- 1Flinders Health and Medical Research Institute, College of Medicine and Public Health, Flinders University Adelaide, Adelaide, SA, Australia
- 2Department of Psychiatry, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 3Research Centre for Public Health, Equity, and Human Flourishing, Torrens University Australia, Adelaide, SA, Australia
- 4School of Psychology, The University of Adelaide, Adelaide, SA, Australia
- 5Institute of Public Health, College of Medicine, and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Patient satisfaction with services is both a direct and indirect indicator of healthcare quality. It influences healthcare outcomes, patient retention, and the likelihood of medical malpractice claims. However, there is limited evidence on patient satisfaction with mental health services in Africa. Therefore, we aimed to assess mental health service satisfaction and its determinants in adult patients with mental illness in an outpatient clinic in Northwest Ethiopia.
Methods: A hospital-based cross-sectional study was conducted from October to March 2023. Participants were selected using systematic random sampling with a sample interval of three, resulting in a total sample size of 638 invited to participate. Service satisfaction was measured using the interviewer-administered Client Satisfaction Questionnaire-8 (CSQ-8). Data entry, coding, and analysis were performed using SPSS-28. To examine the association of sociodemographic, clinical, social support, and substance use factors, bivariate and multivariate logistic regression analyses were applied. Statistical significance was declared at a p-value of <0.05 and 95% CI.
Results: The rate of low mental health service satisfaction among people with mental illness in this study was 24.7%. According to our multivariate logistic regression analysis, people with urban residence 1.77 (1.15, 2.72), poor self-reported health 3.62(1.97, 6.67), having episodic illness ≥2/yr. 0.48 (0.32, 0.74), having relapse 1.75 (1.12, 2.73), and poor drug adherence 2.28 (1.20, 4.35) were more likely to have low mental health service satisfaction than their counterparts.
Conclusions and recommendation: One-quarter of patients with mental illness in the outpatient clinic reported low satisfaction with mental health services. Factors associated with lower satisfaction included urban residency, episodic illness, relapse, poor self-reported health, and poor drug adherence. To enhance patient satisfaction, the clinic should prioritize targeted support for patients facing these challenges.
Introduction
One of the goals of providing mental health services is patient satisfaction, which is also a key indicator of how well the mental health care system performs (1–4). Patient satisfaction is the degree to which patients feel that their overall medical and healthcare demands are being met (5). Satisfaction is affected by expectations and previous consumer perceptions of the consumption experience (6) and is determined by patient experiences (7). In mental health care, service satisfaction is frequently viewed as a vital process and quality indicator of service (8–11). Overall, evidence suggests that satisfied service consumers adhere to their therapy more rigorously, enabling them to gain more from their care service (12, 13). Conversely, dissatisfied people experience worse treatment outcomes, including nonadherence to therapy (14–16).
Rates of service satisfaction differ between nations. For example, in Europe, a survey conducted in Geneva showed that 93% of patients were satisfied with their outpatient psychiatric care (17). In the Netherlands, patients with psychosis reported low (19.4%), intermediate (48.9%), and high (31.7%) (18) service satisfaction; however, in Denmark, non-Western migrants attending specialized outpatient mental health clinics reported an overall satisfaction of 49% (19). In India, 87% of patients were satisfied with services (20), and in Kuwait, the satisfaction score was 27% in patients with schizophrenia (21). In Israel, 17% of psychotic patients reported being dissatisfied, barely satisfied (46%), moderately satisfied (26%) or delighted (12%) (22) with mental health services. In the African context, satisfaction scores range from 55 to 83% (23), with Ethiopia having satisfaction scores ranging from 57 to 99% (24–26).
Patient satisfaction studies are valuable and crucial means to identify gaps and create practical solutions for improving healthcare services (13). As patient satisfaction increases, trust between the patient and the medical staff also grows (27, 28). Quality of life has also been linked to patient satisfaction. For example, a study conducted in Norway showed that an unmet need for therapeutic relationships and quality of life had a negative association (29), and a review of analyses on quality of life and service satisfaction among psychotic patients indicated that there was a strong association (30) between these two indicators. Another study in Nigeria also showed that service satisfaction was correlated with quality of life (31). Satisfaction also affects treatment adherence, contributing to treatment failure and relapse (32, 33).
Available research on sociodemographic and clinical factors associated with patient service satisfaction comes from North American, European, and Pacific countries (12, 34, 35). There is inconsistent information about the influence of demographic factors, with age (13, 36), sex (13, 37), and education level (13, 37) being associated with satisfaction scores. Other studies have shown no association between these factors and satisfaction with age (19, 31) or sex (19, 31). Waiting time has been associated with satisfaction in some studies (13, 37, 38) but not in others (20). Clinical factors, including severe symptoms (39), a diagnosis of psychosis (37) and a diagnosis of schizophrenia (40), were found to be negatively associated with service satisfaction. Service satisfaction in patients with co-occurrence of mental illness and substance use has been studied in different countries. In the U.S., for example, the satisfaction score for adult patients diagnosed with comorbid mental health problems and alcohol and drug disorders was 29% (41). In Ethiopia, the satisfaction scores of mental illness patients with alcohol use disorder and nicotine dependence were 14.3 and 23.3%, (42) respectively. In a Tanzanian study, patient service satisfaction among patients with mental illness was 32.7% for those also with substance use, 21.7% for those with alcohol use, and 19.8% for those with tobacco and cannabis use disorders (12.9%) (43). These studies indicate that substance use affects service satisfaction for patients with mental illness (44).
Although quantitative research studies have shown that patients have high levels of service dissatisfaction, qualitative studies have shown further insight into patient satisfaction. For example, in Sweden, one study found high levels of service dissatisfaction among mental health service users (45), with evidence demonstrating increased satisfaction among service users who feel supported by staff (46). A study from Europe (Netherlands, Denmark, London, Spain and Italy) showed that service satisfaction was lower for individuals who had less support from family members (47). These studies suggest that it is important to look at a broader range of factors that might influence service satisfaction.
Previous studies on patient satisfaction with mental health services in Ethiopia including the study area differ from our study in several key areas. Notably, prior research did not examine the type of mental illness and its relationship to service satisfaction, history of previous admissions, the impact of episodic illness on satisfaction, or the role of family participation in healthcare on patient satisfaction in study area. Additionally, factors such as age of illness onset, duration of illness, and both subjective and objective illness severity in relation to service satisfaction were not addressed from previous study at study facility. These gaps highlight the need for the current study. This study sought to address a gap in evidence from Ethiopia in relation to associated with service satisfaction, as there has been limited research on this topic and only a narrow range of factors. Therefore, this study aimed to measure the magnitude of mental health service satisfaction among patients attending a psychiatry outpatient clinic in university of Gondar hospital Northwest Ethiopia and to examine the clinical, social support, psychoactive substance uses and sociodemographic predictor factors of satisfaction.
Methods
Study design and setting
This cross-sectional study was conducted in Ethiopia among people with mental illness at an outpatient clinic in the Amhara National Regional State at the University of Gondar Comprehensive Specialized Hospital Northwest Ethiopia from October 2022 to March 2023, a public sector institution.
