- Department of Healthcare-Associated Infection Control Center, Sichuan Provincial People's Hospital, University of Electronic Science and Technology of China, Chengdu, China
Background: The purpose of this study is to investigate the risk factors for carbapenem-resistant Klebsiella pneumoniae (CRKP) infection and death of K. pneumoniae infections in acute pancreatitis (AP) patients.
Methods: This was a retrospective analysis of AP patients with K. pneumoniae infection between January 2019 and April 2024. Logistic regression model was used to determine the risk factors for acquisition of CRKP. Cox proportional hazards regression model was used to identify risk factors for mortality of K. pneumoniae infection.
Results: A total of 113 AP patients experienced K. pneumoniae infections, including 66 with CRKP infection and 47 with CSKP infection. The mortality rate of these patients was 36.3%, with a significantly higher mortality rate in the CRKP group than in the CSKP group (P < 0.001). Only mechanical ventilation (OR = 2.301; 95% CI 1.02-5.20; P = 0.045) was the independent risk factor for CRKP infection in patients with AP. Surgery (HR 0.38; 95% CI 0.20–0.75; P = 0.005) and mechanical ventilation (HR 2.93; 95% CI 1.10–7.82; P = 0.032) were the independent risk factors associated with mortality of K. pneumoniae infection in patients with AP.
Conclusion: Klebsiella pneumoniae infection has become a threat to patients with AP. Therefore, implementing preventive and control measures based on risk factors is crucial for the prognosis.
Introduction
Acute pancreatitis (AP) is a common acute abdominal disease, and the incidence rate continues to increase worldwide (1). Severe acute pancreatitis (SAP) is a severe form of AP with systemic organ failure and a mortality rate of up to 30% (2). Infection is a common complication of AP, with nearly a third of patients with AP developing pancreatic or extra-pancreatic infection (3). Secondary infection may be an independent risk factor for poor prognosis in AP (4).
Currently, carbapenem-resistant Klebsiella pneumoniae (CRKP) has become the main nosocomial pathogen, which can cause various types of infections, such as pneumonia, bloodstream infections (BSI), intra-abdominal infections, and urinary tract infections (5). In recent years, the rate of isolation and reporting of CRKP infections has been on the rise globally, with a particularly prominent increase in Asia compared to Europe and the United States (6). CRKP infections have become a significant public health threat, with limited options for antimicrobial treatment, posing a great challenge to both treatment and prevention and control. Klebsiella pneumoniae is a common pathogen of infection in patients with AP. The treatment of AP complicated by CRKP infection is more difficult, resulting in higher mortality rates, longer hospital stays, and a severely compromised prognosis for the patients (7). Previous studies have shown that complications caused by multidrug-resistant bacterial infections increase the mortality rate of AP patients (6, 8, 9). Although strict prevention and control measures have been taken in hospitals for patients with AP, the occurrence of CRKP infection still exists. Therefore, patients with AP complicated by CRKP infection deserve attention. This retrospective cohort study aims to investigate the risk factors for AP patients complicated with CRKP infection, in order to help clinicians better take prevention and control measures, and improve clinical outcomes for these patients in the future.
Methods
Study design and participants
This retrospective cohort study was conducted in Sichuan Academy of Medical Sciences and Sichuan Provincial People's Hospital, a 4,300-bed teaching hospital in Western China. The clinical data of AP patients with K. pneumoniae infection admitted from January 2019 to April 2024 was collected. Patients with K. pneumoniae isolated from any clinical specimen within 48 h after admission and those under the age of 18 were excluded. Patients with incomplete clinical data were also excluded. Only the first episode of K. pneumoniae infection was included during the study period. This study was approved by the Ethics Committee of Sichuan Academy of Medical Sciences and Sichuan Provincial People's Hospital. The ethics committee exempted the requirement for informed consent as it was a retrospective study.
