- 1Department of Basic Courses, Chongqing Medical and Pharmaceutical College, Chongqing, China
- 2The Second Clinical College, Chongqing Medical University, Chongqing, China
- 3College of Paediatrics, Chongqing Medical University, Chongqing, China
- 4Thirteenth People’s Hospital of Chongqing, Chongqing, China
- 5Department of Neurology, Chongqing General Hospital, Chongqing University, Chongqing, China
Background: Depressive symptoms are a common complication in patients with cataracts and may exacerbate cataract symptoms. Therefore, it is important to focus on depressive symptoms and their influencing factors in older people with cataracts. The purpose of this study was to investigate the prevalence rate of depressive symptoms and influencing factors in Chinese older people with cataracts.
Methods: Descriptive analyses were used to report the sociodemographic characteristics, lifestyle, health status, and depressive symptoms of old people with cataracts in China. The chi-square test was used to compare differences between subjects with different demographic characteristics. Binary logistic regression was used to analyze the factors that influenced the depressive symptoms of cataract patients. Meanwhile, a random forest model was developed in this study to rank the importance of the influencing factors.
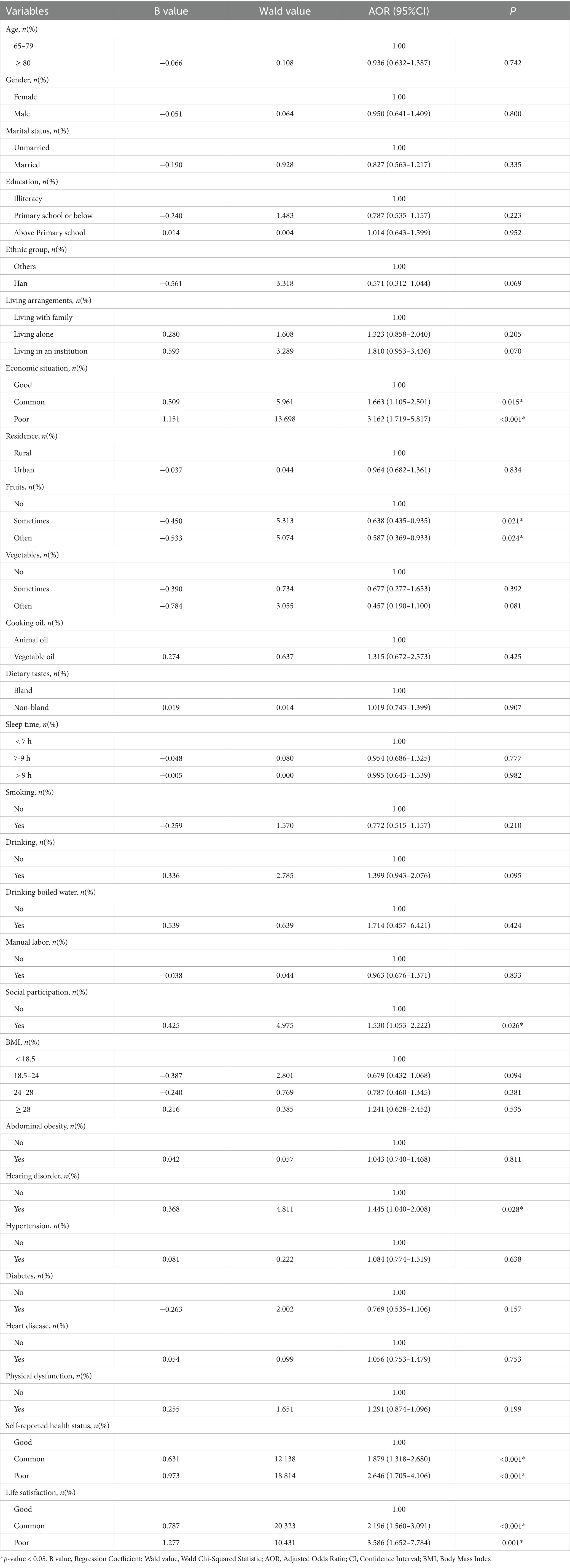
Results: Three hundred and six (25.27%) of 1,211 cataract patients included in this study suffered from depressive symptoms. Logistic regression analysis suggested that poor economic situation (AOR = 3.162, 95%CI: 1.719–5.817), social participation (AOR = 1.530, 95%CI: 1.053–2.222), having hearing disorder (AOR = 1.445, 95%CI: 1.040–2.008), poor self-reported health status (AOR = 2.646, 95%CI: 1.705–4.106), poor life satisfaction (AOR = 3.586, 95%CI: 1.652–7.784) were risk factors for depressive symptoms in cataract patients and consumption of fresh fruits (AOR = 0.587, 95%CI: 0.369–0.933) was a protective factor for depressive symptoms in cataract patients. The results of the random forest showed that self-reported health status was the most important factor influencing depressive symptoms in cataract patients. The other factors, in order of importance, were life satisfaction, economic situation, fruits, hearing disorder, and social participation.
Conclusion: The results suggested that the development of depressive symptoms in cataract patients was influenced by various factors. Medical staff should monitor these influencing factors more closely when treating and caring for patients with cataracts.
1 Introduction
The ocular condition known as cataracts is characterized by a pathological clouding of the lens and a clinical manifestation of vision loss, and its incidence increases significantly with aging (1). Cataract is the primary cause of blindness and the second most common cause of visual impairment worldwide (2). It was considered that over 15 million people worldwide were blind due to cataracts in 2020, accounting for about 45% of the 33.6 million blindness cases all over the world (3). Besides, it was estimated that the prevalence rate of cataracts in China will reach 33.34% among people aged 45–89 years, and the total of cataract cases would reach 240.83 million by the end of 2050 (2). Cataract-induced vision loss not only influences socioeconomic levels and access to education but also reduces patients’ life quality and increases their risk of developing psychological disorders such as depression (4, 5).
Depressive symptoms are a common complication in patients with ocular diseases (5). Studies have reported a combined prevalence rate of depression and depressive symptoms of up to 25% in cataract patients (6). The high prevalence rate of depressive symptoms in patients with cataracts may be due to age-related lens changes, which decrease the transmission of short-wave light, disrupting circadian rhythms and leading to sadness and sleeplessness (7). Secondly, fear of blindness, heavy financial burden, limitation of physical activity, difficulty in social interactions, and decline in life quality may all cause depressive symptoms in cataract patients (8–10). In addition, patients with depressive symptoms are more likely to show HPA axis disorders (11), leading to increased levels of glucocorticoids in the body. Exposure to high levels of glucocorticoids induces changes in the expression of relevant genes and activation of receptors in the lens epithelium (12), exacerbating the symptoms of cataracts. Thus, the high prevalence rate of depressive symptoms in cataract patients and the detrimental effect of depressive symptoms on cataracts create a vicious circle.
Even though depressive symptoms are common among ophthalmic patients in clinical practice, depression often goes unrecognized or untreated in ophthalmology clinics or ophthalmology outpatient clinics (13). Given that symptomatic interventions can improve depressive symptoms in visually impaired older people (14), it’s crucial to focus on the main influencing factors that lead to the development of depressive symptoms in cataract patients. Previous studies have investigated the prevalence rate of depressive symptoms and influencing factors in cataract patients in Chinese populations (8, 15, 16). However, by recruiting small and convenient samples, they did not consider the national representativeness of the influencing factors in Chinese older people. In addition, the research methods in previous related studies tended to be traditional logistic regression analysis. As a machine learning algorithm, Random Forest (RF) has become an excellent research tool due to its powerful classification ability and easy-to-interpret learning mechanism. In recent years, RF has been widely used in the medical aspect for diagnosis and classification of diseases (17), prediction of clinical outcomes (18), and estimation of the significance of exposure to disease-causing factors (19). In summary, we aimed to use the Chinese Longitudinal Healthy Longevity Survey (CLHLS) database to analyze the factors influencing the depressive symptoms of cataract patients in older people in terms of three dimensions: socio-demographic characteristics, lifestyle, and health status, and to apply the RF to the importance ranking.
