- 1Department of Pediatrics, School of Medicine, Arak University of Medical Sciences, Arak, Iran
- 2Department of Medicine, Student Research Center, Iran University of Medical Sciences, Tehran, Iran
- 3Department of Health Services Management, Islamic Azad University, North Tehran Branch, Tehran, Iran
- 4Department of Epidemiology, Faculty of Health, Arak University of Medical Sciences, Arak, Iran
Introduction: The self-medication of antibiotics is a global crisis, posing a significant challenge to healthcare systems worldwide. This study aimed to investigate the frequency of self-medication in the adult population and the factors influencing it.
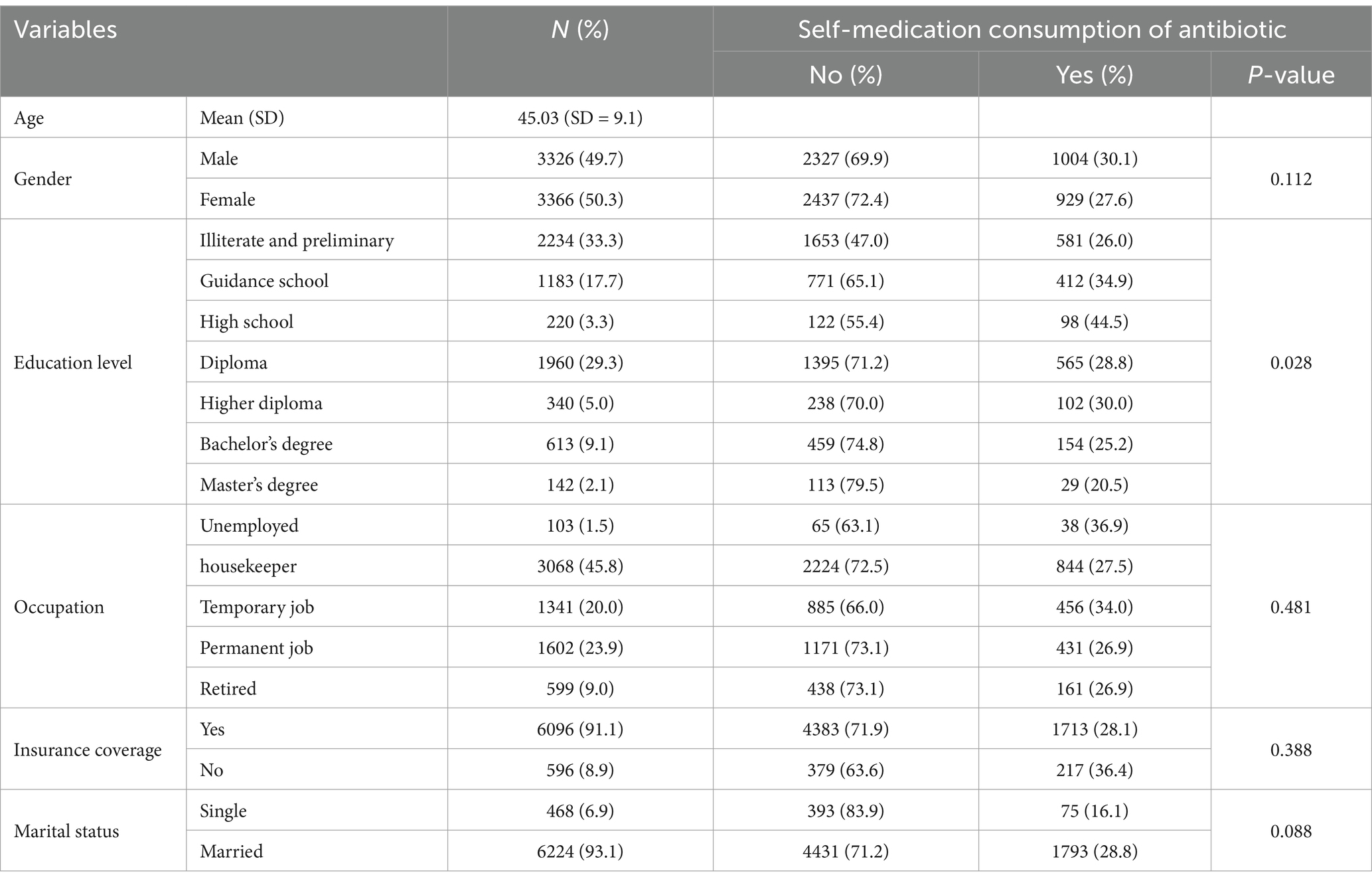
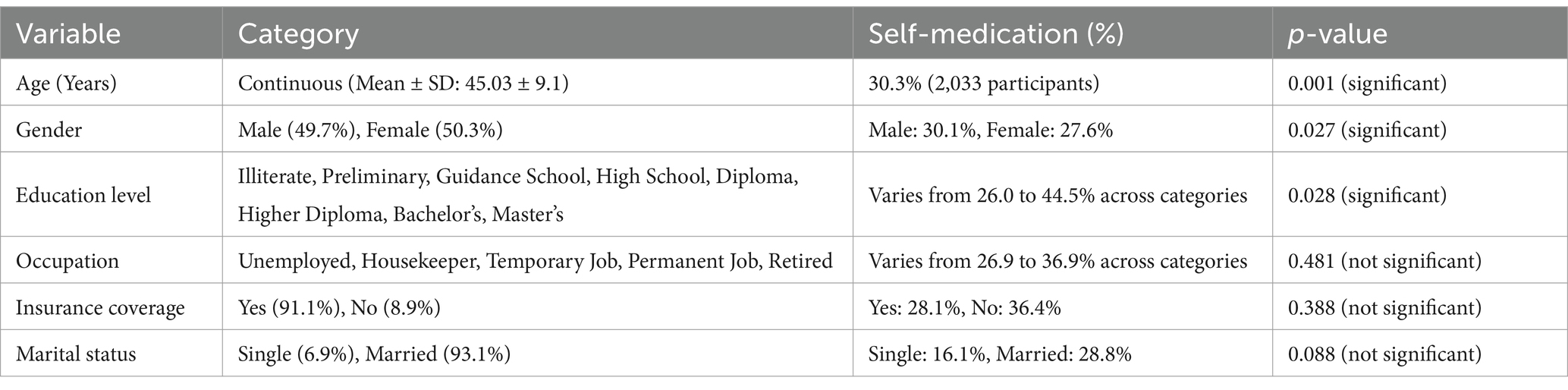
Methods: This population-based cross-sectional study was conducted in Arak, a city in central Iran, from January 2019 to January 2020. Stratified random sampling was used to determine the recruitment criteria, and a total of 6,692 individuals participated in the study. Self-medication of antibiotics was defined as the self-reported annual consumption of antibiotics, as well as a record of antibiotic use registered in insurance services during the same period. The variables examined in this study included age, gender, educational level, occupational status, insurance coverage, and marital status. All gathered data were analyzed using SPSS version 16.0 and STATA version 16.0 software. p-values < 0.05 were considered statistically significant.
