
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Public Health , 18 February 2025
Sec. Public Mental Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1525165
This article is part of the Research Topic Community Series In Mental-Health-Related Stigma and Discrimination: Prevention, Role, and Management Strategies, Volume III View all 19 articles
Background: Gendered racial microaggressions adversely impact Black college women’s mental health, but less is known about rural Black women’s mental health.
Objective: Examine the association between gendered racism, depression, and psychological distress.
Methods: This cross-sectional study included 200 rural Black women from the Southeastern United States. Gendered racism was assessed using the Gendered Racial Microaggressions scale (GRMS). Linear regression was used to assess GRM subscales, depression (PHQ-9) and psychological distress (K6) as outcomes.
Results: Of the 200, 21.5% reported depression and 31% reported moderate psychological distress. Depression increased with increasing stress appraisal of gendered racism, p = 0.002.
Conclusion: Gendered racial microaggressions impact the mental health of rural Black women.
Despite improvements, Black women in the United States (U.S.) continue to suffer from persistent health disparities. Compared to other women in the U.S., Black women experience excess mortality including shorter life expectancies, higher rates of maternal mortality, cardiovascular disease, and obesity (1). The persistent health disparities reflect the structural inequities Black women face and contribute to their mental health (1–3).
Approximately 18% of U.S. adults have been diagnosed with depression (4). Depression is a major risk factor for suicide and serves as both an individual and community health burden (5). As the leading cause of mental illness and disability, depression is twice as likely to occur in women than in men (6). While there are racial disparities in depressive disorder (6, 7), national depression rates specific to Black women are unclear. National data are reported separately based on race (White Americans and Black Americans) or gender (men and women). Thus, national depression rates in Black women are not ascertainable due to the structural mechanisms of data collection (1). Importantly, one recent study found that depression rates significantly worsened in Black Americans compared to their White counterparts after COVID-19 (7).
Despite its severity, depression is poorly recognized and undertreated due in part to the varying presentation of depressive symptoms (8). There are several hundred possible combinations of symptoms that meet criteria for depression, with depressed mood as the most common presentation. However, in Black women, common depressive symptoms include somatic symptoms, irritability, and present with comorbidities. The differences in the presentation of symptoms further complicate clinical diagnosis and may result in underdiagnosis for Black women (8).
Additionally, past research suggests that stigma leaves Black women, particularly in rural settings, unwilling to discuss mental health issues (9, 10). However, a recent health assessment (11) using a community-based participatory approach found that rural Black women were willing to provide information about mental health, citing it as a significant concern. This suggests that community attitudes toward mental health may be shifting (11).
Mental health is influenced by social and structural factors. According to the CDC, social determinants that increase the likelihood of poor mental health include experiencing interpersonal and institutional discrimination, and lack of access to education, housing, healthcare, employment, and economic opportunities (12). Other risk factors include adverse childhood experiences and other types of interpersonal violence and social isolation (12). Despite experiencing multiple risk factors and being overburdened with social inequities, mental health often goes under-reported in Black Americans (13, 14). A review of the literature revealed that underdiagnosis in Black women impacts prevalence rates (8, 14).
The mental health of Black women is also complicated by structural determinants of health, such as gendered racism (2). Gendered racism is defined as the complex oppression experienced by women of color based on the simultaneity of racism and sexism (15). Gendered racism often manifests as microaggressions. Gendered racial microaggressions (GRM) are subtle and daily verbal, behavioral, and environmental expressions of oppression based on the intersection of one’s race and gender (16). GRM has been related to a myriad of adverse mental health outcomes, including psychological distress and depression (16–21).
Though the mental health impact of experiencing GRM is clear, much of the extant literature is based on college samples and those with higher incomes (16–20). There is a dearth of literature on the relationship between GRM and the mental health of rural Black women in the Southeastern U.S. The purpose of this study is to explore the relationships between gendered racial microaggressions (GRM) and mental health within a rural community sample of Black women.
