- 1Department of Nursing, College of Health Science, Mattu University, Mattu, Ethiopia
- 2Armauer Hansen Research Institute, Addis Ababa, Ethiopia
Background: Podoconiosis is non-filarial lymphoedema of the lower extremities. It impairs individuals’ overall lives, including their health, economy, psychology, and social interactions. Podoconiosis is a preventable and effectively manageable disease. The insights and skills of healthcare professionals are vital for the prevention and management of podoconiosis. However, healthcare professionals’ knowledge, attitudes, and practices of podoconiosis management have been poorly studied in Ethiopia.
Objective: The study aimed to assess the healthcare professionals’ knowledge, attitudes, and practices toward podoconiosis management and associated factors in public hospitals in the Ilu Ababor and Buno Bedelle Zones.
Methods: A facility-based cross-sectional study was conducted from December 1, 2022, to January 1, 2023. The data were collected from systematically selected health professionals using a self-administered structured questionnaire. Epi-data and SPSS were used for data entry and analysis, respectively. A binary logistic regression analysis was used to identify factors influencing the outcome variables. In the multivariable analysis, a p-value of ≤0.05 was used to pronounce statistical significance at a 95% confidence interval.
Results: From the total of 399 participants involved, 262 (65.7%) had poor knowledge, 213 (54.3%) had unfavorable attitudes, and 308 (77.2%) had never practiced podoconiosis management. Years of experience, level of education, type of qualification, podoconiosis training, taking courses in education curricula, and attitudes were identified as factors influencing knowledge. The participants’ attitudes were influenced by age, podoconiosis training, receiving technical support, and knowledge. Their practices were significantly affected by age, education level, podoconiosis training, taking podoconiosis courses in educational curricula, and knowledge.
Conclusion: The current study found poor healthcare professionals’ insights and skills in podoconiosis management in the study area. Therefore, concerned bodies need to set up capacity-building training and guidelines for healthcare professionals in the area to boost their knowledge, attitudes, and practice toward podoconiosis management.
Introduction
Podoconiosis is a lymphedema on the lower extremities (foot) that affects a barefoot individual (1). It is the most common cause of tropical lymphedema following lymphatic filariasis (2). It is a non-infectious inflammatory response to the geochemical (smectite, mica, and quartz) substances found in red clay soil (1, 3). The lymphedema can occur on both extremities, however asymmetrical. It is characterized by firm nodules with itching, tingling, and flaring of the forefoot. Moreover, fibrosis, papillomatosis, and nodule-looking moss may be observed (4).
An estimated 4 million people are living with podoconiosis globally, mainly in Africa’s tropical countries, Central and South America, and Southeast Asia. Tropical African countries bear the highest disease burden. In Africa, the disease has been reported in Angola, Burundi, Cameroon, Cape Verde, Chad, the Democratic Republic of Congo, Equatorial Guinea, Ethiopia, Kenya, Madagascar, Mozambique, Niger, Nigeria, Rwanda, São Tomé and Príncipe, Sudan, Tanzania, and Uganda. Podoconiosis has been reported in the Latin American highlands in Brazil, Colombia, Costa Rica, Ecuador, El Salvador, French Guiana, Guatemala, Honduras, Mexico, Peru, and Suriname (5).
Of the 4 million global cases, about 1 million (a quarter of the global load of podoconiosis) are present in Ethiopia. Regionally, its prevalence is higher in the Ilu Ababor Zone (9.1%), Midakegni district of West Shewa Zone (7.4%), Pawe resettlement area (6%), Wolaita Zone (5.5%), Debreelias and Dembecha districts in the Amhara region (3.3%), and Gulliso district of West Wollega Zone (2.8%) (6). A community-based study conducted in the Bedelle district found 5.6% of podoconiosis (7). Geographically, the higher prevalence was observed in the central highlands of Ethiopia, including Amhara, Oromia, and the South Nation, Nationalities, and Peoples (SNNP) regional government. In addition, a higher prevalence was found in the south-western parts of the country (2).
Podoconiosis results in physical disability, psychological trauma, social stigma, and economic unproductivity (8). During acute inflammation, patients may be bedridden and lose economic productivity. Evidence shows that podoconiosis patients lose about 45% of their economic productivity (9). Despite its effect on an individual’s health and productivity and a country’s cumulative economy, the disease has received poor attention from both local and global communities (10).
The healthcare providers’ insights and skills equip them in the prevention and management of podoconiosis. However, different evidence showed that the healthcare providers had inadequate knowledge, a negative attitude, and poor practice toward podoconiosis management (11–13). Poor healthcare providers’ attitudes toward podoconiosis could result in stigma, compromise the quality of care, and overrun patients’ beliefs (14). Local evidence shows healthcare providers’ stigmatizing views and unfavorable attitudes toward podoconiosis management. For instance, a study conducted in northern Ethiopia found healthcare providers’ stigmatizing views toward patients with podoconiosis (12). Another study conducted in the Gamo Zone of southern Ethiopia revealed 44% unfavorable attitudes among healthcare providers (13). A study conducted by Yakob B. also revealed that less than one-half of healthcare providers had unfavorable attitudes (15). However, a study conducted in Rwanda revealed better (86.1% positive) attitudes toward podoconiosis management (11). Regarding podoconiosis management practices, the same study from Rwanda revealed that 6% of healthcare providers have ever managed podoconiosis cases (4). A study by Dellar et al. found healthcare providers’ poor practices in podoconiosis management (12). In the studies conducted in southern Ethiopia, 11.6 and 36% of healthcare providers ever managed patient with podoconiosis (13, 15).
The knowledge, attitude, and practice of podoconiosis management are affected by different sociodemographic and facility-related factors. The knowledge of podoconiosis management was significantly influenced by age, sex, type of profession, service year or experience of the provider, and the type of facility (private or public) (13, 15). Similar to factors influencing the knowledge of knowledge of podoconiosis management, the providers’ age, sex, knowledge of podoconiosis management, type of profession, ever managed podoconiosis, and type of health facility were found to be factors significantly affecting the attitudes toward podoconiosis management (13, 16, 17). The podoconiosis management practices were significantly affected by the sex of the provider and knowledge of podoconiosis (13).
Although the occurrence of podoconiosis in southwest Ethiopia, particularly in the Ilu Ababor and Buno Bedelle Zones, is higher, the knowledge, attitudes, and practices of podoconiosis have not been studied so far in the area. Hence, this study aimed at assessing the healthcare professionals’ knowledge, attitude, and practice of podoconiosis management and associated factors in public hospitals in Ilu Ababor and Buno Bedelle Zones, Southwest Ethiopia. The findings of this study could benefit the concerned bodies in endorsing and strengthening intervention strategies such as podoconiosis case management training for the healthcare professionals in the area.
Materials and methods
Study design, period, and area
A facility-based cross-sectional study was conducted in the public hospitals of Ilu Abba Bor and Buno Bedelle Zones. The study was executed in the period from December 1, 2022, to January 1, 2023. The two zones have an area of 15,135.33 square kilometers covered with 272,555 households. An estimated total of 2,271,609 people were living in the study area. Of these, about 636,986 and 634,623 men and women, respectively. The Ilu Ababor and Buno Bedelle Zones are the 20 Zones of the Oromia Regional State located in Southwest Ethiopia. The Ilu Ababor Zone has one referral [Mettu Karl Comprehensive Specialized Hospital (MKCSH)] and one district (Darimu Primary Hospital) hospital. These hospitals service communities of Southwest Ethiopia, including the Oromia Regional State, Gambella Regional State, Sheka, and Bench Maji Zones of Southwest Ethiopia Regional State. The MKCSH also serves as a pre- and in-services training center in the region. The Buno Bedlee Zone has three hospitals, including Bedelle General Hospital, Chora Primary Hospital, and Danbi Primary Hospital. A total of 451 healthcare professionals were working in the study area during the study period.