Results: The annual prevalence of antibiotic self-medication was 30.3% (n = 2,033). Chi-square and Mann–Whitney tests identified a significant correlation between educational level and self-medication practices (p = 0.028), while no significant associations were observed with gender, occupation, insurance coverage, or marital status. Logistic regression analysis revealed that female participants were less likely to self-medicate (p = 0.027), and both older age and higher levels of education were associated with a reduced likelihood of antibiotic self-medication (p = 0.001 and p = 0.044, respectively).
Conclusion: Factors such as female gender, older age, and higher education levels are significant determinants affecting antibiotic self-medication.
Introduction
While drug therapy has significantly benefited humanity, the indiscriminate use of medications can have severe consequences. Self-medication refers to the practice of individuals treating their self-diagnosed symptoms or conditions without consulting a healthcare professional (1). This encompasses reusing prescribed medications for chronic illnesses or similar symptoms, administering one’s medication to family members, prematurely discontinuing treatment after initial symptom relief, using leftover drugs at home, and experimenting with alternative therapies such as herbal remedies or non-professionally recommended drugs (2, 3). Self-medication poses a myriad of risks, including contributing to global health challenges like antimicrobial resistance, a crisis recognized by the WHO. It also increases the likelihood of drug interactions, heightened side effects, accidental poisoning, delays in proper diagnosis and treatment, wastage of time and financial resources, market interference, and a rise in per capita drug consumption. These factors collectively strain public health systems, economies, and societal well-being (4, 5).
