- 1Nanjing Stomatological Hospital, Affiliated Hospital of Medical School, Institute of Stomatology, Nanjing University, Nanjing, China
- 2Department of Stomatology, Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School, Nanjing, China
Introduction: Periodontal disease is a common chronic inflammatory condition that affects oral health and carries broader public health implications. This study aimed to assess the levels of knowledge, attitudes and practices (KAP) among patients with periodontal disease toward disease management.
Methods: This cross-sectional web-based study was conducted between March 2022 and March 2023. A self-administered questionnaire was designed to evaluate KAP toward disease management.
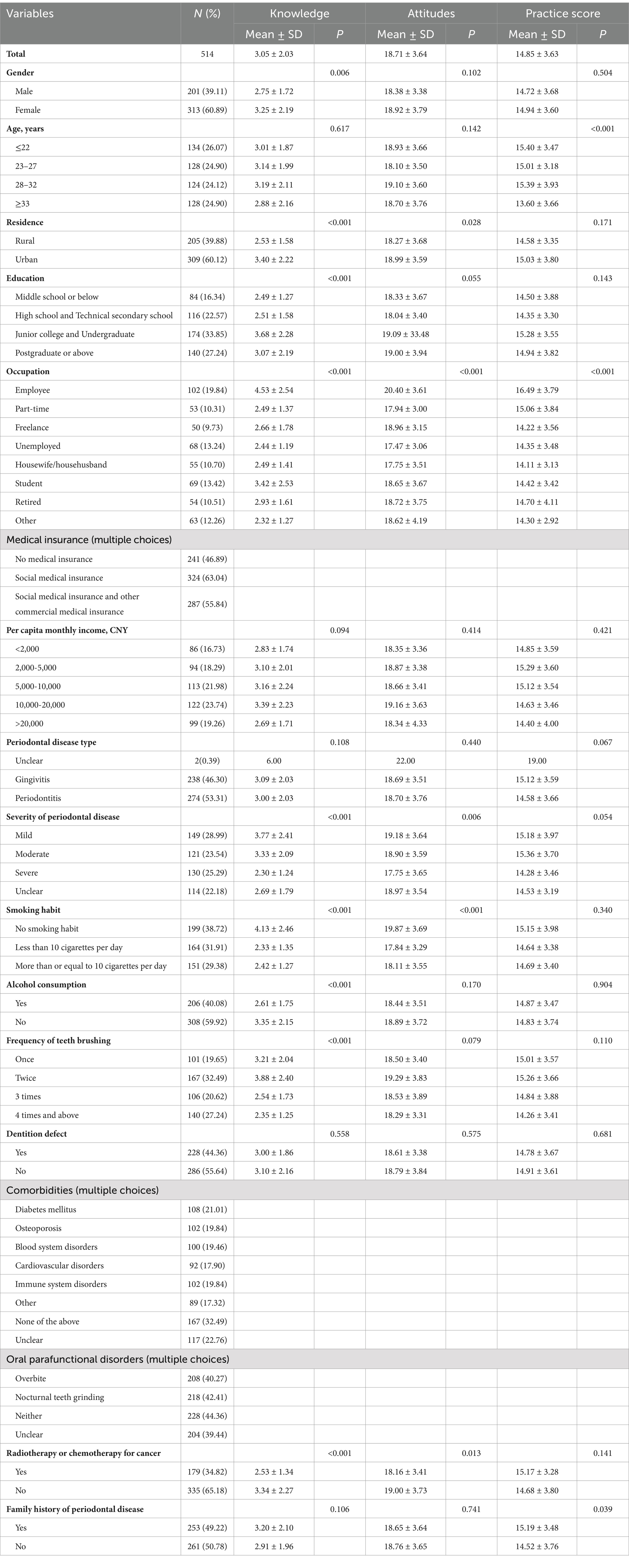
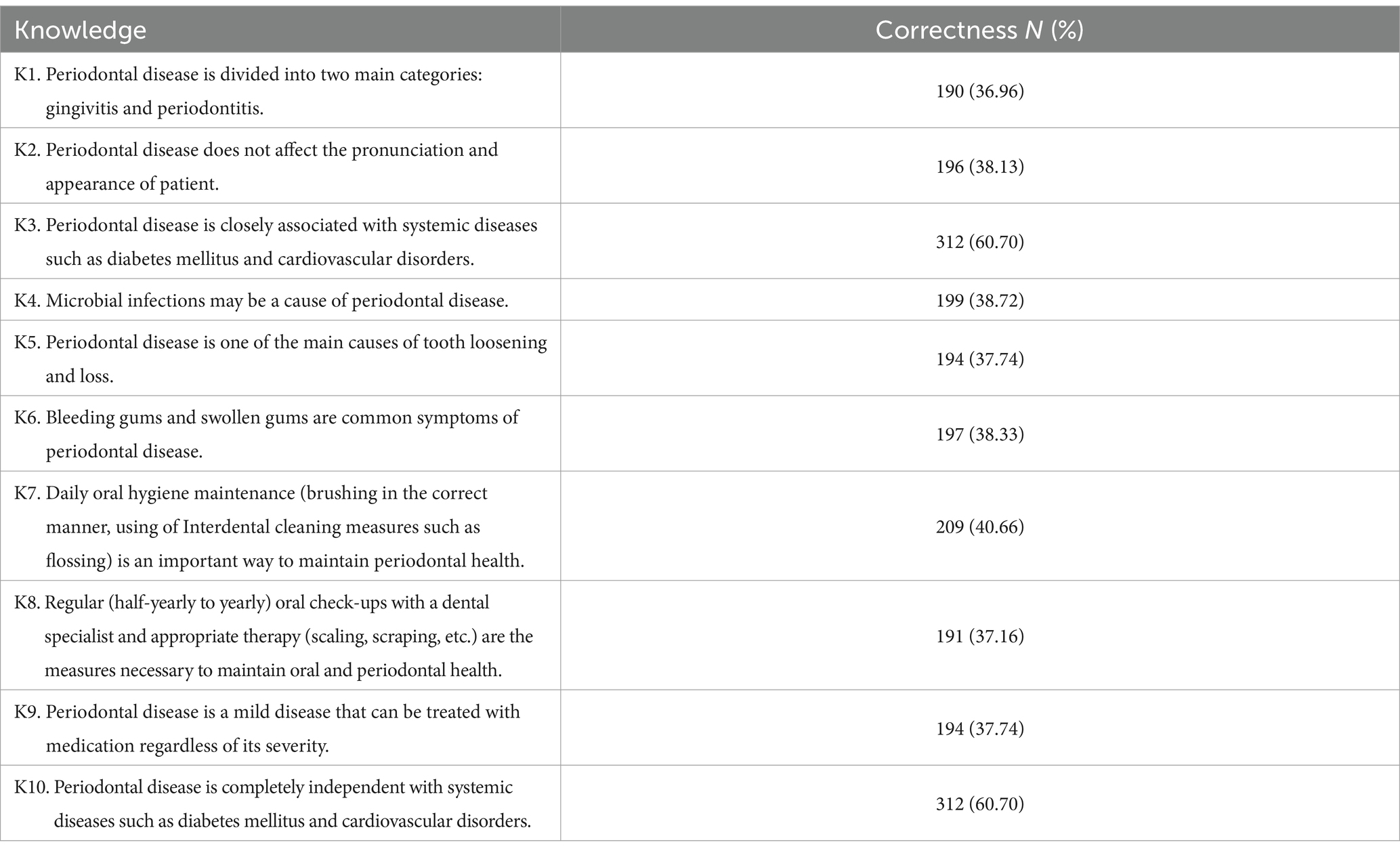
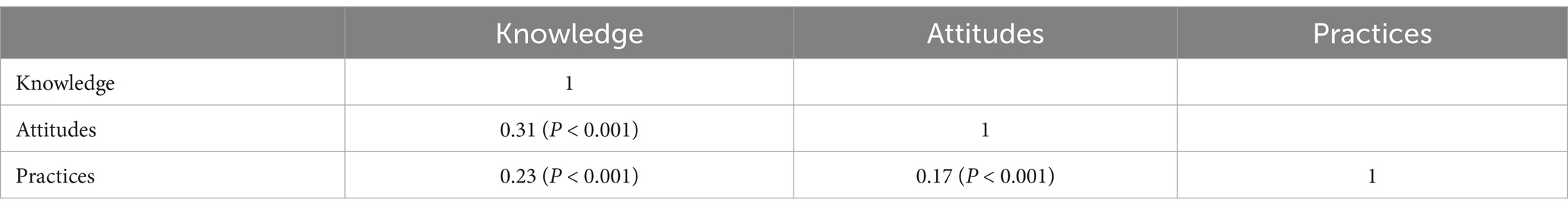
Results: A total of 514 questionnaires were collected. Among the patients, 313 (60.89%) of them were female, 309 (60.12%) resided in urban areas and 130 (25.29%) reported having severe periodontal disease. The mean scores of knowledge, attitudes and practices were 3.05 ± 2.03 (possible range: 0–8), 18.71 ± 3.64 (possible range: 6–30), and 14.85 ± 3.63 (possible range: 5–25), respectively. The knowledge item with highest correctness rate was the link between periodontal disease and systemic health (60.70%), while the lowest correctness rate was seen for understanding disease classification (36.96%). Pearson’s analysis revealed positive correlations between knowledge and attitude (r = 0.31, p < 0.001), knowledge and practices (r = 0.23, p < 0.001) attitudes, as well as attitudes and practices (r = 0.17, p < 0.001). Multivariate logistic regression analysis showed that knowledge (OR = 1.30, 95% CI: 1.14–1.49, p < 0.001), age ≥ 33 years old (OR = 0.33, 95% CI: 0.18–0.62, p = 0.001), housewife/househusband (OR = 0.41, 95% CI: 0.17–0.95, p = 0.037) and student (OR = 0.43, 95% CI: 0.20–0.92, p = 0.029) were independently associated with practices.
Conclusion: Patients with periodontal disease had insufficient knowledge, negative attitudes, and passive practices toward disease management. Further efforts could be directed toward enhancing patient education on periodontal disease to improve knowledge, thereby positively influencing attitudes and disease management practices.
Introduction
Periodontal disease, also known as gum disease, is a chronic inflammatory condition that affects the supporting structures of the teeth, including the gums, periodontal ligament, and alveolar bone (1). The impact of periodontal disease extends beyond individual oral health presenting significant implications for public health on a global scale (2). It’s high prevalence and associated health and economic burdens underscore the importance of effective prevention and treatment strategies (3, 4).