Source and population
All patients who visited the outpatient clinic of the University of Gondar Hospital were considered the source population, and all patients who visited the outpatient clinic of the hospital during the study period were considered the study population. A total of 638 patients with mental illness who were followed up in outpatient clinics were recruited. Those who had received outpatient care for their mental disorders for at least three months were included, a time period after which patients are more likely to be stable with their condition. Patients with acute mental illness who could not communicate because of severe physical or mental illness were excluded. The data were collected by psychiatry Nurses. The university of Gondar comprehensive specialized hospital serves for the catchment area for more than ten million people and service as referral for district region for more than 15 million people in Northwest Ethiopia.
Sampling procedure
This paper reports on an examination of service satisfaction within a broader study of quality of life. The sample size was calculated using a single population proportion formula considering the following assumptions. We used a 41% prevalence of poor quality of life from a broader study conducted in Ethiopia, a 95% confidence level, and a 4% margin of error (48).
The following formula was used: n = (Zα/2)2 * P (1-P)/d2, where n is the minimum sample size needed, Z is a standard normal distribution (Z = 1.96) with a confidence interval of 95% and α = 0.05, d is the absolute precision or tolerable margin of error (4%), and P = estimated proportion is assumed to be 41% (0.41). Then, n = (1.96)2 *(0.41) *(0.59)/(0.04)2 = 580 and 10% nonresponse rates (580 *10/100) =58, with a 10 % nonresponse rate of 580 + 58 = 638. We used a systematic random sampling technique to obtain a total sample size of 638 patients who were followed up for the treatment of their mental illness from a group of 2,400 patients who were followed up at the University of Gondar Comprehensive Specialized Hospital, with a sample interval of three. Finally, 636 patients who had been followed up for at least three months and were 18 years old and older were included in the study, and two patients did not complete the study after commencement. Patients who had a clinical diagnosis of schizophrenia, depression, bipolar disorder, anxiety, other psychotic disorders, stress and trauma-related disorders, or somatization disorders were eligible for inclusion.
Data collection
The data were collected using a standardized questionnaire during a face-to-face interview at the outpatient psychiatry clinic. The questionnaires were prepared in English and translated into the local language, Amharic. Five psychiatry nurses and two MSc psychiatry supervisors participated in the data collection. The data collectors and supervisors received two days of training, and a pre-test of two weeks was conducted but these results were not included in the final analysis. Based on the findings from the pre-test, the questionnaires were revised and finalized. The interview was estimated to take 45 min. As part of the consent process, data collectors sought permission to access the person’s health records, which could assist in providing background information of the patient’s specific diagnosis, medications, and previous history of hospital admission. The data collectors were supervised daily by assigned supervisors, and the filled questionnaires were checked daily by the supervisors and principal investigator. Questionnaires were reviewed daily for completeness by data collectors, supervisors, and then by the researcher throughout data collection. Two incomplete surveys were discarded from the final analysis.
Variables
Mental health service satisfaction was the dependent variable of this study. The independent variables were sociodemographic characteristics (age, sex, marital status, educational status, living condition, job of participant, residence), clinical factors (type of mental illness, age of onset illness, duration of illness, number of episodes of illness per year, history of admission, comorbid illness, type of drug, drug side effects, counseling, duration of treatment, relapse, objective severity of illness, subjective severity of illness, suicidal ideation, family history of mental illness, waiting time in clinic sand self-reported health), social support-related factors (family not participating in patient care, relationship with family) and substance use factors (alcohol use, tobacco use, family history of substance use). Additional variables, such as self-esteem, drug adherence and legal issues, were also included.
Measures
Service satisfaction
The Client Satisfaction Questionnaire-8 (CSQ-8) comprises an eight-item questionnaire for assessing patients’ global satisfaction with services and has good psychometric properties (49). The CSQ-8 measures general satisfaction on eight scale items ranging from 1 (poor) to 4 (excellent), resulting in a total score ranging from 8 to 32. The level of satisfaction is classified as low (8–20), intermediate (21–25), or high (26–32). Psychometric evaluation of the CSQ-8 in the current sample showed high-scale reliability (Cronbach’s alpha = 0.84). The CSQ-8 has been validated in African Egypt and has internal consistency (Cronbach’s α = 0.88) (50).
Self-esteem
Self-esteem was measured with the single-item self-esteem scale. The single-item self-esteem scale is a measure of overall self-esteem. Participants rate the single item on a 5-point Likert scale ranging from 1 (not very true of me) to 5 (very true of me). Although shorter than the Rosenberg Self-Esteem Scale, the scale exhibits good convergent and comparable predictive validity (51). This item has not been validated in Ethiopia.
Medication adherence
The Medication Adherence Scale (MARS-5) assesses patients’ standard treatment adherence through five questions and five response formats (1 = always, 2 = often, 3 = occasionally, 4 = rarely, and 5 = never). Responses are added for a total score ranging from 5 to 25, with higher scores indicating greater adherence. As advised by the developer, we used a cutoff point greater than or equal to 20 (52, 53) to indicate adherence. This scale has been validated in Africa and Nigeria (54).
Substance use
Clients who used substances (for nonmedical purposes) such as alcohol, khat, cigarettes or cannabis in the last year before data collection were considered current substance users (55).
Severity of illness
The Clinical Global Impression (CGI) scale of subjective and objective measurement was used to assess the severity of the illness. Responses 1–3 indicate mild, responses 4 indicate moderate, and responses 5–7 indicate severe according to the CGI scale (56). This scale has not been validated in Ethiopia/Africa.
Data processing and analysis
After verifying accuracy and consistency, all the data were checked, cleaned, coded, and entered into SPSS-28, which was subsequently used to analyses the data. The dependent variable was mental health service satisfaction. First, bivariate logistic regression was used to independently evaluate the relationship between each independent variable and service satisfaction. To control for potential confounding effects, variables with p values less than or equal to 0.2 were fitted to a multivariable logistic regression model (57). After adjusting for odds ratios with 95% CIs, bivariate analysis was applied to identify relationships between dependent and independent variables and measure the associations of strength. A p value of <0.05 and a 95% CI were used to indicate statistical significance.
Ethical clearance
Ethical approval was obtained from the Flinders University Human Research Ethics Committee and the Institutional Review Board of the University of Gondar. Written informed consent was obtained from the people who participated in the study. Respondents were briefed and made aware of the study goal and told of their unrestricted freedom to withdraw from the study at any time. Additionally, code numbers rather than personal identification were used to ensure confidentiality.
Results
Sociodemographic, clinical, substance use, and social support related characteristics of patients with mental illness in an outpatient clinic in Ethiopia, 2023
The study included 636 participants, yielding a 99.7% response rate. The average age was 35.5 years (±11.7). About half of the participants were female (324, 51%), and most (431, 67.8%) were urban residents. Schizophrenia was the most common diagnosis (274, 43%), followed by depression (192, 30.2%), bipolar disorder (50, 7.9%), anxiety disorder (39, 6.1%), other psychotic disorders (68, 10.7%), somatization disorder (7, 1.1%), and stress/trauma-related disorders (6, 0.9%). Antipsychotic medication was used by 301 participants (47.3%), and 135 (21.2%) were taking both antipsychotics and antidepressants. Of the total patients, 199 (31.3%) had been followed for over five years, nearly 589 (92.6%) reported good self-rated health, 412 (64.8%) experienced relapsing illness, 338 (53.1%) had two or more episodes per year, 316 (49.7%) reported low self-esteem, and 87 (13.7%) had poor drug adherence (Table 1).
