
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Public Health , 18 March 2025
Sec. Digital Public Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1524616
This article is part of the Research Topic Extracting Insights from Digital Public Health Data using Artificial Intelligence, Volume III View all 11 articles
Introduction: The application of artificial intelligence (AI) in public health is rapidly evolving, offering promising advancements in various public health settings across Canada. AI has the potential to enhance the effectiveness, precision, decision-making, and scalability of public health initiatives. However, to leverage AI in public health without exacerbating inequities, health equity considerations must be addressed. This rapid narrative review aims to synthesize health equity considerations related to AI application in public health.
Methods: A rapid narrative review methodology was used to identify and synthesize literature on health equity considerations for AI application in public health. After conducting title/abstract and full-text screening of articles, and consensus decision on study inclusion, the data extraction process proceeded using an extraction template. Data synthesis included the identification of challenges and opportunities for strengthening health equity in AI application for public health.
Results: The review included 54 peer-review articles and grey literature sources. Several health equity considerations for applying AI in public health were identified, including gaps in AI epistemology, algorithmic bias, accessibility of AI technologies, ethical and privacy concerns, unrepresentative training datasets, lack of transparency and interpretability of AI models, and challenges in scaling technical skills.
Conclusion: While AI has the potential to advance public health in Canada, addressing equity is critical to preventing inequities. Opportunities to strengthen health equity in AI include implementing diverse AI frameworks, ensuring human oversight, using advanced modeling techniques to mitigate biases, fostering intersectoral collaboration for equitable AI development, and standardizing ethical and privacy guidelines to enhance AI governance.
The use of artificial intelligence (AI) in public health is rapidly evolving, offering promising advancements in surveillance, research, policy, and programming that enhance effectiveness, precision, decision-making, and scalability (1). AI refers to technologies that enable computers and machines to simulate human intelligence and problem-solving capabilities, employing methods such as computer vision, natural language processing, and machine learning (ML) (2–5). ML, a field of AI, develops models for prediction and clustering by using a learning dataset, which includes data split into training, validation, and test sets, to train and evaluate algorithms (6). The training data is a specific subset of the learning dataset used directly to teach the model, enabling it to recognize patterns and relationships within the data (4).
Health equity aims to create equal opportunities for all by eliminating unfair, avoidable differences in health status and life expectancy between socially advantaged and disadvantaged groups, involving efforts both within and beyond the health sector (7). As AI application in public health increases, it is crucial to address health equity considerations to ensure its effective use, without exacerbating existing inequities among priority populations (8, 9). Priority populations are communities who are placed at greater risk of adverse health outcomes due to overlapping and intersecting systems of oppression, including persons with disabilities, 2SLGBTQI+ communities, racialized people, and First Nations, Inuit, and Métis, among others (10).
The use of AI in public health raises several equity concerns, including algorithmic bias, transparency and interpretability of models, and accessibility of AI technologies, bringing into question significant ethical, regulatory, and privacy concerns (11, 12). Addressing these issues is crucial to ensuring that AI contributes to improving public health outcomes for all, rather than reinforcing existing societal inequities and vulnerabilities. Therefore, this review aims to synthesize health equity considerations in the application of AI in public health, offering timely insights as AI adoption accelerates.
A rapid narrative review was conducted to synthesize the evidence on health equity considerations related to AI in public health. A rapid review is a form of knowledge synthesis that accelerates the process of conducting a traditional review to produce evidence in a resource-efficient manner (13). The rapid narrative review protocol was informed by Arksey and O’Malley’s (14) methodological framework and Peters et al.’s (15) updated guidelines and consists of the following steps: scoping, searching, screening, and data extraction and analysis.
A preliminary search using the terms AI, public health, and health equity was conducted in the Government of Canada’s Health Library. Eligibility criteria was established using the populations, issue, context, outcomes (PICO) framework, with the goal of identifying studies that met two main criteria: (1) the use of AI in a public health setting and (2) the explicit or implicit integration of health equity considerations (e.g., biases, privacy, transparency, discrimination). English articles published in Canada between 2014 and 2024 specific to AI application in public health settings were included, while studies published in the same time frame conducted in healthcare, telemedicine, or biomedical settings were excluded for lacking sufficient evidence on health equity related to AI in public health.
A librarian from the Government of Canada’s Health Library developed and executed the search strategy. The search was conducted in Medline and Embase for studies published between January 1, 2014 and June 20, 2024, using search strings related to AI, public health, and health equity (Appendix A). Results were imported into Zotero for management. A grey literature search using search strings related to AI, public health, and health equity was also conducted between May 21, 2024 to July 24, 2024, through targeted website searches, browser keyword searches (including the first 10 pages of Google Scholar), and by identifying literature from cited results.
Screening was conducted in two phases. In level one, titles and abstracts were screened in Covidence (16), with eligible studies moving to full-text review in level two. To ensure inter-rater reliability, MM and SG screened the first 20% of titles and abstracts, resolving discrepancies through discussion. MM then screened the remaining titles and abstracts, discussing ambiguous articles with SG. For level two, MM and DG conducted full-text reviews of the first 10 studies in duplicate, resolving any discrepancies through discussion. MM screened the remaining full-text articles, and any ambiguities were resolved through discussion with SG and DG.