2 Materials and methods
2.1 Data source
CLHLS began in 1998 and aimed to conduct a nationally representative survey of Chinese people aged over 65. The survey covers 23 provinces, municipalities, and autonomous regions across China, involving about 85% of the population. It collects information on the basic characteristics, socioeconomic characteristics, behavioral habits, dietary situation, and physical health of older people (20). The CLHLS received ethical approval from the Biomedical Ethics Committee of Peking University in China (IRB00001052-13074). Each participant completed an informed consent form before data collection.
2.2 Sample
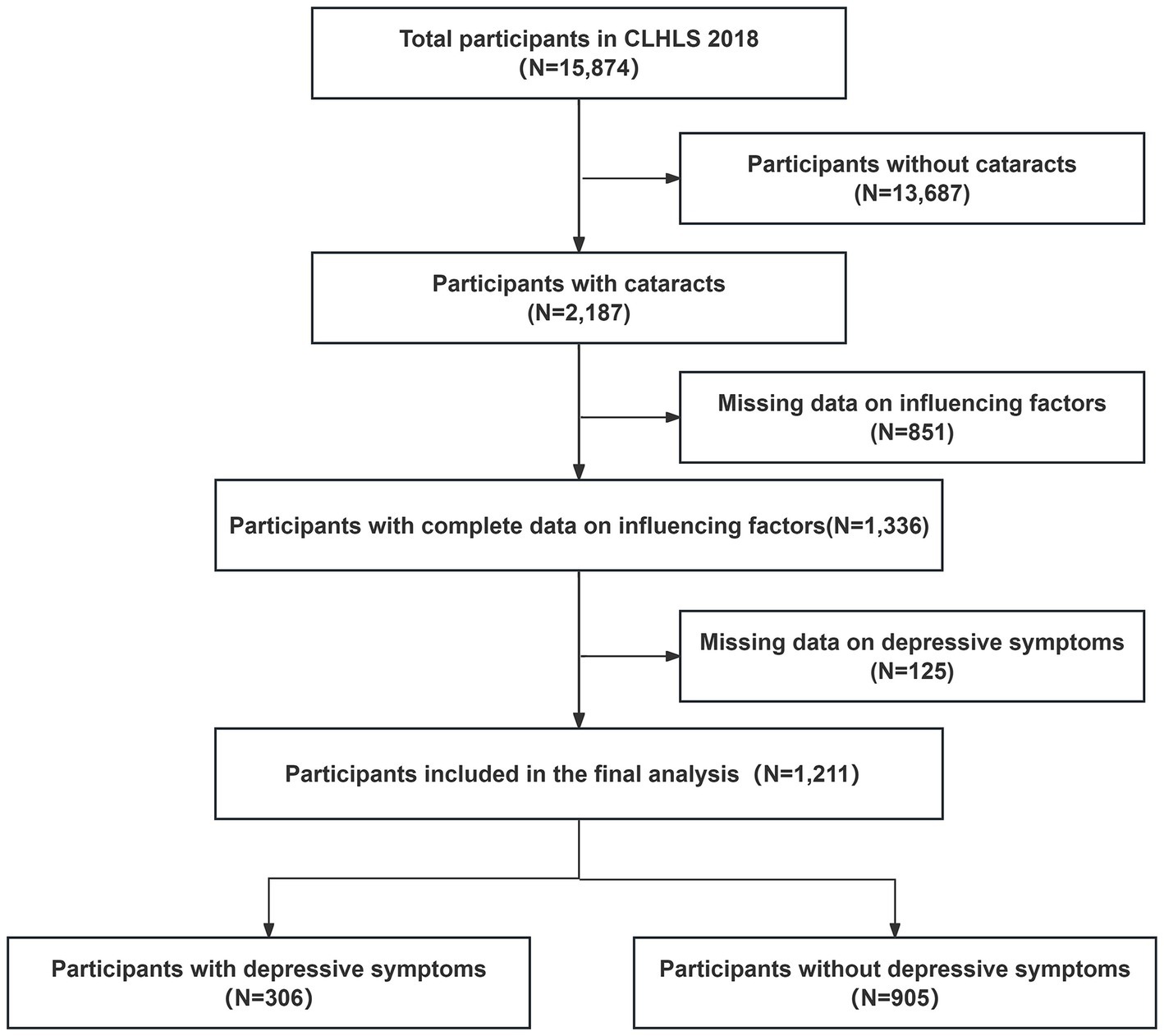
The study sample selection was based on the question in the questionnaire “Have you been diagnosed with cataracts?” Respondents who answered “yes” were involved in our study. A total of 15,874 participants were surveyed for the 2018 CLHLS, of which 2,187 participants were diagnosed with cataracts. After subsequent exclusion of missing data on depressive symptoms and possible influencing factor variables, 1,211 participants aged 65 years and older were included in the analysis. The detailed selection process is shown in Figure 1.
2.3 Patient characteristics
Based on previous studies about depressive symptoms (21–24), we screened 27 possible influencing factors from three dimensions: sociodemographic characteristics, lifestyle, and health status. The detailed variable assignments are in Supplementary Table S1.
Sociodemographic characteristics included age, gender, marital status, education, ethnic group, living arrangements, economic situation, and residence.
Lifestyle included fruits, vegetables, cooking oil, dietary tastes, sleep time, smoking, drinking, drinking boiled water, manual labor, and social participation.
Health status included Body Mass Index (BMI), abdominal obesity, hearing disorder, hypertension, diabetes, heart disease, self-reported health status, physical dysfunction and life satisfaction.
2.4 Assessment of depressive symptoms
The 10-item Center for Epidemiological Studies Depression scale (CESD-10) has been used to assess depressive symptoms in older people. Studies have verified that the scale is reliable for Chinese older people (25). Ten items are included in the scale, and the options for each item include (1) never or hardly (1 day); (2) seldom (1–2 days); (3) sometimes or often (3–4 days); and (4) usually or always (5–7 days). These four options were assigned values of 0, 1, 2, and 3. “Are you hopeful for the future?” and “Do you feel as happy as you did when you were younger?” were reverse-assigned before being summed. Total scores ranged from 0 to 30. Individuals with a depression score of 10 or greater were defined as having depressive symptoms (26).
2.5 Statistical analysis
Categorical variables were described by frequencies and percentages. The Chi-square test was used to compare the differences between different characteristics in the presence or absence of depressive symptoms. To further explore the factors influencing depressive symptoms in cataract patients, we used binary logistic regression models for analysis. The results of the regression analyses were reported as β, standard error, Wald’s chi-square, p-value, AOR, and 95% confidence interval (CI). To assess the importance of different influencing factors, we performed an RF importance ranking of the variables with statistical significance in the logistic regression model. As a machine-learning method based on the principles of ensemble learning, RF can handle classification and regression analysis, and its prediction results are accurate with stable predictive ability. Additionally, it can provide a simple visualization method to accurately rank the importance of relevant factors (27). Compared to traditional regression methods, the RF algorithm can avoid increasing estimated parameters or being insensitive to outliers when dealing with multi-level categorical variables, demonstrating strong resistance to interference. Therefore, applying RF can reduce bias, tolerate outliers, and decrease overfitting, thereby achieving more accurate and stable results (28). The samples were randomly divided into training and test sets on a 7:3 basis, the best parameters of the model were obtained through grid optimization, and the model was tested by a 10-fold cross-validation method. The variables were ranked in terms of importance based on the average reduction in the Gini index. Specifically, the greater the average decrease in the Gini index of a variable, the more important the variable is (29). Sensitivity, specificity, recall, accuracy, F1 score, and area under the curve (AUC) were used to evaluate the performance of the random forest model. All data analyses were performed using SPSS 26.0 and R 4.3.0, and p < 0.05 (two-sided) was considered statistically significant.