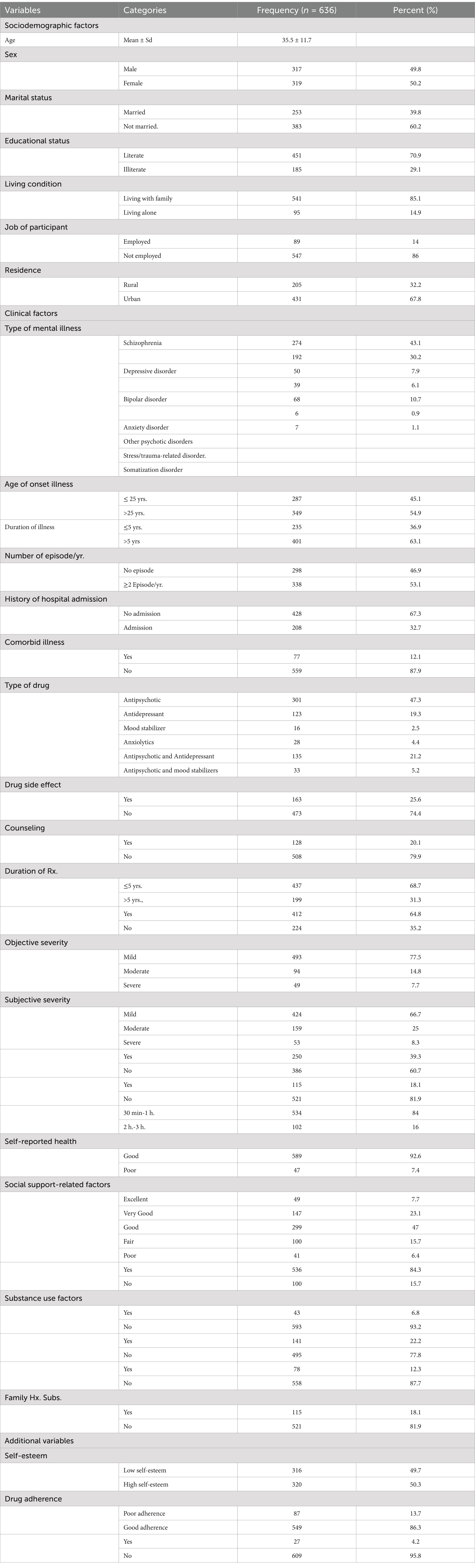
Table 1. Sociodemographic, clinical, substance use, and social support related factors of people with mental illness in an outpatient clinic in Ethiopia, 2023 (n = 636).
Service satisfaction among people with mental illness in an outpatient clinic
The mean and standard deviation of the CSQ-8 score were 23.6 (±4.1), demonstrating intermediate satisfaction. A total of 636 participants [157 (24.7%) reported overall low satisfaction, and 479 (75.3%) reported high satisfaction]. Almost half of the participants (52.8%) said that they received good-quality services; over half (52.5%) reported that they received the kind of service they wanted; some participants (42.6%) reported that the program met their needs; 49.5% of participants would recommend the program to a friend who needed similar help; 50.2% of participants were satisfied with the amount of support they had received; 44.3% patients believed the services they received helped them to deal more effectively with their problems; 38.8% had good satisfaction in a general sense with the service they received; and 49.4% had good responses and would come back if they sought help (Table 2).
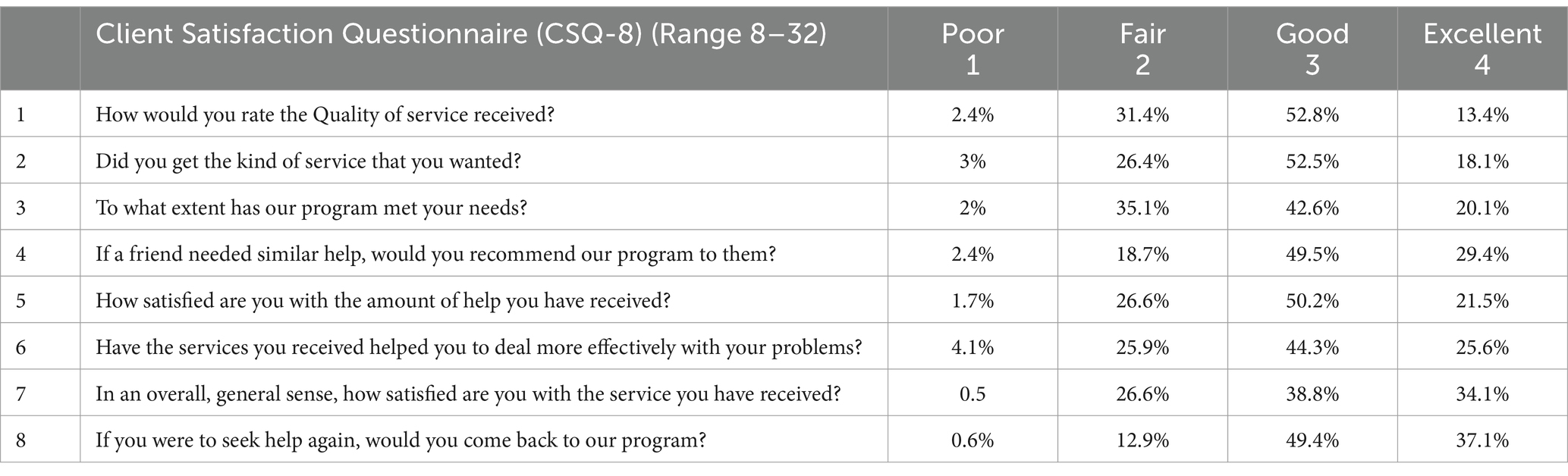
Table 2. Distribution of items of tools to measure service satisfaction in people living with mental illness in Ethiopia, 2023 (n = 636).
Factors associated with low mental health service satisfaction
We used binary and multivariate logistic regression to identify factors associated with mental health service satisfaction. As planned, variables with p values ≤0.2 in the bivariate analysis were fitted into a multivariate logistic regression model to manage the impacts of confounding effects. A total of twenty-three variables had a p value ≤0.2. The sociodemographic factors (marital status, education, job, residence), clinical factors (number of episodes/yr., number of admissions, comorbid illness, duration of treatment, relapse, suicidal ideation, family history of mental illness, waiting time in clinics, self-reported health, objective severity of illness, subjective severity of illness, self-esteem, drug adherence), substance use factors (family history of substance use, tobacco use, khat use), and social support-related factors (relationship with family, family participates in treatment) were identified through analysis.
Multivariate logistic regression revealed that living in urban regions; having poor self-reported health; having a relapse, having episodic illness; and poor drug adherence were significantly associated with low mental health service satisfaction (Table 3).
