- 1College of Chinese Medicine, Changchun University of Chinese Medicine, Changchun, China
- 2College of Clinical Medicine, Changchun University of Chinese Medicine, Changchun, China
- 3Center of Children's Clinic, The Affiliated Hospital to Changchun University of Chinese Medicine, Changchun, China
- 4Chinese Medicine Physician Qualification Certification Center, National Administration of Traditional Chinese Medicine, Beijing, China
Antibiotic resistance is one of the greatest threats to human health, especially children's health. Traditional Chinese medicine encompasses several documented treatments for pediatric infectious diseases. The antibacterial efficacy and potential of traditional Chinese medicine to reverse bacterial resistance are gaining increasing research attention. This study explores the strategies that have been used to implement traditional Chinese medicine to optimize antibiotic use and reduce the burden of antibiotic resistance in children, as well as the challenges encountered. The findings emphasize the necessity for the Chinese government and the health community to take coordinated action, leveraging the unique strengths of traditional Chinese medicine to address the global health challenge posed by antibiotic resistance.
1 Introduction
Antibiotic resistance is one of the greatest threats to human health. A recent study investigating the global burden of antimicrobial resistance showed that an estimated 1.14 million deaths occurred as a result of antibiotic resistance in 2021, and this number is expected to reach 1.91 million by 2050 (1). Antibiotic overuse and misuse are the primary drivers of antibiotic resistance. Therefore, identifying methods to optimize antibiotic use and reduce the burden of antibiotic resistance is crucial.
A recent survey showed that the prevalence of antibiotic use in Chinese children is high. Specifically, the overall prevalence of antibiotic use among outpatients was 63.8%, among inpatients was 81.3%, and at home was 37.8% (2). The 2023 National Antimicrobial Resistance Surveillance Report showed that the detection rates of erythromycin-resistant Streptococcus pneumoniae and methicillin-resistant coagulase-negative staphylococci in children were 88.1% and 75%, respectively (3). Notably, the prevalence of erythromycin-resistant Streptococcus pneumoniae in children was higher than in adults and older adults (3). Given the special physiological characteristics of children, antibiotic abuse and misuse not only increase the burden of antibiotic resistance, but they also lead to adverse events and drug toxicity (4). Therefore, optimizing antibiotic use and reducing antibiotic resistance in children has become an urgent problem that needs to be addressed (5, 6). In line with the objectives of the World Health Organization's Global Action Plan on Antimicrobial Resistance, the Chinese government attaches great importance to the issue of antimicrobial drug resistance.
2 Current strategies of the Chinese government
Traditional Chinese medicine (TCM) is one of the popularly applied health resources across the globe (7). The antimicrobial effects of Chinese herbal medicines and their ability to facilitate the reversal of bacterial drug resistance have become international research hotspots in recent years (8). Chinese researchers have collaborated with the Karolinska Institute in Sweden and the University of Southampton in the United Kingdom to conduct research on the application of TCMs to address the issue of global antibiotic resistance (9, 10).
