- Faculty of Nursing, Health Science Center, Xi'an Jiaotong University, Xi'an, Shaanxi, China
Background: Telemedicine has a positive impact on improving health literacy and disease management ability of chronic disease patients and reducing the medical burden. However, telemedicine still has many problems in chronic disease management. We should actively solve the problems and maximize the functions of telemedicine.
Objective: To explore the application and improvement of telemedicine in chronic disease self-management to provide important insights from functional module analysis for stakeholders, healthcare professionals, and policymakers to promote the development of telemedicine in chronic disease management.
Design: We conducted a systematic review and qualitative synthesis of five English databases including PubMed, Embase, Web of Science, Cochrane Database of Systematic Reviews, and Scopus, as well as three Chinese databases: China National Knowledge Infrastructure (CNKI), WanFang and VIP database. Databases were searched from inception until November 12, 2024.
Methods: This review is reported in accordance with guidelines for Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ). Two reviewers independently performed study selection, data extraction, and quality assessment using the Joanna Briggs Institute's key assessment tools for qualitative research. Thematic analysis was used for data synthesis.
Results: A total of 35 studies were included, and the contents were refined and summarized into 8 new subthemes. Then, four themes were synthesized: Reminder and supervisor, Access to knowledge, Transition in medical treatment mode, and Emotional support platform.
Conclusion: By improving information quality, developing diverse functions, and constructing multidisciplinary coordination mechanisms to meet the needs of patients with chronic diseases, improve the medical service system, maximize the function of telemedicine, and enhance the stickiness of patients to use telemedicine.
1 Introduction
Non-communicable diseases, also known as chronic diseases, are the leading cause of death worldwide. Chronic diseases kill 41 million people each year, which is equivalent to 74% of all deaths worldwide (1). Chronic diseases have a negative impact on patients, families, and society due to the demands of long-term treatment and management (2). With the progress and development of science and technology, digital technology has been widely used in medicine. Especially during the COVID-19 Pandemic, the use rate of telemedicine has increased significantly. Patients have remote consultations with doctors through telephone and video calls. This approach not only avoids the risk of cross-infection but also reduces the burden on the hospital (3). After the COVID-19 pandemic, telemedicine has gradually become a normal medical service mode, especially in the fields of chronic disease management and older patients care. Internet of Things (IoT) technology combined with wearable devices makes remote monitoring more convenient and accurate (4). Telemedicine not only allows patients to remotely monitor and consult patients by using wearable devices or mobile phones but also enables doctors to efficiently and intelligently complete disease diagnosis treatment and teaching by using electronic medical records and artificial intelligence (AI) (5). At present, many studies have confirmed that telemedicine can improve the management and monitoring of patients with chronic diseases (6), increase the accessibility and efficiency of medical services, reduce the incidence of chronic diseases, and effectively improve health literacy and disease management ability of patients with chronic diseases and improve their quality of life (7).
Despite the great potential of telemedicine in chronic disease management, there are still many problems. The study found that the low digital literacy of patients and the difficulty of technical operations hindered the development of telemedicine. At the same time, telemedicine also poses challenges for healthcare professionals and policymakers (8). Telemedicine increases healthcare professional's workload and puts higher demands on their service level and the allocation of national medical resources. However, most of the previous studies focused on the experience and preferences of patients, and there was a lack of systematic research on the application function of telemedicine (9, 10). Cultural background significantly impacts whether patients are willing to use telemedicine services. In areas with a strong traditional culture, patients may prefer face-to-face visits, believing that in-person contact with a doctor is the most reliable form of treatment. The lack of face-to-face interaction in telemedicine can lead to trust issues, especially for older people and low-income groups (11). Efficient and stable network connection is an inevitable requirement of telemedicine, and the lack of mobile devices will hinder the popularization of telemedicine. Compared with developing countries, developed countries have obvious technological advantages, which is conducive to the implementation of telemedicine (12). The study aims to explore the application and improvement of telemedicine in chronic disease self-management to provide important insights from functional module analysis for stakeholders, healthcare professionals, and policymakers to promote the development of telemedicine in chronic disease management.
2 Methods
2.1 Study design and search strategy
A systematic review and thematic synthesis of qualitative research was carried out under the guidance of the framework and reporting guidelines for Enhancing transparency in reporting the synthesis of qualitative research (ENTREQ) (13) (Supplementary material). Searches included five English databases in PubMed, Embase, Web of Science, Cochrane Database of Systematic Reviews, and Scopus, as well as three Chinese databases: China National Knowledge Infrastructure (CNKI), WanFang, and VIP database. Databases were searched from inception until November 12, 2024. The search strategy included a comprehensive keyword combination of chronic disease, telemedicine, and qualitative research. To prevent omissions, we also screened references for included studies and relevant systematic reviews. The search strategy is given in Supplementary material.
2.2 Inclusion and exclusion criteria
Inclusion criteria: (1) Study participants: patients with at least 1 common chronic disease; (2) Context of the study: patients with home-based disease management or interviewed after participating in the telehealth experiment during follow-up. (3) Phenomenon of interest: experience, functional application, and suggestions for improvement of telemedicine; (4) Study methods: qualitative research, including descriptive research, phenomenology, ethnography, grounded theory, narrative or thematic analysis, and so on.
Exclusion criteria: (1) Repeated publication, incomplete data information; (2) Non-Chinese and English literature; (3) Conference or review articles; and (4) Full text is not available.
2.3 Study selection and data extraction
It was independently conducted by 2 researchers in the search team who were trained in evidence-based practice methods. The researchers screened the retrieved study titles and abstracts from the literature search results to exclude studies that did not meet the inclusion criteria. The researchers then further screened the included studies by reading the full text and sought comprehensive information from the authors of the included articles when necessary. If two researchers disagreed, a third researcher was consulted. Use a pre-designed table to extract key descriptive characteristics of the included study, including author, year of publication, country, study purpose, participant characteristics, method of data analysis, and key findings. The authors would be contacted via email for additional or missing information if required. The extracted text was entered verbatim into NVivo 12 plus for management and analysis.