The widespread and arbitrary use of antibiotics presents a formidable challenge to healthcare providers globally. Approximately half of all antibiotics are sold over the counter worldwide, with staggering rates of 82% in the Middle East, 75% in Asia, 74% in Africa, 68% in Europe, and 42% in the United States (6–9). This accessibility contributes significantly to the prevalence of self-medication of antibiotics (SMA), particularly in low to middle-income countries. Factors such as economic instability, easy access to medications without prescriptions, inadequate distribution and availability of antibiotics, limited access to professional healthcare, high healthcare costs, long wait times at medical facilities, and patient distrust in medical advice all contribute to this trend (10, 11). The misuse and overuse of antibiotics by the general population have directly fueled the rise of multidrug-resistant bacterial species. These microorganisms pose a critical threat to the effectiveness of current antibiotic treatments, rendering many antibiotics ineffective. Consequently, resistant pathogens lead to difficult-to-treat infections, prolonged illness durations, more complex and costly treatment regimens, increased medical consultations, extended hospital stays, and in severe cases, fatalities (12, 13).
The initial step in tackling the global challenge of antibiotic resistance involves assessing its prevalence and identifying associated risk factors. Armed with this understanding, efforts can be efficiently directed toward developing strategies to curb indiscriminate antibiotic use and mitigate antibiotic resistance (14). Given the limited information on antibiotic self-medication practices in Iran and their potential community-wide impacts, this study was conducted to investigate the prevalence of self-medication with antibiotics (SMA) and its influencing factors among adults in Iran. By examining the extent of SMA and its determinants, this research aims to provide crucial insights into the behaviors and circumstances surrounding antibiotic use in Iran. These findings are essential for informing targeted interventions and policy initiatives aimed at promoting responsible antibiotic practices, safeguarding public health, and preserving the effectiveness of antibiotics in combating infectious diseases.
Methods
Study design and setting
This study employed a population-based cross-sectional design conducted in Arak city, located in central Iran, from January 2019 to January 2020. Based on the most recent census data available in 2019, the population of Arak city was approximately 520,944. The study aimed to assess the prevalence and determinants of self-medication with antibiotics (SMA) among adults in Arak.
Sample size and sampling technique
The sample size of 6,692 participants was determined using statistical calculations to achieve a confidence level of 95% and a margin of error of 1.2%. Stratified random sampling was utilized to ensure demographic representation across key subgroups such as age, gender, and educational level. Stratification was conducted by dividing the population into strata based on these variables, and participants were randomly selected within each stratum proportional to its size in the population.
Eligibility criteria
Inclusion criteria were as follows:
• Participants had to be Iranian citizens.
• Residents of Arak for a minimum of 3 years.
• Adults aged 18 years and above who were willing to provide informed consent.
Exclusion criteria included individuals who declined to participate or provided incomplete responses.
Definition of self-medication
Self-medication with antibiotics (SMA) was defined as the self-reported annual consumption of antibiotics that were not corroborated by insurance records during the same period. Insurance records were not used to document SMA directly but served as a benchmark for cross-validation. Antibiotic consumption that did not align with insurance claims was classified as potential SMA.
Questionnaire development
The questionnaire used for data collection was adapted from validated tools previously employed in similar studies on SMA. Modifications were made to suit the cultural and contextual nuances of the study population. It included sections on demographic and socio-economic variables (age, gender, educational level, occupational status, insurance coverage, and marital status) as well as antibiotic use practices.
Pilot testing
The adapted questionnaire underwent a pilot test with a subset of 669 participants (10% of the study sample size). Feedback from the pilot study helped refine the questionnaire by identifying ambiguous or irrelevant questions and ensuring cultural appropriateness. Reliability was assessed using Cronbach’s Alpha, which yielded a score of 0.85, indicating good internal consistency.
Data collection
Data collection was conducted through face-to-face interviews by trained personnel. The interviews were held in public areas, healthcare centers, and community hubs in Arak. Participants were informed about the study objectives, and written informed consent was obtained prior to participation. Privacy and confidentiality were strictly maintained throughout the data collection process. Data were anonymized, securely stored, and used solely for research purposes. To ensure data accuracy, all responses were cross-checked with insurance records where applicable. Discrepancies were resolved through follow-up interviews. The validated dataset provided a robust basis for analyzing the prevalence and determinants of SMA.
Ethical considerations
The study was approved by the Ethics Committee of Arak University of Medical Sciences (Ethics Code: IR.ARAKMU.REC.1398.207). All procedures adhered to the principles of the Declaration of Helsinki. Participants provided written informed consent, and no personally identifiable information was collected.
Statistical analysis
Data were analyzed using SPSS version 16.0 and STATA version 16.0 software. Descriptive statistics, including frequencies, means, and standard deviations (SD), were calculated for categorical and continuous variables.