Data was extracted on study characteristics (first author, publication year, study objective, design, and location), public health setting, and health equity considerations. Health equity considerations were based on the Government of Canada’s Health Portfolio Sex- and Gender-Based Analysis Plus (SGBA Plus), an intersectional, analytical framework, which outlines health equity considerations at various levels, including individual social identities, group membership, social context, and systems of oppression (Figure 1) (17). Originating from Black feminist studies, intersectionality theory acknowledges that systems and structures of power, such as racism, sexism, classism, and ableism, do not operate independently (18). Instead, they intersect and overlap, to create distinct experiences of privilege and discrimination based on one’s multi-dimensional identities and social positionality, such as race, ethnicity, gender, socio-economic status, and disability (18). MM extracted data from all studies with guidance from SG. A descriptive analysis was conducted to synthesize key health equity considerations for AI in public health.
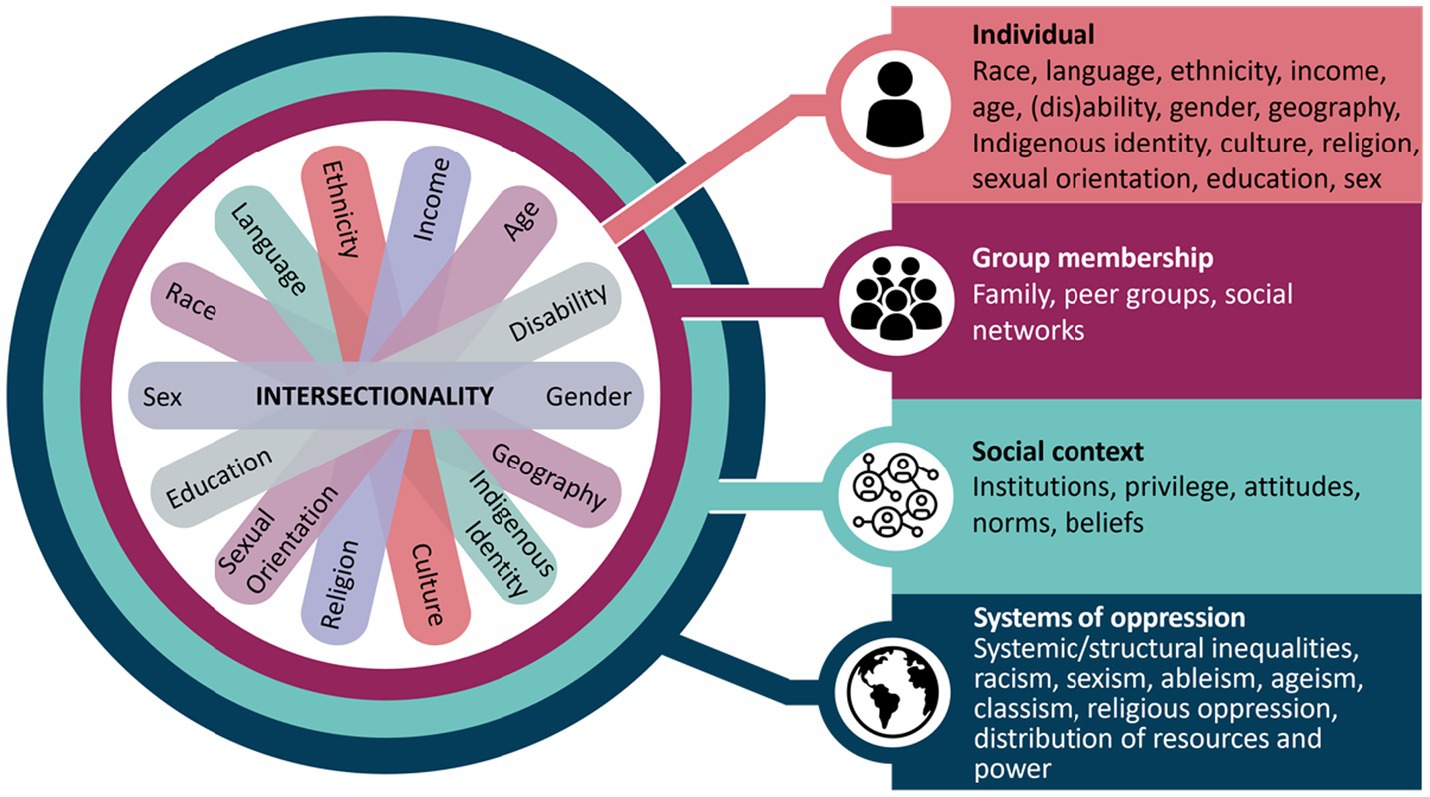
Figure 1. SGBA Plus intersectionality wheel and flower. This figure illustrates some of the determinants of health that intersect to shape our experiences and realities. A figure depicting social identities is centered within a concentric circle of four layers. From the center of the circle, and moving outwards, the figure describes intersectionality considerations related to individual-level factors, group membership, social context, and systems of oppressions, that is, from individual identities to increasingly broad levels of influence. At the center, seven oblong shapes of differing colors overlap and fan out. At the end of each oblong an individual social identity is named. The individual social identities named on the figure are sex, race, language, ethnicity, income, age, (dis) ability, gender, geography, Indigenous identity, culture, religion, sexual orientation, and education. The second layer of the circle directly surrounding the individual social identities is “Group membership” with the following examples listed: family, peer groups, and social networks. The third layer of the circle surrounding group membership is “Social context” with the following examples listed: institutions, privilege, attitudes, norms, and beliefs. The outermost level, which surrounds social context is “systems of oppression,” with the following examples listed: systemic/structural inequalities, racism, sexism, ableism, ageism, classism, religious oppression, and distribution of resources and power. Reprinted with permission from “Integrating Health Equity into Funding Proposals: A Guide for Applicants”, Canada. ca, 2024.