2.4 Quality assessment
The Joanna Briggs Institute Qualitative Assessment and Review tool was used to assess the quality of included studies. The scale consists of 10 questions answered with “yes,” “no,” and “unclear.” These 10 questions are designed to help the researcher conduct a quick and systematic evaluation of the essay. If all the answers are “yes,” the criteria are fully met and the study is rated as A; if the evaluation criteria are partially met, it is rated as B; all answers are “no,” meaning they do not meet the criteria at all and are graded C. Studies rated C were excluded. Two researchers independently assessed the quality of each study, and a third researcher was contacted for judgment if there was a disagreement.
2.5 Data synthesis
Qualitative data were analyzed using Thomas and Harden's three-stage thematic synthesis approach (14). The included studies and extracted data were read repeatedly by three researchers to gain a full understanding before synthesis. In the first stage, all the experiences and preferences associated with the use of m-health for patients with chronic diseases were summarized and coded. In the second stage, the codes are grouped by comparing the similarities and differences of the data in the first stage, grasping the connections, merging similar themes, and creating new descriptive themes. In the final stage, the descriptive topics from the previous stage are re-examined and similar topics are grouped into a comprehensive result (analytical topics). In this process, sub-themes and main themes, namely descriptive themes and analytical themes, are generated, and new interpretations of phenomena are obtained. The first stage of the coding process was carried out by two researchers. Descriptive and analytical themes are identified by one researcher. Subsequently, the data analysis process was checked by the entire research team to ensure consistency in the interpretation of the results and adequacy of the topics analyzed.
3 Results
3.1 Description of studies
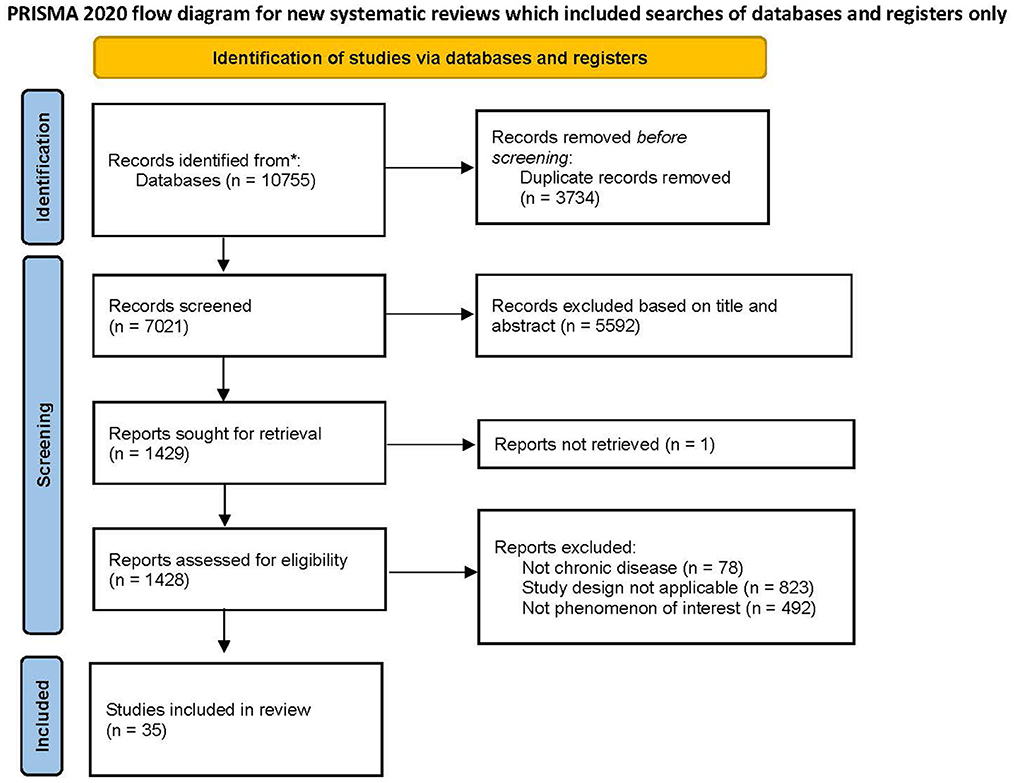
The initial search identified 10,755 articles, and 7,021 articles were left after eliminating the duplicates. Finally, 35 articles were included in this meta-synthesis through the screening of inclusion criteria. The included studies were published between 2008 and 2024 and included a total of 768 patients with chronic disease and 173 healthcare professionals. The search results and process are shown in Figure 1.
3.2 Description and quality assessment of included literature
The majority of studies were from high-income countries, including the United Kingdom (10/35, 29%) (15–24), China (9/35, 26%) (25–33), United States (4/35, 11%) (34–37), Sweden (3/35, 9%) (38–40), Canada (3/35, 9%) (41–43), and each from the Netherlands (44), Australia (45), Denmark (46), Belgium (47), Germany (48), and Norway (49) (1/35, 3%). mHealth technologies were applied to assist the management of the following CNCDs: diabetes (4/35, 11%) (21, 31, 34, 47), chronic obstructive pulmonary disease (10/35, 29%) (16, 17, 19, 23, 24, 28, 29, 32, 46, 49), cardiovascular disease (9/35, 26%) (18, 20, 22, 25–27, 39, 40, 42), kidney disease (1/35, 3%) (35), and multiple chronic conditions (11/35, 31%) (15, 30, 33, 36–38, 41, 43–45, 48). The analytic approaches followed in these qualitative studies included thematic analysis (7/35, 20%) (20, 21, 32, 34, 35, 41, 46), content analysis (11/35, 31%) (31, 33, 37–39, 42–44, 47–49), constant comparative method (2/35, 6%) (22, 24), framework analysis methods (FAMs) (5/35, 14%) (15–18, 36), interpretative phenomenological analysis (2/35, 6%) (19, 40), Colaizzi's seven-step analysis (6/35, 17%) (25–30), and non-specific method (2/35, 6%) (23, 45) (Table 1).
According to the JBI quality assessment scale, 27 studies achieved grade B, and 8 studies achieved grade A (Table 2). Most studies did not describe the investigator's impact on the study. Some studies do not describe the researcher's cultural and theoretical orientation.