Study participant selection and eligibility criteria
All randomly selected healthcare professionals who were working in the selected healthcare facilities and who lived for at least 6 months in the study area were included in this study. However, healthcare professionals who were not available (on annual, maternal, or sick leave) during the study period were excluded from this study.
Sample size estimation and sampling procedure
A single population proportion formula , was used to estimate the sample size, assuming a 95% confidence level, a 5% margin of error, a 40% population proportion (P) taken from a study conducted in Gamo Zone (13), and a 10% non-response rate. A final sample size of 406 was used in this study.
Then the sample was proportionally allocated to each of the five public hospitals (MKCSH, Darimu Primary Hospital, Bedelle General Hospital, Chora Primary Hospital, and Didesa Primary Hospital) in the Ilu Ababor and Buno Bedelle Zones. The study participants were selected using a simple random sampling technique from each selected hospital (Table 1).
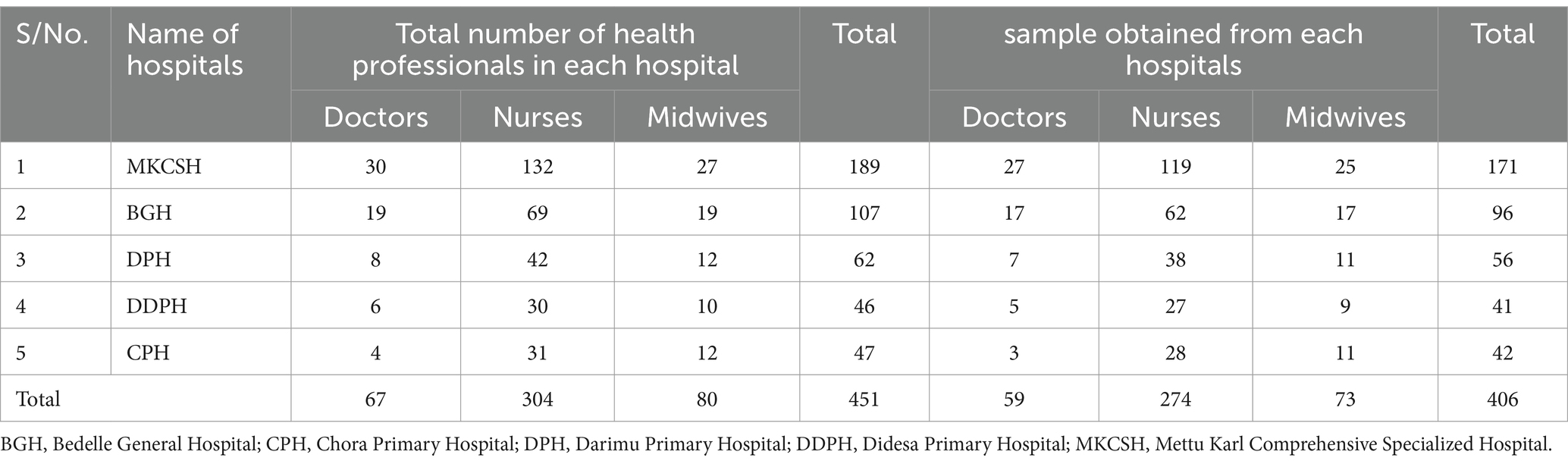
Table 1. Proportional allocation of the sample size to hospitals in Ilu Ababor and Buno Bedelle Zones, Southwest Ethiopia.
Study variables and outcome interest
Healthcare professionals’ knowledge, attitudes, and practices of podoconiosis management were the outcomes of this study. Sociodemographic factors (age, sex, salary, and marital status), profession-related factors (knowledge of podoconiosis, training on podoconiosis, type of profession, service year, level of education, job position, and having taken a course or topic about podoconiosis), and facility-related factors (level of the hospital and presence of management guidelines or manuals) were independent variables included in this study.
Operational definitions
• Knowledge of podoconiosis management
• Good knowledge: Participants who score 75% or more of the knowledge question.
• Poor knowledge: Participants who score less than 75% of the knowledge questions (13).
• Attitude toward podoconiosis management
• Favorable attitude: Participants who score 75% or more of attitude questions.
• Unfavorable attitude: Participants who score below the 75% of attitude questions (13).
• Practice toward podoconiosis management
• Practicing: Those participants who had ever treat podoconiosis patient.
• Not practicing: Those participants who had never treated podoconiosis patient (13).
Data collection instrument, procedure, and quality assurance
A structured, self-administered questionnaire was distributed to the selected participants. The questionnaire was adapted from a previous similar study conducted in southern Ethiopia (13). It contains five sections, including the participants’ sociodemographic information, participants’ knowledge of podoconiosis management among health professionals, participants’ attitudes toward podoconiosis management, participants’ podoconiosis management practices, and professional and facility-related information. Five BSc and two MSc-holder nurse professionals executed the data collection and supervision, respectively.
To ensure data quality, a pre-test was conducted among 5% of the sampled population. It was conducted 2 weeks before the actual data collection date at Gambella General Hospital. Then necessary amendments were made to the questionnaire based on the pre-test results. Data collectors and supervisors were given a one-day training regarding the study’s objectives, benefits, and participants’ rights. A daily check-up for data completeness and consistency was conducted during the data collection period.
Statistical analysis
The collected data were coded and entered into Epi-data version 3.1. Then the data were exported to SPSS version 27.0 for analysis. Data cleaning and missed values were checked before analysis. The computed descriptive statistics were presented using text narrations, frequency tables, proportions, and graphs. The factors influencing knowledge, attitudes, and practice of podoconiosis management were tested using a binary logistic regression analysis. A variance inflation factor (VIF) analysis was conducted to assess multicollinearity. The bivariable analysis identified the candidate variables at a p-value of less than 0.25. The variables with a p-value of less than 0.05 in the multivariable analysis were considered statistically significant at a 95% confidence interval (CI). The adjusted odds ratio was used to show the magnitude and direction of statistical associations. The Hosmer-Lemeshow goodness-of-fit test was used to select the fitting model.
Results
Sociodemographic characteristics of participants
A total of 399 participants responded to the distributed (406 questionnaires), which gives a 98.2% response rate. About 218 (54.6%) of participants were between the ages of 25 and 35, with a mean (±SD) age of 31.73 (±6.31). More than two-thirds (271, 67.9%) of participants were nurses. About 153 (38.3%) of participants had 1–5 years of work experience. More than half (213, 53.4%) of the participants were earning a net salary of 5,000–10,000 Ethiopian Birr (ETB; Table 2).