• Association Testing: Chi-square and Mann–Whitney U tests were used to compare categorical and continuous variables, respectively.
• Regression Analysis: Univariate logistic regression was performed to identify potential predictors of SMA. Variables with a p-value of less than 0.25 were included in a multiple logistic regression model to adjust for confounders and determine independent predictors. Odds ratios (OR) and 95% confidence intervals (CI) were reported.
• Model Validation: The final regression model was assessed for goodness-of-fit and multicollinearity to ensure reliability.
Statistical significance was set at p < 0.05 for all tests, and results were interpreted with confidence interval of 95%.
Results
The descriptive characteristics of the study participants are presented in Table 1. The mean age of participants was 45.03 years (SD = 9.1), with 49.7% being male. A significant portion had attained a diploma as their highest educational level (29.3%), and the majority were employed as housekeepers (45.8%). Insurance coverage was widespread among participants, with 91.1% reporting coverage.
Regarding antibiotic self-medication, the study found an annual prevalence rate of 30.3% (n = 2033). Statistical analyses, including chi-square and Mann–Whitney tests, revealed a significant association between educational level and self-medication of antibiotics (p-value = 0.028). However, no significant differences were observed by gender, occupation, insurance coverage, or marital status.
Logistic regression analysis results, detailed in Table 2, indicated that female participants exhibited a lower likelihood of self-medicating with antibiotics (p-value = 0.027). Furthermore, older age and higher educational attainment were also associated with reduced odds of antibiotic self-medication (p-values 0.001 and 0.044, respectively).
Discussion
This study highlights the significant prevalence of self-medication with antibiotics (SMA) in Arak, Iran, and its contribution to the growing global threat of antimicrobial resistance (AMR). The findings underline the urgent need for practical interventions to curb SMA, including public awareness campaigns to educate communities about the risks associated with AMR and self-prescribing antibiotics. Strict regulatory enforcement is critical to limit over-the-counter access to antibiotics, ensuring they are dispensed only with appropriate prescriptions. Additionally, policymakers should encourage practices such as dispensing antibiotics in precise doses rather than entire packages to reduce leftover medications that often contribute to misuse. Enhancing healthcare accessibility and affordability is also essential to reduce reliance on self-medication. These measures require coordinated efforts from policymakers, healthcare providers, and public health authorities to safeguard the effectiveness of antibiotics and mitigate the burden of SMA on healthcare systems. The self-medication of antibiotics (SMA) poses a global crisis affecting both developed and developing nations. Overuse and misuse of antibiotics have led to widespread antimicrobial resistance among microorganisms, undermining the efficacy of common treatments. While antimicrobial resistance stands as a paramount consequence, SMA also contributes to adverse side effects, drug interactions, and imposes additional economic burdens. Our study focused on investigating the prevalence of SMA and its associated factors among the Iranian adult population. We identified a troublingly high prevalence of SMA and identified several significant factors associated with this practice. These findings underscore the urgent need for health policymakers to reconsider antibiotic stewardship and distribution policies. By limiting public access to over-the-counter antibiotics and promoting responsible use through targeted interventions, we can mitigate the impact of SMA on public health outcomes and preserve the effectiveness of antibiotics for future generations.
In our survey, 30.3% of participants reported practicing SMA over the past year. This rate appears lower compared to previous studies conducted in other regions of Iran. For instance, a study by Heidarifar et al. (15) conducted in Qom, a central province of Iran, reported a SMA prevalence of 57.6% among the general population in 2011. Similarly, research in Shiraz, a southern province, found that approximately 44.5% of patients admitted to primary care centers practiced SMA in 2009 (16). A systematic review from 2015 estimated the overall prevalence of self-medication in Iran to be 53%, with antibiotics being one of the most commonly used over-the-counter medications (17). Over time, there has been a noticeable decline in SMA prevalence in Iran, potentially attributed to factors such as increased public awareness, higher antibiotic costs, and periodic shortages of antibiotics in pharmacies (18, 19). However, compared to other low- to middle-income countries in Asia, Iranian rates remain relatively moderate. For instance, SMA rates were reported as 90.0% in Erbil, Iraq; 84.8% in Karachi, Pakistan; 74.7% in Medina, Saudi Arabia; and 73.2% in Kabul, Afghanistan (20–23). In contrast, many European countries exhibit lower SMA prevalence rates, such as 22% in Lithuania; 20% in Greece; 18.9% in Portugal; and 16% in Romania (24–27). Regarding the sources of antibiotics used in SMA practices in Iran, M. Askarian et al. found that 71.7% of participants obtained antibiotics from pharmacies as over-the-counter medications, while 36% sourced their unprescribed antibiotics from their home drug storage (16). Another study highlighted a high prevalence (82%) of home storage of medications among the Iranian population (28).