In China, a national survey revealed that periodontal disease among adults aged 55–74 was characterized by high prevalence rates of bleeding, probing depths ≥4 mm, and attachment loss >3 mm, underlining the need for targeted public health interventions (5). It is widely recognized that the progression of periodontal disease is influenced by multiple of factors, including microbial pathogens, immune response, tobacco use, and systemic illnesses. In conjunction with the aforementioned biopathological factors, inadequate oral hygiene is a particularly prominent risk element for the initiation of periodontitis. However, it is frequently underappreciated (6, 7). Several studies have demonstrated that periodontal disease patients’ knowledge and attitude toward disease management are potentially important factors affecting their oral health behavior. A cross-sectional study with a sample of 250 adult users of primary health care services in Brazil demonstrated that primary health care users with low oral health literacy exhibited more severe periodontal diseases (8). Similarly, a study on inequities in periodontal disease prevalence, prevention, and management concluded that the frequency of dental visits, oral hygiene, and risk behaviors of patients which impact an individual’s oral health status (9). However, comprehensive study encompassing these facets is conspicuously absent.
Knowledge, attitudes and practices (KAP) studies have been widely used in clinical research (10–12). This provides insights into the determinants that influence decisions and actions, rendering it valuable for crafting precise interventions. Moreover, it contributes to attaining a comprehensive comprehension of the intricate interplay among KAP. Globally, most prior KAP studies on periodontal disease have focused on healthcare professionals (13), pregnant women (14), or other population groups (15), primarily addressing diagnosis, treatment, or prevention, with few studies specifically examining KAP among patients with periodontal disease concerning self-management. Only one study conducted in China reported satisfactory levels of knowledge and attitudes but highlighted gaps in self-management practices related to dental plaque control among these patients (16). Therefore, this study aimed to investigate the KAP among patients with periodontal disease toward disease management.