3.3 Data analysis and meta-synthesis
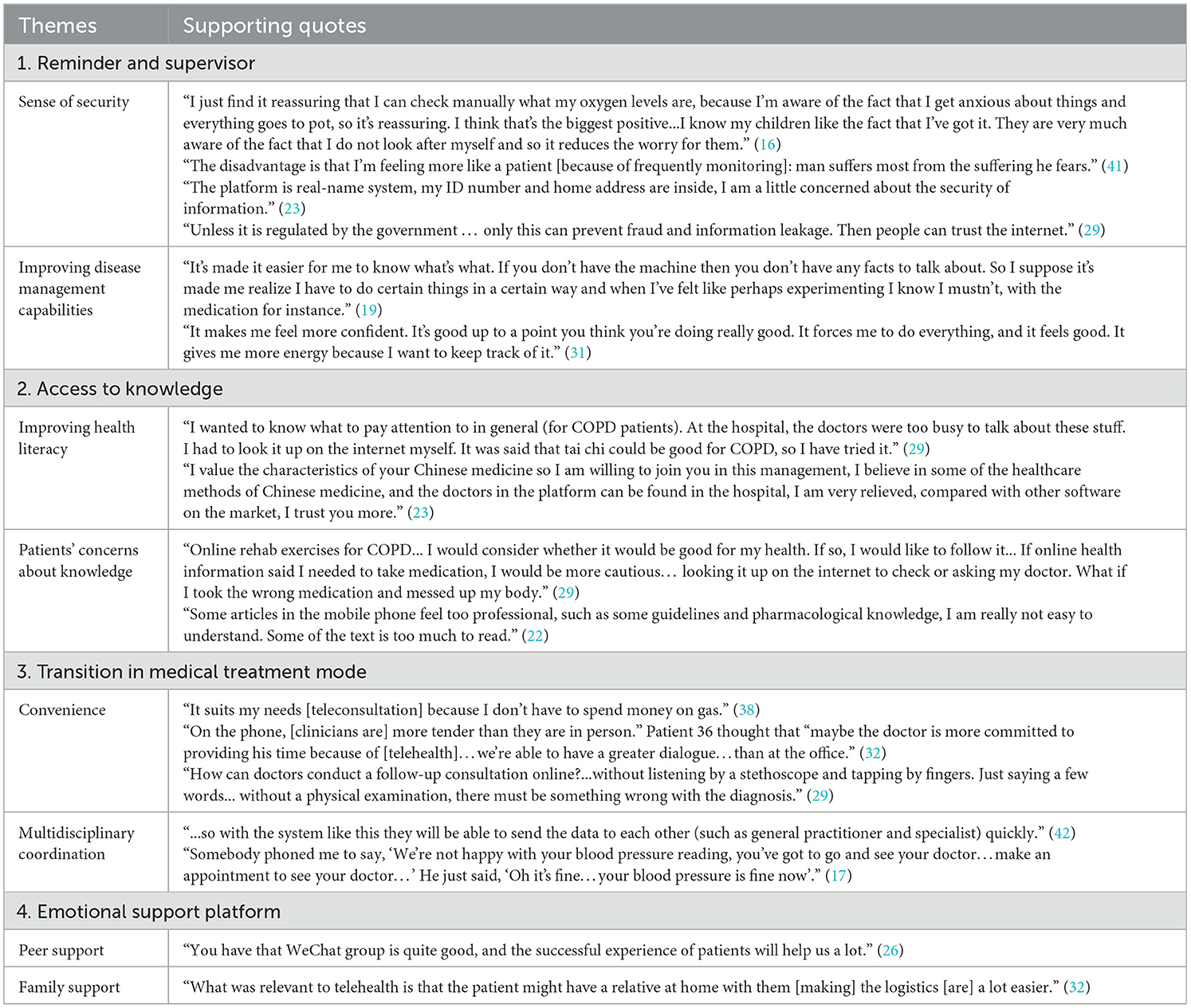
Eight sub-themes were extracted from the 35 included studies. Through meta-synthesis, ten sub-themes were compared and analyzed, and four themes were identified. The needs and improvement suggestions for telemedicine by patients with chronic diseases can be divided into four themes: (1) reminders and supervisors, (2) access to knowledge, (3) transition in medical treatment mode, and (4) emotional support platform. Data are presented as a synthesized finding with supporting themes and component subthemes. Themes with key exemplary quotations are presented below and in Table 3.
3.3.1 Reminder and supervisor
3.3.1.1 Sense of security
Most patients consider peace of mind to be one of the biggest benefits of using telemedicine, as they can see some physiological indicators of their body at any time and understand the progress of their condition, which reduces patients' worry and uncertainty. At the same time, telemedicine brings more security to patients because they know that healthcare professionals will check their data regularly, and the doctor will take the initiative to contact them if there is a problem in time (15, 17–20, 22–24, 26, 33, 34, 36, 38, 42, 44–46). Patients also said that telemedicine can reduce the concerns of patients' families.
“I just find it reassuring that I can check manually what my oxygen levels are, because I'm aware of the fact that I get anxious about things and everything goes to pot, so it's reassuring. I think that's the biggest positive…I know my children like the fact that I've got it. They are very much aware of the fact that I do not look after myself and so it reduces the worry for them.” (19)
However, some patients who use telemonitoring at home may have anxiety about the accuracy of the data and how to handle abnormal data, which is one of the reasons that affect patients' willingness to use telemedicine. One cardiovascular patient said that he was frequently reminded of having a chronic condition.
“The disadvantage is that I'm feeling more like a patient [because of frequently monitoring]: man suffers most from the suffering he fears.” (44)
People with chronic conditions worry about their personal and health information being improperly accessed or misused by non-medical personnel. Frequent news about data breaches makes their doubts about the security of telemedicine (26, 27, 32, 44, 45).
“The platform is real-name system, my ID number and home address are inside, I am a little concerned about the security of information.” (26)
Patients and HCPs emphasized that standard regulation of information by government departments was the only way to relieve people's prejudices about telemedicine.