To understand GRM, we draw from two theoretical frameworks, intersectionality and racial microaggressions. Intersectionality theory (22, 23) has been applied to public health equity research (24, 25). Intersectionality posits that women of color experience multiple, inseparable identities based on race and gender/sex that are tied to multiple marginalizations, such as racism and sexism. An intersectional approach uncovers the health outcomes of women of color made invisible by single-lens metrics that focus on race or gender. Rather, an intersectional lens to health understands that race and gender are inseparable, socially constructed through norms and policies, and vary based on other social identities (e.g., social class, ability, age, immigration history) (25). Thus, gendered racism provides a more complete view of Black women’s experiences of discrimination as it accounts for their gender and race, Gendered racism may be experienced as microaggressions (16). Racial microaggressions theory (26) suggests that subtle forms of oppression are normalized and stem from the idea that racism is normalized, woven into the fabric of American society, and may appear ordinary (15). Identity-based microaggressions include intentional and unintentional insults, putdowns, invalidations, slights, and offensive behaviors as well as through environmental policies and ideologies that cumulatively harm mental health (25).
Depression is severe yet underdiagnosed in Black women. Depressive symptoms often manifest differently in this population due to the influence of social and structural determinants of mental health (33). Absent research that specifically focuses on rural Black women and risk factors such as GRM, prevalence rates will remain unknown. This study aims to determine the prevalence of depression and psychological distress among Black women in rural Alabama and explore the relationship between depression and GRM while controlling for sociodemographic characteristics among Black women in rural Alabama. We also sought to explore the relationship between psychological distress and GRM while controlling for sociodemographic characteristics among Black women in rural Alabama.
As part of a parent community-based participatory research (CBPR) study (11), community health surveys were administered in five rural Alabama communities. The purpose of the CBPR study was to assess health concerns among residents. The study was implemented in partnership with the Alabama Conference of Black Mayors. Community member representatives, selected by their respective mayors because of their knowledge and engagement in their communities, facilitated the data collection process. Convenience sampling was used to recruit participants through a variety of community events. Paper and pencil surveys were distributed at community events organized by the mayors of each community. The events included health fairs, vaccine clinics, and community education meetings. Surveys were also administered via canvassing the community to obtain a representative sample. Each representative completed an orientation process consisting of human subjects research training. Results of the parent study suggested a high prevalence of mental health concerns among residents. In consequence, an additional data-collection phase was added to further identify the mental health concerns of Black women. The University of Alabama’s institutional review board approved this study, protocol #21-03-4465.
Enrolled participants (n = 206) were self-identified Black women living in rural Alabama communities, aged 18 and older. Verbal consent was obtained from all participants before the study commencement.
Inclusion criteria involved self-identification of Black race, female gender, residence in a rural Alabama community among adults over the age of 18. Participants with completed surveys containing non-missing values for depression and psychological distress were eligible for study inclusion. Surveys with missing depression and psychological distress (n = 6) scores were excluded from the analyses. The final analytic sample included 200 participants.
The Gendered Racial Microaggressions Scale (GRMS) is a 26-item multidimensional validated scale that assesses the lifetime frequency and stress appraisal of gendered racial microaggressions (16). A sample item includes: “Someone accused me of being angry when I was speaking in a calm manner.” The GRMS frequency composite is scored using a 6-level response scale, ranging from 0 to 5 where 0 = “never,” 1 = “less than once a year,” 2 = “a few times a year,” 3 = “about once a month,” 4 = “a few times a month,” and 5 = “once a week or more.” The GRMS stress appraisal composite is scored using a 6-level response scale, ranging from 0 to 5 where 0 = “this has never happened to me,” 1 = “not at all stressful,” 2 = “slightly stressful,” 3 = “moderately stressful,” 4 = “very stressful,” and 5 = “extremely stressful.” For each composite, total scores are found by averaging the 26 items; this generates a scoring scale with a range of 0 to 5. GRMS consists of four subscales specific to Black women: beauty assumptions and sexual objectification, silenced and marginalized, Strong Black Woman, and Angry Black Woman. The GRMS frequency (α = 0.95) and stress appraisal (α = 0.97) composites had good internal consistency for this sample (16).
The Patient Health Questionnaire (PHQ-9) assesses the severity of self-reported depressive symptoms over the past two weeks (27). We used eight of the nine questions, known as PHQ-8. The ninth item was deleted as it asks about suicidal attempts and ideation. Although DSM-IV criteria assess suicidal ideation, this item was deemed inappropriate for nonclinical research that lacks the ability to conduct an appropriate intervention (28). A sample item reads, “Over the past two weeks, how often have you been bothered by the following problems? Little interest or pleasure in doing things.” Response categories for each item are based on a 4-point Likert scale where 0 = “not at all,” 1 = “several days,” 2 = “more than half the days,” and 3 = “nearly every day.” Total scores are found by summing the eight items. For scores ≥10, the PHQ-8 has high sensitivity and specificity for depression (27). In this study, scores ≥10 indicate current depression. The PHQ-8 had good internal consistency for this sample (α = 0.91). Higher scores indicate increased depression severity.
