
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 14 January 2025
Sec. Public Health and Nutrition
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1514522
This article is part of the Research Topic Health and Nutrition in The First 1000 Days of Life View all 10 articles
Purpose: This study evaluates the effectiveness of rural maternal health services in improving pregnant women’s health knowledge, practices, and outcomes in northwestern China, focusing on the roles of received public services and policy awareness.
Methods: Baseline surveys were conducted in rural Shaanxi Province in 2021 and 2023, involving 1,152 pregnant women from 85 townships, selected via multistage cluster random sampling. Data were collected through structured face-to-face interviews, covering health knowledge and behaviors. Statistical analyses were performed to assess the impact of maternal health services.
Results: Both received public services (Coefficient: 0.130, 95% CI: 0.015–0.246) and policy awareness (Coefficient: 0.114, 95% CI: 0.001–0.227) significantly improved nutrition and health knowledge but had limited impact on prenatal checkups or health outcomes. Policy awareness (OR: 3.826, 95% CI: 2.743–5.337) significantly increased picking up free folic acid, however, the rate of taking folic acid remained low.
Conclusion: While received public services and policy awareness improved nutrition and health knowledge, and policy awareness increased picking up free folic acid, they did not significantly influence prenatal checkups or health outcomes. More targeted efforts are needed to foster consistent health practices and improve maternal health outcomes in rural areas.
Maternal health is widely recognized as a cornerstone of infant nutrition, health, and development (1, 2). Ensuring the well-being of pregnant women has profound implications not only for birth outcomes but also for the long-term health of the next generation. The Developmental Origins of Health and Disease (DOHaD) theory posits that a mother’s health during pregnancy can have lasting effects on a child’s future health, influencing risks for conditions such as obesity, cardiovascular disease, and diabetes (3, 4). For example, folic acid deficiency during early pregnancy has been proven to be associated with neural tube defects in newborns (5, 6), while anemia during pregnancy has been extensively associated with adverse outcomes, including low birth weight, preterm birth, and maternal mortality (7–9).
Public health interventions, particularly those targeting maternal health, are vital in reducing these risks. Iron and folic acid supplementation (IFAS), along with regular prenatal checkups, has been shown to significantly improve maternal and infant health outcomes (10–13). These services can mitigate complications and enhance birth outcomes by addressing nutritional deficiencies and monitoring maternal health throughout pregnancy (14–17). In response, many countries have implemented policies to enhance maternal health, including mandatory food fortification and free supplementation programs (18). Brazil, Mexico, and Canada, for instance, have enforced food fortification policies to increase iron intake (19), while Kenya provides free iron and folic acid supplements to pregnant women through its IFAS program (20). India’s National Rural Health Mission offers free prenatal checkups and educates pregnant women through community health workers (21).
China has also taken significant steps to improve maternal and child health. In 2009, the government started to distribute free folic acid supplements to women of childbearing age nationwide (22). In 2010, China launched the National Free Preconception Health Examination Program, ensuring that all pregnant women have access to essential prenatal care services (23). Currently, pregnant women are eligible to receive five free prenatal checkups at designated public hospitals, community health centers, or township clinics. However, despite these efforts, significant challenges remain in improving maternal health knowledge, behaviors, and outcomes—particularly in rural areas. Research indicates that antenatal care visits are significantly more common in urban areas, with a rate of 76–77%, compared to only 46% in rural areas, highlighting a substantial disparity in the utilization of maternal and child health services (24, 25).
In rural China, health services and folic acid supplements are underutilized despite their availability. For example, only 44.5% of participants in one study took free folic acid supplements before and during pregnancy, even though 76.4% received the supplements free of charge (26, 27). Similar studies (28, 29) highlighted persistent maternal health challenges, including higher rates of anemia (43–46% in rural areas vs. 30–35% in urban areas), malnutrition, and postpartum depression (13% prevalence). These findings suggest that improving maternal health outcomes requires more than service provision––it also demands addressing gaps in health knowledge and behaviors.
Exploring pregnant women’s health knowledge and behaviors is therefore essential. While previous studies have examined maternal nutrition and health knowledge, health behaviors, and overall health outcomes, they often focus on demographic and socioeconomic factors (30–33), leaving other influences, such as the effectiveness of public health management practices, underexplored. Several studies suggest that maternal and child health services can improve pregnant women’s knowledge of nutrition and health (34–36), but few have specifically analyzed how these services function in rural China.
This study aims to address this research gap by examining the health knowledge, behaviors, and outcomes of pregnant women in rural northwest China, with a particular focus on how maternal health services impact these outcomes. We first describe the women’s nutritional health knowledge, health behaviors (including prenatal checkups, picking up free folic acid, and taking folic acid), and health outcomes. Then, we analyze whether and how received public services and policy awareness influence these aspects, ultimately evaluating the effectiveness of maternal health services in rural China. By identifying key factors that affect maternal health in rural regions, this study provides valuable insights for policymakers seeking to improve health outcomes for pregnant women in these areas.
The data used in this study were drawn from baseline surveys on maternal and infant nutrition and health, conducted by Shaanxi Normal University in rural areas of Shaanxi Province in 2021 and 2023. The project was carried out in five cities across central and southern Shaanxi, with two counties randomly selected from each city, totaling ten counties. Surveys were conducted among rural pregnant women in March 2021, December 2021, and March 2023.
We employed a multistage cluster random sampling method to identify potential participants. The sampling process involved three main steps: first, selecting 10 economically disadvantaged counties from 5 prefecture-level cities in central and southern Shaanxi Province. In each county, the township where the county government is located was excluded due to its higher economic and urbanization levels. Townships were either fully included or randomly sampled if exceeding 10. For ethical and practical reasons, and to ensure the participants were representative of the target population, the inclusion criteria for our participants were as follows: (1) aged between 28 and 40 years; (2) had resided in the locality for at least 2 years; (3) had no history of mental illness or other severe health conditions; (4) priority was given to pregnant women with younger gestational ages. After completing the four sampling steps and excluding cases with missing key variables, the final valid sample for analysis consisted of 1,152 pregnant women from 85 townships in 10 counties. This included 592 cases from March 2021, 228 cases from December 2021, and 332 cases from March 2023.