“Unless it is regulated by the government … only this can prevent fraud and information leakage. Then people can trust the internet.” (32)
3.3.1.2 Improving disease management capabilities
Self-management of chronic diseases is a complex and ongoing process. Telemedicine helps to improve patients' self-management abilities and encourages self-management behaviors. By monitoring the dynamic changes in data, patients can understand their physical condition, which will motivate them to take the initiative in disease management (15, 17, 19–24, 26, 30, 31, 33, 34, 40, 43, 45, 46). The patient said that telemedicine taught her to rely on professional data for self-management.
“It's made it easier for me to know what's what. If you don't have the machine then you don't have any facts to talk about. So I suppose it's made me realize I have to do certain things in a certain way and when I've felt like perhaps experimenting I know I mustn't, with the medication for instance.” (22)
In addition, both good measurement data and praise from healthcare professionals will increase patient confidence and positive perceptions of telemedicine, thus encouraging patients to maintain good self-management and strengthening the user stickiness of telemedicine. A 62-year-old patient with type 2 diabetes said:
“It makes me feel more confident. It's good up to a point you think you're doing really good. It forces me to do everything, and it feels good. It gives me more energy because I want to keep track of it.” (34)
3.3.2 Access to knowledge
3.3.2.1 Improving health literacy
Formal education and training are an important part of patient self-management. Patients often do not know how to manage their disease because of a lack of knowledge about treatment and care. Most patients said their doctors had not told them or told them about their illness when they were in the hospital, but they forgot about it when they were discharged. As a new way to acquire knowledge, patients can query disease-related knowledge and learn proper disease management methods through telemedicine, thus improving their health literacy (17, 19, 24, 28, 30–32, 36, 37, 44).
“I wanted to know what to pay attention to in general (for COPD patients). At the hospital, the doctors were too busy to talk about these stuff. I had to look it up on the internet myself. It was said that tai chi could be good for COPD, so I have tried it.” (32)
Specialized knowledge boards can strengthen patients' willingness to use telemedicine. Tang et al. (26) mentioned TCM-related (Traditional Chinese Medicine-related) functions that were popular with patients.
“I value the characteristics of your Chinese medicine so I am willing to join you in this management, I believe in some of the healthcare methods of Chinese medicine, and the doctors in the platform can be found in the hospital, I am very relieved, compared with other software on the market, I trust you more.”
3.3.2.2 Patients' concerns about knowledge
Faced with a large amount and variety of health knowledge, patients feel that they are unable to judge the reliability and applicability of information. In addition, patients said that much popular science knowledge was too specialized, and they could not understand it. All these have greatly hindered patients' use of telemedicine (18, 25, 28, 30, 32, 39, 43, 47).
“Online rehab exercises for COPD… I would consider whether it would be good for my health. If so, I would like to follow it… If online health information said I needed to take medication, I would be more cautious… looking it up on the internet to check or asking my doctor. What if I took the wrong medication and messed up my body” (32)
“Some articles in the mobile phone feel too professional, such as some guidelines and pharmacological knowledge, I am really not easy to understand. Some of the text is too much to read.” (25)
3.3.3 Transition in medical treatment mode
3.3.3.1 Convenience
In addition to reducing patient travel time and transportation costs to the hospital, telemedicine also allows doctors to telecommute and give timely feedback to patients. Telemedicine realizes the remote communication between patients and medical staff, provides health services such as consultation and diagnosis for patients, and is conducive to the establishment of a healthy and harmonious doctor-patient relationship (15–23, 26, 28, 30, 32, 33, 35–39, 41, 42, 45, 46, 49). Patients said doctors were gentler when they used telemedicine to talk to them.
“It suits my needs [teleconsultation] because I don't have to spend money on gas” (41)
“On the phone, [clinicians are] more tender than they are in person.” Patient 36 thought that “maybe the doctor is more committed to providing his time because of [telehealth]…we're able to have a greater dialogue…than at the office.” (35)
However, telemedicine is only a supplement and continuation of the traditional medical treatment model. Given the lack of face-to-face communication and examination in remote assessment, some patients and doctors believe this may generate some negative conditions, including missed diagnoses, misdiagnoses, and a lack of intimacy (24, 32, 35, 41).
“How can doctors conduct a follow-up consultation online?…without listening by a stethoscope and tapping by fingers. Just saying a few words… without a physical examination, there must be something wrong with the diagnosis.” (32)
3.3.3.2 Multidisciplinary coordination
Telemedicine can facilitate the exchange of patient health-related information among healthcare professionals. By uniting communities and hospitals, patients can be provided with comprehensive continuity of care, which facilitates chronic disease management and follow-up.
“…so with the system like this they will be able to send the data to each other (such as general practitioner and specialist) quickly.” (45)
However, a lot of patients thought they may be under the care of multiple doctors, who would work independently of each other. Because they operate as separate entities, they often do not have complete information about a patient's condition or treatment history, leading to fragmented and poorly coordinated care for patients (16, 18, 20, 36, 43).
“Somebody phoned me to say, ‘We're not happy with your blood pressure reading, you've got to go and see your doctor…make an appointment to see your doctor…' He just said, ‘Oh it's fine…your blood pressure is fine now'.” (20)
3.3.4 Emotional support platform
3.3.4.1 Peer support
“Prolonged illness makes the patient a doctor.” Patients with chronic disease usually develop a relatively comprehensive and in-depth understanding of their condition after a long period of disease management and treatment, and they may become advocates for their health, sharing experiences with others. Telemedicine provides a platform for patients to communicate or organize online support groups, allowing patients to communicate and connect with other patients with similar conditions. They can share experiences, support, enhance mental health, and improve motivation for each other (26, 27, 29, 30, 37).
“You have that WeChat group is quite good, and the successful experience of patients will help us a lot.” (29)
3.3.4.2 Family support
Family support plays a vital role in the self-management of patients with chronic diseases. In the face of complicated treatment and lifestyle adjustment, patients need understanding and help from family members both psychologically and practically. Telemedicine allows family members to monitor the patient's health data in real time, acknowledge the patient's condition and treatment progress, and participate in medical decision-making. Meanwhile, by encouraging and assisting patients to install and use telemedicine applications, family members can reduce patients' fear and resistance to new technologies, and significantly improve patients' acceptance and frequency of use of telemedicine (19, 26, 27, 30, 32, 35, 39, 46–48). HCPs emphasize the importance of family support:
“What was relevant to telehealth is that the patient might have a relative at home with them [making] the logistics [are] a lot easier.” (35)
4 Discussion
This study explores, compares and synthesizes the experience of using telemedicine for chronic patients. While previous studies have mostly focused on patient experiences and preferences, they have failed to systematically articulate suggestions for improvements in telemedicine. Therefore, from the perspective of functional modules, this study reveals four comprehensive themes, which summarize the application functions and improvement suggestions of telemedicine in chronic disease management.