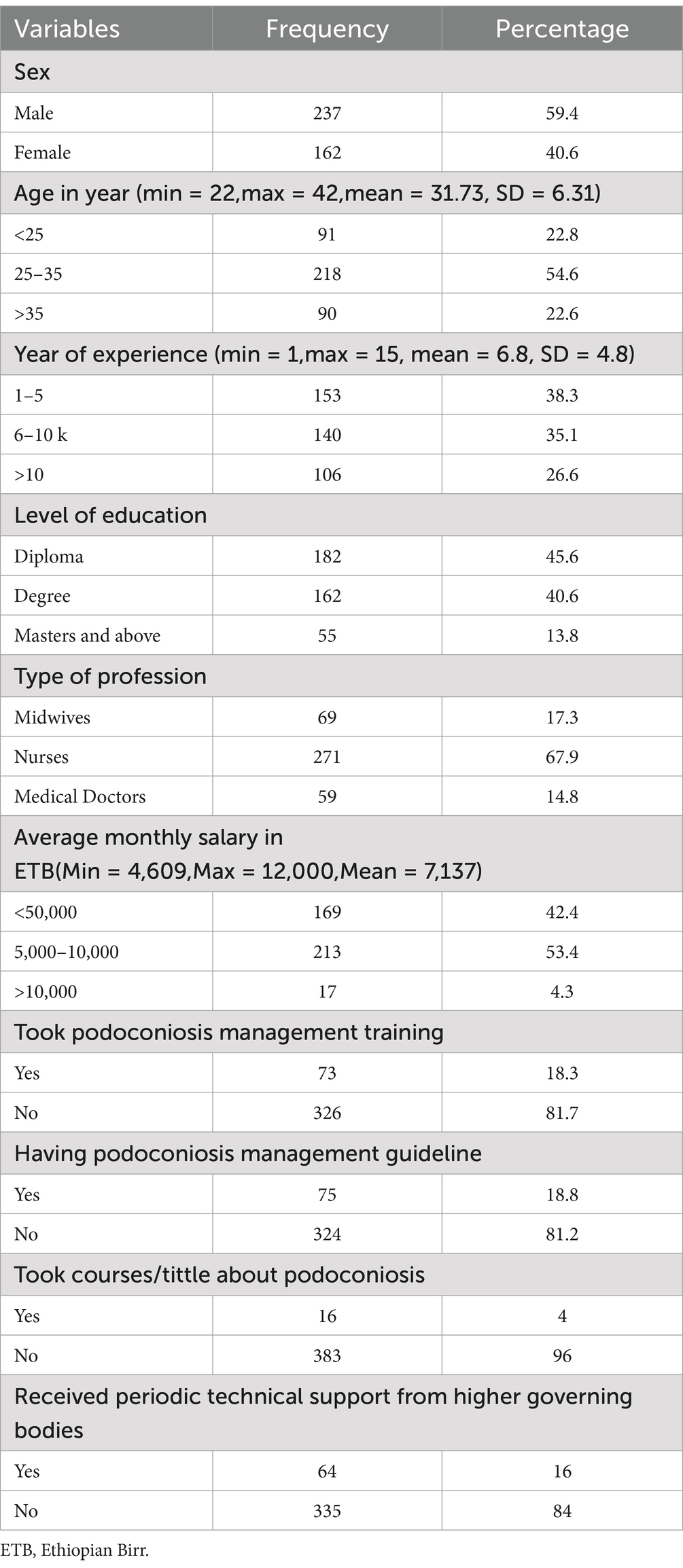
Table 2. Sociodemographic characteristics of healthcare professionals in Ilu Ababor and Buno Bedelle Zones, Southwest Ethiopia (n = 399).
Participants’ knowledge of podoconiosis management
About two-thirds (262, 65.7%) of participants had poor knowledge of podoconiosis management. About 150 (37.59%) of participants answered that podoconiosis is transmitted by contact with soil. About 160 (40%) stated avoiding walking barefoot in the cold as the means of podoconiosis prevention. The majority (364, 91.2%) of participants believed podoconiosis is a treatable disease (Table 3).
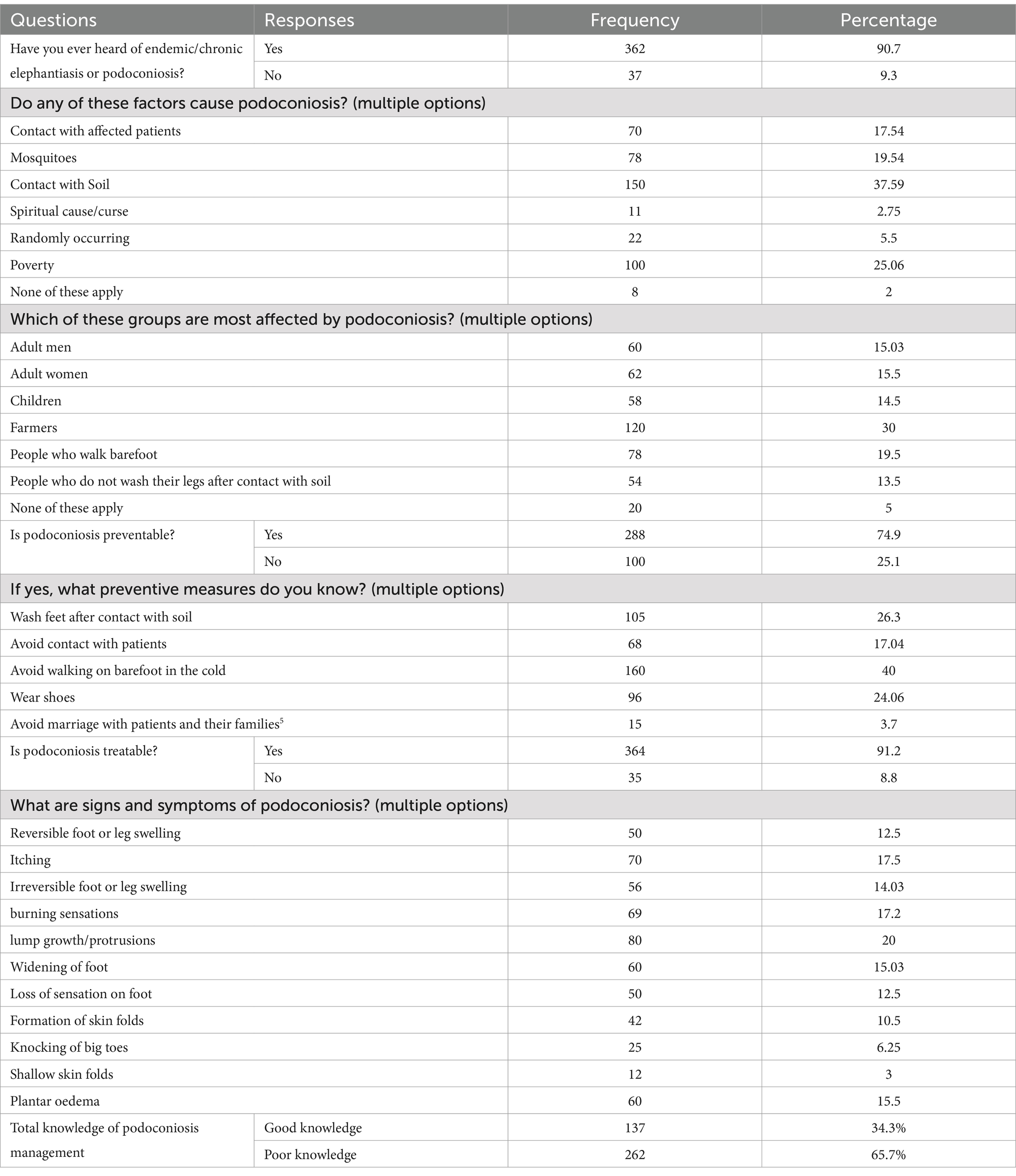
Table 3. Participants’ knowledge of podoconiosis management questions in Ilu Ababor and Buno Bedelle Zones, Southwest Ethiopia.
Participants’ attitudes toward podoconiosis management
More than half (213, 54.3%) of participants had unfavorable attitudes toward podoconiosis management. About 313 (78.4%) participants believed podoconiosis patients deserved love and support. The majority (346, 86.7%) of participants believed that people with podoconiosis deserved treatment and care (Table 4).