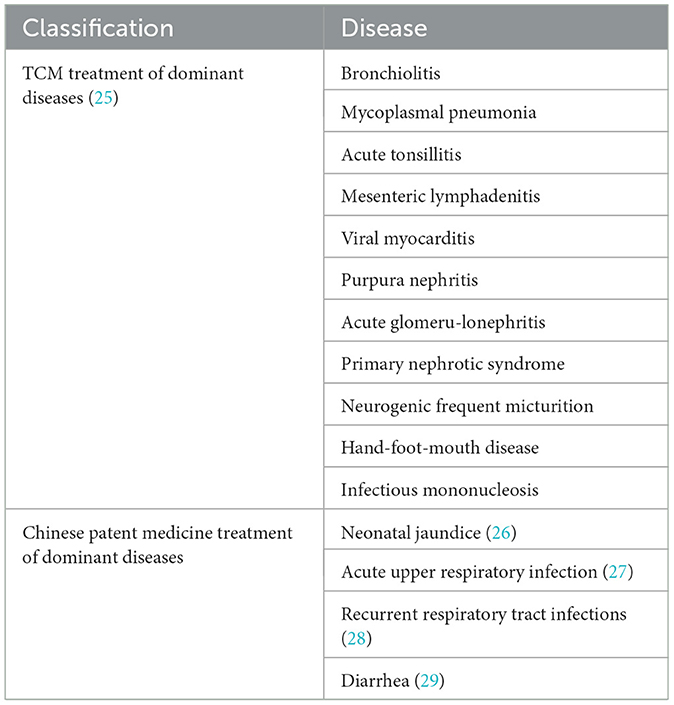
China has an original advantage in TCM, which is a scientific and technological resource (11). The Chinese government strongly promotes research that contributes to improving the understanding of the role of TCMs in reducing antibiotic use and antimicrobial resistance in children. With the support of the National Key Research and Development Program of China, TCM researchers have conducted demonstration studies on the use of TCMs to reduce antibiotic use for bacterial infectious diseases in children (12). The aim of this demonstration study was to clarify the efficacy and mechanism of action of TCMs and to use this understanding to formulate guidelines for the clinical application of TCMs and produce guiding principles for the co-administration of antibiotics with TCMs. Additionally, with funding from various TCM research projects, TCM researchers have conducted a series of clinical studies, showing that TCM can effectively reduce the reliance on antibiotics and decrease antibiotic resistance in children (13–24) (Table 1).With respect to clinical guideline development, the National Administration of Traditional Chinese Medicine has actively promoted the formulation of 11 diagnosis and treatment plans for dominant pediatric diseases using TCM (25), as well as four guidelines for the clinical application of Chinese patent medicines in treating these diseases (26–29) (Table 2). Furthermore, the China Association of Chinese Medicine has published the “Clinical Practice Guideline on Traditional Chinese Medicine Alone or Combined with Antibiotics for Patients with Acute Upper Respiratory Infection in Children” (30). Additionally, the World Federation of Chinese Medicine Societies has initiated the development of “Clinical Guidelines on Traditional Chinese Medicine Alone or Combined with Antibiotics for Children with Bacterial Acute Tonsillitis, Acute Bacterial Infectious Diarrhea, Acute Bacterial Infectious of the Lower Urinary Tract, and Bacterial Pneumonia” (31).