Our study identified the alerting and monitoring functions of telemedicine as the first comprehensive topic. Consistent with Creber's study, patients with chronic diseases improved their knowledge of their disease through telemedicine, which improved their self-care ability and sense of security (10). Telemedicine also improves long-term adherence to self-management in patients with chronic diseases and is a promising way to support patients and clinicians in treating their disease. An RCT study showed that an innovative telemonitoring enhanced care program for Chronic heart failure (ITEC-CHF) improved patient adherence to weight monitoring (50). However, some chronic patients will worry about telemedicine's accuracy and individual information safety. Providing successful cases and establishing the legal framework to protect patients' interests and rights, then enhances the authority and trust of the telemedicine platform. People with chronic diseases often have a dismissive attitude toward their illness, believing that they can control it on their own. Research shows that old age, low income, low education, and other factors affect patients' willingness to use telemedicine (51). Telemedicine should formulate personalized programs for them according to the individual's age, education level, and other aspects. Consistent with other reviews on telemedicine (7, 10), patients question the effectiveness of telemedicine. Existing research is confused about the effectiveness of telemedicine. A systematic review and meta-analysis (52) reported that telemedicine had the potential to improve clinical outcomes for people with diabetes, but the overall quality of its evidence was low to very low. Further prospective studies are needed to gather clinical evidence supporting the effectiveness of telemedicine.
Telemedicine is often used by patients to gain health knowledge. Telemedicine improves patient self-management by providing daily education and health information. The self-management needs of people with chronic illnesses are varied. Telemedicine should focus on the individual needs and preferences of patients, avoid a lot of homogenized information, carry out diversified health education in form and content, recommend personalized knowledge to patients (31), and meet their health needs, which helps to enhance their confidence and sense of control over chronic diseases (53), and thus promote the sustainable development of telemedicine. In addition, patients may question the reliability of health knowledge and the security of personal information. For the sustainable and healthy development of telemedicine, the platform should strengthen information review to ensure the reliability of knowledge. Policymakers should further improve the network information security guarantee mechanism, strengthen the construction of laws and regulations on telemedicine, and ensure the reliability of health information (54). Healthcare professionals should use plain language to provide health education to patients and take the initiative to answer questions related to privacy protection, so as to provide patients with reliable sources of health information, improve their health literacy, and enhance patients' sense of trust (55).
Telemedicine has changed the traditional medical model. Compared with face-to-face methods, telemedicine reduces the time and transportation costs for patients and facilitates remote access to healthcare guidance for patients with chronic diseases, especially those with limited mobility and financial difficulties. Telemedicine can also improve the efficiency of healthcare professionals, promote the sharing of patient health information, provide comprehensive continuity of care for patients, and facilitate the management and follow-up of chronic diseases. This is consistent with Yi's research (56) that telemedicine has a positive effect on chronic disease management. However, telemedicine cannot replace face-to-face consultations. The study found that although telemedicine is widely used in most medical specialties, only a few specialties have strong evidence that the diagnostic and management decisions provided by telemedicine are comparable to face-to-face care (57). Telemedicine is simply an adjunct to medical practice, supporting the work of healthcare professionals when needed. However, telemedicine also poses challenges for healthcare professionals. The use of telemedicine by healthcare professionals often results in members working independently, lack of communication, inability to ensure consistency of treatment plans (41, 43) and poor communication with patients. Therefore, telemedicine should be integrated into the entire healthcare system as a tool to enhance the continuity of the relationship between hospitals, patients, and communities. Develop skills training to improve the remote consultation capacity of healthcare professionals and combine community health resources to ensure continuity of care and improve the working mode of telemedicine. Strengthening the integration of telemedicine with multidisciplinary collaboration allows healthcare professionals from different disciplines to share patient information through electronic health records, video conferencing, and online platforms to improve diagnostic accuracy and quality of care (58).
Vorderstrasse et al. (59) found that telemedicine provides people with type 2 diabetes with interactions with peers, family members, and healthcare professionals that can help them address the challenges and barriers that arise when implementing self-management behaviors. When incorporating telemedicine into the self-management pathway for patients with chronic diseases, healthcare professionals should provide a multifunctional information exchange platform to involve patients and families in care and enhance patient confidence in self-management and treatment compliance.
5 Implications for clinical practice and future studies
The qualitative evidence synthesis of telemedicine in chronic disease self-management explored the application of telemedicine in the field of chronic disease self-management from the functional module, providing a new perspective for telemedicine research. The results show that telemedicine is an adjunct tool to support clinical practice and is conducive to improving patient satisfaction and quality of care. However, the effectiveness of telemedicine needs further research to explore. This study provides recommendations for stakeholders, policymakers, and healthcare professionals to address current issues in telemedicine. Regarding information leakage and online medical insurance, policymakers should introduce effective personal information protection systems and fair medical insurance policies to promote the sustainable development of telemedicine. The hospital realizes data sharing and business collaboration with telemedicine services, and actively provides continuous services such as convenient and efficient online services, follow-up management and remote guidance for patients. Joint community hospitals promote hierarchical diagnosis and treatment and carry out the monitoring and management of the characteristic data of patients with chronic diseases, to reduce medical costs and improve the level of primary medical services. Telemedicine skills training is carried out to improve the communication, interface operation and data processing skills of healthcare professionals, which is conducive to improving the quality of medical care. Future research efforts should prioritize assessing the needs of people with chronic diseases, considering their countries, digital literacy, and healthcare environments. Such an assessment would help improve the feasibility and sustainability of telemedicine. It is worth emphasizing that 77% of chronic disease deaths occur in low—and middle-income countries, but much of the research on telemedicine in chronic disease management originated in high-income countries (1). In low and middle-income countries, there is relatively little research. Low—and middle-income countries should further strengthen telemedicine research to harness its potential more effectively, improve health services and reduce the impact of chronic diseases (60).
