- Affiliated Mental Health Center of Jiangnan University, Wuxi Central Rehabilitation Hospital, Wuxi, Jiangsu, China
Objective: This study aimed to explore the participation of patients with severe mental disorders in community health service management and its influencing factors in Wuxi.
Methods: The data of patients with severe mental disorders were extracted from the Jiangsu Provincial Management System between 2019 and 2021. The participation of patients in community health service management was analyzed. A univariate stratified analysis will be used to assess the impact of various factors on inclusion in community management. Logistic regression modeling will be employed to identify influencing factors. Ultimately, negative factors affecting participation in community health management will be identified, followed by targeted qualitative analysis through interviews.
Results: A total of 27,977 individuals were included in the analysis, with 25,744 participants enrolled in community health service management, resulting in a management rate of 92.02%. Multivariate logistic regression analysis revealed the following negative factors influencing participation in community health service management: Age group 31–40 years (OR = 0.532, 95% CI: 0.434–0.653), Age group 41–50 years (OR = 0.557, 95% CI: 0.468–0.663), Age group 51–60 years (OR = 0.746, 95% CI: 0.635–0.877), Age group >60 years (OR = 0.840, 95% CI: 0.719–0.969), Duration of illness 6–10 years (OR = 0.376, 95% CI: 0.307–0.461), Duration of illness 11–15 years (OR = 0.312, 95% CI: 0.249–0.390), Duration of illness 16–20 years (OR = 0.702, 95% CI: 0.529–0.932), Duration of illness >20 years (OR = 0.701, 95% CI: 0.514–0.957), Education level of college or above (OR = 0.719, 95% CI: 0.560–0.923), Current student status (OR = 0.565, 95% CI: 0.419–0.760), Absence of social welfare benefits (OR = 0.643, 95% CI: 0.572–0.723), History of violent or harmful behavior (OR = 0.553, 95% CI: 0.442–0.692), Non-participation in community rehabilitation activities (OR = 0.170, 95% CI: 0.101–0.284). Conversely, the following factors were identified as positive influences on participation: Being a farmer (OR = 1.423, 95% CI: 1.215–1.665), Widowhood (OR = 2.355, 95% CI: 1.583–3.503), Divorce (OR = 2.992, 95% CI: 2.093–4.278). Qualitative analysis indicated that stigma associated with the illness, concerns over information disclosure, lack of social support, impacts on family members (e.g., children's education or marriage prospects), perceived ineffectiveness of community services, lack of awareness about available community health services, and the belief that services were unnecessary contributed to non-participation in community health service management.
Conclusion: The participation rate of patients with severe mental disorders in health service management is relatively low in the Wuxi. Special attention should be given to patients with severe mental disorders who exhibit negative factors, such as being middle-aged or young, having a long duration of illness, a history of violent or harmful behavior, higher education levels (college and above), student status, or lack of social welfare benefits. Efforts should focus on providing social support activities, reducing stigma associated with the illness, and further improving the management rate.
1 Introduction
Mental health is a major public health issue in China that has been gaining increasing attention as society develops. In July 2009, the Ministry of Health, Ministry of Finance, and other departments jointly issued the “Opinions on Promoting the Gradual Equalization of Basic Public Health Services,” which included the service management of patients with severe mental disorders as one of the public health service projects in China. According to the requirements of the “Management and Treatment Guidelines for Severe Mental Disorders (2018 edition)” (1) and the “National Basic Public Health Service Specifications (Third Edition)” (2) community primary healthcare institutions are required to provide basic public health services to all severe mental disorder patients who meet the six diagnostic categories (schizophrenia, intellectual disability with comorbid mental disorders, bipolar affective disorder, schizoaffective disorder, paranoid schizophrenia, and mental disorders caused by epilepsy) and give informed consent. The specific services include patient follow-up management, risk assessment, medication guidance, rehabilitation treatment, and nursing health education.
Patients with severe mental disorders often have a high risk of relapse and disability. Therefore, effective monitoring of patients is essential to prevent disease relapse, accidents, and situations where the lack of family and community healthcare institution management can result in harm to oneself or others. Disease relapse not only affects the recovery of patients but also increases the burden on patients and society. In some cases, it can seriously disrupt public order and social stability. Therefore, it is crucial to provide effective health service management for patients with severe mental disorders in the community, including disease assessment, health education, and other basic public health services. This not only helps prevent and control disease relapse but also enables targeted interventions for specific situations (3).