3 Results
3.1 Sociodemographic characteristics and depressive symptoms in Chinese cataract patients
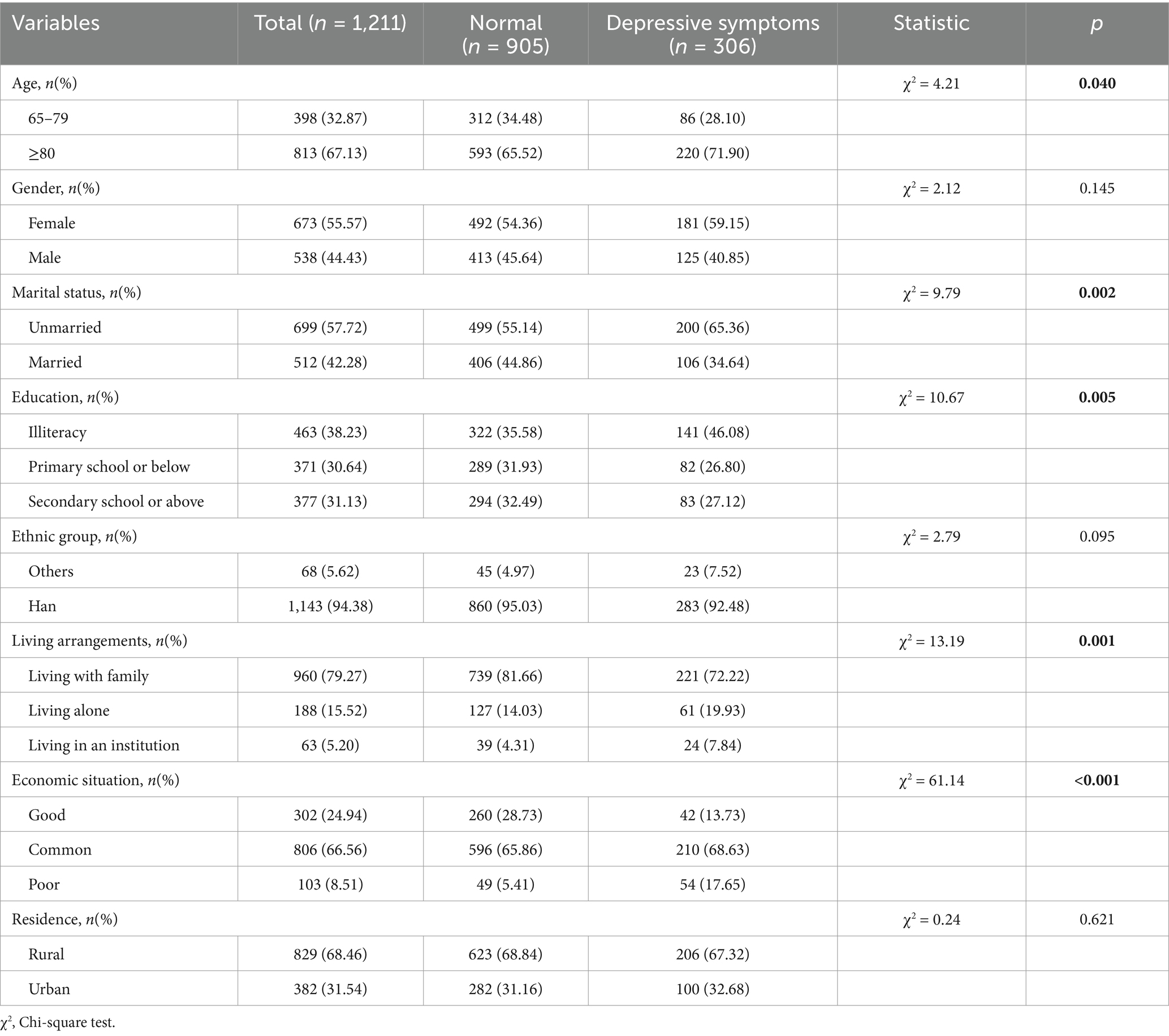
Table 1 shows the descriptive results of sociodemographic characteristics and their chi-square test results with depressive symptoms. Three hundred and six (25.27%) of the 1,211 patients suffered from depressive symptoms, 67.13% of the patients were aged ≥80 years, 44.43% were male, 42.28% were married, 38.23% were illiterate, 30.64% received primary school education or below, and 31.13% received secondary education or above. Most patients were of Han nationality (94.38%), 79.27% lived with their families, and 8.51% had poor economic situation. Patients living in rural areas accounted for 68.46% of the total sample.
The chi-square test results showed that age, marital status, education, living arrangements, and economic situation had an apparent effect on the depressive symptoms in cataract patients (Table 1). Specifically, cataract patients who were ≥ 80 years (71.90% vs. 65.52%, p = 0.040), unmarried (65.36% vs. 55.14%, p = 0.002), and illiterate (46.08% vs. 35.58%, p = 0.005) were more likely to experience depressive symptoms. Those living with family (72.22% vs. 81.66%, p = 0.001) and having good economic situation (13.73% vs. 28.73%, p < 0.001) were less likely to have depressive symptoms.
3.2 Lifestyle and depressive symptoms of Chinese cataract patients
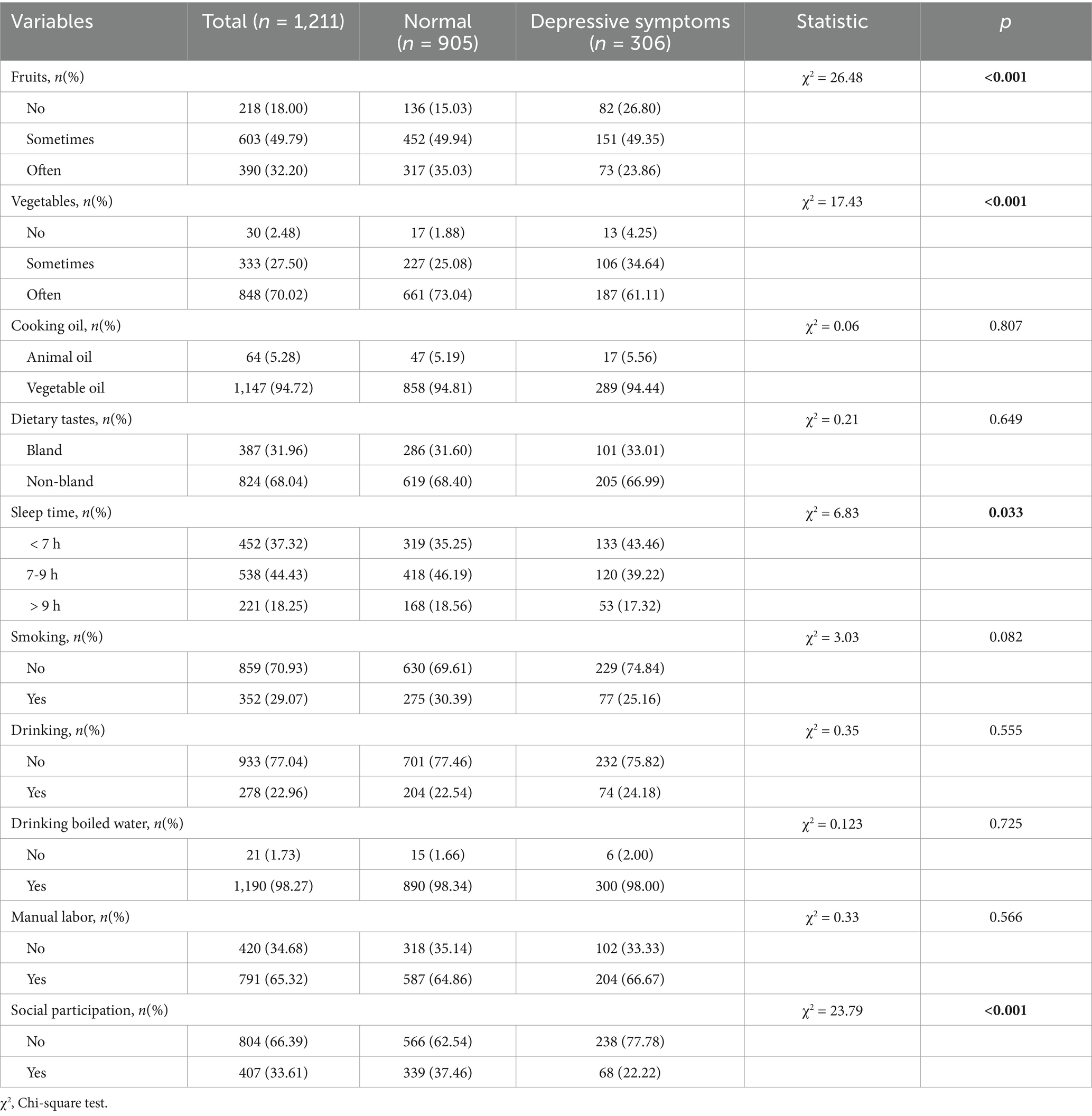
The basic information on lifestyle characteristics and the results of their chi-square test with depressive symptoms are shown in Table 2. The proportion of cataract patients who ate fruits and vegetables every day was 32.20 and 70.02%, respectively. Most patients preferred to consume vegetable oil (94.72%) and drink boiled water (98.27%), while 31.96% had a bland dietary taste. The highest number of patients (538) had a sleep time between 7 and 9 h per day at night. About 29.07% of the patients had a habit of smoking, 22.96% had a habit of drinking, 65.32% used to engage in manual labor regularly, and 33.61% engaged in social participation.
