- 1Department of Practice, Sciences and Health Outcomes Research, University of Maryland Baltimore School of Pharmacy, Baltimore, MD, United States
- 2Peter Lamy Center on Drug Therapy and Aging, University of Maryland Baltimore, School of Pharmacy, Baltimore, MD, United States
- 3Pharmacy Quality Alliance, Alexandria, VA, United States
- 4College of Pharmacy, University of Michigan, Ann Arbor, MI, United States
- 5College of Pharmacy, Purdue University, Indianapolis, IN, United States
- 6College of Public Affairs, University of Baltimore, Baltimore, MD, United States
- 7Henry A. Rosenberg Professor of Government, Business, and Nonprofit Partnerships, University of Baltimore, Baltimore, MD, United States
Medication therapy problems (MTPs) are common among older adults and are associated with considerable morbidity, mortality, and healthcare costs. The Medicare Part D Medication Therapy Management (MTM) program, which includes Comprehensive Medication Reviews (CMRs), Targeted Medication Reviews (TMRs), and guidance on safe medication disposal, is designed to optimize therapeutic outcomes and reduce adverse events by addressing MTPs. Although this program has demonstrated success in reducing MTPs, its utilization remains low, with ongoing concerns about service access disparities, patient satisfaction, and long-term health outcomes. This perspective paper applies the Andersen Behavioral Model (ABM) to the Medicare Part D MTM program to enhance understanding of factors influencing service utilization and impact among older adults. The ABM provides a structured framework to examine how macro-and micro-level factors shape health behaviors and outcomes. By applying ABM framework to MTM, this paper highlights essential research directions to generate rigorous evidence for program evaluation, inform policy adjustments, and make targeted recommendations for improving MTM within the U.S. healthcare system. Furthermore, this work has potential implications for global programs aimed at enhancing medication safety by addressing MTPs and optimizing medication use.
1 Introduction
Medication therapy problems (MTPs) are prevalent among older adults (≥65 years), including issues related to appropriateness (e.g., unwarranted polypharmacy), effectiveness (e.g., subtherapeutic regimens), safety (e.g., adverse drug events, drug–drug interactions, and supratherapeutic doses), access, and adherence (1, 2). Factors such as age-related physiological changes, increased frailty, multiple coexisting conditions, and gaps in care across settings and providers for patients having complex medical conditions, significantly elevate the risk of adverse events in this vulnerable population (3, 4). Preventable adverse drug events contribute to substantial morbidity and mortality, often resulting in avoidable emergency department visits, hospitalizations, diminished quality of life, and unnecessary healthcare expenditures (5–9). Consequently, prioritizing medication safety initiatives for older adults is imperative and historical work can inform future global efforts to address preventable medication related harm (10–12).
In the United States (US), the Medicare Part D medication therapy management (MTM) program represents a strategic approach aimed at optimizing therapeutic outcomes and reducing the risk of adverse events and associated costs by identifying and addressing MTPs (13). This program was established under the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (Public Law 108–173) to benefit eligible beneficiaries, determined by their number of medications, chronic diseases, and Part D drug expenditures (14). Medicare Parts A and B comprise a federal fee-for-service health insurance program for individuals aged 65 or older and younger adults with disabilities (15, 16), while Part D specifically covers outpatient prescription drugs and related services for Medicare beneficiaries (16).
The Medicare Part D MTM program, overseen by the Centers for Medicare & Medicaid Services (CMS), targets high-risk populations vulnerable to MTPs (13, 17). Part D plan sponsors are required to offer MTM services to eligible beneficiaries namely an annual Comprehensive Medication Review (CMR), quarterly Targeted Medication Reviews (TMRs), and guidance on safe prescription medications disposal (17, 18). MTM programs have been shown to significantly reduce MTPs while improving clinical, economic, and humanistic outcomes (19–24). Over nearly two decades, the Part D MTM program has undergone continuous revisions to enhance service delivery, improve quality, and address gaps in care (13, 25). While studies show some success in reducing MTPs, healthcare utilization, and costs compared to standard care (26–28), challenges persist regarding overall service utilization, disparities in access, patient satisfaction, and the long-term effects on health and well-being (29–32).
To better inform research and policy aimed at enhancing MTM service utilization and effectiveness, it is essential to gain a deeper understanding of factors associated with utilization of MTM services and the impact of these services (33). In this perspective paper, we utilize the Andersen Behavioral Model (ABM) to examine the Medicare Part D MTM program, focusing on opportunities to improve our understanding of service utilization and its implications on medication safety for older adults (34).