The prevention and control of community mental health in China began in 1958 (4, 5). Although the development of community mental health prevention and control work was slow in the 19th century, it is widely regarded as the best approach to providing mental health treatment and care (6). Since 2004, due to the growing importance of mental health, China implemented a mental health program known as the “686 Program” (7), establishing a community mental health service system. This program promoted community mental health work in China and became a significant part of the subsequent development of community mental health services.
The community mental health service system primarily involves general practitioners and rural doctors in the early detection, treatment, and relapse prevention of patients with severe mental disorders, as well as patient information management and follow-up visits conducted at least four times a year for stabilized patients. In cases of emergencies or severe medication side effects, free crisis management services are also provided. Nurses are rarely involved in community mental health work. They assist in recording patient follow-up information and help doctors with health education for patients, such as medication guidance and management. By the end of 2020, there were 6.43 million registered patients receiving community mental health services, with a reported prevalence rate of 0.46%; 6.11 million of these patients were under management, resulting in a management rate of 95.12% (8). However, due to various reasons such as stigma, limited accessibility, and the perceived benefits of community services, the utilization rate of community mental health services in China remains low.
In terms of community mental health prevention strategies, apart from providing routine mental health promotion activities for community residents, the main prevention strategy lies in promptly identifying patients with severe mental disorders through community health services and guiding them to specialized mental health institutions for diagnosis and treatment. For registered patients with severe mental disorders in the community, community doctors are required to conduct regular follow-ups to assess their mental state and living conditions, detect signs of relapse or new mental health issues in a timely manner, and provide appropriate interventions. They also offer psychological support to patients and their families, improving their understanding of mental illness. Rehabilitation institutions or services are established in some communities to provide rehabilitation training for mental health patients, enhancing their sense of social belonging and promoting social integration. Although the quality and utilization rate of community mental health services in China remain relatively low, they still serve as the main prevention and control system for community mental health, playing a critical role.
Regarding the cost-benefit analysis of community mental health prevention and control, although certain human, material, and financial resources are required during implementation, the benefits of reducing the prevalence of mental illness, improving patients' health, reducing relapse rates, facilitating patients' reintegration into the community, and promoting social harmony outweigh the costs. These efforts not only alleviate the economic and psychological burden on patients and their families but also save substantial medical and social costs for society (9), contributing to sustainable social development. At the same time, it should be noted that mental health resources are still insufficient to meet the needs of all mental illness patients in current public health planning and resource allocation. Greater attention should be paid to and efforts made to strengthen community mental health prevention and control work, continuously optimizing prevention and control models and resource utilization efficiency to achieve greater cost-effectiveness.
2 Materials and methods
2.1 Data source
The data were obtained from the Jiangsu Provincial Management System for Severe Mental Disorders, covering the period from 2019 to 2021, and specifically focusing on registered patients with severe mental disorders in Wuxi city. Severe mental disorder patients were diagnosed according to the ICD-10 criteria and classified into six categories, including schizophrenia, intellectual disability with comorbid mental disorders, bipolar affective disorder, schizoaffective disorder, paranoid schizophrenia, and mental disorders caused by epilepsy. A total of 27,977 cases were included as study subjects, and their personal basic information and follow-up records were collected. Inclusion criteria for the study subjects were: (1) age ≥ 14 years; (2) clear diagnosis and reporting unit; (3) informed consent was obtained from guardians. Cases with a significant amount of missing basic information and those who had been transferred out of the follow-up management system were excluded. This study was approved by the ethics committee of our institution.
2.2 Survey content and definitions
A cross-sectional study design was used to collect and summarize the basic information and treatment details of registered patients. This included gender, age, education level, occupation, marital status, social welfare status, medical insurance, diagnostic classification, disease duration, duration of medication, and other medical information. Additional information collected included past symptoms of the patients, participation in basic public health projects for community management, community rehabilitation services, and occurrence of harmful incidents (or risk assessment level 3 or above). The determination of harmful incidents was cross-checked and confirmed with the local public security bureau. Social welfare refers to the minimum livelihood guarantee system, which provides subsidies to families with severe disabilities or loss of labor capacity due to illness. Harmful incidents are defined as violations of the Public Security Administration Punishment Law of the People's Republic of China that do not constitute a criminal offense, while harmful events are criminal behaviors that violate relevant articles of the Criminal Law of China (7). The risk assessment is divided into levels 0–5: Level 0: No behavior matching any of the criteria for levels 1–5. Level 1: Verbal threats or shouting, but no destructive behavior. Level 2: Destructive behavior confined to the home, targeting property, and can be stopped through persuasion. Level 3: Significant destructive behavior, indiscriminate of location, targeting property, and cannot be stopped through persuasion. Level 4: Persistent destructive behavior, indiscriminate of location, targeting property or people, and cannot be stopped through persuasion. Level 5: Violent behavior targeting individuals with controlled dangerous weapons, or actions such as arson or explosions. We reviewed the risk assessment levels (0–5) of patients in the archival system and defined levels 3 and above as “violent or harmful behavior.”