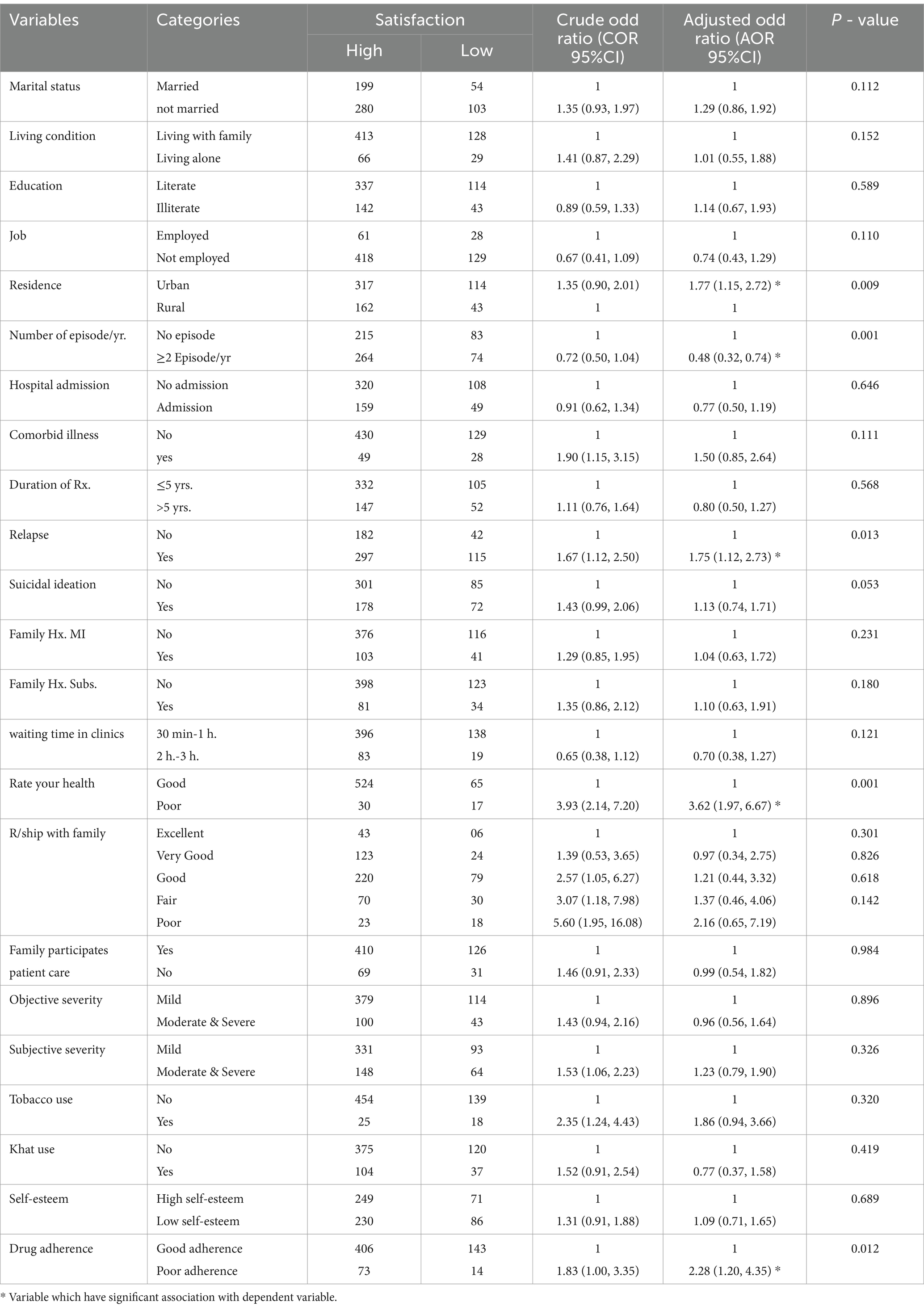
Table 3. Bivariate and multivariate logistic regression analysis of factors associated with low mental health service satisfaction among people with mental illness in Ethiopia, 2023 (n = 636).
Participants from urban regions were 1.77 times more likely (AOR = 1.77, 95% CI: 1.15–2.72) to report lower satisfaction with services compared to those from rural regions.
Patients who self-reported poor health were 3.62 times more likely (AOR = 3.62, 95% CI: 1.97–6.67) to report low service satisfaction compared to those who reported good health.
The odds of low mental health service satisfaction were 1.75 times higher (AOR = 1.75, 95% CI: 1.12–2.73) among participants with relapsed illness compared to those without relapsing illness.
Patients with non-episodic illness were 48% less likely (AOR = 0.48, 95% CI: 0.32–0.74) to experience low mental health service satisfaction compared to those with episodic illness.
Participants with poor drug adherence had 2.28 times higher odds of low mental health service satisfaction (AOR = 2.28, 95% CI: 1.20–4.35) compared to those with good drug adherence.
Discussion
Since service satisfaction is one of the factors that can affect service user quality of life and health outcomes, measuring outpatients’ satisfaction with mental health services in psychiatric clinics is essential. Furthermore, by measuring patient satisfaction, institutions may recognize areas were service delivery needs improvement. The current study was designed to determine mental health service satisfaction and associated factors among patients attending a psychiatry outpatient clinic.
The overall magnitude of high mental health service satisfaction was 75.3% (72–79.1%), while the remaining 24.7% reported low service satisfaction. This magnitude is similar to that of a previous study conducted University of Gondar Hospital in 2017, in which approximately 77.6% of the study participants were satisfied with outpatient care (58). These findings were also consistent with those of another study conducted in an outpatient clinic receiving mental health services at public hospitals in Mekelle town, Ethiopia, which reported a satisfaction rate of 72% (37). This similarity may be because of both studies likely shared similar factors influencing patient satisfaction, such as the quality of care, the approach of patients and healthcare providers, and access to medications and service availability. Additionally, the facilities in both studies were specialized hospitals with similar characteristics, which may have influenced patient satisfaction levels. The similarity of results suggests that common factors, such as improvements in service delivery and the availability of patient support, are key contributors to satisfaction in outpatient mental health services.
The satisfaction score was higher in our study than in other psychiatric outpatient hospital settings in Ethiopia, for example, at St. Poul Hospital in Ethiopia (50.3%) (59), university of Gondar Hospital (65.46%), at Dilla Hospital (55.4%) (38) and at Dessie Hospital (61.2%) (60). The discrepancy in satisfaction scores might be attributable to factors such as the use of different measurement tools, differences in mental health literacy among patients and mental health services, and differences in actual service quality of health care facilities. In general, mental health service satisfaction varies across Ethiopia due to significant differences in health infrastructure, the availability of mental health professionals, and access to essential medications. Urban areas have better facilities and more specialized services compared to rural regions. Additionally, cultural beliefs about mental illness differ across communities, influencing how people perceive and utilize mental health services. In some areas, higher levels of stigma toward mental illness cause to lower satisfaction, as people may face reduced social support and understanding (61, 62). The higher satisfaction score in our study, compared to other psychiatric outpatient settings in Ethiopia, could be attributed to several factors. Our study site has seen recent improvements in service delivery, including better patient-staff communication. As referral hospital, it benefits from senior professionals providing accessible care like psychiatrist, mental health professionals, clinical psychologist and social workers and psychiatry Nurses. additionally, the availability of medications and other resources, such as support services, plays a key role in patient satisfaction. Difference in similar setting may be related to time difference in the study, prior studies done before five years ago due to that there is quality of care difference in the service provided that cause difference in mental health service satisfactions.