Materials and methods
Study design and participants
This web-based cross-sectional study was conducted between March 2022 and March 2023 at the Department of Dentistry, Nanjing Drum Tower Hospital and the First Outpatient Department of Nanjing Stomatological Hospital among patients with periodontal disease. The inclusion criteria were as follows: (1) aged above 18 years, (2) willing to provide informed consent and participate voluntarily, (3) able to communicate effectively in the local language, and (4) a confirmed diagnosis of periodontal disease (gingivitis or periodontitis) from a qualified dentist. Participants with severe cognitive impairment or mental health conditions affecting communication and comprehension were excluded.
Questionnaire
The questionnaire was developed following the Consensus of Chinese stomatological multidisciplinary experts on maintaining periodontal health (First edition) and several related studies (17–19), and subjected to scrutiny by three senior dental specialists. A small-scale pre-test was conducted (n = 59), with a Cronbach’s α value of 0.751, indicating good internal reliability. The questionnaire included cutoffs for knowledge, attitudes, and practices, set at 4, 21, and 17, respectively. These cutoffs correspond to 70% of the total score for each dimension, a criterion chosen to represent sufficient knowledge, positive attitudes, and proactive practices. This threshold is widely used in KAP studies for clear and consistent classification.
The final questionnaire consisted of four dimensions: demographic characteristics, knowledge, attitudes and practices. The selection of demographic characteristics was primarily based on clinical experience, expert consultation, and findings from previous studies. For instance, we included basic demographic characteristics (e.g., gender, age, place of residence), as well as variables related to periodontal disease that are easily self-reported, such as disease type, severity, smoking and drinking habits, and brushing frequency. To enhance response accuracy and quality control, two “trap questions” (K3 and K10) were incorporated into the knowledge dimension. The concept of trap questions involves presenting conflicting statements on the same topic to detect inconsistencies in responses. In this study, K3 stated that “periodontal disease is closely associated with systemic diseases,” whereas K10 stated that it is “completely independent of systemic diseases.” If respondents provided the same response to both questions, the questionnaire was considered logically inconsistent and excluded from analysis. Thus, the knowledge dimension consists of 10 questions, with 1 point for the correct answer and 0 points for the rest, resulting in a total score range of 0–8 after excluding trap questions. The attitude section consists of 6 questions, using a 5-point Likert scale, with each question being assigned a score of 1 point to 5 points for the options from very positive to very negative, with a possible range of 6–30 points. The practice section consists of 5 questions, also using a 5-point Likert scale, with each question being assigned a score of 1 point to 5 points from the highest to the lowest frequency of the practice, with a possible range of 5–25 points.
The data were collected using an online questionnaire hosted on Sojump platform1. The online questionnaire was distributed through WeChat, Internet forums, and web links. All data were collected anonymously. To prevent duplication, an IP restriction was implemented, ensuring that each survey could only be completed once per unique IP address.
Statistical analysis
STATA 17.0 (Stata Corporation, College Station, TX, United States) was used for statistical analysis. The continuous variables were expressed as mean ± SD, and the categorical variables were expressed as n (%). The continuous variables that conformed to a normal distribution were tested by the t-test or ANOVA. Pearson correlation was used to analyze the correlation between knowledge, attitudes, and practices. For multivariate analysis, the cutoff scores for knowledge, attitudes, and practices were established as 4, 21, and 17, respectively, based on 70% of the maximum possible score for each section. This method was selected to ensure that the classification accurately reflects sufficient levels in each category, as used in previous KAP research (20). Scores surpassing this threshold were categorized as indicative of sufficient knowledge, positive attitudes, and proactive practices. As a result, the designated cutoffs for knowledge, attitudes, and practices were set at 4, 21, and 17, respectively. Scores surpassing this threshold were categorized as indicative of sufficient knowledge, positive attitudes, and proactive practices. Two-sided p < 0.05 was considered statistically significant in this study.
Results
A total of 514 questionnaires were collected. Among the patients, 313 (60.89%) were female, 309 (60.12%) resided in urban and 130 (25.29%) reported having severe periodontal disease. The mean score of knowledge, attitudes and practices were 3.05 ± 2.03 (possible range: 0–8), 18.71 ± 3.64 (possible range: 6–30), and 14.85 ± 3.63 (possible range: 6–30), respectively (Table 1).
The three knowledge items with the highest correctness rates were as follows: “Periodontal disease is closely associated with systemic diseases such as diabetes mellitus and cardiovascular disorders” (K3) with a correctness rate of 60.70%, and “Daily oral hygiene maintenance is an important way to maintain periodontal health” (K7), with a correctness rate of 40.66%. On the other hand, the three items with the lowest correctness rates were “Periodontal disease is divided into two main categories: gingivitis and periodontitis” (K1) with a correctness rate of 36.96%, “Regular oral check-ups with a dental specialist and appropriate therapy are necessary to maintain oral and periodontal health” (K8) with a correctness rate of 37.16%, and “Periodontal disease is a mild disease that can be treated with medication regardless of its severity” (K9) with a correctness rate of 37.74% (Table 2).
In this study, 46.11% of the participants strongly agreed/agreed that paying close attention to bleeding and painful gums is important in their daily lives (A2). Similarly, 43.78% strongly agreed/agreed that following doctor’s instructions and regular follow-up appointments was essential for achieving a good therapeutic effect (A6). Moreover, a considerable portion (12.65%) of patients indicated a preference for self-managed measures over seeking medical help (A5) (Table 3).
