
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health, 01 April 2025
Sec. Aging and Public Health
Volume 13 - 2025 | https://doi.org/10.3389/fpubh.2025.1515042
This article is part of the Research TopicReviews and Applications of Implementation Research in Aging and Public HealthView all 13 articles
 Paul A. Estabrooks1*
Paul A. Estabrooks1* Mickey L. Bolyard1
Mickey L. Bolyard1 Tallie Casucci2
Tallie Casucci2 Josh T. Christensen3
Josh T. Christensen3 Bryan Gibson4
Bryan Gibson4 Caitlin A. Golden5
Caitlin A. Golden5 Jennie L. Hill5
Jennie L. Hill5 Linnea Horvath1
Linnea Horvath1 Shinduk Lee6
Shinduk Lee6 Ellen M. Maxfield7
Ellen M. Maxfield7 Mary M. McFarland8
Mary M. McFarland8 James L. Merle5
James L. Merle5 Tzeyu L. Michaud9
Tzeyu L. Michaud9 Megan Miller1
Megan Miller1 Emiliane L. Pereira9
Emiliane L. Pereira9 Chelsey R. Schlechter10
Chelsey R. Schlechter10 Sara E. Simonsen6
Sara E. Simonsen6 David W. Wetter10
David W. Wetter10 Amy B. Locke1,7
Amy B. Locke1,7Introduction: Improving the reach of existing lifestyle interventions focused on health promotion, disease prevention, and self-management delivered in community or clinical settings has the potential to increase the public health impact of these interventions. However, little is known about the overall success of recruitment strategies or the specification of strategy components including the details of how, through which channel, and by whom the recruitment strategies are enacted.
Methods: We conducted a scoping review with guidance from the JBI Manual for Evidence Synthesis. For transparency and reproducibility, we adhered to the PRISMA-S and PRISMA-ScR guidelines for reporting literature searches and scoping reviews. Our eligibility criteria included studies that reported recruitment strategies to improve reach (enrollment number, participation rate, and representativeness of participants) of health promotion, disease prevention, and self-management lifestyle interventions for children or adults worldwide. Recruitment strategies for non-lifestyle interventions, such as pharmaceutical trials, were excluded. Databases included Medline (Ovid), Embase (embase.com), CINAHL Complete (Ebscohost), APA PsycINFO (Ebscohost), and Dissertation and Theses Global (ProQuest). Database search results were retrieved on March 2–3, 2023.
Results: From a total of 9,712 references, 98 studies were included. Eight studies compared recruitment strategies using a randomized controlled trial and 90 studies were evaluations/quasi-experiments that reported on reach. There was a wide variety of recruitment strategies used, with 32% of the studies utilizing more than one recruitment strategy. The average reach, operationalized as participation rate, of the primary strategy (n = 15 defined strategies) being tested ranged from 3 to 41%. Further, participation rates ranged across studies that focused on children (43%), adults (25%), and older adults (16%). Most included studies did not report (1) strategy timing and dose, (2) theoretical basis, or (3) potential mechanisms of improved reach. Finally, differences in how the denominator was operationalized reduced confidence in comparing across strategies.
Discussion: More clarity is needed when reporting on specific recruitment strategies used to improve the reach of lifestyle interventions. Suggestions include guidance on how to consistently define a denominator of eligible participants exposed to recruitment strategies. Furthermore, the use of theoretical approaches and testing of potential mechanisms of effect are needed in future studies to advance the science of improving lifestyle intervention reach.
Systematic review registration: The unique identifier for our scoping review is 3g68b it can be found at this url: https://doi.org/10.17605/OSF.IO/3G68B.
There is a long history of developing and testing health promotion, disease prevention, and disease self-management (secondary prevention) interventions with the intent to have a public health impact (1, 2). As a result there are a myriad of efficacious interventions across these areas that have been compiled into registries to support broad dissemination and implementation (3). However, to achieve a public health impact, there is a need for these interventions to have broad reach and be effective. Reach is an individual-level dissemination outcome and can be defined as the number of participants that enroll, the proportion of eligible people exposed to recruitment activities that enroll, and the representativeness of those enrolled in a given health promotion intervention relative to the intended audience based on demographic characteristics (4). Further underscoring the need to address representativeness, public health goals also focus on increasing the reach of evidence-based interventions in populations that experience health disparities (5).
Within the field of dissemination and implementation science—where understanding the reach, adoption, implementation, and sustainment of evidence-based interventions is foundational—strategies that focus on improving the reach of evidence-based programs for all populations have increased in importance (5, 6). Unfortunately, over the previous 20 years, the degree to which intervention trials have reported on recruitment strategies, or compared strategies, to improve intervention reach have been sparse and what research does exist in this area has been limited (7, 8). In some cases, research has focused on potential participant enablers and barriers to participation (9). Other studies have examined recruitment only from the perspective of providers or physician referrals (10). Still others have examined recruitment relative to a single intervention structure (e.g., group-based) (11) or health behavior outcome (e.g., physical activity) (12).
When considering the reach of health behavior interventions, there are several factors that are hypothesized to determine success (13). These factors include the characteristics of the (1) intended audience, (2) delivery setting and staff, (3) intervention, (4) external factors, and the (5) strategies used to recruit participants (14, 15). Addressing each of these factors within a single study is impractical and the ability to examine potential interactions is likely only possible through a review of literature that has examined reach across a number of populations, delivery settings, intervention structures and foci, and recruitment strategies.
In addition, understanding the underlying mechanisms by which strategies to improve reach achieve a high and representative number and proportion of participants from the intended audience will advance scientific understanding and provide practical principles that can be used to develop additional successful strategies (16). The Practical, Robust, Implementation, and Sustainability Model and Reach, Effectiveness, Adoption, Implementation, and Maintenance Framework (PRISM/RE-AIM) both provide useful guidance on identifying potential mechanisms and ways to operationalize intervention reach. Specifically, the RE-AIM Framework is one of the few dissemination and implementation science frameworks that provides direction on how best to operationalize reach with an emphasis on the number, proportion, and representativeness of participants who are exposed to a recruitment strategy, engage in the recruitment process, and are enrolled in an evidence-based intervention (4). PRISM provides a set of explanatory constructs that can act as contextual moderators or mechanistic mediators in the success of recruitment strategies intended to improve reach which include (1) the multi-level/multi-sector perceptions of a given intervention, (2) multi-leveled staff and setting characteristics, (3) the implementation and sustainability infrastructure of intervention delivery sites, and (4) external environmental factors (15). These constructs provide an opportunity to generate hypotheses to improve dissemination and implementation outcomes that can be used to characterize potential mechanisms (17). Of specific relevance to understanding the utility of strategies to improve reach, PRISM/RE-AIM includes hypotheses related to participant, delivery staff, organizational perceptions and characteristics, the implementation and sustainability infrastructure, characteristics of the intervention, and external factors that may mediate or moderate success (15). The primary objective of this review is to identify recruitment strategies to improve the reach (defined as number, proportion, and representativeness of eligible people) of lifestyle interventions focused on health promotion, disease prevention, and self-management for children and adults delivered in community or clinical settings.
We conducted a scoping review following the JBI Manual for Evidence Synthesis guidance (18). Using the framework as outlined by Arksey and O’Malley, we organized our scoping review into five stages: (1) identifying the research question; (2) identifying relevant studies; (3) selecting the studies; (4) charting the data; and (5) collating, summarizing and reporting the results (19). As the JBI Manual for Evidence Synthesis states, “scoping reviews can be used to map the key concepts that underpin a field of research… the three most common reasons for conducting a scoping review [are] to explore the breadth or extent of the literature, map and summarize the evidence, and inform future research.” (20) For transparency and reproducibility, we adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) (21) and searches (PRISMA-S) (22) for reporting our literature search and review results. The protocol was registered on the Open Science Framework (osf.io) and is available at https://doi.org/10.17605/OSF.IO/3G68B. See Appendix E for differences between the protocol and manuscript.
We used JBI’s mnemonic Population-Concept-Context (PCC) framework to frame our research question and the eligibility criteria (18). Our main research question is “What is known about the use of different types of recruitment strategies to improve the reach of evidence-based lifestyle interventions and how they are reported?” We broadly defined lifestyle interventions to include those aimed at health promotion, disease prevention, and self-management. Further, we were interested in categorizing and comparing strategies based on recruitment success operationalized as participation rate and representativeness. Our secondary purpose was to understand the underlying mechanisms by which strategies improve reach. Here, we addressed two additional questions: (1) to what degree does the (a) intended audience, (b) delivery setting and staff, (c) intervention characteristics, and (d) external factors influence the success of different recruitment strategies? And (2) what are the underlying mechanisms by which successful strategies achieve high reach?
An information specialist (MMM) developed the search strategies using a combination of keywords and database subject headings for the primary databases (Medline) from sentinel studies (i.e., studies identified at protocol stage that examined the utility of recruitment strategies) and team feedback; a librarian (TC) then translated the strategy to the other selected databases. Library colleagues (AM) peer reviewed the strategy according to Peer Review of Electronic Search Strategies (PRESS) guidelines, a structured process to “identify search errors and improve the selection” of controlled vocabulary headings and keyword terms to “enhance the quality and comprehensiveness of the search” which populates the evidence base for the review (23). Databases included Medline (Ovid), Embase (embase.com), CINAHL Complete (Ebscohost), APA PsycINFO (Ebscohost), and Dissertation and Theses Global (ProQuest). The database results were retrieved on March 2–3, 2023. No date limits or other filters, such as language or publication type, were applied. Citation management and duplication detection and removal were accomplished with EndNote, version 21 (Clarivate). No grey literature (i.e., non-commercial publications from government, business, professional organization, or conferences) was searched (24). For studies meeting the inclusion criteria, references were also evaluated for relevancy and potential inclusion. Detailed search strategies are included in Appendix A. The PRISMA-ScR and PRISMA-S Checklists are in Appendix B.