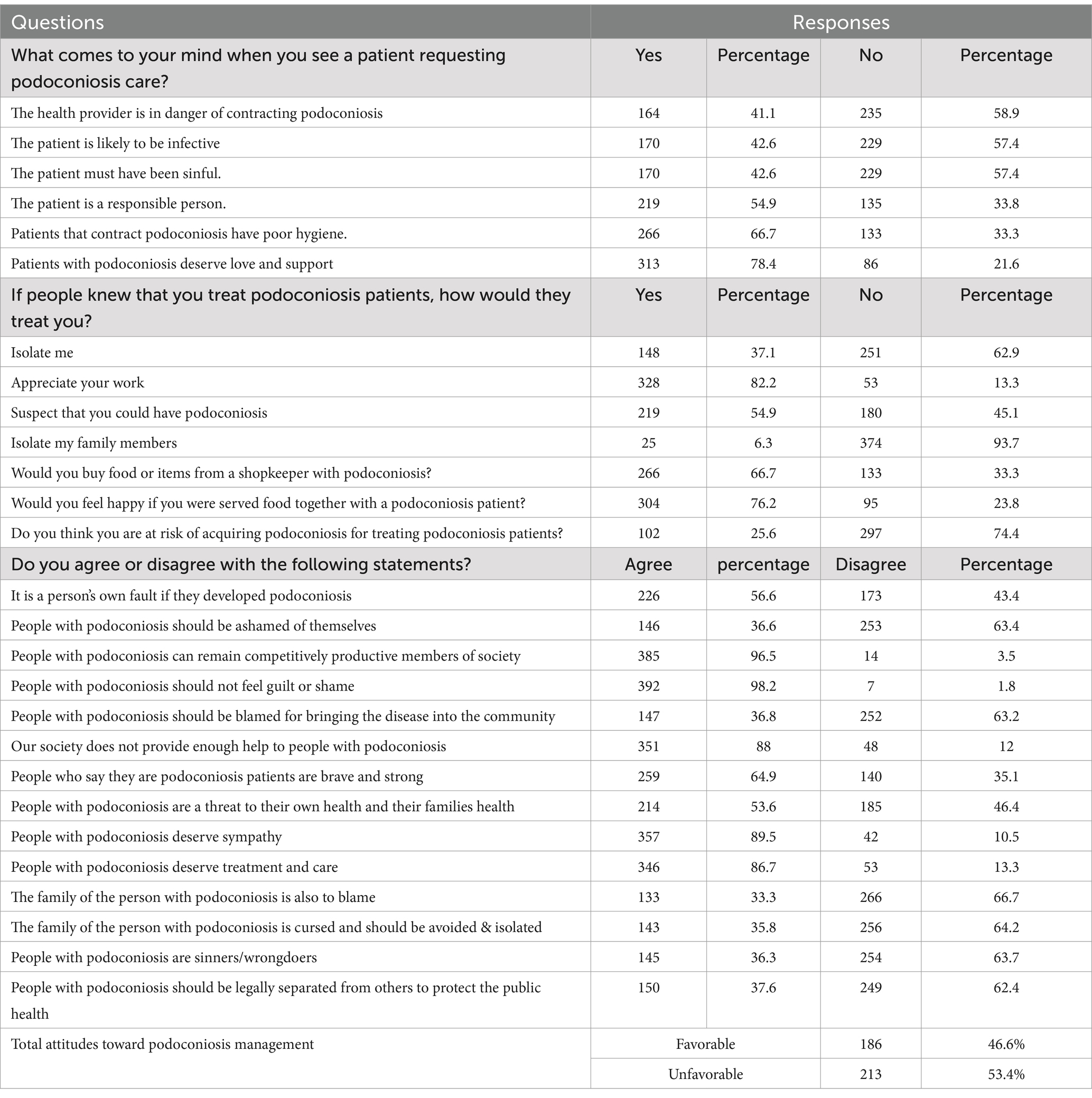
Table 4. Participants’ attitudes toward podoconiosis management questions in Ilu Ababor and Buno Bedelle Zones, Southwest Ethiopia.
Participants’ podoconiosis management practices
More than three-fourths (308, 77.2%) of participants did not ever practice podoconiosis. Of those who ever treated podoconiosis patients, only 62 (15.5%) perceived they were confident in delivering services to podoconiosis patients. More than two-thirds (270, 67.6%) of participants mentioned the unavailability of drugs and supplies as the challenges they faced while treating podoconiosis patients (Table 5).
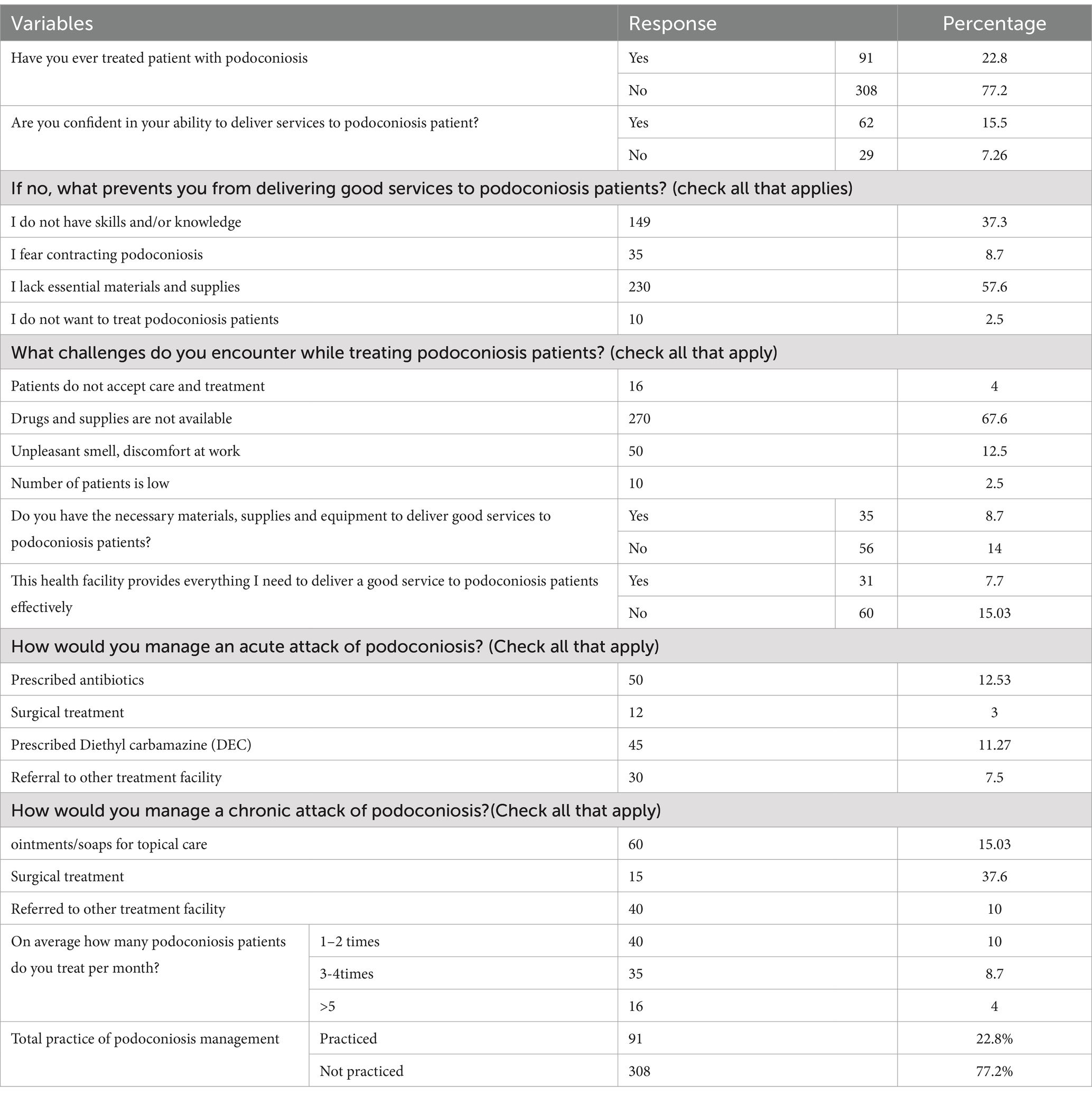
Table 5. Participants’ podoconiosis management practices in Ilu Ababor and Buno Bedelle Zones, Southwest Ethiopia.