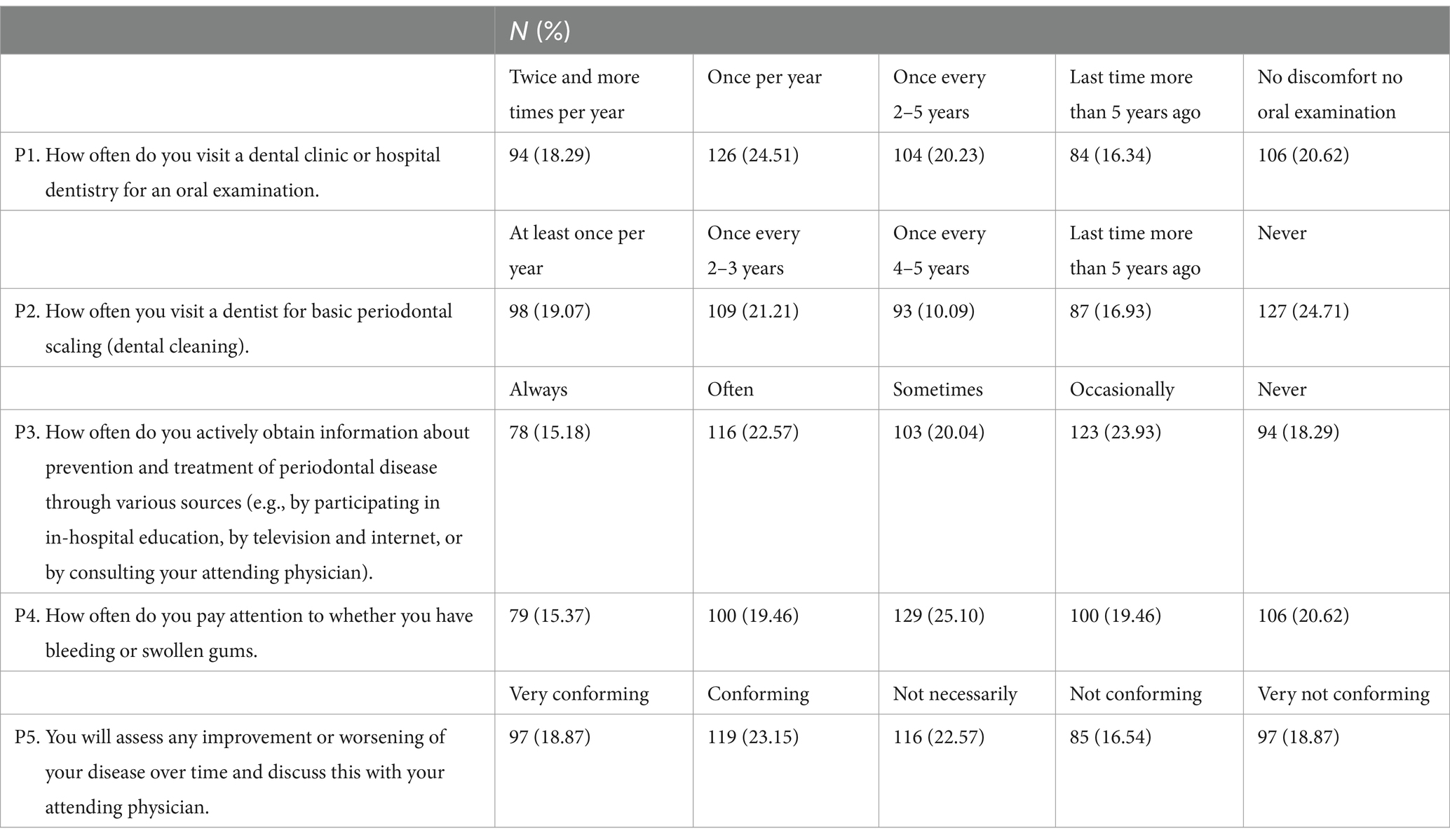
Regarding practices, 18.29% of patients indicated undergoing annual visits to dental clinics or hospital dentistry for oral examinations, while 24.51% exhibited a more rigorous approach with biannual or more frequent visits (P1). Concerning basic periodontal scaling, 21.21% of respondents frequently sought dental intervention, 19.07% adhered to at least an annual schedule, while 16.93% extended their visit gap beyond 5 years (P2). Additionally, a notable trend encompassed the acquisition of knowledge on periodontal disease prevention and treatment, with 22.57% frequently seeking such information and 15.18% consistently engaging in this pursuit (P3). Notably, 25.10% of patients intermittently prioritized the observation of bleeding or swollen gums as a pivotal facet of their oral care regimen (P4) (Table 4).
Pearson’s analysis showed that knowledge and attitudes (r = 0.312, p < 0.001) were positively correlated as well as knowledge and practices (r = 0.230, p < 0.001). Additionally, there was a positive correlation between attitudes and practices (r = 0.171, p < 0.001) (Table 5).
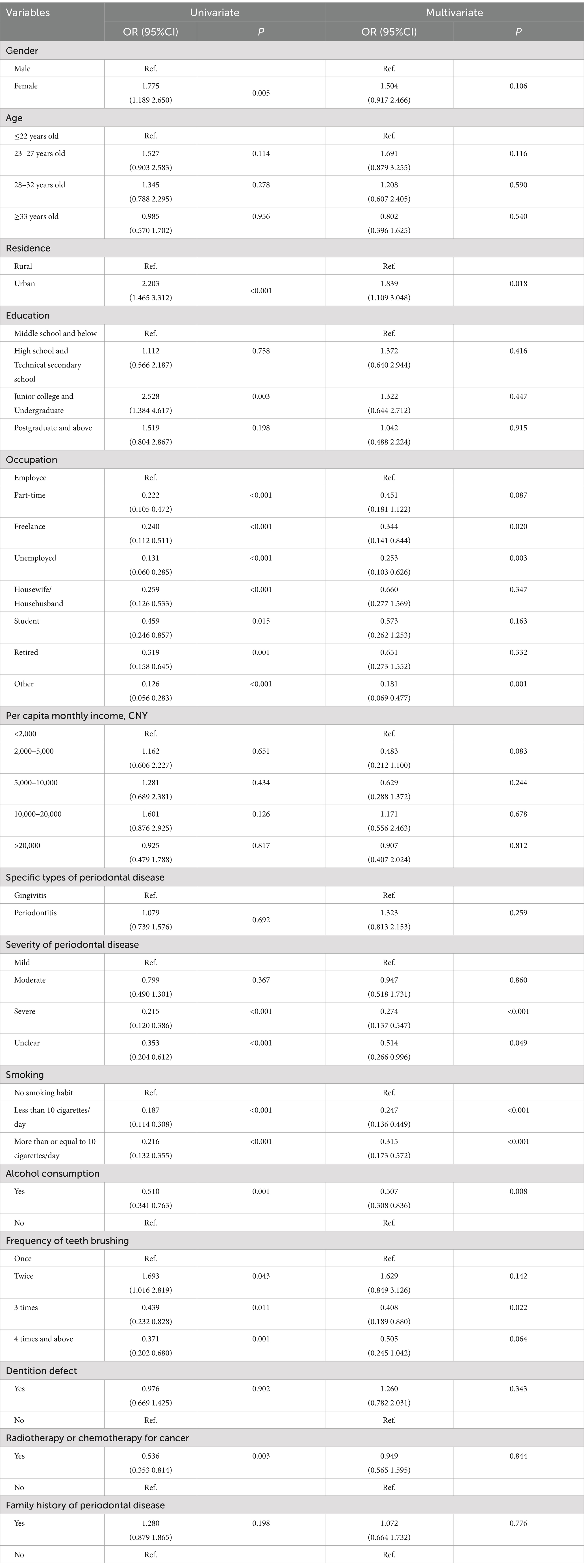
The multivariate logistic regression analysis showed that urban residence (OR = 1.84, 95% CI: 1.11–3.05, p = 0.018), freelance employment (OR = 0.34, 95% CI: 0.14–0.84, p = 0.020), unemployed (OR = 0.25, 95% CI: 0.10–0.63, p = 0.003), severe periodontal disease (OR = 0.27, 95% CI: 0.14–0.55, p < 0.001) and smoking <10 cigarettes per day (OR = 0.25, 95% CI: 0.14–0.45, p < 0.001), smoking ≥10 cigarettes per day (OR = 0.32, 95% CI: 0.17–0.57, p < 0.001), alcohol consumption (OR = 0.51, 95% CI: 0.31–0.84, p = 0.008), brushing teeth 3 times a day (OR = 0.41, 95% CI: 0.19–0.89, p = 0.022) were independently associated with knowledge (Table 6).