A total of 263 articles were identified in a Canadian-based search on equity considerations in the use of AI within public health policy, programs, research, surveillance, and initiatives. This total includes 56 references from other sources, including grey literature and citation searching, as well as seven additional relevant articles identified on July 12, 2024, when SG and MM refined the search strategy with the librarian.
After removing 43 duplicates and 1 redacted article, 233 articles were excluded during level one screening for not meeting eligibility, with common reasons being their focus on healthcare settings, advanced statistical methods without AI, or different use of the acronym “AI” (e.g., Alaskan Indian or American Indian). In level two screening, 32 more articles were excluded for not addressing health equity considerations related to AI use in public health. In total, 54 peer-review articles and grey literature articles were included for analysis.
The review was conducted according to the PRISMA Flow Diagram derived from Covidence (Figure 2) (19). Most studies highlighted health equity considerations related to social context and systems of oppression when using AI in public health (Appendix B).
Mainstream AI is often grounded in Western epistemology, limiting its scope to specific frameworks and datasets (20, 21). For example, AI systems are typically better at processing English data compared to other languages, which restricts the diversity of knowledge and perspectives interpreted (22, 23). This individualistic approach, rooted in Western epistemology, also fails to consider community-based outcomes or the human-AI relationship (20, 21, 24, 25). Bavli and Galea (26) noted that generative AI, like ChatGPT tends to adopt a pro-environmental, left-libertarian ideology, which can lead to biased outputs. Moreover, Indigenous communities and research organizations have found that AI systems neglect Indigenous knowledge systems, such as Two-Eyed Seeing or the Seventh Generation Principle (20, 27). This risks perpetuating biases that can further marginalize priority populations, such as Indigenous Peoples, racialized communities, 2SLGBTQI+ communities, and women (8, 22, 28–30).
Due to gaps in AI epistemology, biases exist throughout the AI lifecycle. Studies highlight various biases in AI, including omitted variable bias, sampling bias, ascertainment bias, selection bias, and measurement errors (9, 31–33). These biases can emerge during the development of AI and its algorithms, often resulting from limited datasets, implicit developer bias, or intentional programming (6, 9, 12, 28, 29, 32, 34–40). Since bias can manifest at any stage of the lifecycle, it complicates the identification of biased outputs and the methods by which biases were introduced into the system (37, 41).
Biases in AI often reflect systems of oppression, such as racism, sexism, and socioeconomic discrimination, exacerbating gender and racial inequalities (6, 8, 12, 39, 41). For instance, Luccioni and Bengio (8) noted a 34.4% error rate in facial recognition technologies for darker-skinned females compared to lighter-skinned males. Text embedding in AI has also been reported to perpetuate gender stereotypes by associating certain statements or terms to a gender (8, 22, 41–43). Unaddressed biases in AI can further exacerbate health inequities in public health decision-making, research, surveillance, resource allocation, and contact tracing (22, 28, 34).
Inequitable access to AI technology and its impacts, known as the “digital divide,” deepens systemic inequities (44, 45). Groups commonly lacking access to AI technologies include those in northern, rural, and remote regions, those with lower socioeconomic status, and older adults (6, 33, 45, 46). For example, public health systems in remote areas, such as Yukon, face limited AI resources and workforce capacity, resulting in outdated technologies that delay public health decision-making, precise surveillance, and early interventions (33, 39, 45, 46).
The data used to train AI models can also reflect these disparities, as available data often excludes priority populations, such as Indigenous Peoples, racialized communities, older adults, and those living on low incomes with limited access to technology (12, 23, 47–49). This exclusion limits representation and access to AI knowledge and skills for priority populations (39, 50).
Additionally, AI technologies contribute to ecological burden disproportionately impacting priority populations who are environmentally vulnerable to climate-related events (22, 41, 44, 51). Furthermore, companies often engaging in inequitable labor practices to rapidly develop AI technologies, exacerbate and perpetuate socio-economic inequalities in the Global South and perpetuate colonial practices through resource exploitation and control (22, 39, 41). This deepens the “digital divide” and worsens health inequities among priority populations.