Our inclusion criteria (PCC) (18) defined participants as children or adults of any age, gender, race, or ethnicity. We further defined inclusion based on our overall concept as studies with (a) at least one recruitment strategy for a lifestyle intervention, (b) information on the recruitment strategy protocol, (c) data on number of people recruited and number of people exposed to recruitment efforts, and (d) a focus on lifestyle intervention targeting physical activity, dietary intake, weight loss, weight loss maintenance, obesity prevention, diabetes prevention, or diabetes self-management. Finally, from the perspective of context we included studies in community or clinical settings from around the world that used experimental or quasi-experimental (including single group observational) designs.
Exclusion criteria around concept included studies in which the (a) recruitment strategy is not specified, (b) no reach outcomes are reported, or (c) recruitment is for non-lifestyle interventions, such as pharmaceutical trials; and study design exclusion criteria involved cross-sectional evaluation of a single recruitment strategy. Non-English studies would be excluded at full-text review.
We used Covidence (Veritas Health Innovation), an online systematic reviewing platform to screen and select studies. Two reviewers from a pool of six (EM; EP; JH; LH; MM; PE) independently screened titles and abstracts, then two reviewers from a pool of eight (BG; EP; JC; LH; MM; PE; SS; TM) independently reviewed the full text for inclusion based on our eligibility criteria. When no consensus could be reached between the two reviewers, a third reviewer (BG; EP; JC; LH; MM; PE; SS; TM) was the deciding vote. No artificial intelligence (AI) tools were used in the conduct of the review, although the team did screen all studies using the ‘most relevant’ sort option in Covidence, which uses machine learning (active learning) to show studies by predicted relevance.
Prior to finalization of the protocol, two reviewers (MM; PE) piloted our data charting form using sentinel articles. Data was charted from our included studies by two reviewers (EP; JC; LH; MB; MM) using Microsoft Excel. A third reviewer (EP; JC; LH; MB; MM) who was not involved in the data charting merged the data from the initial two reviewers. Data elements included year of publication, methods, recruitment strategy, lifestyle intervention type, comparison conditions (if relevant), and PRISM/RE-AIM factors related to recruitment strategy implementation and outcomes.
In compliance with scoping review methodology, no quality assessment of included studies was conducted, as our goal was to rapidly map the literature.
We identified 9,712 references from our database search strategies. After removal of duplicates, 5,347 references were screened at title/abstract, then 208 references were assessed for eligibility through full-text review, and 98 studies from 100 references met our inclusion criteria (25–122). See Figure 1 for our PRISMA flowchart. No relevant studies were identified from checking the references of our included studies. Appendix C is a bibliography of our included studies. Appendix D is a bibliography of our excluded studies with reasons from the full-text screening.
Table 1 provides the recruitment strategies, participation rate, number of participants, and the focus on the intervention to which participants are being recruited. Table 2 defines the 15 unique reach strategies we identified from the data with an example for each that was derived from the reviewed studies. Of note, there was not consistent labeling of recruitment strategy type across studies and the 15 strategies identified in Table 2 were derived to assist in categorization and review of strategy success. It is noteworthy that we identified strategies that included single approaches (e.g., mass media), blended approaches (e.g., population health management), and combinations of approaches (e.g., community led recruitment). Table 3 presents the study and participant characteristics of the included studies. The geographical locations of the eligible studies were primarily in the United States (n = 58) or Europe (n = 32). The vast majority of the studies reported observational data relative to the recruitment strategies being described (n = 90) with only eight (26, 54, 60, 70, 86, 87, 103, 119) testing across recruitment strategies using a randomized controlled trial. Nearly half of the included articles provided additional references that further characterized the recruitment strategies (n = 46), and the evaluation of the recruitment strategy was most often embedded in implementation, effectiveness, or evaluation studies of lifestyle interventions. Most studies also analyzed data at the individual level (n = 85), with quantitative methods employed for the majority of the data analysis (n = 84). Table 3 also highlights the degree to which the included studies reported on participant characteristics. Nearly all included studies defined the population intended to benefit from the study (n = 95), including the age range (n = 78). However, specific information related to the gender [n = 17 (25, 26, 31, 32, 35, 42, 43, 65, 66, 71, 76, 85, 90, 105, 106, 110, 120)], race, and ethnicity [n = 14 (25, 26, 33, 45, 46, 71, 80, 92, 93, 98, 106, 112, 120, 122)] of the intended population was reported much less frequently. Finally, study goals for representation across sub-groups in the population was only reported in about one third of studies [n = 29 (25, 26, 29–31, 33, 34, 44, 45, 50, 51, 54, 64, 67, 69–72, 78, 79, 88, 91, 94–96, 102, 111, 119, 120)].

Table 1. Overview of recruitment strategies, participation rate, number of participants and lifestyle intervention type of the included studies in alphabetical by author.
Table 4 presents concept characteristics of the reach strategy and lifestyle intervention of our included studies. The studies describe the reach strategy and lifestyle interventions but were inconsistent in reporting all factors. About half of the studies (n = 49) reported if the goal of the recruitment strategy was to improve either or all reach outcomes, such as the number of participants enrolled, the participation rate, or representativeness of populations experiencing disparities. Areas of relatively high reporting of the reach strategy components included the setting (n = 93), the channel of delivery (n = 93), and the staff involved in implementing the strategy (n = 73). Specifically, of the studies reporting lifestyle intervention delivery setting, community (20%), healthcare (15%), and home-based (14%) were the most frequently described. Remote or online interventions were also reported for 16% of the studies. Areas with low reporting included the cost of strategy [n = 13 (25, 33, 41, 46, 48, 53, 80, 93, 94, 100, 103, 115, 119)], a guiding theory for the strategy [n = 7 (41, 44, 48, 62, 68, 72, 105)], and the intended mechanism of action [n = 5 (25, 37, 50, 53, 85)]. When considering lifestyle intervention contextual factors, the included studies reported the intervention setting (n = 76), delivery channel (n = 68), and format (n = 62). Information on intervention implementation staff and number (n = 52), participant contact (n = 50), timing (n = 48), and duration of sessions (n = 29) were less reported.
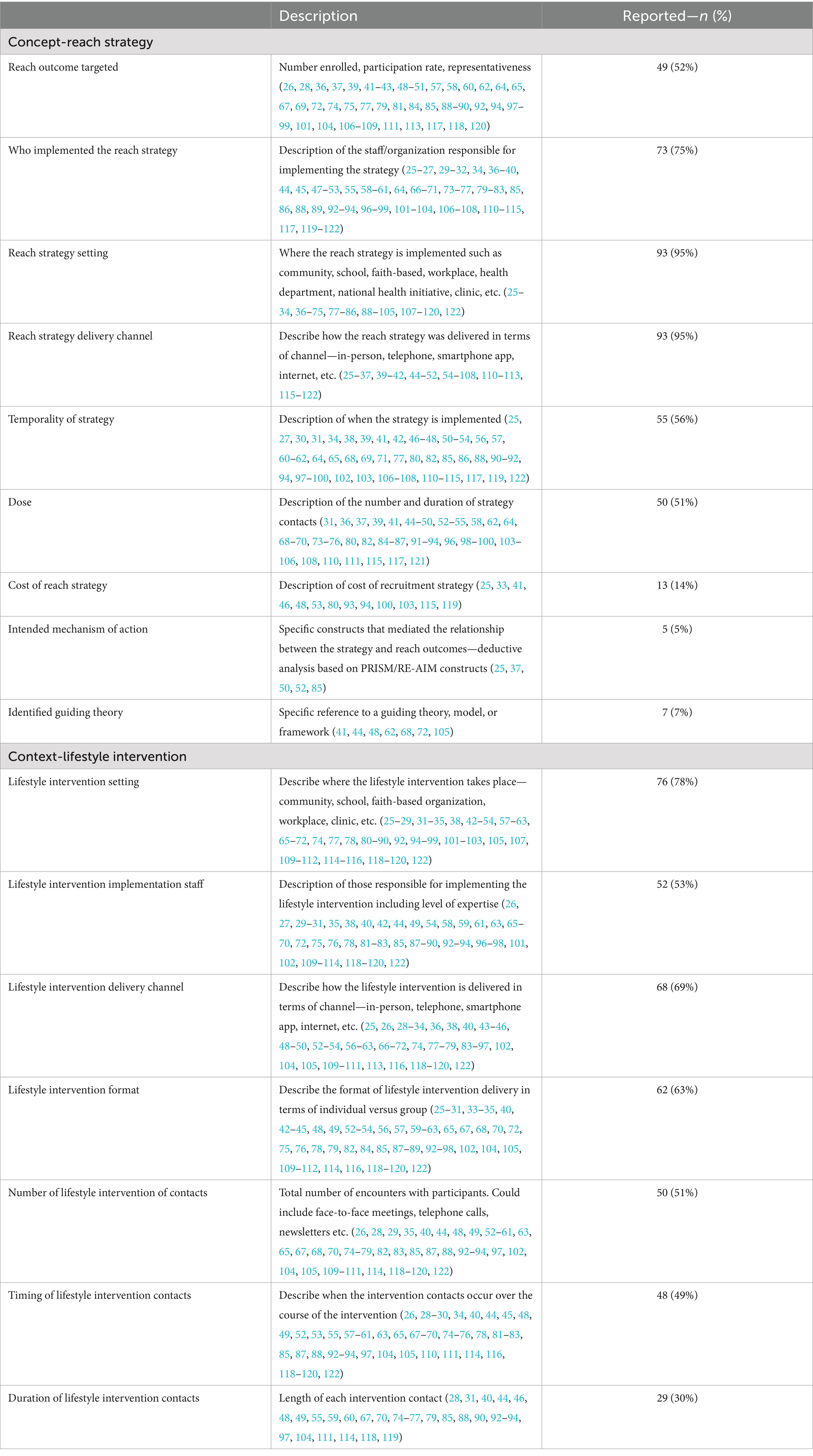
Table 4. Reporting of concept characteristics of the reach strategies and the lifestyle interventions.