Factors associated with participants’ knowledge of podoconiosis management
Participants with more than 10 years of work experience were more than twofold [adjusted odds ratio (AOR): 2.2; 95% CI: 1.13–4.27] more knowledgeable than those with 1–5 years of work experience. Participants who had masters and above were nearly five [AOR: 4.8; 95%CI: 2.12–10.97] times more likely to be knowledgeable than those who had diplomas. Participants with medical doctor qualifications were more than fivefold [AOR: 5.3; 95%CI: 2.10–13.82] more likely to be knowledgeable than midwives. Participants who took podoconiosis training were about twofold [AOR: 2.1; 95%CI: 1.1–4.1] more likely to be knowledgeable compared to their counterparts. Participants who took podoconiosis management courses or titles in their educational curricula had a more than threefold [AOR: 3.6; 95%CI: 1.09–12.36] likelihood of having good knowledge of podoconiosis management. Moreover, participants with favorable attitudes toward podoconiosis management had a sevenfold [AOR: 7.1; 95%CI: 4.22–12.19] higher probability of having good knowledge compared to those with unfavorable attitudes (Table 6).
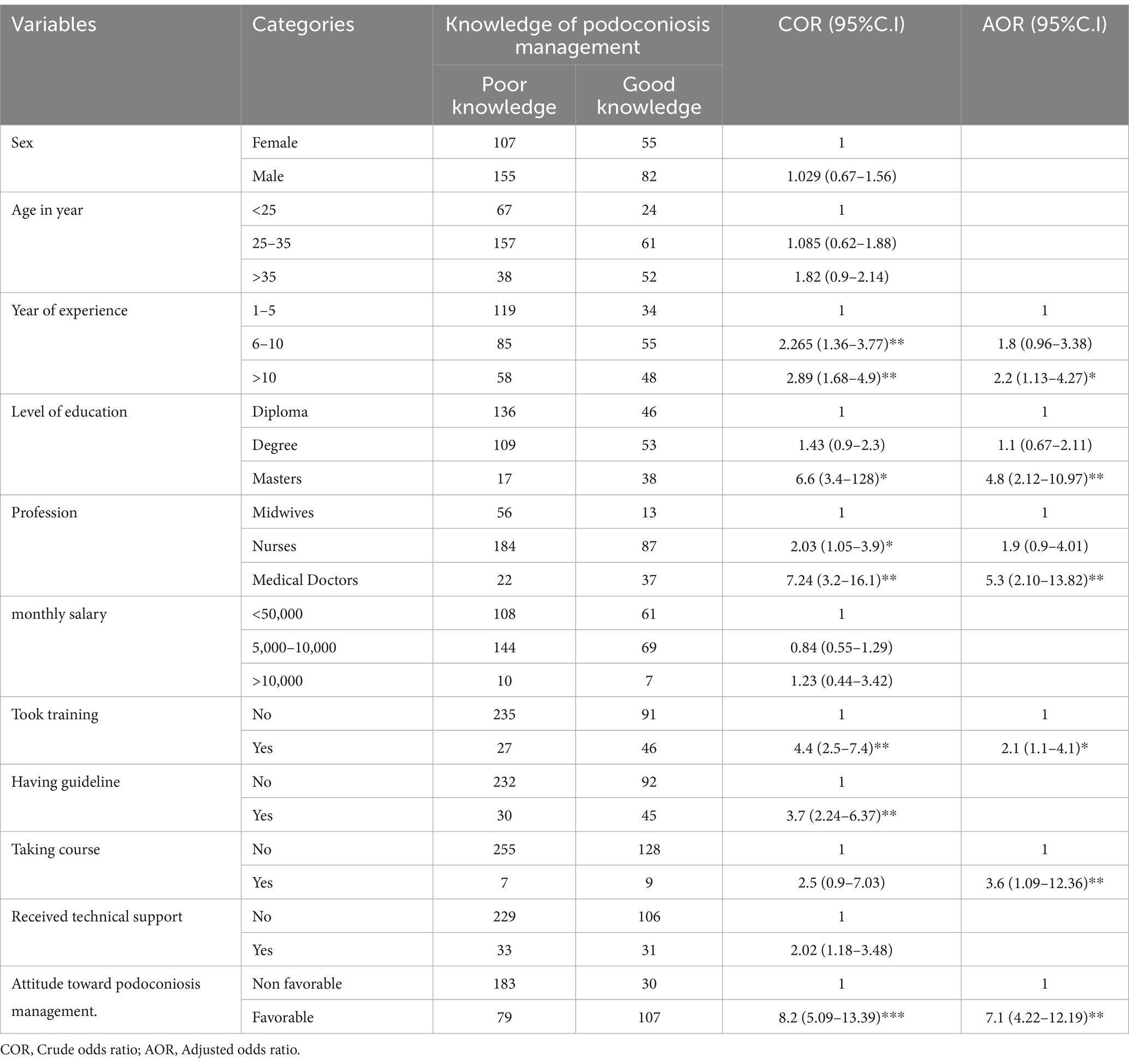
Table 6. Factors associated with participants’ knowledge of podoconiosis management in Ilu Ababor and Buno Bedelle Zones, Southwest Ethiopia.
Factors associated with participants’ attitudes toward podoconiosis management
In this study, participants above 35 were 1.5 [AOR: 1.5; 95%CI: 1.13–3.52] times more likely to have favorable attitudes toward podoconiosis management than those under 25. The probability of having favorable attitudes was about six fold [AOR: 5.9; 95%CI: 1.1–13] higher among participants who had podoconiosis training than their counterparts. Participants who received technical support had nearly two [AOR: 1.8; 95%CI: 1.1–3.2] times higher likelihood of unfavorable attitudes than those who had not received technical support. In addition, participants with good knowledge of podoconiosis management had a nearly eightfold [AOR: 7.7; 95%CI: 4.6–12] higher likelihood of having favorable attitudes (Table 7).