Institutional lag has occurred as AI implementation in public health has outpaced the development of ethical and privacy guidelines (8, 12, 35, 52). Inconsistencies and non-standardized guidelines across institutions are driven by differing cultural and societal values (8, 9, 31, 53, 54). This has resulted in the use of competitive AI technologies that raise ethical and privacy concerns, such as unregulated data mining, copyright issues, and security breaches, which can perpetuate health inequities (22, 27, 30, 34, 46, 55–57). For instance, Gómez-Ramírez et al. (46) demonstrated that facial recognition technology and “immunity passports” during COVID-19 compromised privacy, equity, and human rights, restricted movement and access to services, and eroded public trust, ultimately undermining other effective public health interventions (29). The lack of accountability mechanisms worsens this mistrust, as there are no enforceable regulations to hold institutions liable for AI-related harms (26, 29, 46, 53, 58).
A key challenge in advancing AI in public health is the limited availability of representative data sets for training and use (6, 22, 58, 59). Available data sets often exclude priority populations, including Indigenous Peoples, racialized communities, 2SLGBTQI+ communities, women, and varying age groups (30, 32, 37). Institutional gatekeeping, high costs, and lack of anonymization further restrict access to robust disaggregated data (25, 26, 32, 38, 42, 58–61). Consequently, organizations often rely on lower quality data that fail to capture socio-demographic factors, leading to inaccurate AI outcomes and the potential for bias (22, 42, 52). For example, Gurevich et al. (6) found that training data often reflects predominately White populations, excluding race-based data. Additionally, studies using natural language processing (NLP) often overlooked older adults, youth, and non-English speakers, limiting the use of disaggregated data (23, 25, 31, 47–49). The omission of social determinants of health from training data, such as socioeconomic status, disability, gender, further limits equitable AI (6, 34). Ethical and privacy concerns, regarding the misuse of disaggregated data, contribute to public mistrust, deterring priority populations from participating in data collection, which perpetuates health inequities (46).
It is important to consider the outputs of AI in public health settings, as its lack of interpretability, often described as a “black box,” obscures the reasoning behind results (9, 32, 34, 41, 42, 58, 59). This lack of transparency can perpetuate biases, stereotypes, and discrimination, hindering equitable public health decision-making and implementation. Furthermore, inadequate training data and algorithms can lead to “hallucinations,” which are fabricated data that contribute to misinformation and public mistrust (22, 26, 41). For example, generative AI, including Chat-GPT, has been shown to provide inaccurate information about the COVID-19 pandemic, vaccines, and other public health-related topics (26, 41, 43, 62–64).
Digital literacy and technical skills, combined with public health expertise, are essential for understanding AI systems and preventing adverse outcomes among priority populations. Barriers such as inadequate training, limited funding, lack of infrastructure, and insufficient resources hinder public health professionals from enhancing their technical skills, potentially leading to health equity gaps (22, 32, 33, 38, 46). This leads practitioners to rely on AI developers who may lack public health expertise and hold implicit biases (12, 32, 35, 58). A lack of technical skills, coupled with a non-diverse team that overlooks social and structural determinants of health, can delay equitable AI advancements for priority populations (12, 31, 32, 58).
It is essential to explicitly prioritize health equity in AI technologies for public health, to adequately address issues related to social and structural determinants of health in AI (20, 21, 29, 30, 32, 34, 37, 41, 65). This includes maintaining human oversight throughout the AI lifecycle to reduce biases, system vulnerabilities, and epistemological gaps (12, 22, 34, 41, 66). Involving disproportionately impacted priority populations during the development and validation phases ensures the representation of diverse perspectives, while supporting the identification of potential biases before implementation (21, 31, 32, 35, 41, 58, 66). This approach can also provide social and economic opportunities for those affected by the “digital divide” (58).
Bias mitigation strategies include model interpretability, fairness-aware causal modeling, and incorporating social and structural determinants of health into training data when available (6, 8, 12, 20, 22, 29–32, 34, 36, 38, 41, 42, 52). Acknowledging bias when it cannot be fully mitigated ensures accountability and fosters discussion about AI’s appropriateness in various public health settings (29, 30, 42, 57).
Ethical AI governance requires standardized guidelines centered on privacy, security, and human well-being, alongside substantial investment in AI safety, research, training, and infrastructure (50). Adopting the fair, accountable, secure, transparent, educated, and relevant (FASTER) principles throughout governance structures can promote equitable AI (22, 25, 30, 42, 56, 58, 65). A centralized AI governance body, regular testing, and standardized guidelines are also critical for enhancing accountable, secure, fair, and relevant AI (38, 42, 44, 57, 58, 65, 67).
To enhance transparency, AI models should be interpretable, using techniques like decision trees and Gaussian processes to address “black-box” issues (12, 52, 58, 68). Intersectoral collaboration across sectors can promote data transparency, capacity building, strengthen peer review, and support knowledge exchange between public health professionals and AI developers (12, 30, 32, 35, 36, 38, 41, 42, 56, 58, 62, 67).
