- 1Department of Public Health and Healthcare, Marat Ospanov West Kazakhstan Medical University, Aktobe, Kazakhstan
- 2Department of Preventive Medicine, Poznan University of Medical Sciences, Poznan, Poland
- 3Department of Pharmacology, Poznan University of Medical Sciences, Poznan, Poland
- 4Marat Ospanov West Kazakhstan Medical University, Aktobe, Kazakhstan
- 5Social health insurance and public health department, JSC South Kazakhstan Medical Academy, Shymkent, Kazakhstan
- 6Department of Internal Diseases №1, Marat Ospanov West Kazakhstan Medical University, Aktobe, Kazakhstan
- 7Department of Mental Health, Chair of Psychiatry, Poznan University of Medical Sciences, Poznan, Poland
- 8Geriatrics Unit, Chair of Palliative Medicine, Poznan University of Medical Sciences, Poznan, Poland
- 9Department of Human Nutrition and Dietetics, Poznan University of Life Sciences, Poznan, Poland
- 10Centre for Health Services Studies, University of Kent, Canterbury, Kent, United Kingdom
- 11Department of Occupational Therapy, Poznan University of Medical Sciences, Poznan, Poland
Background: Studies about the needs of older individuals in Central Asia are very sparse. Thus, this study aimed to evaluate the needs of older adults in Kazakhstan with the EASYCare Standard 2010 (EC) questionnaire.
Methods: The study involved 524 participants aged 65 and older from various regions in Kazakhstan. Data were collected by trained research staff, and the participants’ needs were examined using median split with the three summarizing indexes of the EC system (Independence score, Risk of breakdown in care, and Risk of falls).
Results: Subjects with primary education had approximately double odds of scoring above the median compared to those with higher education in Independence score (p < 0.01) and Risk of breakdown in care (p < 0.01). Individuals with primary education also had 60% higher odds of scoring above the Risk of falls scale threshold, indicating a risk in this category (p < 0.05). For the Risk of falls scores, financial situation was also significant; individuals having not enough to make ends meet had 75% higher odds than the remaining ones (p < 0.01).
Conclusion: Our analysis highlights the importance of tailored interventions to address the unmet needs of the Kazakh population, particularly among those with lower education and those with financial concerns. The study also underscores the need for sustainable, comprehensive eldercare policies in Kazakhstan that account for the growing older population.
1 Introduction
The proportion of individuals aged 60 and over is increasing rapidly worldwide. A practical and adequate response to this demographic shift requires an accurate, personalized assessment of older individuals’ needs, which might help prevent the deterioration of their independence (1). All this has highlighted the importance of a multidisciplinary approach and also led to the development of instruments for a combined health and social needs assessment (2). One such tool is the EASYCare Standard 2010 (EC) system. Over the past two decades, it has been made available in languages from all WHO regions (3) and used to evaluate and identify the unmet needs of older individuals (4–6).
The EC system acts as a comprehensive instrument for older adults, addressing specific concerns and priorities related to their needs, health, and overall comfort (7, 8). This tool offers a straightforward and practical approach to assessing various aspects such as activities of daily living (ADL), instrumental activities of daily living (IADL), mental health, social interactions, and well-being.
Based on our literature review, research in Central Asia has been sparse to date, particularly in regard to the needs of older individuals. For example, a study performed on a representative sample of older individuals indicated that a strong family relationship and adherence to a traditional lifestyle were still preserved in Uzbekistan (9). In general, a strong cultural emphasis on respecting and caring for the older members of families was widely present. Older family members were typically held in high regard and treated by younger relatives with deference. This respect for older people is a traditional value that remains significant in Uzbek society, where their well-being and comfort are, as before, often prioritized within familial relationships. This cultural value is also upheld in Kazakhstani society.
Similarly to Uzbekistan, the population of Kazakhstan is still relatively young. In 2022, 8.0% of the population was aged 65 years and older, an increase from 6.7% in 2012. However, a parallel increase in the youngest age group (0–14 years of age) was also observed (25.4% in 2012 compared to 29.7% in 2022) (10). Still, according to current United Nations projections, by 2060, the population of older individuals in Kazakhstan is expected to more than double that of children under five and approach 30% of the working-age population (11). The demographic situation in Kazakhstan differs thus from those countries where the needs of older individuals are well characterized. Hence, the need patterns of older Kazakh citizens, shaped by the presence of relatively strong younger generations and culturally anchored care habits (12) may deviate from those characteristic of the Western world.
Available studies on aging in Kazakhstan focus on demographic trends (13) and quality of life (14). For the wider Central Asian region, two further publications discuss the welfare (15) and challenges faced by older adults (16). Data regarding the needs of the older population in Kazakhstan are available only partially and limited to certain aspects of caregiving and palliative care as well as its socio-economic needs (12, 17–19). Consequently, further studies are necessary to gain a comprehensive understanding of contemporary circumstances and requirements and identify the areas where more support is needed. We thus employed a multidimensional approach using the EC tool in the analysis of the needs of older people, which constitute an important factor in premises for the planning of sustainable eldercare for the future of Kazakhstani society. Beyond the methodological details, we emphasize the clinical and systemic implications of our study.
2 Materials and methods
This study was approved by the West Kazakhstan Marat Ospanov Medical University’s bioethical committee, Aktobe, Kazakhstan (October 14, 2020; № 8) and was funded by the Science Committee of the Ministry of Education and Science of the Republic of Kazakhstan (AP09562783).
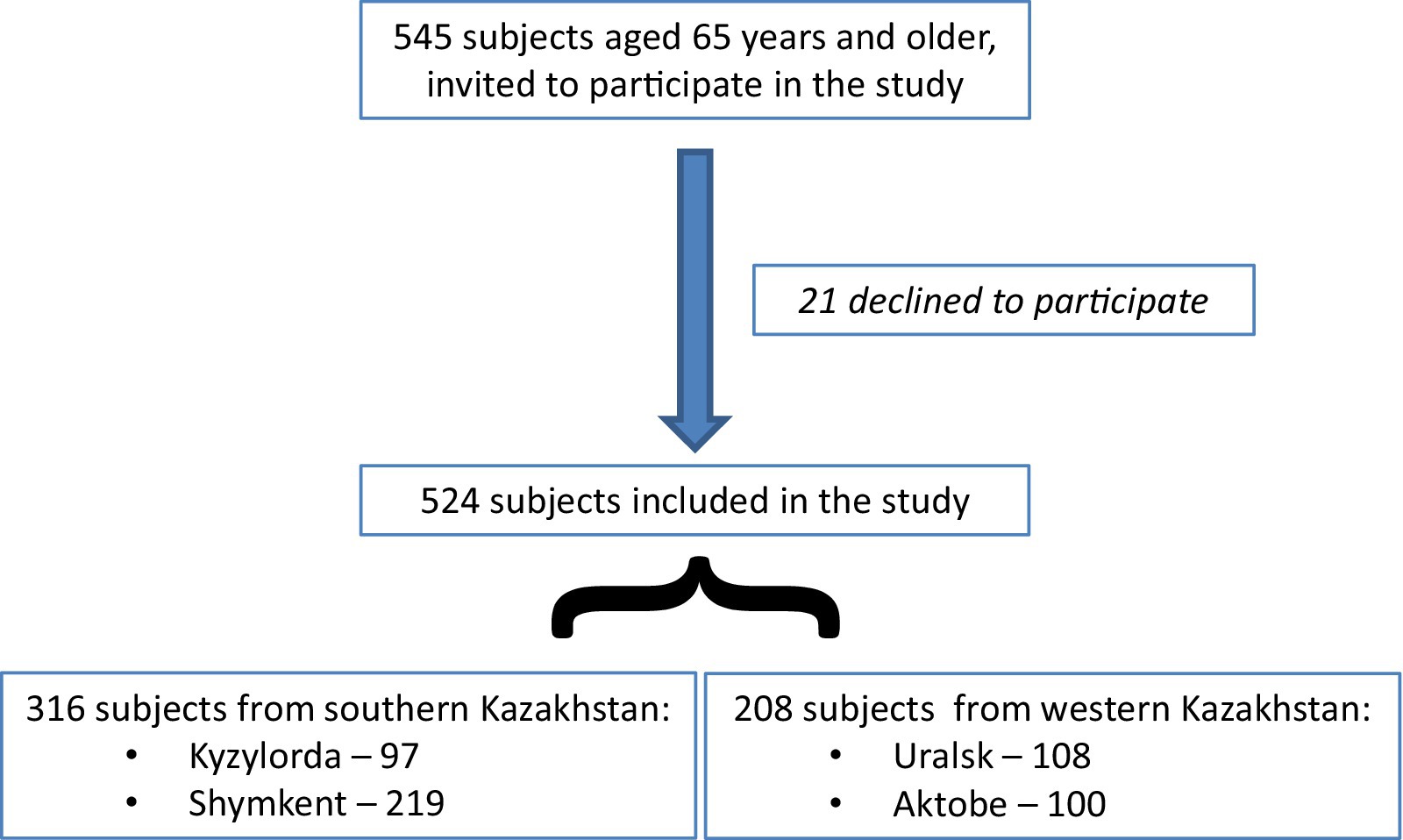
Data were collected by trained research staff (a total of 5 people who also served as support for clarification purposes when needed) during the COVID-19 pandemic in 2020 and 2021. The collection was performed with the help of general practitioners, social workers, and nurses, whose role was limited to the recruitment of older adults from the lists of patients at outpatient clinics (convenience sample). Only individuals with full verbal contact and no cognitive disorders were invited. Twenty-one people declined to participate, citing lack of time or fear of COVID-19 infection. No financial incentive was offered to recruited subjects.