2 Andersen behavioral model (ABM) applied to Medicare Part D MTM program
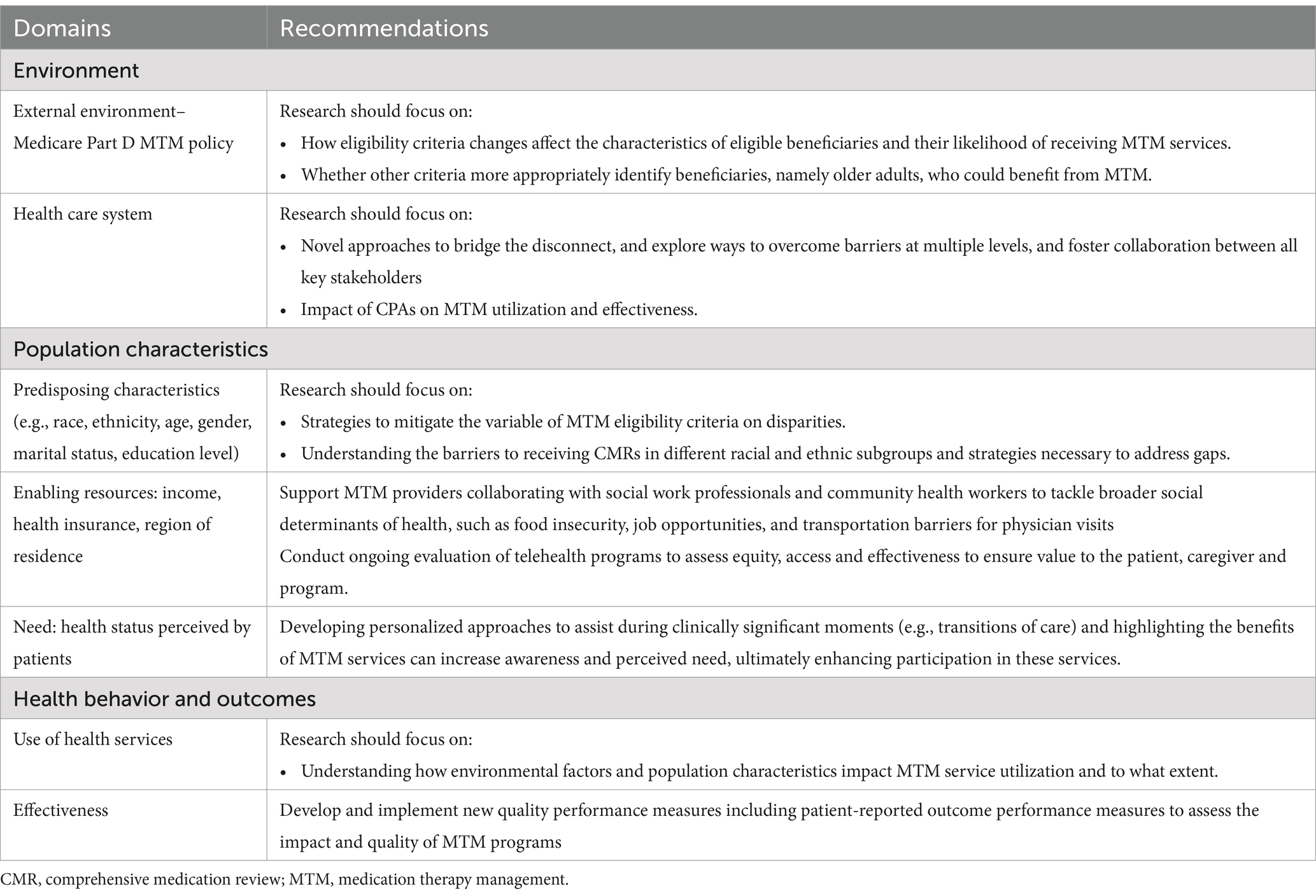
The ABM provides a structured framework for understanding how various factors influence health behaviors and outcomes (33, 34). Within the ABM, these factors are categorized into two primary domains—environmental factors and population characteristics—which further divided into five sections: external environment, healthcare system, predisposing characteristics, enabling factors, and need factors (34, 35).
By considering both environmental and individual-or patient-level (“population”) determinants of health behaviors, the ABM provides a valuable approach for assessing both macro-and micro-level influences on program participation (34). The following sections describe key elements of the ABM when applied to the Medicare Part D MTM program (see Figure 1). Additionally, Table 1 provides recommendations for a multifaceted approach to improve medication safety in older adults.
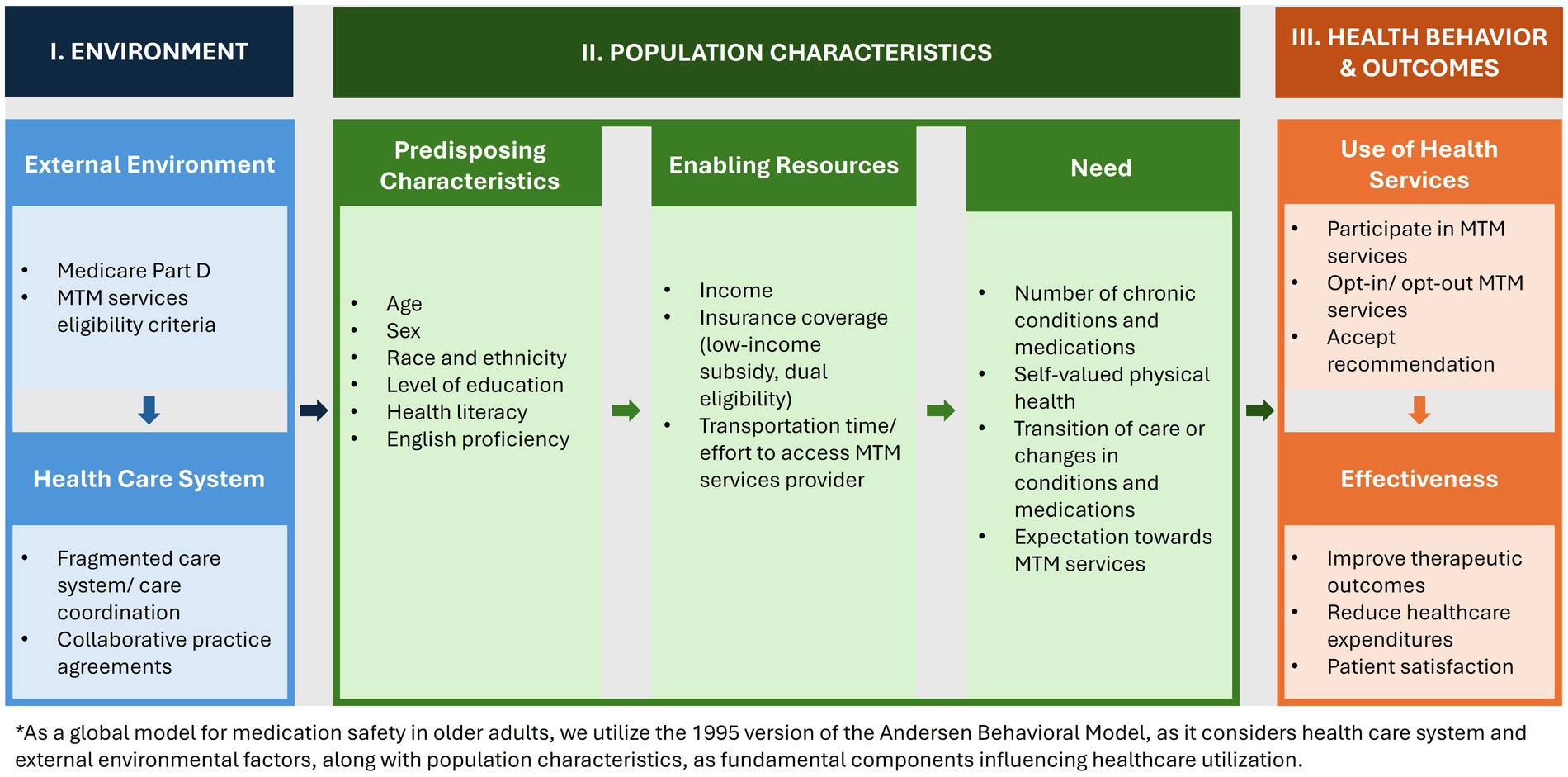
Figure 1. Illustration of Andersen behavioral model applied to medication therapy management (34).