Microbiology
The sensitivity of carbapenem was determined by agar dilution method and interpreted referring to guidelines of the Clinical and Laboratory Standards Institute (CLSI) (10). Disk-diffusion synergistic test recommended by CLSI was used for screening and detecting K. pneumoniae. The automated instrument used the VITEK 2 (BioMerieux, France) compact automatic microbial identification and drug sensitivity analysis system. The disk-diffusion synergistic test adopted the Kirby Bauer method, and the drug sensitive paper was sourced from BBL and Oxoid. Consistent with the CLSI definition, CRKP was defined as K. pneumoniae with a minimum inhibitory concentration (MIC) of ≥2 mg/L for ertapenem or a MIC of ≥4 mg/L for meropenem or imipenem or dolipenem (10).
Data collection
Baseline characteristics of patients were collected from the electronic medical record of the first episode of K. pneumoniae, including age, gender, body mass index (BMI), comorbidities, intravenous catheter, mechanical ventilation, urinary catheterization, surgery, ICU exposure, length of hospitalization, type of infection and mortality, etc. Microbiological and laboratory data were collected from the laboratory information system (LIS), including white blood cells (WBC), hemoglobin, platelet count, C-reactive protein, serum creatinine, albumin, total bilirubin, blood glucose, and procalcitonin (PCT). The data would be entered into an Excel spreadsheet and verified by two dedicated infection control personnel after collection. According to the death events during hospitalization, clinical outcomes were divided into survival group and non-survival group.
Statistical analysis
Quantitative data are represented as mean ± standard deviation or median (range), depending on whether it conforms to normal distribution. The student's t-test or Mann-Whitney U test (as appropriate) was performed to analyze the differences between groups. Categorical variables were expressed in absolute numbers and percentages, and compared with the χ2 test or Fisher exact test. AP patients with K. pneumoniae infection were divided into two groups based on whether they were resistant to carbapenem antibiotics: CRKP infection group and CSKP infection group. We used univariate and multivariate binary logistic regression to identify risk factors for CRKP infection. Univariate and