Based on our findings, age emerges as a significant factor associated with SMA, with older participants showing lower rates of SMA. This aligns with findings from various studies across different regions. For instance, a Turkish study reported that individuals aged 40–49 years were approximately twice as likely to self-medicate with antibiotics compared to those aged 60–69 years (29). Similarly, Bogale et al. (30) found a decreasing prevalence of SMA with increasing age, with individuals over 60 years having the lowest frequency of SMA. In line with these observations, another study identified age as a significant predictor of SMA, highlighting the highest prevalence among the youngest age group (18–34 years) (26). Likewise, research conducted in Jordan indicated a 1.6-fold higher prevalence of SMA among individuals aged 18–39 years compared to those aged 40–59 years (31). Furthermore, studies focusing on specific demographics, such as mothers, have also noted higher rates of SMA among younger age groups (32). However, contrasting results exist in the literature, with some studies finding no significant association between age and SMA (33, 34).
According to our study findings, women exhibit a lower likelihood of consuming antibiotics on an arbitrary basis compared to men. This observation is consistent with studies conducted in other regions. For instance, Ilhan et al. (29) found that male participants self-medicated with antibiotics 1.24 times more frequently than females. Similarly, research among Portuguese individuals indicated a higher prevalence of antibiotic self-medication among males compared to females (26). However, findings on the association between gender and SMA remain controversial. Some studies have reported no significant difference in the prevalence of SMA between genders (30, 33, 34).
Our study also revealed that participants with higher levels of education exhibit a lower prevalence of SMA. This finding aligns with research conducted by Al-Azzam et al. (31), which similarly demonstrated that individuals with a higher educational background are less likely to engage in SMA practices. Consistent results have been reported across various studies, highlighting the role of higher education in reducing the frequency of SMA (30, 33, 34). Across different countries, there remains a notable lack of public knowledge regarding SMA and its implications for antibiotic resistance (35–38). Common misconceptions persist, such as the belief that antibiotics are effective in treating symptoms like fever, cough, and runny nose, regardless of whether the cause is viral or bacterial (39). Such misunderstandings contribute to inappropriate antibiotic use and the perpetuation of SMA practices. Moreover, previous positive experiences with specific antibiotics may lead individuals to reuse them for subsequent symptoms, despite the potential ineffectiveness or harm (40, 41).
The results of our regression analysis reveal that there is no significant association between SMA and occupational status, insurance coverage, or marital status among our study participants. This finding is consistent with previous studies that have also reported no significant relationships between these variables and the prevalence of SMA (30, 32). Further extensive and rigorous research on the association between independent variables and SMA is needed.
To address the high prevalence of self-medication, it is essential for regulatory bodies to enforce existing legislation strictly and to close loopholes that allow over-the-counter sales of antibiotics. Public health campaigns focusing on antimicrobial resistance and responsible antibiotic use could also reduce the rates of inappropriate consumption. Collaborations between healthcare providers, pharmacies, and policymakers are crucial to develop sustainable interventions.
It is important to note that our study provides valuable insights into the prevalence of SMA and associated sociodemographic factors among a substantial sample of the Iranian adult population (n = 6692). To mitigate recall bias, we utilized participants’ insurance records as supplementary data. Given the cross-sectional nature of our study design, it is crucial to acknowledge that we cannot establish a cause-and-effect relationship between SMA and the variables examined. Therefore, future research employing longitudinal strategies, such as cohort studies, is essential to explore and confirm these relationships over time. By conducting more rigorous and longitudinal investigations, we can better understand how factors like occupational status, insurance coverage, and marital status influence antibiotic self-medication practices. This knowledge is vital for developing targeted interventions and policies aimed at promoting appropriate antibiotic use and combating antimicrobial resistance effectively. It is important to note that insurance records may not capture all instances of prescribed antibiotic use, which could lead to some misclassification of self-medication practices.
Conclusion
This study highlights a significant prevalence of self-medication with antibiotics (SMA) among adults in Arak, Iran, and identifies key demographic factors associated with this behavior. Notably, SMA was found to be higher among certain education and occupation groups, while variables such as marital status and insurance coverage showed no significant associations. These findings emphasize the complexity of SMA and its multifactorial nature, shedding light on patterns that are crucial for designing targeted interventions.