2.3 Statistical analysis
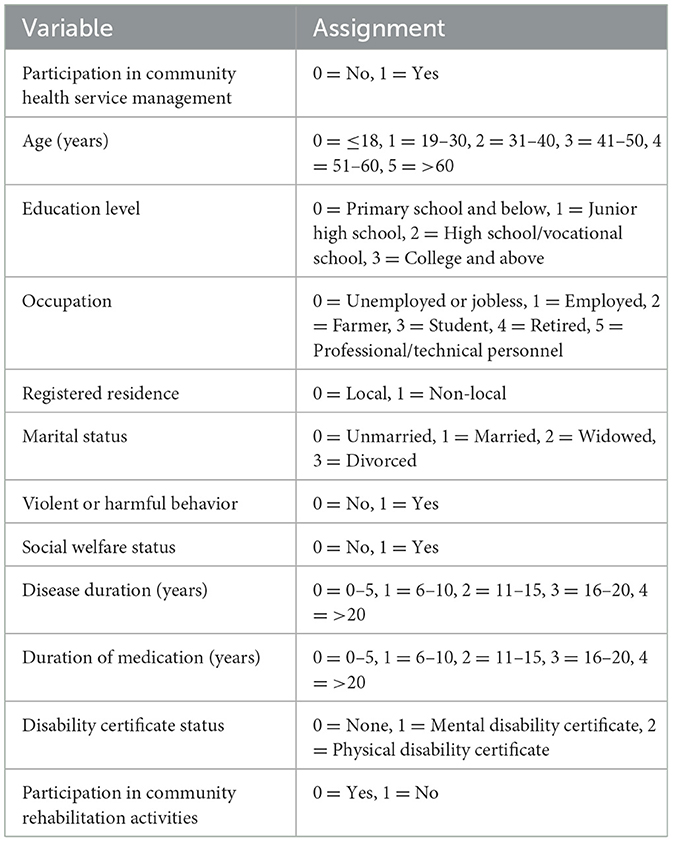
Data analysis was conducted using SPSS 19.0 statistical software. Continuous data were presented as X ± s, while categorical data were tested using the chi-square test. Group comparisons were performed using the chi-square test. Variables with statistically significant differences were included in the multivariable logistic regression analysis. The factors influencing the participation of patients in community health service management were analyzed through regression analysis, with the assignment of independent variables as shown in Table 1. A significance level of P < 0.05 was considered statistically significant. In the qualitative study, we used a convenience sampling method to randomly select some patients who declined community management for interviews. The interviews were conducted with open-ended questions, such as “Why are you unwilling to participate in community management?” to understand the true thoughts and reasons behind patients' refusal to participate in community management.
3 Results
3.1 Demographic characteristics
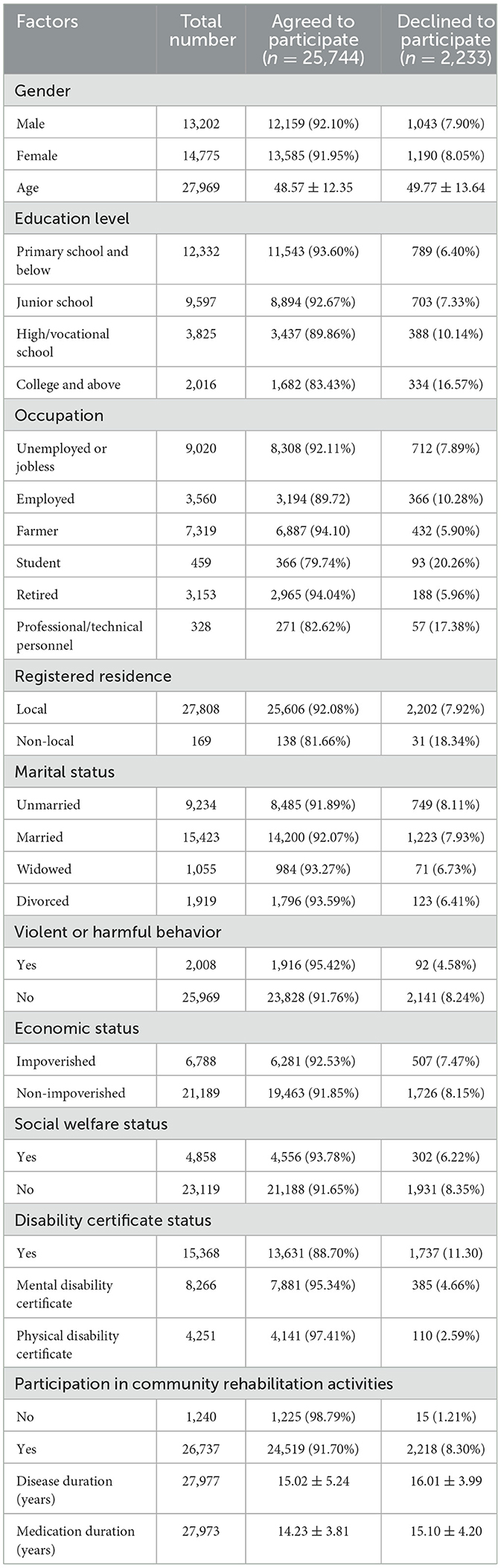
A total of 27,977 patients were included in the study, among which 25,744 patients agreed to participate in community management. Of the patients who agreed to participate, 12,159 were male and 13,585 were female, with an average age of 48.57 ± 12.35 years. The majority had an education level of elementary school or below (11,543 patients). The most common occupation was unemployed or laid-off workers (8,308 patients). Regarding marital status, the highest proportion were married (14,200 patients), and the majority were economically non-poor (19,463 patients). The average duration of illness was 15.02 ± 5.24 years, and the average duration of medication use was 16.01 ± 3.99 years.