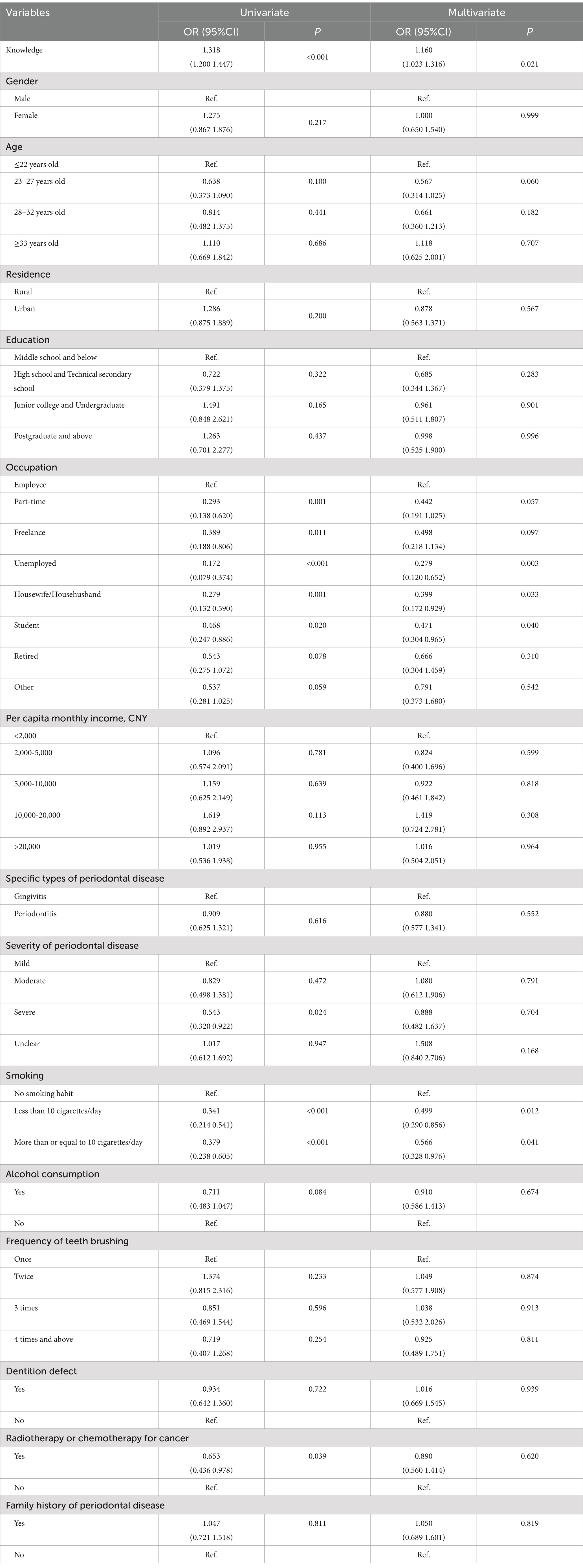
Knowledge (OR = 1.16, 95% CI: 1.02–1.32, p = 0.021), unemployed (OR = 0.28, 95% CI: 0.12–0.65, p = 0.003), housewife/househusband (OR = 0.40, 95% CI: 0.17–0.93, p = 0.033), student (OR = 0.47, 95% CI: 0.30–0.97, p = 0.040) and smoking <10 cigarettes per day (OR = 0.50, 95% CI: 0.29–0.86, p = 0.012) and smoking ≥10 cigarettes per day (OR = 0.57, 95% CI: 0.33–0.98, p = 0.041) were independently associated with attitudes (Table 7).