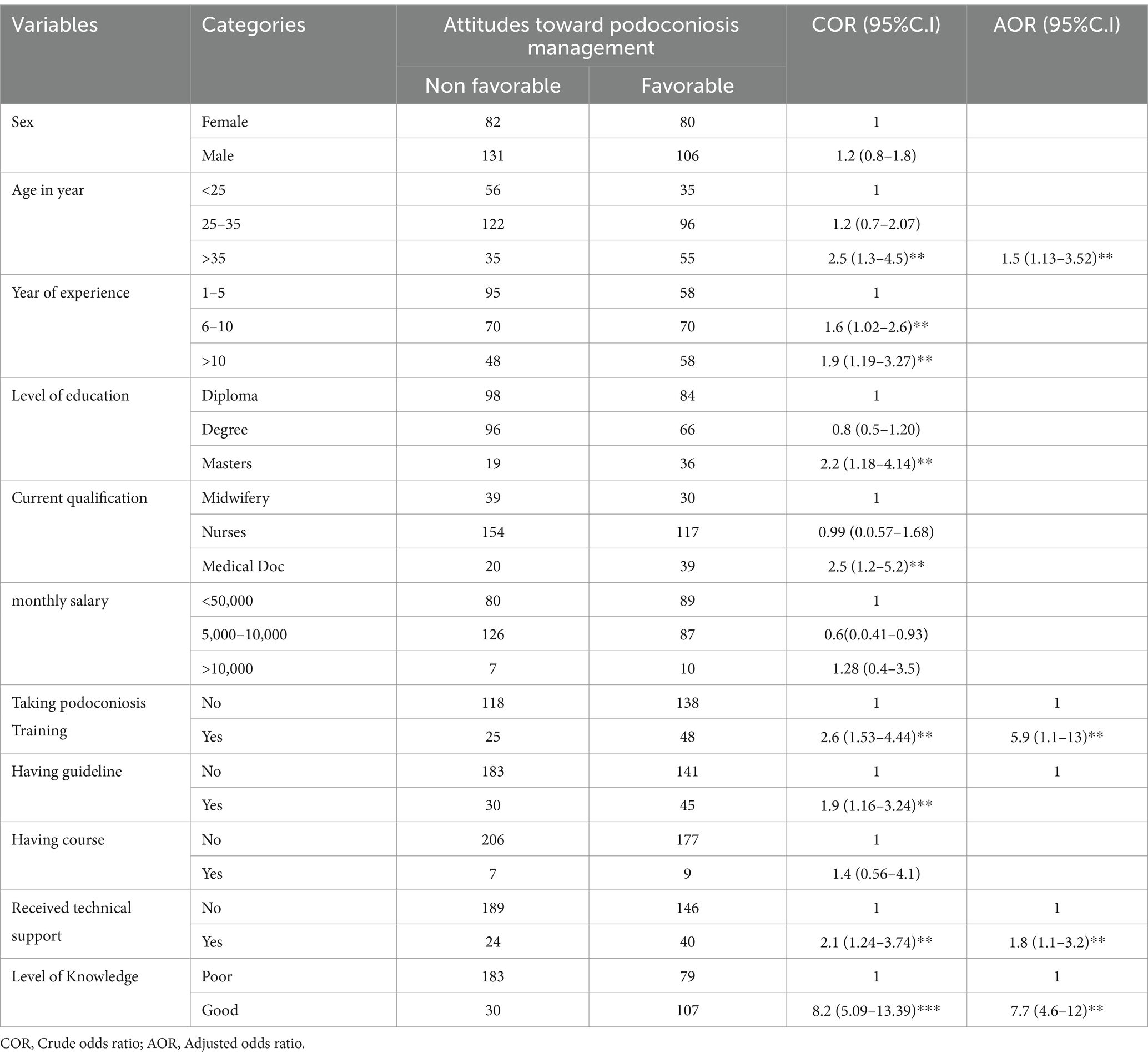
Table 7. Factors associated with participants’ attitudes toward podoconiosis management in Ilu Ababor and Buno Bedelle Zones, Southwest Ethiopia.
Factors associated with participants’ podoconiosis management practices
Participants above 35 were three [AOR: 3.05; 95%CI: 1.35–6.90] times more likely to practice podoconiosis management than those under 25. Participants who had master’s degrees and above were more than two [AOR: 2.4; 95%CI: 1.07–5.48] times more likely to practice podoconiosis management than those who had diplomas. Participants who took podoconiosis training were more than three [AOR: 3.6; 95%CI: 1.81–7.45] times more likely to practice podoconiosis management than their counterparts. Participants who took podoconiosis courses or titles in educational curricula were about threefold [AOR: 3.1; 95%CI: 1.2–10.61] more likely to practice podoconiosis management than those who had not taken the course in their current education. In addition, participants with good knowledge of podoconiosis were twofold [AOR: 2.3; 95%CI: 1.27–4.12] more likely to practice podoconiosis management than their counterparts (Table 8).
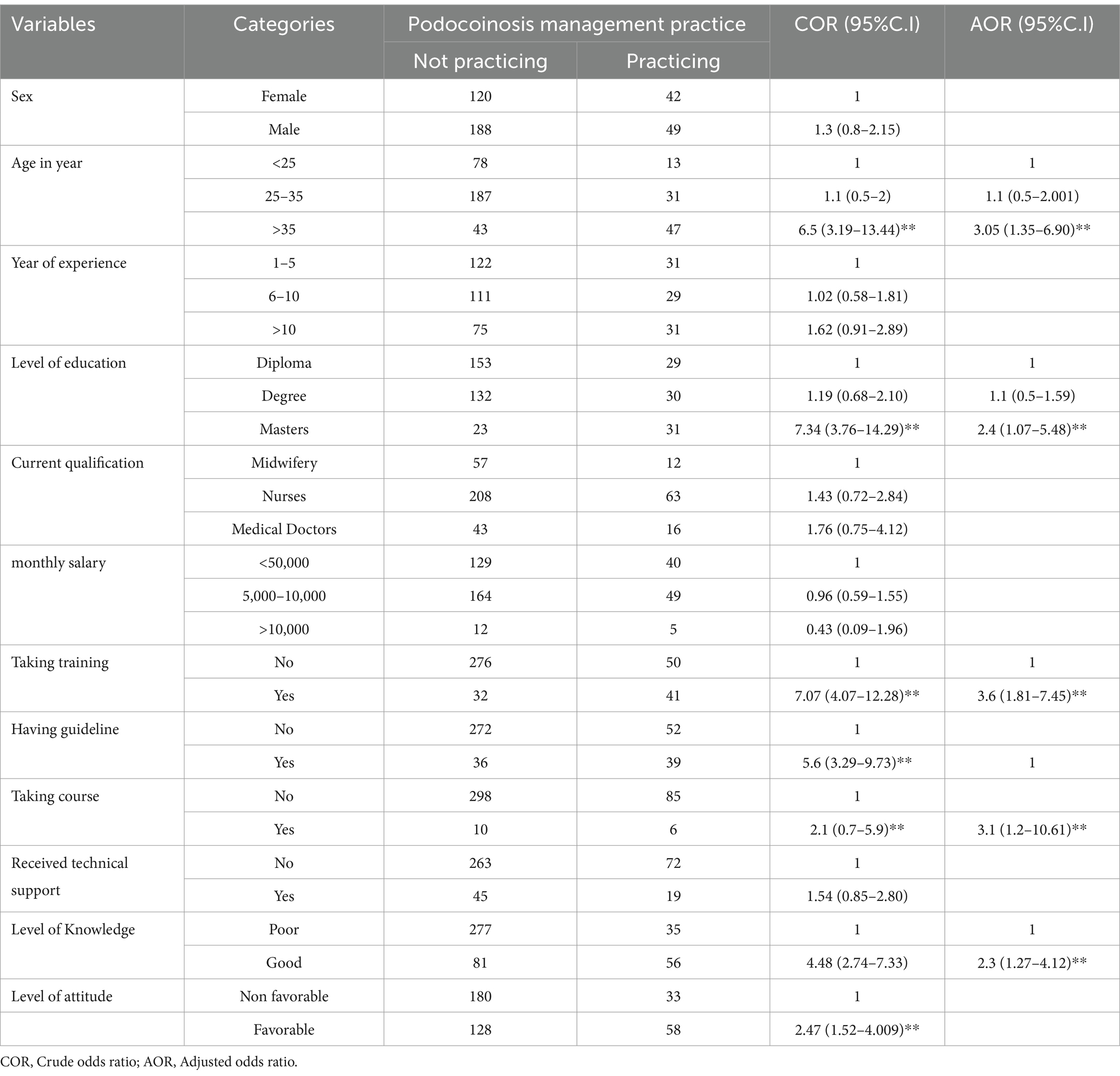
Table 8. Factors associated with participants’ podoconiosis management practices in Ilu Ababor and Buno Bedelle Zones, Southwest Ethiopia.