2.1 Environment
2.1.1 External environment– Medicare Part D MTM policy
Although a later addition to the initial ABM, the external environment was recognized as having an important impact on health services utilization (34). Environmental factors include physical (health organizations), political (health policy), and economic (healthcare resources) components (33, 34). Particularly in the context of the Part D MTM, health policy changes have led to differential impacts on utilization of MTM services.
Specifically, CMS sets MTM program eligibility criteria using minimum and maximum thresholds per patient for number of medications and number of chronic diseases, along with a minimum annual Part D drug costs threshold to qualify for services (36). Moreover, Part D plan sponsors have historically been allowed to specify additional targeting criteria which has led to fewer eligible beneficiaries (36–38). This eligibility and targeting criteria have changed consistently throughout the history of the program, impacting who has the opportunity to receive these medication management services (36, 37).
In 2012, enrollment of beneficiaries into the MTM program by plan sponsor ranged from less than 0.2 percent to more than 57.0 percent, largely determined by higher versus lower eligibility threshold levels, respectively (39). For instance, when Part D plan sponsors only required the presence of two chronic conditions, enrollment was 16.4 percent (39). When this threshold was set at 3 chronic conditions, enrollment was lower at 9.2 percent (39). Similarly, when plan sponsors allowed the use of any Part D drug, enrollment was 12.7 percent compared to an enrollment of 4.4 percent when the use of drugs from specific medication classes were required (39).
With the option to refine targeting criteria, plan sponsors often set more stringent thresholds, likely driven by the incentives to limit access stemming from the absence of reimbursement for MTM services under Part D, as well as the disincentive to promote access linked to quantity-focused measures like the CMR completion rate assessed by CMS (39–42). This had led to only 8% of beneficiaries being eligible for MTM services in 2020 (40).
To partially address these limitations, CMS issued a final rule in April 2024, updating eligibility and limiting plan sponsors’ flexibility in allowable targeting criteria (38). This policy, effective from January 2025, is anticipated to nearly double MTM eligibility from 3.6 million to 7.1 million beneficiaries (43). Under the new guidance, beneficiaries must meet a minimum threshold of 2 to 3 of all 10 CMS-defined chronic diseases (Alzheimer’s disease, bone disease-arthritis, diabetes, heart failure, dyslipidemia, respiratory disease, hypertension, end-stage renal disease, mental health, and HIV/AIDS), fill a minimum of 2 to 8 covered Part D maintenance drugs, and anticipate incurring a designated annual drug cost based on the average for 8 generic covered Part D drugs, a substantial reduction in cost thresholds compared to previous years (40, 43, 44).
As health policy changes directly impact the MTM program, future research should focus on how changes such as these effect beneficiaries’ eligibility and likelihood of receiving MTM services. Additionally, research opportunities remain to determine optimal eligibility criteria to more appropriately identify beneficiaries, namely older adults, who could benefit from MTM services.
2.1.2 Health care system
Factors related to the health care system itself should also be considered within the ABM framework to fully understand service utilization as it pertains to environmental influences (34). From how healthcare systems are organized (or disorganized) to the presence or absence of specific provider types and facilities, the healthcare environment contextualizes health services use (33, 34). The U.S. healthcare system, often characterized as fragmented, is typically operated in silos where physicians are not accustomed to providing coordinated and collaborative care (45–48).
Not unexpectedly, MTM providers and prescribers frequently experience limited care coordination, which hinders the uptake and diminishes potential benefits of the MTM programs (45, 46). A key challenge is the lack of direct communication and collaboration between prescribers and MTM practitioners, typically pharmacists, who perform the CMR (49–51). These practitioners often work for community pharmacies, MTM vendors, or Medicare Part D plan sponsors, rather than within the prescribers’ practice (49–52). This separation limits the integration and effectiveness of MTM services, as pharmacist’s recommendations may not be seamlessly communicated to or implemented by the prescriber (53, 54).
Opportunities to improve utilization of MTM services are through Collaborative Practice Agreements (CPAs), which allow pharmacists to adjust medication regimens and order relevant tests to monitor medication use and ensure safety. CPAs vary state by state in terms of scope and protocol but afford ways to reduce fragmentation and burden (55, 56). Without CPAs, the burden may fall on patients to communicate MTM recommendations to their prescribers, further complicating the care process (48, 55).
Limited care coordination and sharing of medical information between prescribers and MTM practitioners hampers the personalized nature of MTM care (53, 54). Without stronger collaboration and trust between patients, MTM practitioners, and prescribers, the full potential of MTM services is unlikely to be achieved (47, 48). Novel approaches are needed to bridge this communication gap, and further research is essential to explore effective strategies to overcome barriers at multiple levels and foster collaboration between all key stakeholders (49, 58).
2.2 Population characteristics
2.2.1 Predisposing characteristics
According to the ABM, predisposing characteristics form the foundation for differences in an individual’s ability and propensity to utilize health care services (34, 35). Predisposing characteristics are more commonly thought of today as sociodemographic variables like age, education, race and ethnicity (59). Andersen described inequitable access to care as care that was determined based on such predisposing factors (34).
Studies have shown that, despite some improvements, disparities in access to and utilization of MTM services among racial and ethnic subgroups have persisted since the inception of the program (49). While the eligibility criteria, which has been based on number of medications, chronic diseases, Part D drug expenditure, identify at-risk beneficiaries many individuals at high risk for MTPs, they fail to account for differences in healthcare utilization across racial and ethnic subgroups with the same medical conditions (60–64). Studies have found that minorities, such as Black and Hispanic beneficiaries, are less likely to meet Medicare’s minimum thresholds for MTM eligibility compared to White beneficiaries (65, 66). Asian, Hispanic, and Native American beneficiaries are less likely to receive a CMR after being offered the service compared to White beneficiaries (65, 67, 68). Additionally, it typically takes longer for Black, Asian, and Hispanic beneficiaries to receive a CMR after enrolling in MTM services compared to White beneficiaries (65).
Addressing these disparities requires a multifaceted approach that may include refining eligibility criteria, understanding and overcoming barriers to receiving services, such as health literacy and language proficiency, specific to cultural preferences, and focusing on the needs of underserved communities (40, 69–71).