3.3 Health status and depressive symptoms of Chinese cataract patients
Table 3 shows the descriptive results of the health status of cataract patients and the results of the chi-square test with depressive symptoms. About 12.47% of the patients had a BMI < 18.5, while 8.34% had a BMI > 28, and nearly half (47.89%) of the patients had abdominal obesity. Hearing disorder, hypertension, diabetes, and heart disease were present in 39.55, 63.25, 32.95, and 42.36% of the cataract patients, respectively. Approximately 22.13% had impaired daily activity ability. In terms of self-reported health status, 44.76% of the patients considered it good, 37.49% considered it common and 17.75% considered it poor. Only 3.72% of patients were dissatisfied with their life quality status.
Patients who were thin (16.67% vs. 11.05%, p = 0.036) and overweight (9.80% vs. 7.85%, p = 0.036), had hearing disorder (48.69% vs. 36.46%, p < 0.001), and had physical dysfunction (31.05% vs. 19.12%, p < 0.001) were more likely to have depressive symptoms. Cataract patients with depressive symptoms had poor self-reported health status (32.68% vs. 12.71%, p < 0.001) and poor life satisfaction (10.13% vs. 1.55%, p < 0.001).
3.4 Logistic regression analysis of depressive symptoms among Chinese cataract patients
Logistic regression analysis suggested that economic situation, fruit consumption, social participation, hearing disorder, self-reported health status, and life satisfaction were independent factors influencing depressive symptoms in cataract patients (Table 4). Cataract patients with poor economic situation were more likely to develop depressive symptoms than those with good economic situation (AOR = 3.162, 95%CI: 1.719–5.817). Consumption of fresh fruits was a protective factor for depressive symptoms in cataract patients, with cataract patients who ate fresh fruits almost every day being 41.3% less likely to develop depressive symptoms compared to those who did not eat fruits (95%CI: 0.369–0.933). Patients with social participation tended to develop depressive symptoms compared to those without social participation (AOR = 1.530, 95%CI: 1.053–2.222). Patients with hearing disorders were more likely to show depressive symptoms than those without (AOR = 1.445, 95%: 1.040–2.008). Moreover, cataract patients with poor self-reported health status were 2.646 times more likely to exhibit depressive symptoms than those with good self-reported health status (95%CI: 1.705–4.106). Cataract patients with poor life satisfaction were 3.586 times more likely to exhibit depressive symptoms than those with good life satisfaction (95%CI: 1.652–7.784).
3.5 Random Forest results
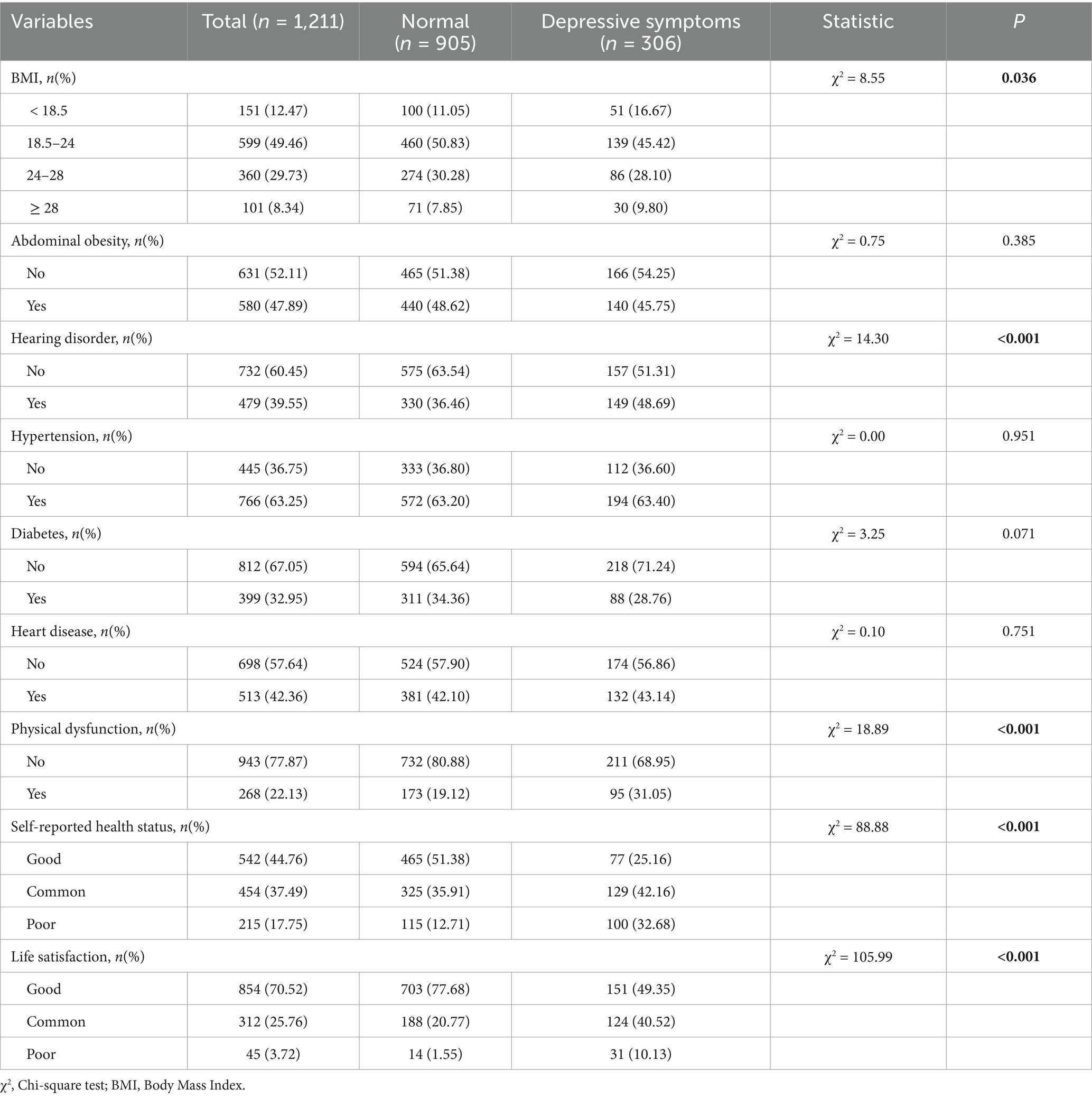
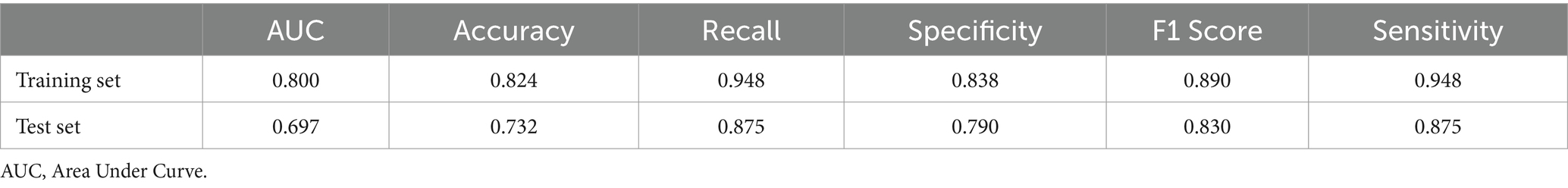