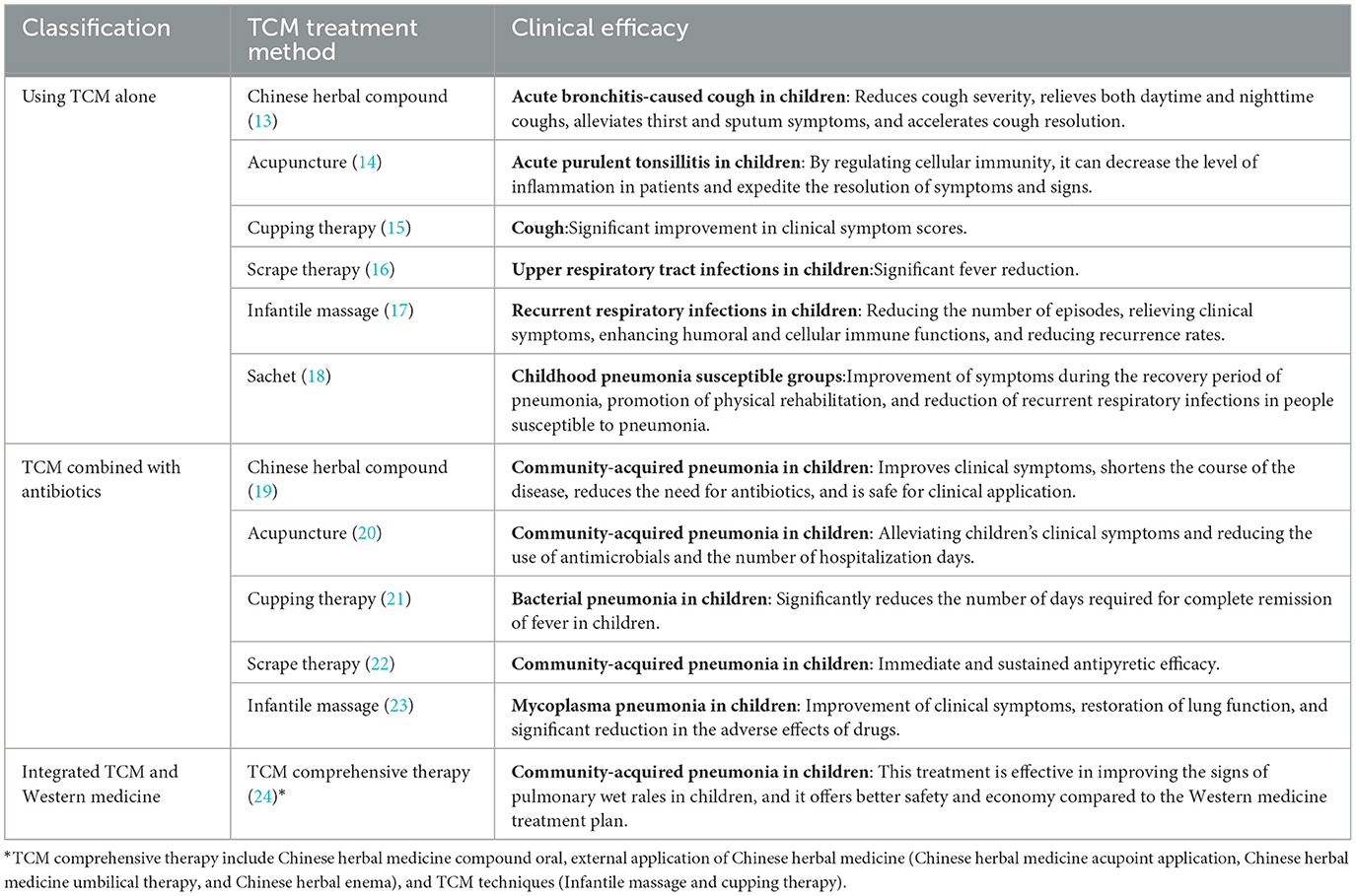
Table 1. Clinical efficacy of TCM: exemplified by the treatment of respiratory diseases in children.
In terms of policy support, the Chinese government formulated the Implementation Plan for Promoting Traditional Chinese Medicine in the Field of Maternal and Child Health (2021–2025) (32), which encourages the strengthening and optimization of TCM in the field of pediatrics. It encourages the screening of diseases for which TCMs may have significant advantages and good clinical efficacy. Moreover, the plan promotes the use of the “Guidelines for the Use of Traditional Chinese Medicine Medical Techniques and Chinese Patent Medicines in Pediatrics”(33) and supports the in-depth fusion of disease prevention using TCM with children's healthcare services. The Action Plan to Improve Child Health (2021–2025) has been issued (34), which focuses on strengthening TCM services for children and promoting TCM healthcare for children, both within households and in the community as a whole. Continuing to develop and refine the National Action Plan to Contain Antimicrobial Resistance (2022–2025) (35), emphasizes the urgency of strengthening research to develop antibiotics that are suitable for children. Moreover, it specifically mentions the importance of developing Chinese patent medicines as alternative antimicrobials.The Opinions on Promoting the High-quality Development of Children's Medical and Health Services has also been issued (36), giving thorough insights into the distinctive advantages of TCM in safeguarding children's health.