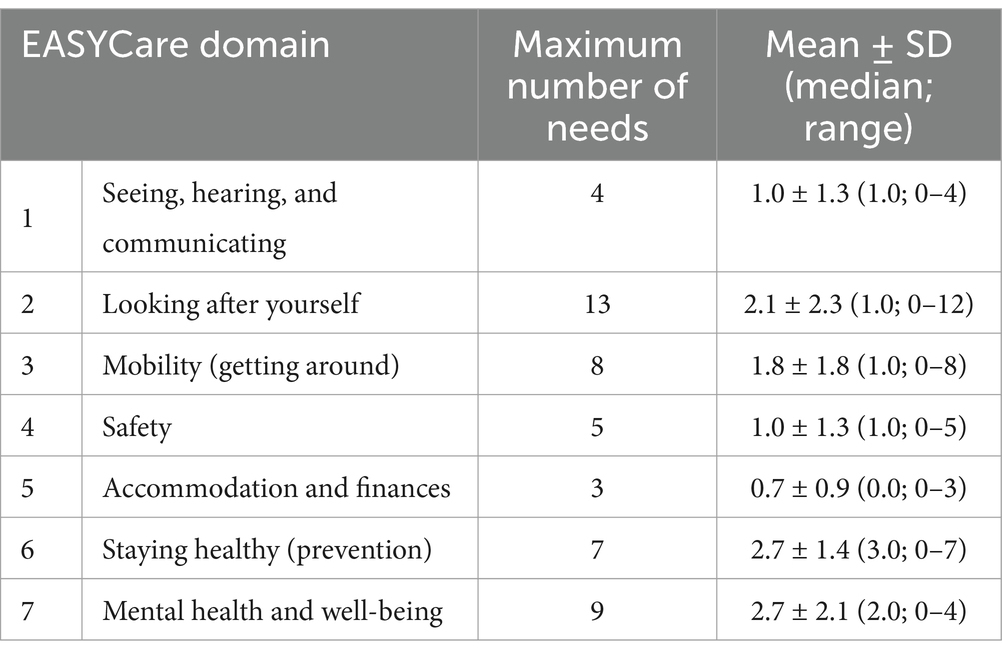
After participants consented by phone to participate, meetings were organized either at their homes or at outpatient clinics as convenient. Participants were informed about the study details and purpose, and written consents were obtained. The total number of participants was 524, with 97 from Kyzylorda, 219 from Shymkent (southern Kazakhstan), 108 from Uralsk (western Kazakhstan), and 100 from Aktobe (Figure 1). Data about their needs were collected using the EASYCare Standard 2010 system questionnaire (ECQ). The ECQ consists of 7 domains (49 questions) that assess the need for physical, mental, and social assistance: (1) seeing, hearing, and communicating; (2) looking after yourself; (3) getting around; (4) safety; (5) accommodation and finances; (6) staying healthy; (7) mental health and well-being.
Based on the results of the questionnaire, three summarizing indexes are calculated for each participant (20, 21):
• Independence score – describes a functional dependency of an individual with a score ranging between 0 and 100 points, where a lower score indicates less dependency,
• Risk of breakdown in care – reflects the threat of being hospitalized, with a score ranging from 0 to 12 points; a higher score indicates an increased risk of the necessity of hospitalization,
• Risk of falls – with a score range from 0 to 8, 3 or more points indicate an increased danger of falling.
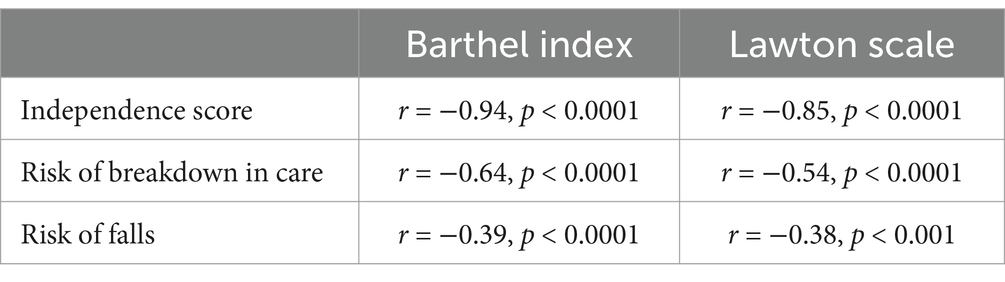
The details on calculating the indexes have already been published (6). As there existed no Kazakh version of the ECQ, a translation from English was performed. Thereafter, the psychometric properties of the Kazakh version were evaluated in the first 100 individuals of the study. Their needs were assessed using the translated ECQ twice, 10–14 days apart. Additionally, their functional capacity in basic and instrumental activities of daily living was analyzed using gold-standard instruments: the independence in basic activities of daily living (ADL) was assessed using the Barthel Index (22) and instrumental activities of daily living (IADL) – with the Lawton Scale (23). The Barthel Index evaluates activities such as feeding, bathing, grooming, dressing, and bowel control – 10 activities in total, with final scores ranging from 0 to 100, where a lower score means greater dependency (24). The Lawton Scale assesses such activities as using the telephone, doing laundry and dressing, shopping and running errands, transportation, meal preparation, medication management, housekeeping activities, and managing finances. IADL scores range between 0 and 8 points, where lower scores indicate greater dependency.
2.1 Statistical analysis
STATISTICA 13.2 software (TIBCO Software, Poland) was used to perform the statistical analysis. Normality in the data distribution was examined using the Shapiro–Wilk test. Descriptive results are presented as means and standard deviations (SD), and due to the lack of normality for some data, also as medians and ranges. Participants were compared with the χ2 test in two age groups (65–74 and 75+) by describing socio-demographic characteristics. Since we only had eight subjects aged 85 years or older, this analysis practically reflects decade cohorts. The χ2 test is used to compare categorical variables.
Once calculated, the three summarizing indexes of the EC questionnaire were also analyzed with the χ2 test. A multiple regression model (logistic regression) was used to assess simultaneous interdependence between many variables, specifying the odds ratio and the confidence interval with a confidence limit of 95%. To divide participants according to the score in the individual indexes, a median split (splitting a continuous variable into high and low values) was used (25). This analysis was performed by comparing the subjects with the Independence score and the score of the Risk of breakdown in care results above the median to those at or below the median, and for the score of Risk of falls – those with increased risk to those without. All studied variables were included in multiple linear regression analysis.
Agreement between the two assessment scores on the individual items of the ECQ was checked using weighted Cohen’s kappa statistic, which is a measure of the agreement between two ordinary scaled samples and is used to compare two measurements. Its interpretation is given by Landis and Koch (26).
Cronbach’s alpha coefficient was calculated to assess internal consistency (by comparing the amount of shared variance among the individual items of a tool to the amount of overall variance), and the test–retest results were analyzed using the Wilcoxon signed-rank test (since there were two matched samples). Content validity was checked against reference instruments (ADL and IADL) with the Spearman correlation coefficient (which is a non-parametric measure of correlation between the rankings of two variables). For the interpretation of Cronbach’s alpha results, the George and Mallery rating was used (27). A p-value of <0.05 was considered statistically significant.