2.2.2 Enabling resources
The ABM describes enabling resources as both community-level and individual-level factors that influence the likelihood of service utilization (34). Community-level factors refer to the presence of health professionals and facilities, which can vary significantly between communities (33). This variation directly impacts the likelihood of service utilization. Previous studies have noted that individuals residing in areas with limited primary care resources or healthcare professional shortages face significant challenges in accessing MTM services, reducing their likelihood of participation even when eligible (70, 72). As Part D MTM services have transitioned from face-to-face interactions to being predominantly delivered via telephone or other electronic means (51, 52), the traditional understanding of community-level resources may be evolving, particularly in today’s telehealth landscape (73, 74).
Individual-level factors include indicators of economic status, such as Medicare-Medicaid dual eligibility, food insecurity or low-income subsidy (LIS) status (59). These factors can either promote or prohibit individuals’ likelihood to receive health care services (34). Studies have reported associations between these economic indicators and both MTM eligibility and CMR completion (59, 68, 75). Beneficiaries with LIS or those who are Medicare-Medicaid dual-eligible often represent a vulnerable population, facing higher healthcare costs, greater medication utilization, and increased rates of high-risk medication use (76). They also demonstrate lower persistence and adherence compared to non-LIS or dual-eligible beneficiaries (76). Previous literature highlights challenges in engaging LIS and Medicare-Medicaid dual enrollees, including lower rates of MTM service uptake and higher rates of opting out of services (68, 75).
Racial and ethnic minorities, who are disproportionally affected by low-income status in the US, often face additional barriers accessing their healthcare needs, despite targeted support from CMS policy (68, 77, 78). To address these challenges, further efforts should explore how MTM providers can collaborate with social work professionals and community health workers to tackle broader social determinants of health, such as food insecurity, job opportunities, and transportation barriers for physician visits (78, 79). Additionally, the ABM can be used to further understand the impact of enabling factors on the utilization and effect of MTM services.
2.2.3 Need
Perceived need plays an important role in the use of health care services (33). How individuals view their own health, their functional state, and how they experience symptoms and complications influence whether they view their condition as requiring assistance or guidance from healthcare professionals (33, 34). The ABM focuses this concept of need based on a patient-centric approach for help-seeking rather than based on a health professional’s determination of need (34). Additionally, the ABM also recognizes the influence of environmental and predisposing factors on the perception of need (34).
Part D MTM eligibility and targeting criteria have primarily addressed “objective” needs, such as numbers of chronic conditions and medication, and drug spending for at risk beneficiaries (40, 43). However, these criteria overlook “subjective” needs, such as patients’ perceptions of their health status (80). Previous literature has highlighted that patients’ perceptions of their health status significantly influence their interest in receiving MTM services (81). For example, patients with a higher number of prescribed medications or concerns about potential adverse effects are more likely to seek a CMR with a pharmacist (81). Beneficiaries have reported that MTM services are particularly valuable during clinically significant moments, such as when starting new medications, adjusting existing medications, or following recent health changes and/or transitions in care (77).
Low participation in Part D MTM services may be due to patients’ lack of awareness about their eligibility, a perception that they do not need the service, or low expectations of its value (82). Novel strategic patient outreach targeting MTM-eligible populations could significantly benefit those currently unaware or uncertain about MTM services (49). Studies have shown that patients are motivated to participate in MTM for reasons such as gaining better understanding of their medication therapy, reviewing the efficacy of their medications, potential cost savings, and benefiting from the pharmacist’s expertise (20, 83). They also value personalized information about their medications (83). Targeted education initiatives, such as presentations in patient-friendly language to local older adult community groups or marketing by community pharmacies that provide MTM services, could further boost awareness, understanding, and motivation for MTM engagement (58, 81).
2.3 Health services use and outcomes
2.3.1 Use of health services
The original ABM focused solely on utilization as the main outcome but was later expanded to include important outcomes of care like patient satisfaction and effectiveness (34, 35). While the literature described here for Part D MTM reports factors individually related to their impact on MTM participation, this may be the greatest opportunity for further research as there is a lack of consensus regarding influences on who ultimately utilizes MTM services and the effectiveness of MTM services (84).
2.3.2 Effectiveness
For example, systematic reviews have indicated that MTM reduced some MTPs, such as inappropriate use, nonadherence, and medication costs, but the heterogeneity of the studies reviewed was a concern limiting the ability to make confident conclusions about the impact of MTM services (26, 29, 85). Furthermore, a five-year demonstration (2017–2021) evaluated whether flexibility in MTM program design along with payment incentives for Part D sponsors could improve therapeutic outcomes and reduce Medicare expenditures (86). The model did not show a significant overall impact on net Medicare Parts A and B expenditures or intermediate measures of medication use (e.g., adherence) (77). It did, however, illustrate a different approach to MTM, with some services designed around a beneficiary’s unique needs such as during transitions in care, a time for heightened medication-related concerns (77).
3 Discussion
Applying the ABM allows for a critical assessment of the factors that affect MTM service utilization and related impact on outcomes (34). These insights have the potential to inform research and policies that aim at improving the MTM program, which can serve as a global model for enhancing medication safety among older adults. While the ABM highlights several key factors, it also recognizes the need for further consideration of additional elements (34). This review provides a foundation for selecting variables associated with MTM service use, with Figure 1 serving as a starting point for identifying the factors that influence this utilization according to the ABM.
The ABM emphasizes the importance of understanding what matters to the patient (34). Patient-reported outcome or experience measures could be used as outcomes in the ABM framework (34). Patient-reported outcomes are directly reported by patients using validated tools, allowing for self-assessment of health-related quality of life, functional status, symptom and symptom burden, health behaviors, or experience with care (25, 87). Patient experience measures focus on aspects of care such as communication with clinicians, responsiveness of staff, ease of scheduling an appointment, spending enough time with the patient, and explaining things in ways the patient can understand (87, 88).
The ABM was initially developed in the 1960s to enhance the utilization of healthcare services (34, 35). Although it was established during an era when healthcare costs were less of a concern, disease burden was significantly lower, and society’s relationship with health professionals were quite different compared to today, the ABM remains relevant in the context of the Part D MTM program (34). This program has been underutilized (52), yet as a preventive service, it has the potential to greatly benefit eligible beneficiaries and should be taken advantage of. However, as described previously, equitable access and uptake of this preventive service continue to be challenged.