multivariate Cox proportional hazards regression models are used to study independent risk factors for mortality. The hazard ratio (HR) and 95% confidence interval (CI), as well as the corresponding P-value are provided. To evaluate the validity of the proportional hazards assumption, Schoenfeld residual tests were further conducted. For continuous variables such as PCT and WBC, appropriate cut-off values were determined based on clinical relevance and previous literature (10, 11). No data transformations were performed in our analysis. All statistical analyses were performed using SPSS 27.0 and R 4.4.2 statistical software. P < 0.05 was considered statistically significant.
Results
Baseline characteristics of patients with AP complicated by K. pneumoniae infection
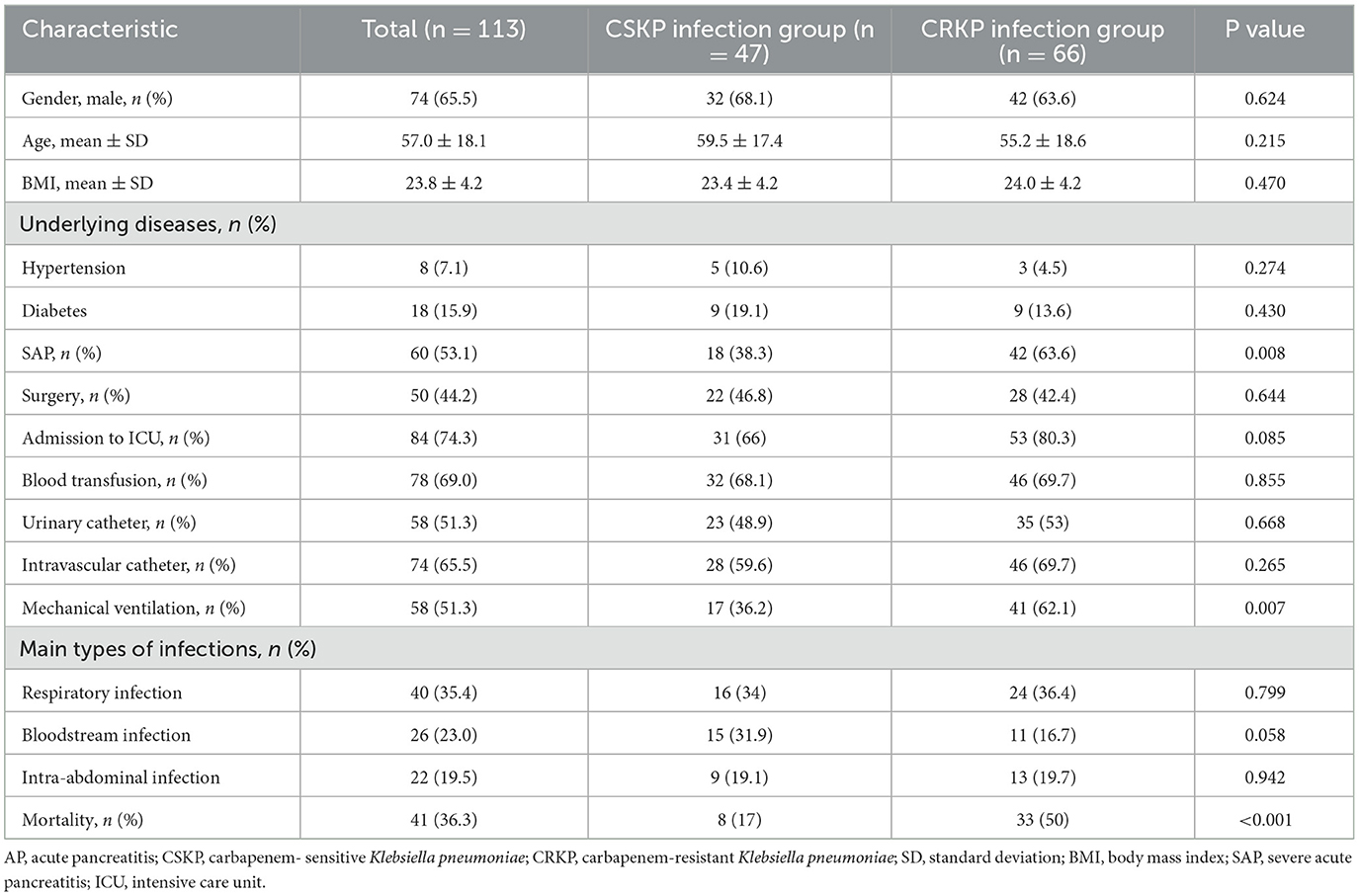
In the past 5 years, a total of 113 AP patients experienced K. pneumoniae infections, including 66 with CRKP infection and 47 with CSKP infection. The average age was 57 years old, with a predominance of males (65.5%). Most isolates were isolated from the respiratory system (35.4%), followed by bloodstream (23.0%) and abdominal cavity (19.5%). There were 60 patients (53.1%) with SAP. Among the 126 patients, 74.3% were admitted to the intensive care unit (ICU) due to worsening conditions. The mortality rate in the CRKP group was significantly higher than that in the CSKP group (P < 0.001). The demographic and clinical characteristics of AP patients with K. pneumoniae infection are shown in Table 1.
Risk factors associated with CRKP infection in patients with AP
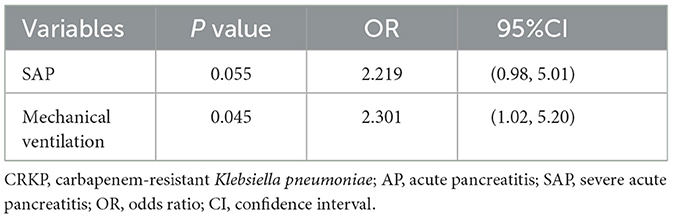
Both the CRKP infection group and CSKP infection group were predominantly male patients, and their ages were comparable. The proportion of SAP and mechanical ventilation in the CRKP infection group was significantly higher than that in the CSKP infection group (P < 0.05). The proportion of patients admitted to ICU in the CRKP infection group was also higher, but the difference had no statistical significance. The univariate logistic analysis of demographic and clinical characteristics of patients with K. pneumoniae infection is shown in Table 1. After logistic multivariate analysis, only mechanical ventilation (OR = 2.301; 95% CI 1.02–5.20; P = 0.045) was the independent risk factor for CRKP infection in patients with AP (Table 2).