The practice of SMA poses a serious threat to public health, contributing to the growing crisis of antimicrobial resistance (AMR). Our study underscores the urgent need for comprehensive public health strategies, including:
1. Policy Reforms: Stricter enforcement of regulations governing antibiotic sales and dispensing, particularly to prevent over-the-counter access without a prescription.
2. Educational Campaigns: Raising awareness about the risks of SMA and AMR through tailored community-level interventions.
3. Pharmacy Practices: Implementing measures such as dispensing antibiotics in exact doses and encouraging the return of unused medications to pharmacies to reduce antibiotic leftovers.
4. Healthcare Accessibility: Enhancing accessibility and affordability of professional healthcare services to reduce reliance on self-medication practices.
Given the limitations of using insurance records as a benchmark for self-medication and the cross-sectional nature of this study, future research should employ longitudinal designs and explore the effectiveness of specific interventions in reducing SMA. Additionally, comparative studies across different regions of Iran and other countries can provide valuable insights into cultural and systemic factors influencing antibiotic misuse.
Our findings serve as a critical call to action for policymakers, healthcare professionals, and public health authorities to address SMA and safeguard the efficacy of antibiotics in the fight against infectious diseases.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Arak University of Medical Sciences, Project ethics code: IR.ARAKMU.REC.1398.207. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JN: Project administration, Writing – review & editing. RG: Investigation, Writing – original draft. NC-S: Validation, Writing – review & editing. RM: Supervision, Writing – review & editing. MN: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fresle, DA, and Wolfheim, C. Public education in rational drug use: a global survey. Geneva, Switzerland: World Health Organization (1997).
2. World Health Organization. Guidelines for the regulatory assessment of medicinal products for use in self-medication. Geneva, Switzerland: World Health Organization (2000).
3. Grigoryan, L, Burgerhof, JG, Haaijer-Ruskamp, FM, Degener, JE, Deschepper, R, Monnet, DL, et al. Is self-medication with antibiotics in Europe driven by prescribed use? J Antimicrob Chemother. (2007) 59:152–6. doi: 10.1093/jac/dkl457
4. Behzadifar, M, Behzadifar, M, Aryankhesal, A, Ravaghi, H, Baradaran, HR, Sajadi, HS, et al. Prevalence of self-medication in university students: systematic review and meta-analysis. East Mediterr Health J. (2020) 26:846–57. doi: 10.26719/emhj.20.052
5. Bell, BG, Schellevis, F, Stobberingh, E, Goossens, H, and Pringle, M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis. (2014) 14:1–25. doi: 10.1186/1471-2334-14-13
6. Morgan, DJ, Okeke, IN, Laxminarayan, R, Perencevich, EN, and Weisenberg, S. Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis. (2011) 11:692–701. doi: 10.1016/S1473-3099(11)70054-8
7. Alhomoud, F, Aljamea, Z, Almahasnah, R, Alkhalifah, K, Basalelah, L, and Alhomoud, FK. Self-medication and self-prescription with antibiotics in the Middle East—do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int J Infect Dis. (2017) 57:3–12. doi: 10.1016/j.ijid.2017.01.014
8. Widowati, IG, Budayanti, NN, Januraga, PP, and Duarsa, DP. Self-medication and self-treatment with short-term antibiotics in Asian countries: a literature review. Pharm Educ. (2021) 21:152–62. doi: 10.46542/pe.2021.212.152162
9. Zhou, Z, Zhao, D, Zhang, H, Shen, C, Cao, D, Liu, G, et al. Understanding parental self-medication with antibiotics among parents of different nationalities: a cross-sectional study. Global Health Res Policy. (2021) 6:1. doi: 10.1186/s41256-021-00226-y
10. Aslam, A, Gajdács, M, Zin, CS, Ab Rahman, NS, Ahmed, SI, Zafar, MZ, et al. Evidence of the practice of self-medication with antibiotics among the lay public in low-and middle-income countries: a scoping review. Antibiotics. (2020) 9:597. doi: 10.3390/antibiotics9090597
11. Torres, NF, Chibi, B, Middleton, LE, Solomon, VP, and Mashamba-Thompson, TP. Evidence of factors influencing self-medication with antibiotics in low and middle-income countries: a systematic scoping review. Public Health. (2019) 168:92–101. doi: 10.1016/j.puhe.2018.11.018
12. Mancuso, G, Midiri, A, Gerace, E, and Biondo, C. Bacterial antibiotic resistance: the most critical pathogens. Pathogens. (2021) 10:1310. doi: 10.3390/pathogens10101310
13. Pachori, P, Gothalwal, R, and Gandhi, P. Emergence of antibiotic resistance Pseudomonas aeruginosa in intensive care unit; a critical review. Genes Dis. (2019) 6:109–19. doi: 10.1016/j.gendis.2019.04.001