In this study, a questionnaire survey method was employed, with trained interviewers conducting face-to-face interviews with each participant. The questionnaire included information on the pregnant women’s sociodemographic characteristics, health status, prenatal checkups, and folic acid intake. Prior to the interviews, informed consent forms were distributed to eligible participants, detailing the project’s objectives, procedures, potential risks, benefits, and privacy protection. To ensure accuracy and consistency during data collection, interviewers underwent centralized training, and a pre-survey was conducted with 20 participants before the large-scale data collection. All interview questions were displayed on tablets, with interviewers asking questions one by one while recording the answers. Each interview was conducted privately between the interviewer and the pregnant woman to prevent interference from other family members.
The dependent variables in this study involve three aspects of pregnant women’s health: health knowledge, practices, and outcomes. Specifically, these include nutrition and health knowledge, prenatal checkups, picking up free folic acid, taking of folic acid, and health outcomes. The nutrition and health knowledge of pregnant women was assessed using a questionnaire consisting of 24 items, with 12 questions addressing maternal nutrition and health, and 12 focusing on neonatal feeding. Each item provides 4–5 answer choices, including one correct answer, one “Do not know” option, and others serving as distractors. One correct answer is awarded one point, yielding a maximum score of 24. Consequently, the nutrition and health knowledge score is treated as a continuous variable. For statistical analyses, the knowledge scores were standardized to ensure comparability across models. Prenatal checkups is defined according to the frequency recommended by the “Guidelines for Preconception and Prenatal Care (2018),” which suggests 7 to 11 checkups during pregnancy, with additional visits for high-risk pregnancies. It is calculated based on participants’ self-reported number of prenatal checkups. If the number of checkups reported meets or exceeds the recommended frequency, the variable is assigned a value of 1; otherwise, it is assigned a value of 0. The variables picking up free folic and taking folic acid are defined based on two distinct survey questions. For picking up free folic, the question is, “Have you picked up free folic acid?” For taking folic acid, the question is, “Have you taken folic acid before or during this pregnancy?” Respondents who answered “Yes” are assigned a value of 1, while those who answered “No” are assigned a value of 0. The variable health outcomes is constructed based on six recent symptoms from the questionnaire and anemia status. Recent symptoms include fever, sore throat, cough, diarrhea, stomach pain, asthma, headache or dizziness, and joint or muscle pain, with each “Yes” response scored as 1 and “No” as 0. Anemia status, determined by hemoglobin levels (37), is scored as 1 for anemia and 0 for non-anemia. These variables were summed to generate the variable health outcomes (range: 0–7), with higher scores indicating poorer health outcomes.
The independent variables in this study include two sub-dimensions of maternal health services: received public services and policy awareness. Received public services and policy awareness are defined based on two distinct survey questions. For received public services, the question is, “During your pregnancy and early childhood of your baby (e.g., vaccinations, check-ups), has anyone provided management services for you, such as notifications, reminders, or consultations?” For policy awareness, the question is, “Were you ever informed that you could receive free folic acid supplements and advised to attend prenatal checkups?” Respondents who answered “Yes” are assigned a value of 1, while those who answered “No” are assigned a value of 0.
The control variables in this study encompass characteristics of pregnant women at three levels: individual, household, and social. At the individual level, the characteristics include age, trimesters, body mass index (BMI; in weight (kg)/height (m)2), completed compulsory education, first pregnancy, and employed. Trimesters is treated as a categorical variable, with values assigned as follows: 0 for the first trimester, 1 for the second trimester, and 2 for the third trimester. BMI is calculated by dividing weight (in kilograms) by the square of height (in meters), measured using standardized scales and measuring tapes under the guidance of local nurses. According to the weight classification criteria for adults outlined in the health industry standards of the People’s Republic of China, BMI is categorized into four groups: < 18.5 kg/m2, 18.5 kg/m2 ≤ BMI < 24.0 kg/m2, 24.0 kg/m2 ≤ BMI < 28.0 kg/m2, and ≥ 28.0 kg/m2. At the household level, we consider whether the pregnant woman resides with her husband and whether the family’s assets fall within the lowest 25% of the sample. The variable family assets in the lowest 25% is defined using an asset index constructed through Principal Component Analysis (PCA) (38), based on responses to nine binary questions about key household assets. Households with an asset index in the bottom quartile are assigned a value of 1, and all others are assigned 0. At the social level, factors include the distance between the pregnant woman’s primary residence and the hospital where she is registered, as well as the survey round. Survey round is treated as a categorical variable indicating the timing of surveys among rural pregnant women. Data were collected during three phases: 0 = March 2021, 1 = December 2021, and 2 = March 2023, with each phase involving different participants.
The data processing and statistical analyses in this study were performed using STATA 18.0 software. Categorical variables were summarized with frequency and percentage, while continuous variables were presented by the mean and standard deviation (SD) in descriptive analyses. Multiple linear regression analyses and multivariate logistic regression analyses were performed to test the relationship between maternal health services and dependent variables, including nutrition and health knowledge, health practices, and health outcomes. The statistical level of significance was p < 0.05 and the outcomes of regression analyses were presented as coefficients or odds ratios (ORs) with their 95% confidence intervals (CIs).
Table 1 presents the basic demographic characteristics of the 1,152 pregnant women included in this study. The average age of the respondents was 29.0 years (SD = 4.4). Over half of these women had not completed high compulsory education, and the majority (90.3%) did not have stable employment during their pregnancies. Additionally, 65.3% of the pregnant women were experiencing their first pregnancy, and 66.8% were in the second trimester.
In Table 2, we describe the status of maternal health services and pregnant women’s health knowledge, practices, and outcomes. Among the 1,152 pregnant women, 692 (60.1%) received public services during their pregnancies; however, 58.0% of the respondents remained unaware of maternal health services policies, including the provision of free folic acid and the promotion of prenatal checkups.