Risk factors for mortality of K. pneumoniae infection in patients with AP
Among patients with AP complicated by K. pneumoniae infection, 41 patients died, with a mortality rate of 36.3%. Cox univariate analysis showed that there was a statistically significant difference in age >60 years old, carbapenem resistance, surgery, mechanical ventilation, and PCT >5 ng/ml between the death and survival groups. In Cox multivariate analysis, surgery (HR 0.38; 95% CI 0.20–0.75; P = 0.005) and mechanical ventilation (HR 2.93; 95% CI 1.10–7.82; P = 0.032) were the independent risk factors associated with mortality (Table 3). To evaluate the effectiveness of the Cox proportional hazards model, Schoenfeld residual test was used for validation. The results showed no significant violation of the proportional hazards assumption (P = 0.392) (Supplementary Table S1, Supplementary Figure S1).
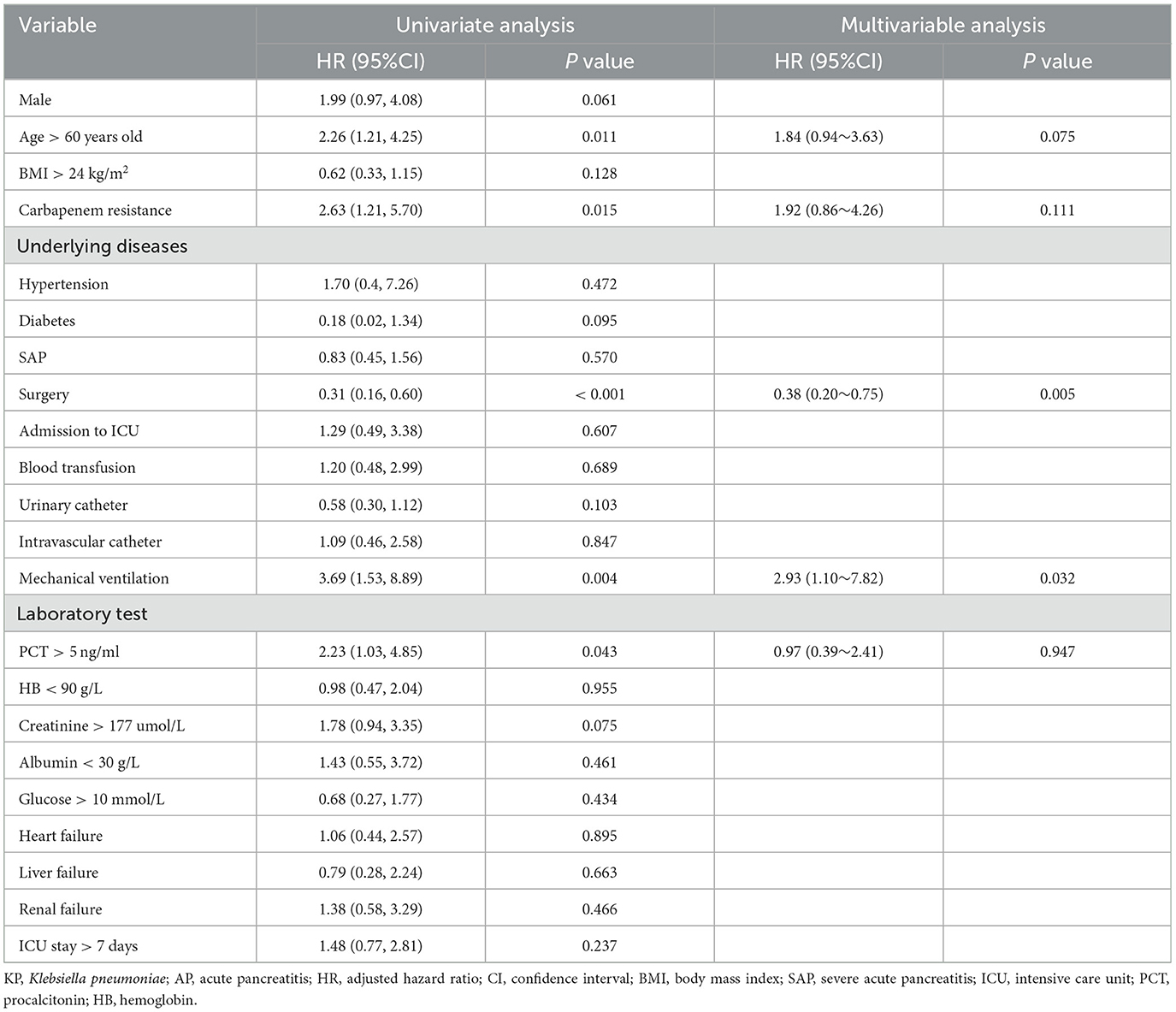
Table 3. Univariate and multivariate analysis of the risk factors for mortality of KP infection in patients with AP.