14. Mali, SB, and Dahivelkar, S. Antibiotic resistance: how to fight. New Delhi, India: Springer Nature. (2020).
15. Heidarifar, R, Koohbor, M, Kazemian Mansourabad, M, Mikaili, P, and Sarahroodi, S. Self medication with antibiotics among Iranian population in Qom state. J Sci Innov Res. (2013) 2:785–9.
16. Askarian, M, Hosseingholizadeh Mahani, M, Danaei, M, and Momeni, M. A study of antibiotics self-medication at primary health care centers in shiraz, southern Iran. J Health Sci Surveill Syst. (2013) 1:1–5.
17. Azami-Aghdash, S, Mohseni, M, Etemadi, M, Royani, S, Moosavi, A, and Nakhaee, M. Prevalence and cause of self-medication in Iran: a systematic review and meta-analysis article. Iran J Public Health. (2015) 44:1580–93.
18. Malik, B, and Bhattacharyya, S. Antibiotic drug-resistance as a complex system driven by socio-economic growth and antibiotic misuse. Sci Rep. (2019) 9:9788. doi: 10.1038/s41598-019-46078-y
19. Kamran, A, Sharifirad, G, Shafaeei, Y, and Mohebi, S. Associations between self-medication, health literacy, and self-perceived health status: a community-based study. Int J Prev Med. (2015) 6:1–7.
20. Muhammed, R, al-Ani, A, and Yassen, A. Self-medication with antibiotic among public population in Erbil city. JPRI. (2021) 33:25–33. doi: 10.9734/jpri/2021/v33i44B32649
21. Afridi, MI, Rasool, G, Tabassum, R, Shaheen, M, and Shujauddin, M. Prevalence and pattern of self-medication in Karachi: a community survey. Pak J Med Sci. (2015) 31:1241–5. doi: 10.12669/pjms.315.8216
22. Allam, AT, and Amer, SM. Prevalence and factors influencing self-medication in Medina Al-Munawara, Saudi Arabia. Arch Pharm Pract. (2020) 11:50–57.
23. Roien, R, Bhandari, D, Hosseini, SM, Mosawi, SH, Ataie, MA, Ozaki, A, et al. Prevalence and determinants of self-medication with antibiotics among general population in Afghanistan. Expert Rev Anti-Infect Ther. (2022) 20:315–21. doi: 10.1080/14787210.2021.1951229
24. Berzanskyte, A, Valinteliene, R, Haaijer-Ruskamp, FM, Gurevicius, R, and Grigoryan, L. Self-medication with antibiotics in Lithuania. Int J Occup Med Environ Health. (2006) 19:246–53. doi: 10.2478/v10001-006-0030-9
25. Lescure, D, Paget, J, Schellevis, F, and Van Dijk, L. Determinants of self-medication with antibiotics in European and Anglo-Saxon countries: a systematic review of the literature. Front Public Health. (2018) 6:370. doi: 10.3389/fpubh.2018.00370
26. Ramalhinho, I, Cordeiro, C, Cavaco, A, and Cabrita, J. Assessing determinants of self-medication with antibiotics among Portuguese people in the Algarve region. Int J Clin Pharm. (2014) 36:1039–47. doi: 10.1007/s11096-014-9992-z
27. Lebanova, HV, Stoev, SN, Veleva, NR, Belcheva, SP, Madzharov, VG, and Gueorguiev, SR. Prevalence of self-medication with antibiotics in Europe: a scoping review. J Biomed Clin Res. (2023) 16:5–16.