The Kessler 6 (K6) is a six-item validated scale that measures non-specific psychological distress (PD) during the past 30 days (29). A sample survey question is, “During the past 30 days, about how often did you feel nervous?” Item responses are based on a 5-point Likert scale from 0 to 4 where 0 = “none of the time” and 5 = “all of the time” (21). Total scores are found by summing the scores from all six questions. Psychological distress scores range from 0 to 24 with scores from 0 to 4 classified as none or low mental distress, scores from 5 to 12 indicating moderate mental distress, and scores ≥13 indicating serious mental distress, possibly warranting further assessment (30). The K6 had good internal consistency for this sample (α = 0.86).
The following sociodemographic characteristics were considered as independent variables in this study: age, education, income, and relationship status. For analysis purposes, we operationalized these variables as follows: age (continuous), education (some high school (reference); high school diploma or GED; some college or college degree), income [≤ $2,999 (reference); $25,000 to $49,999; ≥ $50,000], relationship status [married; not married (reference)]. GRMS frequency and stress appraisal composite scores were also included as covariates.
Descriptive statistics were used to summarize characteristics of the cohort using means and standard deviations for continuous variables and frequencies and percentages for categorical characteristics. We used linear regression to independently examine the association between depression and psychological distress outcomes, GRMS frequency, and stress appraisal composite scores while controlling for age, education, income, and relationship status. We did not impute missing data. Participants missing values for outcome measures were excluded from the analyses. The significance level for comparisons was set at p ≤ 0.05. JMP Pro 18 was used for all analyses.
Participants (N = 200) were Black females and were, on average, 56.6 years (SD = 16.1). The majority (26.3%, n = 45) had completed high school, 21% reported earning a college degree, and 96.7% identified as non-Hispanic. Over half of the sample (51.2%) earned an income of less than $24,999. The relationship status reported by most participants (31.5%) was married; see Table 1.
In this sample, the mean depression score was 6.0 (SD = 6.3, Range: 0–24) with 43 (21.5%) reporting depression (PHQ-8 ≥ 10). For psychological distress, 13 (6.5%) reported serious (K6 ≥ 13), 62 (31%) reported moderate (K6: 5–12), and 125 (62.5%) reported none to low mental distress, with a mean of 4.5 (SD = 4.7, Range: 0–24), Table 1. The GRMS composite subscale of stress appraisal was positively correlated with depression, r (127) = 0.27, p = 0.002, but not with frequency (p = 0.237). As stress appraisal increases, depression increases. Neither GRMS frequency nor stress appraisal was significantly correlated with PD, all p > 0.05; see Table 2.
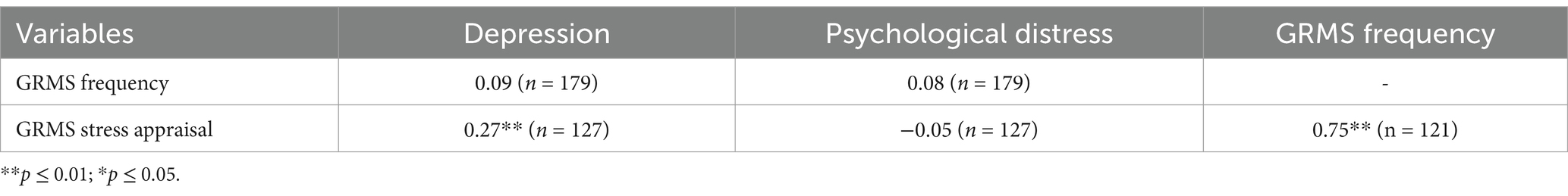
Table 2. Correlations of composite GRMS stress appraisal and frequency, depression, and psychological distress.