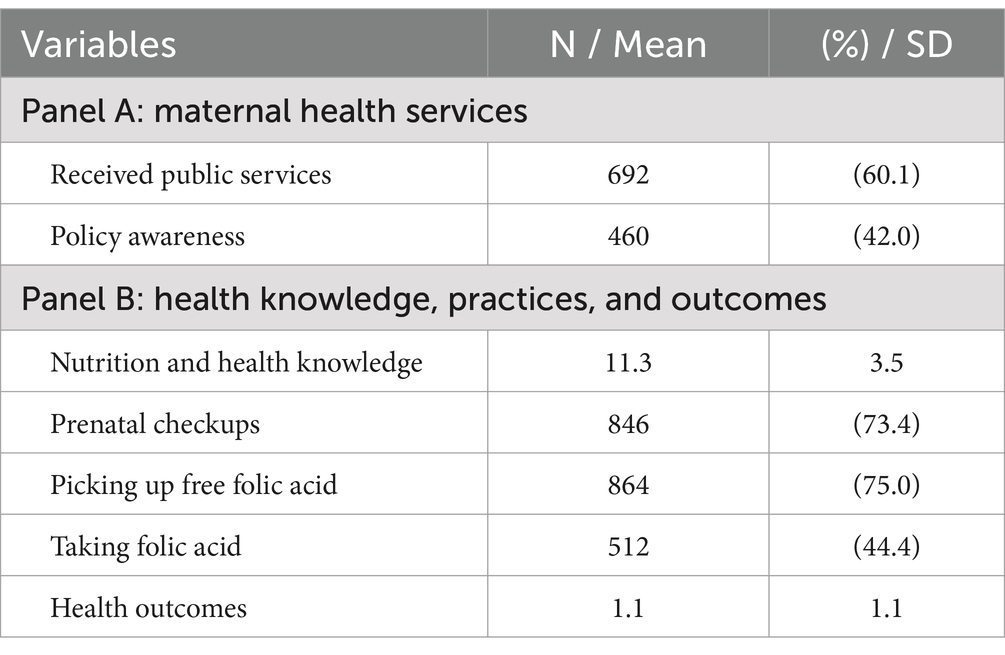
Table 2. Descriptive statistics of maternal health services and health knowledge, practices, and outcomes.
In terms of nutrition and health knowledge, the mean score was 11.3 (SD = 3.5). Among all 1,152 women, 864 (75.0%) reported having picked up free folic acid before or during pregnancy, and only 512 (44.4%) reported taking folic acid before or during this pregnancy. 73.4% of pregnant women underwent prenatal checkups. The mean health outcomes score of 1.1 indicated that, on average, pregnant women experienced just over one recent symptom or health issue from the assessed range of health problems.
The impact of maternal health services on pregnant women’s nutrition and health knowledge is illustrated in Table 3. Results show that both received public services (Coefficient: 0.130, 95% CI: 0.015–0.246) and policy awareness (Coefficient: 0.114, 95% CI: 0.001–0.227) were significantly associated with a positive impact on nutrition and health knowledge. Additionally, a higher level of nutrition and health knowledge was observed in expectant women with advanced educational qualifications, more affluent socioeconomic status, and steady employment, as well as those expecting their first child.
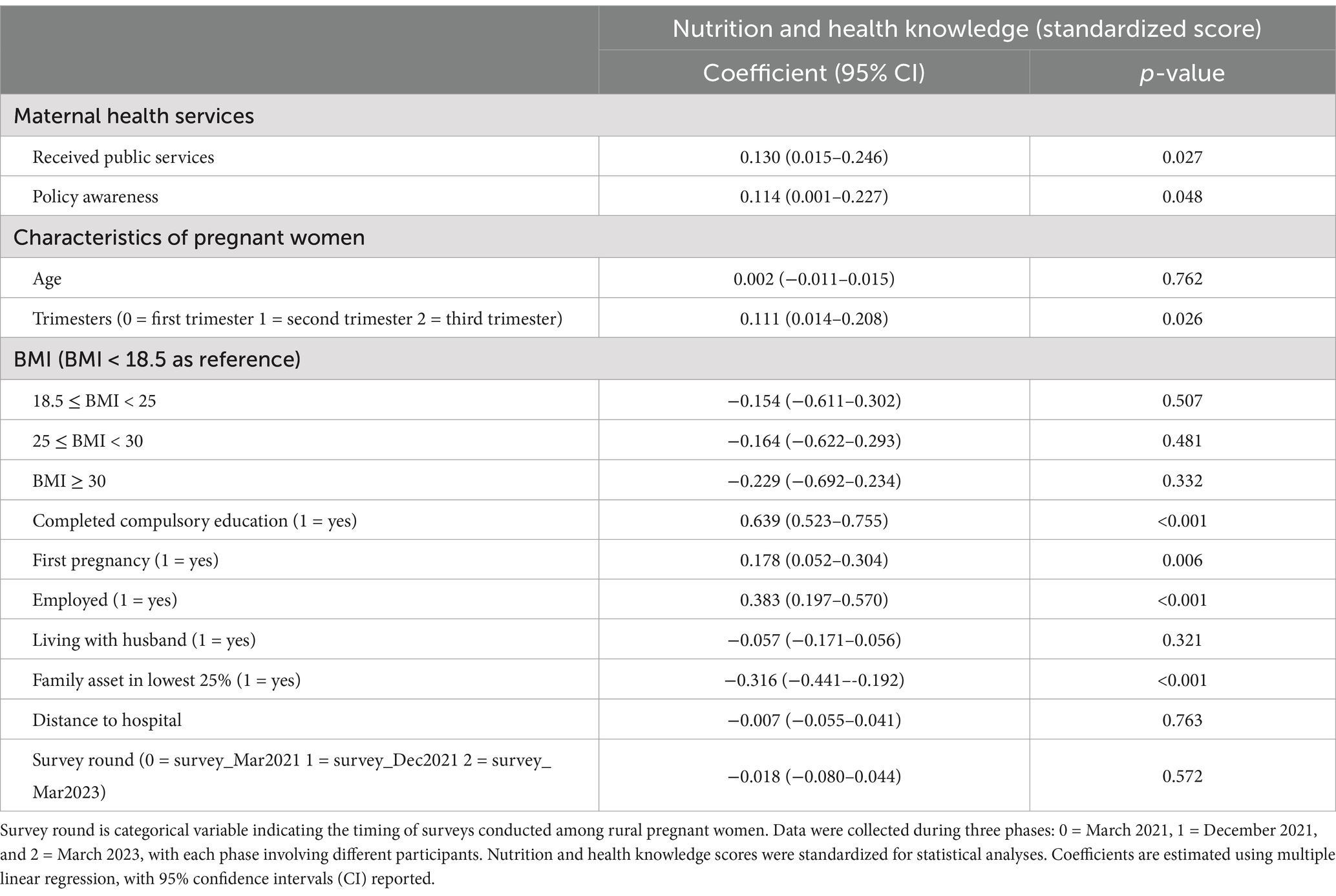
Table 3. Results of multiple linear regression analyses of variables related to nutrition and health knowledge.