6 Limitations
The limitation of this review is that it is limited to papers published in both Chinese and English. Another limitation is that the study is from different countries, and there are differences in patients' cultural backgrounds, and telemedicine devices, which may make it more difficult for researchers to integrate information and affect the quality of the findings. In addition, the operation and cost of telemedicine are not discussed in this review, because we believe that simplifying operation is inconsistent with the concept of fully understanding patients' conditions and providing personalized services for them. Inter-device charging standards and the variation of healthcare systems between countries are too large, stakeholders should solve relevant questions according to national conditions. Technical limitations are a barrier to the adoption of telemedicine in rural areas. However, most of the literature included in this study is from developed countries with fewer technical restrictions, so we do not discuss them in depth.
7 Conclusion
This study systematically reviewed the content of telemedicine promoting chronic disease self-management and deeply discussed the positive role and improved suggestions of telemedicine in chronic disease self-management. Through the Technology Acceptance Model (TAM) (61), patients are provided with operational training and successful cases, and a clear legal regime is established to enhance the authority and trust of the telemedicine platform. In addition, improves the medical service system, establishes a multidisciplinary coordination mechanism, introduces corresponding telemedicine information protection policies, and encourages information sharing among hospitals at all levels, to improve the willingness of patients and hospitals to use telemedicine.
Author contributions
YL: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. QS: Data curation, Formal analysis, Methodology, Resources, Supervision, Validation, Visualization, Writing – original draft. JY: Data curation, Supervision, Writing – review & editing. LR: Data curation, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1510735/full#supplementary-material
References
1. World Health Organization. Noncommunicable diseases. (2023). Available at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed September 16, 2023).
2. Skýbová D, Šlachtová H, Tomášková H, Dalecká A, Madar R. Risk of chronic diseases limiting longevity and healthy aging by lifestyle and socio-economic factors during the life-course - a narrative review. Med Pr. (2021) 72:535–48. doi: 10.13075/mp.5893.01139
3. Hawrysz L, Gierszewska G, Bitkowska A. The research on patient satisfaction with remote healthcare prior to and during the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:338. doi: 10.3390/ijerph18105338
4. Alenoghena CO, Ohize HO, Adejo AO, Onumanyi AJ, Ohihoin EE, Balarabe AI, et al. Telemedicine: a survey of telecommunication technologies, developments, and challenges. J Sensor Actuator Netw. (2023) 12:20. doi: 10.3390/jsan12020020
5. Subramanian M, Wojtusciszyn A, Favre L, Boughorbel S, Shan J, Letaief KB, et al. Precision medicine in the era of artificial intelligence: implications in chronic disease management. J Transl Med. (2020) 18:472. doi: 10.1186/s12967-020-02658-5
6. Alvarez P, Sianis A, Brown J, Ali A, Briasoulis A. Chronic disease management in heart failure: focus on telemedicine and remote monitoring. Rev Cardiovasc Med. (2021) 22:403–13. doi: 10.31083/j.rcm2202046
7. Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. (2015) 17:e52. doi: 10.2196/jmir.3951
8. Sebastiani R, Anzivino A. The long and winding road of eHealth. The service ecosystem perspective. J Bus Ind Market. (2022) 37:2036–49. doi: 10.1108/JBIM-02-2021-0107
9. Walker RC, Tong A, Howard K, Palmer SC. Patient expectations and experiences of remote monitoring for chronic diseases: Systematic review and thematic synthesis of qualitative studies. Int J Med Inform. (2019) 124:78–85. doi: 10.1016/j.ijmedinf.2019.01.013
10. Creber A, Leo DG, Buckley BJR, Chowdhury M, Harrison SL, Isanejad M, et al. Use of telemonitoring in patient self-management of chronic disease: a qualitative meta-synthesis. BMC Cardiovasc Disord. (2023) 23:469. doi: 10.1186/s12872-023-03486-3
11. Lestari HM, Miranda AV, Fuady A. Barriers to telemedicine adoption among rural communities in developing countries: a systematic review and proposed framework. Clin Epidemiol Global Health. (2024) 28:101684. doi: 10.1016/j.cegh.2024.101684
12. Combi C, Pozzani G, Pozzi G. Telemedicine for developing countries. a survey and some design issues. Appl Clin Inform. (2016) 7:1025–50. doi: 10.4338/aci-2016-06-r-0089
13. Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. (2012) 12:181. doi: 10.1186/1471-2288-12-181
14. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. (2008) 8:45. doi: 10.1186/1471-2288-8-45
15. Bond CS, Worswick L. Self management and telehealth: lessons learnt from the evaluation of a dorset telehealth program. Patient. (2015) 8:311–6. doi: 10.1007/s40271-014-0091-y
16. Fairbrother P, Pinnock H, Hanley J, McCloughan L, Sheikh A, Pagliari C, et al. Continuity, but at what cost? The impact of telemonitoring COPD on continuities of care: a qualitative study. Prim Care Respir J. (2012) 21:322–8. doi: 10.4104/pcrj.2012.00068
17. Fairbrother P, Pinnock H, Hanley J, McCloughan L, Sheikh A, Pagliari C, et al. Exploring telemonitoring and self-management by patients with chronic obstructive pulmonary disease: a qualitative study embedded in a randomized controlled trial. Patient Educ Couns. (2013) 93:403–10. doi: 10.1016/j.pec.2013.04.003