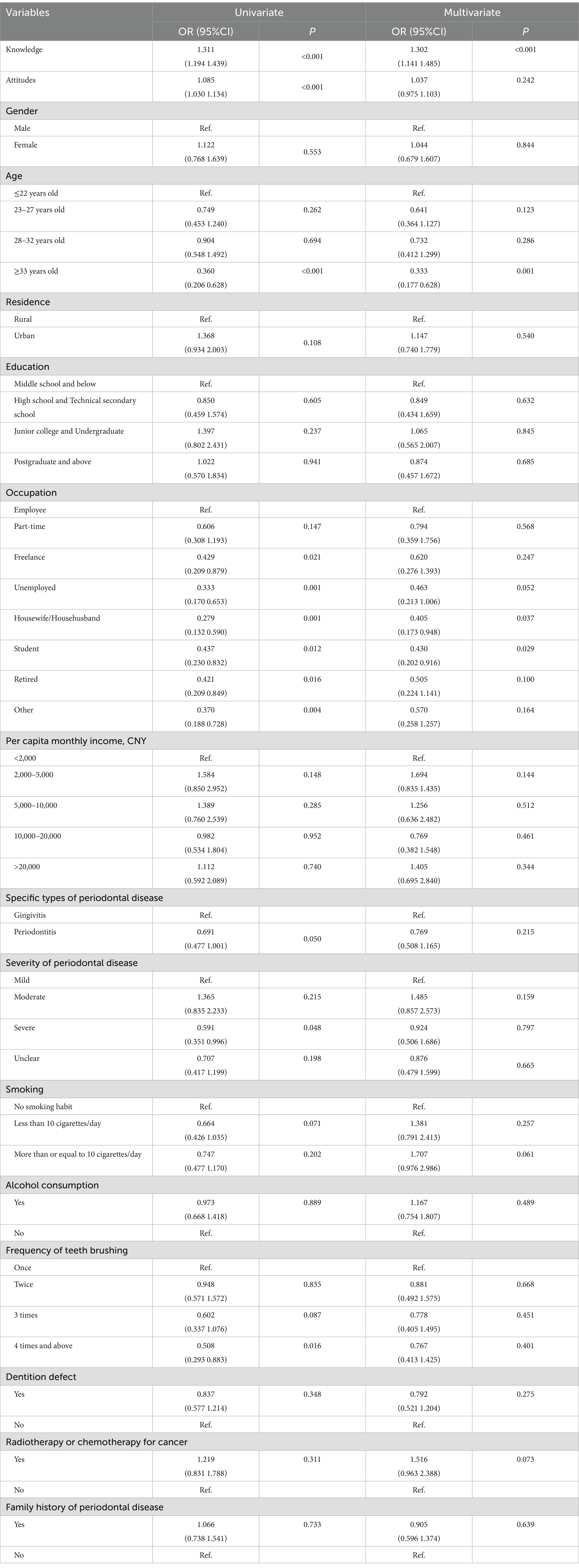
Knowledge (OR = 1.30, 95% CI: 1.14–1.49, p < 0.001), aged ≥33 years old (OR = 0.33, 95% CI: 0.18–0.62, p = 0.001), housewife/househusband (OR = 0.41, 95% CI: 0.17–0.95, p = 0.037) and student (OR = 0.43, 95% CI: 0.20–0.92, p = 0.029) were independently associated with practices (Table 8).
Discussion
In this study, patients with periodontal disease demonstrated insufficient knowledge, negative attitudes, and passive practices. Suggested recommendations to improve clinical practice include in-hospital training, tailored communication, targeted interventions for specific groups, smoking cessation counseling, and public health campaigns.
The participants demonstrated relatively good understanding of the association between periodontal disease and systemic conditions such as diabetes mellitus and cardiovascular disorders. However, this study identified conspicuous gaps in understanding regarding the consequences of periodontal disease on speech articulation and facial appearance, along with the effectiveness of medical interventions, regardless of the severity of the disease. Beyond their role in the masticatory process, teeth substantially contribute to the articulation of sounds, aesthetic presentation, and the growth of the craniofacial complex (21). A targeted educational approach that addresses these relatively underexplored dimensions has the potential to enhance overall levels of awareness, thus fostering improved outcomes within the domain of oral health (22). Moreover, demographic differences in KAP outcomes were observed, with higher education levels and urban residents showing better knowledge and more proactive practices. Additionally, female patients generally demonstrated higher knowledge scores compared to males, aligning with previous findings that gender differences may influence health-related knowledge acquisition (23). These differences highlight the need for tailored educational interventions that consider socioeconomic and demographic characteristics.
While a significant portion of the patients exhibited an inclination toward highlighting the significance of adhering to medical directives and participating in scheduled post-treatment sessions, certain misconceptions endured among a subset of participants who regarded periodontal disease with reduced gravity. Dispelling these misconceptions and educating patients about the potential consequences of untreated periodontal disease can foster more informed and proactive attitudes toward oral health (24). To address the misconceptions about the severity of periodontal disease, a more nuanced educational strategy is needed. This could involve tailored communication campaigns that emphasize the potential long-term consequences of untreated periodontal disease, such as bone loss, systemic health risks, and impacts on overall well-being. In addition, implementing in-hospital training modules that use real-life cases, visual aids, and interactive workshops could help bridge these knowledge gaps. Providing targeted education to high-risk groups, integrating oral health information into community outreach programs, and utilizing digital tools like mobile health apps may also prove effective in enhancing awareness and promoting timely treatment (25, 26). Dental practitioners ought to actively participate in patient-centered dialogs, aimed at dispelling misconceptions and underscoring the gravity of periodontal ailment. Motivating patients to adhere to dentists’ directives and to consistently attend scheduled follow-up consultations holds the potential to bolster constructive dispositions regarding both preventive measures and therapeutic interventions (27, 28).
Regarding practices, although the majority of participants reported adhering to routine dental visits, a substantial proportion acknowledged never having undergone fundamental periodontal scaling procedures. Additionally, differences were observed in the inclination to seek information concerning periodontal disease, and discrepancies emerged in the frequency of self-monitoring practices in this study. Encouragement of regular dental check-ups and consistent self-monitoring regimens can significantly aid in the early identification of periodontal anomalies and the cultivation of proactive oral health behaviors (29, 30). Dental practitioners assume a pivotal role in educating patients about effective self-monitoring strategies for gum health, encompassing regular assessments for indicators such as gum bleeding or inflammation (31, 32). This emphasis on self-awareness and prompt identification of oral health issues empowers patients to adopt a proactive stance toward their oral care, thereby contributing to enhanced oral health outcomes and holistic well-being.
It is imperative to acknowledge the variability in dental attendance frequency exhibited among the participants, wherein a notable proportion reported having their last visit more than 5 years ago. To enhance the rates of dental attendance, the implementation of diverse strategies emerges as a pivotal consideration. Reminiscent of effective tactics encompassing reminder systems, outreach initiatives, and community-oriented oral health endeavors, these approaches can play a pivotal role in bolstering early detection and intervention for cases of periodontal disease (33–35).