A total of 2,233 patients declined to participate in community management. Among them, 1,043 were male and 1,190 were female, with an average age of 44.77 ± 13.64 years. The majority had an education level of elementary school or below (789 patients). The most common occupation was unemployed or laid-off workers (712 patients). Regarding marital status, the highest proportion were married (1,223 patients), and the majority were economically non-poor (1,726 patients). The average duration of illness was 14.23 ± 3.81 years, and the average duration of medication use was 15.10 ± 4.20 years. As shown in Table 2.
3.2 Community health service management participation among patients with severe mental disorders of different characteristics
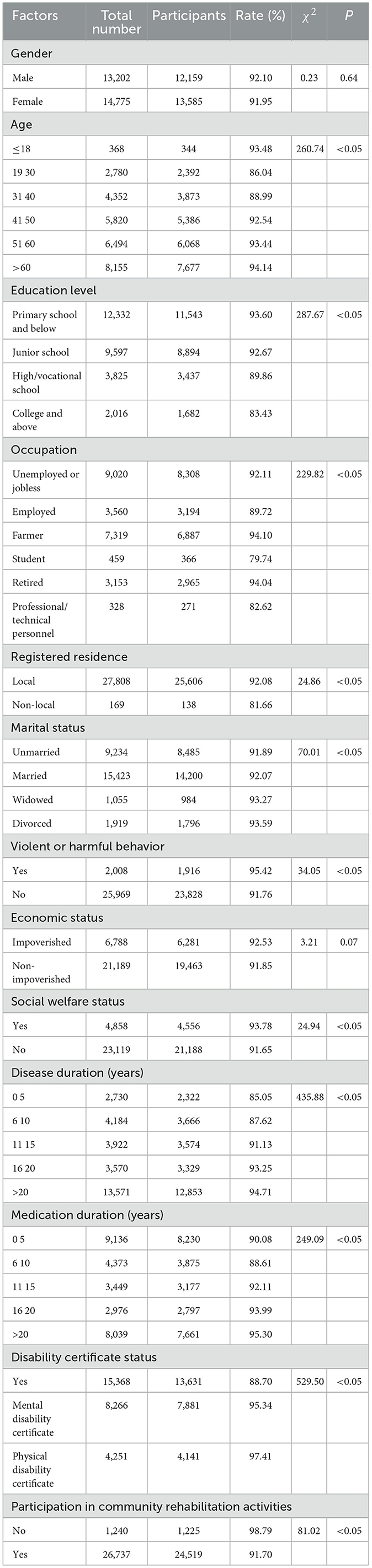
The participation rate of severe mental disorder patients in community health service management was 92.02%. There were significant differences in the participation rate among different age groups, education levels, occupations, marital statuses, disease durations, and durations of medication (P < 0.05). Patients with local registered residence had a higher participation rate compared to non-local patients. Patients with violent or harmful behavior had a higher participation rate compared to those without a history. Patients receiving social welfare benefits had a higher participation rate compared to those without benefits. Patients with a disability certificate had a higher participation rate compared to those without a certificate. Patients who did not participate in community rehabilitation activities had a higher participation rate compared to non-participants. These differences were statistically significant (P < 0.05). Refer to Table 3 for details.