3 Results
3.1 Needs assessment
The characteristics of the study sample are presented in Table 1. It consisted of 524 individuals with a mean age of 70.3 ± 5.3 years (median 69, range 65–87), including 96 subjects aged 75 years and over (18.3%). Within the entire group, 239 were males (45.6%). Notably, almost half of the studied subjects were living with extended family (42.8%), and less than one out of four (22.7%) were living alone. Females were more frequently single (p < 0.001) and were more likely to live alone (p < 0.01) compared to males.
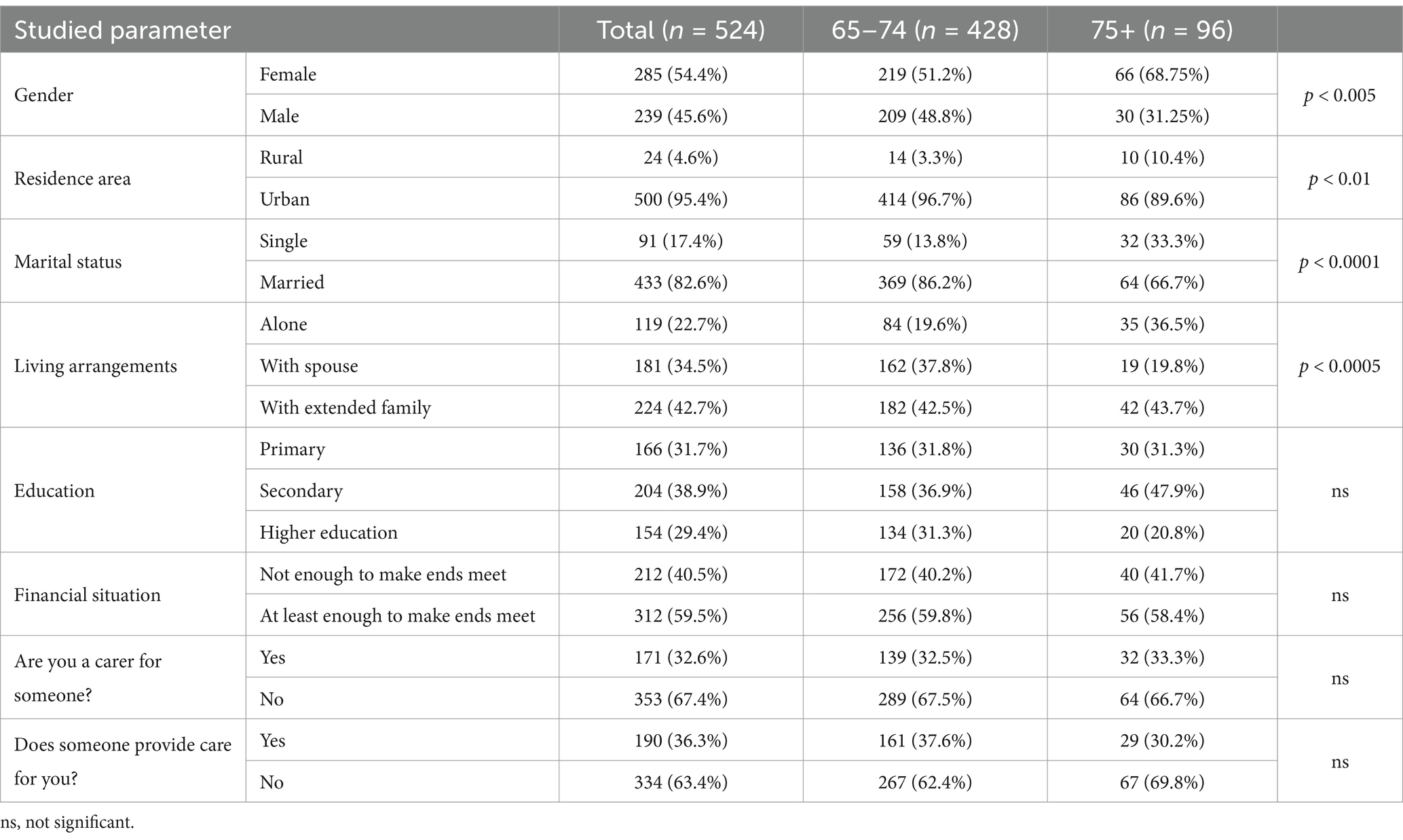
Table 1. Characteristics of studied subjects including age and gender (statistical analysis comparing younger and older subjects).
Based on the ECQ, the average number of needs reported by the participants was 12.1 ± 7.2 (median 11, maximum 36). Among the study participants, there was only one person who did not indicate any needs – a 70-year-old woman, single, living with an extended family.
The majority of participants reported needs in domain 6 (Staying healthy) (n = 496, 94.7%, Figure 2), most frequently in response to the question “Do you take regular exercise?” – 337 individuals (64.3%) answered “No” to this question. Additionally, more women than men had concerns about their weight (156–54.7% vs. 100–41.8%; p < 0.01). In this domain, needs were also frequently reported for the question “Have you checked with your doctor that you are up to date with your vaccinations?” (218; 41.6%; comparably frequently in both genders; 102–35.8% vs. 116–48.5%).
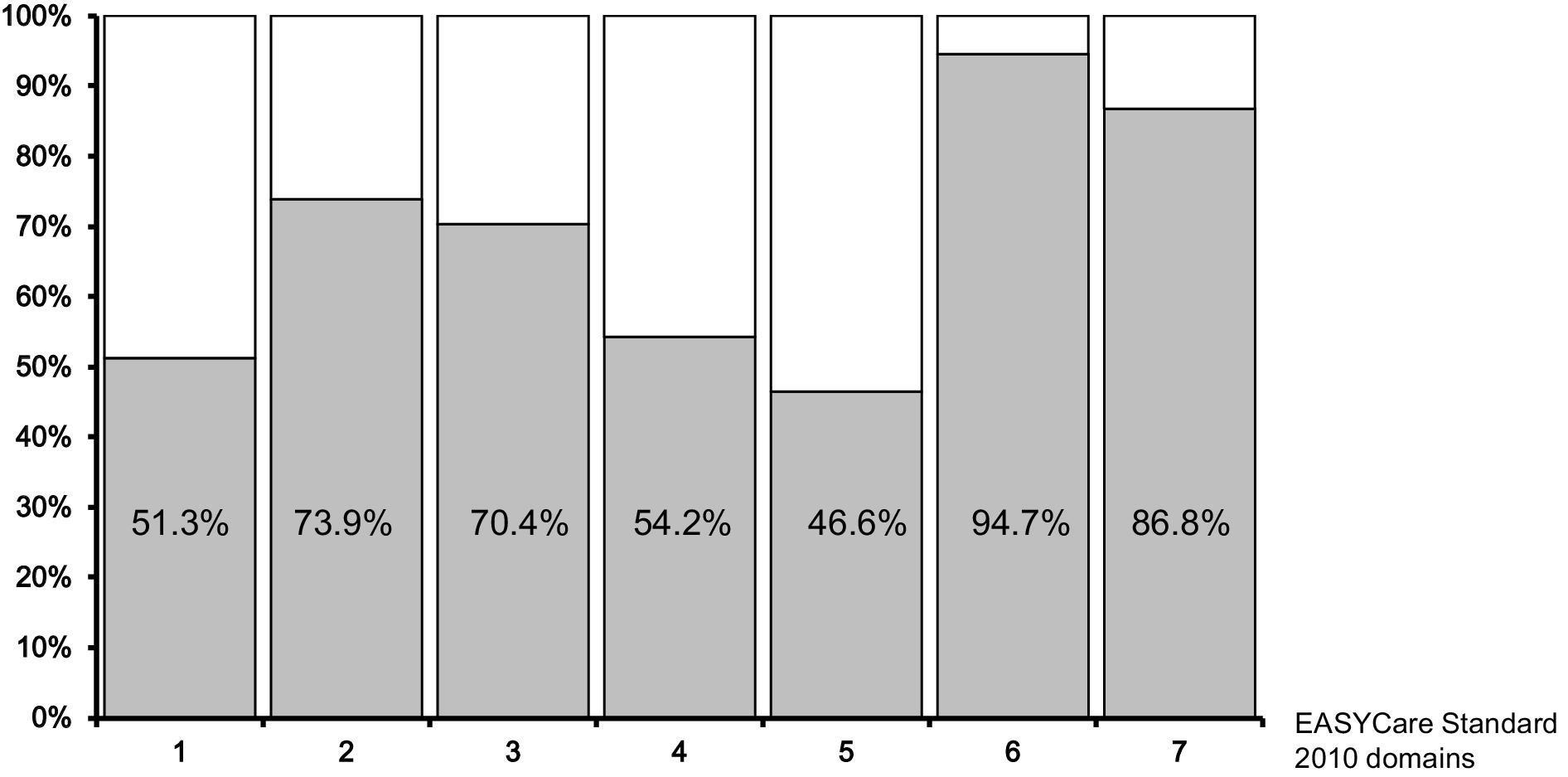
Figure 2. Percentages of participants with needs in the individual domains of the EASYCare 2010 questionnaire.