Logistic regression analyses in Table 4 show that expectant women who were aware of the maternal health services policies had 3.8 times higher odds of picking up free folic acid (OR: 3.826, 95% CI: 2.743–5.337) than their counterparts and were more likely to take folic acid before or during this pregnancy (OR: 1.822, 95% CI: 1.409–2.356). Received public services showed no significant association with pregnant women’s health practices.
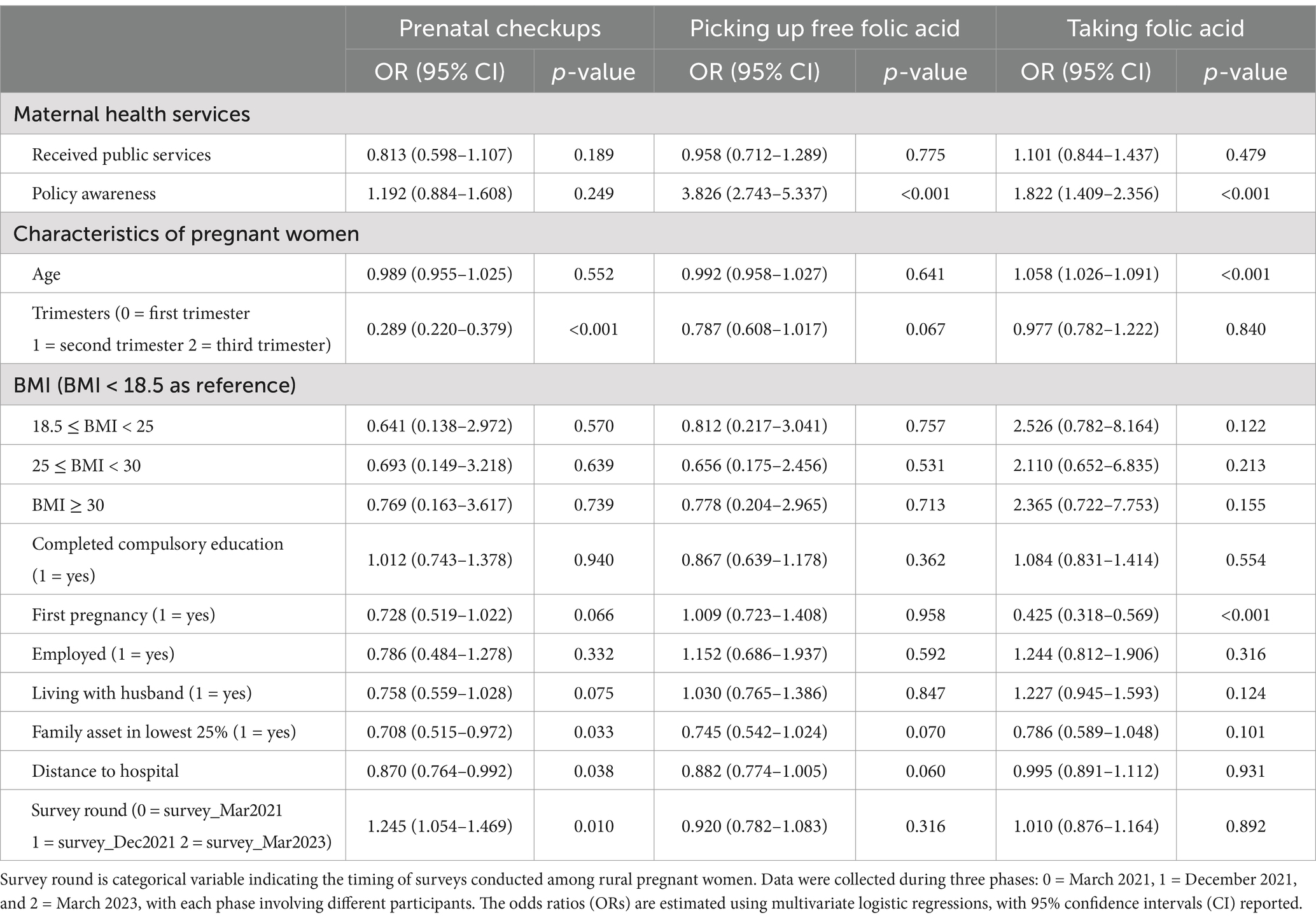
Table 4. Results of multivariate logistic regression analyses of variables related to health practices.
From the multiple linear regression analyses in Table 5, the results indicate that neither received public services nor policy awareness was significantly associated with improvements in the health outcomes of pregnant women. Most other variables were also not significantly associated with pregnant women’s health outcomes.
This study provides a comprehensive overview of the health of pregnant women in rural northwestern China by examining three key aspects: nutrition and health knowledge, health practices, and health outcomes. Additionally, it assesses the effectiveness of maternal health services, including received public services and policy awareness. The results highlight that low policy awareness is a major factor contributing to the low rate of folic acid consumption. While received public services and policy awareness are associated with improved nutritional and health knowledge, they do not significantly influence prenatal checkups or health outcomes. Notably, policy awareness is linked to higher rates of picking up free folic acid.