This study had limitations. Primarily, it was conducted at a single center and followed an observational approach. Moreover, it is crucial to acknowledge that the utilization of self-reported data concerning attitudes and practices might render it susceptible to diverse biases, encompassing the likes of social desirability bias or recall bias (36). These biases could potentially lead to overreporting of positive behaviors or underreporting of negative ones, thus affecting the accuracy of the findings. Additionally, the study did not account for all possible factors that might influence KAP, which may limit the depth of the analysis. This limitation has been acknowledged as it is impossible to collect all relevant variables. Future research could mitigate these biases by incorporating objective measures, such as clinical assessments or validated behavior tracking tools, to complement self-reported data. This study presents noteworthy strengths and holds significant clinical implications. In a clinical context, understanding the knowledge gaps, attitudes, and practices of patients with periodontal disease has direct relevance for healthcare practitioners.
Conclusion
In conclusion, patients with periodontal disease showed insufficient knowledge, negative attitudes, and passive practices toward disease management. Based on the results, clinical practice can be improved by implementing in-hospital training programs to educate patients on periodontal disease prevention and treatment. Targeted interventions should focus on improving practices among specific groups, and smoking cessation counseling should be integrated into patient care protocols.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was approved by the Medical Ethics Committee of Gulou Hospital Affiliated to Nanjing University School of Medicine (2024–386-01). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
SZ: Writing – original draft. YW: Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
KAP, Knowledge, attitudes and practices.
Footnotes
References
1. Tobita, M, Masubuchi, Y, Ogata, Y, Mitani, A, Kikuchi, T, Toriumi, T, et al. Study protocol for periodontal tissue regeneration with a mixture of autologous adipose-derived stem cells and platelet rich plasma: a Multicenter, randomized, open-label clinical trial. Regen Ther. (2022) 21:436–41. doi: 10.1016/j.reth.2022.09.008
2. Wei, Y, Wang, Z, Lei, L, and Chen, L. Global burden of periodontal disease and its relation with socioeconomic development during 1990-2019. Zhejiang Da Xue Xue Bao Yi Xue Ban. (2021) 50:545–52. doi: 10.3724/zdxbyxb-2021-0321
3. Gholami, L, Ghafouri-Fard, S, Mirzajani, S, Arsang-Jang, S, Taheri, M, Dehbani, Z, et al. The Lncrna Anril is Down-regulated in peripheral blood of patients with periodontitis. Noncoding RNA Res. (2020) 5:60–6. doi: 10.1016/j.ncrna.2020.04.001
4. Tan, OL, Safii, SH, and Razali, M. Clinical efficacy of single application local drug delivery and adjunctive agents in non-surgical periodontal therapy: a systematic review and network meta-analysis. Pharmaceutics. (2020) 12:86. doi: 10.3390/pharmaceutics12111086
5. Sun, H, Du, M, Tai, B, Chang, S, Wang, Y, and Jiang, H. Prevalence and associated factors of periodontal conditions among 55- to 74-year-old adults in China: results from the 4th National Oral Health Survey. Clin Oral Investig. (2020) 24:4403–12. doi: 10.1007/s00784-020-03306-4
6. Alshawwa, H, Wang, J-F, Liu, M, and Sun, S-F. Successful Management of a Tooth with endodontic-periodontal lesion: a case report. World J Clin Cases. (2020) 8:5049–56. doi: 10.12998/wjcc.v8.i20.5049
7. Chen, X, Arias, Z, Omori, K, Yamamoto, T, Shinoda-Ito, Y, and Takashiba, S. Autophagy as a potential mechanism underlying the biological effect of 1,25-Dihydroxyvitamin D3 on periodontitis: a narrative review. BMC Oral Health. (2023) 23:90. doi: 10.1186/s12903-023-02802-9
8. Bado, FMR, Barbosa, TS, Soares, GH, and Mialhe, FL. Oral health literacy and periodontal disease in primary health care users. Int Dent J. (2022) 72:654–8. doi: 10.1016/j.identj.2021.12.004
9. Mills, A, and Levin, L. Inequities in periodontal disease prevalence, PreventioN, and management. Quintessence Int. (2022) 53:122–32. doi: 10.3290/j.qi.b1763677
10. Koni, A, Taha, S, Daifallah, A, Koni, M, Abutaha, S, Sabateen, A, et al. A cross-sectional evaluation of knowledge, attitudes, practices, and perceived challenges among Palestinian pharmacists regarding COVID-19. SAGE Open Med. (2022) 10:20503121211069278. doi: 10.1177/20503121211069278
11. Nascimento, LGP, da Silva, AMC, Stedefeldt, E, and da Cunha, DT. Job crafting and burnout as predictors of food safety Behaviors in the foodservice industry. Food Secur. (2022) 11:2671. doi: 10.3390/foods11172671
12. Rakotosamimanana, S, Rakotoarimanana, FJ, Raharimanga, V, Taglioni, F, Ramamonjisoa, J, Randremanana, RV, et al. Influence of Sociospatial determinants on knowledge, attitudes and practices related to the plague in a population living in endemic areas in the central highlands, Madagascar. BMC Public Health. (2021) 21:1102. doi: 10.1186/s12889-021-11101-3
13. Mohamed, AM, Ahmed, F, Gondi, KM, Salem, KA, Mohammed, OB, and Peeran, SW. Knowledge, attitude, and practice of teledentistry in periodontal diagnosis among dental interns at a College in Sebha, Libya: a cross-sectional questionnaire study. Cureus. (2024) 16:e58330. doi: 10.7759/cureus.58330
14. Javali, MA, Saquib, SA, Abdul Khader, M, Khalid, I, AlShahrani, AY, Kanji, MA, et al. Oral health knowledge, attitude, and practice of pregnant women in Deccan, South India: a cross-sectional prenatal survey. J Med Life. (2022) 15:420–4. doi: 10.25122/jml-2019-0095