3 Challenges
Fully harnessing the benefits of TCM in safeguarding children's health still faces challenges. The latest China Statistical Yearbook of Chinese Medicine indicates that there are only 0.518 practicing (assistant) TCM physicians per 1,000 people in China (37), but this number is too small to effectively meet the healthcare needs of children. A national survey evaluating the healthcare service capabilities of grassroots physicians revealed that the competency rate for providing TCM services among these physicians is only 52.7% (38), indicating that the capacity for TCM services at the grassroots level is relatively low. Moreover, the health promotion and popularization of TCM are insufficient, as recent survey data indicate that the level of TCM health literacy of Chinese citizens in 2023 was only 24.62%, with television remaining the primary channel for disseminating TCM health knowledge to the general public (39). In addition, among the seven published clinical practice guidelines on TCM alone or combined with antibiotics to treat common infectious diseases, only one is specific to children (30). Therefore, the existing clinical guidelines are not sufficient to meet clinical needs.
4 Future directions
To fully leverage the unique advantages of TCM in reducing antibiotic use in children and lessening the burden of antibiotic resistance, the Chinese government and health community must take coordinated action. First, the size of the TCM workforce should be continuously expanded, and more TCM professionals, especially TCM pediatricians, should be trained to meet the health needs of children with respect to the provision of TCM. Second, the training of grassroots physicians in the knowledge and skills required for the provision of TCM should be strengthened. Moreover, appropriate technology for facilitating the delivery of TCM to children should be promoted. Additionally, the capacity of grassroots medical and health institutions to provide children's TCM services should be strengthened, and children's TCM health services that are equivalent in quality between urban and rural areas should be developed. Third, channels for the dissemination of TCM health knowledge need to be innovated, and new media should be fully leveraged to emphasize the advantages of TCM in the context of children's health among citizens and the community, which would in turn increase the awareness and acceptance of TCM. Moreover, TCM health culture should be comprehensively incorporated into the curricula of primary and secondary schools to cultivate healthy living concepts and lifestyle habits among students. Finally, the development of more clinical practice guidelines on the use of TCM alone or in combination with antibiotics for the treatment of common infectious diseases in children should be prioritized to standardize the clinical use of TCM as a therapeutic approach.
5 Conclusion
TCM plays an irreplaceable role in optimizing antibiotic use and reducing the burden of antibiotic resistance in children. The joint efforts of the Chinese government and the health community will help promote the use of TCM, bringing it to the front line of primary healthcare for children. This will be conducive to lowering healthcare costs, reducing the reliance of physicians on antibiotics when treating pediatric diseases, and preventing the emergence of an even more widespread problem of antibiotic resistance. TCM is not only highly important for enhancing the health of Chinese children, but it also contributes positively to the vigorous improvement of children's health worldwide.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
ZX: Investigation, Writing – original draft. YZ: Investigation, Writing – original draft. LW: Methodology, Writing – original draft. TT: Visualization, Writing – original draft. JW: Visualization, Writing – original draft. AJ: Conceptualization, Writing – review & editing. LS: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Key Research and Development Program of China (No. 2017YFC1703202), National Natural Science Foundation of China (No. 82374522), Health Science and Technology Capacity improvement Project of Jilin Province (No. 2022JC042), and the Academic Inheritance and Communication Project of the China Academy of Chinese Medical Sciences (No. CI2022E001XB).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. GBD 2021 Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance 1990-2021: a systematic analysis with forecasts to 2050. Lancet. (2024) 404:1199–226.
2. Guo S, Sun Q, Zhao X, Shen L, Zhen X. Prevalence and risk factors for antibiotic utilization in Chinese children. BMC Pediatr. (2021) 21:255. doi: 10.1186/s12887-021-02706-z
3. China Antimicrobial Resistance Surveillance System. National Antimicrobial Resistance Surveillance Report 2023 (Brief Version). (2024). Available at: https://www.carss.cn/Report/Details/978 (accessed November 28, 2024).