In the second health-related area (domain 7, Mental health and well-being), 455 individuals (86.8%) reported needs. No differences in the frequency of indicated needs were found between men and women in this domain. For the majority of items in this domain, needs were reported by more than every third person: 212 subjects (40.5%) declared they were unable to pursue leisure interests, hobbies, work, and learning activities important to them, 207 participants (39.5%) complained about having trouble with sleep in the last month, 199 subjects (38.0%) reported feeling lonely, 190 (36.3%) indicated suffering from any recent loss or bereavement, 181 individuals (34.5%) had much bodily pain in the past month (114–40.0% vs. 67–28.0%; p < 0.01), and 179 (34.2%) reported concerns about memory loss or forgetfulness.
In domain 1 (Seeing, hearing, and communicating), needs were reported by 269 subjects (51.3%); 168 individuals had vision problems (32.1%), 121 had hearing problems (23.1%), and 164 (31.3%) were unable to use the telephone independently. In domain 2 (Looking after yourself), needs were indicated by 387 individuals (73.9%) – almost every third person had problems with their mouth or teeth (151–28.8%), followed by housework (139–26.5%), taking their own medicine (130–24.8%), and preparing meals (117–22.3%).
In domain 3 (Getting around), 369 individuals (70.4%) reported needs, including 141 (26.9%) who had issues getting to public services (66–23.2% vs. 74–31.0%; p < 0.05).
In domain 4 (Safety), 284 subjects (54.2%) reported needs, with over a quarter indicating they lacked someone who would be able to help in case of illness or emergency (151–28.8%). In domain 5 (Accommodation and finance), 244 individuals (46.6%) reported needs, with 213 (40.6%) expressing a desire for advice about financial allowances or benefits.
3.2 Summarizing indexes
The average Independence score was 10.9 ± 12.6 (median 7; range 0–75). Only 12 individuals scored above 50, which is more than half of the possible points on this scale. As many as 118 people had a score of 0.
The mean Risk of breakdown in care index result was 2.8 ± 2.3 (median 2, range: 0–10). On this scale, 41 individuals scored above 6, which is more than 50% of the possible points; 74 subjects had a score of 0 points.
The average Risk of falls index value was 1.9 ± 1.7 (median 2, range: 0–8). A score of 3 or more, indicating an increased risk of falls, was found in 179 individuals (34.2%).
A binary logistic regression analysis of determinants for the number of needs above the median for the first two summary indexes showed their relationship with education level. Participants with primary education had approximately double odds of scoring above the median compared to those with higher education in Independence score (p < 0.01) and Risk of breakdown in care (p < 0.01). Individuals with primary education also had 60% higher odds of scoring above the Risk of falls scale threshold, indicating a risk in this category (p < 0.05). For the Risk of falls scores, financial situation was also significant; individuals having not enough to make ends meet had 75% higher odds than the remaining ones (p < 0.01). Tables 2–4 present the multivariable analysis of determinants of needs in the studied group. Table 5 contains the results of descriptive statistics for needs in the individual ECQ domains.
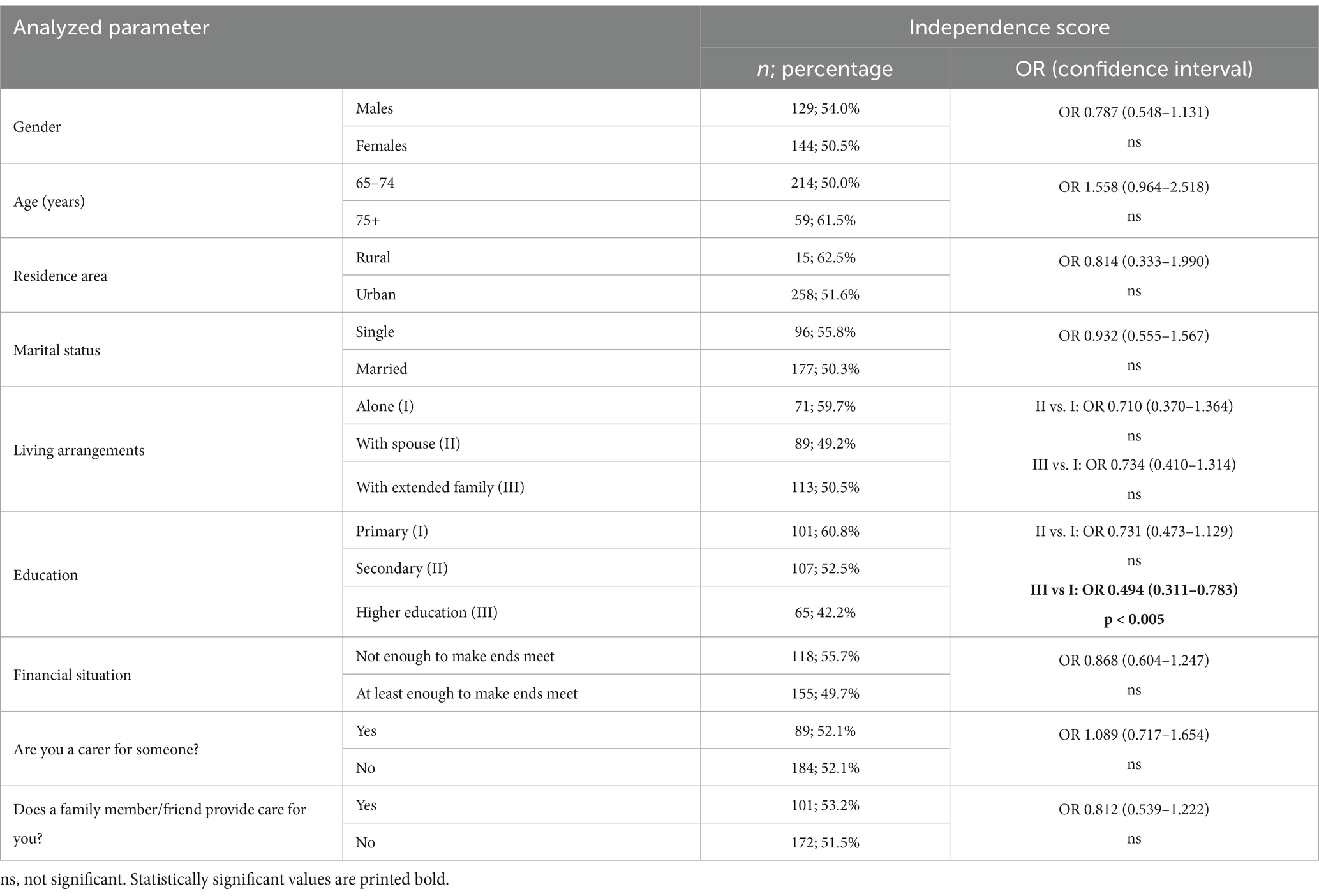
Table 2. Multivariable analysis of determinants for Independence score; odds ratios (OR) and 95% confidence intervals are presented.