GRMS frequency and stress appraisal were assessed in different models per outcome as they were highly correlated. Due to multicollinearity, income was not included in the regression models. The final regression models best explain the variation in depression, psychological distress, GRM, and demographic characteristics. Missingness among GRMS frequency and stress appraisal composite scores was evaluated in this sample. Neither were associated with model covariates nor outcomes, all p ≥ 0.05.
Depression was significantly associated with GRMS stress appraisal, [F (1, 125) = 10.1, R2 = 0.074, p = 0.002]. For every unit increase in stress appraisal, depression scores increased by 1.2 units; see Table 3. Models containing GRMS frequency and other covariates were not statistically significant, p > 0.05.
Psychological distress was significantly associated with education, but not with GRMS stress appraisal (p = 0.9212), [F (3, 104) = 2.7, R2 = 0.072, p = 0.0483]. Compared to those who completed some high school, participants with some college or a college degree saw a decrease of 3.5 units in psychological distress scores, and participants with a high school diploma or GED saw a decrease of 1.5 units; see Table 4. In a separate model, psychological distress was significantly associated with education, but not with GRMS frequency, age (p = 0.0779), or relationship status (p = 0.4055), [F (5, 136) = 2.5, R2 = 0.084, p = 0.0331]. Compared to those who completed some high school, participants with some college or a college degree saw a decrease of 3 units in psychological distress scores, and participants with a high school diploma or GED saw a decrease of 1.1 units; see Table 5.
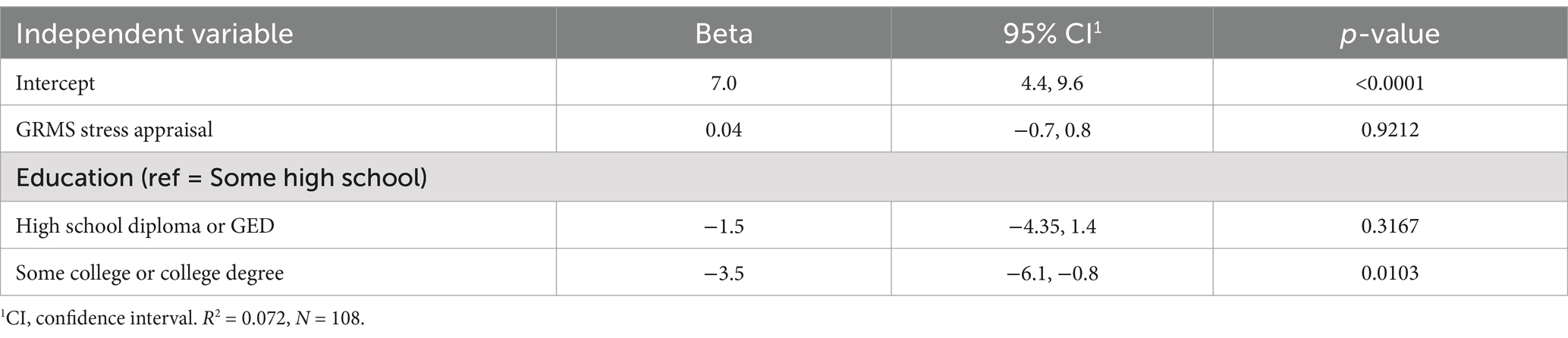
Table 4. Linear regression analysis of GRMS stress appraisal, sociodemographic characteristics, and psychological distress.
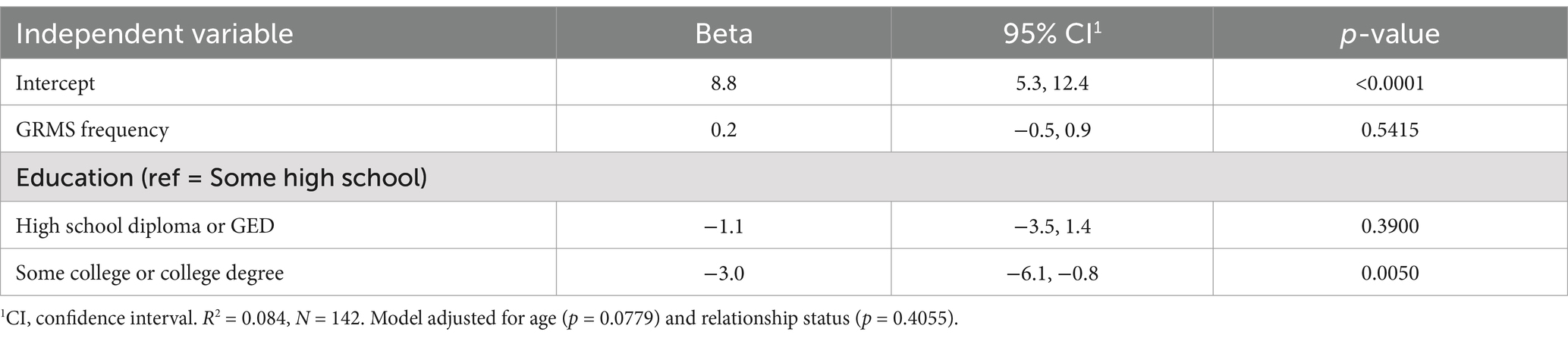
Table 5. Linear regression analysis of GRMS frequency, sociodemographic characteristics, and psychological distress.