Across the included studies, the average number of recruitment strategies applied was 2.5 (± 2.1; see Table 1). Nearly half (40/98) of the studies included bundled strategies and did not differentiate reach based by single strategies. These bundled strategies averaged a participation rate of 16% of the intended population. Strategies consisting of population health management [n = 21 (28, 41, 43, 46, 51–53, 57, 64, 74, 79, 83, 87, 94, 98, 106, 108, 111, 117, 119, 121)], point of care referrals [n = 13 (36–38, 44, 61, 67, 73, 75, 82, 87, 91, 107, 114)], place-based strategies [n = 9 (40, 55, 59, 62, 66, 69, 76, 89, 116)], and direct mail [n = 8 (35, 42, 54, 63, 86, 95, 102, 103)] reported, respectively, median participation rates of 12, 21, 43, and 13%. Eight studies that focused on Black/African American participants reported a 17% participation rate (25, 33, 80, 93, 98, 106, 120, 122) relative to a 21% participation rate when racial groups were not differentiated. Similarly, only 17 studies differentiated on gender, with three studies focusing on men reporting an 8% participation rate (32, 42, 106) relative to a 22% participation rate for women. Studies did report on ages and the reported participation rates were highest for children (43%) and lowest for older adults (16%). Participation rates based on delivery channel were clustered between 19 and 22% except for word of mouth which reported 9% participation rate across six studies (26, 48, 62, 88, 101, 117). Further, differences in who delivered the recruitment strategy, study design, and intervention type did not appear to result in differences in reported participation rate, ranging from 18 to 25% of the intended population.
Twenty-four included studies described using some portion of the PRISM/RE-AIM framework in the design, implementation, or evaluation of their study (25–27, 33, 36, 38, 40, 44, 51, 54, 59, 60, 65, 72, 78, 85, 88–90, 110, 112, 118, 120, 122). However, only seven studies reported a theoretical framework that guided recruitment strategy development [e.g., Diffusion of Innovation (123), Self-Determination Theory (124), or Social Marketing (125)] (41, 44, 48, 62, 68, 72, 105) and only five highlighted potential mechanisms of improved reach (e.g., confidence or social support) (25, 37, 50, 52, 85). No studies examined differences in participation rates based on the intended audience, delivery setting and staff, intervention characteristics, or external factors—the PRISM/RE-AIM contextual factors were hypothesized to moderate and mediate successful reach.
The objective of this review was to identify recruitment strategies to improve the reach of lifestyle interventions focused on health promotion, disease prevention, and self-management for children and adults delivered in community or clinical settings. We also intended to report on the application of theory or conceptual models to improve the reach of lifestyle interventions across participants of all ages. We found that it appears as though place-based strategies achieve the highest participation rate, followed by point of care referrals, bundled strategies, and population health management. Of note, several strategies have only been used as part of recruitment bundles (e.g., engaging leaders to support recruitment or orientation events), making it difficult to determine the utility of these strategies.
In connection with this research topic area focused on aging, we documented that studies that focused on children recruited an average of 43% of the intended audience compared to 25% in adults and 16% for older adults when examined independently or with the full age range of adulthood. Compared to their younger counterparts, older adults may face unique barriers, such as deteriorating health and increasing social isolation, for participating in health promotion, disease prevention, and disease self-management interventions (126). In addition, older adults constitute a greater proportion of the population size in rural communities than urban communities, and older adults in rural communities can have fewer opportunities for such interventions (i.e., unavailability of the interventions) and greater transportation barriers to the interventions that may also influence reach (127).
However, it is likely premature to suggest that children are more likely to engage with lifestyle interventions; it may be more likely that there is a unique context of reach in these different age groups. For example, children and adolescents tend to be physically bound within school settings and have different types of social relationships that can influence recruitment (e.g., peers, teachers, and parents) compared to adults. Likely even more powerful is that recruitment through schools for school-based interventions has an inherently high reach (62). Similarly, a review of participation rates in workplace health promotion programs found an average participation rate just below 50%, which may be less related to the specific strategies and more related to having a known denominator in a setting where lifestyle interventions may be attractive as an employee benefit (128). Another review of enrollment of adults (18 years and older) with cancer and their caregivers in psychosocial or behavioral interventions trials (RCTs) resulted in an average enrollment rate of 33% (129). Both reviews observed participation rates that are higher than our participation rates ranging from 12 to 25% across strategies tested in more than 10 studies. These findings suggest the importance of considering the intended population and setting when planning reach strategies.
Our findings provide several directions for future research that examines the relative utility of different recruitment strategies to improve reach. First, there is a need to better define specific recruitment strategies and improve the application of theory or conceptual models to the design and application of strategies. Second, in addition to providing a recruitment strategy definition, dissemination science as it relates to reach would be better advanced by specifying strategies based on the strategy enactor, components, potential mechanism of improved reach, timing, dose, and intended reach outcome (6). Third, addressing the challenge of improving the reach of lifestyle interventions requires agreement on appropriate assessment of numerators, denominators, and characteristics of potential participants across temporal aspects of reach from exposure to recruitment activities, engagement in the enrollment process, enrollment itself, attendance at intervention sessions, and completion of the intervention (56). Fourth, despite the limitations of the current literature, participant characteristics such as age appear to be related to intervention reach, with higher rates of reach found for younger participants and lower rates with older adults.
Reach is a primary challenge across the spectrum of evidence-based lifestyle interventions whether during efficacy, effectiveness, or implementation trials (56, 87, 130–132). It is unsurprising that we identified 98 unique studies that evaluated or tested different recruitment strategies. We defined 15 unique strategies that were intended to improve intervention reach based on activities described to improve reach across studies (Table 2). However, we acknowledge that these definitions, while helpful, require additional scientific vetting due to potential overlap or muddling of recruitment setting and recruitment strategy. As the Expert Recommendations for Implementation Change compendium of strategies to improve implementation outcomes filled a gap in the implementation science literature (133), future work in this area should focus on addressing the gap in available and consistent labels and definitions for individual-level dissemination strategies that facilitate recruitment of those who would benefit from lifestyle interventions—and allow comparisons across populations, settings, and interventions.
While the field of dissemination and implementation science has a cornucopia of available theories, models, and frameworks, recent scoping reviews have suggested that there is an overemphasis on implementation and an underemphasis on dissemination (134). This may be surprising given the foundational work of Everett Rogers on the Diffusions of Innovation theory, which provides processes and mechanisms for both setting (i.e., adoption of innovations) and individual (i.e., reach of innovations within a population) level dissemination (135, 136). Still, our review supports the conclusion that there has been a lack of reporting the theory applied to the design, testing, and identification of mechanisms of change of strategies intended to improve reach. Indeed, only seven studies (25, 42, 47, 52, 60, 70, 118) referenced a theoretical approach and only five provided a description of potential mechanisms of change (25, 37, 50, 53, 85).
Understanding the underlying mechanisms or reasons why a specific strategy is successful allows for generalizability to other settings and provides guidance for recruitment strategy design in settings with different levels of resources to support recruitment. For example, population health management approaches may be designed to leverage the patient-provider relationship to improve potential participant normative beliefs of the benefits of enrolling in a lifestyle program (i.e., mechanism), which in turn leads to a higher participation rate. If one were to apply concepts from the Theory of Planned Behavior (137) to this example, qualitative and quantitative approaches could be used to see if leveraging the patient-provider relationship resulted in increased perceptions of subjective norm which lead to improved reach. Other authors have also highlighted the importance of understanding the mechanisms by which recruitment strategies can enhance participant engagement and adherence with, and to, evidence-based intervention components (138). Described as adjunctive interventions, Smith and colleagues suggest that methods targeting potential participants for health-focused interventions recruitment strategies can be designed to enhance motivation, self-efficacy, or capacity to engage with a health intervention (138).
In addition to underreporting of underlying theories and mechanisms to improve reach, we found that studies were highly variable in the degree to which they specified strategies based on the way, by who (including demographics and role), how often, and at what dose strategies were applied to improve reach. Important considerations for both the use and success of strategies to improve reach include the cost [reported by only 13 studies (25, 33, 41, 46, 48, 52, 80, 93, 94, 100, 103, 115, 119)], dose [reported by 50 (31, 36, 37, 39, 41, 44–50, 52–55, 58, 62, 64, 68–70, 73–76, 80, 82, 84–87, 91–94, 96, 98–100, 103–106, 108, 110, 111, 115, 117, 121)], and temporality [reported by 55 (25, 27, 30, 31, 34, 38, 39, 41, 42, 46–48, 50–54, 56, 57, 60–62, 64, 65, 68, 69, 71, 77, 80, 82, 85, 86, 88, 90–92, 94, 97–100, 102, 103, 106–108, 110–115, 117, 119, 122)]. Without this information, replication of strategies, and generalizing strategies into typical community or clinical settings is genuinely compromised.