In order to assess the importance of significant influencing factors in the logistic regression model on the impact of depressive symptoms, we further established an RF model to rank the variable importance. Specifically, this study established a random forest model with the parameter ‘mtry’ set to 3 and the parameter ‘ntree’ set to 500 by randomly selecting 70% of the overall data as the training set and 30% as the test set. The RF algorithm measured the impact of each variable on the dependent variable through the importance score of the variables. The greater the average decrease in the Gini index, the more important the variable. The results of RF indicated that self-reported health status was the key factor affecting depressive symptoms in cataract patients, with other factors influencing depressive symptoms in cataract patients in the following order of importance: life satisfaction, economic situation, fruits, hearing disorder, and social participation (Figure 2). Table 5 shows the performance metrics of the random forest model on the training and test sets, all of which indicate that the model performs well.
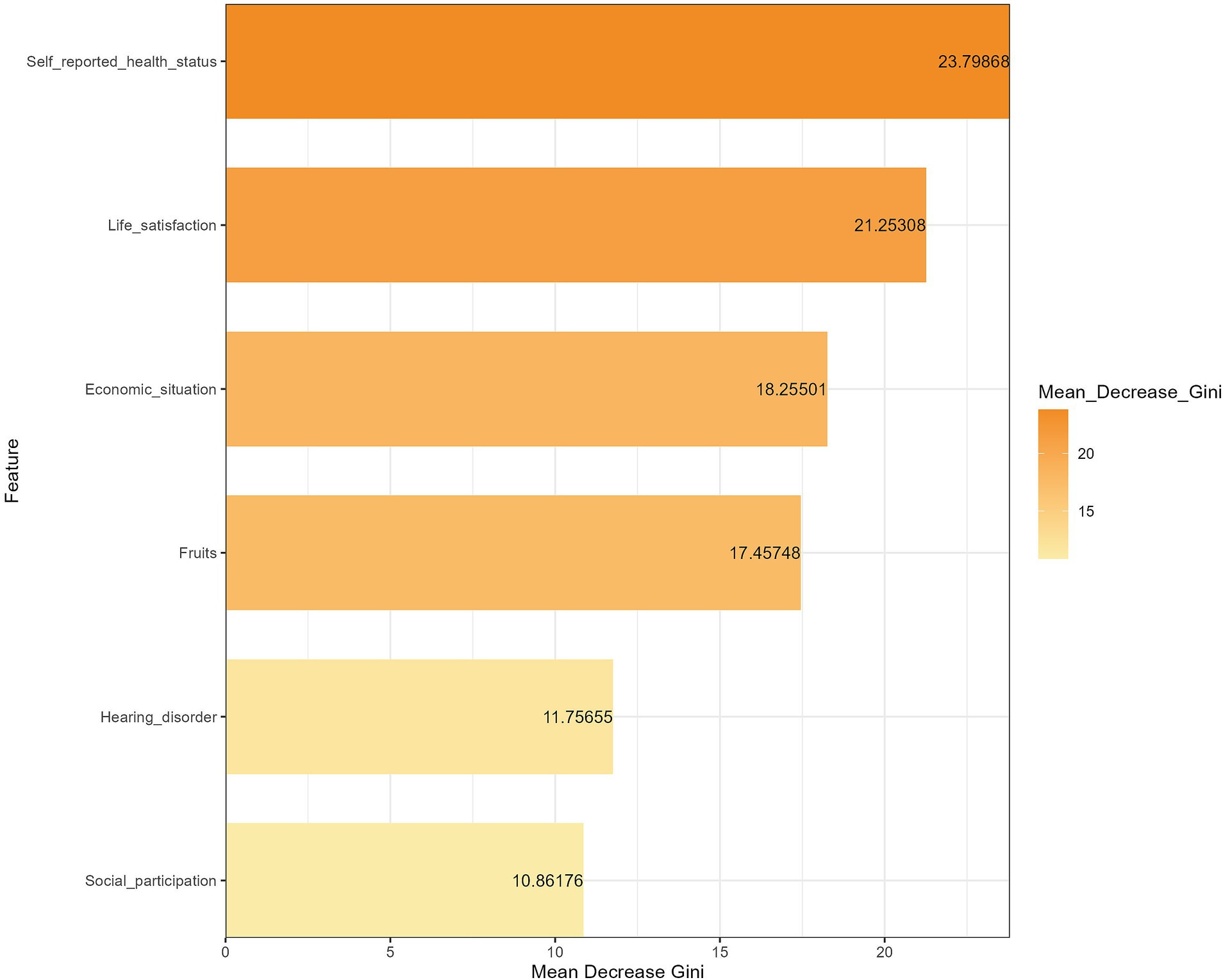
Figure 2. Ranking of the importance of different factors on depressive symptoms among Chinese cataract patients.
4 Discussion
To our knowledge, this study is the first to report on the prevalence and influencing factors of depressive symptoms in older people with cataracts in China. Based on a nationally representative database, we explored the factors that influenced depressive symptoms in cataract patients from three dimensions: sociodemographic characteristics, lifestyle, and health status. We also performed a random forest importance ranking of the significant factors. We observed that depressive symptoms prevalence rate in Chinese older people with cataracts was 25.27%, which is comparable to the results of Liu et al. (16). Dandan Zhang et al. reported a prevalence rate of 18.00% of depressive symptoms in Chinese cataract patients, compared with 5.2% in healthy individuals (8), which suggests that cataract patients have higher risk of developing depressive symptoms. Moreover, a 16-year longitudinal survey confirmed the higher risk of clinically diagnosed depression in cataract patients (30). In addition, several studies in the United States, Australia, and Japan have consistently indicated that cataract patients experience more severe depressive symptoms than healthy individuals (31–33).
Individuals with cataracts in poor economic situations are at increased risk of developing depressive symptoms compared to those in better economic situations. A meta-analysis carried out by Lorant et al. indicated that individuals of low socioeconomic status were at higher risk of depression, with each 1% increase in income rank being associated with a 0.74 decline in the log odds of developing depressive symptoms (34). In general, cataract patients with poor economic situations have poor life quality and daily health care and may have more irregularities in cataract intervention care (35), which may exacerbate cataracts to some extent. And the deterioration of the disease and the low quality of life will increase the psychological burden of patients and increase the risk of depressive symptoms. In addition, people with poor economic situations may not have sufficient social support resources to deal with their mental health problems, leading to an increased risk of depressive symptoms in these patients.