These findings are consistent with previous research showing that maternal health services, particularly received public services and policy awareness, can improve pregnant women’s nutrition and health knowledge (39–41). This suggests that the dissemination of information through health services is effective to some extent. We find that pregnant women’s nutrition and health knowledge may be related to pregnancy order, as first-time mothers appear to be more proactive in learning about maternal and infant health (35, 42), which could explain the association between first pregnancy and higher nutrition and health knowledge. However, our study also finds that the improved knowledge does not necessarily translate into better health behaviors or outcomes, which points to a gap between knowledge acquisition and behavior change.
The failure to translate received public services and policy awareness into improved health practices can be attributed to several factors, including limited economic resources and low educational attainment (43–46). Many rural women face barriers such as inadequate transportation, long distances to healthcare facilities, and high out-of-pocket costs for certain prenatal services, even when subsidies or free care are available. In some cases, traditional family practices take precedence over public health services (47), which may diminish the uptake of services like regular prenatal checkups. These barriers reduce the likelihood of consistent health service utilization and limit the effectiveness of maternal health programs in rural areas.
Although the rate of picking up free folic acid is relatively high, the actual usage among pregnant women remains suboptimal. This is in line with other studies conducted in rural areas (48, 49), where only 44.4% of women took folic acid before and during pregnancy, despite 75.0% having collected the supplements (26). This discrepancy suggests that a large portion of the free folic acid distributed may go unused. Behavioral economics, particularly the sunk cost theory, helps explain this phenomenon. According to the theory (50, 51), individuals are more likely to value and use products they have invested in, even when the cost is irrelevant to future use. Since free folic acid requires no financial investment, pregnant women may feel less motivated to consistently use it, despite its potential health benefits. This lack of cost creates a lower perceived value, which can lead to greater waste and lower adherence to recommended supplementation.
Our findings also suggest that policy awareness is critical in boosting both the collection and usage of free folic acid supplements among pregnant women. In rural areas, access to and consumption of folic acid is largely dependent on awareness of relevant health policies (52). This highlights the need for more effective dissemination strategies to ensure that women not only pick up the supplements but also use them appropriately. Therefore, enhancing policy dissemination and awareness campaigns is essential for increasing folic acid consumption and ultimately improving maternal health outcomes (53).
Despite the positive impact of policy awareness on health knowledge and supplement uptake, our study finds that neither received public services nor policy awareness significantly improves the overall health status of pregnant women. Research has shown that although most rural women in China are aware of the importance of prenatal care and folic acid supplementation, there remains a significant gap between awareness, practices, and actual health improvements (52, 54, 55). This gap can be better understood through the lens of perceived barriers (56). Perceived barriers refer to the tangible difficulties that hinder individuals from taking action, even when they understand the importance of health behaviors. Previous studies have identified that limited healthcare facilities, high costs, and transportation challenges often present significant obstacles for pregnant women seeking prenatal checkups or obtaining folic acid supplements (57–59). These practical factors may substantially diminish the effectiveness of public health services, as individuals may refrain from acting on their health knowledge if they perceive the effort to overcome these barriers as too burdensome (60).
Moreover, social norms play a critical role in shaping the health behaviors of pregnant women. In rural areas, traditional beliefs and customs can profoundly influence women’s decisions, even when they are well informed about the benefits of folic acid supplementation. Women may face resistance from family or community members, particularly when these individuals hold divergent health views or lack relevant knowledge (61). This phenomenon aligns with existing research, which demonstrates that health decisions are influenced not only by individual knowledge but also by social behaviors and collective expectations (62–64).
Bridging the gap between health knowledge and behaviors among pregnant women is an area deserving greater policy attention. This can be achieved by improving the accessibility of healthcare services and implementing family-centered health education programs, thereby reducing perceived barriers and reshaping social norms. These measures are vital to enhancing the effectiveness of maternal and child public health services in rural areas.
This study has several limitations. First, our research subjects are from rural areas in Shaanxi, China, so the findings may not be generalizable to other regions. Second, due to data limitations, we categorized received public services and policy awareness as binary variables based solely on participant responses. This simplified approach prevents us from capturing the quality of maternal health services, which may have impacted the accuracy and depth of our results to some extent. Future research should focus on incorporating service quality indicators to provide a more nuanced understanding of the effectiveness of maternal health programs in rural settings. Third, due to data limitations, we were unable to control for potential confounding variables such as access to healthcare beyond public services, cultural and social factors, and the level of family support, which might influence the study results. Future research should focus on more comprehensive data collection, incorporating qualitative research methods, and adopting stratified analyses or study designs with stronger causal inference to explore the role of these variables and further elucidate their mechanisms of influence. Fourth, as the data on pregnant women’s health practices and outcomes were collected retrospectively through self-reports, there is a possibility of recall bias, which may have affected the accuracy of the measurements.
In summary, our findings indicated that despite a high rate of picking up free folic acid, the actual taking of folic acid among rural pregnant women was unsatisfactory. Both received public services and policy awareness significantly enhanced the nutritional health knowledge of pregnant women. Additionally, policy awareness promoted picking up free folic acid and its taking. However, neither received public services nor policy awareness had a significant impact on prenatal checkups or the health outcomes of pregnant women.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
The study was approved by the Medical Ethics Committee of Shaanxi Normal University and Xi’an Jiaotong University of China (No: 2020-1240). Each eligible participant received a consent form with information regarding program objectives, procedures, potential risks, benefits, and an explanation of privacy protection. Participants provided informed consent for inclusion in the study before engaging in a face-to-face interview with a single enumerator.
JY: Writing – original draft, Writing – review & editing. JC: Data curation, Writing – review & editing. YX: Writing – review & editing. YuL: Writing – review & editing. JW: Investigation, Writing – review & editing. YaL: Investigation, Writing – review & editing. JN: Project administration, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was funded by the 111 Project (Grant No. B16031); Major project of National Social Science Foundation (Grant No. 21&ZD112); Humanities and Social Science Research Project of Ministry of Education (Grant No. 22YJC840023); Excellent Graduate Training Program of Shaanxi Normal University (Grant No. LHRCTS23019).