Proctor and colleagues recommend specification of strategies based on the actor (i.e., who enacts the strategy), the action (i.e., the steps involved in the strategy), the factor or people intended to be influenced by the action (i.e., mechanism of change; priority population to be reached), temporality (i.e., when the strategy is used), dose (i.e., the duration of the strategy), the implementation outcome (i.e., fidelity or sustainment), and the justification (i.e., empirical or theoretical rational for using the strategy) (6). Previous reviews of literature using the RE-AIM framework provide direction on specifying factors related to the intended audience, intervention, and delivery settings (7, 139). For example, to improve reporting on characteristics of the intervention into which potential participants are being recruited, we recommend that the target intervention of the recruitment strategy also be specified in terms of the intervention delivery setting, staff, delivery mode and format, number, frequency and length of sessions. Similarly, we recommend defining the intended audience including subgroups that may experience health differences and the plan to assess reach for priority populations including the number, proportion, and representativeness to that priority population (140). In addition, studies that use community-engaged approaches to identify, engage, and enroll participants in lifestyle interventions typically provide details on the co-creation of the lifestyle intervention but do not describe, in detail, the engagement process in the selection and creation of recruitment strategies (23). We recommend that those using participatory approaches to develop recruitment strategies provide detail on the process of partnership development and involvement in recruitment strategy identification, creation, and deployment in addition to specifying the recruitment strategy factors (34).
It is of note that we used the reported participation rates from each included study. Unfortunately, the degree to which studies defined a denominator of those exposed to recruitment strategies varied widely, which makes conclusions around participation rate comparisons challenging. One of the key areas of inconsistency was around the operationalizing and reporting of a specific denominator based on the temporality of the recruitment process. Harden and colleagues highlighted this issue and proposed that proportional reach (i.e., participation rate) should be considered across four indicators (56). These were the proportion of the population (1) exposed to the recruitment strategy, (2) who respond to the recruitment strategy and express interest, (3) who enroll in the intervention, and (4) who attend intervention sessions over time. We would add to this characterization by adding a final temporal state of the proportion who complete the intervention and recommend that representativeness and tracking of priority population rates be assessed across each of these phases.
While our review excluded studies that focused only on recruitment strategies for clinical trials they may provide context to our recommendations given the potential similarities in recruitment barriers and facilitators. For example, our review included surprisingly few studies that applied financial incentives to support recruitment. In clinical trials, financial incentives to address social needs, transportation, and childcare have demonstrated success in recruiting under-represented populations (141). Similarly, strategies that ensure interventions are culturally relevant or have demographic concordance between the recruiter/implementer and participant have also been proposed to improve trust and recruitment into clinical trials (142). These findings may provide alternative methods to categorize strategies based on the underlying barrier or facilitator they are designed to address (e.g., trust, logistics). Still, differences between recruitment for clinical trials and lifestyle change intervention studies likely exist where, in one case, participants are asked to agree to testing a medication or providing biospecimens and, in the other, are asked to enroll in an intervention that promotes healthy behaviors. This raises questions about the characteristic of the innovation and underlying perceptions of the intended study population toward that innovation. These differences likely necessitate the application of different types, dose, and delivery channel of recruitment strategies—excellent areas of future research on strategies to promote lifestyle intervention reach. Finally, even within the variety of lifestyle change interventions it is likely that there are interactions between recruitment strategy type and the format of the intervention.
While this review sheds lights on an important gap in dissemination and implementation science related to strategies intended to improve lifestyle intervention reach, it is not without limitations. We provided labels, definitions, and categories of recruitment strategies for the studies we reviewed, but we anticipate that these labels and definitions are not exhaustive and present opportunities for further refinement. Additionally, although several databases were searched and references of our included studies were reviewed, published or unpublished studies might have been missed due to the vast number of lifestyle intervention studies conducted. We did not reach out to authors to address unreported data or for clarification. Since only eight studies used randomized controlled trials to test recruitment strategy influence on reach with little content overlap between these studies (26, 54, 60, 70, 86, 87, 103, 119), along with no assessment of quality or risk of bias conducted on included studies, the specific results should be interpreted with caution and used as a starting point rather than as a final destination for understanding participation rate. Although active learning was used in Covidence for screening, all studies were screened, selected and extracted in pairs by humans without artificial intelligence (AI) ensuring transparency and reproducibility.
In conclusion, the strengths of our review included a broad conceptualization of recruitment strategies and outcomes across 98 included studies to provide valuable information on available reach strategies, possible definitions, and a resource for others looking for research on improving reach. We analyzed studies to identify effective recruitment strategies for lifestyle interventions aimed at health promotion, disease prevention, and self-management. We found a variety of recruitment strategies, with 32% of studies using multiple strategies. Participation rates ranged from 3 to 41%, with higher rates observed in children (43%) compared to adults (25%) and older adults (16%). Most studies lacked detailed reporting on strategy timing, dose, theoretical basis, and mechanisms of improved reach, making comparisons difficult. The review highlights the need for consistent definitions of eligible participant denominators and the inclusion of theoretical approaches and mechanisms in future studies to enhance the understanding and effectiveness of recruitment strategies. Future research should focus on clearer reporting of recruitment strategies, including timing, dose, and theoretical underpinnings. Identifying and testing mechanisms that improve reach is crucial, as is considering the unique contexts of different age groups and settings. This will help develop more effective recruitment strategies that will improve enrollment for lifestyle interventions across all populations.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
PE: Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Funding acquisition, Methodology. MB: Writing – review & editing, Formal analysis, Investigation, Validation. TC: Writing – review & editing, Data curation, Investigation, Methodology. JC: Writing – review & editing, Formal analysis, Investigation, Validation. BG: Writing – review & editing, Conceptualization, Formal analysis, Validation. CG: Writing – review & editing, Formal analysis, Validation. JH: Writing – review & editing, Conceptualization. LH: Writing – review & editing, Formal analysis, Investigation, Validation. SL: Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis. EM: Writing – review & editing, Conceptualization, Investigation. MMM: Writing – review & editing, Data curation, Investigation, Methodology. JM: Writing – review & editing, Methodology. TM: Writing – review & editing, Conceptualization, Formal analysis, Investigation, Methodology, Validation. MM: Writing – review & editing, Formal analysis, Investigation, Validation. EP: Writing – review & editing, Formal analysis, Investigation, Methodology. CS: Writing – review & editing, Conceptualization. SS: Writing – review & editing, Conceptualization, Formal analysis. DW: Writing – review & editing, Conceptualization. AL: Conceptualization, Funding acquisition, Investigation, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This review was supported by a grant from the Margolis Foundation. This investigation was supported by the University of Utah Translational Research: Implementation, Analysis, and Design (TRIAD), Systematic Review Core (SR Core) with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UM1TR004409 (formerly 5UL1TR001067-05, 8UL1TR000105 and UL1RR025764).
We would like to thank Alfred Mowdood for peer-reviewing the Medline (Ovid) search strategy.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1515042/full#supplementary-material
1. Flay, BR. Efficacy and effectiveness trials (and other phases of research) in the development of health promotion programs. Prev Med. (1986) 15:451–74. doi: 10.1016/0091-7435(86)90024-1
2. Van Rhoon, L, Byrne, M, Morrissey, E, Murphy, J, and McSharry, J. A systematic review of the behaviour change techniques and digital features in technology-driven type 2 diabetes prevention interventions. Digit Health. (2020) 6:2055207620914427. doi: 10.1177/2055207620914427
3. Harden, SM, Steketee, A, Glasgow, T, Glasgow, RE, and Estabrooks, PA. Suggestions for advancing pragmatic solutions for dissemination: potential updates to evidence-based repositories. Am J Health Promot. (2021) 35:289–94. doi: 10.1177/0890117120934619
4. Reilly, KL, Kennedy, S, Porter, G, and Estabrooks, P. Comparing, contrasting, and integrating dissemination and implementation outcomes included in the RE-AIM and implementation outcomes frameworks. Front Public Health. (2020) 8:430. doi: 10.3389/fpubh.2020.00430
5. Shelton, RC, Chambers, DA, and Glasgow, RE. An extension of RE-AIM to enhance sustainability: addressing dynamic context and promoting health equity over time. Front Public Health. (2020) 8:134. doi: 10.3389/fpubh.2020.00134
6. Proctor, EK, Powell, BJ, and McMillen, JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. (2013) 8:139. doi: 10.1186/1748-5908-8-139
7. Glasgow, RE, Harden, SM, Gaglio, B, Rabin, B, Smith, ML, Porter, GC, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front Public Health. (2019) 7:64. doi: 10.3389/fpubh.2019.00064
8. Glasgow, RE, Klesges, LM, Dzewaltowski, DA, Estabrooks, PA, and Vogt, TM. Evaluating the impact of health promotion programs: using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Educ Res. (2006) 21:688–94. doi: 10.1093/her/cyl081
9. Zurynski, Y, Smith, C, Siette, J, Nic Giolla Easpaig, B, Simons, M, and Knaggs, GT. Identifying enablers and barriers to referral, uptake and completion of lifestyle modification programmes: a rapid literature review. BMJ Open. (2021) 11:e045094. doi: 10.1136/bmjopen-2020-045094
10. Tomlinson-Perez, S, Machaczek, KK, Firth, J, Pollard, N, Meda, G, Keddie, E, et al. Evaluation of the uptake, retention and effectiveness of exercise referral schemes for the management of mental health conditions in primary care: a systematic review. BMC Public Health. (2022) 22:249. doi: 10.1186/s12889-022-12638-7
11. Begum, S, Povey, R, Ellis, N, and Gidlow, C. A systematic review of recruitment strategies and behaviour change techniques in group-based diabetes prevention programmes focusing on uptake and retention. Diabetes Res Clin Pract. (2020) 166:108273. doi: 10.1016/j.diabres.2020.108273
12. Blane, DN, Macdonald, S, and O'Donnell, CA. What works and why in the identification and referral of adults with comorbid obesity in primary care: a realist review. Obes Rev. (2020) 21:e12979. doi: 10.1111/obr.12979
13. Mutrie, N, Foster, C, Estabrooks, P, Burton, NW, and Baker, G. Recruiting hard-to-reach populations to physical activity studies: evidence and experiences. J Phys Act Health. (2010) 7:S329–31.