18. Fairbrother P, Ure J, Hanley J, McCloughan L, Denvir M, Sheikh A, et al. Telemonitoring for chronic heart failure: The views of patients and healthcare professionals - a qualitative study. J Clin Nurs. (2014) 23:132–44. doi: 10.1111/jocn.12137
19. Gorst SL, Coates E, Armitage CJ. “It's sort of a lifeline”: chronic obstructive pulmonary disease patients' experiences of home telehealth. Health Psychol. (2016) 35:60–8. doi: 10.1037/hea0000246
20. Hanley J, Fairbrother P, Krishan A, McCloughan L, Padfield P, Paterson M, et al. Mixed methods feasibility study for a trial of blood pressure telemonitoring for people who have had stroke/transient ischaemic attack (TIA). Trials. (2015) 16:117. doi: 10.1186/s13063-015-0628-y
21. Hanley J, Fairbrother P, McCloughan L, Pagliari C, Paterson M, Pinnock H, et al. Qualitative study of telemonitoring of blood glucose and blood pressure in type 2 diabetes. BMJ Open. (2015) 5:e008896. doi: 10.1136/bmjopen-2015-008896
22. Riley JP, Gabe JP, Cowie MR. Does telemonitoring in heart failure empower patients for self-care? A qualitative study. J Clin Nurs. (2013) 22:2444–55. doi: 10.1111/j.1365-2702.2012.04294.x
23. Ure J, Pinnock H, Hanley J, Kidd G, McCall Smith E, Tarling A, et al. Piloting tele-monitoring in COPD: a mixed methods exploration of issues in design and implementation. Prim Care Respir J. (2012) 21:57–64. doi: 10.4104/pcrj.2011.00065
24. Williams V, Price J, Hardinge M, Tarassenko L, Farmer A. Using a mobile health application to support self-management in COPD: a qualitative study. Br J General Pract. (2014) 64:E392–400. doi: 10.3399/bjgp14X680473
25. Lan C, Qiu X, Shen M, Xiao X, Li J. Qualitative study on the real experience of patients with low willingness to accept heart failure mobile medical App. Chin J New Clin Med. (2021) 14:1238–41. doi: 10.3969/j.issn.1674-3806.2021.12.18
26. Tang C, Zhang X, Li B, Zhang A. Qualitative study on application experience of mobile medical platform for hypertension patients. Modern Nurse. (2022) 29:61–6. doi: 10.19791/j.cnki.1006-6411.2022.10.018
27. Li B, Zhang X, Tang C. Reasons for hypertension patients' refusal to use mobile health platform: a qualitative study. J Nurs Sci. (2019) 34:37–40. doi: 10.3870/i.issn.1001-4152.2019.05.037
28. Tang L, Guo A, Yu J, Chen Y. A qualitative study on the needs of health education based on mobile health in community-dwelling older patientswith Chronic Obstructive Pulmonary Disease. Chin Nurs Manage. (2022) 22:537–42. doi: 10.3969/j.issn.1672-1756.2022.04.012
29. Zhang Y, Xu Q, Li G. Qualitative study on remote pulmonary rehabilitation nursing needs of patients with chronic obstructive pulmonary disease. Chin J Prac Nurs. (2023) 39:2263–9. doi: 10.16460/j.issn.1008-9969.2024.15.062
30. Zhou T, Su M, Tian Y, Chen Y, Gu S. The Experience of using smart pillboxes among elderly patients with chronic conditions in communities based on the acceptance model of mobile medical application technology: a qualitative study Miltary Nurs. (2024) 41:1–4. doi: 10.3969/j.issn.2097-1826.2024.01.001
31. Chang CP, Lee TT, Mills ME. Experience of home telehealth technology in older patients with diabetes. CIN. (2017) 35:530–7. doi: 10.1097/CIN.0000000000000341
32. Jiang Y, Sun P, Chen Z, Guo J, Wang S, Liu F, et al. Patients' and healthcare providers' perceptions and experiences of telehealth use and online health information use in chronic disease management for older patients with chronic obstructive pulmonary disease: a qualitative study. BMC Geriatr. (2022) 22:9. doi: 10.1186/s12877-021-02702-z
33. Lu JF, Chi MJ, Chen CM. Advocacy of home telehealth care among consumers with chronic conditions. J Clin Nurs. (2014) 23:811–9. doi: 10.1111/jocn.12156
34. Alkawaldeh MY, Jacelon CS, Choi J. Older adults' experiences with a tablet-based self-management intervention for diabetes mellitus type II: a qualitative study. Geriatr Nurs. (2020) 41:305–12. doi: 10.1016/j.gerinurse.2019.11.010
35. Ladin K, Porteny T, Perugini JM, Gonzales KM, Aufort KE, Levine SK, et al. Perceptions of telehealth vs in-person visits among older adults with advanced kidney disease, care partners, and clinicians. JAMA Netw Open. (2021) 4:e2137193. doi: 10.1001/jamanetworkopen.2021.37193
36. Portz JD, Bayliss EA, Bull S, Boxer RS, Bekelman DB, Gleason K, et al. Using the technology acceptance model to explore user experience, intent to use, and use behavior of a patient portal among older adults with multiple chronic conditions: Descriptive qualitative study. J Med Internet Res. (2019) 21:e11604. doi: 10.2196/11604
37. Zulman DM, Jenchura EC, Cohen DM, Lewis ET, Houston TK, Asch SM. How can eHealth technology address challenges related to multimorbidity? Perspectives from patients with multiple chronic conditions. J Gen Intern Med. (2015) 30:1063–70. doi: 10.1007/s11606-015-3222-9
38. Ekstedt M, Nordheim ES, Hellström A, Strandberg S, Hagerman H. Patient safety and sense of security when telemonitoring chronic conditions at home: the views of patients and healthcare professionals - a qualitative study. BMC Health Serv Res. (2023) 23:581. doi: 10.1186/s12913-023-09428-1
39. Hägglund E, Strömberg A, Hagerman I, Lyngå P. Theory Testing of Patient Perspectives Using a Mobile Health Technology System in Heart Failure Self-care. J Cardiovasc Nurs. (2019) 34:448–53. doi: 10.1097/JCN.0000000000000595
40. Lyngå P, Fridlund B, Langius-Eklöf A, Bohm K. Perceptions of transmission of body weight and telemonitoring in patients with heart failure? Int J Qual Stud Health Well-being. (2013) 8:21524. doi: 10.3402/qhw.v8i0.21524