We extend our gratitude to the researchers from Shaanxi Normal University for their valuable assistance in developing the study protocol. We also sincerely thank all the respondents who participated in this study and the enumerators for their dedicated efforts in data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Hambidge, KM, and Krebs, NF. Strategies for optimizing maternal nutrition to promote infant development. Reprod Health. (2018) 15:87. doi: 10.1186/s12978-018-0534-3
2. Requejo, JH, and Bhutta, ZA. The post-2015 agenda: staying the course in maternal and child survival. Arch Dis Child. (2015) 100:S76–81. doi: 10.1136/archdischild-2013-305737
3. Lacagnina, S. The developmental origins of health and disease (DOHaD). Am J Lifestyle Med. (2019) 14:47–50. doi: 10.1177/1559827619879694
4. Campbell, F, Conti, G, Heckman, JJ, Moon, SH, Pinto, R, Pungello, E, et al. Early childhood investments substantially boost adult health. Science. (2014) 343:1478–85. doi: 10.1126/science.1248429
5. Botto, LD, Moore, CA, Khoury, MJ, and Erickson, JD. Neural-tube defects. N Engl J Med. (1999) 341:1509–19. doi: 10.1056/NEJM199911113412006
6. Czeizel, AE, and Dudás, I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med. (1992) 327:1832–5. doi: 10.1056/NEJM199212243272602
7. Steer, P, Alam, MA, Wadsworth, J, and Welch, A. Relation between maternal haemoglobin concentration and birth weight in different ethnic groups. BMJ. (1995) 310:489–91. doi: 10.1136/bmj.310.6978.489
8. Jung, J, Rahman, MM, Rahman, MS, Swe, KT, Islam, MR, Rahman, MO, et al. Effects of hemoglobin levels during pregnancy on adverse maternal and infant outcomes: a systematic review and meta-analysis. Ann N Y Acad Sci. (2019) 1450:69–82. doi: 10.1111/nyas.14112
9. Shi, H, Chen, L, Wang, Y, Sun, M, Guo, Y, Ma, S, et al. Severity of anemia during pregnancy and adverse maternal and fetal outcomes. JAMA Netw Open. (2022) 5:e2147046. doi: 10.1001/jamanetworkopen.2021.47046
10. Xu, J, Li, X, and Zhou, Q. Nationwide-free preconception care strategy: experience from China. Front. Public Health. (2022) 10:934983. doi: 10.3389/fpubh.2022.934983
11. Black, RE, Victora, CG, Walker, SP, Bhutta, ZA, Christian, P, de Onis, M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
12. Das, JK, Salam, RA, Kumar, R, and Bhutta, ZA. Micronutrient fortification of food and its impact on woman and child health: a systematic review. Syst Rev. (2013) 2:67. doi: 10.1186/2046-4053-2-67
13. Thomas, MS, Demirchyan, A, and Khachadourian, V. How effective is iron supplementation during pregnancy and childhood in reducing anemia among 6–59 months old children in India? Front. Public Health. (2020) 8:234. doi: 10.3389/fpubh.2020.00234
14. Abdollahi, Z, Elmadfa, I, Djazayery, A, Golalipour, MJ, Sadighi, J, Salehi, F, et al. Efficacy of flour fortification with folic acid in women of childbearing age in Iran. Ann Nutr Metab. (2011) 58:188–96. doi: 10.1159/000329726
15. Jiang, Y, Guo, C, Kuang, M, Lin, L, Xu, G, Pan, N, et al. Examining associations of folic acid supplements administered to mothers during pre-conceptional and prenatal periods with autism spectrum disorders in their offspring: insights from a multi-center study in China. Front. Public Health. (2024) 12:1321046. doi: 10.3389/fpubh.2024.1321046
16. Gera, T, Sachdev, HS, and Boy, E. Effect of iron-fortified foods on hematologic and biological outcomes: systematic review of randomized controlled trials. Am J Clin Nutr. (2012) 96:309–24. doi: 10.3945/ajcn.111.031500
17. Hotz, C, Porcayo, M, Onofre, G, García-Guerra, A, Elliott, T, Jankowski, S, et al. Efficacy of iron-fortified ultra rice in improving the iron status of women in Mexico. Food Nutr Bull. (2008) 29:140–9. doi: 10.1177/156482650802900208
18. Osendarp, SJM, Martinez, H, Garrett, GS, Neufeld, LM, De-Regil, LM, Vossenaar, M, et al. Large-scale food fortification and biofortification in low-and middle-income countries: a review of programs, trends, challenges, and evidence gaps. Food Nutr Bull. (2018) 39:315–31. doi: 10.1177/0379572118774229
19. Chakraborty, H, Nyarko, KA, Goco, N, Moore, J, Moretti-Ferreira, D, Murray, JC, et al. Folic acid fortification and women’s folate levels in selected communities in Brazil – a first look. Int J Vitam Nutr Res. (2014) 84:286–94. doi: 10.1024/0300-9831/a000215
20. Kamau, MW, Mirie, W, and Kimani, S. Compliance with iron and folic acid supplementation (IFAS) and associated factors among pregnant women: results from a cross-sectional study in Kiambu county, Kenya. BMC Public Health. (2018) 18:580. doi: 10.1186/s12889-018-5437-2
21. The national rural health mission in India. Its impact on maternal, neonatal, and infant mortality. Semin Fetal Neonatal Med. (2015) 20:315–20. doi: 10.1016/j.siny.2015.06.003
22. National Health Commission of the PRC. (2009). Notice of the National Health Commission on the project of supplementing folic acid to prevent neural tube defects. Available at: http://www.nhc.gov.cn/bgt/s9510/200906/8db449bd394344e9940f93bae522ade2.shtml (Accessed October 19, 2024).