To explore whether GRM impacts rural Black women’s mental health, we first examined the rates of self-reported depression and psychological distress. In this sample, approximately 21.5% reported depression and approximately 38% reported moderate or serious psychological distress. While depression rates in this sample are similar to the average in the state of Alabama (24%) in 2020, the current findings add nuance to state and national-level data on depression. National and state prevalence tends to vary by age and race (5). Typically, younger adults (21.5%) have higher rates than older adults (14.2%), and White adults (21.9%) have higher rates than Black adults (16.2%) (5). Given this sample’s older average age of 56 years and race, one might expect lower depression rates as suggested by national trends. However, our findings suggest that older, Black women’s rate of depression is higher than expected.
In addition to depression, PD was also prevalent in this sample, with 31% indicating moderate PD. Moderate PD has been deemed clinically meaningful because it optimally identifies individuals needing mental health treatment. Further, those in the moderate category are at risk for substance use, sedentary behavior, and obesity further underscoring the link between mental and physical health (30).
Current findings suggest that GRM is associated with depression. The stressfulness of GRM accounted for 7.4% of the variance in depression. While GRM was not associated with psychological distress, our results indicate that rural Black women who have completed some college or have obtained a college degree have lower mental distress than those who completed some high school. Substantial evidence has been presented on education as a social determinant of health (1, 12) and our research supports the buffering impact of increased education on mental distress. These findings add to the growing body of literature that supports GRM’s association with adverse mental health outcomes (16–21, 31).
This study must be viewed in light of some limitations that could be addressed in future research. First, participant data was captured at a single point in time using a cross-sectional study design. Therefore, we were not able to assess how the relationship between GRM and mental health outcomes changes over time. Second, convenience sampling was used to enroll participants, resulting in sampling bias. Thus, our results may not be generalizable to Black women residing in non-rural counties or outside the state of Alabama. Third, our survey utilized self-report instruments, increasing the potential for response bias. Consequently, participant responses may not accurately reflect mental health dispositions. Finally, we did not ask participants about their personal experiences of gendered racism and their effect on overall well-being. Future studies should employ longitudinal designs with a qualitative component to track participant metrics in a comprehensive manner. Including participant narratives will help close the gap in our understanding of the complex relationship between mental health and experiences of gendered racial microaggressions in this population. In addition, simple random sampling methods and objective metrics for mental health outcomes may also be employed to enhance the generalizability of study results. Despite the limitations of our study, our findings add to the mental health literature on the structural inequities rural Black women face that may harm their mental health.
According to the CDC, 18.4% of US adults reported having ever been diagnosed with depression. Furthermore, Alabama ranks in the top 10 states with the highest prevalence of depression (5). The prevalence rates of depression and psychological distress in this sample of rural Black women emphasize the importance of not only allocating resources to the areas of greatest need (5) but to do so using an intersectional approach to mental health interventions (32) to account for the inequities associated with gendered racism. While national data reports stratify mental health prevalence rates by age, ethnicity, gender, etc., the mental health prevalence of the intersection of these groups, such as Black women, is not presented with these results. This gap in the national data collection mechanism warrants the need for exploratory studies that aim to capture and describe the mental health of specific subgroups while considering how the social and structural determinants of health influence the well-being of the population. Results from such studies will help inform culturally sensitive interventions designed to impact these populations in a meaningful way.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the University of Alabama Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because data were collected at health fairs and other community events. Participants provided verbal assent.