While Canada is prioritizing AI development and implementation, it is lagging in addressing challenges related to its use in public health and across social policy more broadly (24). Biases, unrepresentative datasets, and institutional lag are barriers to integrating health equity in AI for public health. Opportunities include adopting FASTER principles to strengthen ethical, security, and privacy guidelines, enhancing AI governance, and promoting intersectoral collaboration. However, implementing these opportunities in practice remains uncertain. For example, addressing the “digital divide” in remote regions by providing AI technology and engaging with communities requires sustained technological and workforce resources, both of which are currently limited (33, 39, 45, 46). Furthermore, the environmental impact of new technologies and the difficulty of standardizing guidelines across sectors could delay progress, risking deepening inequities as AI advances.
Biases in AI are particularly concerning given that they can be introduced at any point during the AI lifecycle, influencing decisions that can exacerbate inequities (37, 41). Thomasian et al. (12) describes this as the “submerged state,” where discrimination goes unnoticed but influences key public health decisions, such as how resources are allocated, and which priority populations receive interventions. Left unaddressed, these biases could further marginalize priority populations by skewing early intervention efforts, resource distribution, and data collection. A concern is whether adopting AI may shift public health priorities, focusing more on disease control and less on addressing social and structural determinants of health and equity. Without adequate disaggregated data collection on priority populations, AI risks perpetuating existing inequities. Future research should explore how AI interacts with socio-demographic factors to ensure these variables are accurately represented in AI training datasets without compromising privacy.
The study has limitations. Not all articles were screened by two independent reviewers, introducing potential selection bias. Additionally, the academic search terms were also limited, potentially missing relevant studies. The search strategy for the evidence synthesis was restricted to studies that mentioned geographic location in Canada in the title, abstract, or keywords. This limits the generalizability of findings, as it excludes international perspectives and insights that could broaden the understanding of effective practices. Moreover, limiting this review to English-language articles may have excluded relevant French-language research, introducing potential language bias. However, some gaps were addressed by revising search terms with the help of a librarian. Furthermore, the emerging nature of the topic meant a limited number of articles met the eligibility criteria, forcing reliance on grey literature and handpicked studies, further contributing to selection bias. Despite these limitations, the study offers critical insights into the integration of health equity in AI for public health.
This review contributes to a rapidly evolving field, addressing a gap by examining health equity in AI. By adopting an intersectional lens, it offers valuable insights for public health professionals, researchers, and organizations, helping guide decision-making for developing equitable AI practices. The inclusion of both academic and grey literature enriches the analysis, capturing diverse perspectives, often absent from academic discourse. This broader approach provides a more comprehensive understanding of health equity implications in AI.
AI can advance public health in Canada, but health equity must be considered to avoid deepening inequities among priority populations. Key challenges include gaps in AI epistemology, biases across the AI lifecycle, the “digital divide,” unrepresentative training datasets, and ethical and privacy concerns. These issues disproportionately impact priority populations, including Indigenous Peoples, racialized communities, 2SLGBTQI+ communities, women, those living on low-incomes, youth, older adults, and those in northern, rural, and remote regions. Opportunities to strengthen equity in AI include implementing diverse frameworks, ensuring human oversight throughout the AI lifecycle, using advanced modeling techniques to mitigate biases, promoting intersectoral collaboration to develop equitable AI, and standardizing ethical and privacy guidelines to enhance AI governance. Future research should explore the feasibility of these equity-informed approaches and the impact of using disaggregated data in testing datasets to enhance AI models.
SG: Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. MM: Conceptualization, Project administration, Methodology, Formal analysis, Writing – original draft, Writing – review & editing. DG: Formal analysis, Writing – review & editing. JR: Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This study was led by employees working at Public Health Agency of Canada with no additional funding from grants. No funds, grants, or other support was received.