41. Poitras ME, Poirier MD, Couturier Y, T Vaillancourt V, Cormier C, Gauthier G, et al. Chronic conditions patient's perception of post-COVID-19 pandemic teleconsulting continuation in primary care clinics: a qualitative descriptive study. BMJ Open. (2022) 12:e066871. doi: 10.1136/bmjopen-2022-066871
42. Seto E, Leonard KJ, Masino C, Cafazzo JA, Barnsley J, Ross HJ. Attitudes of heart failure patients and health care providers towards mobile phone-based remote monitoring. J Med Internet Res. (2010) 12:e55. doi: 10.2196/jmir.1627
43. Sultan M, Kuluski K, McIsaac WJ, Cafazzo JA, Seto E. Turning challenges into design principles: Telemonitoring systems for patients with multiple chronic conditions. Health Informatics J. (2019) 25:1188–200. doi: 10.1177/1460458217749882
44. Huygens MW, Vermeulen J, Swinkels IC, Friele RD, van Schayck OC, de Witte LP. Expectations and needs of patients with a chronic disease toward self-management and eHealth for self-management purposes. BMC Health Serv Res. (2016) 16:232. doi: 10.1186/s12913-016-1484-5
45. Rahimpour M, Lovell NH, Celler BG, McCormick J. Patients' perceptions of a home telecare system. Int J Med Inform. (2008) 77:486–98. doi: 10.1016/j.ijmedinf.2007.10.006
46. Huniche L, Dinesen B, Nielsen C, Grann O, Toft E. Patients' use of self-monitored readings for managing everyday life with COPD: A qualitative study. Telemed e-Health. (2013) 19:396–402. doi: 10.1089/tmj.2012.0135
47. Poppe L, Crombez G, De Bourdeaudhuij I, Van der Mispel C, Shadid S, Verloigne M. Experiences and opinions of adults with type 2 diabetes regarding a self-regulation-based ehealth intervention targeting physical activity and sedentary behaviour. Int J Environ Res Public Health. (2018) 15:954. doi: 10.3390/ijerph15050954
48. Scheibe M, Lang C, Druschke D, Arnold K, Luntz E, Schmitt J, et al. Independent use of a home-based telemonitoring app by older patients with multimorbidity and mild cognitive impairment: qualitative study. JMIR Hum Factors. (2021) 8:e27156. doi: 10.2196/27156
49. Vatnøy TK, Thygesen E, Dale B. Telemedicine to support coping resources in home-living patients diagnosed with chronic obstructive pulmonary disease: patients' experiences. J Telemed Telecare. (2017) 23:126–32. doi: 10.1177/1357633X15626854
50. Ding H, Jayasena R, Chen SH, Maiorana A, Dowling A, Layland J, et al. The effects of telemonitoring on patient compliance with self-management recommendations and outcomes of the innovative telemonitoring enhanced care program for chronic heart failure: randomized controlled trial. J Med Internet Res. (2020) 22:e17559. doi: 10.2196/17559
51. Reiners F Sturm J Bouw LJW and Wouters EJM. Sociodemographic factors influencing the use of ehealth in people with chronic diseases. Int J Environ Res Public Health. (2019) 16:645. doi: 10.3390/ijerph16040645
52. Timpel P, Oswald S, Schwarz PEH, Harst L. Mapping the evidence on the effectiveness of telemedicine interventions in diabetes, dyslipidemia, and hypertension: an umbrella review of systematic reviews and meta-analyses. J Med Internet Res. (2020) 22:e16791. doi: 10.2196/16791
53. Hanlon P, Daines L, Campbell C, McKinstry B, Weller D, Pinnock H. Telehealth interventions to support self-management of long-term conditions: a systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. J Med Internet Res. (2017) 19:e172. doi: 10.2196/jmir.6688
54. Akbar S, Coiera E, Magrabi F. Safety concerns with consumer-facing mobile health applications and their consequences: a scoping review. J Am Med Inform Assoc. (2020) 27:330–40. doi: 10.1093/jamia/ocz175
55. Haveland S, Islam S. Key considerations in ensuring a safe regional telehealth care model: a systematic review. Telemed J E Health. (2022) 28:602–12. doi: 10.1089/tmj.2020.0580
56. Yi M, Hui Y, Hu L, Zhang W, Wang Z. The experiences and perceptions of older adults with multimorbidity toward e-health care: a qualitative evidence synthesis. Telemed J E Health. (2024) 30:2527–44. doi: 10.1089/tmj.2024.0211
57. Hersh W, Helfand M, Wallace J, Kraemer D, Patterson P, Shapiro S, et al. A systematic review of the efficacy of telemedicine for making diagnostic and management decisions. J Telemed Telecare. (2002) 8:197–209. doi: 10.1258/135763302320272167
58. Ndlovu K, Mars M, Scott RE. Interoperability frameworks linking mHealth applications to electronic record systems. BMC Health Serv Res. (2021) 21:459. doi: 10.1186/s12913-021-06473-6
59. Vorderstrasse A, Lewinski A, Melkus GD, Johnson C. Social support for diabetes self-management via eHealth interventions. Curr Diab Rep. (2016) 16:56. doi: 10.1007/s11892-016-0756-0
60. McCool J, Dobson R, Whittaker R, Paton C. Mobile health (mHealth) in low- and middle-income countries. Annu Rev Public Health. (2022) 43:525–39. doi: 10.1146/annurev-publhealth-052620-093850
Keywords: telemedicine, chronic disease management, electronic health, qualitative meta-synthesis, self-management
Citation: Li Y, Shi Q, Yang J and Ran L (2025) Exploring the impact of telemedicine in chronic patients from diverse socioeconomic contexts: systematic review of qualitative studies. Front. Public Health 12:1510735. doi: 10.3389/fpubh.2024.1510735
Received: 13 October 2024; Accepted: 31 December 2024;
Published: 29 January 2025.
Edited by:
Uffe Kock Wiil, University of Southern Denmark, DenmarkReviewed by:
Claudia Affonso Silva Araujo, Federal University of Rio de Janeiro, BrazilVirtudes Pérez-Jover, Miguel Hernández University, Spain
Copyright © 2025 Li, Shi, Yang and Ran. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qifang Shi, cWlmYW5nc2hpQG1haWwueGp0dS5lZHUuY24=
 Yuzhe Li
Yuzhe Li Qifang Shi*
Qifang Shi*