Gaining a clearer understanding of individuals’ likelihood of participation in the Part D MTM program is one step toward connecting these influences on specific outcomes. It should be recognized that understanding the relationships between the factors and outcomes may lead to implications that have varying degrees of actionability (33). For example, environmental and predisposing factors are often very difficult to change whereas enabling factors and perception of need may be more modifiable.
4 Conclusion
This perspective paper applied the Andersen Behavioral Model for Health Services Use to the Medicare Part D MTM program, which provides a guide for needed research in generating rigorous evidence for program evaluation to inform additional policy changes and to make specific recommendations for interventions to improve the service. The application of this framework seeks to ensure that MTM programs meet the needs of older adults, thereby improving medication safety. In the long term, we hope this framework can be applied not only to the Medicare Part D MTM program within the U.S. healthcare system but also to global programs aimed at improving medication safety by addressing MTPs and optimizing medication use.
Author contributions
Y-HF: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. MC-B: Conceptualization, Writing – original draft, Writing – review & editing. AC: Conceptualization, Writing – original draft, Writing – review & editing. MS: Conceptualization, Writing – original draft, Writing – review & editing. CC: Conceptualization, Writing – original draft, Writing – review & editing. CV: Conceptualization, Writing – original draft, Writing – review & editing. LH: Conceptualization, Writing – original draft, Writing – review & editing. AL: Conceptualization, Writing – original draft, Writing – review & editing. NB: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Coe was supported by the National Institutes of Health National Institute on Aging (K08AG071856). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Semla, TP, Steinman, M, Beizer, J, Brandt, N, Digmann, R, Dombrowski, R, et al. American Geriatrics Society 2023 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. (2023) 71:2052–81. doi: 10.1111/jgs.18372
2. Tuiskula, KA, Kanaan, AO, Warholak, TL, and Nau, DP. Quality & Safety in pharmacy practice. New York, NY: McGraw-hill medical. Am J Pharm Educ. (2010) 75
3. ElDesoky, ES. Pharmacokinetic-pharmacodynamic crisis in the elderly. Am J Ther. (2007) 14:488–98. doi: 10.1097/01.mjt.0000183719.84390.4d
4. Zazzara, MB, Palmer, K, Vetrano, DL, Carfì, A, and Onder, G. Adverse drug reactions in older adults: a narrative review of the literature. Eur Geriatr Med. (2021) 12:463–73. doi: 10.1007/s41999-021-00481-9
5. Classen, DC, Pestotnik, SL, Evans, RS, Lloyd, JF, and Burke, JP. Adverse drug events in hospitalized patients. Excess length of stay, extra costs, and attributable mortality. JAMA. (1997) 277:301–6. doi: 10.1001/jama.1997.03540280039031
6. Budnitz, DS, Lovegrove, MC, Shehab, N, and Richards, CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. (2011) 365:2002–12. doi: 10.1056/NEJMsa1103053
7. Lohman, MC, Cotton, BP, Zagaria, AB, Bao, Y, Greenberg, RL, Fortuna, KL, et al. Hospitalization risk and potentially inappropriate medications among Medicare home health nursing patients. J Gen Intern Med. (2017) 32:1301–8. doi: 10.1007/s11606-017-4157-0
8. Budnitz, DS, Shehab, N, Kegler, SR, and Richards, CL. Medication use leading to emergency department visits for adverse drug events in older adults. Ann Intern Med. (2007) 147:755–65. doi: 10.7326/0003-4819-147-11-200712040-00006
9. Shehab, N, Lovegrove, MC, Geller, AI, Rose, KO, Weidle, NJ, and Budnitz, DS. US emergency department visits for outpatient adverse drug events, 2013-2014. JAMA. (2016) 316:2115–25. doi: 10.1001/jama.2016.16201
10. Fulda, TR, Lyles, A, Pugh, MC, and Christensen, DB. Current status of prospective drug utilization review. J Manag Care Pharm. (2004) 10:433–41. doi: 10.18553/jmcp.2004.10.5.433
11. Harjivan, C, and Lyles, A. Improved medication use in long-term care: building on the consultant pharmacist's drug regimen review. Am J Manag Care. (2002) 8:318–26.
12. World Health Organization. Medication without harm: Policy brief. (2023). Available at: https://iris.who.int/bitstream/handle/10665/376212/9789240062764-eng.pdf?sequence=1. (Accessed August 20, 2024).
13. Centers for Medicare and Medicaid Services. Medication therapy management model. (2024). Available at: https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/MTM (Accessed October 13, 2023).
14. The Law Library of Congress. Medicare prescription drug, improvement, and modernization act of 2003. 1st ed. 108th Cong. (2004). Available at: https://www.congress.gov/bill/108th-congress/house-bill/1 (Accessed October 19,2024).
15. Centers for Medicare and Medicaid Services. What original Medicare covers. (2024). Available at: https://www.medicare.gov/providers-services/original-medicare (Accessed October 19, 2024).
16. Centers of Medicare and Medicaid. Parts of Medicare. (2024). Available at: https://www.medicare.gov/basics/get-started-with-medicare/medicare-basics/parts-of-medicare. (Accessed October 19, 2024).