The authors thank Anne Summerhays from the Government of Canada Health Library for her assistance with the literature review search.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1524616/full#supplementary-material
1. Olawade, DB, Wada, OJ, David-Olawade, AC, Kunonga, E, Abaire, O, and Ling, J. Using artificial intelligence to improve public health: a narrative review. Front Public Health. (2023) 11:1196397. doi: 10.3389/fpubh.2023.1196397
2. Sarker, IH. Deep learning: a comprehensive overview on techniques, taxonomy, applications and research directions. SN Comput Sci. (2021) 2:420. doi: 10.1007/s42979-021-00815-1
3. Sarker, IH. AI-based modeling: techniques, applications and research issues towards automation, intelligent and smart systems. SN Comput Sci. (2022) 3:158. doi: 10.1007/s42979-022-01043-x
4. Alzubaidi, L, Zhang, J, Humaidi, AJ, Al-Dujaili, A, Duan, Y, Al-Shamma, O, et al. Review of deep learning: concepts, CNN architectures, challenges, applications, future directions. J Big Data. (2021) 8:53. doi: 10.1186/s40537-021-00444-8
5. Sarker, IH. Machine learning: algorithms, real-world applications and research directions. SN Comput Sci. (2021) 2:160. doi: 10.1007/s42979-021-00592-x
6. Gurevich, E, El Hassan, B, and El Morr, C. Equity within AI systems: what can health leaders expect? Healthc Manage Forum. (2022) 36:119–24. doi: 10.1177/08404704221125368
7. Whitehead, M. The concepts and principles of equity and health. Int J Health Serv Plan Adm Eval. (1992) 22:429–45. doi: 10.2190/986L-LHQ6-2VTE-YRRN
8. Luccioni, A, and Bengio, Y. On the morality of artificial intelligence. IEEE Technol Soc Mag. (2020) 39:16–25. doi: 10.1109/MTS.2020.2967486
9. Hernandez, A. Public health practitioners’ adoption of artificial intelligence: The role of health equity perceptions and technology readiness. Georgia State University; (2024), Available at: https://scholarworks.gsu.edu/bus_admin_diss/202/
10. Government of Canada. Health portfolio sex and gender-based analysis plus policy. (2023). Available at: https://www.canada.ca/en/health-canada/corporate/transparency/corporate-management-reporting/heath-portfolio-sex-gender-based-analysis-policy.html
11. Weeks, WB, Taliesin, B, and Lavista, JM. Using artificial intelligence to advance public health. Int J Public Health. (2023) 68:1606716. doi: 10.3389/ijph.2023.1606716
12. Thomasian, NM, Eickhoff, C, and Adashi, EY. Advancing health equity with artificial intelligence. J Public Health Policy. (2021) 42:602–11. doi: 10.1057/s41271-021-00319-5
13. Smela, B, Toumi, M, Świerk, K, Francois, C, Biernikiewicz, M, Clay, E, et al. Rapid literature review: definition and methodology. J Mark Access Health Policy. (2023) 11:2241234. doi: 10.1080/20016689.2023.2241234
14. Arksey, H, and O’Malley, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
15. Peters, MDJ, Marnie, C, Tricco, AC, Pollock, D, Munn, Z, Alexander, L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. (2020) 18:2119–26. doi: 10.11124/JBIES-20-00167
16. Veritas Health Innovation. Covidence systematic review software. Melbourne, Australia, Veritas Health Innovation. Available at: www.covidence.org.
17. Health Canada. Government of Canada. (2017). Health portfolio sex and gender-based analysis policy. Available at: https://www.canada.ca/en/health-canada/corporate/transparency/heath-portfolio-sex-gender-based-analysis-policy.html
18. Crenshaw, K. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. U Chi Leg F. (1989) 1:1989:139.
19. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DGPRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
20. Jason, Edward L. Indigenous protocol and artificial intelligence position paper. Concordia University Library; (2020) Available at: https://spectrum.library.concordia.ca/id/eprint/986506
21. New Frontiers in Research Fund. Government of Canada. (2023). Indigenous-led AI: How indigenous knowledge systems could push AI to be more inclusive. Available at: https://www.sshrc-crsh.gc.ca/funding-financement/nfrf-fnfr/stories-histoires/2023/inclusive_artificial_intelligence-intelligence_artificielle_inclusive-eng.aspx
22. Treasury Board Secretariat. Government of Canada. (2024) Guide on the use of generative artificial intelligence. Available at: https://www.canada.ca/en/government/system/digital-government/digital-government-innovations/responsible-use-ai/guide-use-generative-ai.html
23. Feizollah, A, Anuar, NB, Mehdi, R, Firdaus, A, and Sulaiman, A. Understanding COVID-19 halal vaccination discourse on Facebook and twitter using aspect-based sentiment analysis and text emotion analysis. Int J Environ Res Public Health. 19:21. doi: 10.3390/ijerph19106269
24. Canadian Institute for Advanced Research. AICan 2020 CIFAR Pan-Canadian AI strategy impact report. (2020). Available at: https://cifar.ca/wp-content/uploads/2020/11/AICan-2020-CIFAR-Pan-Canadian-AI-Strategy-Impact-Report.pdf
25. Canadian Institute for Advanced Research. Application of artificial intelligence approaches to tackle public health challenges. (2018). Available at: https://cihr-irsc.gc.ca/e/documents/artificial_intelligence_approaches-en.pdf
26. Bavli, I, and Galea, S. Key considerations in the adoption of artificial intelligence in public health. PLOS Digit Health. (2024) 3:e0000540. doi: 10.1371/journal.pdig.0000540
27. Bourgeois-Doyle, D, and Two-Eyed, AI: A reflection on artificial intelligence. Canadian Commission for UNESCO’s IdeaLab. (2019).