Fruits and vegetables have been treated as a crucial part of a healthy diet all the time, and their rich nutrients (e.g., polyphenols, flavonoids, and antioxidant vitamins) are able to counteract oxidative stress and inflammation, playing an important role in improving cataract progression (36). Also, the protective effect of fruits and vegetables against depressive symptoms has long been demonstrated (37). Their beneficial effects on depression may be attributed to the high levels of antioxidants, dietary fiber, and vitamins they contain that play a role in inflammation, oxidative stress, and gut microbiota (38). Interestingly, only fruits were observed to have a protective effect on depressive symptoms in our study, which may be due to differences in how fruits and vegetables are consumed. In China, vegetables are usually cooked, leading to the degradation or loss of certain beneficial nutrients, such as the antioxidant vitamin C, whereas fruits are usually consumed raw. This nutrient loss during cooking may lead to the unobserved protective effect of vegetables on depressive symptoms in cataract patients in our study. Further research is needed to find the effects of different vegetable processing methods on depressive symptoms.
Studies have shown that social participation is a crucial mediator in mitigating the effects of visual impairment on depressive symptoms (39). The study by Simone Croezen et al. also indicated that social participation can reduce the risk of depressive symptoms in older people, which contradicts our research findings (40). Activity Theory suggests that engaging in social activities may help maintain a positive self-perception and boost self-esteem, thereby buffering the negative impact of aging on mental health (41). The Role Accumulation Theory holds that a large number of role identifications imply extensive social support, which can help older people maintain a certain level of social participation, thereby promoting positive mental health outcomes (42). Social participation may provide opportunities for older people to establish social relationships and engage in emotional exchanges, resulting in higher levels of perceived connection and lower levels of loneliness (43). However, our study showed that cataract patients who had social participation were more likely to have depressive symptoms. We hypothesized that due to severe vision problems, older people with cataracts feel isolated and stressed and have difficulty adapting to social participation, leading to an inability to engage in effective social participation (44). In addition, comparisons with others, difficulties with self-expression, and stigma and discrimination may exacerbate feelings of shame and lower self-esteem in people with cataracts, and this negative change in self-image may also lead to depressive symptoms (45). Once people experience negative social events or social rejection, they may become inertial or resistant to social participation, which may become a vicious cycle (46) and cause high depressive symptoms prevalence.
The prevalence rate of hearing disorder is higher in cataract patients, and hearing disorder has a significant correlation with depressive symptoms in cataract patients. The prevalence rate of poor hearing and vision is high in older people, which is considered to be an age-related degeneration (47). A cohort study showed that patients with both hearing and visual disorders were at significantly higher risk of developing depressive symptoms, with patients who have dual sensory impairment showing more severe depressive symptoms (48). Loneliness and social isolation caused by dual sensory deprivation in cataract patients with hearing disorders may contribute to their high prevalence of depressive symptoms (49, 50).
Our findings showed that poor self-reported health status and poor life satisfaction were significantly associated with depressive symptoms in cataract patients. Research has indicated that older people with visual impairment are more likely to report their poor health (51). Patients with cataracts may have certain lifestyle and health management challenges, such as an unbalanced diet and insufficient physical activity, which may raise the risk of developing chronic diseases and lead to a greater likelihood of reporting poor health. Persistent physical discomfort, dysfunction, and decreased life quality after multiple chronic conditions can increase the risk of developing depressive symptoms (52, 53). Life satisfaction refers to an individual’s overall well-being, which is strongly linked to health outcomes such as pain, physical functioning, chronic disease, and mortality (54). When people experience vision loss, well-being may be significantly reduced and accompanied by a range of adverse health conditions, resulting in a greater likelihood of reporting poor life satisfaction. And previous studies have also reported that people who report poor life satisfaction are more likely to experience depressive symptoms (55), which explains the significant association between life satisfaction and depressive symptoms in cataract patients.
The results of this study using RF indicate that self-reported health status is the most important factor affecting depressive symptoms in cataract patients, followed by life satisfaction, economic situation, fruits, hearing disorder, and social participation. Therefore, strategies to improve depressive symptoms in older people with cataracts should primarily focus on enhancing their awareness and ability to self-evaluate their health. Public health departments urgently need to take action by widely disseminating health knowledge through diverse channels such as community forums, television broadcasts, and online platforms to deepen cataract patients’ understanding and assessment of their own health conditions. Specifically, for this vulnerable group, educational forms that are more aligned with their needs should be adopted, such as face-to-face lectures and home visit services, to overcome their reading barriers with written materials. Public health education and promotion should emphasize the importance of individuals assessing and perceiving their own health conditions, encouraging cataract patients to regularly self-evaluate their health and promptly identify and report psychological issues. At the same time, regular health check-ups and chronic disease screenings should be promoted as routine practices, with systematic follow-up management for diagnosed patients, assisting them in comprehensively understanding their health conditions through effective communication. Additionally, this study calls for the government and all sectors of society to pay attention to the economic difficulties faced by older people with cataracts and to alleviate their financial burden through improved medical insurance policies and medical assistance. In terms of nutritional guidance, a balanced diet should be advocated, especially increasing the intake of foods rich in vitamins and minerals, particularly fruits, to enhance the body’s resistance. For cataract patients with hearing disorder, hearing screenings should be implemented, and hearing aids or interventions should be provided in a timely manner to reduce the negative impact of hearing impairments on mental health. Comprehensive measures should be taken from multiple dimensions, such as medical care, lifestyle, mental health, and social support, to improve the life satisfaction and well-being of older people with cataracts. It is worth noting that the complex relationship between social participation and depressive symptoms in older people with cataracts still needs further exploration and research. In summary, public health departments should formulate and implement comprehensive intervention strategies to comprehensively improve the depressive symptoms of older people with cataracts.
5 Summary
Based on the CLHLS database, this study evaluated the prevalence of depressive symptoms among older people with cataracts aged 65 and above in China and identified related influencing factors. A random forest model was used to rank the importance of these factors. The results showed that self-reported health status is the most important factor influencing depressive symptoms in cataract patients. Other factors were ranked in order of importance as life satisfaction, economic situation, fruits, hearing disorder, and social participation. Based on this, medical staff should monitor these influencing factors more closely when treating and caring for patients with cataracts.
6 Limitations
There are several limitations of this study. Firstly, the selection of influencing factors for this study was limited by the structure of the questionnaire. Therefore, we cannot guarantee that all potential factors were included in this study. Second, the variables we studied were all measured by self-reported questions, which may lead to recall bias. Third, the data we used were obtained from a cross-sectional survey, which precludes any causal inference about the relationship between depressive symptoms and their influencing factors in cataract patients.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: the data of CLHLS are available at: https://opendata.pku.edu.cn/dataverse/CHADS.
Ethics statement
This study was based on publicly available datasets (CLHLS). Ethical review and approval was not required for the study, in accordance with the local legislation and institutional requirements. Written informed consent from the participants or the participants’ legal guardian/next of kin] was not required to participate in this study in accordance with the national legislation and the institutional requirements. CLHLS received ethical approval from the Biomedical Ethics Committee of Peking University in China (IRB00001052-13074); each participant completed an informed consent form before data collection.
Author contributions
TN: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. SC: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. XW: Investigation, Validation, Visualization, Writing – review & editing. XX: Formal analysis, Visualization, Writing – review & editing. CL: Data curation, Project administration, Supervision, Writing – review & editing. JM: Data curation, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Medical Scientific Research Project of Chongqing Municipal Health Commission (grant nos. 2020MSXM106 and 2024MSXM127).