14. Holtrop, JS, Estabrooks, PA, Gaglio, B, Harden, SM, Kessler, RS, King, DK, et al. Understanding and applying the RE-AIM framework: clarifications and resources. J Clin Transl Sci. (2021) 5:e126. doi: 10.1017/cts.2021.789
15. Feldstein, AC, and Glasgow, RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf. (2008) 34:228–43. doi: 10.1016/S1553-7250(08)34030-6
16. Lewis, CC, Boyd, MR, Walsh-Bailey, C, Lyon, AR, Beidas, R, Mittman, B, et al. A systematic review of empirical studies examining mechanisms of implementation in health. Implement Sci. (2020) 15:21. doi: 10.1186/s13012-020-00983-3
17. McCreight, MS, Rabin, BA, Glasgow, RE, Ayele, RA, Leonard, CA, Gilmartin, HM, et al. Using the practical, robust implementation and sustainability model (PRISM) to qualitatively assess multilevel contextual factors to help plan, implement, evaluate, and disseminate health services programs. Transl Behav Med. (2019) 9:1002–11. doi: 10.1093/tbm/ibz085
18. Peters, MDJ, Marnie, C, Tricco, AC, Pollock, D, Munn, Z, Alexander, L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. (2020) 18:2119–26. doi: 10.11124/JBIES-20-00167
19. Arksey, H, and O’Malley, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
20. Peters, MDJ, Godfrey, C, McInerney, P, Munn, Z, Tricco, AC, and Khalil, H. Why a scoping review. In: E Aromataris, C Lockwood, K Porritt, B Pilla, and Z Jordan, editors. JBI manual for evidence synthesis : JBI (2024)
21. Tricco, AC, Lillie, E, Zarin, W, O'Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
22. Rethlefsen, ML, Kirtley, S, Waffenschmidt, S, Ayala, AP, Moher, D, Page, MJ, et al. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst Rev. (2021) 10:39. doi: 10.1186/s13643-020-01542-z
23. McGowan, J, Sampson, M, Salzwedel, DM, Cogo, E, Foerster, V, and Lefebvre, C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. (2016) 75:40–6. doi: 10.1016/j.jclinepi.2016.01.021
24. Aromataris, E, Lockwood, C, Porritt, K, Pilla, B, and Jordan, Z. Grey literature. In JBI manual for evidence synthesis. The publisher is the Joanna Briggs Institute. (2024) doi: 10.46658/JBIMES-24-01
25. Adams, R, Hebert, CJ, Mcvey, L, and Williams, R. Implementation of the YMCA diabetes prevention program throughout an integrated health system: a translational study. Perm J. (2016) 20:15–241. doi: 10.7812/TPP/15-241
26. Alexander, GL, Divine, GW, Couper, MP, McClure, JB, Stopponi, MA, Fortman, KK, et al. Effect of incentives and mailing features on online health program enrollment. Am J Prev Med. (2008) 34:382–8. doi: 10.1016/j.amepre.2008.01.028
27. Bajraktari, S, Zingmark, M, Pettersson, B, Rosendahl, E, Lundin-Olsson, L, and Sandlund, M. Reaching older people with a digital fall prevention intervention in a Swedish municipality context-an observational study. Front Public Health. (2022) 10:857652. doi: 10.3389/fpubh.2022.857652
28. Bayley, A, Stahl, D, Ashworth, M, Cook, DG, Whincup, PH, Treasure, J, et al. Response bias to a randomised controlled trial of a lifestyle intervention in people at high risk of cardiovascular disease: a cross-sectional analysis. BMC Public Health. (2018) 18:1092. doi: 10.1186/s12889-018-5939-y
29. Bean, C, Dineen, T, Locke, SR, Bouvier, B, and Jung, ME. An evaluation of the reach and effectiveness of a diabetes prevention behaviour change program situated in a community site. Can J Diabetes. (2021) 45:360–8. doi: 10.1016/j.jcjd.2020.10.006
30. Befort, CA, Kurz, D, VanWormer, JJ, and Ellerbeck, EF. Recruitment and reach in a pragmatic behavioral weight loss randomized controlled trial: implications for real-world primary care practice. BMC Fam Pract. (2020) 21:47. doi: 10.1186/s12875-020-01117-w
31. Benedetti, TRB, Rech, CR, Konrad, LM, Almeida, FA, Brito, FA, Chodzko-Zajko, W, et al. Re-thinking physical activity programs for older Brazilians and the role of public health centers: a randomized controlled trial using the RE-AIM model. Front Public Health. (2020) 8:48. doi: 10.3389/fpubh.2020.00048
32. Bracken, K, Hague, W, Keech, A, Conway, A, Handelsman, DJ, Grossmann, M, et al. Recruitment of men to a multi-Centre diabetes prevention trial: an evaluation of traditional and online promotional strategies. Trials. (2019) 20:1–14. doi: 10.1186/s13063-019-3485-2
33. Brewer, LC, Jenkins, S, Lackore, K, Johnson, J, Jones, C, Cooper, LA, et al. mHealth intervention promoting cardiovascular health among African-Americans: recruitment and baseline characteristics of a pilot study. JMIR Res Protoc. (2018) 7:e31. doi: 10.2196/resprot.8842
34. Brierley, ML, Smith, LR, Chater, AM, and Bailey, DP. A-REST (activity to reduce excessive sitting time): a feasibility trial to reduce prolonged sitting in police staff. Int J Environ Res Public Health. (2022) 19:27. doi: 10.3390/ijerph19159186
35. Brown, SD, Lee, K, Schoffman, DE, King, AC, Crawley, LVM, and Kiernan, M. Minority recruitment into clinical trials: experimental findings and practical implications. Contemp Clin Trials. (2012) 33:620–3. doi: 10.1016/j.cct.2012.03.003
36. Brunisholz, KD, Kim, J, Savitz, LA, Hashibe, M, Gren, LH, Hamilton, S, et al. A formative evaluation of a diabetes prevention program using the RE-AIM framework in a learning health care system, Utah, 2013-2015. Prev Chronic Dis. (2017) 14:E58. doi: 10.5888/pcd14.160556
37. Carter, A, Humphreys, L, Snowdon, N, Sharrack, B, Daley, A, Petty, J, et al. Participant recruitment into a randomised controlled trial of exercise therapy for people with multiple sclerosis. Trials. (2015) 16:468. doi: 10.1186/s13063-015-0996-3
38. Chinn, DJ, White, M, Howel, D, Harland, JOE, and Drinkwater, CK. Factors associated with non-participation in a physical activity promotion trial. Public Health. (2006) 120:309–19. doi: 10.1016/j.puhe.2005.11.003
39. Chow, EJ, Baldwin, LM, Hagen, AM, Hudson, MM, Gibson, TM, Kochar, K, et al. Communicating health information and improving coordination with primary care (CHIIP): rationale and design of a randomized cardiovascular health promotion trial for adult survivors of childhood cancer. Contemp Clin Trials. (2020) 89:105915. doi: 10.1016/j.cct.2019.105915
40. Clark, AF, Wilk, P, Mitchell, CA, Smith, C, Archer, J, and Gilliland, JA. Examining how neighborhood socioeconomic status, geographic accessibility, and informational accessibility influence the uptake of a free population-level physical activity intervention for children. Am J Health Promot. (2018) 32:315–24. doi: 10.1177/0890117117718433
41. Coughlin, JW, Martin, LM, Zhao, D, Goheer, A, Woolf, TB, Holzhauer, K, et al. Electronic health record-based recruitment and retention and Mobile health app usage: multisite cohort study. J Med Internet Res. (2022) 24:e34191. doi: 10.2196/34191
42. Crane, MM, LaRose, JG, Espeland, MA, Wing, RR, and Tate, DF. Recruitment of young adults for weight gain prevention: randomized comparison of direct mail strategies. Trials. (2016) 17:282. doi: 10.1186/s13063-016-1411-4
43. Daley, A, Winter, H, Grimmett, C, McGuinness, M, McManus, R, and MacArthur, C. Feasibility of an exercise intervention for women with postnatal depression: a pilot randomised controlled trial. Br J Gen Pract. (2008) 58:178–83. doi: 10.3399/bjgp08X277195
44. Dettlaff-Dunowska, M, Brzeziński, M, Zagierska, A, Borkowska, A, Zagierski, M, and Szlagatys-Sidorkiewicz, A. Changes in body composition and physical performance in children with excessive body weight participating in an integrated weight-loss programme. Nutrients. (2022) 14:3647. doi: 10.3390/nu14173647
45. Eakin, EG, Bull, SS, Riley, K, Reeves, MM, Gutierrez, S, and McLaughlin, P. Recruitment and retention of Latinos in a primary care-based physical activity and diet trial: the resources for health study. Health Educ Res. (2007) 22:361–71. doi: 10.1093/her/cyl095
46. Effoe, VS, Katula, JA, Kirk, JK, Pedley, CF, Bollhalter, LY, Brown, WM, et al. The use of electronic medical records for recruitment in clinical trials: findings from the lifestyle intervention for treatment of diabetes trial. Trials. (2016) 17:496. doi: 10.1186/s13063-016-1631-7
47. Estabrooks, PA, Bradshaw, M, Dzewaltowski, DA, and Smith-Ray, RL. Determining the impact of walk Kansas: applying a team-building approach to community physical activity promotion. Ann Behav Med. (2008) 36:1–12. doi: 10.1007/s12160-008-9040-0
48. Felix, HC, Adams, B, Fausett, JK, Krukowski, RA, Prewitt, TE, and West, DS. Calculating reach of evidence-based weight loss and memory improvement interventions among older adults attending Arkansas senior centers, 2008-2011. Prev Chronic Dis. (2012) 9:E63. doi: 10.5888/pcd9.110141