CE: Data curation, Formal analysis, Writing – original draft, Conceptualization, Methodology, Software, Writing – review & editing, Validation, Visualization. WB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft. SN: Funding acquisition, Resources, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This project was supported by the Office of Minority Health of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $2.9 M with 100 percent funded by HHS (# CPIMP211265) awarded to the Town of Fort Deposit.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
The authors declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HHS, or the U.S. Government. For more information, please visit https://www.minorityhealth.hhs.gov/.
1. Chinn, JJ, Martin, IK, and Redmond, N. Health equity among black women in the United States. J Women's Health. (2021) 30:212–9. doi: 10.1089/jwh.2020.8868
2. Lewis, JA, Williams, MG, Peppers, EJ, and Gadson, CA. Applying intersectionality to explore the relations between gendered racism and health among black women. J Couns Psychol. (2017) 64:475–86. doi: 10.1037/cou0000231
3. Ricci, F, Torales, J, Bener, A, Castaldelli-Maia, JM, Chumakov, E, Bellomo, A, et al. Mental health of ethnic minorities: the role of racism. Int Rev Psychiatry. (2023) 35:258–67. doi: 10.1080/09540261.2023.2189951
4. Moreno-Agostino, D, Wu, YT, Daskalopoulou, C, Hasan, MT, Huisman, M, and Prina, M. Global trends in the prevalence and incidence of depression: a systematic review and meta-analysis. J Affect Disord. (2021) 281:235–43. doi: 10.1016/j.jad.2020.12.035
5. Lee, B, Wang, Y, Carlson, SA, Greenlund, KJ, Lu, H, Liu, Y, et al. National, state-level, and county-level prevalence estimates of adults aged ≥18 years self-reporting a lifetime diagnosis of depression — United States, 2020. MMWR Morb Mortal Wkly Rep. (2023) 72:644–50. doi: 10.15585/mmwr.mm7224a1
6. Weaver, A, Himle, JA, Taylor, RJ, Matusko, NN, and Abelson, JM. Urban vs rural residence and the prevalence of depression and mood disorder among African American women and non-Hispanic white women. JAMA Psychiatry. (2015) 72:576–83. doi: 10.1001/jamapsychiatry.2015.10
7. Thomeer, MB, Moody, MD, and Yahirun, J. Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. J Racial Ethnic Health Disparities. (2023) 10:961–76. doi: 10.1007/s40615-022-01284-9
8. Perez, NB, Melkus, GDE, Wright, F, Yu, G, Vorderstrasse, AA, Sun, YV, et al. Latent class analysis of depressive symptom phenotypes among black/African American mothers. Nurs Res. (2023) 72:93–102. doi: 10.1097/NNR.0000000000000635
9. Crumb, L, Mingo, TM, and Crowe, A. “Get over it and move on”: the impact of mental illness stigma in rural, low-income United States populations. Mental Health Prevention. (2019) 13:143–8. doi: 10.1016/j.mhp.2019.01.010
10. Planey, AM, Smith, SM, Moore, S, and Walker, TD. Barriers and facilitators to mental health help-seeking among African American youth and their families: a systematic review study. Child Youth Serv Rev. (2019) 101:190–200. doi: 10.1016/j.childyouth.2019.04.001
11. Newman, SD, Moss, K, Pichon, M, Scott, D, Rogers, K, Orr, A, et al. The health of rural black communities during COVID: some affirmations, some surprises. Front Pub Health. (2023) 11:932451. doi: 10.3389/fpubh.2023.932451
12. Centers for Disease Control and Prevention (CDC). (2024). Content Source: National Center for Injury Prevention and Control. Available at: https://www.cdc.gov/mental-health/about/index.html (Accessed August 8, 2024).