Risk factors for mortality of CRKP infection in patients with AP
Among 66 patients infected with CRKP, 33 died with a mortality rate of 50%. In the Cox univariate analysis, male, age > 60 years old, surgery, mechanical ventilation and renal failure were associated with the mortality of CRKP infection. After Cox multivariate analysis, male (HR 2.73; 95% CI 1.23–6.08; P = 0.014), age > 60 years old (HR 2.00; 95% CI 1.03–3.88; P = 0.041), surgery (HR 0.32; 95% CI 0.16–0.64; P = 0.001) and mechanical ventilation (HR 2.82; 95% CI 1.05–7.55; P = 0.040) were independent risk factors for mortality of CRKP infection (Table 4). The Schoenfeld residuals test showed no significant violations of the proportional hazards assumption (P = 0.190) (Supplementary Table S2, Supplementary Figure S2).
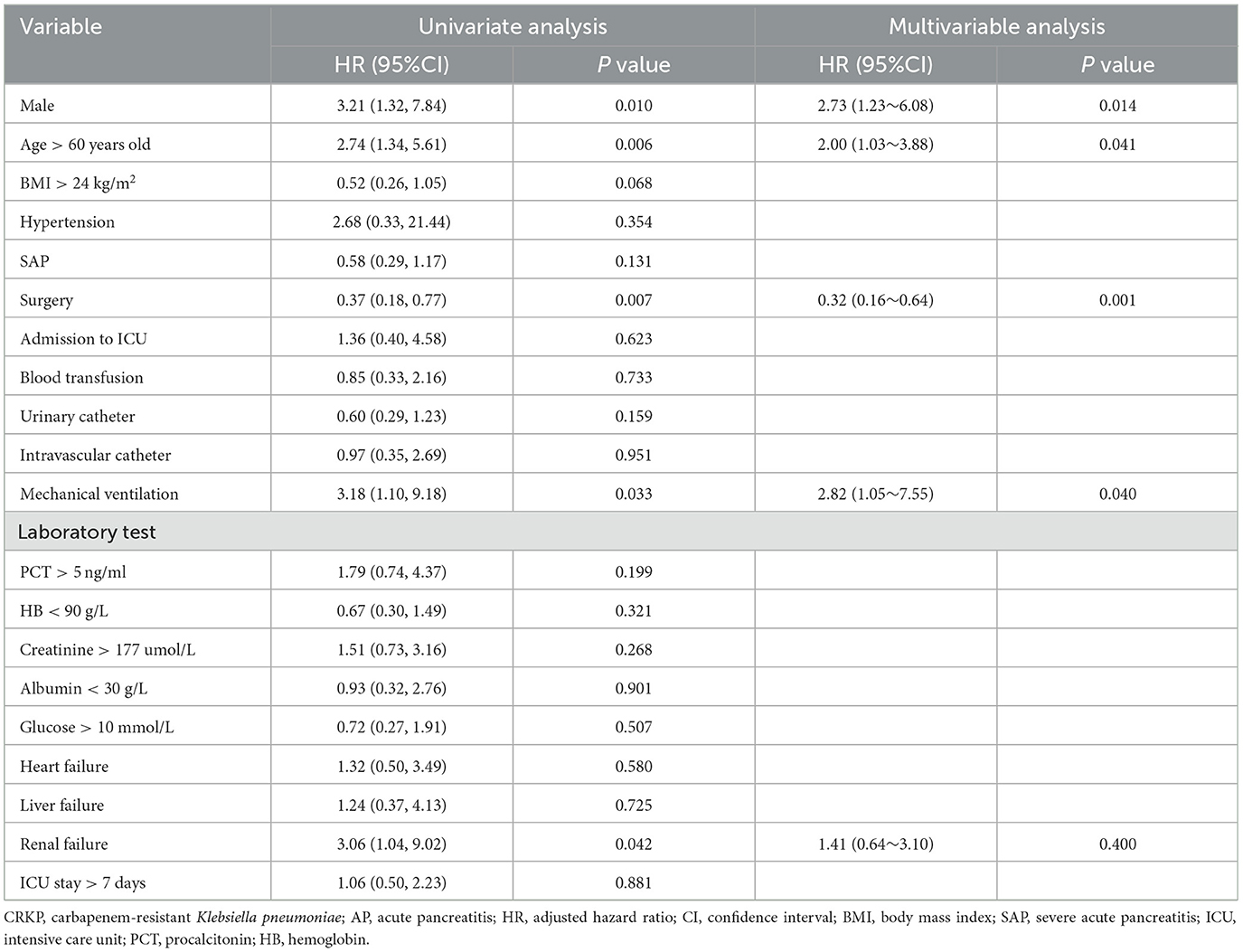
Table 4. Risk factors for mortality of CRKP infection in AP patients with univariate and multivariate analysis.