Acknowledgments
The authors would like to thank all the participants involved in this project for their contribution and dedication sincerely.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1504275/full#supplementary-material
References
1. Asbell, PA, Dualan, I, Mindel, J, Brocks, D, Ahmad, M, and Epstein, S. Age-related cataract. Lancet. (2005) 365:599–609. doi: 10.1016/S0140-6736(05)70803-5
2. Song, P, Wang, H, Theodoratou, E, Chan, KY, and Rudan, I. The national and subnational prevalence of cataract and cataract blindness in China: a systematic review and meta-analysis. J Glob Health. (2018) 8:010804. doi: 10.7189/jogh.08.010804
3. GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the right to sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. (2021) 9:e144–60. doi: 10.1016/S2214-109X(20)30489-7
4. Lou, L, Wang, J, Xu, P, Ye, X, and Ye, J. Socioeconomic disparity in global burden of cataract: an analysis for 2013 with time trends since 1990. Am J Ophthalmol. (2017) 180:91–6. doi: 10.1016/j.ajo.2017.04.008
5. Wang, S, Du, Z, Lai, C, Seth, I, Wang, Y, Huang, Y, et al. The association between cataract surgery and mental health in older adults: a review. Int J Surg. (2024) 110:2300–12. doi: 10.1097/JS9.0000000000001105
6. Zheng, Y, Wu, X, Lin, X, and Lin, H. The prevalence of depression and depressive symptoms among eye disease patients: a systematic review and meta-analysis. Sci Rep. (2017) 7:46453. doi: 10.1038/srep46453
7. Turner, PL, and Mainster, MA. Circadian photoreception: ageing and the eye's important role in systemic health. Br J Ophthalmol. (2008) 92:1439–44. doi: 10.1136/bjo.2008.141747
8. Zhang, D, Fan, Z, Gao, X, Huang, W, Yang, Q, Li, Z, et al. Illness uncertainty, anxiety and depression in Chinese patients with glaucoma or cataract. Sci Rep. (2018) 8:11671. doi: 10.1038/s41598-018-29489-1
9. Evans, JR, Fletcher, AE, and Wormald, RP. Depression and anxiety in visually impaired older people. Ophthalmology. (2007) 114:283–8. doi: 10.1016/j.ophtha.2006.10.006
10. Morse, AR. Vision function, functional vision, and depression. JAMA Ophthalmol. (2013) 131:667–8. doi: 10.1001/jamaophthalmol.2013.61
11. Dwyer, JB, Aftab, A, Radhakrishnan, R, Widge, A, Rodriguez, CI, Carpenter, LL, et al. Hormonal treatments for major depressive disorder: state of the art. Am J Psychiatry. (2020) 177:686–705. doi: 10.1176/appi.ajp.2020.19080848
12. Wang, JJ, Rochtchina, E, Tan, AG, Cumming, RG, Leeder, SR, and Mitchell, P. Use of inhaled and oral corticosteroids and the long-term risk of cataract. Ophthalmology. (2009) 116:652–7. doi: 10.1016/j.ophtha.2008.12.001
13. Parravano, M, Petri, D, Maurutto, E, Lucenteforte, E, Menchini, F, Lanzetta, P, et al. Association between visual impairment and depression in patients attending eye clinics: a meta-analysis. JAMA Ophthalmol. (2021) 139:753–61. doi: 10.1001/jamaophthalmol.2021.1557
14. van der Aa, HP, van Rens, GH, Comijs, HC, Margrain, TH, Gallindo-Garre, F, Twisk, JW, et al. Stepped care for depression and anxiety in visually impaired older adults: multicentre randomised controlled trial. BMJ. (2015) 351:h 6127. doi: 10.1136/bmj.h6127
15. Wang, H, Sun, HP, Wang, P, Xu, Y, and Pan, CW. Cataract and depressive symptoms among older Chinese adults. Optom Vis Sci. (2016) 93:1479–84. doi: 10.1097/OPX.0000000000000960
16. Liu, ZH, Chen, CZ, Gao, C, and Zhou, DY. Prevalence and correlates of depressive symptoms among Chinese patients with cataracts treated in tertiary general hospitals. Peer J. (2020) 8:e9397. doi: 10.7717/peerj.9397
17. Wang, ST, Wang, YY, Wang, DJ, Yin, YQ, Wang, YZ, and Jin, YC. An improved random forest-based rule extraction method for breast cancer diagnosis. Appl Soft Comput. (2020) 86:105941. doi: 10.1016/j.asoc.2019.105941
18. Guo, L, Wang, Z, Du, Y, Mao, J, Zhang, J, Yu, Z, et al. Random-forest algorithm based biomarkers in predicting prognosis in the patients with hepatocellular carcinoma. Cancer Cell Int. (2020) 20:251. doi: 10.1186/s12935-020-01274-z
19. Liu, Y, Xu, Y, Yang, X, Miao, G, Wu, Y, and Yang, S. The prevalence of anxiety and its key influencing factors among the elderly in China. Front Psych. (2023) 14:1038049. doi: 10.3389/fpsyt.2023.1038049
20. Lv, Y, Zhang, Y, Li, X, Gao, X, Ren, Y, Deng, L, et al. Body mass index, waist circumference, and mortality in subjects older than 80 years: a Mendelian randomization study. Eur Heart J. (2024) 45:2145–54. doi: 10.1093/eurheartj/ehae206
21. Anderson, E, Crawford, CM, Fava, M, Ingelfinger, J, Nikayin, S, Sanacora, G, et al. Depression-understanding, identifying, and diagnosing. N Engl J Med. (2024) 390:e41. doi: 10.1056/NEJMp2310179
22. Alexopoulos, GS. Depression in the elderly. Lancet. (2005) 365:1961–70. doi: 10.1016/S0140-6736(05)66665-2
23. Wassink-Vossen, S, Collard, RM, Wardenaar, KJ, Verhaak, PFM, Rhebergen, D, Naarding, P, et al. Trajectories and determinants of functional limitations in late-life depression: a 2-year prospective cohort study. Eur Psychiatry. (2019) 62:90–6. doi: 10.1016/j.eurpsy.2019.09.003
24. Jeuring, HW, Stek, ML, Huisman, M, Oude Voshaar, RC, Naarding, P, Collard, RM, et al. A six-year prospective study of the prognosis and predictors in patients with late-life depression. Am J Geriatr Psychiatry. (2018) 26:985–97. doi: 10.1016/j.jagp.2018.05.005
25. Zhao, X, Ruan, Z, Tian, Y, Du, W, and Fan, L. Estimating the joint effect of household solid fuel use and social isolation on depression among middle-aged and older adults in China. Sci Total Environ. (2023) 901:166411. doi: 10.1016/j.scitotenv.2023.166411
26. Li, H, Zheng, D, Li, Z, Wu, Z, Feng, W, Cao, X, et al. Association of depressive symptoms with incident cardiovascular diseases in middle-aged and older Chinese adults. JAMA Netw Open. (2019) 2:e1916591. doi: 10.1001/jamanetworkopen.2019.16591
27. Ren, H, Yang, T, Yin, X, Tong, L, Shi, J, Yang, J, et al. Prediction of high-level fear of cancer recurrence in breast cancer survivors: an integrative approach utilizing random forest algorithm and visual nomogram. Eur J Oncol Nurs. (2024) 70:102579. doi: 10.1016/j.ejon.2024.102579
28. Chen, Z, Ying, TC, Chen, J, Wang, Y, Wu, C, and Su, Z. Assessment of renal fibrosis in patients with chronic kidney disease using shear wave elastography and clinical features: a random Forest approach. Ultrasound Med Biol. (2023) 49:1665–71. doi: 10.1016/j.ultrasmedbio.2023.03.024
29. Grömping, U. Variable importance assessment in regression: linear regression versus random Forest. Am Stat. (2009) 63:308–19. doi: 10.1198/tast.2009.08199