17. Medicare program; Medicare prescription drug benefit. Final rule. Fed Regist. (2005) 70:4193–585.
18. Bennett, MS, Chater, RW, Croley, KS, Deck, R, Delafuente, JC, Downard, SL, et al. Medication therapy management in pharmacy practice: core elements of an MTM service model (version 2.0). J Am Pharm Assoc. (2003). 2008) 48:341–53. doi: 10.1331/JAPhA.2008.08514
19. Pellegrino, AN, Martin, MT, Tilton, JJ, and Touchette, DR. Medication therapy management services: definitions and outcomes. Drugs. (2009) 69:393–406. doi: 10.2165/00003495-200969040-00001
20. McGivney, MS, Meyer, SM, Duncan-Hewitt, W, Hall, DL, Goode, JV, and Smith, RB. Medication therapy management: its relationship to patient counseling, disease management, and pharmaceutical care. J Am Pharm Assoc. (2003). 47:620–8. doi: 10.1331/JAPhA.2007.06129
21. Rao, P, and Hung, A. Impact of medication therapy management programs on potentially inappropriate medication use in older adults: a systematic review. J Manag Care Spec Pharm. (2024) 30:3–14. doi: 10.18553/jmcp.2024.30.1.03
22. Costello, J, Barras, M, Foot, H, and Cottrell, N. The impact of hospital-based post-discharge pharmacist medication review on patient clinical outcomes: a systematic review. Explor Res Clin Soc Pharm. (2023) 11:100305. doi: 10.1016/j.rcsop.2023.100305
23. de Souza, CM, Cruz-Cazarim, ELC, Boyd, K, Wu, O, and Nunes, AA. Effect of medication therapy management by pharmaceutical care on blood pressure and cardiovascular risk in hypertension: a systematic review, meta-analysis, and meta-regression. Pharmaceuticals. (2023) 16. doi: 10.3390/ph16060845
24. Bloomfield, HE, Greer, N, Linsky, AM, Bolduc, J, Naidl, T, Vardeny, O, et al. Deprescribing for community-dwelling older adults: a systematic review and meta-analysis. J Gen Intern Med. (2020) 35:3323–32. doi: 10.1007/s11606-020-06089-2
25. Cooke, CE, Olshanskaya, S, Lee, M, and Brandt, NJ. Evolution of the comprehensive medication review completion rate for Medicare part D plans: what do the stars tell us? Sr Care Pharm. (2022) 37:357–65. doi: 10.4140/TCP.n.2022.357
26. Marupuru, S, Roether, A, Guimond, AJ, Stanley, C, Pesqueira, T, and Axon, DR. A systematic review of clinical outcomes from pharmacist provided medication therapy management (MTM) among patients with diabetes, hypertension, or dyslipidemia. Healthcare. (2022) 10. doi: 10.3390/healthcare10071207
27. Isetts, BJ, Schondelmeyer, SW, Artz, MB, Lenarz, LA, Heaton, AH, Wadd, WB, et al. Clinical and economic outcomes of medication therapy management services: the Minnesota experience. J Am Pharm Assoc. (2003). 2008) 48:203–14. doi: 10.1331/JAPhA.2008.07108
28. de Oliveira, DR, Brummel, AR, and Miller, DB. Medication therapy management: 10 years of experience in a large integrated health care system. J Manag Care Spec Pharm. (2020) 26:1057–66. doi: 10.18553/jmcp.2020.26.9.1057
29. Viswanathan, M, Kahwati, LC, Golin, CE, Blalock, SJ, Coker-Schwimmer, E, Posey, R, et al. Medication therapy management interventions in outpatient settings: a systematic review and meta-analysis. JAMA Intern Med. (2015) 175:76–87. doi: 10.1001/jamainternmed.2014.5841
30. Wang, J, and Qiao, Y. Historical trend of disparity implications of Medicare MTM eligibility criteria. Res Social Adm Pharm. (2013) 9:758–69. doi: 10.1016/j.sapharm.2012.09.003
31. Wang, J, Mullins, CD, Brown, LM, Shih, YC, Dagogo-Jack, S, Hong, SH, et al. Disparity implications of Medicare eligibility criteria for medication therapy management services. Health Serv Res. (2010) 45:1061–82. doi: 10.1111/j.1475-6773.2010.01118.x
32. Castora-Binkley, M, Hines, L, Vaffis, S, Dhatt, H, Anderson, E, Le, D, et al. It is time for a new comprehensive medication review quality measure. J Manag Care Spec Pharm. (2023) 29:680–4. doi: 10.18553/jmcp.2023.29.6.680
33. Aday, LA, and Andersen, R. A framework for the study of access to medical care. Health Serv Res. (1974) 9:208–20.
34. Andersen, RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. (1995) 36:1–10. doi: 10.2307/2137284
35. Andersen, R, and Newman, JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. (1973) 51:95–124. doi: 10.2307/3349613
36. Code of Federal Regulations. Title 42, public health. CFR § 423.153 (2024). Available at: https://www.ecfr.gov/current/title-42/section-423.153 (Accessed October 16, 2024).
37. Gray, C, Cooke, CE, and Brandt, N. Evolution of the Medicare part D medication therapy management program from inception in 2006 to the present. Am Health Drug Benefits. (2019) 12:243–51.
38. Centers for Medicare & Medicaid Services. Medicare program; contract year 2024 policy and technical changes to the Medicare advantage program, Medicare prescription drug benefit program, Medicare cost plan program, and programs of all-inclusive care for the elderly. Available at: https://www.federalregister.gov/documents/2023/04/12/2023-07115/medicare-program-contract-year-2024-policy-and-technical-changes-to-the-medicare-advantage-program (Accessed July 28, 2024) [
39. Stuart, B, Hendrick, FB, Shen, X, Dai, M, Tom, SE, Dougherty, JS, et al. Eligibility for and enrollment in Medicare part D medication therapy management programs varies by plan sponsor. Health Aff. (2016) 35:1572–80. doi: 10.1377/hlthaff.2016.0258
40. Centers for Medicare & Medicaid Services. Medicare Program. Contract year 2024 policy and technical changes to the Medicare advantage program, Medicare prescription drug benefit program, Medicare cost plan program, Medicare parts a, B, C, and D overpayment provisions of the affordable care act and programs of all-inclusive Care for the Elderly. Health Information Technol Standards Implement Specific. (2022):79452–749.
41. Centers for Medicare and Medicaid Services. CMS Measures Management System. Types of measures. (2024). Available at: https://mmshub.cms.gov/about-quality/new-to-measures/types (Accessed August 18, 2024).
42. Pharmacy Quality Alliance. PQA measure manual: Completion rate for comprehensive medication review (CMR). (2024). Available at: https://www.pqaalliance.org/. (Accessed May 22, 2024).
43. Federal Register. Medicare program; Contract year 2024 policy and technical changes to the medicare advantage program, medicare prescription drug benefit program, medicare cost plan program, and programs of all-inclusive care for the elderly. (2023). Available at: https://www.federalregister.gov/documents/2023/04/12/2023-07115/medicare-program-contract-year-2024-policy-and-technical-changes-to-the-medicare-advantage-program (Accessed October 19, 2024).
44. Centers for Medicare and Medicaid Services. Medicare; contract year 2023 medication therapy management program information and submission instructions. (2022).Available at: https://www.cms.gov/files/document/memo-contract-year-2023-medication-therapy-management-mtm-program-submission-v041522.pdf (Accessed October 19, 2024).