Discussion
The rapid emergence of multidrug-resistant bacteria in the past decade has become a global threat to public health system (12). In recent years, with the overuse of antibiotics, the incidence of CRKP has increased and has become an important pathogen of hospital-acquired infections. CRKP has been listed as one of the key priority bacteria by the World Health Organization, which would increase mortality and make treatment more difficult (13, 14). Infection is one of the most common complications in AP patients (15). Due to the early and widespread use of antibiotics, patients with AP have become a high-risk group for CRKP infection. Previous study found that carbapenem-resistant Enterobacteriaceae infection was a key factor in the mortality of AP patients in ICU (16). In this study, the mortality rate among patients with AP complicated by K. pneumoniae infection was 36.3%, while the mortality rate reached 50% in those complicated by CRKP infection, which was similar to previous reports (10, 17).
The results showed that the most common site of infection was lower respiratory tract infection, with 51.3% of K. pneumoniae infected patients received mechanical ventilation. Moreover, multivariate analysis showed that mechanical ventilation was the independent risk factor for CRKP infection, indicating that drug-resistant bacteria was prone to invade the respiratory tract. Therefore, infection prevention and control measures should be taken to prevent cross infection during tracheal intubation.
This study suggested that surgery and mechanical ventilation were independent risk factors for death in K. pneumoniae infection. Carbapenems were once considered the most effective drugs against multidrug-resistant Gram-negative pathogens (18, 19). However, the widespread use of carbapenem has led to an increase in resistant gram-negative bacteria. The emergence of drug-resistant bacteria significantly limited the available therapeutic options, and affected the prognosis. Our results showed that the mortality rate of CRKP infected patients was 50%, significantly higher than that of CSKP infected patients, which was consistent with previous research finding (20). Therefore, strict infection control measures and reasonable antibiotic selection should be taken to reduce the occurrence of CRKP infection. In this study, surgery was a protective factor for the prognosis of AP patients with KP infection. For patients with SAP combined with peripheral tissue necrosis and infection, surgery is the main treatment method at present. Surgical removal of necrotic tissue can clear the infection site, which is beneficial for infection control and patient recovery. However, there is still controversy over whether AP patients need surgery and the surgical methods used. The current consensus is that surgery should be performed on patients with clinically unstable infectious necrosis (21). For most AP patients with sterile inflammation, conservative treatment can be administered regardless of the amount and extent of exudate (22). The decision to perform surgery in AP patients should be carefully weighed against the potential benefits and risks. For patients who need surgery, the surgical risk should be assessed before surgery, appropriate surgical methods should be adopted, and infection monitoring should be done after surgery to reduce the infection rate. Mechanical ventilation, while providing therapeutic benefits to patients, may also affect the prognosis of critically ill patients by affecting the function of various organs (23). Therefore, careful management of ventilation is crucial. For patients undergoing mechanical ventilation, it is advisable to minimize the duration of mechanical ventilation and implement standardized infection control measures such as oral care and elevated bed heads to reduce the risk of respiratory infections and improve prognosis.