3.3 Influencing factors of the participation of patients with severe mental disorders in community health service management
The variables with statistical significance in the stratified analysis were included in a multivariate logistic regression model. The results indicated that the main factors influencing participation in community health service management among patients with severe mental disorders include age, duration of illness, marital status, education level, presence of social welfare benefits, occupation, history of violent or harmful behavior, and participation in community rehabilitation activities. Compared with the < 18-year-old group, patients in the 31–40, 41–50, 51–60, and >60 age groups were more likely to refuse participation in community health service management. Compared with the group with a duration of illness of 0–5 years, patients with a duration of 6–10 years, 11–15 years, 16–20 years, and >20 years were more likely to refuse participation. Patients with a college education or above, students, those without social welfare benefits, those with a history of violent or harmful behavior, and those who do not participate in community rehabilitation activities were negative factors for participation in community health service management. On the other hand, being a farmer, widowed, or divorced were positive factors for participation (see Table 4).
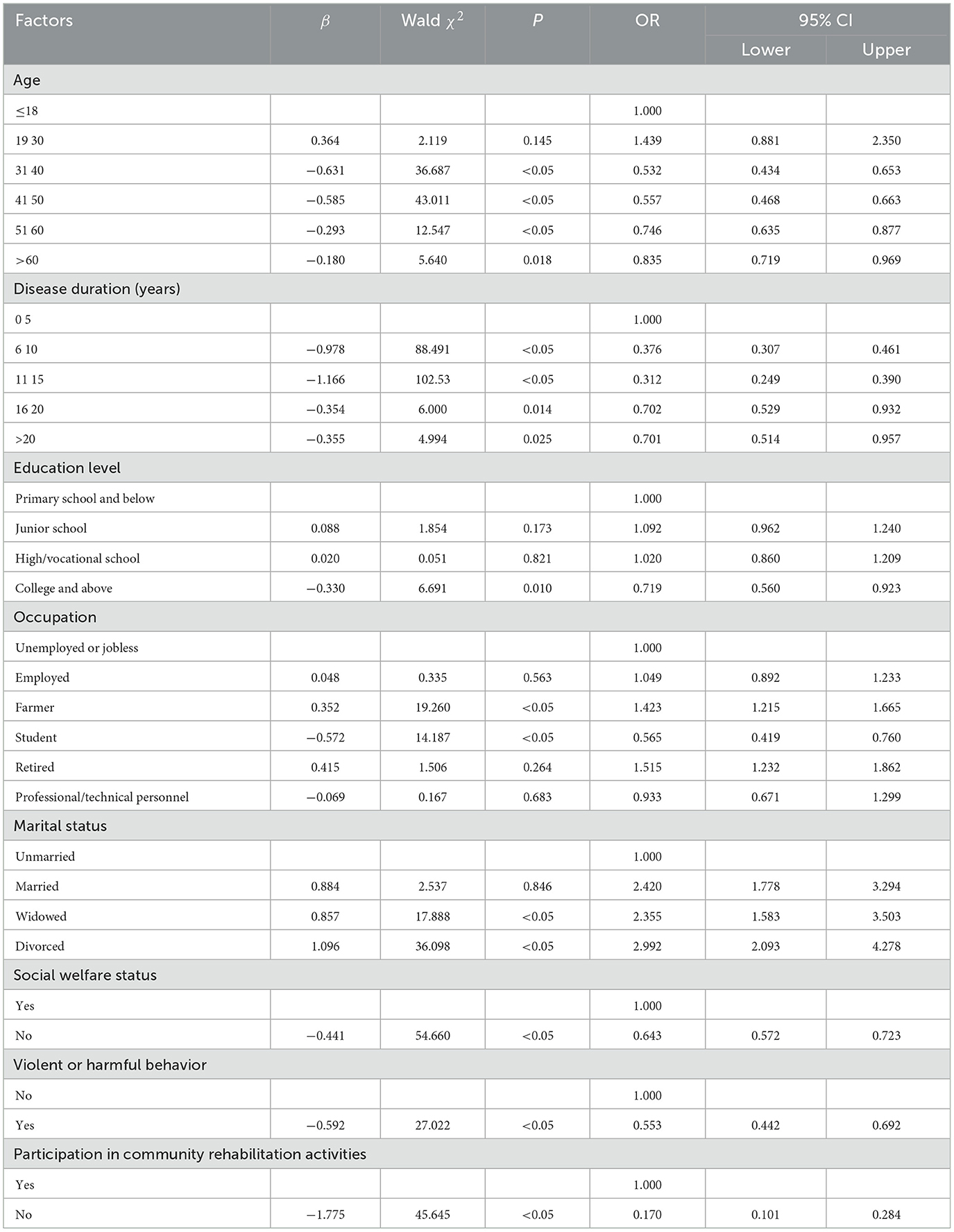
Table 4. Multivariate logistic regression analysis of factors influencing the participation of patients with severe mental disorders in community health service management.