30. Chen, PW, Liu, PP, Lin, SM, Wang, JH, Huang, HK, and Loh, CH. Cataract and the increased risk of depression in general population: a 16-year nationwide population-based longitudinal study. Sci Rep. (2020) 10:13421. doi: 10.1038/s41598-020-70285-7
31. Frank, CR, Xiang, X, Stagg, BC, and Ehrlich, JR. Longitudinal associations of self-reported vision impairment with symptoms of anxiety and depression among older adults in the United States. JAMA Ophthalmol. (2019) 137:793–800. doi: 10.1001/jamaophthalmol.2019.1085
32. Palagyi, A, Rogers, K, Meuleners, L, McCluskey, P, White, A, Ng, JQ, et al. Depressive symptoms in older adults awaiting cataract surgery. Clin Experiment Ophthalmol. (2016) 44:789–96. doi: 10.1111/ceo.12800
33. Ishii, K, Kabata, T, and Oshika, T. The impact of cataract surgery on cognitive impairment and depressive mental status in elderly patients. Am J Ophthalmol. (2008) 146:404–9. doi: 10.1016/j.ajo.2008.05.014
34. Lorant, V, Deliège, D, Eaton, W, Robert, A, Philippot, P, and Ansseau, M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. (2003) 157:98–112. doi: 10.1093/aje/kwf182
35. Theilla, M, Singer, P, Tadmor, B, Bendavid, I, Hellerman, M, and Kagan, I. Community optimized management for better eating after hospital sTay among geriatric patients of poor socio-economic status - the COMEAT study. Clin Nutr. (2022) 41:1746–51. doi: 10.1016/j.clnu.2022.06.023
36. Sella, R, and Afshari, NA. Nutritional effect on age-related cataract formation and progression. Curr Opin Ophthalmol. (2019) 30:63–9. doi: 10.1097/ICU.0000000000000537
37. Matison, AP, Mather, KA, Flood, VM, and Reppermund, S. Associations between nutrition and the incidence of depression in middle-aged and older adults: a systematic review and meta-analysis of prospective observational population-based studies. Ageing Res Rev. (2021) 70:101403. doi: 10.1016/j.arr.2021.101403
38. Marx, W, Lane, M, Hockey, M, Aslam, H, Berk, M, Walder, K, et al. Diet and depression: exploring the biological mechanisms of action. Mol Psychiatry. (2021) 26:134–50. doi: 10.1038/s41380-020-00925-x
39. He, W, Li, P, Gao, Y, You, J, Chang, J, Qu, X, et al. Self-reported visual impairment and depression of middle-aged and older adults: the chain-mediating effects of internet use and social participation. Front Public Health. (2022) 10:957586. doi: 10.3389/fpubh.2022.957586
40. Croezen, S, Avendano, M, Burdorf, A, and van Lenthe, FJ. Social participation and depression in old age: a fixed-effects analysis in 10 European countries. Am J Epidemiol. (2015) 182:168–76. doi: 10.1093/aje/kwv015
41. Hao, Y. Productive activities and psychological well-being among older adults. J Gerontol B Psychol Sci Soc Sci. (2008) 63:S64–72. doi: 10.1093/geronb/63.2.S64
42. Adelmann, PK. Multiple roles and psychological well-being in a national sample of older adults. J Gerontol. (1994) 49:S277–85. doi: 10.1093/geronj/49.6.S277
43. Park, NS, Jang, Y, Lee, BS, Haley, WE, and Chiriboga, DA. The mediating role of loneliness in the relation between social engagement and depressive symptoms among older Korean Americans: do men and women differ? J Gerontol B Psychol Sci Soc Sci. (2013) 68:193–201. doi: 10.1093/geronb/gbs062
44. Senra, H, Barbosa, F, Ferreira, P, Vieira, CR, Perrin, PB, Rogers, H, et al. Psychologic adjustment to irreversible vision loss in adults: a systematic review. Ophthalmology. (2015) 122:851–61. doi: 10.1016/j.ophtha.2014.10.022
45. Jackson, SE, Hackett, RA, Pardhan, S, Smith, L, and Steptoe, A. Association of Perceived Discrimination with Emotional Well-being in older adults with visual impairment. JAMA Ophthalmol. (2019) 137:825–32. doi: 10.1001/jamaophthalmol.2019.1230
46. Morse, AR. Addressing the maze of vision loss and depression. JAMA Ophthalmol. (2019) 137:832–3. doi: 10.1001/jamaophthalmol.2019.1234
47. Huang, CQ, Dong, BR, Lu, ZC, Yue, JR, and Liu, QX. Chronic diseases and risk for depression in old age: a meta-analysis of published literature. Ageing Res Rev. (2010) 9:131–41. doi: 10.1016/j.arr.2009.05.005
48. Han, JH, Lee, HJ, Jung, J, and Park, EC. Effects of self-reported hearing or vision impairment on depressive symptoms: a population-based longitudinal study. Epidemiol Psychiatr Sci. (2019) 28:343–55. doi: 10.1017/S2045796018000045
49. Ho, VM, Arac, A, and Shieh, PB. Hearing and vision loss in an older man. JAMA Neurol. (2018) 75:1439–40. doi: 10.1001/jamaneurol.2018.1868
50. Huang, AR, Rebok, GW, Swenor, BK, Reed, N, Griswold, M, Zhu, X, et al. Concurrent hearing and vision impairment and 8-year memory decline in community-dwelling older adults. Alzheimers Dement. (2023) 19:2307–16. doi: 10.1002/alz.12887
51. Crews, JE, and Campbell, VA. Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Public Health. (2004) 94:823–9. doi: 10.2105/AJPH.94.5.823
52. Laird, E, Rasmussen, CL, Kenny, RA, and Herring, MP. Physical activity dose and depression in a cohort of older adults in the Irish longitudinal study on ageing. JAMA Netw Open. (2023) 6:e2322489. doi: 10.1001/jamanetworkopen.2023.22489
53. Read, JR, Sharpe, L, Modini, M, and Dear, BF. Multimorbidity and depression: a systematic review and meta-analysis. J Affect Disord. (2017) 221:36–46. doi: 10.1016/j.jad.2017.06.009
54. Cho, H, and Lee, H. Latent class analysis of health lifestyle among older adults living alone and associations with life satisfaction and depressive symptoms. J Affect Disord. (2024) 361:172–81. doi: 10.1016/j.jad.2024.05.162
55. O'Brien, E, Whitman, K, Buerke, M, Galfalvy, H, and Szanto, K. Life-satisfaction, engagement, mindfulness, flourishing, and social support: do they predict depression, suicide ideation, and history of suicide attempt in late life? Am J Geriatr Psychiatry. (2023) 31:415–24. doi: 10.1016/j.jagp.2022.12.192
Keywords: cataracts, depressive symptoms, older people, CLHLS, random forest
Citation: Niu T, Cao S, Wang X, Xian X, Luo C and Ma J (2025) Depressive symptoms and its influencing factors of older people with cataracts in China: a national cross-sectional survey. Front. Public Health. 13:1504275. doi: 10.3389/fpubh.2025.1504275
Edited by:
Anthony Vee Yee Alexander Chong, Monash University Malaysia, MalaysiaReviewed by:
Essam Mohamed Elmatbouly Saber, Benha University, EgyptQing Liu, Gansu Provincial Maternal and Child Health Hospital, China
Copyright © 2025 Niu, Cao, Wang, Xian, Luo and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunyang Luo, MjY2NTQ4OTA4OEBxcS5jb20=; Jingxi Ma, MTI0MTM3MjQ3QHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Tengfei Niu
Tengfei Niu Shiwei Cao
Shiwei Cao Xiaoyu Wang
Xiaoyu Wang Xiaobing Xian
Xiaobing Xian Chunyang Luo5*
Chunyang Luo5* Jingxi Ma
Jingxi Ma