28. Dubay, L. Creating an equitable AI policy for indigenous communities. First Policy Response (2021). Available at: https://policyresponse.ca/creating-an-equitable-ai-policy-for-indigenous-communities/
29. World Health Organization. Ethics and governance of artificial intelligence for health. (2021). Available at: https://iris.who.int/bitstream/handle/10665/341996/9789240029200-eng.pdf?sequence=1
30. Canadian institutes of health research. AI for Public Health Equity. (2019). Available at: https://cihr-irsc.gc.ca/e/documents/ai_public_health_equity-en.pdf
31. Mhasawade, V, Zhao, Y, and Chunara, R. Machine learning and algorithmic fairness in public and population health. Nat Mach Intell. (2021) 3:659–66. doi: 10.1038/s42256-021-00373-4
32. Vishwanatha, JK, Christian, A, Sambamoorthi, U, Thompson, EL, Stinson, K, and Syed, TA. Community perspectives on AI/ML and health equity: AIM-AHEAD nationwide stakeholder listening sessions. PLOS Digit Health. (2023) 2:e0000288. doi: 10.1371/journal.pdig.0000288
33. Bouchouar, E, Hetman, BM, and Hanley, B. Development and validation of an automated emergency department-based syndromic surveillance system to enhance public health surveillance in Yukon: a lower-resourced and remote setting. BMC Public Health. 21:1247. doi: 10.1186/s12889-021-11132-w
34. Dankwa-Mullan, I, Scheufele, EL, Matheny, ME, Quintana, Y, Chapman, WW, Jackson, G, et al. A proposed framework on integrating health equity and racial justice into the artificial intelligence development lifecycle. J Health Care Poor Underserved. (2021) 32:300–17. doi: 10.1353/hpu.2021.0065
35. Kung, J. (2019). Ethical AI: A discussion. Available at: https://cifar.ca/cifarnews/2019/07/29/ethical-ai-a-discussion/
36. Kung, J. (2021). A focus on ethics in AI research. Available at: http://cifar.ca/cifarnews/2021/02/12/a-focus-on-ethics-in-ai-research/
37. Morgenstern, JD, Rosella, LC, Costa, AP, and Anderson, LN. Development of machine learning prediction models to explore nutrients predictive of cardiovascular disease using Canadian linked population-based data. Appl Physiol Nutr Metab Physiol Appl Nutr Metab. (2022) 47:529–46. doi: 10.1139/apnm-2021-0502
38. Yip, C, Rosella, LC, Nayani, S, Sanmartin, C, Hennessy, D, Faye, L, et al. Laying the groundwork for Artifical intelligence to advance public health in Canada; (2024). Available at: https://ai4ph-hrtp.ca/wp-content/uploads/2024/06/AI-to-advance-public-health-in-Canada-2024-FINAL.pdf
39. Berridge, C, and Grigorovich, A. Algorithmic harms and digital ageism in the use of surveillance technologies in nursing homes. Front Sociol. (2022) 7:957246. doi: 10.3389/fsoc.2022.957246
40. Baclic, O, Tunis, M, Young, K, Doan, C, Swerdfeger, H, and Schonfeld, J. Challenges and opportunities for public health made possible by advances in natural language processing. Can Commun Dis Rep. (2020) 46:161–8. doi: 10.14745/ccdr.v46i06a02
41. Kamyabi, A, Iyamu, I, Saini, M, May, C, McKee, G, and Choi, A. Advocating for population health: the role of public health practitioners in the age of artificial intelligence. Can J Public Health Rev Can Sante Publique. (2024) 115:473–6. doi: 10.17269/s41997-024-00881-x
42. Fisher, S, and Rosella, LC. Priorities for successful use of artificial intelligence by public health organizations: a literature review. BMC Public Health. (2022) 22:2146. doi: 10.1186/s12889-022-14422-z
43. Chin, H, Lima, G, Shin, M, Zhunis, A, Cha, C, Choi, J, et al. User-Chatbot conversations during the COVID-19 pandemic: study based on topic modeling and sentiment analysis. J Med Internet Res. 25:e40922. doi: 10.2196/40922
44. Couture, V, Roy, MC, Dez, E, Laperle, S, and Bélisle-Pipon, JC. Ethical implications of artificial intelligence in population health and the Public’s role in its governance: perspectives from a citizen and expert panel. J Med Internet Res. (2023) 25:e44357. doi: 10.2196/44357
45. Koohsari, MJ, McCormack, GR, Nakaya, T, Yasunaga, A, Fuller, D, Nagai, Y, et al. The Metaverse, the built environment, and public health: opportunities and uncertainties. J Med Internet Res. (2023) 25:e43549. doi: 10.2196/43549
46. Gómez-Ramírez, O, Iyamu, I, Ablona, A, Watt, S, Xu, AXT, Chang, HJ, et al. On the imperative of thinking through the ethical, health equity, and social justice possibilities and limits of digital technologies in public health. Can J Public Health. (2021) 112:412–6. doi: 10.17269/s41997-021-00487-7
47. Kaushal, A, Mandal, A, Khanna, D, and Acharjee, A. Analysis of the opinions of individuals on the COVID-19 vaccination on social media. Digit Health. (2023) 9:20552076231186246. doi: 10.1177/20552076231186246
48. Zhou, F, Robar, J, Stewart, M, and Jones, J. Implementation of National Guidelines on the Management of Vaccine Preventable Illness in patients with inflammatory bowel disease: perceived barriers and intervention functions amongst gastroenterologists. J Can Assoc Gastroenterol. (2023) 6:49. doi: 10.1093/jcag/gwac036.090