When asked about their satisfaction specifically with the quality of care that was provided, almost half of the survey participants (52.8%) reported receiving good quality services in mental health care in the study setting. This observation was similar to the findings of a hospital-based study in Ethiopia, where almost 50% of patients were satisfied with the quality of service received in a psychiatry outpatient clinic, and better than the findings of another study conducted in Ethiopia on the perceived quality of a general medical outpatient service, where only 35% of participants reported receiving good quality service (63). These differences could have been a result of a variation of care in different settings, i.e., between services provided in specialized psychiatry outpatient clinics and those provided by general medical outpatient services, with specialized clinics receiving higher satisfaction scores compared to general medical services where electroconvulsive therapy and senior specialists were present.
According to international comparisons, the service satisfaction score in our study was greater than that reported in studies conducted among patients with mental illness in outpatient clinics in other African countries, including 50% in Egypt and 52.4% in Nigeria (64). Differences in service satisfaction scores across these studies may come from variations in data collection methods and study designs. For instance, while other studies included all patients attending psychiatric outpatient clinics, the Nigerian study focused exclusively on patients with schizophrenia. This narrower cohort of participants may have influenced the satisfaction scores.
Other studies across different continents have reported varying satisfaction scores; for example, in a study conducted in Pakistan, 72% of participants were satisfied with mental health services and in a study conducted in Geneva, 85% of patients reported satisfaction with their mental health outpatient treatment (17). Furthermore, equivocal findings have been demonstrated in different studies that aimed to measure mental health service satisfaction in more developed settings globally; for example, 45% of anxiety outpatients in Los Angeles, 53% of patients with mental health in Mexico and 52% of patients with mental illness in Ireland (65). These differences might be attributable to factors such as the study setting, cultural context and patient expectations of the facilities (36); differences in the data collection methods and study design; and variation in the satisfaction measurement tools used.
In terms of the factors associated with service satisfaction, the satisfaction level of participants in this study was significantly related to area of residence. Participants who were from urban areas were 1.77 times more likely to report low mental health service satisfaction than were those who came from rural areas. Previous studies have reported similar findings in mental health care services in Ethiopia; urban residence was found to be a factor associated with low satisfaction with mental health services provided in an outpatient psychiatry service of Dilla University referral hospital in southern Ethiopia (38), and in Dessie, those living in urban areas were less likely to be satisfied (60). This may be related to urban residents often have higher expectations for service quality due to the greater availability of resources and better infrastructure. Although urban areas offer a wide range of mental health services, in my opinion rural areas may benefit from stronger social networks and family or community-centered support systems. In addition, in my opinion informal support systems in rural areas are common and it can supplement formal care service, leading to higher patient satisfaction and future research should focus to study between service satisfaction and residency status.
This study found that patients with relapsed illness were 1.75 times more likely to report low satisfaction with mental health services compared to those without a relapsing illness. To our knowledge, no previous quantitative studies have directly compared these outcomes with our findings. It may be that patients who experience relapse may feel that the treatments and support provided are not effectively meeting their needs, leading to frustration and disappointment with mental health services. In addition, the increased time and financial demands associated with relapse can add stress, further affecting their overall satisfaction. Additionally, relapse may intensify feelings of stigma, which can lower their satisfaction with the care received (66, 67).
In this study, patients with poor self-rated health were 3.62 times more likely to report low satisfaction with mental health services compared to those with good self-rated health. This could be attributed to individuals with mental illness and poor self-rated health often experiencing life dissatisfaction, low mood or depression, memory and concentration difficulties, and challenges in maintaining positive social relationships with family, friends, and neighbors (68). These findings align with a national survey conducted in Australia, which explored poor self-rated health and its association with somatization disorder (69).
The results obtained from this study showed that patients who had poor drug adherence were more than twice as likely to have low mental health service satisfaction than participants with good drug adherence. Previous studies have reported similar findings showing that drug nonadherence is associated with service dissatisfaction, an indication that patients with mental illnesses may be more prone to not taking their medications as prescribed and may consequently develop low service satisfaction (70).
Studies considering factors associated with mental health service satisfaction have previously shown a statistical correlation between the short waiting time for services in the hospital (71–75). In this study, approximately 157 patients (25%) had low satisfaction with the wait time at the outpatient clinic; however, waiting time was not significantly associated with patient satisfaction in the final analysis. In contrast, another study in Ethiopia that was conducted in a medical outpatient clinic showed that having a waiting time of less than one hour was a predictor of perceived good quality care by patients with mental illness (63).
Notably, in the present study, unlike in other studies, age, marital status, education, job, type of diagnosis, suicidal ideation, and family history of mental illness were not significantly correlated with low service satisfaction among participants. Previous Ethiopian studies have shown the following variables to be associated with service satisfaction: being male, being widowed, having been diagnosed with schizophrenia, having poor social functioning, living a long distance from the hospital, waiting for the service for a long time, having a low monthly income (38), not being hospitalized, receiving medications from the hospital and having strong social support (76). The cause may be attributed to variations in the diagnosis of patients receiving care at facilities, and potential methodological variations in the study method should also be considered.
Strengths and limitations of the study
This study has several strengths and limitations. One of the strengths of this study is that this is the first study to show overall mental health service satisfaction among patients with mental illness in an outpatient clinic of a comprehensive specialized hospital in Ethiopia, including patients with different clinical diagnoses, such as schizophrenia, depression, bipolar disorder and other psychosis disorders. This is the first study to comprehensively examine the impact of sociodemographic, clinical, substance use, and social support-related factors on patients’ satisfaction with mental health services in Ethiopia. Additionally, factors such as relapse, episodic illness, and self-rated health have shown an association with low mental health service satisfaction. These are new factors that had not been previously assessed as predictors of low mental health service satisfaction among patients with mental illness.
This study has several limitations that should be considered, including (i) social desirability bias that could affect the questionnaire responses and data collectors are clinical stuffs working in the study area (ii) its cross-sectional nature and ability to determine the temporal relationship between patient satisfaction and related parameters, and (iii) the ability of the clinic to recruit patients who were more likely to be satisfied, the effect of which could have increased the satisfaction score for the study and lastly the study excluded severely ill patient who did not communicate that makes the result biased. It is also possible that those patients who were not satisfied with the service provision may have not attended the follow-up in the outpatient clinic and were therefore missing among the study participants.
Conclusion and recommendations
The findings of this study showed that almost 25% of patients in outpatient clinics had low mental health service satisfaction, which requires improvement. Those from urban residences with episodic illness; with a relapse illness; with self-reported health, poor and good health; and poor drug adherence were found to have lower mental health service satisfaction. Therefore, hospital administrations, lawmakers, and accountable authorities should work on activities that increase patient satisfaction, considering these factors. Future research should focus on to study the relationship between service satisfaction and some variables like residence being urban and rural, and informal and formal support.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Flinders University Human Research Ethics and Biosafety Committee as well as the University of Gondar. Written informed consent to participate in this study was provided by the patient.