49. Franklin, PD, Ploutz-Snyder, R, Rosenbaum, PF, Carey, MP, Smith, N, and Roizen, MF. Worksite e-mail health promotion trial: early lessons. Eval Program Plann. (2006) 29:405–12. doi: 10.1016/j.evalprogplan.2006.08.010
50. Garip, G, Morton, K, Bridger, R, and Yardley, L. Evaluating the feasibility of a web-based weight loss programme for naval service personnel with excess body weight. Pilot Feasibility Stud. (2017) 3:6. doi: 10.1186/s40814-017-0122-2
51. Ghai, NR, Reynolds, KD, Xiang, AH, Massie, K, Rosetti, S, Blanco, L, et al. Recruitment results among families contacted for an obesity prevention intervention: the obesity prevention tailored for health study. Trials. (2014) 15:463. doi: 10.1186/1745-6215-15-463
52. Glasgow, RE, and Toobert, DJ. Brief, computer-assisted diabetes dietary self-management counseling: effects on behavior, physiologic outcomes, and quality of life. Med Care. (2000) 38:1062–73. doi: 10.1097/00005650-200011000-00002
53. Glasgow, RE, Nelson, CC, Kearney, KA, Reid, R, Ritzwoller, DP, Strecher, VJ, et al. Reach, engagement, and retention in an internet-based weight loss program in a multi-site randomized controlled trial. J Med Internet Res. (2007) 9:e11. doi: 10.2196/jmir.9.2.e11
54. Gopalan, A, Paramanund, J, Shaw, PA, Patel, D, Friedman, J, Brophy, C, et al. Randomised controlled trial of alternative messages to increase enrolment in a healthy food programme among individuals with diabetes. BMJ Open. (2016) 6:e012009. doi: 10.1136/bmjopen-2016-012009
55. Guertler, D, Meyer, C, Dörr, M, Braatz, J, Weymar, F, John, U, et al. Reach of individuals at risk for cardiovascular disease by proactive recruitment strategies in general practices, job centers, and health insurance. Int J Behav Med. (2017) 24:153–60. doi: 10.1007/s12529-016-9584-5
56. Harden, SM, Fanning, JT, Motl, RW, McAuley, E, and Estabrooks, PA. Determining the reach of a home-based physical activity program for older adults within the context of a randomized controlled trial. Health Educ Res. (2014) 29:861–9. doi: 10.1093/her/cyu049
57. Hirsch, SH, Mayer-Oakes, A, Schweitzer, S, Atchison, KA, Lubben, JE, and DeJong, F. Enrolling community physicians and their patients in a study of prevention in the elderly. Public Health Rep. (1992) 107:142–9.
58. Horowitz, CR, Brenner, BL, Lachapelle, S, Amara, DA, and Arniella, G. Effective recruitment of minority populations through community-led strategies. Am J Prev Med. (2009) 37:S195–200. doi: 10.1016/j.amepre.2009.08.006
59. Jago, R, Tibbitts, B, Porter, A, Sanderson, E, Bird, E, Powell, JE, et al. A revised teaching assistant-led extracurricular physical activity programme for 8- to 10-year-olds: the action 3:30R feasibility cluster RCT. Public Health Res. (2019) 7:1–128. doi: 10.3310/phr07190
60. Jalkanen, K, Järvenpää, R, Tilles-Tirkkonen, T, Martikainen, J, Aarnio, E, Männikkö, R, et al. Comparison of communication channels for large-scale type 2 diabetes risk screening and intervention recruitment: empirical study. JMIR Diabetes. (2021) 6:e21356. doi: 10.2196/21356
61. Johnson, EM, Oddone, EZ, Van Treese, K, Gierisch, JM, Dollar, KM, Dundon, M, et al. Implementing evidence-based telephone coaching for health behavior program enrollment: a quality improvement project. Fam Syst Health. (2022) 17:17. doi: 10.1037/fsh0000758
62. Jong, ST, Croxson, CHD, Foubister, C, Brown, HE, Guell, C, Lawlor, ER, et al. Reach, recruitment, dose, and intervention Fidelity of the GoActive school-based physical activity intervention in the UK: a mixed-methods process evaluation. Children. (2020) 7:17. doi: 10.3390/children7110231
63. Kerry, SM, Morgan, KE, Limb, E, Cook, DG, Furness, C, Carey, I, et al. Interpreting population reach of a large, successful physical activity trial delivered through primary care. BMC Public Health. (2018) 18:170. doi: 10.1186/s12889-018-5034-4
64. Kirley, K, Khan, T, Aquino, G, Brown, A, Meier, S, Chambers, N, et al. Using a certified electronic health record technology platform to screen, test and refer patients with prediabetes. JAMIA Open. (2021) 4:ooab101. doi: 10.1093/jamiaopen/ooab101
65. Kozica, SL, Harrison, CL, Teede, HJ, Ng, S, Moran, LJ, and Lombard, CB. Engaging rural women in healthy lifestyle programs: insights from a randomized controlled trial. Trials. (2015) 16:413. doi: 10.1186/s13063-015-0860-5
66. Lawlor, ER, Cupples, ME, Donnelly, M, and Tully, MA. Promoting physical activity among community groups of older women in socio-economically disadvantaged areas: randomised feasibility study. Trials. (2019) 20:234. doi: 10.1186/s13063-019-3312-9
67. Lewis, ZH, Ottenbacher, KJ, Fisher, SR, Jennings, K, Brown, AF, Swartz, MC, et al. The feasibility and RE-AIM evaluation of the TAME health pilot study. Int J Behav Nutr Phys Act. (2017) 14:106. doi: 10.1186/s12966-017-0560-5
68. Linnan, LA, Emmons, KM, Klar, N, Fava, JL, LaForge, RG, and Abrams, DB. Challenges to improving the impact of worksite cancer prevention programs: comparing reach, enrollment, and attrition using active versus passive recruitment strategies. Ann Behav Med. (2002) 24:157–66. doi: 10.1207/S15324796ABM2402_13
69. Linnan, L, Tate, DF, Harrington, CB, Brooks-Russell, A, Finkelstein, E, Bangdiwala, S, et al. Organizational- and employee-level recruitment into a worksite-based weight loss study. Clin Trials. (2012) 9:215–25. doi: 10.1177/1740774511432554
70. Liu, S, Hodgson, C, Zbib, AM, Payne, AYM, and Nolan, RP. The effectiveness of loyalty rewards to promote the use of an internet-based heart health program. J Med Internet Res. (2014) 16:e163. doi: 10.2196/jmir.3458
71. Liu, J, Wilcox, S, Wingard, E, Burgis, J, Schneider, L, and Dahl, A. Strategies and challenges in recruiting pregnant women with elevated body mass index for a behavioral lifestyle intervention. Women's Health Rep. (2020) 1:556–65. doi: 10.1089/whr.2020.0089
72. Long, DA, and Sheehan, P. A case study of population health improvement at a Midwest regional hospital employer. Popul Health Manag. (2010) 13:163–73. doi: 10.1089/pop.2008.0034
73. Madsen, K, Garber, A, Martin, M, Gonzaga, M, and Linchey, J. The feasibility of a physical activity referral network for pediatric obesity. Child Obes. (2014) 10:169–74. doi: 10.1089/chi.2013.0118
74. Markert, J, Alff, F, Zschaler, S, Gausche, R, Kiess, W, and Blüher, S. Prevention of childhood obesity: recruiting strategies via local paediatricians and study protocol for a telephone-based counselling programme. Obes Res Clin Pract. (2013) 7:e476–86. doi: 10.1016/j.orcp.2012.07.008
75. Mas-Alos, S, Planas-Anzano, A, Peirau-Teres, X, Real-Gatius, J, and Galindo-Ortego, G. Feasibility assessment of the let's walk programme (CAMINEM): exercise training and health promotion in primary health-care settings. Int J Environ Res Public Health. (2021) 18:19. doi: 10.3390/ijerph18063192
76. McEachan, RRC, Santorelli, G, Bryant, M, Sahota, P, Farrar, D, Small, N, et al. The HAPPY (healthy and active parenting programmme for early years) feasibility randomised control trial: acceptability and feasibility of an intervention to reduce infant obesity. BMC Public Health. (2016) 16:1–15. doi: 10.1186/s12889-016-2861-z
77. Mills, KM, Stewart, AL, King, AC, Roihz, K, Sepsis, PG, Ritter, PL, et al. Factors associated with enrollment of older adults into a physical activity promotion program. J Aging Health. (1996) 8:96–113. doi: 10.1177/089826439600800105
78. Mullane, SL, Rydell, SA, Larouche, ML, Toledo, MJL, Feltes, LH, Vuong, B, et al. Enrollment strategies, barriers to participation, and reach of a workplace intervention targeting sedentary behavior. Am J Health Promot. (2019) 33:225–36. doi: 10.1177/0890117118784228
79. Oddone, EZ, Gierisch, JM, Sanders, LL, Fagerlin, A, Sparks, J, McCant, F, et al. A coaching by telephone intervention on engaging patients to address modifiable cardiovascular risk factors: a randomized controlled trial. J Gen Intern Med. (2018) 33:1487–94. doi: 10.1007/s11606-018-4398-6
80. Okhomina, VI, Seals, SR, and Marshall, GD Jr. Recruitment and enrollment of African Americans into health promoting programs: the effects of health promoting programs on cardiovascular disease risk study. Ethn Health. (2020) 25:825–34. doi: 10.1080/13557858.2018.1458074