45. McDonald, KM, Sundaram, V, Bravata, DM, Lewis, R, Lin, N, Kraft, SA, et al. Closing the quality gap: A critical analysis of quality improvement strategies (Vol. 7: care coordination). Rockville (MD): gency for Healthcare Research and Quality (US) (2007). Available from: https://www.ncbi.nlm.nih.gov/books/NBK44015/ (Accessed October 19, 2024).
46. Moses, H 3rd, Matheson, DH, Dorsey, ER, George, BP, Sadoff, D, and Yoshimura, S. The anatomy of health care in the United States. JAMA. (2013) 310:1947–63. doi: 10.1001/jama.2013.281425
47. Timmins, L, Kern, LM, Ghosh, A, Urato, C, and Rich, E. Predicting fragmented care: beneficiary, physician, practice, and market characteristics. Med Care. (2022) 60:919–30. doi: 10.1097/MLR.0000000000001786
48. Timmins, L, Kern, LM, O'Malley, AS, Urato, C, Ghosh, A, and Rich, E. Communication gaps persist between primary care and specialist physicians. Ann Fam Med. (2022) 20:343–7. doi: 10.1370/afm.2781
49. Hung, A, Wilson, L, Smith, VA, Pavon, JM, Sloan, CE, Hastings, SN, et al. Comprehensive medication review completion rates and disparities after Medicare star rating measure. JAMA Health Forum. (2024) 5:e240807. doi: 10.1001/jamahealthforum.2024.0807
50. Centers for Medicare and Medicaid Services. Evaluation of the Part D enhanced medication therapy management (MTM) model: Fifth evaluation report. Available at: https://www.cms.gov/priorities/innovation/data-and-reports/2023/mtm-fifth-evalrept (Accessed July 28, 2024).
51. Centers for Medicare and Medicaid Services. (2019) Medicare Part D medication therapy management (MTM) programs and fact sheet summary of 2019 MTM programs. Available at: https://www.hhs.gov/guidance/document/2019-medicare-part-d-medication-therapy-management-mtm-programs-and-fact-sheet-summary-0 (Accessed October 18, 2024).
52. Pestka, DL, Zillich, AJ, Coe, AB, Farris, KB, Adeoye, OA, Snyder, ME, et al. Nationwide estimates of medication therapy management delivery under the Medicare prescription drug benefit. J Am Pharm Assoc. (2003) 60:456–61. doi: 10.1016/j.japh.2019.12.002
53. McGrath, SH, Snyder, ME, Dueñas, GG, Pringle, JL, Smith, RB, and McGivney, MS. Physician perceptions of pharmacist-provided medication therapy management: qualitative analysis. J Am Pharm Assoc. (2003) 50:67–71. doi: 10.1331/JAPhA.2010.08186
54. Lounsbery, JL, Green, CG, Bennett, MS, and Pedersen, CA. Evaluation of pharmacists' barriers to the implementation of medication therapy management services. J Am Pharm Assoc. (2003). 2009) 49:51–8. doi: 10.1331/JAPhA.2009.07158
55. Cernasev, A, Aruru, M, Clark, S, Patel, K, DiPietro, MN, Subramaniam, V, et al. Empowering public health pharmacy practice-moving from collaborative practice agreements to provider status in the U.S. Pharmacy. (2021) 9. doi: 10.3390/pharmacy9010057
56. American Pharmacist Association. Lauren Howel. Collaborative practice now allowed in all 50 states. (2021). Available at: https://www.pharmacist.com/CEO-Blog/collaborative-practice-now-allowed-in-all-50-states#:~:text=Some%20of%20the%20differences%20in,Author:%20Roger%20Selvage (Accessed October 19, 2024).
58. Taylor, AM, Axon, DR, Campbell, P, Fair, MK, Nelson, M, Boesen, K, et al. What patients know about services to help manage chronic diseases and medications: findings from focus groups on medication therapy management. J Manag Care Spec Pharm. (2018) 24:904–10. doi: 10.18553/jmcp.2018.24.9.904
59. World Health Organization. A conceptual framework for action on the social determinants of health. Discussion paper. WHO Document Production Services, Geneva, Switzerland.
60. Gornick, ME, Eggers, PW, Reilly, TW, Mentnech, RM, Fitterman, LK, Kucken, LE, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. (1996) 335:791–9. doi: 10.1056/NEJM199609123351106
61. Gornick, ME. The association of race/socioeconomic status and use of Medicare services. A little-known failure in access to care. Ann N Y Acad Sci. (1999) 896:497–500. doi: 10.1111/j.1749-6632.1999.tb08180.x
62. Gornick, ME. Disparities in Medicare services: potential causes, plausible explanations, and recommendations. Health Care Financ Rev. (2000) 21:23–43.
63. Chen, JY, Diamant, A, Pourat, N, and Kagawa-Singer, M. Racial/ethnic disparities in the use of preventive services among the elderly. Am J Prev Med. (2005) 29:388–95. doi: 10.1016/j.amepre.2005.08.006
64. Hanchate, AD, Dyer, KS, Paasche-Orlow, MK, Banerjee, S, Baker, WE, Lin, M, et al. Disparities in emergency department visits among collocated racial/ethnic Medicare enrollees. Ann Emerg Med. (2019) 73:225–35. doi: 10.1016/j.annemergmed.2018.09.007
65. Allen, A, and Hung, A. Racial and ethnic disparities related to the Medicare part D medication therapy management program. J Manag Care Spec Pharm. (2024) 30:609–16. doi: 10.18553/jmcp.2024.30.6.609
66. Spivey, CA, Qiao, Y, Wang, J, Shih, YT, Wan, JY, Dagogo-Jack, S, et al. Comparative effectiveness of medication therapy management eligibility criteria across racial/ethnic groups. J Am Geriatr Soc. (2019) 67:581–7. doi: 10.1111/jgs.15754
67. Spivey, CA, Wang, J, Qiao, Y, Shih, YT, Wan, JY, Kuhle, J, et al. Racial and ethnic disparities in meeting MTM eligibility criteria based on star ratings compared with the Medicare modernization act. J Manag Care Spec Pharm. (2018) 24:97–107. doi: 10.18553/jmcp.2018.24.2.97
68. Coe, AB, Adeoye-Olatunde, OA, Pestka, DL, Snyder, ME, Zillich, AJ, Farris, KB, et al. Patterns and predictors of older adult Medicare part D beneficiaries' receipt of medication therapy management. Res Social Adm Pharm. (2020) 16:1208–14. doi: 10.1016/j.sapharm.2019.12.007
69. Rasu, RS, Bawa, WA, Suminski, R, Snella, K, and Warady, B. Health literacy impact on national healthcare utilization and expenditure. Int J Health Policy Manag. (2015) 4:747–55. doi: 10.15171/ijhpm.2015.151
70. Lee, M, Zarowitz, BJ, Pellegrin, K, Cooke, CE, Fleming, SP, and Brandt, N. Social determinants predict whether Medicare beneficiaries are offered a comprehensive medication review. Res Social Adm Pharm. (2023) 19:184–8. doi: 10.1016/j.sapharm.2022.09.015
71. Berkman, ND, Sheridan, SL, Donahue, KE, Halpern, DJ, and Crotty, K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. (2011) 155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005
72. GoddRx. Mapping healthcare deserts: 80% of the country lacks adequate access to healthcare. Available at: https://www.goodrx.com/healthcare-access/research/healthcare-deserts-80-percent-of-country-lacks-adequate-healthcare-access (Accessed October 19, 2024).