Discussion
The present study aimed to assess the participant’s knowledge, attitude, and practice toward podoconiosis management and associated factors in the Ilu Ababor and Buno Bedelle Zones of southwest Ethiopia. About 65.7% of healthcare professionals had poor knowledge of podoconiosis. The current study reveals a higher level of poor knowledge about podoconiosis than a Rwandan study (11). This variation could be related to the differences in health education curricula, training accessibility, and technical support for healthcare professionals in the two countries. However, the current proportion of poor knowledge of podoconiosis is congruent with the previous findings from the Gamo (13) and Wolaita (15) Zones. It might be associated with a lack of pre- and in-service training about podoconiosis. Therefore, pre- and in-service training should be given to improve health professionals’ podoconiosis management knowledge.
In the current study, years of experience were significantly associated with knowledge of podoconiosis management. The odds of podoconiosis management knowledge were 2.2 times higher among participants with more than 10 years of experience than those with 1 to 5 years of experience. This was a plausible finding because knowledge of a certain disease condition increases as years of experience increase because of repeated exposure to different case management in clinical settings. This finding was supported by a study conducted in Gamo Zone (13). However, this association was not supported by a study finding from the Wolaita Zone, southern Ethiopia (15). Level of education was another factor that showed a significant association with knowledge of podoconiosis management in this study. Participants who studied for master’s degrees had 4.8 times higher odds of podoconiosis management knowledge than those with diploma certificates. This association was a novel and has not been supported by earlier literature. The finding was based on the fact that the knowledge level increases with education. It could also be due to the variations in the contents of the curriculum at different levels of degrees. In a previous study, public health officers, BSc nurses, and diploma nurses had a higher probability of having good podoconiosis management knowledge than other healthcare professions (13). However, medical doctors had more than fivefold odds of good knowledge of podoconiosis management in this study. This could be related to the curriculum variations among the healthcare professional educations in the country. Participants who took training had two times the odds of podoconiosis management knowledge than their counterparts. The training was not significantly associated with knowledge of podoconiosis management in a previous study (13). Pre- and in-service training are crucial in boosting the knowledge and skills of healthcare professionals in case management. Healthcare professionals who learned podoconiosis in course materials had a 3.6 times higher probability of having good knowledge of podoconiosis management. This could be due to recalling the previous knowledge of podoconiosis. Since this was a novel attribute of this study, no previous evidence supported it. Participants who had favorable attitudes toward podoconiosis management had sevenfold higher odds of podoconiosis management knowledge compared to their counterparts. This significant association was also found in a study conducted in the Gamo Zone (13).
The study identified healthcare professionals’ attitudes toward podoconiosis management. Accordingly, more than half (53.4%) of the healthcare professionals had an unfavorable attitude. This finding is comparable to a finding from northern Ethiopia, where healthcare provides stigmatizing views toward podoconiosis patients (12). However, it is higher compared to a study by Yakob B. et al., where about 48% of healthcare professionals had unfavorable attitudes (15). The current proportion is higher than that of the proportion found in the Gamo Zone, where around 44% of healthcare professionals had an unfavorable attitude (13). Moreover, the healthcare providers’ unfavorable attitude in the area was more than threefold higher than in Rwanda’s finding, where only 13.9% had an unfavorable attitude (11). This variation could be associated with a lack of podoconiosis management training for the professionals in the study setting.
Healthcare professionals who were under 25 years old had 1.5 times higher odds of a favorable attitude toward podoconiosis management compared to those who were 35 years and older. This is a brand-new discovery that has not been corroborated by earlier literature. The likelihood of having a positive attitude was around six times higher among healthcare professionals with training than their counterparts. Previous literature did not provide evidence for this. The training improves the attitudes toward the phenomenon. Receiving technical support was also demonstrated to have a strong correlation with a favorable attitude toward podoconiosis management. As a result, compared to healthcare workers who did not receive technical support, those who did had roughly two-fold higher odds of having favorable attitudes toward podoconiosis management. In addition, the podoconiosis management knowledge of healthcare professionals was identified as a significant factor affecting the professionals’ attitudes. Healthcare professionals who had good knowledge of podoconiosis management had nearly eight-fold higher likelihood of having a favorable attitude. This finding asserts that a higher level of knowledge about a certain phenomenon increases the attitude toward the condition.
In this study, more than three-fourths (77.20%) of healthcare professionals were not practicing podoconiosis management. The practice proportion found in this study is higher than the previous finding from the Wolaita Zone, where 64% of healthcare providers did not practice podoconiosis management (15). However, the current proportion is lower than a finding from Rwanda, where only 94% of the healthcare professionals did not practice podoconiosis management (11). This difference might be related to the variations in the distribution of podoconiosis cases in the two countries, health service coverage, and availability of in-service and pre-service training.
Participants whose age was 35 years and above were three times more likely to practice podoconiosis management compared to those whose age was less than 25 years. This finding agrees with the findings of the Gamo and Wolaita Zones (13, 15). This could be due to healthcare professionals’ increased exposure to podoconiosis patients for a long period of time. Educational status was found to be another factor affecting professionals’ podoconiosis management practice. Participants who held master’s degrees had a roughly twofold higher chance of practicing podoconiosis management than those who held diplomas. This association is similar to the truth that a higher level of education leads to higher practice competence. Participants who took training had about 3.6 times higher probability of practicing podoconiosis management than those who did not take training. This finding was supported by a study conducted by Churko et al. (13). Participants who took podoconiosis courses in their curriculum had threefold higher odds of practicing podoconiosis management than their counterparts. Moreover, participants with good knowledge of podoconiosis management had a twofold higher likelihood of practicing podoconiosis management than those with poor knowledge. This finding is consistent with a study by B. Yakob et al. (15).
Limitations of the study
The distribution of self-administered questionnaires could be subject to response bias from each respondent. Since the study utilized a cross-sectional design, it could not assert a temporal relationship between the outcome and explanatory variables. Moreover, these qualitative findings could not explore possible sociocultural barriers to podoconiosis management.
Conclusion
Podoconiosis is a neglected disease both in a local and global context. Although podoconiosis cases are prevalent in the study area, the healthcare professionals’ knowledge, attitudes, and practice of podoconiosis management were found to be poor. Given that building the capacity of healthcare professionals is crucial to the prevention and treatment of podoconiosis, the concerned bodies, including the federal and regional health bureaus and other non-governmental organizations, should endorse podoconiosis training opportunities and provide podoconiosis management guidelines to the healthcare professionals. The Ministry of Education, in collaboration with the Ministry of Health, shall also include podoconiosis in the educational curricula. At the individual level, healthcare professionals should struggle to improve their knowledge and skills in managing podoconiosis patients. Moreover, researchers in the field need to undertake follow-up studies and explore further contributors to healthcare professionals’ inadequacies in podoconiosis management.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The study was conducted according to Helsinki’s ethical principles. First, the ethical clearance letter (Ref. No. RPG/280) was obtained from the Research Ethics Review Committee of the College of Health Sciences, Mattu University. Then, a letter of cooperation was submitted to each public hospital in the study area. Each study participant signed an informed consent after being fully informed about the study’s aim, benefit, and risk. No identifier was included in the questionnaire, and we collected data to ensure the participant’s information was kept confidential.