81. Olij, BF, Erasmus, V, Barmentloo, LM, Burdorf, A, Smilde, D, Schoon, Y, et al. Evaluation of implementing a home-based fall prevention program among community-dwelling older adults. Int J Environ Res Public Health. (2019) 16:26. doi: 10.3390/ijerph16061079
82. Parkinson, MD, Hammonds, T, Keyser, DJ, Wheeler, JR, and Peele, PB. Impact of physician referral to health coaching on patient engagement and health risks: an observational study of UPMC's prescription for wellness. Am J Health Promot. (2020) 34:366–75. doi: 10.1177/0890117119900588
83. Parra-Medina, D, D'antonio, A, Smith, SM, Levin, S, Kirkner, G, Mayer-Davis, E, et al. Successful recruitment and retention strategies for a randomized weight management trial for people with diabetes living in rural, medically underserved counties of South Carolina: the POWER study. J Am Diet Assoc. (2004) 104:70–5. doi: 10.1016/j.jada.2003.10.014
84. Partridge, SR, Balestracci, K, Wong, ATY, Hebden, L, McGeechan, K, Denney-Wilson, E, et al. Effective strategies to recruit Young adults into the TXT2BFiT mHealth randomized controlled trial for weight gain prevention. JMIR Res Protoc. (2015) 4:e66. doi: 10.2196/resprot.4268
85. Peck, LE, Sharpe, PA, Burroughs, EL, and Granner, ML. Recruitment strategies and costs for a community-based physical activity program. Health Promot Pract. (2008) 9:191–8. doi: 10.1177/1524839906292819
86. Peels, DA, Bolman, C, Golsteijn, RHJ, de Vries, H, Mudde, AN, van Stralen, MM, et al. Differences in reach and attrition between web-based and print-delivered tailored interventions among adults over 50 years of age: clustered randomized trial. J Med Internet Res. (2012) 14:e179. doi: 10.2196/jmir.2229
87. Porter, G, Michaud, TL, Schwab, RJ, Hill, JL, and Estabrooks, PA. Reach outcomes and costs of different physician referral strategies for a weight management program among rural primary care patients: type 3 hybrid effectiveness-implementation trial. JMIR Form Res. (2021) 5:e28622. doi: 10.2196/28622
88. Ramsay, JE, Hogan, CK, Janevic, MR, Courser, RR, Allgood, KL, and Connell, CM. Comparison of recruitment strategies for engaging older minority adults: results from take heart. J Gerontol A Biol Sci Med Sci. (2020) 75:922–8. doi: 10.1093/gerona/glz112
89. Robroek, SJ, Lindeboom, DE, and Burdorf, A. Initial and sustained participation in an internet-delivered long-term worksite health promotion program on physical activity and nutrition. J Med Internet Res. (2012) 14:e43. doi: 10.2196/jmir.1788
90. Samuel-Hodge, CD, Garcia, BA, Johnston, LF, Kraschnewski, JL, Gustafson, AA, Norwood, AF, et al. Rationale, design, and sample characteristics of a practical randomized trial to assess a weight loss intervention for low-income women: the weight-wise II program. Contemp Clin Trials. (2012) 33:93–103. doi: 10.1016/j.cct.2011.08.009
91. Sanchez, A, Silvestre, C, Campo, N, and Grandes, G. Type-2 diabetes primary prevention program implemented in routine primary care: a process evaluation study. Trials. (2016) 17:254. doi: 10.1186/s13063-016-1379-0
92. Santoyo-Olsson, J, Cabrera, J, Freyre, R, Grossman, M, Alvarez, N, Mathur, D, et al. An innovative multiphased strategy to recruit underserved adults into a randomized trial of a community-based diabetes risk reduction program. Gerontologist. (2011) 51:S82–93. doi: 10.1093/geront/gnr026
93. Sharpe, PA, Stucker, J, Wilcox, S, Liese, AD, and Bell, BA. Recruitment and retention for the evaluation of a healthy food initiative in economically disadvantaged, majority African American communities. Fam Community Health. (2021) 44:43–51. doi: 10.1097/FCH.0000000000000259
94. Snyder, DC, Morey, MC, Sloane, R, Stull, V, Cohen, HJ, Peterson, B, et al. Reach out to ENhancE Wellness in older cancer survivors (RENEW): design, methods and recruitment challenges of a home-based exercise and diet intervention to improve physical function among long-term survivors of breast, prostate, and colorectal cancer. Psycho-Oncology. (2009) 18:429–39. doi: 10.1002/pon.1491
95. Speck, RM, Hill, RK, Pronk, NP, Becker, MP, and Schmitz, KH. Assessment and outcomes of HealthPartners 10,000 steps program in an academic work site. Health Promot Pract. (2010) 11:741–50. doi: 10.1177/1524839908330745
96. Spittaels, H, and De Bourdeaudhuij, I. Who participates in a computer-tailored physical activity program delivered through the internet? A comparison of participants' and non-participants' characteristics. Int J Behav Nutr Phys Act. (2007) 4:39. doi: 10.1186/1479-5868-4-39
97. Stevens, M, de Jong, J, and Lemmink, KA. The Groningen active living model, an example of successful recruitment of sedentary and underactive older adults. Prev Med. (2008) 47:398–401. doi: 10.1016/j.ypmed.2008.07.004
98. Stineman, MG, Strumpf, N, Kurichi, JE, Charles, J, Grisso, JA, and Jayadevappa, R. Attempts to reach the oldest and frailest: recruitment, adherence, and retention of urban elderly persons to a falls reduction exercise program. Gerontologist. (2011) 51:S59–72. doi: 10.1093/geront/gnr012
99. Stopponi, MA, Alexander, GL, McClure, JB, Carroll, NM, Divine, GW, Calvi, JH, et al. Recruitment to a randomized web-based nutritional intervention trial: characteristics of participants compared to non-participants. J Med Internet Res. (2009) 11:e38. doi: 10.2196/jmir.1086
100. Taradash, J, Kramer, M, Molenaar, D, Arena, V, Vanderwood, K, and Kriska, AM. Recruitment for a diabetes prevention program translation effort in a worksite setting. Contemp Clin Trials. (2015) 41:204–10. doi: 10.1016/j.cct.2015.01.010
101. Tercyak, KP, Donze, JR, Prahlad, S, Mosher, RB, and Shad, AT. Identifying, recruiting, and enrolling adolescent survivors of childhood cancer into a randomized controlled trial of health promotion: preliminary experiences in the survivor health and resilience education (SHARE) program. J Pediatr Psychol. (2006) 31:252–61. doi: 10.1093/jpepsy/jsj013
102. Terry, PE, Fowles, JB, and Harvey, L. Employee engagement factors that affect enrollment compared with retention in two coaching programs--the ACTIVATE study. Popul Health Manag. (2010) 13:115–22. doi: 10.1089/pop.2009.0040
103. Thilsing, T, Larsen, LB, Sonderlund, AL, Andreassen, SS, Christensen, JR, Svensson, NH, et al. Effects of a co-design-based invitation strategy on participation in a preventive health check program: randomized controlled trial. JMIR Public Health Surveill. (2021) 7:e25617. doi: 10.2196/25617
104. Tidwell, L, Holland, SK, Greenberg, J, Malone, J, Mullan, J, and Newcomer, R. Community-based nurse health coaching and its effect on fitness participation. Lippincotts Case Manag. (2004) 9:267–79. doi: 10.1097/00129234-200411000-00006
105. Toobert, DJ, Strycker, LA, Glasgow, RE, and Bagdade, JD. If you build it, will they come? Reach and adoption associated with a comprehensive lifestyle management program for women with type 2 diabetes. Patient Educ Couns. (2002) 48:99–105. doi: 10.1016/S0738-3991(02)00120-9
106. Turner, CD, Lindsay, R, and Heisler, M. Peer coaching to improve diabetes self-management among low-income black veteran men: a mixed methods assessment of enrollment and engagement. Ann Fam Med. (2021) 19:532–9. doi: 10.1370/afm.2742
107. van der Giesen, FJ, van Lankveld, W, Hopman-Rock, M, de Jong, Z, Munneke, M, Hazes, JMW, et al. Exploring the public health impact of an intensive exercise program for patients with rheumatoid arthritis: a dissemination and implementation study. Arthritis Care Res. (2010) 62:865–72. doi: 10.1002/acr.20138
108. van Dongen, EJ, Duijzer, G, Jansen, SC, ter Beek, J, Huijg, JM, Leerlooijer, JN, et al. Process evaluation of a randomised controlled trial of a diabetes prevention intervention in Dutch primary health care: the SLIMMER study. Public Health Nutr. (2016) 19:3027–38. doi: 10.1017/S1368980016001282
109. van Holland, BJ, Brouwer, S, de Boer, MR, Reneman, MF, and Soer, R. Process evaluation of a workers' health surveillance program for meat processing workers. J Occup Rehabil. (2017) 27:307–18. doi: 10.1007/s10926-016-9657-y
110. Verburgh, M, Verdonk, P, Appelman, Y, Brood, M, Hulshof, C, and Nieuwenhuijsen, K. Workplace health promotion among ethnically diverse women in midlife with a low socioeconomic position. Health Educ Behav. (2022) 13:S282–3. doi: 10.1016/j.shaw.2021.12.1635
111. Vermunt, PWA, Milder, IEJ, Wielaard, F, van Oers, JAM, and Westert, GP. An active strategy to identify individuals eligible for type 2 diabetes prevention by lifestyle intervention in Dutch primary care: the APHRODITE study. Fam Pract. (2010) 27:312–9. doi: 10.1093/fampra/cmp100