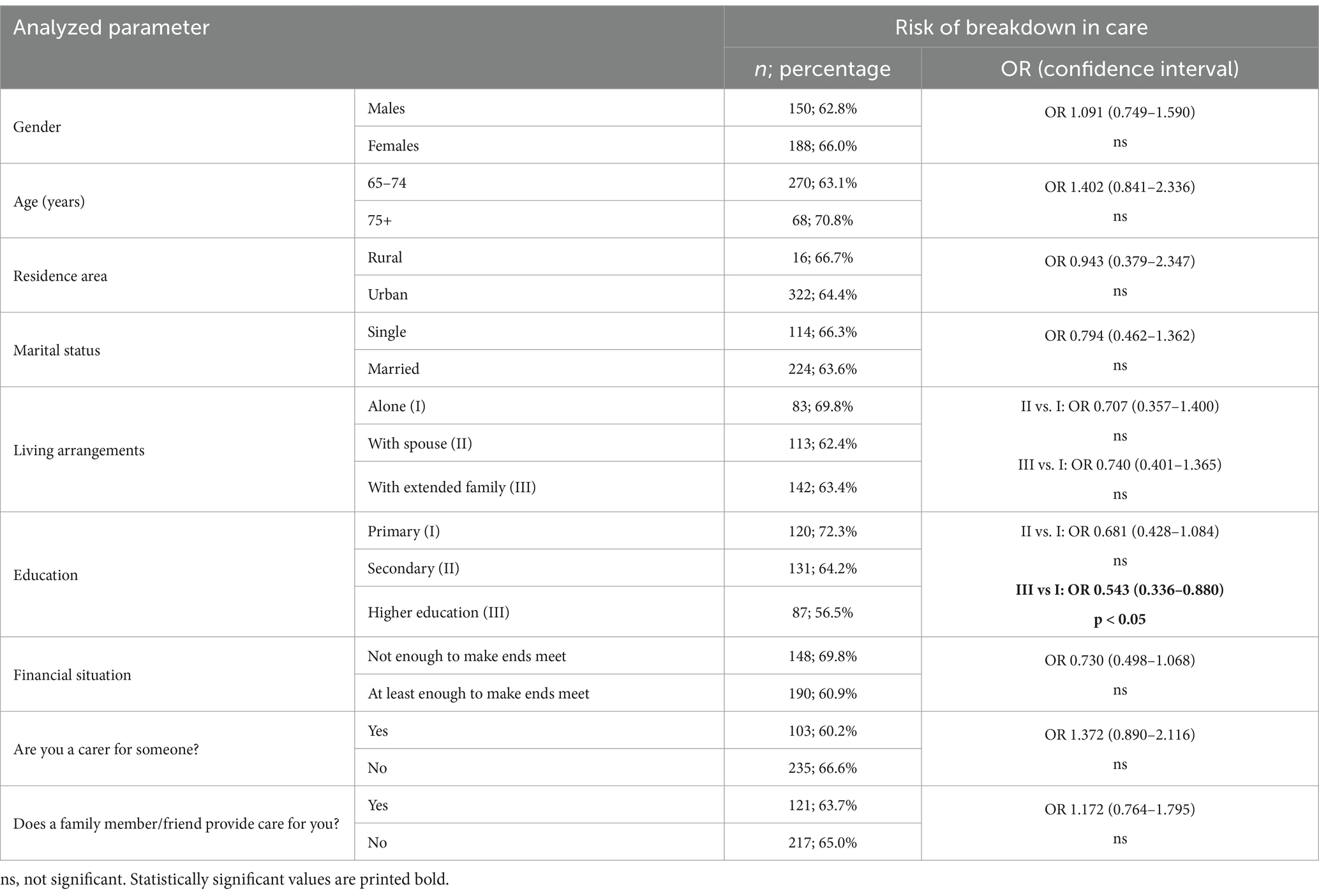
Table 3. Multivariable analysis of determinants for the Risk of breakdown in care; odds ratios (OR) and 95% confidence intervals are presented.
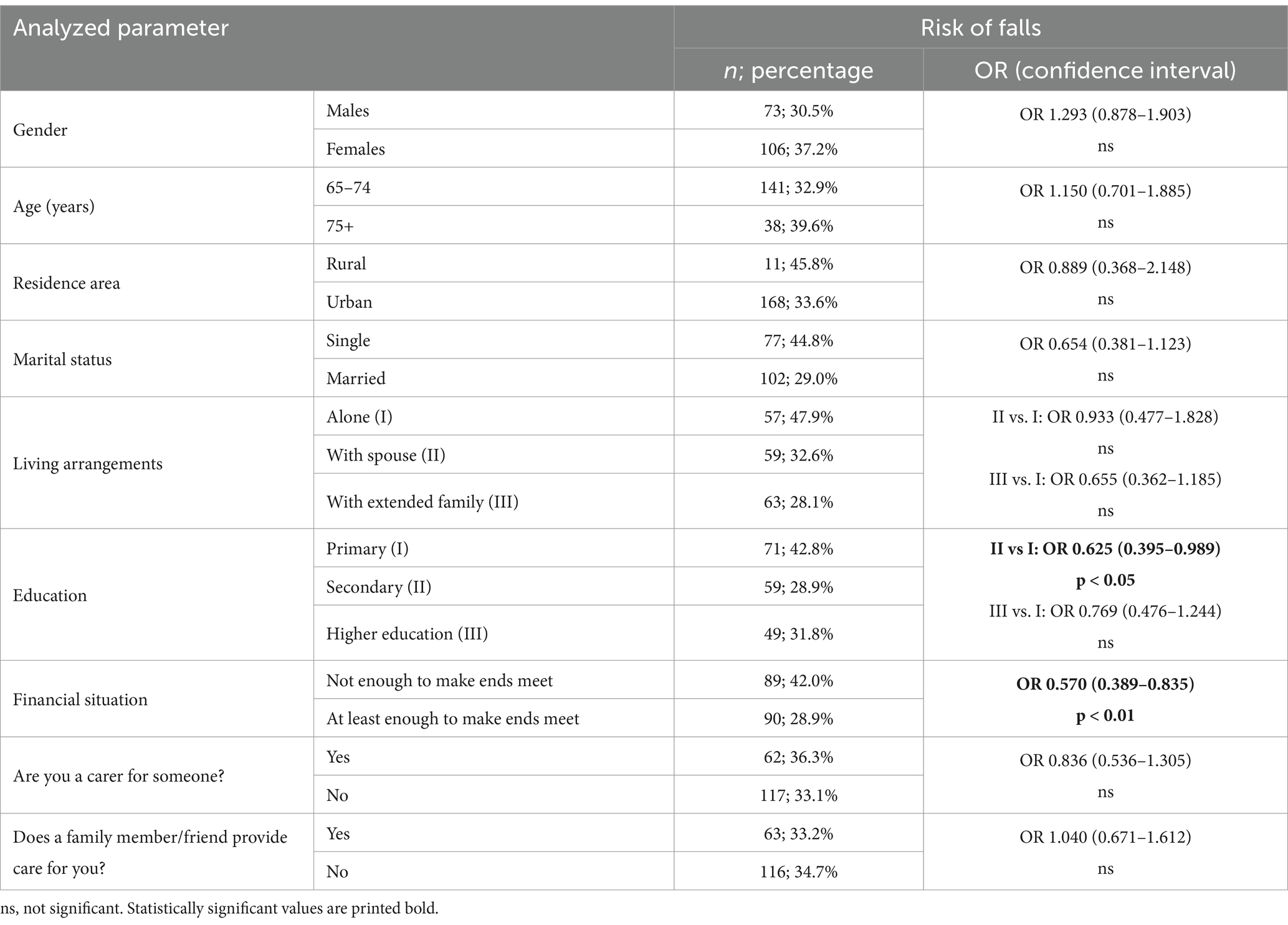
Table 4. Multivariable analysis of determinants of Risk of falls; odds ratios (OR) and 95% confidence intervals are presented.
3.3 The validation study
The mean age of study subjects who completed the ECQ twice (n = 100) was 70.7 ± 4.6 years (median: 70, range: 65–85). Among them, 38 were males. The validation group did not differ from the general study sample in terms of gender, residence area, marital status, financial situation, living arrangements, being a carer for someone or being a care recipient; differences were present for education only (due to the fractions of primary and higher education subgroups - 14.0% vs. 31.7 and 44.0% vs. 29.4%, respectively). The Cronbach’s alpha coefficient for the whole ECQ was 0.83.
No significant differences were found in the Independence score, Risk of breakdown in care, and Risk of falls between the two assessments. Cohen’s kappa coefficient across all domains ranged between 0.81 and 0.95, showing almost perfect agreement between all scale domains (Table 6).