73. The National Board of Medication Therapy Mangement. Chapter 8: MTM models - telephonic mode. Available at: https://www.nbmtm.org/mtm-reference/mtm-models/. (Accessed October 23, 2024).
74. Urick, BY, Adams, JK, and Bruce, MR. State Telepharmacy policies and pharmacy deserts. JAMA Netw Open. (2023) 6:e2328810-e. doi: 10.1001/jamanetworkopen.2023.28810
75. Chou, J, Pellegrin, K, Cooke, CE, Zarowitz, B, Hanlon, A, Lozano, A, et al. Understanding the socioeconomic and geographical characteristics of beneficiaries receiving a comprehensive medication review. J Manag Care Spec Pharm. (2020) 26:1276–81. doi: 10.18553/jmcp.2020.26.10.1276
76. Priest, J, Buikema, A, Engel-Nitz, NM, Cook, CL, and Cantrell, CR. Quality of care, health care costs, and utilization among Medicare part D enrollees with and without low-income subsidy. Popul Health Manag. (2012) 15:101–12. doi: 10.1089/pop.2011.0008
77. Acumen, LLC and Westat, Inc. Evaluation of the part D enhanced medication therapy management (MTM) model: Fifth evaluation report. (2023). https://www.cms.gov/priorities/innovation/data-and-reports/2023/mtm-fifth-evalrept (Accessed: August 1, 2024).
78. Beech, BM, Ford, C, Thorpe, RJ Jr, Bruce, MA, and Norris, KC. Poverty, racism, and the public health crisis in America. Front Public Health. (2021) 9:699049. doi: 10.3389/fpubh.2021.699049
79. Almodóvar, AS, Ross, E, Nahata, MC, and Bingham, JM. Social needs of dual-enrolled Medicare-Medicaid patients with medication nonadherence in a telehealth medication therapy management program. J Manag Care Spec Pharm. (2023) 29:210–5. doi: 10.18553/jmcp.2023.29.2.210
80. Pharmacy Quality Alliance. Advancing medication therapy management quality measurement. Available at: (https://www.pqaalliance.org/assets/Research/PQA_QuIRC_MTM_Report.pdf).
81. Coe, AB, Farris, KB, Solway, E, Singer, DC, Kirch, M, Kullgren, JT, et al. Predictors of receipt of comprehensive medication reviews in older adults. J Gerontol A Biol Sci Med Sci. (2023) 78:463–9. doi: 10.1093/gerona/glac096
82. Schnur, ES, Adams, AJ, Klepser, DG, Doucette, WR, and Scott, DM. PCMHs, ACOs, and medication management: lessons learned from early research partnerships. J Manag Care Pharm. (2014) 20:201–5. doi: 10.18553/jmcp.2014.20.2.201
83. Garcia, GM, Snyder, ME, McGrath, SH, Smith, RB, and McGivney, MS. Generating demand for pharmacist-provided medication therapy management: identifying patient-preferred marketing strategies. J Am Pharm Assoc. (2003) 49:611–6. doi: 10.1331/JAPhA.2009.08089
84. Donabedian, A. The quality of care. How can it be assessed? JAMA. (1988) 260:1743–8. doi: 10.1001/jama.1988.03410120089033
85. Giberson, S, Yoder, S, and Lee, MP: Improving patient and health system outcomes through advanced pharmacy practice. A report to the U.S. surgeon general, Rockville, MD, Office of the Chief Pharmacist, US public health services. (2011). Available at: https://jcpp.net/wp-content/uploads/2015/09/Improving-Patient-and-Health-System-Outcomes-through-Advanced-Pharmacy-Practice.pdf (Accessed October 19, 2024).
86. Centers for Medicare and Medicaid Services. Part D enhanced medication therapy management model. Available at: https://www.cms.gov/priorities/innovation/innovation-models/enhancedmtm. (Accessed October 24, 2024).
87. Pharmacy Quality Alliance. Patient-reported outcomes: best practices on selection and data collection - final technical report. National Quality Forum (2020). Available at: https://www.qualityforum.org/Publications/2020/09/Patient-Reported_Outcomes__Best_Practices_on_Selection_and_Data_Collection_-_Final_Technical_Report.aspx. (Accessed December 20, 2021).
Keywords: medication safety, chronic disease management, Medicare Part D Medication Therapy Management, Andersen Behavioral Model, access to healthcare, geriatric pharmacotherapy
Citation: Fu Y-H, Castora-Binkley M, Coe AB, Snyder ME, Cooke CE, Vogel CE, Hines L, Lyles A and Brandt N (2024) Applying the Andersen behavioral model to the medication therapy management program: an approach for improving medication safety in older adults. Front. Public Health. 12:1499362. doi: 10.3389/fpubh.2024.1499362
Edited by:
Yen-Ming Huang, National Taiwan University, TaiwanReviewed by:
Bilgen Basgut, Baskent University, TürkiyeHsiu-Ting Chien, National Taiwan University, Taiwan
Matthew Witry, The University of Iowa, United States
Kathleen Fairman, Midwestern University, United States
Copyright © 2024 Fu, Castora-Binkley, Coe, Snyder, Cooke, Vogel, Hines, Lyles and Brandt. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu-Hua Fu, eXUtaHVhLmZ1QHVtYXJ5bGFuZC5lZHU=
 Yu-Hua Fu
Yu-Hua Fu Melissa Castora-Binkley3
Melissa Castora-Binkley3 Nicole Brandt
Nicole Brandt