23. National Health and Family Planning Commission of the PRC. (2010). Notice of the National Health and family planning commission on the issuance of technical service specifications (trial) for the National Free Preconception Health Examination Pilot Project. Available at: http://www.nhc.gov.cn/fys/jslgf/201307/4bad01a08a07468e87b583b28f082d53.shtml (Accessed October 19, 2024).
24. Shen, M, Wu, Y, and Xiang, X. Hukou-based rural–urban disparities in maternal health service utilization and delivery modes in two Chinese cities in Guangdong Province. Int J Equity Health. (2021) 20:145. doi: 10.1186/s12939-021-01485-4
25. Yan, C, Tadadej, C, Chamroonsawasdi, K, Chansatitporn, N, and Sung, JF. Ethnic disparities in utilization of maternal and child health Services in Rural Southwest China. Int J Environ Res Public Health. (2020) 17:8610. doi: 10.3390/ijerph17228610
26. Yang, J, Reheman, Z, Liu, Y, Wang, Y, Wang, N, Ye, J, et al. The compliance of free folic acid supplements among pregnant women in rural areas of northwestern China: the role of related knowledge. Front Public Health. (2023) 10:1079779. doi: 10.3389/fpubh.2022.1079779
27. Sununtnasuk, C, D’Agostino, A, and Fiedler, JL. Iron+folic acid distribution and consumption through antenatal care: identifying barriers across countries. Public Health Nutr. (2016) 19:732–42. doi: 10.1017/S1368980015001652
28. Qiao, Y, Di, J, Yin, L, Huang, A, Zhao, W, Hu, H, et al. Prevalence and influencing factors of anemia among pregnant women across first, second and third trimesters of pregnancy in monitoring areas, from 2016 to 2020: a population-based multi-center cohort study. BMC Public Health. (2024) 24:1100. doi: 10.1186/s12889-024-18610-x
29. Jiang, Q, Guo, Y, Zhang, E, Cohen, N, Ohtori, M, Sun, A, et al. Perinatal mental health problems in rural China: the role of social factors. Front. Psychiatry. (2021) 12:636875. doi: 10.3389/fpsyt.2021.636875
30. Nasir, M, Ayele, HM, Aman, R, and Hussein, K. Magnitude of anemia and associated factors among pregnant women attending antenatal care in governmental health facilities of shashemene town, Oromia region, Ethiopia. Front. Public Health. (2024) 12:1409752. doi: 10.3389/fpubh.2024.1409752
31. Abdi, KA, Jayamohan, MK, and Adem, M. The nexus between poverty and maternal healthcare utilization with a focus on antenatal care visits and choice of place of birth in somaliland. Front Public Health. (2024) 12:1417883. doi: 10.3389/fpubh.2024.1417883
32. Poston, L, Caleyachetty, R, Cnattingius, S, Corvalán, C, Uauy, R, Herring, S, et al. Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol. (2016) 4:1025–36. doi: 10.1016/S2213-8587(16)30217-0
33. Frey, HA, and Klebanoff, MA. The epidemiology, etiology, and costs of preterm birth. Semin Fetal Neonatal Med. (2016) 21:68–73. doi: 10.1016/j.siny.2015.12.011
34. Hasan, AMR, Selim, MA, Anne, FI, Escobar-DeMarco, J, Ireen, S, Kappos, K, et al. Opportunities and challenges in delivering maternal and child nutrition services through public primary health care facilities in urban Bangladesh: a qualitative inquiry. BMC Health Serv Res. (2023) 23:1172. doi: 10.1186/s12913-023-10094-6
35. Sebastian, FMG, Mercado, WA, Rondaris, MVA, Regal, MAS, and Gemira, EC. Strengthening nutrition knowledge of pregnant women through nutrition education during public health emergencies. J Med Univ St Tomas. (2022) 6:906–15. doi: 10.35460/2546-1621.2021-0091
36. Perumal, N, Cole, DC, Ouédraogo, HZ, Sindi, K, Loechl, C, Low, J, et al. Health and nutrition knowledge, attitudes and practices of pregnant women attending and not-attending ANC clinics in western Kenya: a cross-sectional analysis. BMC Pregnancy Childbirth. (2013) 13:146. doi: 10.1186/1471-2393-13-146
37. WHO Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Available at: https://www.who.int/publications/i/item/WHO-NMH-NHD-MNM-11.1 (Accessed October 19, 2024).
38. Nie, J, Zhang, L, Song, S, Hartnett, AJ, Liu, Z, Wang, N, et al. Exclusive breastfeeding in rural western China: does father’s co-residence matter? BMC Public Health. (2021) 21:1981. doi: 10.1186/s12889-021-12025-8
39. Ibikunle, HA, Okafor, IP, and Adejimi, AA. Pre-natal nutrition education: health care providers’ knowledge and quality of services in primary health care centres in Lagos, Nigeria. PLoS One. (2021) 16:e0259237. doi: 10.1371/journal.pone.0259237
40. Ilozumba, O, Van Belle, S, Dieleman, M, Liem, L, Choudhury, M, and Broerse, JEW. The effect of a community health worker utilized mobile health application on maternal health knowledge and behavior: a quasi-experimental study. Front. Public Health. (2018) 6:133. doi: 10.3389/fpubh.2018.00133
41. Blondin, JH, and JA, LG. Pregnant women’s knowledge and awareness of nutrition. Appl Nurs Res. (2018) 39:167–74. doi: 10.1016/j.apnr.2017.11.020
42. Papežová, K, Kapounová, Z, Zelenková, V, and Riad, A. Nutritional health knowledge and literacy among pregnant women in the Czech Republic: analytical cross-sectional study. Int J Environ Res Public Health. (2023) 20:3931. doi: 10.3390/ijerph20053931
43. Fite, MB, Roba, KT, Oljira, L, Tura, AK, and Yadeta, TA. Compliance with iron and folic acid supplementation (IFAS) and associated factors among pregnant women in sub-saharan africa: a systematic review and meta-analysis. PLoS One. (2021) 16:e0249789. doi: 10.1371/journal.pone.0249789
44. Singh, PK, Dubey, R, Singh, L, Kumar, C, Rai, RK, and Singh, S. Public health interventions to improve maternal nutrition during pregnancy: a nationally representative study of iron and folic acid consumption and food supplements in India. Public Health Nutr. (2020) 23:2671–86. doi: 10.1017/S1368980020001007
45. Seifu, CN, Whiting, SJ, and Hailemariam, TG. Better-educated, older, or unmarried pregnant women comply less with iron-folic acid supplementation in southern Ethiopia. J Diet Suppl. (2020) 17:442–53. doi: 10.1080/19390211.2019.1629145
46. Nilsen, RM, Leoncini, E, Gastaldi, P, Allegri, V, Agostino, R, Faravelli, F, et al. Prevalence and determinants of preconception folic acid use: an italian multicenter survey. Ital J Pediatr. (2016) 42:65. doi: 10.1186/s13052-016-0278-z
47. Aryastami, NK, and Mubasyiroh, R. Traditional practices influencing the use of maternal health care services in Indonesia. PLoS One. (2021) 16:e0257032. doi: 10.1371/journal.pone.0257032
48. Nasir, BB, Fentie, AM, and Adisu, MK. Adherence to iron and folic acid supplementation and prevalence of anemia among pregnant women attending antenatal care clinic at tikur anbessa specialized hospital, Ethiopia. PLoS One. (2020) 15:e0232625. doi: 10.1371/journal.pone.0232625
49. Wu, T, and Dang, S. Status and influencing factors of folic acid intake by childbearing-aged women in Shaanxi province. J Xi’an Jiaotong Univ. (2017):337–42.