13. Erving, CL, Thomas, CS, and Frazier, C. Is the black-white mental health paradox consistent across gender and psychiatric disorders? Am J Epidemiol. (2019) 188:314–22. doi: 10.1093/aje/kwy224
14. Phimphasone-Brady, P, Page, CE, Ali, DA, Haller, HC, and Duffy, KA. Racial and ethnic disparities in women’s mental health: a narrative synthesis of systematic reviews and meta-analyses of the US-based samples. Fertil Steril. (2023) 119:364–74. doi: 10.1016/j.fertnstert.2023.01.032
15. Essed, P. Understanding everyday racism: An interdisciplinary theory, vol. 2. Newbury Park, CA: Sage (1991).
16. Lewis, JA, and Neville, HA. Construction and initial validation of the gendered racial microaggressions scale for black women. J Couns Psychol. (2015) 62:289–302. doi: 10.1037/cou0000062
17. Burton, WM, Paschal, AM, Jaiswal, J, Leeper, JD, and Birch, DA. Gendered racial microaggressions and black college women: a cross-sectional study of depression and psychological distress. J Am Coll Heal. (2022) 72:1–8. doi: 10.1080/07448481.2022.2133567
18. Jones, MK, Leath, S, Settles, IH, Doty, D, and Conner, K. Gendered racism and depression among black women: examining the roles of social support and identity. Cult Divers Ethn Minor Psychol. (2022) 28:39–48. doi: 10.1037/cdp0000486
19. Watson, NN, and Hunter, CD. Anxiety and depression among African American women: the costs of strength and negative attitudes toward psychological help-seeking. Cultur Divers Ethnic Minor Psychol. (2015) 21:604–12. doi: 10.1037/cdp0000015
20. Woods-Giscombé, CL, and Lobel, M. Race and gender matter: a multidimensional approach to conceptualizing and measuring stress in African American women. Cult Divers Ethn Minor Psychol. (2008) 14:173–82. doi: 10.1037/1099-9809.14.3.173
21. Szymanski, DM, and Lewis, JA. Gendered racism, coping, identity centrality, and African American college women’s psychological distress. Psychol Women Q. (2016) 40:229–43. doi: 10.1177/0361684315616113
22. Crenshaw, K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev. (1991) 43:1241–99. Collins 2000
23. Collins, PH. Black feminist thought: Knowledge, consciousness, and the politics of empowerment. 2nd ed. New York and London: Routledge (2000).
24. Bauer, GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. (2014) 110:10–7. doi: 10.1016/j.socscimed.2014.03.022
25. Bowleg, L. The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health. (2012) 102:1267–73. doi: 10.2105/AJPH.2012.300750
26. Sue, DW, Capodilupo, CM, and Holder, A. Racial microaggressions in the life experience of black Americans. Prof Psychol Res Pr. (2008) 39:329–36. doi: 10.1037/0735-7028.39.3.329
27. Kroenke, K, Spitzer, RL, and Williams, JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
28. Kroenke, K, Strine, TW, Spitzer, RL, Williams, JB, Berry, JT, and Mokdad, AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. (2009) 114:163–73. doi: 10.1016/j.jad.2008.06.026
29. Kessler, RC, Green, JG, Gruber, MJ, Sampson, NA, Bromet, E, Cuitan, M, et al. Screening for serious mental illnesses in the general population with the K6 screening scale: results for the WHO world mental health (WMH) survey initiative. Int J Methods Psychiatr Res. (2010) 19:4–22. doi: 10.1002/mpr.310
30. Prochaska, JJ, Sung, HY, Max, W, Shi, Y, and Ong, M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res. (2012) 21:88–97. doi: 10.1002/mpr.1349
31. Keum, BT, and Wong, MJ. Congruence and discrepancy in Asian American women's perception and stress appraisal of gendered racial microaggressions: relationships with depressive symptoms and internalized racism. Front Public Health. (2022) 10:954897. doi: 10.3389/fpubh.2022.954897
32. Burton, WM. Gendered racism: a call for an intersectional approach. J Psychosoc Nurs Ment Health Serv. (2022) 60:3–4. doi: 10.3928/02793695-20221109-01
Keywords: rural, women, Black – African, microaggressions, mental health, depression, gendered racism, social determinants of health
Citation: Ezemenaka CJ, Burton WM and Newman S (2025) Exploring gendered racism and the mental health of rural Black women. Front. Public Health. 13:1525165. doi: 10.3389/fpubh.2025.1525165
Received: 08 November 2024; Accepted: 03 February 2025;
Published: 18 February 2025.
Edited by:
Samer El Hayek, American Center for Psychiatry and Neurology, United Arab EmiratesReviewed by:
Stacie Craft DeFreitas, Prairie View A&M University, United StatesCopyright © 2025 Ezemenaka, Burton and Newman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wanda Martin Burton, d21idXJ0b25AdWEuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.