Author contributions
ST: Conceptualization, Formal analysis, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – original draft. YL: Data curation, Funding acquisition, Methodology, Project administration, Supervision, Visualization, Writing – original draft. KB: Conceptualization, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft. BA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Supervision, Visualization, Writing – original draft, Writing – review & editing. AD: Data curation, Formal analysis, Investigation, Methodology, Resources, Supervision, Validation, Writing – review & editing. YN: Formal analysis, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft. WG: Data curation, Formal analysis, Methodology, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study funded by Mattu University (Budget release Ref. no: MaU/120/43).
Acknowledgments
We thank Mattu University for releasing the budget to execute this study. We also thank the hospital staff for their support and cooperation during the study. We are also grateful for the study participants, supervisors, and data collectors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1454979/full#supplementary-material
References
1. Deribe, K, Kebede, B, Tamiru, M, Mengistu, B, Kebede, F, Martindale, S, et al. Integrated morbidity management for lymphatic filariasis and podoconiosis, Ethiopia. Bull World Health Organ. (2017) 95:652–6. doi: 10.2471/BLT.16.189399
2. Deribe, K, Brooker, SJ, Pullan, RL, Sime, H, Gebretsadik, A, Assefa, A, et al. Epidemiology and individual, household and geographical risk factors of podoconiosis in Ethiopia: results from the first nationwide mapping. American J Tropical Med Hygiene. (2015) 92:148–58. doi: 10.4269/ajtmh.14-0446
3. Kebede, B, Martindale, S, Mengistu, B, Kebede, B, Mengiste, A, H/Kiros, F, et al. Integrated morbidity mapping of lymphatic filariasis and podoconiosis cases in 20 co-endemic districts of Ethiopia. PLoS Negl Trop Dis. (2018) 12:e0006491. doi: 10.1371/journal.pntd.0006491
4. Bekele, K, Deribe, K, Amberbir, T, Tadele, G, Davey, G, and Samuel, A. Burden assessment of podoconiosis in Wayu Tuka woreda, east Wollega zone, western Ethiopia: a community-based cross-sectional study. BMJ Open. (2016) 6:e012308. doi: 10.1136/bmjopen-2016-012308
5. Tasew, FS. Podoconiosis, the non-filarial elephantiasis, a means of discrimination and poverty in Ethiopia. American J Biomedical and Life Sci. (2015) 3:67–70. doi: 10.11648/j.ajbls.20150303.17
6. Health FDRoEMo. Of Ethiopia National Master Plan for neglected tropical diseases. Ethiopia: Federal Ministry of Health Ethiopia Addis Ababa (2016). e0006491 p.
7. Tekola Ayele, F, Alemu, G, Davey, G, and Ahrens, C. Community-based survey of podoconiosis in Bedele Zuria woreda, West Ethiopia. Int Health. (2013) 5:119–25. doi: 10.1093/inthealth/iht003
8. Semrau, M, Davey, G, Beng, AA, Ndongmo, WPC, Njouendou, AJ, Wanji, S, et al. Depressive symptoms amongst people with podoconiosis and lower limb lymphoedema of other cause in Cameroon: a cross-sectional study. Tropical Med Infectious Dis. (2019) 4:102. doi: 10.3390/tropicalmed4030102
9. Tekola, FH, Mariam, D, and Davey, G. Economic Costs of Endemic Non-filarial Elephantiasis in Wolaita Zone, Ethiopia. Trop Med Int Health. (2006) 11:1136–44. doi: 10.1111/j.1365-3156.2006.01658.x
10. Deribe, K, Cano, J, Giorgi, E, Pigott, DM, Golding, N, Pullan, RL, et al. Estimating the number of cases of podoconiosis in Ethiopia using geostatistical methods. Wellcome Open Res. (2017) 2:2. doi: 10.12688/wellcomeopenres.12483.2
11. Bayisenge, U, Schurer, J, Wong, R, Amuguni, H, and Davey, G. Podoconiosis in Rwanda: knowledge, attitudes and practices among health professionals and environmental officers. PLoS Negl Trop Dis. (2020) 14:e0008740. doi: 10.1371/journal.pntd.0008740
12. Dellar, R, Ali, O, Kinfe, M, Tesfaye, A, Fekadu, A, Davey, G, et al. Knowledge, attitudes and practices of health professionals towards people living with lymphoedema caused by lymphatic filariasis, podoconiosis and leprosy in northern Ethiopia. Int Health. (2022) 14:530–6. doi: 10.1093/inthealth/ihab067
13. Churko, C, Asnakew Asfaw, M, Tunje, A, Girma, E, and Zerdo, Z. Knowledge, attitude, practice and associated factors of health professionals towards podoconiosis in Gamo zone, Ethiopia, 2019. J Foot and Ankle Res. (2021) 14:1–10. doi: 10.1186/s13047-021-00464-w
14. Yakob, B, Deribe, K, and Davey, G. High levels of misconceptions and stigma in a community highly endemic for podoconiosis in southern Ethiopia. Trans R Soc Trop Med Hyg. (2008) 102:439–44. doi: 10.1016/j.trstmh.2008.01.023
15. Yakob, B. Assessment of Knowledge, Attitudes and Practices of Community and Health Professionals towards Podoconiosis in Wolaita Zone, Southern Ethiopia (Doctoral dissertation, Addis Ababa University). (2007).
16. Yakob, B, Deribe, K, and Davey, G. Health professionals' attitudes and misconceptions regarding podoconiosis: potential impact on integration of care in southern Ethiopia. Trans R Soc Trop Med Hyg. (2010) 104:42–7. doi: 10.1016/j.trstmh.2009.07.021
Keywords: podoconiosis, management, healthcare professionals, Ilu Ababor, Southwest Ethiopia
Citation: Tamiru S, Lulu Y, Bidira K, Amsalu B, Duguma A, Nigusu Y and Gezimu W (2025) Healthcare professionals’ knowledge, attitudes, and practice of podoconiosis management and associated factors in public hospitals in Ilu Ababor and Buno Bedelle zones, Southwest Ethiopia: a cross-sectional study. Front. Public Health. 13:1454979. doi: 10.3389/fpubh.2025.1454979
Edited by:
Pier Luigi Sacco, University of Studies G. d’Annunzio Chieti and Pescara, ItalyReviewed by:
Manuel Ritter, University Hospital Bonn, GermanyMarianyoly Ortiz Ortiz, Puerto Rico Science, Technology & Research Trust, Puerto Rico
Abdallah Ngenya, National Institute of Medical Research, Tanzania
Copyright © 2025 Tamiru, Lulu, Bidira, Amsalu, Duguma, Nigusu and Gezimu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wubishet Gezimu, d3ViaXNoZXQxNTFAZ21haWwuY29t
†ORCID: Wubishet Gezimu, orcid.org/0000-0002-5503-1360
 Sanbato Tamiru
Sanbato Tamiru Yohanis Lulu1
Yohanis Lulu1 Abdissa Duguma
Abdissa Duguma Yared Nigusu
Yared Nigusu Wubishet Gezimu
Wubishet Gezimu