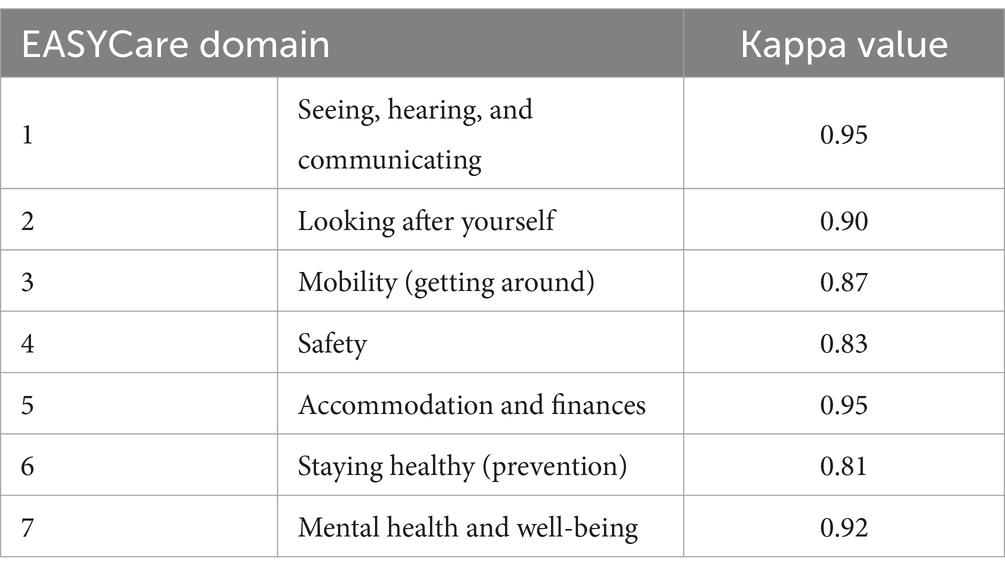
Table 6. Weighted Cohen’s kappa values of the validation study for two assessments in all domains of the questionnaire.
The mean Barthel Index of studied subjects was 94.0 ± 10.4 (median 100; range: 45–100), and the Lawton scale–7.5 ± 1.2 (median 8, range 2–8). Independence score and Risk of breakdown in care showed a good correlation with the scores of both the Barthel Index and the Lawton scale, which are gold-standard instruments for the assessment of functional independence (Table 7). For Risk of falls, moderate correlation was found.
4 Discussion
We analyzed the care needs of older adults in Kazakhstan. As far as we know, this is the first study on this topic in the whole of Central Asia. All countries in this region have a similar history – they gained independence from the Soviet Union at the end of the 20th century and then undertook substantial health system reforms (28). They also share a crucial role of adherence to traditional lifestyles and strong family bonds (29), and their populations are relatively young (28). Therefore, similarities in needs and ways of their satisfaction can be expected.
Due to the lack of a standardized tool in the Kazakh language, we translated the English ECQ and validated the resulting tool. We have shown that the Kazakh version of ECQ has good to excellent psychometric properties and, therefore, can be used to assess the needs of older people.
According to our analyses, participants frequently reported needs in health-related domains (6—Staying healthy and 7—Mental health and well-being). Our previous studies on the Polish population have similarly highlighted a significant number of needs in these areas (30), which was also shown by a recent study from South Korea (31). Importantly, while the needs of older people related to healthcare are universal, there are culturally specific differences in the ways of their satisfaction (due to such factors as the presence of family support, healthcare practices or social activity patterns) (32, 33). The high prevalence of needs related to lifestyle factors (like physical activity or concerns about weight) is characteristic of other regions of the world as well (34–36). It is also noteworthy that there is a substantial need for information about vaccinations and financial support. This creates a coherent picture with necessary changes in lifestyle intertwined with the need to provide crucial information.
One-third of the respondents reported experiencing pain. The prevalence of chronic pain in older people varies greatly depending on the population studied and is expressed differently in various age subgroups (37–41). Novel approaches to pain management involving the principles of person-centered care are thus welcome (42, 43).
A substantial number of our respondents indicated that they had nobody who would be able to help them in case of illness or emergency. This is remarkable given the emphasis on the traditional family model in Kazakhstan, where nearly half of the respondents lived with extended family. This finding may, however, be influenced by the timing of the study (during the COVID-19 pandemic), as one-third of the respondents also reported suffering from recent loss or bereavement.
It is imperative to note that the ECQ inherently addresses unmet needs. Therefore, it draws attention to people with vision or hearing disorders who, despite potential corrective measures, still report difficulties. Importantly, this helps identify areas where further support is necessary. Despite a high number of subjects reporting needs, similarly to what we have previously shown for the Polish population (30), the summarizing indexes were low, indicating good functional capacity among the study participants. One may thus expect that interventions tailored for this target group will be effective. In this study, lower education was the most important determinant of poorer scores across all indexes. Analogous findings were observed in another analysis of the Polish population using the same needs assessment tool (44). In this context, a recent publication on data characterizing Kazakhstan notably stresses that, in order to support health-promoting behaviors, measures are being planned to increase the health literacy of the population (45).
In a population study from Kosovo that used the ECQ, gender has been an important determinant of the summarizing indexes (46). However, it should be noted that women differed significantly from men. Many of them had no education, and this may reflect the specific characteristics of the older population in Kosovo during the study period, almost 15 years ago.
In our investigation, a worse financial situation increased the risk of falls by the participants. This is worth noting because this factor was also shown to be significant in the earlier-mentioned paper from Kosovo (46). In our study, living alone was not observed as a significant factor for increased risk of falling. Still, living alone, particularly in an urban area, is often considered an important risk factor for falls (47, 48).
Our research has some limitations. Despite the large study group, the sample was not representative of the whole Kazakh population. The vast majority of participants lived in large cities, and there are known regional disparities in access to healthcare in Kazakhstan (49). Additionally, due to historical factors, part of the population in Kazakhstan is Russian-speaking [e.g., in West Kazakhstan, about 20%, (49)]. To generalize the results to the entire population, it is necessary to conduct studies in this demographic as well. The use of convenience sampling also means that the results reflect the needs of older people in contact with medical services rather than the general population. Furthermore, since the study is cross-sectional, it is not possible to discuss causal relationships.
A strong point of our study is addressing the needs of older adults in Central Asia, a region that is still relatively young and has strong family ties but for which demographic aging projections are similar to other regions of the world. This necessitates preparing the healthcare system; yet, among the identified seven strategic priorities to improve the efficiency and effectiveness of the healthcare system in Kazakhstan (45), none are related to aging and demographic challenges.
In an effort to establish a viable approach to problems related to aging, smart homes and Internet of Things (IoT) solutions have been recently taken into consideration in Kazakhstan (50). While the use of new technologies in sustainable geriatric care has been discussed in various contexts (51–54), it is imperative to implement them in a properly prepared way. This includes studying the needs and requirements of future users and reflecting them in the design process (55–57). The EC system can be a solid base for such an approach.
Our analysis is also meant to be a voice in the discussion on addressing the Sustainable Development Goals in care for older adults, which, so far, seems to insufficiently consider the differences in needs of various age groups across contemporary societies (58). Comprehensive assessment of the needs of older people requires dedicated tools, such as the EC system, which should be available in local languages to ensure a proper understanding of the questions posed and take into account the local context. The importance of cross-cultural adaptation is stressed in various scenarios (59, 60).
5 Conclusion
We showed that the Kazakh version of the ECQ demonstrated good to excellent psychometric properties, indicating its reliability and validity for assessing the needs of older people in Kazakhstan. The study found a significant number of unmet needs among older adults in Kazakhstan, particularly in areas related to health, safety, and activities of daily living. Socio-economic factors, including education level and financial situation, were significant determinants of the needs and risks among older adults: those with lower education and those with poorer financial status were particularly vulnerable to higher dependency and greater health risks. The findings suggest that tailored interventions are necessary to address the specific needs of older adults in Kazakhstan, particularly for those at higher risk of unmet needs due to lower education levels, worse financial situation, or having limited access to social and health support. The study also underscores the need for sustainable, comprehensive eldercare policies in Kazakhstan that account for the growing older population.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the bioethical committee of the West Kazakhstan Marat Ospanov Medical University’s, Aktobe, Kazakhstan (October 14, 2020; Protocol № 8). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KK: Conceptualization, Investigation, Writing – review & editing, Validation. LY: Investigation, Writing – review & editing, Methodology, Validation. DT: Writing – review & editing, Methodology. MD: Methodology, Writing – review & editing. GSu: Investigation, Writing – review & editing. GSa: Investigation, Writing – review & editing. YB: Investigation, Writing – review & editing. PA: Investigation, Writing – review & editing. AS: Data curation, Writing – review & editing. KW-T: Conceptualization, Data curation, Formal analysis, Methodology, Writing – review & editing. IP: Formal analysis, Writing – review & editing. ST: Conceptualization, Data curation, Methodology, Supervision, Validation, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was funded by the Science Committee of the Ministry of Education and Science of the Republic of Kazakhstan (AP09562783).