Author contributions
WA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. LM: Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. CD: Methodology, Supervision, Writing – original draft. TA: Investigation, Methodology, Supervision, Writing – review & editing. AZ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We want to thank all the study participants, data collectors, and supervisors who contributed their time and effort to complete the research. In addition, Wondale Getinet Alemu thanks Flinders University and the Australian Government Research Training Programme (RTP) for funding his PhD scholarship. This research was supported by the Australian Government Research Training Program (RTP) and Flinders University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, Adjusted odds ratio; CI, Confidence interval; COR, Crude odds ratio; CSQ, Client satisfaction questionnaire; MARS-5, Medication Adherence Rate Scale; CGI, Clinical Global Impression Scale; OR, Odds ratio; SD, Standard deviation; SPSS-28, Statistical Package for Social Science.
References
1. Blenkiron, P, and Hammill, C. What determines patients’ satisfaction with their mental health care and quality of life? Postgrad Med J. (2003) 79:337–40. doi: 10.1136/pmj.79.932.337
2. Bramesfeld, A, Wedegärtner, F, Elgeti, H, and Bisson, S. How does mental health care perform in respect to service users' expectations? Evaluating inpatient and outpatient care in Germany with the WHO responsivenessconcept. BMC Health Serv Res. (2007) 7:1–12. doi: 10.1186/1472-6963-7-99
3. Leonard, KL. Is patient satisfaction sensitive to changes in the quality of care? An exploitation of the Hawthorne effect. J Health Econ. (2008) 27:444–59. doi: 10.1016/j.jhealeco.2007.07.004
4. Al-Abri, R, and Al-Balushi, A. Patient satisfaction survey as a tool towards quality improvement. Oman Med J. (2014) 29:3–7. doi: 10.5001/omj.2014.02
5. McMillan, SS, Kendall, E, Sav, A, King, MA, Whitty, JA, Kelly, F, et al. Patient-centered approaches to health care: a systematic review of randomized controlled trials. Med Care Res Rev. (2013) 70:567–96. doi: 10.1177/1077558713496318
6. Gill, L, and White, L. A critical review of patient satisfaction. Leadersh Health Serv. (2009) 22:8–19. doi: 10.1108/17511870910927994
7. Bjertnaes, OA, Sjetne, IS, and Iversen, HH. Overall patient satisfaction with hospitals: effects of patient-reported experiences and fulfilment of expectations. BMJ Quality Safety. (2012) 21:39–46. doi: 10.1136/bmjqs-2011-000137
8. Priebe, S, and Miglietta, E. Assessment and determinants of patient satisfaction with mental health care. World Psychiatry. (2019) 18:30–1. doi: 10.1002/wps.20586
9. Shipley, K, Hilborn, B, Hansell, A, Tyrer, J, and Tyrer, P. Patient satisfaction: a valid index of quality of care in a psychiatric service. Acta Psychiatr Scand. (2000) 101:330–3. doi: 10.1034/j.1600-0447.2000.101004330.x
10. Ruggeri, M. Patients' and relatives' satisfaction with psychiatric services: the state of the art of its measurement. Soc Psychiatry Psychiatr Epidemiol. (1994) 29:212–27. doi: 10.1007/BF00796380
11. Stamboglis, N, and Jacobs, R. Factors associated with patient satisfaction of community mental health services: a multilevel approach. Community Ment Health J. (2020) 56:50–64. doi: 10.1007/s10597-019-00449-x
12. Fortin, M, Bamvita, J-M, and Fleury, M-J. Patient satisfaction with mental health services based on Andersen’s behavioral model. Can J Psychiatry. (2018) 63:103–14. doi: 10.1177/0706743717737030
13. Chandra, S, Ward, P, and Mohammadnezhad, M. Factors associated with patient satisfaction in outpatient department of Suva sub-divisional Health Center, Fiji, 2018: a mixed method study. Front Public Health. (2019) 7:183. doi: 10.3389/fpubh.2019.00183
14. Smith, D, Roche, E, O’Loughlin, K, Brennan, D, Madigan, K, Lyne, J, et al. Satisfaction with services following voluntary and involuntary admission. J Ment Health. (2014) 23:38–45. doi: 10.3109/09638237.2013.841864
15. Chaka, B. Adult patient satisfaction with nursing care. Gray literature: MPH thesis, department of community health, Addis Ababa University (2005).
16. Shahbaz, S, Hans, RK, and Mudassar, S. Service quality, word of mouth and trust: drivers to achieve patient satisfaction. Sci Res Essays. (2010) 5:2457–62.
17. Davy, B, Keizer, I, Croquette, P, Bertschy, G, Ferrero, F, Gex-Fabry, M, et al. Patient satisfaction with psychiatric outpatient care in Geneva: a survey in different treatment settings. Schweizer Archiv Fuer Neurologie Und Psychiatrie. (2009) 160:240–5. doi: 10.4414/sanp.2009.02087
18. Vermeulen, J, Schirmbeck, N, van Tricht, M, and de Haan, L. Satisfaction of psychotic patients with care and its value to predict outcomes. Eur Psychiatry. (2018) 47:60–6. doi: 10.1016/j.eurpsy.2017.10.003
19. Lindberg, LG, Mundy, SS, Kristiansen, M, Johansen, KS, and Carlsson, J. Satisfaction with mental health treatment among patients with a non-Western migrant background: a survey in a Danish specialized outpatient mental health clinic. Eur J Pub Health. (2019) 29:700–5. doi: 10.1093/eurpub/ckz090
20. Jena, S, and Gupta, M. A survey of patient satisfaction of patients attending a psychiatry outpatient clinic at a tertiary care Centre. Int J Commun Med Public Health. (2018) 5:2026. doi: 10.18203/2394-6040.ijcmph20181717
21. Zahid, MA, Ohaeri, JU, and Al-Zayed, AA. Factors associated with hospital service satisfaction in a sample of Arab subjects with schizophrenia. BMC Health Serv Res. (2010) 10:1–11. doi: 10.1186/1472-6963-10-294
22. Ratner, Y, Zendjidjian, XY, Mendyk, N, Timinsky, I, and Ritsner, MS. Patients' satisfaction with hospital health care: identifying indicators for people with severe mental disorder. Psychiatry Res. (2018) 270:503–9. doi: 10.1016/j.psychres.2018.10.027
23. Iliyasu, Z, Abubakar, I, Abubakar, S, Lawan, U, and Gajida, A. Patients' satisfaction with services obtained from Aminu Kano teaching hospital, Kano, northern Nigeria. Niger J Clin Pract. (2010) 13:371–8.
24. Dagnew, M, and Zakus, D. Community perception on OPD performance of a teaching hospital in Gondar town. Ethiop Med J. (1997) 35:153–60.
25. Afework, S, Mariam, DH, and Demeke, B. Assessment of quality of services in private clinics in Addis Ababa. Ethiopia Ethiopian Medical J. (2003) 41:267–78.