4. Rogawski ET, Platts-Mills JA, Seidman JC, John S, Mahfuz M, Ulak M, et al. Use of antibiotics in children younger than two years in eight countries: a prospective cohort study. Bull World Health Organ. (2017) 95:49–61. doi: 10.2471/BLT.16.176123
5. Yin X, Song F, Gong Y, Tu X, Wang Y, Cao S, et al. A systematic review of antibiotic utilization in China. J Antimicrob Chemother. (2013) 68:2445–52. doi: 10.1093/jac/dkt223
6. Medernach RL, Logan LK. The growing threat of antibiotic resistance in children. Infect Dis Clin North Am. (2018) 32:1–17. doi: 10.1016/j.idc.2017.11.001
7. WHO. WHO International Standard Terminologies on Traditional Chinese Medicine. Geneva: World Health Organization. (2022).
8. Su T, Qiu Y, Hua X, Ye B, Luo H, Liu D, et al. Novel opportunity to reverse antibiotic resistance: to explore traditional chinese medicine with potential activity against antibiotics-resistance bacteria. Front Microbiol. (2020) 11:610070. doi: 10.3389/fmicb.2020.610070
9. China Net of Traditional Chinese Medicine. Traditional Chinese Medicine “Rooted” in the Birthplace of the Nobel Prize in Medicine on the Internationalization of a New Starting Point. (2017). Available at: http://www.cntcm.com.cn/news.html?aid=126423 (accessed November 28, 2024).
10. Global Network for Anti-Microbial Resistance and Infection Prevention. UK-China Project to Tackle Antimicrobial Resistance. Available at: https://www.southampton.ac.uk/namrip/research/ecr-posters/xiao-yang-hu-poster.page (accessed November 28, 2024).
11. The State Council Information Office of the People's Republic of China. Traditional Chinese Medicine in China. (2016). Available at: https://english.http://www.gov.cn/archive/white_paper/2016/12/06/content_281475509333700.htm (accessed November 28, 2024).
12. National Science and Technology Information System. Demonstration Study on the use of Antibiotics in Reducing Bacterial Infectious Diseases in Children with Traditional Chinese Medicine. (2019). Available at: https://www.nstrs.cn (accessed October 11, 2024).
13. Liu J, Wang M, Jin X, Chi Y, Ma C, Liu X, et al. Evaluation of the efficacy and safety of Xiao'er Huangjin Zhike Granules in the treatment of acute bronchitis-caused cough (syndrome of phlegm-heat obstructing the lung) in children. Chin J Appl Clini Pediat. (2024) 39:774–79. doi: 10.3760/cma.j.cn101070-20240620-00390
14. Feng H, Xi L, Guo K, Zhao X, Li Y. Therapeutic observation of bloodletting plus Chinese medication in treating acute suppurative tonsillitis in children. Shanghai J Acupunct Moxibus. (2024) 43:719–24. doi: 10.13460/j.issn.1005-0957.2024.07.0719
15. Zhao L. Cupping at Feishu acupoint for the treatment of pediatric phlegm-dampness-embedded lung cough in 50 cases. Chin J Ethnomed Ethnopharm. (2017) 26:104–6.
16. Xu S. Clinical efficacy and timeliness of scraping at the Shoulder Well point in the treatment of 30 cases of pediatric exogenous fever. Jiangsu J Tradit Chin Med. (2012) 44:60–1.
17. Xia T, Fu J, Tang H, Chu A, Pang J. Clinical observation on the effect of Tuina in prevention and treatment of recurrent respiratory infection induced by pediatric lung Qi deficiency. J Nanj Univers Trad Chin Med. (2018) 34:273–6. doi: 10.14148/j.issn.1672-0482.2018.0273
18. Wang L, Li J, Zhou Z, Cai X, Mo X, Cai Y. Study on the intervention effect of disease-preventing sachet of Zhuang medicine on susceptible people with pneumonia in children. J Guangxi Univer Chin Med. (2019) 22:29–34.