Conflict of interest
The EASYCare tool and all its features are the copyright of the EASYCare Foundation Ltd which is a not-for-profit company limited by guarantee. IP is a Director. The EASYCare Foundation licenses use of the tool for research purposes without fees to researchers with no restriction on academic freedoms to publish their findings.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American Geriatrics Society Expert Panel on Person-Centered Care. Person-centered care: a definition and essential elements. J Am Geriatr Soc. (2016) 64:15–8. doi: 10.1111/jgs.13866
2. Philp, I. Can a medical and social assessment be combined? J R Soc Med. (1997) 90:11–3. doi: 10.1177/014107689709032S04
3. Philip, KE, Alizad, V, Oates, A, Donkin, DB, Pitsillides, C, Syddall, SP, et al. Development of EASY-care, for brief standardized assessment of the health and care needs of older people; with latest information about cross-national acceptability. J Am Med Dir Assoc. (2014) 15:42–6. doi: 10.1016/j.jamda.2013.09.007
4. Brandao, MP, Martins, L, Philp, I, and Cardoso, MF. Reliability and validity of the EASYCare-2010 standard to assess elderly people in Portuguese primary health care. Aten Primaria. (2017) 49:576–85. doi: 10.1016/j.aprim.2016.11.016
5. Pınar, R, Ergün, A, Erol, S, Kurtuluş, Z, Gür, K, Sert, H, et al. The adaptation of the EASY-care standard assessment instrument into Turkish and evaluation of psychometric properties among Turkish older people. Prevention. (2015) 49:53.
6. Tobis, S, Jaracz, K, Talarska, D, Kropinska, S, Zasadzka, E, Pawlaczyk, M, et al. Validity of the EASYCare standard 2010 assessment instrument for self-assessment of health, independence, and well-being of older people living at home in Poland. Eur J Ageing. (2018) 15:101–8. doi: 10.1007/s10433-017-0422-7
7. Olde-Rikkert, MG, Long, JF, and Philp, I. Development and evidence base of a new efficient assessment instrument for international use by nurses in community settings with older people. Int J Nurs Stud. (2013) 50:1180–3. doi: 10.1016/j.ijnurstu.2012.08.007
8. Philp, I. EASY-care: a systematic approach to the assessment of older people. Geriatr Med. (2000) 30:15–9.
9. Pulatova, G, Harun-Or-Rashid, M, Yoshida, Y, and Sakamoto, J. Elderly health and its correlations among Uzbek population. Nagoya J Med Sci. (2012) 74:71–82.
11. United Nations. Population division-data portal (2024). Available at: https://population.un.org/dataportal/data/indicators/46,70/locations/398/start/2010/end/2070/table/pivotbylocation?df=0ef1d582-387a-43d9-8ae7-20225d13ea98
12. Zhylkybekova, A, Turlayev, A, Grjibovski, AM, and Koshmaganbetova, GK. Measures to support informal care for the older adults in Kazakhstan: a review of the current status. Front Public Health. (2023) 11:1247684. doi: 10.3389/fpubh.2023.1247684
13. Sidorenko, AV, Eshmanova, AK, and Abikulova, AK. Aging of the population in Kazakhstan. 1. Problems and opportunities. Adv Gerontol. (2018) 8:12–21. doi: 10.1134/S2079057018010113
14. Abdina, A, and Uyzbayeva, A. Philosophy of well-being: quality of life and inclusion of the elderly population of Kazakhstan in the era of digitalization. Bull LN LN Gumilyov Eurasian Natl University. (2024) 148:164–77. doi: 10.32523/2616-7255-2024-148-3-164-177
15. Makhanov, K. A brief review of elderly welfare in. Central Asia: Eurasian Research Institute (2022).
17. Zhylkybekova, A, Grjibovski, AM, Glushkova, N, and Koshmaganbetova, GK. Exploring the burden and support needs of informal caregivers for the older adults in Kazakhstan: a mixed-methods study protocol. Front Public Health. (2023) 11:1248104. doi: 10.3389/fpubh.2023.1248104
18. Kunirova, G, and Shakenova, A. Palliative Care in Kazakhstan. J Pain Symptom Manag. (2018) 55:S36–40. doi: 10.1016/j.jpainsymman.2017.03.028
19. Alimbekova, GT, Shabdenova, AB, Moldakulova, G, and Zshusupova, AS. Оценка социально-экономического положения и потребностей пожилых людей в Казахстане (результаты комплексного национального социологического исследования) [Assessment of the Socio-Economic Situation and Needs of Elderly People in Kazakhstan (Results of a Comprehensive National Sociological Survey)] (2020). Available at: https://kazakhstan.unfpa.org/sites/default/files/pub-pdf/rus_otchet_ciom_itogi_socilog_obsledovaniya_polozheniya_pozhilyh_lyudey_v_kazahstane_2020_rus_3.pdf. (Accessed November 4, 2024).
20. Craig, C, Chadborn, N, Sands, G, Tuomainen, H, and Gladman, J. Systematic review of EASY-care needs assessment for community-dwelling older people. Age Ageing. (2015) 44:559–65. doi: 10.1093/ageing/afv050
21. Jotheeswaran, AT, Dias, A, Philp, I, Patel, V, and Prince, M. Calibrating EASY-care independence scale to improve accuracy. Age Ageing. (2016) 45:890–3. doi: 10.1093/ageing/afw106
22. Mahoney, FI, and Barthel, DW. Functional evaluation: the Barthel index. Md State Med J. (1965) 14:61–5.
23. Lawton, MP, and Brody, EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. (1969) 9:179–86.
24. Chindaprasirt, J, Sawanyawisuth, K, Chattakul, P, Limpawattana, P, Tiamkao, S, Aountri, P, et al. Age predicts functional outcome in acute stroke patients with rt-PA treatment. ISRN Neurol. (2013) 2013:710681:1–4. doi: 10.1155/2013/710681
25. DeCoster, J, Gallucci, M, and Iselin, A-MR. Best practices for using median splits, artificial categorization, and their continuous alternatives. J Exp Psychopathol. (2011) 2:197–209. doi: 10.5127/jep.008310
26. Landis, JR, and Koch, GG. The measurement of observer agreement for categorical data. Biometrics. (1977) 33:159–74. doi: 10.2307/2529310
27. George, D. SPSS for windows step by step: A simple study guide and reference, 17.0 update Pearson Education India. 10th Ed. Pearson, Boston (2010).
28. Rechel, B, Sydykova, A, Moldoisaeva, S, Sodiqova, D, Spatayev, Y, Ahmedov, M, et al. Primary care reforms in Central Asia-on the path to universal health coverage? Health Policy Open. (2023) 5:100110. doi: 10.1016/j.hpopen.2023.100110
29. Roche, S. The family in Central Asia: New perspectives Walter de Gruyter Gmb H & Co KG: Berlin. (2020).
30. Ryszewska-Łabędzka, D, Tobis, S, Kropińska, S, Wieczorowska-Tobis, K, and Talarska, D. The Association of Self-Esteem with the level of independent functioning and the primary demographic factors in persons over 60 years of age. Int J Environ Res Public Health. (2022) 19:1–12. doi: 10.3390/ijerph19041996
31. Chung, W. Deconstructing subjective unmet healthcare needs: a south Korean case study with policy implications. Front Public Health. (2024) 12:1385951. doi: 10.3389/fpubh.2024.1385951
32. Lor, M, Crooks, N, and Tluczek, A. A proposed model of person-, family-, and culture-centered nursing care. Nurs Outlook. (2016) 64:352–66. doi: 10.1016/j.outlook.2016.02.006
33. Sokolovsky, J. The cultural context of aging: Worldwide perspectives Bloomsbury Publishing USA: Santa Barbara, California (2020).