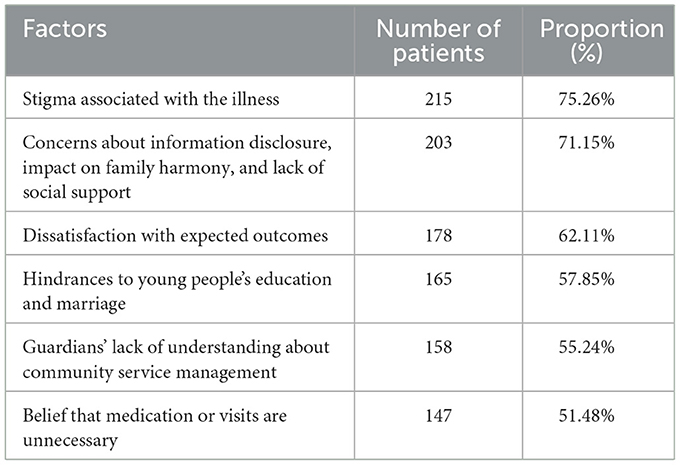
3.4 Qualitative study on patients who declined community management
Based on preliminary telephone and in-home interviews conducted for this study, we investigated 286 patients who declined community management. Among them, 102 patients were interviewed in person during home visits, and 184 patients were surveyed via telephone. The primary characteristics of these patients included high educational attainment and being part of a mobile population. The reasons for refusing community management were mainly composed of stigma associated with the illness, concerns about information disclosure, lack of social support, impacts on family harmony, hindrances to young people's education and marriage, dissatisfaction with the perceived outcomes of community services, lack of understanding about community health services, and the belief that services or medication were unnecessary. See Table 5 for details.
4 Discussion
Patients with severe mental disorders often experience relapses and have long-term illness durations. The majority of their recovery time is spent in the community, making community health service management particularly important for these patients. It plays a crucial role in promoting the long-term stability of patients with severe mental disorders. In China, the government has included the management and treatment of severe mental disorders in the national basic public health service program (1).
This study found that the rate of community health service management among patients with severe mental disorders in Wuxi was 92.02%, which is lower than the national rate of 95.12% (8). The level of economic development, cultural background, and assistance policies in different regions influence the community health service management of patients with severe mental disorders. There are often regional disparities in development and significant differences in the utilization of public health services (10, 11). This study provides scientific evidence to improve the management rate in the local area by analyzing the participation of patients with severe mental disorders in community health service management and its influencing factors.
Effective management of patients with severe mental disorders not only helps alleviate the economic and family burden for patients and their families but also reduces the social burden through increased social support and basic public health services (12). This study found that older patients are less willing to participate in community health service management compared to younger patients. This may be due to older patients being less aware of community health service management policies and having difficulty understanding the meaning of basic public health services, making it more challenging for them to accept such services. We also found that longer duration of illness is a negative factor for participating in community health service management. This may be because patients with longer illness durations experience repeated episodes, long-term medication, and lose hope in the treatment of their illness, leading to a negative attitude toward the disease and a lack of confidence in primary community health services (13). Patients with higher education levels, particularly those with college and above education, are also less likely to accept community health service management. This could be attributed to increased awareness and understanding of mental illnesses with higher levels of education, as well as concerns about privacy, making it more challenging for them to participate in community health service management (14). Compared to unemployed individuals, students show a negative association with participating in community health service management. This could be because students may feel protected in their school environment and may be reluctant to disclose their mental illnesses, experiencing stigma and avoiding community health service management (15). Patients who do not receive social welfare support also show a negative association with participating in community health service management. Patients who do not qualify for social welfare support often have better financial conditions and more ability and experience in taking care of themselves, making them less inclined to participate in free community health service management programs. Patients who do not participate in community rehabilitation activities also show a negative association with participating in community health service management. Compared to patients who participate in community rehabilitation activities, those who do not receive the same level of social support, including care from the neighborhood or community, and planned rehabilitation activities from mental health professionals. These factors can promote patient recovery, improve their community functioning, reduce self-stigma, alleviate the burden on families, and facilitate the acceptance of basic public health services (16, 17).