49. Jang, H, Rempel, E, Roth, D, Carenini, G, and Janjua, NZ. Tracking COVID-19 discourse on twitter in North America: Infodemiology study using topic modeling and aspect-based sentiment analysis. J Med Internet Res. 23:e25431. doi: 10.2196/25431
50. L’Allié, WT, and Gardhouse, K. Governing AI: a plan for Canada five high-impact actions needed in white paper by 2024/2025; (2024). Available at: https://aigs.ca/white-paper.pdf
51. Warin, T. Global research on coronaviruses: metadata-based analysis for public health policies. JMIR Med Inform. (2021) 9:e31510. doi: 10.2196/31510
52. Cote, JN, Germain, M, Levac, E, and Lavigne, E. Vulnerability assessment of heat waves within a risk framework using artificial intelligence. Sci Total Environ. (2024) 912:169355. doi: 10.1016/j.scitotenv.2023.169355
53. Rilkoff, H, Struck, S, Ziegler, C, Faye, L, Paquette, D, and Buckeridge, D. Innovations in public health surveillance: an overview of novel use of data and analytic methods. Can Commun Dis Rep. (2024) 50:93–101. doi: 10.14745/ccdr.v50i34a02
54. Smith, MJ, Axler, R, Bean, S, Rudzicz, F, and Shaw, J. Four equity considerations for the use of artificial intelligence in public health. Bull World Health Organ. (2020) 98:290–2. doi: 10.2471/BLT.19.237503
55. Stobbe, R, and Law, Field. (2023). Addressing the legal issues arising from the use of AI in Canada. Available at: https://www.fieldlaw.com/News-Views-Events/219302/Addressing-the-Legal-Issues-Arising-from-the-Use-of-AI-in-Canada
56. Canadian Institutes of Health Research, Canadian institute for advanced research. CPHA collaborator panel session: Exploring the ethics of AI approaches in public health. (2018). Available at: https://cihr-irsc.gc.ca/e/51249.html
57. Priest, E, Fyshe, A, and Lizotte, D. (2019). Artificial Intelligence’s societal impacts, governance, and ethics: Introduction to the 2019 Summer Institute on AI and society and its rapid outputs. Available at: https://escholarship.org/uc/item/2gp9314r
58. Berdahl, CT, Baker, L, Mann, S, Osoba, O, and Girosi, F. Strategies to improve the impact of artificial intelligence on health equity: scoping review. JMIR AI. (2023) 2:e42936. doi: 10.2196/42936
59. Borgesius, FZ. Discrimination, artificial intelligence, and algorithmic decision-making [internet]. Directorate General of Democracy, Council of Europe; (2018). Available at: https://rm.coe.int/discrimination-artificial-intelligence-and-algorithmic-decision-making/1680925d73
60. Fonseka, TM, Bhat, V, and Kennedy, SH. The utility of artificial intelligence in suicide risk prediction and the management of suicidal behaviors. Aust N Z J Psychiatry. (2019) 53:954–64. doi: 10.1177/0004867419864428
61. Gilbert, JP, Ng, V, Niu, J, and Rees, EE. A call for an ethical framework when using social media data for artificial intelligence applications in public health research. Can Commun Dis Rep. (2020) 46:169–73. doi: 10.14745/ccdr.v46i06a03
62. Rolnick, D. (2024). AI research driven by real-world problems. Available at: https://mila.quebec/en/insight/ai-research-driven-by-real-world-problems
63. Biswas, SS. Role of chat GPT in public health. Ann Biomed Eng. (2023) 51:868–9. doi: 10.1007/s10439-023-03172-7
64. Kleiner, K. (2024). The age of deception. Available at: https://magazine.utoronto.ca/research-ideas/culture-society/age-of-deception-artificial-intelligence/
65. Statistics Canada. (2023) Artificial intelligence at statistics Canada. Available at: https://www.statcan.gc.ca/en/trust/collecting-your-data/artificial-intelligence
66. Brooks, J. (2024). How can we make AI that works for everyone? Available at: https://cifar.ca/cifarnews/2024/05/14/how-can-we-make-ai-that-works-for-everyone/
67. Mila. (2024). 14 takeaways from Mila’s first international conference on human rights and AI. Available at: https://mila.quebec/en/news/14-takeaways-from-milas-first-international-conference-on-human-rights-and-ai
Keywords: artificial intelligence, health equity, public health, AI biases, AI ethics
Citation: Ghanem S, Moraleja M, Gravesande D and Rooney J (2025) Integrating health equity in artificial intelligence for public health in Canada: a rapid narrative review. Front. Public Health. 13:1524616. doi: 10.3389/fpubh.2025.1524616
Received: 07 November 2024; Accepted: 29 January 2025;
Published: 18 March 2025.
Edited by:
Steven Fernandes, Creighton University, United StatesReviewed by:
Hong Xiao, Fred Hutchinson Cancer Center, United StatesCopyright © 2025 His Majesty the King in Right of Canada. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samantha Ghanem, c2FtYW50aGEuZ2hhbmVtQHBoYWMtYXNwYy5nYy5jYQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.