19. Wei R, Lyu J, Li X, Yuan F, Wang L, Wu L, et al. Randomized, double-blind, single-simulation, placebo-controlled, multicenter clinical trial of An'erning granules in reducing use of antibiotics for children's community-acquired pneumonia. Chin J Exp Tradi Med Formu. (2022) 28:105–114. doi: 10.13422/j.cnki.syfjx.20221994
20. Qiao M, Liu L, Xu D, Luo Z, Gu Y. Acupuncture at Sifeng (EX-UE 10) as adjuvant treatment for pneumonia of phlegm-heat blocking lung type in children: a randomized controlled tria. Chin Acupunct Moxibust. (2020) 40:1076–80. doi: 10.13703/j.0255-2930.20200302-k0001
21. Xu Y, Cui S, Bai L, Yang J, Li J, Xie T, et al. Cupping treatment combined with antibiotics for bacterial pneumonia in children: a randomized controlled trial. Chin Acupunct Moxibust. (2021) 41:283–7. doi: 10.13703/j.0255-2930.20200804-k0004
22. Zhang N, Chen H, Wu L, Liao X. Study on the Intervention Effect of Bladder Meridian Scraping on the Antifebrile Effect of Pneumonia in Children. Jiangsu Journal of Traditional Chinese Medicine. (2021) 53:46–49. doi: 10.19844/j.cnki.1672-397X.2021.12.016
23. Wang X. Observation on the efficacy of infantile massage combined with azithromycin sequential treatment of Mycoplasma pneumoniae pneumonitis. Yunnan J Tradit Chin Med Materia Medica. (2022) 43:68–70. doi: 10.16254/j.cnki.53-1120/r.2022.02.021
24. Zhao X, Wang X, Shen K, Liu J, Shang Y, Cui Z, et al. Comparative study of integrated traditional chinese and western medicine versus western medicine for children's community-acquired pneumonia: a prospective cohort. J Tradit Chin Med. (2022) 63:1745–52. doi: 10.13288/j.11-2166/r.2022.18.009
25. National Administration of Traditional Chinese Medicine. Circular of the Office of the National Administration of Traditional Chinese Medicine on the Implementation of Traditional Chinese Medicine Clinical Paths and Traditional Chinese Medicine Diagnosis and Treatment Plans for 95 Traditional Chinese Medicine Dominant Diseases, Including Wind-Temperature and Lung-Heat Disease (Severe Pneumonia). (2019). Available at: http://www.natcm.gov.cn/yizhengsi/zhengcewenjian/2019-01-21/8896.html (accessed November 28, 2024).
26. Standardization Project Group of Guidelines for Clinical Application of Chinese Patent Medicines in Treating Dominant Diseases. Guidelines on the clinical application of chinese patent medicines for the treatment of neonatal jaundice 2020. Chin J Integ Tradi Western Med. (2021) 41:280–5. doi: 10.7661/j.cjim.20210114.161
27. Standardization Project Group of Guidelines for Clinical Application of Chinese Patent Medicines in Treating Dominant Diseases. Guidelines on the clinical application of chinese patent medicines for the treatment of acute upper respiratory infection in children 2020. Chin J Integ Tradi Western Med. (2021) 41:143–50. doi: 10.7661/j.cjim.20210120.135
28. Standardization Project Group of Guidelines for Clinical Application of Chinese Patent Medicines in Treating Dominant Diseases. Guidelines on the clinical application of chinese patent medicines for the treatment of recurrent respiratory tract infections in children 2021. Chin J Integ Tradi Western Med. (2022) 42:133–42. doi: 10.7661/j.cjim.20211224.196
29. Standardization Project Group of Guidelines for Clinical Application of Chinese Patent Medicines in Treating Dominant Diseases. Guidelines on the clinical application of chinese patent medicines for the treatment of diarrhea in children 2021. Chin J Integ Tradi Western Med. (2022) 42:915–21. doi: 10.7661/j.cjim.20220318.039
30. China Association of Chinese Medicine. Announcement for 7 Standards Including “Clinical Practice Guideline on Traditional Chinese Medicine Alone or Combined with Antibiotics for Patients with Community Acquired Pneumonia”. (2017). Available at: https://www.cacm.org.cn/2017/06/07/4787/ (accessed October 11, 2024).