112. Vincent, D, McEwen, MM, Hepworth, JT, and Stump, CS. Challenges and success of recruiting and retention for a culturally tailored diabetes prevention program for adults of Mexican descent. Diabetes Educ. (2013) 39:222–30. doi: 10.1177/0145721713475842
113. Wages, JG, Jackson, SF, Bradshaw, MH, Chang, M, and Estabrooks, PA. Different strategies contribute to community physical activity program participation in rural versus metropolitan settings. Am J Health Promot. (2010) 25:36–9. doi: 10.4278/ajhp.080729-ARB-143
114. Ward, DS, Vaughn, AE, Burney, RV, and Østbye, T. Recruitment of family child care homes for an obesity prevention intervention study. Contemp Clin Trials Commun. (2016) 3:131–8. doi: 10.1016/j.conctc.2016.05.001
115. Ware, LJ, Hurling, R, Bataveljic, O, Fairley, BW, Hurst, TL, Murray, P, et al. Rates and determinants of uptake and use of an internet physical activity and weight management program in office and manufacturing work sites in England: cohort study. J Med Internet Res. (2008) 10:e56. doi: 10.2196/jmir.1108
116. Weston, KL, Innerd, A, Azevedo, LB, Bock, S, and Batterham, AM. Process evaluation of project FFAB (fun fast activity blasts): a multi-activity school-based high-intensity interval training intervention. Front Sports Act Living. (2021) 3:737900. doi: 10.3389/fspor.2021.737900
117. Wilson, KE, Michaud, TL, Almeida, FA, Schwab, RJ, Porter, GC, Aquilina, KH, et al. Using a population health management approach to enroll participants in a diabetes prevention trial: reach outcomes from the PREDICTS randomized clinical trial. Transl Behav Med. (2021) 11:1066–77. doi: 10.1093/tbm/ibab010
118. Withall, J, Jago, R, and Fox, KR. The effect a of community-based social marketing campaign on recruitment and retention of low-income groups into physical activity programmes – a controlled before-and-after study. BMC Public Health. (2012) 12:836. doi: 10.1186/1471-2458-12-836
119. Xiao, H, Adams, SR, Goler, N, Sanna, RS, Boccio, M, Bellamy, DJ, et al. Wellness coaching for people with prediabetes: a randomized encouragement trial to evaluate outreach methods at Kaiser Permanente, northern California, 2013. Prev Chronic Dis. (2015) 12:E207. doi: 10.5888/pcd12.150251
120. Yancey, AK, Miles, OL, McCarthy, W, Sandoval, G, Hill, J, Leslie, JJ, et al. Differential response to targeted recruitment strategies to fitness promotion research by African-American women of varying body mass index. Ethn Dis. (2001) 11:115–23.
121. Yank, V, Stafford, RS, Rosas, LG, and Ma, J. Baseline reach and adoption characteristics in a randomized controlled trial of two weight loss interventions translated into primary care: a structured report of real-world applicability. Contemp Clin Trials. (2013) 34:126–35. doi: 10.1016/j.cct.2012.10.007
122. Yeary, KHK, Moore, PC, Gauss, CH, Cornell, C, Prewitt, TE, Shakya, S, et al. Reach and adoption of a randomized weight loss maintenance trial in rural African Americans of faith: the WORD (wholeness, oneness, righteousness, deliverance). Am J Health Promot. (2019) 33:549–57. doi: 10.1177/0890117118805065
123. Rogers, EM. Diffusion of preventive innovations. Addict Behav. (2002) 27:989–93. doi: 10.1016/S0306-4603(02)00300-3
124. Ryan, RM, and Deci, EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. (2000) 55:68–78. doi: 10.1037/0003-066X.55.1.68
125. Andreasen, AR. Social marketing – its definition and domain. J Public Policy Mark. (1994) 13:108–14. doi: 10.1177/074391569401300109
126. Liljas, AEM, Walters, K, Jovicic, A, Iliffe, S, Manthorpe, J, Goodman, C, et al. Strategies to improve engagement of 'hard to reach' older people in research on health promotion: a systematic review. BMC Public Health. (2017) 17:349. doi: 10.1186/s12889-017-4241-8
127. Rohr, S, Wittmann, F, Engel, C, Enzenbach, C, Witte, AV, Villringer, A, et al. Social factors and the prevalence of social isolation in a population-based adult cohort. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:1959–68. doi: 10.1007/s00127-021-02174-x
128. Bensa, K, and Sirok, K. Is it time to re-shift the research agenda? A scoping review of participation rates in workplace health promotion programs. Int J Environ Res Public Health. (2023) 20:1–30. doi: 10.3390/ijerph20032757
129. Song, L, Qan'ir, Y, Guan, T, Guo, P, Xu, S, Jung, A, et al. The challenges of enrollment and retention: a systematic review of psychosocial behavioral interventions for patients with Cancer and their family caregivers. J Pain Symptom Manag. (2021) 62:e279–304. doi: 10.1016/j.jpainsymman.2021.04.019
130. Tchouankam, T, Estabrooks, P, Cloyd, A, Notice, M, Teel-Williams, M, Smolsky, A, et al. Recruiting low-income African American men in mental Health Research: a community-based participatory research feasibility study. Am J Mens Health. (2021) 15:15579883211018418. doi: 10.1177/15579883211018418
131. Nhim, K, Gruss, SM, Porterfield, DS, Jacobs, S, Elkins, W, Luman, ET, et al. Using a RE-AIM framework to identify promising practices in National Diabetes Prevention Program implementation. Implement Sci. (2019) 14:81. doi: 10.1186/s13012-019-0928-9
132. Lee, RE, Reese-Smith, JY, Mama, SK, Medina, AV, Wolfe, KL, and Estabrooks, PA. Reach and representativeness of ethnic minority women in the health is Power study: a longitudinal analysis. Transl Behav Med. (2017) 7:106–14. doi: 10.1007/s13142-016-0385-9
133. Powell, BJ, Waltz, TJ, Chinman, MJ, Damschroder, LJ, Smith, JL, Matthieu, MM, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. (2015) 10:21. doi: 10.1186/s13012-015-0209-1
134. Baumann, AA, Hooley, C, Kryzer, E, Morshed, AB, Gutner, CA, Malone, S, et al. A scoping review of frameworks in empirical studies and a review of dissemination frameworks. Implement Sci. (2022) 17:53. doi: 10.1186/s13012-022-01225-4
136. Estabrooks, PA, Brownson, RC, and Pronk, NP. Dissemination and implementation science for public health professionals: an overview and call to action. Prev Chronic Dis. (2018) 15:E162. doi: 10.5888/pcd15.180525
137. Michie, S, and Abraham, C. Interventions to change health behaviours: evidence-based or evidence-inspired? Psychol Health. (2004) 19:29–49. doi: 10.1080/0887044031000141199
138. Smith, JD, Li, DH, Merle, JL, Keiser, B, Mustanski, B, and Benbow, ND. Adjunctive interventions: change methods directed at recipients that support uptake and use of health innovations. Implement Sci. (2024) 19:10. doi: 10.1186/s13012-024-01345-z
139. Estabrooks, PA, and Glasgow, RE. Developing a dissemination and implementation research agenda for aging and public health: the what, when, how, and why? Front Public Health. (2023) 11:1123349. doi: 10.3389/fpubh.2023.1123349
140. Fort, MP, Manson, SM, and Glasgow, RE. Applying an equity lens to assess context and implementation in public health and health services research and practice using the PRISM framework. Front Health Serv. (2023) 3:1139788. doi: 10.3389/frhs.2023.1139788
141. Morris, HN, Winslow, AT, Barreiro-Rosado, JA, Torian, S, and Charlot, M. Scoping Review of Barriers and Facilitators to Recruitment of Black People With Cancer in Biospecimen-Based Research. JCO Precision Oncology. (2024) 8. doi: 10.1200/PO.23.00708
Keywords: dissemination science, individual-level dissemination strategies, participant engagement, participant identification, participation rate, representativeness
Citation: Estabrooks PA, Bolyard ML, Casucci T, Christensen JT, Gibson B, Golden CA, Hill JL, Horvath L, Lee S, Maxfield EM, McFarland MM, Merle JL, Michaud TL, Miller M, Pereira EL, Schlechter CR, Simonsen SE, Wetter DW and Locke AB (2025) Identifying recruitment strategies to improve the reach of evidence-based health promotion, disease prevention, and disease self-management interventions: a scoping review. Front. Public Health. 13:1515042. doi: 10.3389/fpubh.2025.1515042
Received: 29 October 2024; Accepted: 06 February 2025;
Published: 01 April 2025.
Edited by:
Angela Kong, University of Illinois Chicago, United StatesReviewed by:
Tony Kuo, University of California, Los Angeles, United StatesCopyright © 2025 Estabrooks, Bolyard, Casucci, Christensen, Gibson, Golden, Hill, Horvath, Lee, Maxfield, McFarland, Merle, Michaud, Miller, Pereira, Schlechter, Simonsen, Wetter and Locke. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paul A. Estabrooks, cGF1bC5lc3RhYnJvb2tzQGhlYWx0aC51dGFoLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.