There were several potential limitations in our study. Firstly, this was a single-center retrospective cohort study with a relatively small sample size, so the results may differ from other studies. Further multicenter and prospective studies are needed. Secondly, this study did not involve antibiotic treatment or other factors, and further large-scale studies are needed to include more factors to determine the risk factors for K. pneumoniae occurrence or death in AP patients.
Conclusions
In conclusion, K. pneumoniae is a common pathogen of infection in patients with AP. In our research, only mechanical ventilation was the independent risk factor for CRKP infection in AP patients. Surgery and mechanical ventilation were independent risk factors for death in AP patients with K. pneumoniae infection. It is necessary to take corresponding prevention and control measures based on these risk factors to reduce the occurrence of drug-resistant bacterial infection.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Sichuan Academy of Medical Sciences and Sichuan Provincial People's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
JC: Conceptualization, Methodology, Writing – original draft. QX: Supervision, Writing – review & editing. J-yW: Supervision, Writing – review & editing. X-JZ: Data curation, Writing – review & editing. X-yJ: Investigation, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1533765/full#supplementary-material
References
1. Forsmark Ch E, Vege SS, Wilcox CM. Acute pancreatitis. N Engl J Med. (2017) 376:598–9. doi: 10.1056/NEJMc1616177
2. Mederos MA, Reber HA, Girgis MD. Acute pancreatitis: a review. JAMA. (2021) 325:382–90. doi: 10.1001/jama.2020.20317
3. Brown LA, Hore TA, Phillips AR, Windsor JA, Petrov MS. A systematic review of the extra-pancreatic infectious complications in acute pancreatitis. Pancreatology. (2014) 14:436–43. doi: 10.1016/j.pan.2014.09.010
4. Choi JH, Kim MH, Cho DH, Oh D, Lee HW, Song TJ, et al. Revised Atlanta classification and determinant-based classification: which one better at stratifying outcomes of patients with acute pancreatitis? Pancreatology. (2017) 17:194–200. doi: 10.1016/j.pan.2017.01.004
5. Wei L, Wu L, Wen H, Feng Y, Zhu S, Liu Y, et al. Spread of carbapenem-resistant Klebsiella pneumoniae in an intensive care unit: a whole-genome sequence-based prospective observational study. Microbiol Spectr. (2021) 9:e0005821. doi: 10.1128/Spectrum.00058-21
6. Ning C, Huang G, Shen D, Bonsu A, Ji L, Lin C, et al. Adverse clinical outcomes associated with multidrug-resistant organisms in patients with infected pancreatic necrosis. Pancreatology. (2019) 19:935–40. doi: 10.1016/j.pan.2019.09.008
7. Lin H, Wang P, Lu Y, Gao K, Hao H, Tong Z, et al. Clinical and genomic characteristics of carbapenem-resistant Klebsiella pneumoniae isolates from acute pancreatitis with infection in China. Clin Lab. (2023) 69:221017. doi: 10.7754/Clin.Lab.2022.221017
8. Wu D, Ding J, Jia Y, Liu H, Xiao J, Peng J. Predictors of mortality in acute pancreatitis complicated with multidrug-resistant Klebsiella pneumoniae infection. BMC Infect Dis. (2021) 21:977. doi: 10.1186/s12879-021-06709-0
9. Li X, Li L, Liu L, Hu Y, Zhao S, Sun J, et al. Risk factors of multidrug resistant pathogens induced infection in severe acute pancreatitis. Shock. (2020) 53:293–8. doi: 10.1097/SHK.0000000000001371
10. Jia Y, Liu Y, Huang Y, Wang J, Wang H, Tan S, et al. Clinical characteristics, drug resistance, and risk factors for death of Klebsiella pneumoniae infection in patients with acute pancreatitis: a single-center retrospective study from China. Infect Drug Resist. (2023) 16:5039–53. doi: 10.2147/IDR.S410397