50. Jessup, RK, Assaad, LB, and Wick, K. Why choose wisely if you have already paid? Sunk costs elicit stochastic dominance violations. Judgm Decis Mak. (2018) 13:575–86. doi: 10.1017/S1930297500006604
51. Arked, HR, and Blumer, C. The psychology of sunk cost. Organ Behav hum Decis Process. (1985) 35:124–40. doi: 10.1016/0749-5978(85)90049-4
52. Lin, Q, Yang, L, Li, F, Qin, H, Li, M, Chen, J, et al. A village-based intervention: promoting folic acid use among rural Chinese women. Nutrients. (2017) 9:174. doi: 10.3390/nu9020174
53. Akwaa Harrison, O, Ifie, I, Nkwonta, C, Dzandu, BA, Gattor, AO, Adimado, EE, et al. Knowledge, awareness, and use of folic acid among women of childbearing age living in a peri-urban community in Ghana: a cross-sectional survey. BMC Pregnancy Childbirth. (2024) 24:241. doi: 10.1186/s12884-024-06408-z
54. Yang, L, and Wang, H. Primary health care among rural pregnant women in China: achievements and challenges in maternal mortality ratio. Prim Health Care Res Dev. (2019) 20:e97. doi: 10.1017/S1463423619000306
55. Liu, J, Jin, L, Meng, Q, Gao, L, Zhang, L, Li, Z, et al. Changes in folic acid supplementation behaviour among women of reproductive age after the implementation of a massive supplementation programme in China. Public Health Nutr. (2015) 18:582–8. doi: 10.1017/S1368980014000950
56. Tan, PPS, Sandhu, RS, Zain, SM, Hall, D, Tan, NC, Lim, HM, et al. Health motivations and perceived barriers are determinants of self-care behaviour for the prevention of hypertension in a malaysian community. PLoS One. (2022) 17:e0278761. doi: 10.1371/journal.pone.0278761
57. Asim, M, Saleem, S, Ahmed, ZH, Naeem, I, Abrejo, F, Fatmi, Z, et al. We won’t go there: barriers to accessing maternal and newborn care in district thatta, Pakistan. Healthcare. (2021) 9:1314. doi: 10.3390/healthcare9101314
58. Aziz, A, Saleem, S, Nolen, TL, Pradhan, NA, McClure, EM, Jessani, S, et al. Why are the pakistani maternal, fetal and newborn outcomes so poor compared to other low and middle-income countries? Reprod Health. (2020) 17:190. doi: 10.1186/s12978-020-01023-5
59. Rural Health Information Hub Barriers to improving rural maternal health - RHIhub toolkit. Available at: https://www.ruralhealthinfo.org/toolkits/maternal-health/1/barriers (Accessed December 7, 2024).
60. Alicia, N.. What is the health belief model? An updated look. (2024) Available at: https://positivepsychology.com/health-belief-model/ (Accessed December 7, 2024).
61. Udenigwe, O, Okonofua, FE, Ntoimo, LFC, and Yaya, S. Seeking maternal health care in rural Nigeria: through the lens of negofeminism. Reprod Health. (2023) 20:103. doi: 10.1186/s12978-023-01647-3
62. Short, SE, and Mollborn, S. Social determinants and health behaviors: conceptual frames and empirical advances. Curr Opin Psychol. (2015) 5:78–84. doi: 10.1016/j.copsyc.2015.05.002
63. Nouwens, SPH, Veldwijk, J, Pilli, L, Swait, JD, Coast, J, and Bekker-Grob, EW. A socially interdependent choice framework for social influences in healthcare decision-making: a study protocol. BMJ Open. (2024) 14:e079768. doi: 10.1136/bmjopen-2023-079768
Keywords: received public services, policy awareness, health knowledge, health practices, pregnancy, rural areas
Citation: Yang J, Chen J, Xie Y, Liu Y, Wu J, Li Y and Nie J (2025) Challenges in rural maternal health: how received public services and policy awareness affect health knowledge and practices. Front. Public Health. 12:1514522. doi: 10.3389/fpubh.2024.1514522
Received: 21 October 2024; Accepted: 24 December 2024;
Published: 14 January 2025.
Edited by:
Qi Zhang, Old Dominion University, United StatesReviewed by:
Wei Jie Gong, Shenzhen University Health Science Centre, ChinaCopyright © 2025 Yang, Chen, Xie, Liu, Wu, Li and Nie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jingchun Nie, bmllamluZ2NodW5AeWVhaC5uZXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.