. (2024) 7:e2420466. doi: 10.1001/jamanetworkopen.2024.20466
31. Bourmistrova, NW, Solomon, T, Braude, P, Strawbridge, R, and Carter, B. Long-term effects of COVID-19 on mental health: a systematic review. J Affect Disord. (2022) 299:118–25. doi: 10.1016/j.jad.2021.11.031
32. Chadda, RK, and Deb, KS. Indian family systems, collectivistic society and psychotherapy. Indian J Psychiatry. (2013) 55:S299–309. doi: 10.4103/0019-5545.105555
33. Sagar, R, and Singh, S. National Tele-Mental Health Program in India: a step towards mental health care for all? Indian J Psychiatry. (2022) 64:117–9. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_145_22
Keywords: mental health, anxiety, depression, post-traumatic stress disease, COVID-19, rural area
Citation: Gahwai D, Dayama S, Mishra A, Chandraker SK, Sahu B, Sharma M and Kumar R (2025) Food scarcity and decrease in income are associated with depression after COVID-19 pandemic in rural settings. Front. Public Health. 13:1526300. doi: 10.3389/fpubh.2025.1526300
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Suvarna Sanjay Sane, ICMR-National Institute of Translational Virology & AIDS Research, IndiaGiulia Menculini, University of Perugia, Italy
Ramji Bogati, Nepal Open University, Nepal
Copyright © 2025 Gahwai, Dayama, Mishra, Chandraker, Sahu, Sharma and Kumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sonal Dayama, c29uYWxkYXlhbWFAZ21haWwuY29t; Ravindra Kumar, cmF2aW5kcmEua3VtQGljbXIuZ292Lmlu
 Dharmendra Gahwai1
Dharmendra Gahwai1 Sonal Dayama
Sonal Dayama Sandip Kumar Chandraker
Sandip Kumar Chandraker Ravindra Kumar
Ravindra Kumar