15. Kedlaya, MN, Puzhankara, L, Mahendra, M, K, V, Sinha, SP, Singh, A, et al. Development and validation of a structured questionnaire to assess the knowledge, attitude and practice (Kap) regarding the effect of yoga on periodontal health among Indian adults. F1000Res. (2024) 12:1404. doi: 10.12688/f1000research.140245.2
16. Sun, J, Tong, D, Sun, C, Wang, X, Zuo, Z, Liu, Y, et al. Knowledge, attitude, and practice toward self-control of dental plaque among patients with periodontal diseases: a cross-sectional study. BMC Oral Health. (2023) 23:628. doi: 10.1186/s12903-023-03352-w
17. Xiao, L, Karapen, K, Dong, S, Yang, H, and Zhang, X. Epidemiology of periodontal disease in adolescents in mainland China, 1983-2020: a systematic review and meta-analysis. Ann Palliat Med. (2021) 10:45–60. doi: 10.21037/apm-20-1919
18. Han, P, Tang, J, Wang, X, Su, Y, Li, G, and Deng, K. Research on the distribution Spectrum of atherosclerotic plaques in patients with suspected coronary artery disease and the non-invasive screening model for coronary atherosclerosis burden. Quant Imaging Med Surg. (2021) 11:3274–85. doi: 10.21037/qims-20-901
19. Chinese Stomatological A. Consensus of Chinese Stomatological multidisciplinary experts on maintaining periodontal health (first edition). Zhonghua Kou Qiang Yi Xue Za Zhi. (2021) 56:127–35. doi: 10.3760/cma.j.cn112144-20210112-00013
20. Lee, F, and Suryohusodo, AA. Knowledge, attitude, and practice assessment toward Covid-19 among communities in East Nusa Tenggara, Indonesia: a cross-sectional study. Front Public Health. (2022) 10:957630. doi: 10.3389/fpubh.2022.957630
21. Garot, E, Couture-Veschambre, C, Manton, D, Beauval, C, and Rouas, P. Analytical evidence of enamel hypomineralisation on permanent and primary molars amongst past populations. Sci Rep. (2017) 7:1712. doi: 10.1038/s41598-017-01745-w
22. Sanaeinasab, H, Saffari, M, Taghavi, H, Karimi Zarchi, A, Rahmati, F, Al Zaben, F, et al. An educational intervention using the health belief model for improvement of oral health behavior in grade-schoolers: a randomized controlled trial. BMC Oral Health. (2022) 22:94. doi: 10.1186/s12903-022-02132-2
23. Gil, M, Rudy, M, Stanisławczyk, R, Duma-Kocan, P, and Żurek, J. Gender differences in eating habits of polish young adults aged 20-26. Int J Environ Res Public Health. (2022) 19:5280. doi: 10.3390/ijerph192215280
24. Khan, A, and Shaikh, BT. An all time low utilization of intrauterine contraceptive device as a birth spacing method--a qualitative descriptive study in district Rawalpindi, Pakistan. Reprod Health. (2013) 10:10. doi: 10.1186/1742-4755-10-10
25. Jaraszek, M, Hanke, W, and Marcinkiewicz, A. Nutritional education and the state of Oral health in adolescents. Int J Environ Res Public Health. (2022) 19:8686. doi: 10.3390/ijerph19148686
26. Naidu, RS, and Nunn, JH. Oral health knowledge, attitudes and behaviour of parents and caregivers of preschool children: implications for Oral health promotion. Oral Health Prev Dent. (2020) 18:245–52. doi: 10.3290/j.ohpd.a43357
27. Inglehart, MR, Albino, J, Feine, JS, and Okunseri, C. Sociodemographic changes and Oral health inequities: dental workforce considerations. JDR Clin Trans Res. (2022) 7:5S–15S. doi: 10.1177/23800844221116832
28. Wu, B, Mao, W, Qi, X, and Pei, Y. Immigration and Oral health in older adults: an integrative approach. J Dent Res. (2021) 100:686–92. doi: 10.1177/0022034521990649
29. Mohd-Said, S, Mohd-Norwir, NA, Ariffin, AN, Teo, HS, Nik-Azis, NM, Rani, H, et al. Validation of a simplified digital periodontal health screening module for general dental practitioners. Healthcare. (2022) 10:1916. doi: 10.3390/healthcare10101916
30. Ziaei, N, Hosseinpour, S, Nazari, H, Rezaei, M, and Rezaei, K. Halitosis and its associated factors among Kermanshah high school students (2015). Clin Cosmet Investig Dent. (2019) 11:327–38. doi: 10.2147/CCIDE.S215869
31. Won, J, Huang, P-C, Spillman, DR, Chaney, EJ, Adam, R, Klukowska, M, et al. Handheld optical coherence tomography for clinical assessment of dental plaque and gingiva. J Biomed Opt. (2020) 25:6011. doi: 10.1117/1.JBO.25.11.116011
32. Yang, B, Pang, X, Guan, J, Liu, X, Li, X, Wang, Y, et al. The Association of Periodontal Diseases and Sjogren's syndrome: a systematic review and meta-analysis. Front Med. (2022) 9:904638. doi: 10.3389/fmed.2022.904638
33. Alhazmi, SA, Maashi, AQ, Shabaan, SK, Majrashi, AA, Thakir, MA, Almetahr, SM, et al. The health belief model modifying factors associated with missed clinic appointments among individuals with sickle cell disease in the Jazan Province, Saudi Arabia. Healthcare. (2022) 10:2376. doi: 10.3390/healthcare10122376
34. Lee, Y-L, Hu, H-Y, Yen, Y-F, Chu, D, Yang, N-P, Chou, S-Y, et al. Impact of the Covid-19 pandemic on the utilization of medical and dental Services in Taiwan: a cohort study. J Dent Sci. (2021) 16:1233–40. doi: 10.1016/j.jds.2021.02.001
35. Liu, X, Du, C, Hu, F, Zhao, Y, Zhou, J, Wang, Q, et al. Management of Acute Exacerbation of chronic obstructive pulmonary disease under a tiered medical system in China. Ther Adv Respir Dis. (2022) 16:17534666221075499. doi: 10.1177/17534666221075499
Keywords: knowledge, attitudes, practices, cross-sectional study, oral health, periodontal disease
Citation: Zhao S and Wu Y (2024) Knowledge, attitudes and practices among patients with periodontal disease toward disease management. Front. Public Health. 12:1500586. doi: 10.3389/fpubh.2024.1500586
Edited by:
Dalia Almaghaslah, King Khalid University, Saudi ArabiaReviewed by:
Arwa Khaled, King Khalid University, Saudi ArabiaGeetha Kandasamy, King Khalid University, Saudi Arabia
Copyright © 2024 Zhao and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanyun Wu, bWFyaW5hX3d5eUBob3RtYWlsLmNvbQ==
 Siyu Zhao
Siyu Zhao Yanyun Wu
Yanyun Wu