34. Herr, M, Arvieu, JJ, Aegerter, P, Robine, JM, and Ankri, J. Unmet health care needs of older people: prevalence and predictors in a French cross-sectional survey. Eur J Pub Health. (2014) 24:808–13. doi: 10.1093/eurpub/ckt179
35. Shaikh, RA, Siahpush, M, Singh, GK, and Tibbits, M. Socioeconomic status, smoking, alcohol use, physical activity, and dietary behavior as determinants of obesity and body mass index in the United States: findings from the National Health Interview Survey. Int J MCH AIDS. (2015) 4:22–34. doi: 10.21106/ijma.53
36. Fabbian, F, Rodriguez-Munoz, PM, Lopez-Carrasco, JC, Cappadona, R, Rodriguez-Borrego, MA, and Lopez-Soto, PJ. Google trends on obesity, smoking and alcoholism: global and country-specific interest. Healthcare (Basel). (2021) 9:190. doi: 10.3390/healthcare9020190
37. Kozak-Szkopek, E, Broczek, K, Slusarczyk, P, Wieczorowska-Tobis, K, Klich-Raczka, A, Szybalska, A, et al. Prevalence of chronic pain in the elderly polish population - results of the pol senior study. Arch Med Sci. (2017) 13:1197–206. doi: 10.5114/aoms.2015.55270
38. Mantyselka, P, Kumpusalo, E, Ahonen, R, Kumpusalo, A, Kauhanen, J, Viinamaki, H, et al. Pain as a reason to visit the doctor: a study in Finnish primary health care. Pain. (2001) 89:175–80. doi: 10.1016/S0304-3959(00)00361-4
39. Ai, Z, Tang, C, Peng, P, Wen, X, and Tang, S. Prevalence and influencing factors of chronic pain in middle-aged and older adults in China: results of a nationally representative survey. Front Public Health. (2023) 11:1110216. doi: 10.3389/fpubh.2023.1110216
40. Goyal, AK, and Mohanty, SK. Association of pain and quality of life among middle-aged and older adults of India. BMC Geriatr. (2022) 22:939. doi: 10.1186/s12877-022-03480-y
41. Radojcic, MR, Perera, RS, Hart, DJ, Spector, TD, and Arden, NK. Prevalence, incidence, and re-occurrence risk of musculoskeletal pain in older adults in the United Kingdom: a population-based study. Front Pain Res. (2023) 4:1197810. doi: 10.3389/fpain.2023.1197810
42. Rejula, V, Anitha, J, Belfin, RV, and Peter, JD. Chronic pain treatment and digital health era-an opinion. Front Public Health. (2021) 9:779328. doi: 10.3389/fpubh.2021.779328
43. Kowalski, G, Leppert, W, Adamski, M, Szkutnik-Fiedler, D, Baczyk, E, Domagalska, M, et al. Rectal enema of bupivacaine in cancer patients with tenesmus pain – case series. J Pain Res. (2019) 12:1847–54. doi: 10.2147/JPR.S192308
44. Talarska, D, Pacholska, R, Strugala, M, and Wieczorowska-Tobis, K. Functional assessment of the elderly with the use of EASY-care standard 2010 and comprehensive geriatric assessment. Scand J Caring Sci. (2016) 30:419–26. doi: 10.1111/scs.12241
45. Gulis, G, Aringazina, A, Sangilbayeva, Z, Zhan, K, de Leeuw, E, and Allegrante, JP. Population health status of the Republic of Kazakhstan: trends and implications for public health policy. Int J Environ Res Public Health. (2021) 18:12235. doi: 10.3390/ijerph182212235
46. Jerliu, N, Burazeri, G, Toci, E, Philp, I, Czabanowska, K, Ramadani, N, et al. Application of EASY-care standard 2010 instrument in a population-based survey in transitional Kosovo. Eur J Pub Health. (2019) 29:367–71. doi: 10.1093/eurpub/cky172
47. Kharicha, K, Iliffe, S, Harari, D, Swift, C, Gillmann, G, and Stuck, AE. Health risk appraisal in older people 1: are older people living alone an ‘at-risk’ group? Brit J Gen Pract. (2007) 57:271–6.
48. Lage, I, Braga, F, Almendra, M, Meneses, F, Teixeira, L, and Araujo, O. Falls in older persons living alone: the role of individual, social and environmental factors. Enferm Clin (Engl Ed). (2022) 32:396–404. doi: 10.1016/j.enfcli.2022.04.002
49. Baspakova, A, Abitova, AZ, Mussin, NM, Kaliyev, AA, Yerimbetova, G, Zhumagaliyeva, S, et al. Sex differentials in the prevalence of behavioral risk factors and non-communicable diseases in adult populations of West Kazakhstan. Front Public Health. (2024) 12:1333887. doi: 10.3389/fpubh.2024.1333887
50. Akhmetzhanov, B, Akhmetzhanov, B, Ozdemir, S, and Zhakiyev, N. Advancing affordable IoT solutions in smart homes to enhance independence and autonomy of the elderly. J Infras Policy Dev. (2024) 8:1–12. doi: 10.24294/jipd.v8i3.2899
51. Pekkarinen, S, Melkas, H, and Hyypiä, M. Elderly care and digital services: toward a sustainable sociotechnical transition In: M Toivonen and E Saari, editors. Human-centered digitalization and services. Singapore: Springer Nature Singapore (2019). 259–84. doi: 10.1007/978-981-13-7725-9_14
52. Morato, J, Sanchez-Cuadrado, S, Iglesias, A, Campillo, A, and Fernández-Panadero, C. Sustainable Technologies for Older Adults. Sustain Technol Older Adults Sustain. (2021) 13:8465. doi: 10.3390/su13158465
53. Tobis, S, Cylkowska-Nowak, M, Wieczorowska-Tobis, K, Pawlaczyk, M, and Suwalska, A. Occupational therapy Students' perceptions of the role of robots in the Care for Older People Living in the community. Occup Ther Int. (2017) 2017:1–6. doi: 10.1155/2017/9592405
54. Ozsungur, F. Gerontechnological factors affecting successful aging of elderly. Aging Male. (2020) 23:520–32. doi: 10.1080/13685538.2018.1539963
55. Tobis, S, Piasek-Skupna, J, Neumann-Podczaska, A, Religioni, U, and Suwalska, A. Determinants of attitude to a humanoid social robot in Care for Older Adults: a post-interaction study. Med Sci Monit. (2023) 29:e941205. doi: 10.12659/MSM.941205
56. Tobis, S, Piasek-Skupna, J, Neumann-Podczaska, A, Suwalska, A, and Wieczorowska-Tobis, K. The effects of stakeholder perceptions on the use of humanoid robots in Care for Older Adults: Postinteraction cross-sectional study. J Med Internet Res. (2023) 25:e46617. doi: 10.2196/46617
57. Tobis, S, Neumann-Podczaska, A, Kropinska, S, and Suwalska, A. UNRAQ—A questionnaire for the use of a social robot in Care for Older Persons. A multi-stakeholder study and psychometric properties. Int J Environ Res Public Health. (2021) 18:6157. doi: 10.3390/ijerph18116157
58. Shevelkova, V, Mattocks, C, and Lafortune, L. Efforts to address the sustainable development goals in older populations: a scoping review. BMC Public Health. (2023) 23:456. doi: 10.1186/s12889-023-15308-4
59. Beaton, DE, Bombardier, C, Guillemin, F, and Ferraz, MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). (2000) 25:3186–91. doi: 10.1097/00007632-200012150-00014
Keywords: older adults, needs assessment, sustainable eldercare, tool validation, functional independence, EASYCare Standard 2010
Citation: Kimatova K, Yermukhanova L, Talarska D, Dworacka M, Sultanova G, Sarsenbayeva G, Bazargaliyev Y, Aitmaganbet P, Suwalska A, Wieczorowska-Tobis K, Philp I and Tobis S (2025) Needs of older adults in Kazakhstan: analysis and psychometric properties of the localized version of the EASYCare standard 2010 instrument. Front. Public Health. 13:1487827. doi: 10.3389/fpubh.2025.1487827
Edited by:
Kshitija Wason, University of Delhi, IndiaReviewed by:
Ximena Ferrada, Universidad del Desarrollo, ChileAgnieszka Ptak-Wojciechowska, Poznań University of Technology, Poland
Copyright © 2025 Kimatova, Yermukhanova, Talarska, Dworacka, Sultanova, Sarsenbayeva, Bazargaliyev, Aitmaganbet, Suwalska, Wieczorowska-Tobis, Philp and Tobis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Slawomir Tobis, c3RvYmlzQHVtcC5lZHUucGw=
 Kerbez Kimatova
Kerbez Kimatova Lyudmila Yermukhanova1
Lyudmila Yermukhanova1 Marzena Dworacka
Marzena Dworacka Aleksandra Suwalska
Aleksandra Suwalska Katarzyna Wieczorowska-Tobis
Katarzyna Wieczorowska-Tobis Slawomir Tobis
Slawomir Tobis