26. Oljira, L, and Gebre-Selassie, S. Satisfaction with outpatient health services at Jimma hospital, south West Ethiopia. Ethiop J Health Dev. (2001) 15:179–84.
27. Riklikienė, O, Didenko, O, Ciutiene, R, Daunoriene, A, and Ciarniene, R. Balancing nurses’ workload: a case study with nurse anaesthetists and intensive care nurses. Econ Soc. (2020) 13:11–25. doi: 10.14254/2071-789X.2020/13-2/1
28. Jakubowska, A, Bilan, S, and Werbiński, J. Chronic diseases and labour resources:" old and new" European Union member states. J Int Stud. (2021) 14:129–38. doi: 10.14254/2071-8330.2021/14-1/9
29. Ådnanes, M, Kalseth, J, Ose, SO, Ruud, T, Rugkåsa, J, and Puntis, S. Quality of life and service satisfaction in outpatients with severe or non-severe mental illness diagnoses. Qual Life Res. (2019) 28:713–24. doi: 10.1007/s11136-018-2039-5
30. Petkari, E, and Pietschnig, J. Associations of quality of life with service satisfaction in psychotic patients: a meta-analysis. PLoS One. (2015) 10:e0135267. doi: 10.1371/journal.pone.0135267
31. Afe TOBello-Mojeed, M, and Ogunsemi, O. Perception of service satisfaction and quality of life of patients living with schizophrenia in Lagos, Nigeria. J Neurosci Rural Practice. (2016) 7:216–22. doi: 10.4103/0976-3147.178652
32. Hudak, PL, Hogg-Johnson, S, Bombardier, C, McKeever, PD, and Wright, JG. Testing a new theory of patient satisfaction with treatment outcome. Med Care. (2004) 42:726–39. doi: 10.1097/01.mlr.0000132394.09032.81
33. Leebov, W, and Scott, G. Service quality Improvemenk the customer satisfaction strategy for healthcare. J Healthcare Qual. (1996) 18:35. doi: 10.1097/01445442-199607000-00009
34. Clignet, F, Houtjes, W, van Straten, A, Cuijpers, P, and van Meijel, B. Unmet care needs, care provision and patient satisfaction in patients with a late life depression: a cross-sectional study. Aging Ment Health. (2019) 23:491–7. doi: 10.1080/13607863.2018.1426716
35. Kelly, PJ, Kyngdon, F, Ingram, I, Deane, FP, Baker, AL, and Osborne, BA. The client satisfaction Questionnaire-8: psychometric properties in a cross-sectional survey of people attending residential substance abuse treatment. Drug Alcohol Rev. (2018) 37:79–86. doi: 10.1111/dar.12522
36. Thi, PLN, Briancon, S, Empereur, F, and Guillemin, F. Factors determining inpatient satisfaction with care. Soc Sci Med. (2002) 54:493–504. doi: 10.1016/S0277-9536(01)00045-4
37. Desta, H, Berhe, T, and Hintsa, S. Assessment of patients’ satisfaction and associated factors among outpatients received mental health services at public hospitals of Mekelle town, northern Ethiopia. Int J Ment Heal Syst. (2018) 12:1–7. doi: 10.1186/s13033-018-0217-z
38. Kassaw, C, Eskeziya, A, and Anbesaw, T. Magnitude of patient satisfaction and its associated factors at the outpatient psychiatry service of Dilla university referral hospital, southern Ethiopia, Dilla, 2020. PLoS One. (2022) 17:e0272485. doi: 10.1371/journal.pone.0272485
39. McGranahan, R, Hansson, L, and Priebe, S. Psychopathological symptoms and satisfaction with mental health in patients with schizophrenia. Psychopathology. (2018) 51:192–7. doi: 10.1159/000487399
40. Alkaabi, S, Al-Balushi, N, Al-Alawi, M, Mirza, H, Al-Huseini, S, Al-Balushi, M, et al. Level and determinants of patient satisfaction with psychiatric out-patient services, Muscat. Oman Int J Mental Health. (2019) 48:80–94. doi: 10.1080/00207411.2019.1585226
41. Regier, DA, Farmer, ME, Rae, DS, Locke, BZ, Keith, SJ, Judd, LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA. (1990) 264:2511–8. doi: 10.1001/jama.1990.03450190043026
42. Dawud, B, Yeshigeta, E, Negash, A, Mamaru, A, Agenagnew, L, Tolosa, D, et al. Community-based cross-sectional study. Clin Med Insights. (2017) 2021:1179557321989699.
43. Karino, K, Ambikile, JS, and Iseselo, MK. Prevalence and factors associated with self-reported substance use among patients with mental illness in Dar Es Salaam, Tanzania: a cross-sectional analytical study. Ment Illn. (2023) 2023:1–8. doi: 10.1155/2023/3923793
44. Stallvik, M, Flemmen, G, Salthammer, JA, and Nordfjærn, T. Assessing health service satisfaction among users with substance use disorders within the municipalities in Norway. Subst Abuse Treat Prev Policy. (2019) 14:18. doi: 10.1186/s13011-019-0207-4
45. Svensson, B, and Hansson, L. Satisfaction with mental health services. A user participation approach. Nord J Psychiatry. (2006) 60:365–71. doi: 10.1080/08039480600937090
46. Skar-Fröding, R, Clausen, HK, Šaltytė Benth, J, Ruud, T, Slade, M, and Sverdvik, HK. Relationship between satisfaction with mental health services, personal recovery and quality of life among service users with psychosis: a cross-sectional study. BMC Health Serv Res. (2021) 21:1–8. doi: 10.1186/s12913-021-06409-0
47. Ruggeri, M, Lasalvia, A, Bisoffi, G, Thornicroft, G, Vazquez-Barquero, JL, Becker, T, et al. Satisfaction with mental health services among people with schizophrenia in five European sites: results from the EPSILON study. Schizophr Bull. (2003) 29:229–45. doi: 10.1093/oxfordjournals.schbul.a007000
48. Shumye, S, Amare, T, Derajew, H, Endris, M, Molla, W, and Mengistu, N. Perceived quality of life and associated factors among patients with severe mental illness in Ethiopia: a cross-sectional study. BMC Psychol. (2021) 9:1–8. doi: 10.1186/s40359-021-00664-w
49. Attkisson, CC, and Greenfield, TK. The client satisfaction questionnaire (CSQ) scales and the service satisfaction scale-30 (SSS-30). Outcomes Assessment Clinical Practice. (1996) 120:120–7.