Furthermore, this study found that patients with occupations as farmers are more likely to participate in community-based health service management. This could be attributed to their limited knowledge of mental health and reliance on primary community health services, leading to better compliance with community health service management. In contrast, compared to unmarried patients, those who are widowed or divorced are more likely to participate in community health service management. This may be because patients rely more on social support after marital failure and tend to have greater trust in community health workers (18). This can help them effectively manage their mental illness, prevent relapses, and reduce the occurrence of harmful behaviors. Several studies have shown that comprehensive community management interventions for patients with severe mental disorders have positive effects, reducing relapses and harmful behaviors, and alleviating the burden on both society and patients (19, 20). Therefore, it is essential to encourage the participation of patients with severe mental disorders in basic public health service programs, promote their social functioning, and integrate them into society.
In the qualitative interviews targeting patients less likely to participate in community management, we found that 50% of individuals cited stigma, concerns about information disclosure, worries about the impact of their illness on family finances, education, and social interactions, as well as insufficient awareness of community health services, as the main reasons for not participating. It is not difficult to imagine that discrimination against mental illness is still prevalent in society. Many parents teach their children to avoid mental illness patients, highlighting the challenges of integrating patients with mental disorders into society. Furthermore, the confidentiality concerns raised by some patients and families stem from community staff collecting patient information and conducting home visits or telephone follow-ups according to guidelines, which can cause distress. Some patients also reported that receiving community health services did not improve their condition, leading to a gradual loss of interest in these services and their refusal to participate in follow-up management. Additionally, there are patients who believe their condition is stable and that reducing or discontinuing medication has no impact on their health, making them less reliant on community management.
The strengths of this study lie in its large sample size, which investigated whether patients with severe mental disorders participate in community health service management and explored the influencing factors. Additionally, qualitative interviews with patients who declined community management were conducted to understand their subjective perceptions, providing valuable insights for future mental health work. However, this study has certain limitations. First, the data were sourced from Wuxi City, making the data source singular. The exclusion of patients with incomplete information and those without a confirmed diagnosis also impacts the results, limiting the generalizability of the findings across other regions in China. Furthermore, the lack of information about patient caregivers, as well as details regarding patient satisfaction, relapse rates, and the efficiency of basic public health services after participating in community health service management, requires further exploration. Future research will adopt longitudinal designs, more detailed variable definitions, advanced statistical analyses, and additional data sources to further investigate related topics.
In conclusion, patients with severe mental disorders should be encouraged to participate in basic public health service programs to promote their recovery of social functioning and reintegration into society, while providing adequate social support. Policies supporting free medication for impoverished patients, increasing the frequency and amount of medical assistance (21), and reducing societal discrimination against patients and their families should be implemented. For patients who decline participation in community health service management, targeted health education and policy promotion should be conducted to improve the management rate of community health services for patients with severe mental disorders.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Committee of Wuxi Mental Health Centre. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YJ: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. QY: Data curation, Investigation, Methodology, Writing – original draft. JY: Data curation, Investigation, Methodology, Project administration, Validation, Writing – original draft. QY: Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. ZH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The work was supported by the National Natural Science Foundation of China (82104244), Wuxi Municipal Science and Technology Bureau (K20231039 and K20231049), Top Talent Support Program for young and middle-aged people of Wuxi Health Committee (HB2023088), Scientific Research Program of Wuxi Health Commission (M202211, Q202457), Wuxi Taihu Talent Project (WXTTP2021), and Wuxi Medical Development Discipline Project (FZXK2021012).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Notice of the National Health Commission on the issuance of the “Management and Treatment Work Specification for Severe Mental Disorders (2018 Edition).” Gazette of the State Council of the People's Republic of China. China Government Net (2018).
2. Notice of the National Health and Family Planning Commission on the issuance of the “National Basic Public Health Service Specification (Third Edition).” Bulletin of the National Health and Family Planning Commission of the People's Republic of China. National Health and Family Planning Commission (2017).
3. Xu F, He H, Pan W, Xue L, Li K. Analysis of the management status of patients with severe mental disorders in Gansu Province from 2019 to 2020. Chin J Public Health Manage. (2022) 38:633–5+639.
4. Liu J, Ma H, He YL, Xie B, Xu YF, Tang HY, et al. Mental health system in China: history, recent service reform and future challenges. World Psychiatry. (2011) 10:210–6. doi: 10.1002/j.2051-5545.2011.tb00059.x
5. Ma Z, Huang H, Chen Q, Chen F, Abdullah AS, Nie G, et al. Mental health services in rural China: a qualitative study of primary health care providers. Biomed Res Int. (2015) 2015:151053. doi: 10.1155/2015/151053
6. Ma H, Liu J, He YL, Xie B, Xu Y, Hao W, et al. An important direction for reforming China's mental health service model: the 686 program. Chinese Mental Health Journal. (2011) 25:725–8.