31. World Federation of Chinese Medicine Societies. World Federation of Chinese Medicine Societies Announcement for International Standards. (2019). Available at: http://en.wfcms.org/index.php/show/21/2733.html (accessed October 11, 2024).
32. National Administration of Traditional Chinese Medicine. Circular on the Issuance of the Implementation Plan for Promoting Traditional Chinese Medicine in the Field of Maternal and Child Health (2021–2025). (2021). Available at: http://www.natcm.gov.cn/yizhengsi/zhengcewenjian/2021-04-29/21627.html (accessed November 28, 2024).
33. National Health and Family Planning Commission Maternal and Child Health Service Department and and National Administration of Traditional Chinese Medicine Medical Administration Department. Guidelines for the Use of Traditional Chinese Medicine Medical Techniques and Chinese Patent Medicines in Pediatrics. Beijing: China Press of Chinese Medicine. (2015).
34. The National Health Commission. Circular of the National Health Commission on the Issuance of the Action Plan to Improve Child Health (2021–2025). (2021). Available at: https://www.gov.cn/zhengce/zhengceku/2021-11/05/content_5649019.htm (accessed November 28, 2024).
35. The National Health Commission. Circular on the issuance of the National Action Plan to Contain Antimicrobial Resistance (2022–2025). (2022). http://www.nhc.gov.cn/yzygj/s7659/202210//2875ad7e2b2e46a2a672240ed9ee750f.shtml (accessed November 28, 2024).
36. The National Health Commission. The Opinions on Promoting the High-quality Development of Children's Medical and Health Services. (2024). Available at: https://www.gov.cn/zhengce/zhengceku/202401/content_6925268.htm (accessed November 28, 2024).
37. National Administration of Traditional Chinese Medicine. China Statistical Yearbook of Chinese Medicine. (2021). Available at: http://www.natcm.gov.cn/ (accessed October 11, 2024).
38. Lian L, Chen J, Wang X, Li Y, Zhu Y. Current situation and countermeasure of medical service capacity of primary care physicians in China. Chinese General Pract. (2023) 26:4246–53. doi: 10.12114/j.issn.1007-9572.2023.0289
39. China News of Traditional Chinese Medicine. The Level of Health Literacy of Chinese Citizens in Traditional Chinese Medicine Continues to Grow. (2024). Available at: http://paper.cntcm.com.cn/bz/html/index.html?date=2024-07-31&pageIndex=1&cid=1 (accessed October 11, 2024).
Keywords: traditional Chinese medicine, antibiotic, antibiotic resistance, pediatrics, children
Citation: Xue Z, Zheng Y, Wei L, Tian T, Wu J, Jin A and Sun L (2024) Traditional Chinese medicine strategies to optimize antibiotic use and reduce the burden of antibiotic resistance in Chinese children. Front. Public Health 12:1530018. doi: 10.3389/fpubh.2024.1530018
Received: 18 November 2024; Accepted: 10 December 2024;
Published: 19 December 2024.
Edited by:
Karolina Sobczyk, Medical University of Silesia, PolandReviewed by:
Jatindra Nath Mohanty, Centurion University of Technology and Management, IndiaEsraa Halawa, Cairo University, Egypt
Rabiya Khan, Shri Mata Vaishno Devi University, India
Copyright © 2024 Xue, Zheng, Wei, Tian, Wu, Jin and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aning Jin, SmluYW5pbmdAcXEuY29t; Liping Sun, c2xwY2N6eXlkeEBzaW5hLmNvbQ==
 Zhilong Xue
Zhilong Xue Yanzhi Zheng
Yanzhi Zheng Lina Wei1,3
Lina Wei1,3 Liping Sun
Liping Sun