50. Shorub, EM, Rasas, HH, and Kalifa, AG. Satisfaction with Ain shams outpatient mental health services. Middle East current. Psychiatry. (2015) 22:186–92. doi: 10.1097/01.XME.0000470974.85176.c7
51. Robins, RW, Hendin, HM, and Trzesniewski, KH. Measuring global self-esteem: construct validation of a single-item measure and the Rosenberg self-esteem scale. Personal Soc Psychol Bull. (2001) 27:151–61. doi: 10.1177/0146167201272002
52. Stone, JK, Shafer, LA, Graff, LA, Lix, L, Witges, K, Targownik, LE, et al. Utility of the MARS-5 in assessing medication adherence in IBD. Inflamm Bowel Dis. (2021) 27:317–24. doi: 10.1093/ibd/izaa056
53. Ediger, JP, Walker, JR, Graff, L, Lix, L, Clara, I, Rawsthorne, P, et al. Predictors of medication adherence in inflammatory bowel disease. LWW. (2007) 102:1417–26. doi: 10.1111/j.1572-0241.2007.01212.x
54. Ubaka, CM, Ibe, OG, Amorha, KC, Isah, A, and Okonta, MJ. Medication adherence among Nigerian patients with rheumatoid arthritis: a two instruments survey. J Pharm Health Serv Res. (2021) 12:11–7. doi: 10.1093/jphsr/rmaa007
55. Humeniuk, R, Ali, R, Babor, TF, Farrell, M, Formigoni, ML, Jittiwutikarn, J, et al. Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction. (2008) 103:1039–47. doi: 10.1111/j.1360-0443.2007.02114.x
56. Kadouri, A, Corruble, E, and Falissard, B. The improved clinical global impression scale (iCGI): development and validation in depression. BMC Psychiatry. (2007) 7:1–7. doi: 10.1186/1471-244X-7-7
57. Nakagawa, S, and Cuthill, IC. Effect size, confidence interval and statistical significance: a practical guide for biologists. Biol Rev. (2007) 82:591–605. doi: 10.1111/j.1469-185X.2007.00027.x
58. Woldekidan, NA, Gebresillassie, BM, Alem, RH, Gezu, BF, Abdela, OA, and Asrie, AB. Patient satisfaction with psychiatric outpatient Care at University of Gondar specialized hospital: a cross-sectional survey. Psychiatry J. (2019) 2019:1–7. doi: 10.1155/2019/5076750
59. Goben, KW, Abegaz, ES, and Abdi, ST. Patient satisfaction and associated factors among psychiatry outpatients of St Paulo's hospital, Ethiopia. Gen Psychiatr. (2020) 33:e100120. doi: 10.1136/gpsych-2019-100120
60. Yimer, S, Yohannis, Z, Getinet, W, Mekonen, T, Fekadu, W, Belete, H, et al. Satisfaction and associated factors of outpatient psychiatric service consumers in Ethiopia. Patient Prefer Adherence. (2016) 10:1847–52. doi: 10.2147/PPA.S115767
61. Sibitz, I, Amering, M, Unger, A, Seyringer, M, Bachmann, A, Schrank, B, et al. The impact of the social network, stigma and empowerment on the quality of life in patients with schizophrenia. Eur Psychiatry. (2011) 26:28–33. doi: 10.1016/j.eurpsy.2010.08.010
62. Wang, D-F, Zhou, Y-N, Liu, Y-H, Hao, Y-Z, Zhang, J-H, Liu, T-Q, et al. Social support and depressive symptoms: exploring stigma and self-efficacy in a moderated mediation model. BMC Psychiatry. (2022) 22:117. doi: 10.1186/s12888-022-03740-6
63. Utino, L, Birhanu, B, Getachew, N, and Ereso, BM. Perceived quality of medical services at outpatient department of public hospitals in Dawro zone, southern Ethiopia. BMC Health Serv Res. (2023) 23:209. doi: 10.1186/s12913-023-09178-0
64. Omoronyia, FR, Ndiok, AE, Enang, KO, and Obande, EI. Patients’ satisfaction with psychiatric nursing care in Benin, Nigeria. Int J Africa Nur Sci. (2021) 14:100282. doi: 10.1016/j.ijans.2021.100282
65. Lally, J, Byrne, F, McGuire, E, and McDonald, C. Patient satisfaction with psychiatric outpatient care in a university hospital setting. Ir J Psychol Med. (2013) 30:271–7. doi: 10.1017/ipm.2013.54
66. Corrigan, PW, and Watson, AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. (2002) 1:16–20.
67. Link, BG, Struening, EL, Neese-Todd, S, Asmussen, S, and Phelan, JC. Stigma as a barrier to recovery: the consequences of stigma for the self-esteem of people with mental illnesses. Psychiatr Serv. (2001) 52:1621–6. doi: 10.1176/appi.ps.52.12.1621
68. Yang, H, Deng, Q, Geng, Q, Tang, Y, Ma, J, Ye, W, et al. Association of self-rated health with chronic disease, mental health symptom and social relationship in older people. Sci Rep. (2021) 11:14653. doi: 10.1038/s41598-021-94318-x
69. Mewton, L, and Andrews, G. Poor self-rated health and its associations with somatisation in two Australian national surveys. BMJ Open. (2013) 3:e002965. doi: 10.1136/bmjopen-2013-002965
70. Lacro, JP, Dunn, LB, Dolder, CR, and Jeste, DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. (2002) 63:892–909. doi: 10.4088/JCP.v63n1007
71. Abolfotouh, MA, Al-Assiri, MH, Alshahrani, RT, Almutairi, ZM, Hijazi, RA, and Alaskar, AS. Predictors of patient satisfaction in an emergency care Centre in Central Saudi Arabia: a prospective study. Emerg Med J. (2017) 34:27–33. doi: 10.1136/emermed-2015-204954
72. Renzi, C, Picardi, A, Abeni, D, Agostini, E, Baliva, G, Pasquini, P, et al. Association of dissatisfaction with care and psychiatric morbidity with poor treatment compliance. Arch Dermatol. (2002) 138:337–42. doi: 10.1001/archderm.138.3.337
73. Sran, M, Pyra, T, Chen, L, Holroyd, B, and McCabe, C. P116: a scoping review of factors affecting patient satisfaction with care in North American adult emergency departments. Canadian. J Emerg Med. (2017) 19:S117. doi: 10.1017/cem.2017.318
74. Preyde, M, Crawford, K, and Mullins, L. Patients' satisfaction and wait times at Guelph general hospital emergency department before and after implementation of a process improvement project. Can J Emerg Med. (2012) 14:157–68. doi: 10.2310/8000.2012.110590
75. Renzi, C, Abeni, D, Picardi, A, Agostini, E, Melchi, C, Pasquini, P, et al. Factors associated with patient satisfaction with care among dermatological outpatients. Br J Dermatol. (2001) 145:617–23. doi: 10.1046/j.1365-2133.2001.04445.x
Keywords: service satisfaction, mental health service satisfaction, factors, outpatient, Ethiopia
Citation: Alemu WG, Mwanri L, Due C, Azale T and Ziersch A (2025) Mental health service satisfaction among adults with mental illness attending a psychiatric outpatient clinic: a cross-sectional study. Front. Public Health. 13:1471297. doi: 10.3389/fpubh.2025.1471297
Edited by:
Carolyn Dewa, University of California, Davis, United StatesReviewed by:
Snehil Gupta, All India Institute of Medical Sciences, IndiaTesfaye Engidawu Segon, Mettu University, Ethiopia
Copyright © 2025 Alemu, Mwanri, Due, Azale and Ziersch. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wondale Getinet Alemu, Z2V0aTAwMDFAZmxpbmRlcnMuZWR1LmF1
 Wondale Getinet Alemu
Wondale Getinet Alemu Lillian Mwanri
Lillian Mwanri Clemence Due4
Clemence Due4 Telake Azale
Telake Azale