7. Zhang WF, Ma N, Wang X, Wu X, Zhao M, Chen R, et al. Analysis of the current situation of management and treatment of patients with severe mental disorders in China in 2020. Chin J Psychiatry. (2022) 55:122–8.
8. Pennington M, McCrone P. The cost of relapse in schizophrenia. Pharmacoeconomics. (2017) 35:921–36. doi: 10.1007/s40273-017-0515-3
9. Jiang F, Yan G. Analysis of factors influencing the occurrence of harmful behaviors in severely mentally ill patients managed in the community in Chengdu. Modern Prevent Med. (2019) 14:2584–7.
10. Zhang W, Hou H, Li X, Ma Q, Zhang Q, Ren Q. Analysis of the utilization of public health services and influencing factors among severely mentally ill patients in rural areas of Wenchang Lake District. J Chron Dis. (2022) 23:1281–5+1289. doi: 10.16440/J.CNKI.1674-8166.2022.09.01
11. Sun S, Bai J, Yun Q, Li Y, Chang C. Analysis of the management and treatment services for severe mental disorders in China from 2014 to 2017 and its equity. Chin J Mental Health. (2022) 36:185–90.
12. Lu C, Cheng J, Qing L, Liu C, Su H, Lin W. Characteristics and community management status of severe mental disorder patients in Bao'an District, Shenzhen. Chin J General Pract. (2022) 20:1901–4. doi: 10.16766/j.cnki.issn.1674-4152.002731
13. Guo Z, Wang Y, Wang C, Wang H, Zhang R, Yao F. Medication compliance and its influencing factors in patients with severe mental disorders in Henan Province. Chin J Psychiatry. (2020) 53:321–7. doi: 10.3760/cma.j.cn113661-20190731-00254
14. Xie F, Li H, Cao N. Investigation of the knowledge and attitudes toward mental health among family members of patients with severe mental disorders. South China J Prevent Med. (2022) 48:1029–32.
15. Zhang Q, Tao H, Ju K. Analysis of the current situation of illness stigma among patients with mental disorders in a certain district of Shanghai. Shanghai J Prevent Med. (2022) 34:168–72. doi: 10.19428/j.cnki.sjpm.2022.21439
16. Zhao W, Zhu Y, Luo X, Liu S, Ma X, Wang X. Proactive community treatment models for the management and treatment of severe mental disorders (review). Chin J Mental Health. (2014) 28: 89–96.
17. Lin H, Liang Z, Liang P, Liu C, Li Q, Liu Z, et al. Investigation and intervention of illness stigma among patients with severe mental disorders and their family members. Chin J General Pract. (2014) 2014:1551–3.
18. Wang R, Song S, Zhou Y, Liu Y. Analysis of the current status of social support and its influencing factors among family caregivers of severe mental disorder patients. Chin J General Pract. (2022) 25:480–8.
19. Xu Y, Li Y, Jiang B. Meta-analysis of the effect of comprehensive management interventions on harmful behaviors of severe mental illness patients in the community. Chin J Public Health. (2015) 31:1091–4.
20. Zhang P, Zhang B. Evaluation of the effect of continuous “specialized and comprehensive” management model for severe mental disorder patients. Chin J Neurol Psychiatry. (2022) 48:360–4.
Keywords: severe mental disorders, community health service management, influencing factors, Wuxi, China
Citation: Li S, Ji Y, Yang Q, Jiang Y, Yin Q and Zhu H (2025) Influencing factors of the participation of patients with severe mental disorders in community health service management. Front. Public Health 13:1424399. doi: 10.3389/fpubh.2025.1424399
Received: 28 April 2024; Accepted: 02 January 2025;
Published: 17 January 2025.
Edited by:
Edmund Howe, Uniformed Services University of the Health Sciences, United StatesReviewed by:
Devashish Konar, Mental Health Care Centre, IndiaOshin Miranda, Brown University, United States
Copyright © 2025 Li, Ji, Yang, Jiang, Yin and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haohao Zhu, emh1aGhAamlhbmduYW4uZWR1LmNu; Qitao Yin, eXF0MTIwOUAxNjMuY29t
†These authors have contributed equally to this work
 Shiming Li
Shiming Li Yingying Ji†
Yingying Ji† Ying Jiang
Ying Jiang Haohao Zhu
Haohao Zhu