28. Sahebi, L, and Vahidi, RG. Self-medication and storage of drugs at home among the clients of drugstores in Tabriz. Curr Drug Saf. (2009) 4:107–12. doi: 10.2174/157488609788172982
29. Ilhan, MN, Durukan, E, Ilhan, SÖ, Aksakal, FN, Özkan, S, and Bumin, MA. Self-medication with antibiotics: questionnaire survey among primary care center attendants. Pharmacoepidemiol Drug Saf. (2009) 18:1150–7. doi: 10.1002/pds.1829
30. Bogale, AA, Amhare, AF, Chang, J, Bogale, HA, Betaw, ST, Gebrehiwot, NT, et al. Knowledge, attitude, and practice of self-medication with antibiotics among community residents in Addis Ababa, Ethiopia. Expert Rev Anti-Infect Ther. (2019) 17:459–66. doi: 10.1080/14787210.2019.1620105
31. Al-Azzam, SI, Al-Husein, BA, Alzoubi, F, Masadeh, MM, and Al-Horani, S. Self-medication with antibiotics in Jordanian population. Int J Occup Med Environ Health. (2007) 20:373–80. doi: 10.2478/v10001-007-0038-9
32. Nazari, J, Chezani-Sharahi, N, Eshrati, B, Yadegari, A, Naghshbandi, M, Movahedi, H, et al. Prevalence and determinants of self-medication consumption of antibiotics in children in Iran: a population-based cross-sectional study, 2018–19. PLoS One. (2022) 17:e0278843. doi: 10.1371/journal.pone.0278843
33. Jamhour, A, El-Kheir, A, Salameh, P, Abi Hanna, P, and Mansour, H. Antibiotic knowledge and self-medication practices in a developing country: a cross-sectional study. Am J Infect Control. (2017) 45:384–8. doi: 10.1016/j.ajic.2016.11.026
34. Pavydė, E, Veikutis, V, Mačiulienė, A, Mačiulis, V, Petrikonis, K, and Stankevičius, E. Public knowledge, beliefs and behavior on antibiotic use and self-medication in Lithuania. Int J Environ Res Public Health. (2015) 12:7002–16. doi: 10.3390/ijerph120607002
35. Nepal, G, and Bhatta, S. Self-medication with antibiotics in WHO southeast Asian region: a systematic review. Cureus. (2018) 10:2428. doi: 10.7759/cureus.2428
36. Widayati, A, Suryawati, S, de Crespigny, C, and Hiller, JE. Self medication with antibiotics in Yogyakarta City Indonesia: a cross sectional population-based survey. BMC Res Notes. (2011) 4:1–8. doi: 10.1186/1756-0500-4-491
37. Elong Ekambi, GA, Okalla Ebongue, C, Penda, IC, Nnanga Nga, E, Mpondo Mpondo, E, and Eboumbou Moukoko, CE. Knowledge, practices and attitudes on antibiotics use in Cameroon: self-medication and prescription survey among children, adolescents and adults in private pharmacies. PLoS One. (2019) 14:e0212875. doi: 10.1371/journal.pone.0212875
38. Karimy, M, Rezaee-Momtaz, M, Tavousi, M, Montazeri, A, and Araban, M. Risk factors associated with self-medication among women in Iran. BMC Public Health. (2019) 19:1–7. doi: 10.1186/s12889-019-7302-3
39. Kurniawan, K, Posangi, J, and Rampengan, N. Association between public knowledge regarding antibiotics and self-medication with antibiotics in teling atas community health center, East Indonesia. Med Jo Univ Indones. (2017) 26:62–9. doi: 10.13181/mji.v26i1.1589
40. Effah, CY, Amoah, AN, Liu, H, Agboyibor, C, Miao, L, Wang, J, et al. A population-base survey on knowledge, attitude and awareness of the general public on antibiotic use and resistance. Antimicrob Resist Infect Control. (2020) 9:1–9. doi: 10.1186/s13756-020-00768-9
Keywords: self-medication, antibiotics, antibiotics resistance, prevalence, self-consumption
Citation: Nazari J, Ghafoury R, Chezani-Sharahi N, Moradzadeh R and Naghshbandi M (2024) Prevalence and determinants of self-medication consumption of antibiotics in adults in Iran: a population based cross-sectional study, 2019–2020. Front. Public Health. 12:1502074. doi: 10.3389/fpubh.2024.1502074
Edited by:
Raphael Zozimus Sangeda, Muhimbili University of Health and Allied Sciences, TanzaniaReviewed by:
Aida Bianco, University of Magna Graecia, ItalyWael Mansy, King Saud University, Saudi Arabia
Copyright © 2024 Nazari, Ghafoury, Chezani-Sharahi, Moradzadeh and Naghshbandi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mobin Naghshbandi, bmFnaHNoYmFuZGkubW9iaW43N0BnbWFpbC5jb20=
 Javad Nazari
Javad Nazari Roya Ghafoury
Roya Ghafoury Nahid Chezani-Sharahi3
Nahid Chezani-Sharahi3 Mobin Naghshbandi
Mobin Naghshbandi