11. Wu D, Huang Y, Xiao J, Qin G, Liu H, Peng J. Risk factors for mortality among critical acute pancreatitis patients with carbapenem-resistant organism infections and drug resistance of causative pathogens. Infect Dis Ther. (2022) 11:1089–101. doi: 10.1007/s40121-022-00624-w
12. Qureshi S, Maria N, Zeeshan M, Irfan S, Qamar FN. Prevalence and risk factors associated with multi-drug resistant organisms (MDRO) carriage among pediatric patients at the time of admission in a tertiary care hospital of a developing country. A cross-sectional study. BMC Infect Dis. (2021) 21:547. doi: 10.1186/s12879-021-06275-5
13. Zhang Y, Guo LY, Song WQ, Wang Y, Dong F, Liu G. Risk factors for carbapenem-resistant K. pneumoniae bloodstream infection and predictors of mortality in Chinese paediatric patients. BMC Infect Dis. (2018) 18:248. doi: 10.1186/s12879-018-3160-3
14. Massinga AJ, Garrine M, Messa A Jr, Nobela NA, Boisen N, Massora S, et al. Klebsiella spp. cause severe and fatal disease in Mozambican children: antimicrobial resistance profile and molecular characterization. BMC Infect Dis. (2021) 21:526. doi: 10.1186/s12879-021-06245-x
15. Lu JD, Cao F, Ding YX, Wu YD, Guo YL, Li F. Timing, distribution, and microbiology of infectious complications after necrotizing pancreatitis. World J Gastroenterol. (2019) 25:5162–73. doi: 10.3748/wjg.v25.i34.5162
16. Timsit JF, Bassetti M, Cremer O, Daikos G, de Waele J, Kallil A, et al. Rationalizing antimicrobial therapy in the ICU: a narrative review. Intensive Care Med. (2019) 45:172–89. doi: 10.1007/s00134-019-05520-5
17. Tian H, Chen L, Wu X, Li F, Ma Y, Cai Y, et al. Infectious complications in severe acute pancreatitis: pathogens, drug resistance, and status of nosocomial infection in a university-affiliated teaching hospital. Dig Dis Sci. (2020) 65:2079–88. doi: 10.1007/s10620-019-05924-9
18. Guo D, Dai W, Shen J, Zhang M, Shi Y, Jiang K, et al. Assessment of prophylactic carbapenem antibiotics administration for severe acute pancreatitis: an updated systematic review and meta-analysis. Digestion. (2022) 103:183–91. doi: 10.1159/000520892
19. Livermore DM. The impact of carbapenemases on antimicrobial development and therapy. Curr Opin Investig Drugs. (2002) 3:218–24.
20. Xu L, Sun X, Ma X. Systematic review and meta-analysis of mortality of patients infected with carbapenem-resistant Klebsiella pneumoniae. Ann Clin Microbiol Antimicrob. (2017) 16:18. doi: 10.1186/s12941-017-0191-3
21. Tenner S, Vege SS, Sheth SG, Sauer B, Yang A, Conwell DL, et al. American College of gastroenterology guidelines: management of acute pancreatitis. Am J Gastroenterol. (2024) 119:419–37. doi: 10.14309/ajg.0000000000002645
22. Tenner S Baillie J DeWitt J Vege SS American American College of G. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. (2013) 108:1400–15. doi: 10.1038/ajg.2013.218
Keywords: acute pancreatitis, Klebsiella pneumoniae, carbapenem resistance, risk factor, mortality
Citation: Chen J, Xiang Q, Wu J-y, Zheng X-J and Jiang X-y (2025) Characteristics and risk factors for infection and mortality caused by Klebsiella pneumoniae in patients with acute pancreatitis. Front. Public Health 12:1533765. doi: 10.3389/fpubh.2024.1533765
Received: 24 November 2024; Accepted: 31 December 2024;
Published: 17 January 2025.
Edited by:
Fu Qiao, West China Hospital, Sichuan University, ChinaReviewed by:
Ata Nevzat Yalcin, Akdeniz University, TürkiyeMao E. N. Qiang, Shanghai Jiao Tong University, China
Copyright © 2025 Chen, Xiang, Wu, Zheng and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao-yan Jiang, Mjk1ODUwNzY0QHFxLmNvbQ==
 Jing Chen
Jing Chen Qian Xiang
Qian Xiang Jia-yu Wu
Jia-yu Wu